Abstract
The co-occurrence of posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD) is widely known, yet few studies have examined whether and how AUD symptoms co-occur with PTSD symptom clusters of hypervigilance, avoidance/numbing, and re-experiencing. The purpose of this study was to examine potential overlap between AUD and posttraumatic stress symptomatology, and to characterize the resultant latent classes in terms of demographics, drinking behaviors, parental AUD, and specific traumas experienced (physical violence, sexual violence, and non-assaultive trauma). We hypothesized that classes would be differentiated by type and severity of AUD and PTS symptoms. Drawing from a sample of white and Black participants from the Collaborative Study on the Genetics of Alcoholism (COGA), we examined young adults between the ages of 18–35 who had experienced trauma (N = 2478). A series of LCA models based on the type of trauma experienced, posttraumatic stress symptoms and problematic alcohol use were then fitted to the data. A four-class solution provided the best fit, consisting of a low symptom class (N = 1134), moderate alcohol/low PTS severity (N = 623), mild alcohol/high PTS severity (N = 544), and high symptom severity (N = 177). Higher prevalence of sexual assault was associated with membership in high PTS severity classes, and parent AUD was associated with membership in each class, particularly when the mother or both parents had the disorder. Using person-centered methods such as LCA is a commonsense approach to understanding the heterogeneity of symptoms, trauma types, and individual-level characteristics associated with trauma-exposed individuals and comorbid AUD-PTSD, and our study is one of relatively few to empirically ascertain the co-occurrence of alcohol and PTS symptoms in a high-risk family sample.
Keywords: Alcohol use disorder, Posttraumatic stress disorder, Latent class analysis, Trauma, COGA
1. Introduction
The co-occurrence of alcohol use disorder (AUD) and posttraumatic stress disorder (PTSD) has been extensively documented (Blanco et al., 2013; Goldstein et al., 2016; Kessler et al., 2005). Parent AUD may explain a great deal of the shared etiology between AUD and PTSD through inherited factors (Bowers and Yehuda, 2016; Buss et al., 2017; Heath et al., 1997; Merikangas et al., 1998; Nelson et al., 2004) as well as environmental influences (Bucholz et al., 2017; Yoon et al., 2013). Studies have shown that, in addition to elevating offspring risk for problematic drinking and/or developing AUD, having one or more parents with AUD is associated with higher odds of experiencing childhood physical and sexual violence (Anda et al., 2006; Bender et al., 2020). The offspring of individuals diagnosed with AUD thus represent a subpopulation at increased risk for not only trauma exposure but also the development of both AUD and PTSD.
In recent years, researchers have employed person-centered analytic methods such as latent class analysis (LCA) to examine the underlying structures of many psychiatric and substance use disorders, which have uncovered distinct subtypes in both AUD and PTSD as well as comorbid AUD-PTSD (Kessler et al., 2005; Olino et al., 2012; Vaidyanathan et al., 2011). Another body of scholarship has focused on symptom clusters within AUD (Bucholz et al., 1996; Moss et al., 2007) as well as PTSD (Breslau et al., 2005; Forbes et al., 2010). Studies have revealed commonalities between the expression of symptoms of both disorders as well as their co-occurrence which include dissociative subtypes among PTSD sufferers (Blevins et al., 2014; Wolf et al., 2012), and internalizing versus externalizing symptom profiles among those with comorbid AUD-PTSD (Forbes et al., 2010; Kessler et al., 2005; Olino et al., 2012). Generally, evidence from these and other studies of the two disorders indicates specific subtypes of individuals distinguished by those largely unaffected, those with internalizing symptoms or behaviors, those with externalizing symptoms or behaviors, and a combination internalizing-externalizing group.
However, few studies have examined potentially subclinical alcohol misuse and posttraumatic stress (PTS) symptomology. Notable exceptions include Shankman and colleagues’ (2009) longitudinal study of subthreshold psychiatric conditions, which found that subclinical alcohol use (that is, the presence of multiple symptoms falling slightly below the diagnostic threshold) was significantly associated with the development PTSD over a 15-year period among 1505 young adults. Another study, drawing data from two community samples, differentiated groups of trauma-exposed individuals by mean number and type of PTS symptoms—those with pervasive disturbance, those with intermediate disturbance, and those with no disturbance (Breslau et al., 2005). The main differentiator between the pervasive and intermediate disturbance groups was a greater mean number of numbing and avoidance symptoms among those with pervasive disturbance (Breslau et al., 2005). An examination of the alcohol use patterns and PTS symptomology among young adults with lifetime trauma exposure would enable us to ascertain whether and how alcohol and trauma symptoms cluster together in a sample of trauma-exposed young adults, and furthermore to explore associations of trauma type and parent AUD status with these frequently co-occurring experiences. Where symptoms do not merit a full diagnosis, evidence suggests they could nonetheless represent a risk for the eventual development of each disorder (Shankman et al., 2009) or at least cause significant emotional distress, leading to poor quality of life and impaired functioning. Understanding whether and how alcohol and PTS symptoms co-occur may thus illuminate possibilities for the early detection of disorders and implications for treatment based on class membership probabilities.
The purpose of this study was, therefore, to examine the clustering of all 11 AUD criteria and PTSD symptom clusters B (re-experiencing), C (avoidance/numbing), and D (hyperarousal), and to characterize the resultant latent classes in terms of demographics, drinking behaviors, and specific traumas experienced—e.g., physical violence, sexual violence, and non-assaultive trauma. We hypothesized that classes would be differentiated by type and severity of AUD symptoms as well as type and severity of PTS symptoms. We hypothesized that the high alcohol/low PTS severity group would be mostly male and comprised of physical trauma victims (due to males’ higher likelihood of physical assault victimization than females in the data source used for this analysis [Bender et al., 2020]), lower prevalence of PTSD compared to females (Tolin & Foa, 2006), and greater propensity to use alcohol as an enhancing mechanism (Lehavot et al., 2014)—that is, problematic alcohol use as an externalizing behavior. We hypothesized that there would be a mostly female high PTS/low alcohol group comprised of sexual trauma and non-assaultive trauma victims (due to greater number of females experiencing both sexual assault [Elliott, Mok & Briere, 2004], higher prevalence of PTSD than males [Liberzon et al., 2017; Tolin & Foa, 2006]), and greater propensity to use alcohol as a coping mechanism (Lehavot et al., 2014)—characterized as an internalizing behavior in our study.
Secondly, we examined associations of trauma types and parental AUD status with the latent classes of AUD and PTSD symptom clusters, using multinomial logistic regression. This model enabled us to determine the association of mother-only, father-only, or both-parent AUD with the class profiles. For the regressions, we hypothesized that the presence of one or more parents with AUD would be significantly, positively associated with experiencing any trauma, and that this relationship would be particularly strong for family configurations in which the mother was affected by AUD, in keeping with a previous analysis of these data (e.g. Bender et al., 2020).
2. Methods
2.1. Sample
The Collaborative Study on the Genetics of Alcoholism (COGA), from which the data for this analysis was drawn, is a multi-site investigation of the genetic factors underlying familial transmission of alcohol use disorder and related phenotypes that began in 1989. Descriptions of COGA’s complex methodology have been fully described elsewhere, notably by Nurnberger et al. (2004) and Reich et al. (1998). Briefly, the first phase of COGA recruited families of individuals receiving treatment for AUD at inpatient and outpatient facilities at six sites1 across the United States with the only major restriction for comorbid intravenous drug dependence. Researchers interviewed first-degree relatives of these probands with a highly reliable tool, the Semi-Structured Assessment for the Genetics of Alcoholism [SSAGA] (Bucholz et al., 1994; Hesselbrock et al., 1999). A set of comparison families was also drawn from the same communities as the families recruited through an alcoholic proband. Since 2004, adolescent and young adult relatives in the original families of the subjects (e.g., offspring, grandchildren, nieces and nephews, as well as offspring of comparison families) who had at least one parent interviewed at earlier phases of the COGA study have been recruited into the prospective study. Every two years, subjects undergo a comprehensive assessment using an updated form of the SSAGA interview that includes lifetime measures of psychiatric diagnoses (including PTSD) as well as histories of alcohol, tobacco, and illicit drug use and problems to obtain DSM-IV and DSM-5 (for substances) diagnoses (Bucholz et al., 2017). Data for these analyses were derived from the September 2018 harvest, master file 93, and included 3,691 individuals aged to 12 to 35.
For the purposes of the current study, we selected a sub-sample of the prospective population comprised of subjects who were 18 or older at the time of their most recent interview, had ever had one full drink of alcohol, and who had experienced at least one potentially traumatic event (PTE) per Criterion A for DSM-IV PTSD (N = 2,478). A PTE is defined as the experience or witnessing of an event(s) that involved actual or threatened death or serious injury, and which caused intense fear, helplessness, or horror (American Psychiatric Association, 2000). Conditioning subject inclusion on ever experiencing a PTE and ever drinking a full drink of alcohol in one’s lifetime was necessary because each are qualifiers for PTSD and AUD assessment, respectively. Additionally, due to the low number of individuals of other race/ethnic backgrounds, and correspondingly low power to detect inter-group differences, only individuals self-identifying as white (European American) or Black (African American) were included in these analyses (these individuals comprised 92% of the eligible group).
2.2. Instruments and variables
The SSAGA-IV interview enables researchers to assess for lifetime DSM-IV Alcohol Abuse, Alcohol Dependence, and PTSD as well as the ICD-10 equivalents. An algorithm harmonizing DSM-IV alcohol abuse and dependence with DSM-5 AUD enables researchers to apply the current diagnostic criteria to participants. The 11 symptoms for DSM-5 AUD were included in the LCA, with cutoff points of mild (two symptoms), moderate (three to six symptoms), and severe (seven or more symptoms) used to determine severity of the disorder (American Psychiatric Association, 2013). Additionally, information such as the age at which subjects first tried a full drink of an alcoholic beverage, age at which they first got drunk, age at which they first met criteria for AUD (if at all), and current AUD status were included for descriptive purposes.
The SSAGA-IV assesses for PTSD using a modified version of the Traumatic Life Events Questionnaire (Kubany et al., 2000). Assessment is conditional, meaning an interviewee must endorse one or more traumatic experiences on the checklist. These experiences encapsulate a variety of experiences that are exceedingly distressing, terrifying, or life-threatening, and which we have sorted into categories representing physical violence, sexual violence, and non-assaultive trauma exposure. We defined these three broad categories as follows: physical assault means subjects had been shot, stabbed, mugged or threatened with a weapon, tortured, or held captive. Sexual assault meant unwanted penetration or touching by an object or body part. Non-assaultive trauma included events such as witnessing the death of another person, having a motor vehicle accident, experiencing natural disaster, being poisoned with dioxin, diagnosis with a life-threatening illness, experiencing a life-threatening injury, sudden death of a close family member, friend or relative, unexpectedly discovering a dead body, learning of a traumatic event that happened to another person, or experiencing any other event that the subject found especially terrifying or life-threatening. If Criterion A (trauma exposure) was met, subjects were included in the analysis.
Criterion B (re-experiencing) includes a set of five symptoms that indicate trauma: a persistent re-experiencing of the trauma through flashbacks, night terrors, intrusive thoughts, and/or intense distress, one or more of which must be met to proceed with further assessment. Criterion C (numbing) involves the persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness. Three or more of Criterion C’s seven symptoms must be endorsed to proceed with assessment. Criterion D (hyperarousal) involves experiencing two or more symptoms out of five of increased arousal, such as difficulty sleeping, irritability or outbursts of anger, difficulty concentrating, hypervigilance, and an exaggerated startle response. All three criteria must be met, in addition to the duration of symptoms lasting one month or longer, for the subject to qualify for a diagnosis of PTSD.
The DSM-5 has revised the diagnostic criteria by increasing the number of overall symptoms from 17 to 20 and adding a fourth symptom cluster which essentially separated the avoidance and numbing symptoms into two separate groups (Pai, Suris & North, 2017). However, it was not possible to apply DSM-5 criteria to the PTSD section in SSAGA-IV; therefore we use and report the DSM-IV post-traumatic stress and PTSD criteria in this study.
Parent alcohol information was derived from reports by the parent (s) themselves or a first-degree relative and linked to offspring via a unique family identifier. At least one parent of a subject interviewed in COGA’s prospective wave would have been assessed for AUD during an earlier phase of the COGA study. Dummy variables representing biological mother-only AUD (father unaffected), biological father-only AUD (mother unaffected), and both biological parents affected by AUD were created, using families with no parental AUD as the referent. We also included dummy variables where parent alcohol information was missing, diagnostically subthreshold, or incomplete as covariates in the analysis.
2.3. Data analysis
Individual-level data from each of the seven interview waves that comprise the prospective study were combined, creating one dataset in which subjects’ alcohol and posttraumatic stress history, and AUD and/or PTSD diagnoses were coded positive if a participant reported experiencing them at any interview. The dataset also included information on DSM-IV qualifying PTEs during the interview wave in which they were first reported as well as demographics at each subject’s most recent interview. After running descriptive statistics on the sample’s characteristics and bivariate tests between the alcohol and posttraumatic stress variables of interest, the 11 symptoms used to generate a diagnosis of DSM-5 AUD and the three clusters of symptoms (re-experiencing, numbing, and hyperarousal) used to determine DSM-IV PTSD were fitted to a series of LCA models with two through six class solutions. LCA is a data reduction technique that aims to empirically categorize typologies from a set of observed, discrete variables (McCutcheon, 1987). A multinomial logistic regression, adjusted for age, sex, race, household income, current drinking status, and familial clustering, examined associations of the latent classes with specific traumas and parent AUD status. All analyses were performed in SAS software, version 9.4 (SAS Institute, 2015), using a macro for LCA developed by Lanza et al. (2015).
3. Results
Table 1 provides overall descriptive information on the sample, which included 2,478 individuals between the ages of 18–35 (Mean age at most recent interview: 24.5, Std. Dev.: 4.3) ever exposed to trauma who also endorsed ever drinking at least one full drink of alcohol. Nearly everyone in the sample had experienced at least one non-assaultive form of trauma (97.7%), with physical assault being the second most common reported trauma type, endorsed by 36.7% of the sample. Approximately 17% had experienced sexual assault, and 7.3% (a total of 182 individuals) had experienced all three trauma types—non-assaultive trauma, physical assault, and sexual assault. A larger proportion of the sample met criteria for AUD (35.5%) than PTSD (9.6%). Slightly under two-thirds of the sample (61.9%) had at least one parent who had been diagnosed with AUD during their lifetime.
Table 1.
Sample Description of Young Adult Participants Exposed to Trauma (N = 2478).
| Frequency | Percent of sample | |
|---|---|---|
| Sex | ||
| Male | 1180 | 47.6 |
| Female | 1298 | 52.4 |
| Race | ||
| Black | 780 | 31.5 |
| White | 780 | 68.5 |
| Age at Last Interview | ||
| Mean, Standard deviation | 24.6, Std. Dev (SD) = 4.3 | |
| Range | 18–35 | |
| Annual Income at Last Interview | ||
| Less than $29,999 | 924 | 37.4 |
| $30,000 – $49,999 | 332 | 15.5 |
| $50,000 – $74,999 | 659 | 26.6 |
| Less than $29,999 | 559 | 22.6 |
| Highest Education Completed | ||
| < High school | 295 | 11.9 |
| High school/GED | 256 | 10.3 |
| 2–3 years college | 539 | 21.8 |
| College graduate | 930 | 37.5 |
| Post-graduate degre | 548 | 18.5 |
| Experienced physical assault | 909 | 36.7 |
| Experienced sexual assault | 420 | 16.9 |
| Experienced non-assaultive trauma | 2422 | 97.7 |
| Endorsed PTSD Cluster B (Re-experiencing) Sx | 796 | 32.1 |
| Mean number Cluster B (Re-experiencing) Sxa | 1.0, SD = 1.6 | |
| Range | 0–5 | |
| Endorsed PTSD Cluster C (Numbing) Sx | 491 | 19.8 |
| Mean number Cluster C (Numbing) Sxb | 1.6, SD = 2.2 | |
| Range | 0–7 | |
| Endorsed PTSD Cluster D (Hyperarousal) Sx | 547 | 22.1 |
| Mean number Cluster D (Hyperarousal) Sxc | 0.9, SD = 1.5 | |
| Range | 0–5 | |
| Met criteria for lifetime PTSD | 238 | 9.6 |
| Endorsed any AUD Sx | 1398 | 56.4 |
| Met criteria for lifetime AUD | 881 | 35.6 |
| Parent Alcohol Use Disorder | ||
| Mother only AUD | 413 | 16.7 |
| Father only AUD | 615 | 24.8 |
| Both parents AUD | 505 | 20.4 |
| Parent AUD info missing | 175 | 7.1 |
Among those endorsing any Cluster B (Re-experiencing) symptoms.
Among those endorsing any Cluster C (Numbing) symptoms.
Among those endorsing any Cluster D (Hyperarousal) symptoms.
A four-class solution provided the most parsimonious, informative, and readily interpreted fit to the data (see Table 2 for model fit statistics). Although indicators of good model fit (e.g. AIC, BIC) decreased as more classes were included, for solutions with more than four classes, some of the class prevalences were very low (two classes ≤ 5% in the five- and six-class solutions), precluding meaningful interpretation. Therefore a four-class solution was chosen. Fig. 1 provides a graphic overview of the LCA results. Class 1, or the “lowest severity” class, was the largest at (n = 1134, 44% of sample) and included low to moderate endorsement on all alcohol and PTS symptoms (cutoff: endorsement probability [EP] < 0.60). Across all classes, the most commonly endorsed alcohol symptoms were those reflective of symptom 1 (alcohol is taken in larger quantities and over a longer period of time than intended), symptom 2 (more than once tried to cut back on drinking but could not), symptom 8 (more than once got into situations after drinking that increased chances of getting hurt) and 10 (had to drink more to achieve the desired effect). The second-largest class (n = 623, 26%) was characterized by moderate endorsement of the majority of alcohol symptoms coupled with low PTS symptoms. A third class consisted of low alcohol and high PTS symptoms (n = 544, 23%), while the fourth and most severe class (n = 177, 7%) was characterized by uniformly high endorsement of most alcohol and all PTS symptoms.
Table 2.
Model fit statistics and latent class of individuals exposed to trauma and their posttraumatic stress and alcohol use symptoms.
| Classes | G-squared | Log-likelihood | AIC | BIC | Entropy |
|---|---|---|---|---|---|
| 2 | 6492.6 | −13188.6 | 6550.6 | 6719.2 | 0.9 |
| 3 | 3741.5 | −11813.0 | 3829.5 | 4085.4 | 0.9 |
| 4 | 2570.9 | −11227.8 | 2688.9 | 3032.0 | 0.9 |
| 5 | 2209.6 | −11047.0 | 2357.6 | 2357.6 | 0.9 |
| 6 | 1858.9 | −10871.8 | 2036.9 | 2554.5 | 0.9 |
Fig. 1.
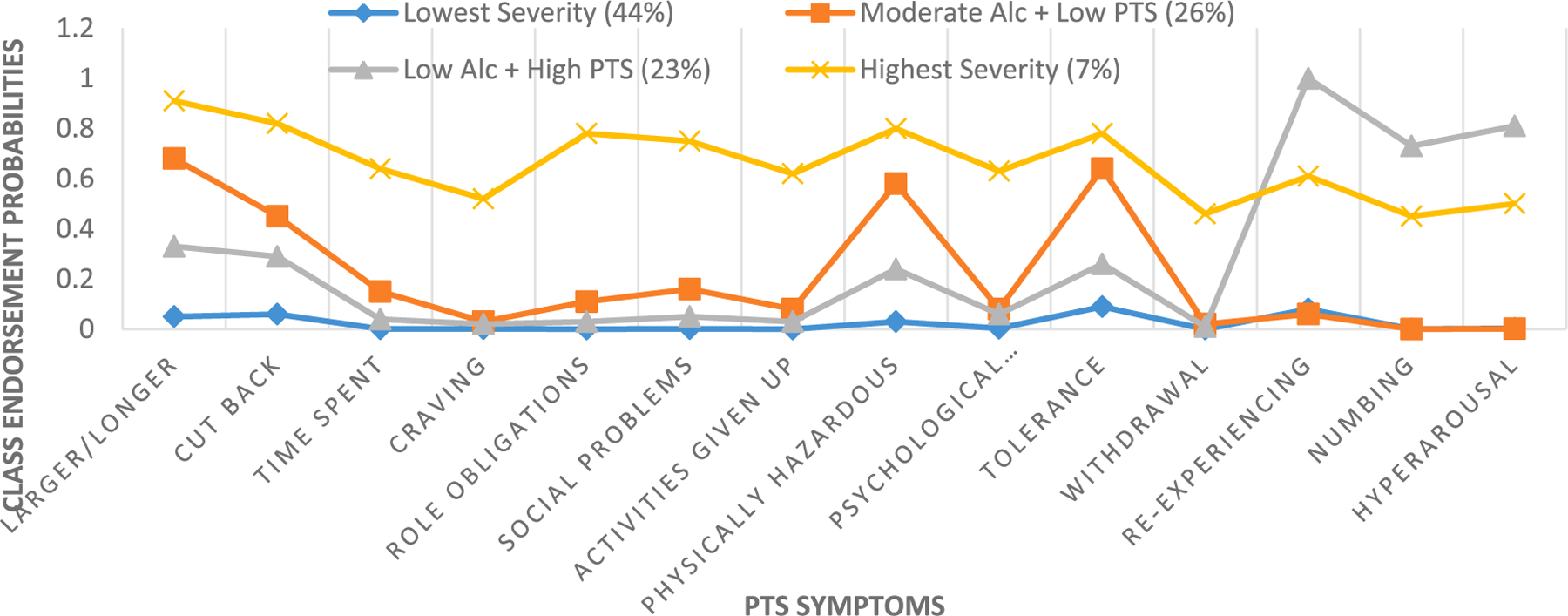
Latent classes of alcohol and posttraumatic stress symptomology. Note: Variables displayed from left to right are AUD symptoms 1–11, abbreviated to fit within the figure. Regarding PTS symptoms Cluster B refers to “re-experiencing” symptoms; Cluster C refers to “numbing” symptoms; Cluster D refers to “hyperarousal” symptoms.
The proportion of membership in each class according to sex, race, trauma type, and alcohol use characteristics is described in Table 3. Class 2, “Moderate alcohol and low PTS” (N = 623), characterized by moderate alcohol and mild PTS severity, consisted mostly of males (61.8%) and Whites (78.8%), with a comparatively low proportion of sexual assault (11.2%). Class 3, “Low alcohol and high PTS” (N = 544), on the other hand, consisted of majority females (62.8%) and a higher proportion of African Americans (41.2%), as well as a higher percentage of physical and sexual assault. Additionally, Class 3 had the highest proportion of individuals whose mother had AUD (21.3%). The smallest class, Class 4, “Highest severity” (N = 177), was almost evenly divided between males and females and was majority White (82.5%). This final and most severe class consisted of a high proportion of individuals who had experienced all forms of trauma, initiated drinking earlier than those in other groups, and came from families where the father or both parents had AUD (Table 4).
Table 3.
Class characteristics (sex, race, age, alcohol and trauma).
| Class 1 : Lowest Symptom | Class 2 : Moderate Alcohol + Mild PTS | Class 3 : Mild Alcohol + High PTS | Class 4 : Highest Symptom | |
|---|---|---|---|---|
| Severity | Severity | Severity | Severity | |
| N = 1134 | N = 623 | N = 544 | N = 177 | |
| Male, % | 44.6 | 61.8 | 37.1 | 49.2 |
| Female, % | 55.4 | 38.2 | 62.9 | 50.9 |
| Black, % | 34.7 | 21.2 | 41.2 | 17.5 |
| White, % | 65.3 | 78.8 | 58.8 | 82.5 |
| Experienced physical assault, % | 25.9 | 39.3 | 48.5 | 59.9 |
| Age first physical assault, Mean (SD) | 15.1 (4.8) | 15.9 (4.4) | 15.2 (5.0) | 15.6 (4.0) |
| Experienced sexual assault, % | 9.5 | 11.2 | 33.5 | 33.9 |
| Age first sexual assault, Mean (SD) | 11.8 (5.7) | 11.7 (5.9) | 11.9 (5.4) | 12.6 (5.1) |
| Experienced non-assaultive trauma, % | 97.6 | 97.1 | 98.4 | 98.9 |
| Age first non-assaultive trauma, Mean (SD) | 12.9 (5.5) | 14.0 (5.4) | 13.3 (5.5) | 13.9 (5.6) |
| Met PTSD diagnosis criteria, % | 0 | 0 | 34.0 | 29.9 |
| Age first drink, Mean (SD) | 16.7 (2.5) | 15.0 (2.2) | 15.9 (2.8) | 13.9 (2.3) |
| Age first got drunk, Mean (SD) | 17.7 (2.4) | 15.9 (2.1) | 17.2 (2.6) | 15.1 (2.2) |
| Met AUD diagnosis criteria, % | 0.09 | 82.2 | 35.1 | 100.0 |
| Age first met AUD criteria, Mean (SD) | 22.0 (–)a | 18.7 (2.7) | 19.8 (2.7) | 17.5 (3.1) |
| Mother AUD | 14.7 | 17.2 | 21.3 | 13.6 |
| Father AUD | 23.3 | 24.6 | 25.4 | 33.9 |
| Both parents AUD | 15.4 | 25.2 | 20.0 | 36.7 |
Only 1 person met these criteria.
Table 4.
Associations of trauma types and parent alcohol use disorder with latent class membership.
| Class 1: Low Symptom | Class 2: Moderate Alcohol + Low PTS | Class 3: Low Alcohol + High PTS | Class 4: High Symptom | |
|---|---|---|---|---|
| Severity | Severity | Severity | Severity | |
| Odds Ratios, 95% Confidence Intervals for Class Membership Based on Condition | ||||
| Sex (M v. F) | 1.0 | 1.7 (1.3–2.2)* | 0.7 (0.5–0.9)* | 1.1 (0.7–1.6)* |
| Race (B v. W) | 1.0 | 0.8 (0.6–1.1) | 1.5 (1.1–1.9)* | 0.6 (0.4–1.0)* |
| Physical Assault | 1.0 | 1.2 (0.9–1.7) | 2.5 (1.9–3.3)* | 3.0 (2.0–4.6)* |
| Sexual Assault | 1.0 | 1.2 (0.8–1.9) | 4.4 (3.1–6.2)* | 3.7 (2.2–6.2)* |
| Non-assaultive Trauma | 1.0 | 0.9 (0.4–1.9) | 2.4 (1.0–5.6)* | 4.0 (0.8–19.6) |
| Mother AUD | 1.0 | 1.7 (1.1–2.6)* | 1.7 (1.2–2.6)* | 2.1 (1.1–4.5)* |
| Father AUD | 1.0 | 1.0 (0.7–1.4) | 1.3 (0.9–1.8) | 2.7 (1.5–5.0)* |
| Both parents AUD | 1.0 | 1.4 (0.9–2.0) | 1.5 (1.0–2.3)* | 3.6 (1.9–6.7)* |
Models adjusted for age at last interview, household income at most recent interview, missing or complete information on parent alcohol status, offspring current drink status, and familial clustering.
p < .05.
There were some between-group differences by sex, race, and rate of lifetime AUD and PTSD diagnoses (see Supplemental Table 1). Compared to Class 1, which contained individuals with the least severe symptom profiles, individuals in Classes 2, 3, and 4 had between one and four higher odds of experiencing physical and sexual assault. The odds of membership in Class 4 were most highly associated with parent AUD status, especially when both parents had the disorder, at over three times that compared to the least severe class.
4. Discussion
This study characterized alcohol and posttraumatic stress symptomatology in a sample of young adults who had experienced a serious traumatic event. Consistent with other studies of comorbid AUD-PTSD, we found substantial overlap between alcohol and PTS symptoms in three groups. This indicates that subjects who did not necessarily meet the full diagnostic criteria for either AUD or PTSD experienced potentially debilitating symptoms of both disorders. Additionally, having a mother with AUD was associated with increased odds of membership in classes where alcohol symptoms ranged from moderate to high, while paternal AUD was associated only with membership in the high symptom severity class. While the link between parental AUD and offspring’s later alcohol and posttraumatic stress symptomology cannot be directly inferred from this analysis, young adult offspring exposed to trauma and who have moderate to high drinking problems were significantly more likely to have a parent (or both) with an AUD.
4.1. Hypothesis 1: Latent classes of alcohol and PTS symptoms
Our first hypothesis was confirmed to a degree. A four-class solution fit the data best, although Class 2 was characterized by moderate as opposed to high alcohol severity as hypothesized. Furthermore, the expression of symptoms from low to high severity was associated with sex and the type of trauma experienced. Researchers have found ample evidence suggesting sex differences in both alcohol use (Erol & Karpyak, 2015), exposure to certain types of trauma (Silove et al., 2017; Tolin & Foa, 2006), and trauma response (Olff, 2017). Higher mean counts of AUD symptoms of AUD symptoms were associated with being male and having experienced physical assault; these findings were expected but directionality cannot be assumed. The only group with substantial overlap between AUD and PTS symptoms was the high-severity group, Class 4, in which 60% of the individuals in that group met PTS Criterion B (re-experiencing), 44% met Criterion C (numbing/avoidance), and 49% met Criterion D (hyperarousal). The other class with a significant combination of AUD and PTS symptoms, Class 3, endorsed fewer AUD symptoms overall, with the most commonly occurring AUD criteria being symptom 1 (larger/longer) at 32%, symptom 2 (inability to cut back) at 28%, and symptom 10 (tolerance) at 26%. The most commonly endorsed AUD symptoms across Classes 2, 3, and 4 (Class 1 had only one person meeting AUD diagnosis criteria) were symptoms 1 (alcohol is taken in larger quantities or over a longer period of time than intended) and 2 (persistent desire or unsuccessful efforts to cut down on alcohol use). Class 2 and Class 4 also shared substantial overlap between AUD symptoms 8 (recurrent use in situations that are physically hazardous) and symptom 10 (tolerance).
Overall, the internalizing-externalizing model did not appear to fit our data well with the possible exception of Classes 3 and 4. Both of these classes were characterized by high levels of sexual assault and high to moderately high severity on PTS symptoms (Class 3), indicative of internalizing symptoms, or AUD (Class 4), indicative of externalizing symptoms. Criterion B, the cluster of symptoms linked to persistent re-experiencing of trauma, had the highest endorsement in both groups at 99% for Class 3 and 60% for Class 4, and while alcohol use was fairly mild in Class 3, the top two symptoms endorsed—larger/longer (32%) and inability to cut back (28%)—were also the top two symptoms endorsed in Class 4, which may indicate some shared etiology between the use of alcohol in larger quantities than intended, the inability to cut back, and the cluster of PTS symptoms that characterize persistent re-experiencing of trauma—internalizing symptoms. Breslau (2009) had previously found that females exposed to assaultive traumas demonstrated a higher preponderance of avoidance/numbing symptoms than did men and females not exposed to trauma, which coupled with Lehavot and colleagues’ (2014) work on women’s greater likelihood of alcohol use as a coping mechanism following trauma exposure led us to expect more loadings on the numbing symptom cluster with alcohol symptoms. Still, future research parsing out these differences is necessary. Our sample was comprised entirely of trauma-exposed individuals, perhaps rendering distinctions between classes of symptoms more subtle than in studies comparing those with trauma versus those without. It could also be the case that an internalizing-externalizing model does not provide the best explanation for comorbid symptoms of alcohol and PTS.
4.2. Hypothesis 2: Parent AUD increases likelihood of offspring alcohol and PTS symptoms
As hypothesized, parent AUD was significantly associated with increased odds of membership in each of the three groups with higher symptom severity for family configurations in which the mother only was affected and when both parents were affected (Classes 2 through 4). For Class 4 only, father-only AUD was also significantly associated with increased likelihood of membership in this highest symptom severity group. This was unsurprising. The list of studies highlighting the association between parent AUD and offspring trauma exposure is lengthy and includes a heightened risk of physical and sexual abuse (Dube et al., 2001; Walsh, MacMillan, & Jamieson, 2003), lifetime PTSD (Alisic et al., 2014; Cloitre et al., 2009; Kessler et al., 2005), and alcohol problems (Heath et al., 1997). Likewise, the development of comorbid disorders in the relatives of COGA probands, including AUD and PTSD, has been established (Nurnberger et al., 2004). Consistent with a previous examination of parental AUD and offspring trauma among White and Black youth and young adults in COGA (Bender et al., 2020), our study found that family configurations in which the mother or both parents experienced AUD were associated with the highest risks of offspring sexual trauma and high PTS symptom severity (Classes 3 and 4), and confirms that these family alcohol risks may also contribute to offspring alcohol symptom severity, as in Class 4.
4.3. Class differences: Least to highest severity
The largest distinctions in terms of number and severity of symptoms were evinced by Classes 1 and 4. Interestingly, these two groups represented individuals with very similar demographic traits, with roughly equivalent proportions of males (44% in Class 1 versus 49% in Class 4) and females (55% in Class 1 versus 50% in Class 4). Both classes were also majority White and had experienced uniformly high levels of non-assaultive trauma (though exposure to some kind of trauma, broadly defined, was a criterion for inclusion in the study). However, membership in Class 4 was also characterized by very high levels of physical (26% versus 60%) and sexual (9% in Class 1 versus 34% in Class 4) assault. Physical and sexual assault rates were highest in Class 4 and lowest in Class 1 compared to all groups. Class 4 members had also initiated drinking behaviors earlier than members in other classes, at 13 years and 9 months. By contrast, Class 1 members reported the lowest mean age of first drink, at 16 and a half. The rate of both parents having AUD was over twice as high in Class 4 than in Class 1.
The differences in symptom severity between Classes 1 and 4 may thus be partially explained by a greater likelihood of parental AUD, increased odds of physical and sexual assault, and early initiation of drinking behaviors. Studies have routinely demonstrated a link between parental AUD and a greater likelihood of exposure to childhood physical and sexual abuse, as noted above (Anda et al., 2006; Bender et al., 2020). Our exploration of latent classes and subsequent analyses revealed that comorbid AUD-PTSD is associated with a likelihood of both physical and sexual trauma in families where both parents are affected by AUD, and that the majority of this trauma appears to take place during childhood. Thus parent AUD seems to be a key risk factor for a childhood environment that includes trauma exposure, whether or not that trauma was initiated by the parent, another family member, or non-related individuals—an observation in keeping with the vast literature on Adverse Childhood Experiences (Anda et al., 2006).
4.4. Limitations
The clusters of symptoms do not reveal the temporal relationship between alcohol and posttraumatic stress symptoms. However, given that the mean age of AUD onset, at 18.7 years, is higher than that of the average age of first trauma exposure for physical assault (15.4 years), sexual assault (12 years), and non-assaultive trauma (13.4 years), we believe it is likely that the majority of the sample experienced some form of trauma at least prior to heavy, sustained alcohol use. Our analysis did not control or account for other types of parental pathology, such as a history of trauma, that might have contributed to offspring risk for problematic alcohol use or PTSD. It is also likely that individuals in our sample may have been experiencing additional symptoms typically associated with another psychiatric disorder (such as depression or conduct disorder) that we did not include among our covariates. As with all measures that ask the participant to self-report past negative experiences, especially trauma, there is the potential of recall bias among our sample. We also did not assess whether the parent with AUD was the custodial parent during the offspring’s childhood, which may have affected the environment in which the subject was reared. Income information was derived from the subject’s most recent interview, which spanned over a decade; this could have introduced the possibility of income discrepancy over time given that an annual income of $35,000 might mean something very different in 2008 than in 2018. The heterogeneity of the 8% of race/ethnic groups not identified as Black or White in our sample meant that numbers for many other racial groups were too small to permit multivariable analysis, but also limits the generalizability of our findings to diverse populations. It must also be acknowledged that COGA is comprised of a majority of high-risk families, specifically recruited for the study due to familial history of AUD and/or other disorders, and thus our findings may not be generalizable to other populations.
5. Conclusion
The contribution of early environmental influences, such as parental AUD, to offspring trauma exposure—whether or not the parent was responsible for the trauma—and negative mental health and substance use sequelae among individuals trauma exposed cannot be overstated. Our study finds that these sequelae may include problem drinking or even AUD, as well as clinically significant posttraumatic stress symptoms among some young adult offspring of parents with AUD. Additionally, our study is one of relatively few that uses a high-risk sample to empirically ascertain the co-occurrence of alcohol and PTS symptoms among young adults. Using LCA to determine whether and how alcohol and PTS symptoms cluster together is one way to understand how individuals exposed to trauma may express subthreshold features of one or both disorders, or how certain traumatic experiences (e.g. physical assault, sexual assault) could induce varied responses that may involve problematic drinking in addition to PTS symptoms. The young ages at which subjects first reported trauma underscores further the clinical importance of early detection and intervention in families where there is a history of AUD. Increasingly COGA researchers have noted that trauma exposure is salient to our understanding of family alcoholism (Bender et al., 2020; Meyers et al., 2019). Among the offspring of parents with AUD, trauma exposure is common and symptomology is complex, involving features of multiple psychiatric disorders. Using person-centered methods such as LCA is a commonsense approach to understanding the heterogeneity of symptoms, trauma types, and individual-level characteristics associated with trauma-exposed individuals and comorbid AUD-PTSD. We situate our findings within the understanding that research into effective prevention and treatment strategies for AUD ought to take the likelihood of trauma exposure and the co-occurrence of PTS symptoms into account.
Supplementary Material
HIGHLIGHTS.
Parent AUD is associated with offspring trauma exposure, AUD and PTS symptoms.
Latent class analysis can empirically test typologies of subclinical comorbid AUD-PTSD.
Understanding sublinical AUD-PTSD may guide research and clinical practice.
Acknowledgements
The Collaborative Study on the Genetics of Alcoholism (COGA), Principal Investigators B. Porjesz, V. Hesselbrock, T. Foroud; Scientific Director, A. Agrawal; Translational Director, D. Dick, includes eleven different centers: University of Connecticut (V. Hesselbrock); Indiana University (H.J. Edenberg, T. Foroud, J. Nurnberger Jr., Y. Liu); University of Iowa (S. Kuperman, J. Kramer); SUNY Downstate (B. Porjesz, J. Meyers, C. Kamarajan, A. Pandey); Washington University in St. Louis (L. Bierut, J. Rice, K. Bucholz, A. Agrawal); University of California at San Diego (M. Schuckit); Rutgers University (J. Tischfield, A. Brooks, R. Hart); The Children’s Hospital of Philadelphia, University of Pennsylvania (L. Almasy); Virginia Commonwealth University (D. Dick, J. Salvatore); Icahn School of Medicine at Mount Sinai (A. Goate, M. Kapoor, P. Slesinger); and Howard University (D. Scott). Other COGA collaborators include: L. Bauer (University of Connecticut); L. Wetherill, X. Xuei, D. Lai, S. O’Connor, M. Plawecki, S. Lourens (Indiana University); L. Acion (University of Iowa); G. Chan (University of Iowa; University of Connecticut); D.B. Chorlian, J. Zhang, S. Kinreich, G. Pandey (SUNY Downstate); M. Chao (Icahn School of Medicine at Mount Sinai); A. Anokhin, V. McCutcheon, S. Saccone (Washington University); F. Aliev, P. Barr (Virginia Commonwealth University); H. Chin and A. Parsian are the NIAAA Staff Collaborators. We continue to be inspired by our memories of Henri Begleiter and Theodore Reich, founding PI and Co-PI of COGA, and also owe a debt of gratitude to other past organizers of COGA, including Ting- Kai Li, P. Michael Conneally, Raymond Crowe, and Wendy Reich, for their critical contributions. This national collaborative study is supported by NIH Grant U10AA008401 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA).
Funding
This study was supported by NIH Grant U10AA008401 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA).
Footnotes
CRediT authorship contribution statement
Annah K. Bender: Conceptualization, Methodology, Formal analysis, Writing - original draft. Jacquelyn L. Meyers: . Stacey Subbie-Saenz di Viteri: . Marc Schuckit: Supervision, Project administration. Grace Chan: . Laura Acion: . Chella Kamarajan: . John Kramer: Supervision, Project administration. Andrey Anohkin: . Sivan Kinreich: . Ashwini Pandey: . Victor Hesselbrock: Funding acquisition. Michie Hesselbrock: . Kathleen K. Bucholz: Supervision, Project administration, Data curation. Vivia V. McCutcheon: Data curation, Project administration, Software, Validation.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.addbeh.2020.106640.
These sites were/are: SUNY Downstate Health Sciences Center (Brooklyn, NY); University of Connecticut (Storrs, CT); Indiana University (Bloomington, IN); Washington University (St. Louis, MO); University of Iowa (Iowa City, IA) and the University of California (San Diego, CA).
References
- Alisic E, Zalta AK, Van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, & Smid GE (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. The British Journal of Psychiatry, 204(5), 335–340. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders, text revision (4th ed.). Arlington, VA: Author. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield CH, Perry BD, … Giles WH (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender AK, Bucholz KK, Edenberg HJ, Kramer JR, Anokhin AP, Meyers JL, … McCutcheon VV (2020). Trauma exposure and post-traumatic stress disorder among youth in a high-risk family study: Associations with maternal and paternal alcohol use disorder. Journal of Family Trauma, Child Custody & Child Development, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, Pérez-Fuentes G, Okuda M, & Wang S (2013). Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from National Epidemiological Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 132(3), 630–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, & Witte TK (2014). Dissociation and posttraumatic stress disorder: A latent profile analysis. Journal of Traumatic Stress, 27(4), 388–396. [DOI] [PubMed] [Google Scholar]
- Bowers ME, & Yehuda R (2016). Intergenerational transmission of stress in humans. Neuropsychopharmacology, 41(1), 232–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N (2009). The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse, 10(3), 198–210. [DOI] [PubMed] [Google Scholar]
- Breslau N, Reboussin BA, Anthony JC, & Storr CL (2005). The structure of posttraumatic stress disorder: Latent class analysis in 2 community samples. Archives of General Psychiatry, 62(12), 1343–1351. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Reich T, Schmidt I, & Schuckit MA (1994). A new, semi-structured psychiatric interview for use in genetic linkage studies: A report of the reliability of the SSAGA. Journal of Studies on Alcohol, 55, 149–158. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Reich T, Hesselbrock VM, Krarner JR, Nurnberger JI Jr, & Schuckit MA (1996). Can we subtype alcoholism? A latent class analysis of data from relatives of alcoholics in a multicenter family study of alcoholism. Alcoholism: Clinical and Experimental Research, 20(8), 1462–1471. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, McCutcheon VV, Agrawal A, Dick DM, Hesselbrock VM, Kramer JR, Kuperman S, Nurnberger JI, Salvatore JE, Shuckit MA, Bierut LJ, Foroud TM, Chan G, Hesselbrock M, Meyers JL, Edenberg HJ, & Porjesz B (2017). Comparison of parent, peer, psychiatric, and cannabis use influences across stages of offspring alcohol involvement: Evidence from the COGA prospective study. Alcohol: Clinical and Experimental Research, 41, 359–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss C, Entringer S, Moog NK, Toepfer P, Fair DA, Simhan HN, … Wadhwa PD (2017). Intergenerational transmission of maternal childhood maltreatment exposure: Implications for fetal brain development. Journal of the American Academy of Child & Adolescent Psychiatry, 56(5), 373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, Kolk BVD, Pynoos R, Wang J, & Petkova E (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Croft JB, Edwards VJ, & Giles WH (2001). Growing up with parental alcohol abuse: Exposure to childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 25(12), 1627–1640. [DOI] [PubMed] [Google Scholar]
- Elliott DM, Mok DS, & Briere J (2004). Adult sexual assault: Prevalence, symptomatology, and sex differences in the general population. Journal of Traumatic Stress, 17(3), 203–211. [DOI] [PubMed] [Google Scholar]
- Erol A, & Karpyak VM (2015). Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug and Alcohol Dependence, 156, 1–13. [DOI] [PubMed] [Google Scholar]
- Forbes D, Elhai JD, Miller MW, & Creamer M (2010). Internalizing and externalizing classes in posttraumatic stress disorder: A latent class analysis. Journal of Traumatic Stress, 23(3), 340–349. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang H, … Grant BF (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1137–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath AC, Bucholz KK, Madden PA, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, Dunne MP, Whitfield JB, & Martin NG (1997). Genetic and environmental contributions to alcohol dependence risk in a national twin sample: Consistency of findings in women and men. Psychological Medicine, 27, 1381–1396. [DOI] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit MA, & Hesselbrock VM (1999). A validity study of the SSAGA – A comparison with the SCAN. Addiction, 94, 1361–1370. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, & Burns K (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment, 12(2), 210–224. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Dziak JJ, Huang L, Wagner A & Collins LM (2015). PROC LCA & PROC LTA users’ guide (version 1.3.2) University Park: The Methodology Center, Penn State. Retrieved from http://methodology.psu.edu. [Google Scholar]
- Lehavot K, Stappenbeck CA, Luterek JA, Kaysen D, & Simpson TL (2014). Gender differences in relationships among PTSD severity, drinking motives, and alcohol use in a comorbid alcohol dependence and PTSD sample. Psychology of Addictive Behaviors, 28(1), 42–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberzon I, Duncan L, Nievergelt C, Ressler K, & Koenen K (2017). First wave genome wide study in PTSD: Genetic overlap and sex differences in heritability. European Journal of Neuropsychopharmacology, 27(3), S415–S416. [Google Scholar]
- McCutcheon AL (1987). Latent class analysis. (Sage University Paper Series on Quantitative Applications in the Social Sciences, No. 07–054) Newbury Park, CA: Sage. [Google Scholar]
- Merikangas KR, Stevens DE, Fenton B, Stolar M, O’Malley S, Woods SW, & Risch N (1998). Co-morbidity and familial aggregation of alcoholism and anxiety disorders. Psychological Medicine, 28, 773–788. [DOI] [PubMed] [Google Scholar]
- Meyers J, McCutcheon VV, Pandey AK, Kamarajan C, Subbie S, Chorlian D, … Bauer L (2019). Early sexual trauma exposure and neural response inhibition in adolescence and young adults: Trajectories of frontal theta oscillations during a go/no-go task. Journal of the American Academy of Child & Adolescent Psychiatry, 58(2), 242–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss HB, Chen CM, & Yi HY (2007). Subtypes of alcohol dependence in a nationally representative sample. Drug and Alcohol Dependence, 91(2–3), 149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EC, Heath AC, Bucholz KK, Madden PA, Fu Q, Knopik V, … Martin NG (2004). Genetic epidemiology of alcohol-induced blackouts. Archives of General Psychiatry, 61(3), 257–263. [DOI] [PubMed] [Google Scholar]
- Nurnberger JI, Wiegand R, Bucholz K, O’Connor S, Meyer ET, Reich T, Rice J, Schuckit M, King L, Petti T, Bierut L, Hinrichs AL, Kuperman S, Hesselbrock V, & Porjesz B (2004). A family study of alcohol dependence: Coaggregation of multiple disorders in relatives of alcohol-dependent probands. Archives of General Psychiatry, 61, 1246–1256. [DOI] [PubMed] [Google Scholar]
- Olff M (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(sup4), 1351204. [Google Scholar]
- Olino TM, Klein DN, Farmer RF, Seeley JR, & Lewinsohn PM (2012). Examination of the structure of psychopathology using latent class analysis. Comprehensive Psychiatry, 53(4), 323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai A, Suris AM, & North CS (2017). Posttraumatic Stress Disorder in the DSM-5: Controversy, Change, and Conceptual Considerations. Behavioral Sciences (Basel, Switzerland), 7(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich T, Edenberg HJ, Goate A, Williams JT, Rice JP, Van Eerdewegh P, Foroud T, Hesselbrock V, Schuckit M, Bucholz K, Porjesz B, Li T-K, Conneally M, Nurnberger J, Tischfield J, Crowe R, Cloninger CR, Wu W, Shears S, Carr K, Crose C, Willig C, & Begleiter H (1998). Genome-wide search for genes affecting the risk of alcohol dependence. American Journal of Medical Genetics, 81, 207–215. [PubMed] [Google Scholar]
- SAS Institute (2015). Base SAS 9.4 procedures guide SAS Institute. [Google Scholar]
- Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, & Altman SE (2009). Subthreshold conditions as precursors for full syndrome disorders: A 15-year longitudinal study of multiple diagnostic classes. Journal of Child Psychology and Psychiatry, 50(12), 1485–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silove D, Baker JR, Mohsin M, Teesson M, Creamer M, O’Donnell M, … Bryant R (2017). The contribution of gender-based violence and network trauma to gender differences in Post-Traumatic Stress Disorder. PloS One, 12(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin D, & Foa E (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959–992. [DOI] [PubMed] [Google Scholar]
- Vaidyanathan U, Patrick CJ, & Iacono WG (2011). Patterns of comorbidity among mental disorders: A person-centered approach. Comprehensive Psychiatry, 52(5), 527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh C, MacMillan HL, & Jamieson E (2003). The relationship between parental substance abuse and child maltreatment: Findings from the Ontario Health Supplement. Child Abuse & Neglect, 27(12), 1409–1425. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Reardon AF, Ryabchenko KA, Castillo D, & Freund R (2012). A latent class analysis of dissociation and posttraumatic stress disorder: Evidence for a dissociative subtype. Archives of General Psychiatry, 69(7), 698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon G, Westermeyer J, Kuskowski MA, & Nesheim L (2013). Impact of the number of parents with alcohol use disorder on alcohol use disorder in offspring: A population-based study. The Journal of Clinical Psychiatry, 74(8), 795–801. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


