Abstract
Introduction: In 2019, the Beta-Blockers for the Prevention of Acute Exacerbations of Chronic Obstructive Pulmonary Disease study (BLOCK-COPD) evaluated the effect of metoprolol on exacerbation risk and mortality in a COPD population without indications for beta-blocker use. We hypothesized that an imaging metric of coronary artery disease (CAD), the coronary artery calcium (CAC) score, would predict exacerbation risk and identify a differential response to metoprolol treatment.
Methods: The study population includes participants in the BLOCK-COPD study from multiple study sites. Participants underwent clinically indicated thoracic computed tomography (CT) scans ± 12 months from enrollment. The Weston scoring system quantified CAC. Adjusted Cox proportional hazards models evaluated for associations between CAC and time to exacerbation.
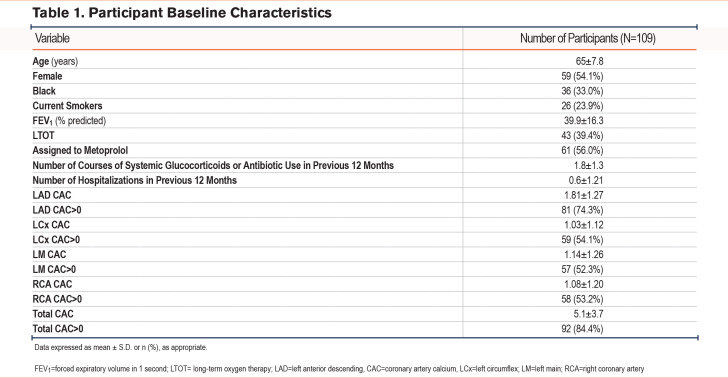
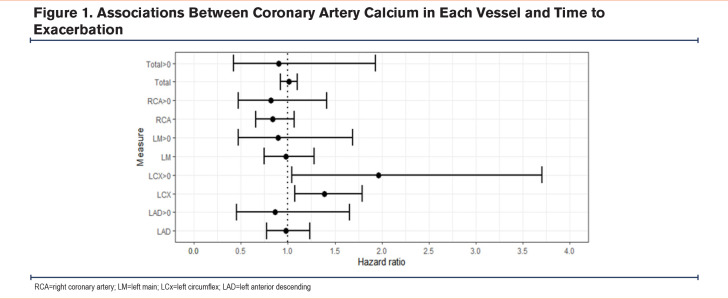
Results: Data is included for 109 participants. The mean CAC score was 5.1±3.7, and 92 participants (84%) had CAC scores greater than 0. Over a median (interquartile range) follow-up time of 350 (280 to 352) days, there were 61 mild exacerbations and 19 severe/very severe exacerbations. No associations were found between exacerbations of any severity and CAC>0 or total CAC. Associations were observed between total CAC and CAC>0 in the left circumflex (LCx) and time to exacerbation of any severity (adjusted hazard ratio [aHR]=1.39, confidence interval [CI]: 1.08–1.79, p=0.01) and (aHR=1.96, 95% CI: 1.04–3.70, p= 0.04), respectively.
Conclusion: CAD is a prevalent comorbidity in COPD accounting for significant mortality. Our study confirms the high prevalence of CAD using the CAC score; however, we did not discover an association between CAC and exacerbation risk. We did find novel associations between CAC in the LCx and exacerbation risk which warrant further investigation in larger cohorts.
Keywords: COPD, acute exacerbations, coronary artery calcium, beta-blockers
Introduction
Note: A portion of this manuscript was presented at the 2021 American Thoracic Society International Conference as an abstract/poster presentation.
The Beta-Blockers for the Prevention of Acute Exacerbations of COPD (BLOCK-COPD) study investigated whether metoprolol would reduce exacerbation risk in patients with COPD who did not have an evidence-based indication for beta-blocker use, namely coronary artery disease (CAD) with recent reperfusion intervention or congestive heart failure.1 This trial was incepted due to prior reports suggesting beta-blockers may be associated with a reduced risk of acute exacerbations.1 BLOCK-COPD failed to demonstrate exacerbation risk reduction with metoprolol but observed an increase in severe-to-very severe exacerbations leading to early study termination. Since BLOCK-COPD largely sought to enroll individuals without CAD, it is not clear whether participants with subclinical or unrecognized CAD might have a differential response to metoprolol. The coronary artery calcium (CAC) score can be used to assess for CAD using chest computed tomography (CT) scans.2 This imaging biomarker evaluates the deposition of calcified plaque in the coronary vasculature, and a visual score of greater or equal to 7 is associated with incident coronary vascular events in COPD.3 We hypothesized that CAC would be associated with an increased exacerbation risk and differential response to metoprolol treatment within BLOCK-COPD. Some of the results from this study were previously reported in the form of an abstract.4
Methods
The study population includes participants in the BLOCK-COPD study from 5 study sites (University of Maryland, University of Michigan, Northwestern University, Temple University, and University of Alabama at Birmingham) who underwent clinically indicated thoracic CT imaging within a timeframe of 12 months before/after enrollment. Comprehensive clinical, spirometry, exacerbation, and mortality data were collected at regular intervals as part of the BLOCK-COPD protocol.5 An exacerbation of COPD was defined as an increase in or a new onset of 2 or more respiratory symptoms that required treatment with antibiotics or systemic steroids for at least 3 days.5 All participants completed informed consent for enrollment in BLOCK-COPD, and the post-hoc analysis was approved by the institutional review board at each participating institution.
We used the Weston scoring system to quantify CAC using an ordinal scale wherein 0 indicates no vessel calcium and a score of 1–3 indicates increasing calcification severity.6 The Weston score ranges from 0–12 and is derived by summing the individual scores from each of the 4 major coronary arteries: right coronary artery (RCA), left main (LM), left anterior descending (LAD), and left circumflex (LCx). An investigator at each clinical site, blinded to clinical parameters, determined the CAC score for each participant.
Cox proportional hazards models were used to measure associations between CAC in each vessel (and the interaction between CAC and treatment assignment) and time to exacerbation. Adjusted models included age, sex, race, smoking status, baseline FEV1 percentage predicted, number of hospitalizations for COPD during the previous year, number of exacerbations treated with glucocorticoids or antibiotics during the previous year, and treatment assignment and were stratified by center. CAC was evaluated both as a continuous variable and as a binary variable indicated by CAC greater than zero. Analyses were performed using R statistical software (version 3.6.0). P-values were not adjusted for multiple comparisons.
Results
Imaging and clinical data were included for 109 participants. The mean age was 65±8 years with 54% female, 33% Black race, and 24% active smokers (Table 1). Sixty-one (56%) participants were assigned to the metoprolol treatment arm. Over a median (interquartile [IQR]) follow-up time of 350 (280 to 352) days, 61 individuals experienced at least one exacerbation.
The mean CAC score was 5.1±3.7, with 92 participants (84%) having CAC >0. Associations were observed between CAC in the LCx and shorter time to exacerbation (adjusted hazard ratio [aHR]=1.39 for 1 unit increase in score, 95% confidence interval [CI]: 1.08–1.79, p=0.01). When treating CAC as a dichotomous variable, associations were again observed between LCx CAC and shorter time to exacerbation (aHR= 1.96, 95% CI: 1.04–3.70, p= 0.04). No associations were observed between LM, LAD, or total CAC and time to exacerbation. No interaction was observed between total or any vessel CAC and treatment assignment to either metoprolol or placebo. A summary of the findings is depicted in Figure 1.
Discussion
We identified that CAC, as a reflection of underlying CAD, was associated with COPD exacerbation risk in a well-characterized COPD population. However, we did not observe a beneficial effect of metoprolol on exacerbation risk reduction in BLOCK-COPD participants with any visible CAC. Interestingly, we found that CAD (by CAC >0) was highly prevalent in this subgroup of patients despite the BLOCK-COPD design excluding patients with CAD requiring recent revascularization. Our study is novel in that it links an imaging biomarker of CAD with COPD control and further investigated associations between CAC and beta-blocker treatment. CAC is an important imaging biomarker that is implicated in COPD morbidity.3 The observation between LCx CAC and exacerbation risk is thought-provoking with several potential mechanisms at play. Elevated CAC scores in the LCx have been implicated in large myocardial ischemia deficits on nuclear perfusion scans.7 Additionally, the LCx can perfuse a large portion of the left ventricle including the mitral valve. Several publications report associations between total CAC and left ventricular diastolic dysfunction.8,9 Given that diastolic dysfunction is associated with an increased risk of severe exacerbations, it is possible that impaired left ventricular perfusion increases diastolic dysfunction and increases exacerbation risk.10 Interestingly, the LCx perfuses the sinoatrial (SA) node in up to 25% of individuals.11 Existing reports indicate associations between atrial arrhythmias and increased COPD exacerbation risk, so it is reasonable to posit that poor perfusion of the SA node may increase the incidence of arrhythmias and subsequently contribute to exacerbation risk.12 Thus, poor myocardial perfusion and resultant impairment in cardiac function may lead to increased respiratory symptoms. Our study is limited by its post hoc design and small sample size, which precludes matching between groups or inferences regarding causality. In addition, given that the study was terminated early, some participants had limited follow-up time. Further, we are limited to participants who underwent thoracic CT for clinical reasons outside of the BLOCK-COPD protocol, which may introduce confounding by indication.
Conclusions
We found associations between CAC in the LCx and exacerbation risk, expanding the relevance of CAC measurement in COPD. Future investigations should incorporate the use of CAC measurement to better understand exacerbation risk prediction as well as to disentangle complex heart-lung interactions.
Abbreviations
Abbreviations: aHR=adjusted hazard ratio; BLOCK-COPD=Beta-Blockers for the Prevention of Acute Exacerbation of COPD study; CAC=coronary artery calcium; CAD=coronary artery disease; CI=confidence interval; IQR=interquartile range; LAD=left anterior descending; LCx=left circumflex; LM=left main; LTOT=long-term oxygen therapy; RCA=right coronary artery; SA=sinoatrial
Funding Statement
U.S. Department of Defense (W81XWH-15-1-0705)
References
- 1.Etminan M,Jafari S,Carleton B,FitzGerald JM. Beta-blocker use and COPD mortality: a systematic review and meta-analysis. BMC Pulm Med. 2012;12:48. doi: https://doi.org/10.1186/1471-2466-12-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Detrano R,Guerci AD,Carr JJ,et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336-1345. doi: https://doi.org/10.1056/NEJMoa072100 [DOI] [PubMed] [Google Scholar]
- 3.Bhatt SP,Kazerooni EA,Newell JD,et al. Visual estimate of coronary artery calcium predicts cardiovascular disease in COPD. Chest. 2018;154(3):579-587. doi: https://doi.org/10.1016/j.chest.2018.05.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wade RC,Ling S,Helgeson E,et al. Metoprolol attenuates exacerbation risk in subjects with elevated coronary artery calcium scores: a post-hoc analysis of BLOCK-COPD. Am J Respir Crit Care Med. 2021;203:A2257. doi: https://doi.org/10.1164/ajrccm-conference.2021.203.1_MeetingAbstracts.A2257 [Google Scholar]
- 5.Dransfield MT,Voelker H,Bhatt SP,et al. Metoprolol for the prevention of acute exacerbations of COPD. N Engl J Med. 2019;381(24):2304-2314. doi: https://doi.org/10.1056/NEJMoa1908142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirsch J,Buitrago I,Mohammed TL,Gao T,Asher CR,Novaro GM. Detection of coronary calcium during standard chest computed tomography correlates with multi-detector computed tomography coronary artery calcium score. Int J Cardiovasc Imaging. 2012;28(5):1249-1256. doi: https://doi.org/10.1007/s10554-011-9928-9 [DOI] [PubMed] [Google Scholar]
- 7.Lai HM,Holtzman D,Aronow WS,et al. Association of coronary artery calcium with severity of myocardial ischemia in left anterior descending, left circumflex, and right coronary artery territories. Clin Cardiol. 2012;35(1):61-63. doi: https://doi.org/10.1002/clc.20997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mansour MJ,Chammas E,Hamoui O,Honeine W,AlJaroudi W. Association between left ventricular diastolic dysfunction and subclinical coronary artery calcification. Echocardiography. 2020;37(2):253-259. doi: https://doi.org/10.1111/echo.14580 [DOI] [PubMed] [Google Scholar]
- 9.Maragiannis D,Schutt RC,Gramze NL,et al. Association of left ventricular diastolic dysfunction with subclinical coronary atherosclerotic disease burden using coronary artery calcium scoring. J Atheroscler Thromb. 2015;22(12):1278-1286. doi: https://doi.org/10.5551/jat.29454 [DOI] [PubMed] [Google Scholar]
- 10.Abusaid GH,Barbagelata A,Tuero E,Mahmood A,Sharma G. Diastolic dysfunction and COPD exacerbation. Postgrad Med. 2009;121(4):76-81. doi: https://doi.org/10.3810/pgm.2009.07.2033 [DOI] [PubMed] [Google Scholar]
- 11.Vikse J,Henry BM,Roy J,et al. Anatomical variations in the sinoatrial nodal artery: a meta-analysis and clinical considerations. PLoS One. 2016;11(2):e0148331. doi: https://doi.org/10.1371/journal.pone.0148331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhatt SP,Nanda S,Kintzer JS. Arrhythmias as trigger for acute exacerbations of chronic obstructive pulmonary disease. Respir Med. 2012;106(8):1134-1138. doi: https://doi.org/10.1016/j.rmed.2012.04.007 [DOI] [PubMed] [Google Scholar]