Abstract
The recent spread of the monkeypox virus (MPXV), causing monkeypox (mpox), to non-endemic areas, and the atypical and unusual clinical manifestations observed during its 2022 outbreak has focused international interest on the clinical features of the disease. Mpox is usually a self-limiting disease with mild symptoms with common manifestations, including fever and skin lesions; however, severe manifestations could occur in some vulnerable groups (children and those with impaired immune systems) and may present multisystem complications and fatal outcomes. In most cases, a fever is the first sign of disease, followed by the development of various inflammatory lesions on the skin, such as vesiculopustular rashes and ulcers. Pneumonitis, encephalitis, keratitis, secondary bacterial infections, acute kidney injury, and myocarditis are all possible outcomes of the infection. Myocarditis has been reported to be caused by orthopoxviruses, and it is a serious condition of which its pathophysiology is little understood. Recent reports have indicated myocarditis with cardiac involvement as a possible atypical and unusual consequence of the MPXV infection during present outbreak. This review provides an overview of the clinical manifestations of mpox with a special focus on its effects on the heart, including myocarditis. The evidence of the myocarditis in mpox patients and its possible pathogenesis are discussed.
Keywords: Monkeypox, mpox, outbreak, pathogenesis, myocarditis
Introduction
Monkeypox (mpox) is a vesicular-pustular illness caused by a zoonotic Orthopoxvirus under the Poxviridae family, monkeypox virus (MPXV) [1,2]. Previously, the disease was mainly endemic to West and Central Africa, and the first human case was identified in 1970 in the Democratic Republic of Congo (DRC) [3,4]. From May 6, 2022, MPXV has swiftly spread to multiple nations outside the established endemic areas with symptoms matching smallpox, leading to outbreaks in numerous countries in 2022. This rapid spread of the virus and escalating mpox cases posed a Public Health Emergency of International Concern (PHEIC) to be declared by the World Health Organization (WHO) on July 23, 2022 [5]. As of March 29, 2023, a total of 86,746 confirmed cases of mpox from 110 countries and 112 deaths have been reported [6].
Mpox has been prevalent in Central Africa since the 1980s, but serological data suggests it also existed in West Africa [7,8]. It is possible for MPXV to infrequently infect people while still maintaining a reservoir in wild animals due to the adaptability of the virus [9]. Many lines of evidence suggest that small mammals are the principal wild animal reservoirs of MPXV, although none of the evidence is conclusive [2,10]. MPXV transmission mainly occurs via exposure to bodily fluids from infected animals, human-to-human transmission by respiratory droplets, and close contact with contaminated materials from lesions and mpox-affected patients [11,12]. Sexual activity with several partners, particularly among men who engage in sex with men (MSM), is proven to be another method of MPXV transmission [13]. Despite not being a sexually transmitted disease, mpox can nonetheless spread through sexual contact [13].
The primary method for determining MPXV infection is laboratory diagnosis. Viral culture is less accurate but still helps in verifying the infection and a positive PCR test of skin or mucosal lesion swabs or scabs is the main approach used to identify MPXV infection [14,15].
Despite the fact that immunization against smallpox can provide protection against infection with MPXV, no medications have been approved particularly for treating mpox [16]. The two licensed vaccines available for use in preventing smallpox in the United States are JYNNEOS and ACAM2000, which have been recommended against mpox, while researches are being carried out for developing specific vaccines against mpox [9,17–19]. Smallpox drugs such as tecovirimat, brincidofovir, and cidofovir have been suggested for treating mpox patients, while the development of specific drugs against mpox is underway [20,21]. Intravenous vaccinia immune globulin (VIGIV) may be considered for patients with complex MPXV infection or as prophylaxis for T-cell immunodeficiency patients [22]. Antiviral treatment is a valuable option for patients with severe mpox disease, pregnant women, people with impaired immune systems, and children younger than 8 years old [22].
Vulnerable individuals with immunosuppressed conditions and comorbidities, non-vaccinated individuals, children, and pregnant women, workers who come into contact with MPXV-infected humans or animals in the course of their employment, and health workers and medical staff attending disease outbreaks all fall into the high-risk category [23]. Therefore, reducing human contact with infected wildlife and stopping the spread of virus from person to person are essential components to fight against mpox [14]. To prevent MPXV infection, it is crucial not to touch skin lesions or items handled by mpox patients. Whether the diagnosis of MPXV infection is suspected or confirmed, the patient must be promptly isolated and masked.
Although the MPXV infection is self-limiting, some patients need to be hospitalized due to certain consequences, including myocarditis, excruciating anorectal pain, eye lesions, kidney damage, or soft tissue superinfections [16]. Potentially causing immune-mediated damage to the heart, MPXV may exhibit a preference for this organ to cause myocarditis [24]. This article highlights an overview of clinical manifestations of mpox with a special focus on myocarditis caused by the MPXV in affected patients, its pathogenesis and management.
General clinical manifestation of mpox
MPXV infection share many similar clinical characteristics with smallpox, but has differential characteristics such as lymphadenitis -especially in the cervical, submandibular, and inguinal regions [7]. MPXV infection typically takes 5 to 21 days to incubate before showing symptoms [25]. The disease itself is self-limiting, yet might cause serious illness and even death in several circumstances such as during pregnancy and immunocompromised conditions [22]. Clinical manifestations of MPXV have been found to vary in terms of their severity based on factors including age, gender, and immunization status [26].
Although most cases of mpox in the current outbreak are mild, severe illness as well as atypical and unusual clinical manifestations can occur in some people. The most common manifestations are fever and skin lesions. Yet, some patients may acquire severe manifestations, involving complications across many body systems, which might prove fatal. Fever, vomiting, malaise, conjunctivitis, and lymphadenopathy are prodromal signs. Nevertheless, several life-threatening consequences such as bronchopneumonia, vision-threatening keratitis, encephalitis, secondary bacterial infections, epiglottitis, acute renal damage, proctitis, and myocarditis have been reported [27,28].
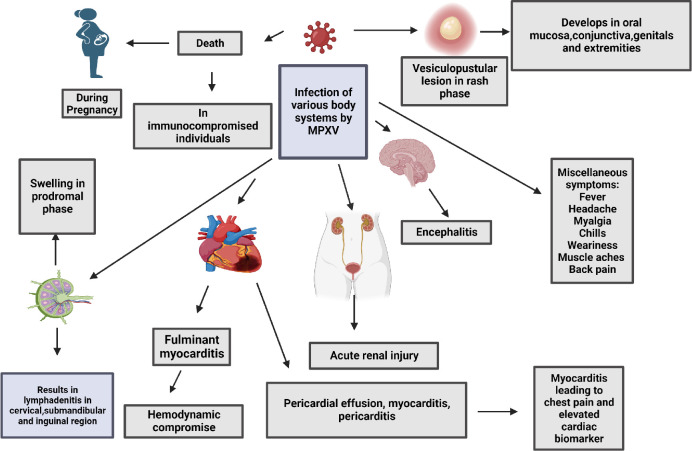
A pictorial depiction of the clinical manifestations and pathology of MPXV in mpox patients is presented in Figure 1.
Figure 1.
Clinical manifestations and pathology of monkeypox virus infection in affected patients.
MPXV infection is divided into two main phases: (1) the prodromal phase, which develops 4–17 days after viral exposure and lasts 0–3 days, and is characterized by swollen lymph nodes, fever, headache, chills, weariness, back pain, and muscular aches; and (2) the rash phase, which appears 3 days following the start of prodrome symptoms and lasts 7–21 days [29–32]. Typically, mpox has distinguishing lesions [15]; it is a painful or pruritic maculopapular rash that evolves into a vesiculopustular lesion. The rash is roughly the same size, well-circumscribed, and can spread, but usually concentrates more on the face and extremities. The conjunctiva, oral mucosa, genitals (30%), and extremities such as the palms and soles of the feet are also affected. In 10 days or less, the lesions often develop from the stage of macules through papules, vesicles, pustules, crusts, and scabs before falling off, and a new layer of skin or mucosa will be formed underneath [30,31,33]. The person is deemed contagious from the time of illness until all lesions have crusted over [34].
Additionally, studies have shown that MPXV infection also causes neurological symptoms, ranging from non-specific ones such as headache and myalgia to more uncommon ones such as seizures and encephalitis [35,36]. Unfortunately, the psychological effects or psychiatric manifestations associated with MPXV infection are still not well identified [14,37–39]. Special attention on how the MPXV might affect mental health is warranted as the WHO recently urged people to concentrate their attention on issues with mental health and suicide avoidance during disease epidemics [25,40].
It is also important to raise awareness about abnormal symptoms of the illness. For instance, the skin lesions are solely present at the site of sexual organs with the absence of prodromal symptoms [16,41,42]. Moreover, laboratory findings associated with mpox are still unclear as compared to smallpox in which thrombocytopenia and thrombocytopenia are obvious [43]. Furthermore, studies point to a link between MPXV infections and heart inflammatory disorders. It is important to not disregard chest pain in MPXV infected patients and to do a thorough examination to rule out myocarditis [4,44].
Acute renal injury, myocarditis, sepsis pneumonitis, eyesight-threatening keratitis, encephalitis, secondary bacterial infections, and conjunctivitis with corneal scarring, are among the severe sequelae-associated complications with MPXV infection. A patient's prognosis is based on the existence or absence of severe consequences, which rely on several variables, such as prior immunization status, baseline health state, and the occurrence of concomitant disorders and comorbidities [30,45,46].
It is critical to note that mpox cases may be mistaken for more commonly observed infections, including herpes simplex, molluscum contagiosum, varicella zoster, or sexually transmitted infections due to lesions in the vaginal and perianal regions [33]. Complex, atypical and unusual disease presentation along with asymptomatic MPXV infections reported amid the 2022 mpox outbreaks urges for enhancing prevention and control measures [40,47,48].
Myocarditis and its challenges
For a long time, myocarditis was thought to be caused by smallpox, a virus that is quite similar to MPXV but is much deadlier. Moreover, post-vaccination myocarditis and myopericarditis, both as cardiac consequences of smallpox immunization, have been described since the 1950s in Europe. Since the MPXV is closely related, it is reasonable to assume that it too may exhibit tropism for myocardial tissue or may cause immune-mediated harm to the heart [49,50]. Myocarditis has also been reported after receiving a smallpox vaccination, wherein virus replicates during vaccinia-based vaccinations in children and adolescents; consequently, the cardiac involvement of Orthopoxvirus infections has been documented [51,52]. Several case reports have revealed detailed symptoms that suggest clinically suspected myocarditis following the coronavirus disease 2019 (COVID-19). However, there have been limited cases of histologically confirmed myocarditis, and direct viral myocarditis caused by SARS-CoV-2 that has not been verified but is presumed based on epidemiological circumstances [44,53].
It is challenging to establish a myocarditis diagnosis because of its heterogeneous clinical findings and histological forms. Clinical findings and noninvasive procedures may be used to diagnose clinically suspected myocarditis, including echocardiography, electrocardiogram, and typical cardiac magnetic resonance (CMR) abnormalities [44]. Myocarditis is associated with ongoing or recurring symptoms and indicators of damage to the heart muscle. Both acute myocarditis and chronic inflammatory cardiomyopathy can result in ongoing or recurring symptoms and elevated indicators of heart muscle damage. In severe cases, myocarditis can lead to heart failure, cardiogenic shock, or other complications such as ventricular arrhythmias or high-degree atrioventricular block [54].
The prognosis of myocarditis mainly depends on the etiology and disease stage. Acute myocarditis is either recovered in a few weeks or worsens into persistent cardiac dysfunction and chronic inflammatory cardiomyopathy. Moreover, it might progress to fulminant myocarditis, with hemodynamic compromise and the need for cardiovascular support [55].
Myocarditis in mpox patients: the evidence
On March 12, 2023, we searched three databases (Scopus, Google Scholar, and PubMed) to obtain evidence on myocarditis in mpox patients. The search terms utilized were ("monkeypox" OR "monkeypox virus" OR "mpox") AND ("myocarditis" OR "pericarditis"). Two authors (SKA and MGM) selected the articles based on the titles and abstracts, followed by a screening of the full texts. Regardless of research design, language, or location, any article discussing myocarditis or myopericarditis of mpox in 2022 and 2023 were included. The detailed of the cases are presented in Table 1.
Table 1. Characteristics and outcomes of patients with myocarditis related to mpox and summary of pooled data from included published research papers have been reported in the literature (n=12).
| Author/Year of publication | Shaik et al. (2022) [56] | Rodriguez- Nava et al. (2022) [4] | Brouillard et al. (2022) [49] | Tan et al. (2022) [57] | Pinho et al. (2022) [44] | Guerrero et al. (2023) [58] | Dumont et al. (2022) [50] | Luis et al. (2023) [59] | Krainin et al. (20223) [60] | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| Country | USA | USA | Canada | Canada | Portugal | Spain | France | Puerto Rico | USA | |
| Study design | Case report | Case series | Case report | Case report | Case report | Case report | Case series | Case report | Case report | |
| Sample size | 1 | 2 | 1 | 1 | 1 | 1 | 3 | 1 | 1 | |
| Age (year) | 51 | 32 and 37 | 34 | 40 | 31 | 40 | 21, 25 and 32 | 21 | 31 | 32.9 years |
| Gender | Male | Male | Male | Male | Male | Male | Male | Male | 100% male | |
| Days to symptom | 7 | 15 and 13 | 3 | 12 | 8 | 14 | 6, 5 and 10 | 9 | NR | 8.4 days |
| onset | ||||||||||
| Presenting | Chest pain | Chest pain | Chest pain, | Chest pain | Chest pain | Chest pain | Chest pain | Chest pain, | Chest pain, | Chest pain, |
| symptom | dyspnea | dyspnea | dyspnea | dyspnea | ||||||
| Treatment | NSAIDs, | Tecovirimat, | Tecovirimat, | NR | NSAIDs | Tecovirimat, | Tecovirimat, | Aspirin | Tecovirimat, | |
| colchicine, | supportive | ACE inhibitor, | NSAIDs, | bisoprolol, | supportive | |||||
| aspirin, | care | NSAIDs | colchicine | ramipril | care | |||||
| nitroglycerin | ||||||||||
| Follow-up (day) | 7 | 10 and 4 | 10 | 25 | 7 | 6 | 30, 4 and 30 | 5 | NR | 12.5 days |
| Outcome | Recovered | Recovered | Recovered | Recovered | Recovered | Recovered | Recovered | Recovered | Recovered | 100% recovered |
NSAID: non-steroidal anti-inflammatory drug, NR: non reported
A total of nine studies with 12 mpox patients were examined. Four cases were from USA [4,56,60], three from France [50], two from Canada [49,57], one from Portugal [44], one from Spain [58], and one from Puerto Rico [59]. The patients' mean age was 32.9 years, with a range of 21 to 51 years, and all patients in these studies were male. The average time to symptom onset was 8.4 days, and chest pain was the primary symptom in all patients. Various medications, including NSAIDs, colchicine, aspirin, nitroglycerine, tecovirimat, and ACE inhibitors, were used to treat the patients. The follow-up period ranged from 4 to 30 days, with an average of 12.5 days, and one study did not provide follow-up data. All patients revealed recovery from their symptoms.
Rodriguez-Nava et al. noted that two mpox patients registered complain of chest pain, dyspnea, and elevated cardiac biomarkers, whereas echocardiography was normal without wall motion abnormalities [4]. A case report presented three cases of MPXV infection and suggested an association between MPXV infections and cardiovascular inflammatory sequelae [50]. Another case report showed that acute myocarditis affected an adult man with a confirmed MPXV infection after the eruption of skin lesions and myocardial inflammation was proved by cardiac magnetic resonance study [44]. Moreover, Sayad et al. mentioned in their systematic review that seven confirmed mpox cases had different cardiac complications, including pericardial effusion, pericarditis, myopericarditis, and acute myocarditis [61]. In addition, Thornhill et al. mentioned two incidences of self-limited myocarditis in mpox patients that cleared up in seven days without significant complications [62].
Myocarditis in mpox patients: The possible pathogeneses
Myocarditis is an inflammation of the myocardium that can lead to dilated cardiomyopathy, acute arrhythmia, and heart failure. Outcomes may vary depending on the type of myocarditis, with acute myocarditis often improving within a few weeks, chronic inflammatory cardiomyopathy requiring long-term treatment, and fulminant myocarditis requiring circulatory support measures due to severe hemodynamic impairment [45,63]. Myocarditis is known to be caused by viruses such as adenovirus, parvovirus B19, HIV, or enterovirus [50].
Histopathologic investigation of samples from viral vaccine recipients who developed myocarditis revealed no evidence of direct viral infection of the myocardial cells, leading some researchers to speculate that the disease is actually an autoimmune response [49,62]. Lymphocytic myocarditis with myonecrosis is the predominant pathogenesis of viral myocarditis, which typically manifests itself 10–14 days after infection and may be self-limiting or progress to fulminant myocarditis. Myocardial fibrosis, cardiac failure, and dilated cardiomyopathy are hallmarks of the non-infectious chronic phase of viral myocarditis.
The pathophysiology of MPXV-induced myocarditis remains undetermined due to the rarity of human cases of mpox-associated myocarditis. Most of the symptoms in myocarditis are moderate and self-limited; serious complications, such as dilated cardiomyopathy, are rare [64]. MPXV infection of cardiac muscle cells is a proposed mechanism for the development of myocarditis in mpox patients. The virus is able to infect a variety of host cells, including cardiac myocytes, which can result in inflammation and damage to the heart muscle tissue, ultimately leading to cell death.
An immunological response to the virus is another probable explanation for the development of myocarditis in mpox patients. When the immune system identifies a viral infection, it releases cytokines and other inflammatory mediators, which can lead to myocarditis [65]. In severe cases, the immune response can become uncontrollable and trigger a cytokine storm, resulting in an extensive tissue damage, including heart muscle injury [65].
In conclusion, the development of myocarditis in mpox patients is believed to entail both direct viral infection of the heart muscle cells and an immune-mediated response to the virus. Therefore, additional research is required to acquire a comprehensive understanding of the mechanisms behind the development of myocarditis in mpox patients
Conclusion and future prospects
The resurgence of mpox as a major threat to public health emphasizes the importance of maintaining high vigilance and investing in infectious disease research and response capabilities. It is critical to be ready to respond swiftly and effectively to such threats in order to reduce the impact they have on human health and well-being, as more outbreaks of emerging viruses and other diseases are predicted to occur in the future. Mpox has established itself as a global public health problem with its peak of outbreaks in 2022 revealing dynamic epidemiology and rapid spread to a large number of countries where it was not endemic.
Myocarditis is just one example of an unusual complication seen in mpox cases during current outbreak, highlighting the need for conducting more researches and developing effective vaccines and antiviral medicines along with adopting effectual infection prevention and control measures. Chest pain in an MPXV-infected patient should never be underestimated and there is need to always elicit early myocarditis investigations. It is important to investigate for MPXV infection in the differential diagnosis of myocarditis particularly during mpox outbreaks and incidences. Investigations on the pathogenesis and clinical features of mpox, such as the virus's ability to cause myocarditis are critical to be conducted.
Acknowledgments
The authors acknowledge their respective universities/institutes/organizations.
Ethics approval
Not required.
Conflict of interest
All the authors declare that there are no conflicts of interest.
Funding
This study received no external funding.
Underlying data
All data underlying the results are available as part of the article and no additional source data are required.
How to cite
Ahmed SK, Dabou EA, Abdelsamad S, et al. Monkeypox virus infection and myocarditis: A review of current evidence and possible pathogenesis. Narra J 2023; 3 (1): e104 - http://doi.org/10.52225/narra.v3i1.104.
References
- 1.Magnus P von, Andersen EK, Petersen KB, et al. A pox-like disease in cynomolgus monkeys. Acta Pathol Microbiol Scand 1959; 46 (2):156–76. [Google Scholar]
- 2.Hutin YJ, Williams RJ, Malfait P, et al. Outbreak of human monkeypox, Democratic Republic of Congo, 1996 to 1997. Emerg Infect Dis 2001; 7 (3):434–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ježek Z, Grab B, Szczeniowski M, et al. Clinico-epidemiological features of monkeypox patients with an animal or human source of infection. Bull World Health Organ 1988; 66 (4):459–464. [PMC free article] [PubMed] [Google Scholar]
- 4.Rodriguez-Nava G, Kadlecik P, Filardo TD, et al. Myocarditis attributable to monkeypox virus infection in 2 patients, United States, 2022. Emerg Infect Dis 2022; 28 (12):2508–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chandran D, Dhama K, Chakraborty S, et al. Monkeypox: An update on current knowledge and research advances. J Exp Biol Agric Sci 2022; 10:679–88. [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) . 2022 Monkeypox Outbreak Global Map. CDC 2022. Available from: https://www.cdc.gov/poxvirus/mpox/response/2022/world-map.html. Accessed: 2 April 2023. [Google Scholar]
- 7.MacNeil A, Abel J, Reynolds MG, et al. Serologic evidence of human orthopoxvirus infections in Sierra Leone. BMC Res Notes 2011; 4 (1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ježek Z, Szczeniowski M, Paluku KM, Mutombo M.. Human monkeypox: clinical features of 282 patients. J Infect Dis 1987; 156 (2):293–8. [DOI] [PubMed] [Google Scholar]
- 9.Reynolds MG, Carroll DS, Olson VA, et al. A silent enzootic of an orthopoxvirus in Ghana, West Africa: evidence for multi-species involvement in the absence of widespread human disease. Am J Trop Med Hyg 2010; 82 (4):746–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nolen LD, Osadebe L, Katomba J, et al. Extended human-to-human transmission during a monkeypox outbreak in the Democratic Republic of the Congo. Emerg Infect Dis 2016; 22 (6):1014–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ophinni Y, Frediansyah A, Sirinam S, et al. Monkeypox: Immune response, vaccination and preventive efforts. Narra J 2022; 2 (3):e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed SK, El-Kader RGA, Abdulqadir SO, et al. Monkeypox clinical symptoms, pathology, and advances in management and treatment options: an update. Int J Surg 2023; 109.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sah R, Abdelaal A, Reda A, et al. Monkeypox and its Possible Sexual Transmission: Where are we now with its evidence? Pathogens 2022; 11 (8):924.36015044 [Google Scholar]
- 14.Pastula DM, Tyler KL.. An overview of monkeypox virus and its neuroinvasive potential. Ann Neurol 2022; 92 (4):527–31. [DOI] [PubMed] [Google Scholar]
- 15.Minhaj FS, Ogale YP, Whitehill F, et al. Monkeypox outbreak—Nine states, May 2022. Am J Transplant 2022; 71 (23):764–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heskin J, Belfield A, Milne C, et al. Transmission of monkeypox virus through sexual contact-A novel route of infection. J Infect 2022; 83 (3):334–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chandran D, Nandanagopal VG, Gopan M.. Major advances in monkeypox vaccine research and development an update. J Pure Appl Microbiol 2022; 16 (suppl 1):3083–95. [Google Scholar]
- 18.Chakraborty S, Mohapatra RK, Chandran D, et al. Monkeypox vaccines and vaccination strategies: Current knowledge and advances. An update–Correspondence. Int J Surg 2022; 105:106869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed SK. Prevention, vaccination, management and infection control of monkeypox outbreak: an update global recommendation for the next year 2023. J Pure Appl Microbiol 2022; 16 (1):3189–91. [Google Scholar]
- 20.Rizk JG, Lippi G, Henry BM, Forthal DN, Rizk Y.. Prevention and treatment of monkeypox. Drugs 2022; 82:957–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chakraborty S, Chandran D, Mohapatra RK, et al. Clinical management, antiviral drugs and immunotherapeutics for treating monkeypox. An update on current knowledge and futuristic prospects. Int J Surg 2022; 105:106847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmed SK, Mohamed MG, Dabou EAAR, et al. Monkeypox (mpox) in immunosuppressed patients. F1000Research 2023; 12 (127):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmed SK, El-Kader RGA, Lorenzo JM, et al. Hospital-based salient prevention and control measures to counteract the 2022 monkeypox outbreak. Heal Sci Reports 2023; 6 (1):e1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Srivastava G, Srivastava G.. Human monkeypox disease. Clin Dermatol 2022; 40 (5):604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmed SK, Rashad EAA, Mohamed MG, et al. The global human monkeypox outbreak in 2022: An overview. Int J Surg 2022; 104:106794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karagoz A, Tombuloglu H, Alsaeed M, et al. Monkeypox (mpox) virus: Classification, origin, transmission, genome organization, antiviral drugs, and molecular diagnosis. J Infect Public Health 2023; 16 (4):531–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huhn GD, Bauer AM, Yorita K, et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin Infect Dis 2005; 41 (12):1742–51. [DOI] [PubMed] [Google Scholar]
- 28.Sukhdeo SS, Aldhaheri K, Lam PW, Walmsley S.. A case of human monkeypox in Canada. CMAJ 2022; 194 (29):E1031–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bunge EM, Hoet B, Chen L, et al. The changing epidemiology of human monkeypox—A potential threat? A systematic review. PLoS Negl Trop Dis 2022; 16 (2):e0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Girometti N, Byrne R, Bracchi M, et al. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: an observational analysis. Lancet Infect Dis 2022; 22 (9):1321–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yinka-Ogunleye A, Aruna O, Ogoina D, et al. Reemergence of human monkeypox in Nigeria, 2017. Emerg Infect Dis 2018; 24 (6):1149–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harapan H, Ophinni Y, Megawati D, et al. Monkeypox: A comprehensive review. Viruses 2022; 14 (10):2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chalali F, Merlant M, Truong A, et al. Histological features associated with human monkeypox virus infection in 2022 outbreak in a nonendemic country. Clin Infect Dis 2022:ciac856. [DOI] [PubMed] [Google Scholar]
- 34.Reynolds MG, Yorita KL, Kuehnert MJ, et al. Clinical manifestations of human monkeypox influenced by route of infection. J Infect Dis 2006; 194 (6):773–80. [DOI] [PubMed] [Google Scholar]
- 35.Billioux BJ, Mbaya OT, Sejvar J, Nath A.. Neurologic complications of smallpox and monkeypox: a review. JAMA Neurol 2022; 79 (11):1180–6. [DOI] [PubMed] [Google Scholar]
- 36.Badenoch JB, Conti I, Rengasamy ER, et al. Neurological and psychiatric presentations associated with human monkeypox virus infection: a systematic review and meta-analysis. EClinicalMedicine 2022; 52:101644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ogoina D, Mohammed A, Yinka-Ogunleye A, Ihekweazu C.. A case of suicide during the 2017 monkeypox outbreak in Nigeria. IJID Reg 2022; 3:226–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmed SK, Abdulqadir SO, Hussein SH, et al. The impact of monkeypox outbreak on mental health and counteracting strategies: A call to action. Int J Surg 2022; 106:106943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmed SK, Saied AA, Ravi RK, et al. The 2022 monkeypox outbreak and associated psychiatric morbidities. Int J Surg 2022; 106:106913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Otu A, Ebenso B, Walley J, Barceló JM, Ochu CL.. Global human monkeypox outbreak: atypical presentation demanding urgent public health action. The Lancet Microbe 2022; 3 (8):E554–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davido B, D'anglejan E, Jourdan J, Robinault A, Davido G.. Monkeypox 2022 outbreak: cases with exclusive genital lesions. J Travel Med 2022; 29 (6):taac077. [DOI] [PubMed] [Google Scholar]
- 42.A'aB A-T, Albakri R, Alabsi S.. The Outbreak of Human Monkeypox in 2022: A Changing epidemiology or an Impending aftereffect of smallpox eradication. Front Trop Dis 2022; 3:951380. [Google Scholar]
- 43.Tiecco G, Degli Antoni M, Storti S, Tomasoni LR, Castelli F, Quiros-Roldan E.. Monkeypox, a literature review: what is new and where does this concerning virus come from? Viruses 2022; 14 (9):1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pinho AI, Braga M, Vasconcelos M, et al. Acute myocarditis: a new manifestation of Monkeypox infection? Case Reports 2022; 4 (21):1424–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lampejo T, Durkin SM, Bhatt N, Guttmann O.. Acute myocarditis: aetiology, diagnosis and management. Clin Med (Northfield Il) 2021; 21 (5):e505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guarner J, Del Rio C, Malani PN.. Monkeypox in 2022—what clinicians need to know. JAMA 2022; 28 (2):139–40. [DOI] [PubMed] [Google Scholar]
- 47.Reda A, El-Qushayri AE, Shah J.. Asymptomatic monkeypox infection: a call for greater control of infection and transmission. The Lancet Microbe 2023; 4 (1):e15–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yuan S, Jiang S-C, Zhang Z-W, et al. Multi-origins and complex transmission paths of monkeypox viruses. Travel Med Infect Dis 2022; 50:102444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brouillard P, Valin-Thorburn A, Provost Y, et al. Monkeypox associated myocarditis: A case report. IDCases 2022; 30:e01628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dumont M, Guilhou T, Gerin M, et al. Myocarditis in monkeypox-infected patients: a case series. Clin Microbiol Infect 2022; 29 (3):390.e5-390.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mora LF, Khan AH, Sperling LS.. Cardiac complications after smallpox vaccination. South Med J 2009; 102 (6):615–9. [DOI] [PubMed] [Google Scholar]
- 52.Engler RJM, Nelson MR, Collins Jr LC, et al. A prospective study of the incidence of myocarditis/pericarditis and new onset cardiac symptoms following smallpox and influenza vaccination. PLoS One 2015; 10 (3):e0118283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ahmed SK. Myocarditis after BNT162b2 and mRNA-1273 COVID-19 vaccination: A report of 7 cases. Ann Med Surg 2022:103657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sanromán Guerrero MA, Sánchez EH, Ruanes B de N, et al. Case report: From monkeypox pharyngitis to myopericarditis and atypical skin lesions. Front Cardiovasc Med 2023; 9:1046498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Caforio ALP, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2013; 34 (33):2636–48. [DOI] [PubMed] [Google Scholar]
- 56.Shaik TA, Voloshyna D, Nasr TH, et al. Monkeypox-Associated Pericarditis: A Maiden Case. Cureus 2022; 14 (9):e29638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tan DHS, Jaeranny S, Li M, et al. Atypical clinical presentation of monkeypox complicated by myopericarditis. Open Forum Infect Dis 2022; 9: 2022:ofac394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Guerrero MAS, Sánchez EH, de Nicolás Ruanes B, et al. Case report: From monkeypox pharyngitis to myopericarditis and atypical skin lesions. Front Cardiovasc Med 2023; 9:1046498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Luis IV E, Pabón-González F, Colón-Fontánez F.. Monkeypox induced acute myocarditis in a young healthy adult. JAAD Case Reports 2023; 34:5–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Krainin J, Harris C, Bugni WJ, Mester SW, Milani D.. Monkeypox Myocarditis. J Am Coll Cardiol 2023; 81 (8_Supplement):2494. [Google Scholar]
- 61.Sayad R, Siddiq A, Hashim A, Elsaeidy AS.. Can the current monkeypox affect the heart? A Comprehensive Systematic Review. Res Sq 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox virus infection in humans across 16 countries—April–June 2022. N Engl J Med 2022; 387:679–91. [DOI] [PubMed] [Google Scholar]
- 63.Sozzi FB, Gherbesi E, Faggiano A, et al. Viral myocarditis: classification, diagnosis, and clinical implications. Front Cardiovasc Med 2022; 9:908663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morgan J, Roper MH, Sperling L, et al. Myocarditis, pericarditis, and dilated cardiomyopathy after smallpox vaccination among civilians in the United States, January–October 2003. Clin Infect Dis 2008; 46 (Supplement_3):S242–50. [DOI] [PubMed] [Google Scholar]
- 65.Martens CR, Accornero F.. Viruses in the heart: direct and indirect routes to myocarditis and heart failure. Viruses 2021; 13 (10):1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required.