Abstract
Study Design
Systematic literature review.
Objectives
To analyze the evidence available reporting complications in single or two-level anterior cervical discectomy and fusion (ACDF) using a demineralized bone matrix (DBM), hydroxyapatite (HA), or beta-tricalcium phosphate (β-TCP).
Methods
A systematic review of the literature using PubMed, EMBASE, Cochrane Library, and ClinicalTrials.gov databases was performed in August 2020 to identify studies reporting complications in one or two-level ACDF surgery using DBM, HA, or β-TCP. The study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.
Results
A total of 1857 patients were included, 981 male and 876 female, across 17 articles; 5 prospective, and 12 retrospectives. We noted heterogeneity among the included studies concerning the study design and combination of graft materials utilized in them. However, we noted a higher incidence of adjacent segment disease (17.7%) and pseudoarthrosis (9.3%) in fusion constructs using DBM. Studies using β-TCP reported a higher incidence of pseudoarthrosis (28.2%) and implant failures (17.9%).
Conclusions
Degenerative cervical conditions treated with one or two-level ACDF surgery using DBM, HA, or β-TCP with or without cervical plating are associated with complications such as adjacent segment disease, dysphagia, and pseudarthrosis. However, consequent to the study designs and clinical heterogeneity of the studies, it is not possible to correlate these complications accurately with any specific graft material employed. Further well-designed prospective studies are needed to correctly know the related morbidity of each graft used for achieving fusion in ACDF.
Keywords: demineralized bone matrix, hydroxyapatite, beta-tricalcium phosphate, anterior cervical discectomy and fusion, complications, pseudarthrosis, dysphagia
Introduction
Single or two-level anterior cervical discectomy and fusion (ACDF) surgery is a surgical procedure with a low risk of complications. 1 However, there is significant variability among surgeons regarding the perception of impact and severity of reported complications in the literature. In fact, despite dysphagia being one of the most frequently observed adverse events in ACDF surgery, 58% of surgeons consider it as a minor complication with significant disagreement. 2 In the context of cervical degenerative diseases, the main aim is to achieve decompression of the neural structures with interbody fusion, and an autograft is the first and most widely used for this purpose.
Nonetheless, donor site complications such as pain and infection due to the harvesting procedure can have negative consequences, 3 and therefore different osteobiologics have been used to maintain the fusion rates in the place of autograts. In addition, there is great interest in the spine surgery community to understand more about osteobiologics because of the higher cost involved in their use. The commercially available grafts apart from the bone morphogenic proteins (BMP) have emerged rapidly while their efficacy and complications with their use are not being completely understood.
In a constant effort to avoid complications in ACDF surgery, the commonly employed graft alternatives to autograft include substances such as demineralized bone matrix (DBM), hydroxyapatite (HA), and beta-tricalcium phosphate (β-TCP) to achieve promising results in the fusion rates during one or two-level ACDF surgery. The specific spectrum of related complications with their usage is lacking, which precludes the decision-making process in clinical practice for their routine usage. Therefore, this systematic review aims to analyze the best evidence available reporting complications in 1-2 level ACDF using these osteobiologics.
Methods
We performed a systematic review of the literature using PubMed, EMBASE, Cochrane Library, and ClinicalTrials.gov databases in August 2020 to identify studies reporting complications in one or two-level ACDF surgery using DBM, HA, and/or β-TCP. The systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. 4
Search Strategy, Inclusion, and Exclusion Criteria
Three authors (J.P.C., N.A, Y.W.) performed the database search and initially screened articles published from January 2000 to August 2020. The screening process of all articles was performed at the titles and abstracts level, and the selected articles were analyzed for eligibility in full-text and assessed by 2 independent reviewers. A mismatch in the selection of any article was resolved by a third reviewer. The inclusion and exclusion criteria are summarized in the PICO table (Supplementary Material Table 1).
Complications Included
We categorized the reported complications as follows: peri-operative surgical complications, medical complications, mid or long-term outcomes, and other complications.
Peri-Operative Surgical Complications
Neurologic deterioration ≥1 motor grade in American Spinal Cord Injury Association (ASIA) 5 motor scale, new post-operative radiculitis or neuropathic pain, wound dehiscence, superficial wound infection, deep wound infection, airway compromise requiring surgical intervention, dysphagia, dysphonia/hoarseness of voice, anterior cervical hematoma/seroma, epidural hematoma/seroma, cerebrospinal fluid leak/meningocele, vertebral artery injury, esophageal perforation, Horner´s Syndrome, and peri-operative death.
Mid or Long-Term Complications
Nonunion, construct failure with loss of correction (screw pull out, plate dislodgement), construct failure without loss of correction (screw pull out, plate dislodgement), and revision surgery for incomplete neurologic decompression and persistent symptoms.
Medical Complications
Cardiac arrest/failure/arrhythmia, deep vein thrombosis, delirium, gastrointestinal bleeding, myocardial infarction, pneumonia, pressure sores, pulmonary embolism, systemic infection, and urinary tract infection.
Other Complications
Complications that were not included above.
List of Osteobiologics Included
Each study included in this systematic review was categorized according to the number of treated levels and the osteobiologics reported in the article. The osteobiologics included were demineralized bone matrix (DBM), hydroxyapatite (HA); beta-tricalcium phosphate (β-TCP).
Risk of Bias Assessment
We used the Cochrane tool (RoB-2) 6 for the assessment of the risk of bias for randomized trials. In addition, non-randomized studies were assessed with the Methodological Index for Nonrandomized Studies (MINORS), 7 for comparative and non-comparative studies. The maximum score is 16 for non-comparative studies and 24 for comparative studies.
Results
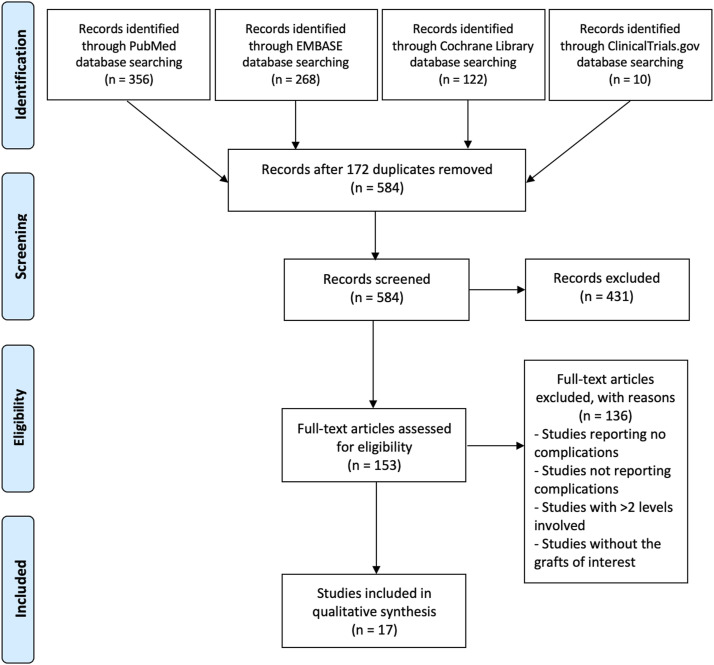
A total of 756 articles were found in the initial search of all four databases used. After the removal of duplicated articles, 584 articles were analyzed and 431 of them were excluded. A total of 153 articles were assessed by two independent reviewers for eligibility and finally 17 articles – 5 prospective and 12 retrospective – were included.8–24 The search mechanism used in the review is shown in Figure 1.
Figure 1.
PRISMA flow diagram for identification and selection of studies for analysis.
There were 1857 patients included in the study with 981 male and 876 female patients. Single-level surgery was performed in 1231 patients, two-level ACDF surgery in 481 patients, and 145 patients were not differentiated between one or two levels. The minimum mean time of follow-up was 12 months. The demographics and other baseline characteristics are summarized in Table 1.
Table 1.
Demographic and Baseline Characteristics of the Included Studies.
| First Author | Year | Country | Study Design | Number of Patients | Mean Age (Years) | Male/Female | 1 Level ACDF | 2 Levels ACDF |
|---|---|---|---|---|---|---|---|---|
| Hacker RJ et al 6 | 2000 | USA | Prospective | 488 | 44 ± 9/47 ± 7∞ | 95/84 | 390 | 98 |
| 43 ± 8/47 ± 7∞ | 80/87 | |||||||
| 44 ± 9/48 ± 8∞ | 74/68 | |||||||
| Agrillo U et al 7 | 2002 | Italy | Retrospective | 45 | 49.7 | 26/19 | 33 | 12 |
| Cauthen JC et al 8 | 2003 | USA | Retrospective | 88 | 49.5 (34.4-66.1) | 15/15 | 43 | 45 |
| 51.1 (32.9-67.4) | 12/20 | |||||||
| 51.4 (29.6-70.3) | 13/13 | |||||||
| Cosar M et al 9 | 2008 | Turkey | Retrospective | 17 | 46 (33-60) | 8/9 | 17 | — |
| Akula M et al 10 | 2008 | UK | Retrospective | 50 | 51 (31-90) | 31/19 | 42 | 8 |
| Moon HJ et al 11 | 2010 | South Korea | Retrospective | 27 | 50.8 (31-67) | 18/9 | — | 27 |
| Niu CC et al 12 | 2010 | Taiwan | Retrospective | 53 | 49.5 ± 11.5 | 15/13 | 35 | 18 |
| 52.2 ± 10.5 | 12/13 | |||||||
| Zagra A et al 13 | 2013 | Italy | Retrospective | 86 | 32-60 | 13/11 | 80 | 6 |
| 28-29 | 15/14 | |||||||
| 29-63 | 17/16 | |||||||
| Kim CH et al 14 | 2013 | South Korea | Prospective | 52 | 49.5 ± 12.8 | 17/12 | 52 | — |
| 55.2 ± 12.4 | 14/9 | |||||||
| Shin JS et al 15 | 2014 | Korea | Retrospective | 60 | 50.0 ± 12.0 | 7/13 | 60 | — |
| 49.0 ± 11.0 | 12/8 | |||||||
| 44.3 ± 9.7 | 13/7 | |||||||
| Kim SJ et al 16 | 2014 | Korea | Retrospective | 96 | 51.9 ± 13.5 | 25/23 | 96 | — |
| 46.5 ± 10.5 | 24/24 | |||||||
| Xie Y et al 17 | 2015 | China | Prospective | 68 | 54.6 ± 12.7 | 20/15 | 29 | 39 |
| 56.3 ± 10.5 | 16/17 | |||||||
| Yi J et al 18 | 2015 | Korea | Prospective | 77 | 51.9 ± 11.7 | 25/13 | 77 | — |
| 51.3 ± 12.4 | 26/13 | |||||||
| Chin K et al 19 | 2017 | United States | Retrospective | 145 | 53 ± 1.0 | 33/42 | NR | NR |
| 53.4 ± 1.6 | 34/36 | |||||||
| Farrokhi MR et al 20 | 2017 | Iran | Prospective | 64 | 47.6 | 12/20 | 64 | — |
| 45.3 | 14/18 | |||||||
| Yu J et al 21 | 2017 | Korea | Retrospective | 247 | 53.7 ± 10.2 | 43/33 | 115 | 132 |
| 53.8 ± 10.9 | 46/36 | |||||||
| 51.7 ± 9.9 | 65/24 | |||||||
| Shiban E et al 22 | 2018 | Germany | Retrospective | 194 | 54 | 91/103 | 98 | 96 |
∞ denotes 1-level/2-level.
ACDF – Anterior Cervical Discectomy and Fusion.
Risk of Bias Assessment
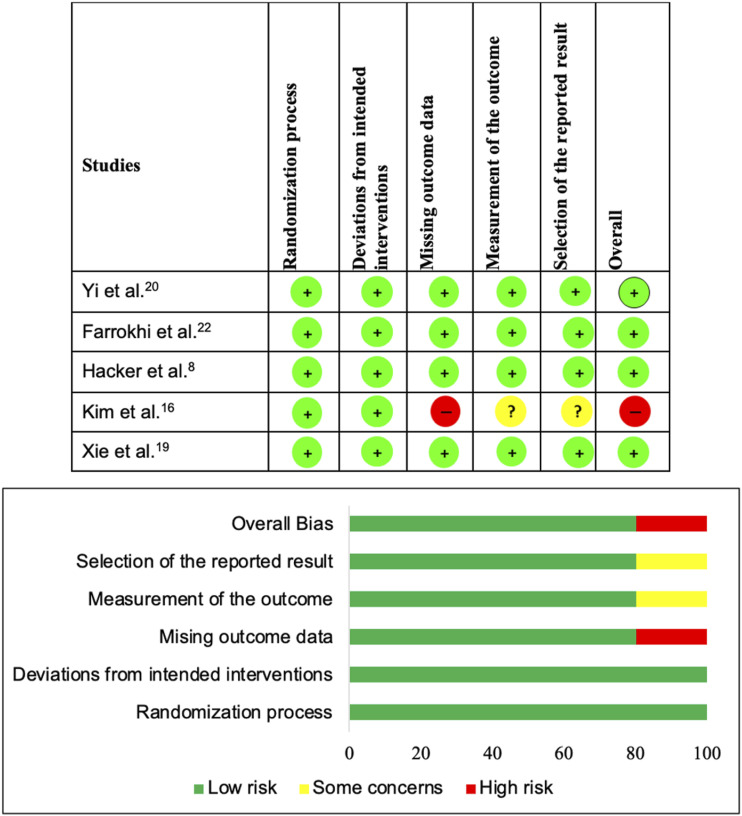
The perceived risk of bias across the retrospective studies was assessed using the MINORS assessment tool in twelve studies which included 5 non-comparative studies9,11–13,24 that scored from 8 to 12 points for a total of 16 points for non-comparative studies, and 7 comparative studies10,14,15,17,18,21,23 that scored from 15 to 21 points for a total of 24 points for comparative studies (Supplementary Material Table 2). The risk of bias across the prospective studies was assessed using RoB-2 in 5 randomized controlled trials, having 4 studies8,19,20,22 with a low risk of bias and 1 study 16 with a high risk of bias (Figure 2).
Figure 2.
Risk of Bias analysis for the prospective randomized trials included in the review using RoB-2 assessment tool.
Overall Reported Complications
The most frequently reported complications among 1857 patients included from 17 articles were radiological and/or clinical adjacent segment disease (ASD) in 53 (2.85%) patients, followed by dysphagia/dysphonia or swallowing problems in 49 (2.64%) patients. We noted heterogeneity among the included studies concerning the study design and combination of graft materials utilized in them as shown in Supplementary Material Table 3. However, we noted a higher incidence of adjacent segment disease (17.7%) and pseudoarthrosis (9.3%) in fusion constructs using DBM. Studies using β-TCP reported a higher incidence of pseudoarthrosis (28.2%) and implant failures (17.9%). We noted comparable dysphagia/dysphonia rates across all the osteobiologics analyzed. Individual risks of these complications among osteobiologics such as DBM, HA, and β-TCP are provided as a heatmap in Table 2.
Table 2.
Heatmap of the Complications Analysed Across the Included Studies.
| Complications | Autograft | DBM | β-TCP | HA |
|---|---|---|---|---|
| Neck pain | 0.6 | 2 | NA | 4.7 |
| Dysphagia | 4.8 | 4.2 | NA | 3 |
| Dysphonia | 2.9 | 3.1 | 4.7 | 2.4 |
| ASD | 2.8 | 17.7 | 3.1 | NA |
| Pseudoarthrosis | 2.5 | 9.3 | 28.2 | 1.2 |
| Implant failure | 0.9 | 1.8 | 17.9 | 0 |
| Graft migration | 3 | 0 | 0 | 0 |
| Medical complications | 1.4 | 3.8 | 0 | 0.6 |
| Neurological worsening | 0 | 2 | 0 | 2.3 |
| Additional surgery | 5.3 | 0 | 2.2 | 2.4 |
| Infection | 0 | 3.3 | 0 | 3.4 |
| Dural tear | 0.6 | NA | NA | 0 |
ASD: adjacent segment disease; DBM: demineralised bone matrix; β-TCP: beta tricalcium phosphate; HA: hyaluronic acid; NA: not available.
Discussion
The present systematic review attempted to analyze the rate of postoperative complications associated with the use of DBM, HA, or β-TCP in ACDF surgery which resulted in identifying only 17 studies with suboptimal quality. From the included studies the most frequently reported complications to include adjacent segment disease, dysphagia, and pseudarthrosis. Although we attempted to individualize the complications per the graft materials analyzed the heterogeneity of the included studies precluded us from generating strong conclusions for clinical practice related to safety.
The gold standard graft used in ACDF surgery has been the autologous iliac bone graft demonstrating good results in achieving intervertebral body fusion. However, it is not free from complications. The harvesting procedure of the autograft leads to donor-site complications 3 such as pain, paresthesia, infection, and hematoma formation. Apart from the donor site-related complications, autograft requires additional plate instrumentation with screws to avoid graft collapse and better restoration of the cervical lordosis, increasing the cost and the rate of dysphagia. 25 Therefore, we performed this systematic review for understanding the spectrum of complications related to some osteobiologics growingly used in ACDF surgery such as DBM, HA, and β-TCP.
Notably, we found seventeen studies reporting complications in 1-2 level ACDF using the osteobiologics of interest such as DBM, HA, or β-TCP. However, the heterogeneity in the study designs and heterogeneity in the graft material usage prevented us from generating strong conclusions concerning their complications. We did not include complications such as donor-site complications from the studies using autografts and subsidence from the studies using cages in our analysis as mentioned in the exclusion criteria to avoid further heterogeneity in the generated results.
Interbody fusion is the final objective in ACDF, and the fusion rate could be variable due to the radiological method used, time of follow-up, and subjective criteria employed.26,27 There was one study reporting fusion rates of 76% at 6 months of follow-up when a stand-alone PEEK cage filled with hydroxyapatite compared with 92% in tricortical iliac bone graft with plating. 16 Nonetheless, hydroxyapatite showed over 87% of fusion rates when follow-up is until 12 months and mixed with autologous graft 8 or with DBM/β-TCP. 20 The negative face of the same outcome, ie non-union or pseudarthrosis, was reported in some of the included studies with heterogeneity. For example, Yi et al 20 compared a plate augmented PEEK cage construct filled with HA + DBM vs HA + β-TCP and reported that the rate of non-union at 12 months was 13% in both groups. Such combined usage of osteobiologic prevented us from identifying the material that is responsible for pseudoarthrosis. Moreover, the study of Yu et al 23 comparing stand-alone PEEK cage filled with DBM vs PEEK cage + DBM with plating vs iliac bone graft with plating reported similar rates of fusion. Still, the supplementation with plate fixation especially while using autologous graft is beneficial in reducing the time to fusion. A recent study including 1-3 levels of ACDF treated with self-locking stand-alone cages filled with hydroxyapatite reported pseudarthrosis at single level ACDF in 15.4% of patients while at 2-level ACDF in 15.2% of patients, and they reported that symptomatic pseudarthrosis occurred in 6.1% requiring reoperation. 28
Dysphagia is one of the most common observed complications in ACDF and has significant heterogeneity in its reporting due to the variability in its definition and measuring methods. 29 Similarly, we noted a variable incidence of dysphagia across the included studies. Patients using autograft in their fusion construct reported the highest incidence of dysphagia (4.8%) followed by patients with DBM (4.2%) in their fusion construct. This could be explained by the higher use of plated constructs in the autograft group which resulted in a higher incidence of dysphagia. 25 Shin et al 17 confirmed this phenomenon by comparing zero-profile and stand-alone PEEK cages packed with DBM vs iliac bone graft with plating with a significantly higher rate of dysphagia in the last group. However, cervical plating plays a role in preventing cage subsidence and restoration of cervical lordosis when compared with stand-alone cages. 25 Moreover, the incidence rates were comparable across the materials compared in this study.
We noted higher rates (17.9%) of implant failure in patients where β-TCP was used as an osteobiologic along with higher rates of pseudoarthrosis (28.2%) as noted in some preclinical studies on β-TCP which needs further investigation. 30
Limitations
The present systematic review has some limitations needing recognition for an adequate interpretation of the results. First, the heterogeneity in the included studies concerning the study designs and graft usage prevented us from giving strong recommendations based on the results obtained. We did not analyze the complications such as donor site complications and subsidence of the grafted material which might mask the real incidence of the complications analyzed. We did not include studies that used these grafts without any report of complications, since our primary objective is to identify the rate of occurrence of each complication following ACDF surgery.
Authors Perspective
Upon analyzing the studies for the osteobiologics to aid in fusion in ACDF surgery, compared to the autografts, none of the included materials such as DBM or β-TCP, or HA had an evident rise in immediate complications such as dysphagia, dysphonia, neck pain, neurological worsening, infection or dural tear. Hence, their immediate safety is well established. However, complications such as implant failure, and pseudoarthrosis were predominantly noted in fusion constructs using β-TCP while ASD is predominantly noted in fusion constructs using DBM. Hence, future studies are warranted to analyze the material properties of β-TCP and DBM on their suitability for use in ACDF fusion constructs. We stress that the results were all derived from studies with limited methodological robustness and caution should be exercised before considering the results for clinical translation.
Conclusions
Degenerative cervical conditions treated with one or two-level ACDF surgery using DBM, HA, or β-TCP with or without cervical plating are associated with complications such as adjacent segment disease, dysphagia, and pseudarthrosis. However, consequent to the study designs and clinical heterogeneity of the studies, it is not possible to correlate these complications accurately with any specific graft material employed. Further well-designed prospective studies are needed to correctly know the related morbidity of each graft used for achieving fusion in ACDF.
Supplemental Material
Supplemental Material for Complications With Demineralized Bone Matrix, Hydroxyapatite and Beta-Tricalcium Phosphate in Single and Two-Level Anterior Cervical Discectomy and Fusion Surgery by Juan P. Cabrera, Sathish Muthu, Mohamed K. Mesregah, Ricardo Rodrigues-Pinto, Neha Agarwal, Arun Kumar, Yabin Wu, Gianluca Vadalà, Christopher Martin, Jeffrey C. Wang, Hans-Jörg Meisel, Zorica Buser,and AO Spine Knowledge Forum Degenerative in Global Spine Journal
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: ATEC-attended course in San Diego, travel and lodging supported by ATEC, ATEC-own stock options that were purchased personally. Fehling Instruments GmbH, Stayble Therapeutics Via Regenerate Life Sciences GmbH, Mundipharma Via Regenerate Life Sciences GmbH, Spinplant GmbH. Depuy Synthes. Yes, various lawfirms me, AO Foundation Board reimbursements, Bone biologics Personal investment, Surgitech Personal investment, Pearldiver Personal investment. SeaSpine (past, paid to the institution), Next Science (paid directly to institution), Motion Metrics (past, paid to the institution), NIH SBIR grant NIH SBIR Subaward, MAX BioPharma, Cerapedics (past), The Scripps Research Institute (past), AO Spine (past), Xenco Medical (past), AO Spine, North American Spine Society, US 2014O194364A1, US010391142B2, North American Spine Society: committee member, Lumbar Spine Society: Co-chair Educational Committee, AOSpine Knowledge Forum Degenerative: Associate member, AOSNA Research committee-committee member. Medtronic, Baxter, SafeOrthopaedics, Croatian Society of Vertebrology, Medtronic, Paid consultant for company, SI Bone Research support to institution, AO Spine Research support to institution, Mizuho Orthopedics Systems Research support to institution, Medtronic Paid consultant for company.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This supplement was organized and financially supported by AO Spine through the AO Spine Knowledge Forum Degenerative, a focused group of international spine experts.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Juan P. Cabrera https://orcid.org/0000-0003-4685-6106
Sathish Muthu https://orcid.org/0000-0002-7143-4354
Mohamed Kamal Mesregah https://orcid.org/0000-0002-8047-9159
Ricardo Rodrigues-Pinto https://orcid.org/0000-0002-6903-348X
Yabin Wu https://orcid.org/0000-0002-1836-7674
Hans Jörg Meisel https://orcid.org/0000-0003-3838-1489
Zorica Buser https://orcid.org/0000-0002-5680-0643
References
- 1.Martin C, D’Oro A, Buser Z, et al. Trends and costs of anterior cervical discectomy and fusion: A comparison of inpatient and outpatient procedures. Iowa Orthop J. 2018;38:167-176. [PMC free article] [PubMed] [Google Scholar]
- 2.Lebude B, Yadla S, Albert T, et al. Defining “‘complications’” in spine surgery neurosurgery and orthopedic spine surgeons’ survey. J Spinal Disord Tech. 2010;23(8):493-500. [DOI] [PubMed] [Google Scholar]
- 3.Pollock R, Alcelik I, Bhatia C, et al. Donor site morbidity following iliac crest bone harvesting for cervical fusion: A comparison between minimally invasive and open techniques. Eur Spine J. 2008;17(6):845-852. doi: 10.1007/s00586-008-0648-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirshblum S, Snider B, Rupp R, Read MS. Updates of the international standards for neurologic classification of spinal cord injury: 2015 and 2019. Phys Med Rehabil Clin N Am. 2020;31(3):319-330. doi: 10.1016/j.pmr.2020.03.005 [DOI] [PubMed] [Google Scholar]
- 6.Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:I4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 7.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-716. [DOI] [PubMed] [Google Scholar]
- 8.Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine. 2000;25(20):2646-2654. [DOI] [PubMed] [Google Scholar]
- 9.Agrillo U, Mastronardi L, Puzzilli F. Anterior cervical fusion with carbon fiber cage containing coralline hydroxyapatite: Preliminary observations in 45 consecutive cases of soft-disc herniation. J Neurosurg. 2002;96(3 suppl l):273-276. [DOI] [PubMed] [Google Scholar]
- 10.Cauthen JC, Theis RP, Allen AT. Anterior cervical fusion: A comparison of cage, dowel and dowel-plate constructs. Spine J. 2003;3(2):106-117. [DOI] [PubMed] [Google Scholar]
- 11.Cosar M, Ozer AF, Celal Iplikcioglu A, et al. The results of b-tricalcium phosphate coated hydroxyapatite (b-TCP/HA) grafts for interbody fusion after anterior cervical discectomy. J Spinal Disord Tech. 2008;21(6):436-441. [DOI] [PubMed] [Google Scholar]
- 12.Akula M, Taha M, Mathew B, O’Reilly G. The plate cage benezech implant as an alternative to autologous bone graft in the treatment of cervical spondylosis: Clinical and functional outcome. Br J Neurosurg. 2008;22(4):542-545. doi: 10.1080/02688690802057326 [DOI] [PubMed] [Google Scholar]
- 13.Moon HJ, Kim JH, Kim JH, Kwon TH, Chung HS, Park YK. The effects of anterior cervical discectomy and fusion with stand-alone cages at two contiguous levels on cervical alignment and outcomes. Acta Neurochir. 2011;153(3):559-565. doi: 10.1007/s00701-010-0879-z [DOI] [PubMed] [Google Scholar]
- 14.Niu C-C, Liao J-C, Chen W-J, Chen L-H. Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech. 2010;23(5):310-316. [DOI] [PubMed] [Google Scholar]
- 15.Zagra A, Zagra L, Scaramuzzo L, Minoia L, Archetti M, Giudici F. Anterior cervical fusion for radicular-disc conflict performed by three different procedures: Clinical and radiographic analysis at long-term follow-up. Eur Spine J. 2013;22 Suppl 6(suppl 6):S905-S909. doi: 10.1007/s00586-013-3006-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim CH, Chung CK, Hahn S. Autologous iliac bone graft with anterior plating is advantageous over the stand-alone cage for segmental lordosis in single-level cervical disc disease. Neurosurgery. 2013;72(2):257-265. doi: 10.1227/NEU.0b013e31827b94d4 [DOI] [PubMed] [Google Scholar]
- 17.Shin JS, Oh SH, Cho PG. Surgical outcome of a zero-profile device comparing with stand-alone cage and anterior cervical plate with iliac bone graft in the anterior cervical discectomy and fusion. Korean J Spine. 2014;11(3):169-177. doi: 10.14245/kjs.2014.11.3.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim S, Kim S. Anterior cervical discectomy and fusion using a double cylindrical cage versus an anterior cervical plating system with iliac crest autografts for the treatment of cervical degenerative disc disease. J Korean Neurosurg Soc. 2014;55(1):12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie Y, Li H, Yuan J, Fu L, Yang J, Zhang P. A prospective randomized comparison of PEEK cage containing calcium sulphate or demineralized bone matrix with autograft in anterior cervical interbody fusion. Int Orthop. 2015;39(6):1129-1136. doi: 10.1007/s00264-014-2610-9 [DOI] [PubMed] [Google Scholar]
- 20.Yi J, Lee GW, Nam WD, et al. A prospective randomized clinical trial comparing bone union rate following anterior cervical discectomy and fusion using a polyetheretherketone cage: Hydroxyapatite/B-Tricalcium phosphate mixture versus hydroxyapatite/demineralized bone matrix mixture. Asian Spine J. 2015;9(1):30-38. doi: 10.4184/asj.2015.9.1.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chin KR, Pencle FJR, Seale JA, Valdivia JM. Soft tissue swelling incidence using demineralized bone matrix in the outpatient setting. World J Orthop. 2017;8(10):770-776. doi: 10.5312/wjo.v8.i10.770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farrokhi MR, Nikoo Z, Gholami M, Hosseini K. Comparison between acrylic cage and polyetheretherketone (PEEK) cage in single-level anterior cervical discectomy and fusion. Clin Spine Surg. 2017;30(1):38-46. doi: 10.1097/BSD.0000000000000251 [DOI] [PubMed] [Google Scholar]
- 23.Yu J, Ha Y, Shin JJ, et al. Influence of plate fixation on cervical height and alignment after one- or two-level anterior cervical discectomy and fusion. Br J Neurosurg. 2018;32(2):188-195. doi: 10.1080/02688697.2017.1394980 [DOI] [PubMed] [Google Scholar]
- 24.Shiban E, Nies M, Kogler J, et al. No correlation between radiological and clinical outcome 1 year following cervical arthrodesis. Acta Neurochir. 2018;160(4):845-853. doi: 10.1007/s00701-018-3495-y [DOI] [PubMed] [Google Scholar]
- 25.Cheung ZB, Gidumal S, White S, et al. Comparison of anterior cervical discectomy and fusion with a stand-alone interbody cage versus a conventional cage-plate technique: A systematic review and meta-analysis. Global Spine J. 2019;9(4):446-455. doi: 10.1177/2192568218774576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oshina M, Oshima Y, Tanaka S, Riew KD. Radiological fusion criteria of postoperative anterior cervical discectomy and fusion: A systematic review. Global Spine J. 2018;8(7):739-750. doi: 10.1177/2192568218755141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhee JM, Chapman JR, Norvell DC, Smith J, Sherry NA, Riew KD. Radiological determination of postoperative cervical fusion: A systematic review. Spine. 2015;40(13):974-991. doi: 10.1097/BRS.0000000000000940 [DOI] [PubMed] [Google Scholar]
- 28.Iunes EA, Barletta EA, Belsuzarri TAB, et al. Pseudarthrosis in anterior cervical discectomy and fusion with a self-locking, stand-alone cage filled with hydroxyapatite: A retrospective study with clinical and radiological outcomes of 98 levels with a minimum 2-year follow-up. J Neurosurg Spine. 2020;33(6):717-726. doi: 10.3171/2020.4.SPINE20357 [DOI] [PubMed] [Google Scholar]
- 29.Tetreault L, Lange SF, Chotai S, et al. A systematic review of definitions for dysphagia and dysphonia in patients treated surgically for degenerative cervical myelopathy. Global Spine J. 2022;12:1535-1545. doi: 10.1177/21925682211035714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu H, Zhou Y, Ma Y, et al. Current application of beta-tricalcium phosphate in bone repair and its mechanism to regulate osteogenesis. Front Mater. 2021;8:698915. doi: 10.3389/fmats.2021.698915 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Complications With Demineralized Bone Matrix, Hydroxyapatite and Beta-Tricalcium Phosphate in Single and Two-Level Anterior Cervical Discectomy and Fusion Surgery by Juan P. Cabrera, Sathish Muthu, Mohamed K. Mesregah, Ricardo Rodrigues-Pinto, Neha Agarwal, Arun Kumar, Yabin Wu, Gianluca Vadalà, Christopher Martin, Jeffrey C. Wang, Hans-Jörg Meisel, Zorica Buser,and AO Spine Knowledge Forum Degenerative in Global Spine Journal