Abstract
Children are susceptible and a potential source of transmission for coronavirus disease 2019 (COVID-19). However compulsory COVID-19 vaccination programs among children have not been a focus in Malaysia. The aim of this study was to measure parents’ willingness to pay (WTP) for the COVID-19 vaccine and analyze the effects of socioeconomic variables on parents’ WTP. An online cross-sectional study was conducted in Malaysia with two waves of surveys (i.e., different samples for each wave), March and June 2021. The study participants were Malaysian parents above 18 years old. Parents were randomized between two vaccine effectiveness profiles (95% and 50% effectiveness) and two risk levels of an adverse event (5% and 20% risk of fever). The WTP was estimated using a double-bounded dichotomous choice. Socioeconomic variables such as age of parent, gender, insurance, income, and education were examined. A total of 292 parents in March 2021 and 271 in June 2021 were included in the study. The vaccine safety and effectiveness profile did not significantly impact the WTP. In March 2021, the estimated WTP ranged from RM344.74 to RM399.64 (US$82.5 to US$95.6) across vaccine profiles and between RM377.55 and RM444.33 (US$90.3 to US$106.3) in June. Insurance status was associated with the parents’ WTP, and during the June wave, the age of parents influenced the WTP. Implementing subsidies or free vaccinations is considerable to increase herd immunity and prevent transmission of COVID-19 in Malaysia.
Keywords: COVID-19 vaccination, children, parent, willingness-to-pay, Malaysia
Introduction
As of November 21, 2021, Southeast Asia recorded more than 44 million cumulative confirmed cases and 700,000 associated deaths of coronavirus disease 2019 (COVID-19) since the onset of the pandemic [1]. During the same period, Malaysia reported more than 2.5 million cumulative cases and more than 30,000 associated deaths period [2]. Malaysia has undergone three waves of COVID-19, with the initial reported on January 25, 2020, followed by the second wave on March 18, 2020, and the third wave on September 8, 2020 [3]. The government enforced multiple phases of movement restrictions and implemented public health preventative measures such as physical distancing, mandatory wearing of face masks, and contact tracing [4,5].
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for COVID-19, appears to transmit with a relatively high basic reproduction number (R0) [6] and can infect people of all ages including children. In Malaysia, COVID-19 cases among children aged between 5 to 11 years old made up around 9−11% of total confirmed cases between September and November 2021 [2]. Generally, most COVID-19 cases in children are either asymptomatic or mild, although severe manifestations or deaths have been reported in children with underlying health conditions [7-9]. Despite the severity, prolonged COVID-19 symptoms have also been reported in children [10,11]. Moreover, the development of multisystem inflammatory syndrome (MIS) associated with COVID-19 further complicates the recovery from COVID-19 in children [10,12]. These children could potentially transmit the virus to others including vaccinated parents with low immune response [13]. In the absence of a definitive cure, a safe and effective COVID-19 vaccine is much needed to protect children and their families from COVID-19.
As of November 17, 2021, more than 52 million doses of vaccines have been administered and 76.6% of the population has been fully vaccinated since Malaysia commenced its National COVID-19 Immunization Programme (NIP) on February 24, 2021 [2,14]. In the United States of America (USA), the Food and Drug Administration (FDA) authorized the Pfizer-BioNTech COVID-19 vaccine for emergency use in children 5−11 years old on October 29, 2021 [15]. Following that, the Malaysian government proceeded to procure the vaccine formulation for children and was expected to receive its first batch of vaccines towards the end of the second quarter of 2022 [16]. In March 2022, only 35.58% of Malaysian children aged 5−11 years old were vaccinated, emphasizing the need for parental assurance and support for their vaccination [17]. However, vaccine uptake in the country is voluntary, and the decision to vaccinate the children is within the purview of the parents and/or other guardians [18]. A study reported that 33.8% of people were not in favor of the vaccination before the vaccination introduction [19].
Studies on parental acceptance and willingness to pay (WTP) for vaccines for their children are important but yet limited. A study among parents in the USA found that parents were willing to pay between USD228 to USD321 for their children’s vaccine and the WTP was directly associated with the number of children within the family [20]. Other studies reported the parents’ or guardians’ intention to vaccinate their children ranges from 33% to 85% [21-34]. This wide disparity in COVID-19 vaccination acceptance for children has been observed globally and is associated with sociodemographic characteristics, routine vaccinations, vaccine safety and effectiveness, along with other factors [35-37]. Recognizing that parents’ acceptance and WTP play an important role in the vaccination program for children, the aim of the study was to measure parents’ WTP for the COVID-19 vaccine and analyze the effects of socioeconomic variables on parents’ WTP.
Methods
Study design
A cross-sectional study was conducted in Malaysia with two waves of surveys (i.e., different samples for each wave) between March and June 2021. Details of the study are available elsewhere [35]. In the original study, eligibility criteria included Malaysian residences and being 18 years or older.
Sampling method and participants
The sample of individuals in this study was selected through social media and advertisements by the market survey research firm Dynata. Participants could access the survey in either English or Bahasa Malaysia. According to the original study’s aims [35], we attempted to obtain a sample size of 800 for each wave of data collection. This assumes that the margin of error was 4%, with an alpha of 0.05, a power of 80%, and a proportion of 50% (a statistically conservative estimate of the population willing to pay). In this additional analysis, we further limit our sample to individuals who were parents of children <18 years old.
Study variables and data collection
Prior to assessing the WTP, the participants were asked: “Would you accept a COVID-19 vaccine for your child which is (95%) effective, with a (5%) risk of a side effect like fever? (95%) effective means that there is a (95%) reduction in disease among those vaccinated compared to those unvaccinated.” Participants were then randomized to one of four groups, with effectiveness varying between 95% and 50%, and risk of fever as side effects varying between 5% and 20%. We varied the vaccine profile in this way because previous studies have shown that parents have strong concerns about the safety and effectiveness of the vaccine [36-37].
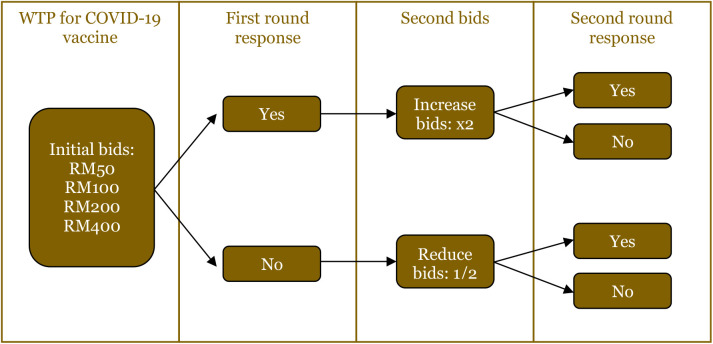
The parent’s WTP for the vaccine was then followed with WTP questions. A double-bounded dichotomous choice question was adopted in this study. The double dichotomous choice contingent valuation (CV) questioned if participants were willing to purchase the vaccine at stated bid amounts (Figure 1). The bids were changed (either increased by double the initial bid or decreased by half) in the second round and were asked for a second response to the change. The initial bid amounts of RM50, RM100, RM200, and RM400 were randomly distributed among different participants. This study used an exchange rate of 1 USD = RM4.18 as of October 2021.
Figure 1. Flowchart of how willingness to pay (WTP) was measured during the survey.
We examined the following socioeconomic variables: age of parent, gender, insurance, income, and education. In our multivariable models, age was inserted as a continuous variable. The other variables were dichotomous. For income, we dichotomized into less or above RM3000 ($717.70), and for education, we dichotomized based on high school or less, if not university or above. For insurance, we dichotomized based on whether the individual had any medical insurance (regardless of source).
Statistical analysis
Two statistical analyses were conducted. First, we displayed basic summary statistics. Second, the data obtained using a double-bounded dichotomous choice (DBDC) format was analyzed using a probabilistic WTP function approach [38,39]. The main function underlying this approach is a linear model for the true WTP value for the ith respondent (WTPi):
Where xi is a vector of socio-demographic characteristics, β is a corresponding vector of coefficients, and εi is an error term. Information from the responses to the discrete choice question and an assumed distribution for εi can then be used to define probabilities for the WTPi and subsequently, to estimate the vector β using maximum likelihood estimation procedures [38]. The error term was assumed to be normally distributed. Two models were estimated. The first model only included an intercept in xi; thus, the estimated β can be interpreted as the unconditional mean WTP value. The second model included various demographic characteristics in xi; therefore, β is the vector of marginal effects on the mean WTP (i.e., they are interpreted as the coefficients of a linear regression model). The Stata software (StataCorp, Texas, USA) was used to estimate the model [38]. We assessed significance at an alpha level of 0.05.
Results
Participants’ characteristics
A total of 749 responses were obtained in March 2021 and 779 in June 2021, of these, 446 (59.6%) and 450 (57.8%) were parents, respectively. Individuals with missing demographic information were excluded, leaving a final total of 292 parents in March 2021 and 271 in June 2021 with WTP for children vaccination, as presented in Table 1. In both waves, a majority of parents were female (52.1% and 52.4%) and aged 35 to 54 (54.8% and 53.14%). Most of the parents in both waves earned an income of over RM3000 (88.36% and 78.97%) and were ethnically Malay (75% and 67.53%). Many parents in both waves had insurance (82.88% and 78.60%) and were employed (89.04% and 84.87%). Moreover, a vast majority of the parents were from urban areas and had a tertiary degree.
Table 1: Characteristics of parents in the two-waves-survey in Malaysia.
| Variable | March 2021 Frequency (%) | June 2021 Frequency (%) |
|---|---|---|
| Age | ||
| 18−34 | 120 (41.1) | 103 (38.00) |
| 35−54 | 160 (54.8) | 144 (53.14) |
| ≥55 | 12 (4.1) | 24 (8.86) |
| Gender | ||
| Male | 140 (47.9) | 129 (47.6) |
| Female | 152 (52.1) | 142 (52.4) |
| Income | ||
| Less than RM3000 | 34 (11.64) | 57 (21.03) |
| RM3000 or higher | 258 (88.36) | 214 (78.97) |
| Ethnic | ||
| Malay | 219 (75.0) | 183 (67.53) |
| Non-Malay | 73 (25) | 88 (32.47) |
| Insurance | ||
| Yes | 242 (82.88) | 213 (78.60) |
| No | 50 (17.12) | 58 (21.40) |
| Employment | ||
| Employed | 260 (89.04) | 230 (84.87) |
| Unemployed | 32 (10.96) | 41 (15.13) |
| State | ||
| Johor | 54 (18.49) | 48 (17.7) |
| Kedah | 11 (3.77) | 13 (4.8) |
| Kelantan | 11 (3.77) | 12 (4.4) |
| Perak | 15 (5.14) | 7 (2.6) |
| Selangor | 60 (20.55) | 68 (25.1) |
| Melaka | 16 (5.48) | 5 (1.8) |
| Negeri Sembilan | 10 (3.42) | 8 (3) |
| Pahang | 14 (4.79) | 13 (4.8) |
| Perlis | 2 (0.68) | 0 (0) |
| Penang | 16 (5.48) | 20 (7.4) |
| Sabah | 12 (4.11) | 22 (8.1) |
| Sarawak | 13 (4.45) | 8 (3) |
| Terengganu | 6 (2.05) | 9 (3.3) |
| Wilayah Persekutuan, Kuala Lumpur | 51 (17.47) | 37 (13.7) |
| Labuan | 1 (0.34) | 1 (0.4) |
| Rural | ||
| Yes | 140 (47.95) | 129 (47.60) |
| No | 152 (52.05) | 142 (52.40) |
| Education | ||
| University or above | 241 (82.53) | 187 (69.00) |
| High school or less | 51 (17.47) | 84 (31.00) |
Willingness to pay for childhood COVID-19 vaccine and its associated factors
A model of WTP with only the vaccine effectiveness and safety profile found that neither vaccine profile variable significantly affected WTP. In extended models that also adjusted for socioeconomic variables, other variables beyond the safety and effectiveness profile were significantly associated (Table 2). In the March wave, those with insurance were significantly more likely to have a higher WTP (RM241.77 higher, or $57.18). In June 2021, age was significantly associated with WTP, with each increasing year of age being willing to pay RM5.78 less ($1.38).
Table 2. Estimation result of parents’ willingness to pay (WTP) for childhood COVID-19 vaccines in linear regression models, Malaysia.
| Variable | March 2021 (RM) | June 2021 (RM) | ||
|---|---|---|---|---|
| Basic model | Extended model | Basic model | Extended model | |
| Constant | 293.59 (96.27)* | 146.18 (154.14) | 343.76 (91.69)* | 504.40 (154.32)* |
| Effectiveness | 0.94 (1.09) | 1.08 (1.05) | 1.12 (1.10) | 1.22 (1.09) |
| Risk | 0.84 (3.29) | 0.87 (3.21) | -1.09 (3.30) | -1.72 (3.24) |
| Age | -3.58 (2.45) | -5.78 (2.14) * | ||
| Gender | 116.32 (48.45) | 3.04 (49.01) | ||
| Insurance | 241.77 (65.78)* | 19.34 (61.22) | ||
| Income | 98.19 (77.22) | 1.74 (67.94) | ||
| Education | -90.45 (68.81) | 54.16 (60.56) | ||
| Sigma | 360.55 (27.17)* | 342.68 (25.68) * | 337.76 (26.89)* | 328.21 (26.17)* |
| Sample size | 292 | 292 | 271 | 271 |
| Wald chi | 0.78 | 21.50 | 1.10 | 9.61 |
| p-value | 0.67 | 0.0031 | 0.58 | 0.21 |
| Log-likelihood | -387.39 | -376.54 | -302.13 | -297.89 |
Standard errors in parentheses
Statistically significant at p<0.001
Across both waves, WTP was higher for a 95% effective vaccine vs. a 50% effective vaccine (Table 3). For example, in March 2021, a 95% effective vaccine with a 5% risk of fever had a WTP of RM386.96 (95% CI: 200.73−473.20), whereas a 50% effective vaccine with a 5% risk was RM344.74 (95% CI: 255.05−434.43). There was less of a difference in modifying the risk percentage even with the same effectiveness. Between March 2021 and June 2021, there were increases in the amount of parents’ WTP, especially for a vaccine that was 95% effective with a 5% risk of fever, for which individuals in June 2021 were willing to pay RM57.37 more.
Table 3. Mean willingness to pay (WTP) across different vaccine profiles.
| Vaccine profile | March 2021 | June 2021 | Differences in WTP between June compared to March | ||
|---|---|---|---|---|---|
| Mean WTP | 95% CI | Mean WTP | 95% CI | ||
| 95% efficacy, 5% risk | RM386.96 | 300.73- | RM444.33 | 358.58- | RM57.37 |
| (US$92.6) | 473.20 | (US$106.3) | 530.08 | (US$13.7) | |
| 95% efficacy, 20% risk | RM399.64 | 315.67- | RM427.94 | 342.70- | RM28.3 |
| (US$95.6) | 483.61 | (US$102.4) | 513.18 | (US$6.8) | |
| 50% efficacy, 5% risk | RM344.74 | 255.05- | RM393.93 | 309.56- | RM49.19 |
| (US$82.5) | 434.43 | (US$94.2) | 478.31 | (US$11.8) | |
| 50% efficacy, 20% risk | RM357.41 | 274.51- | RM377.55 | 285.93- | RM20.14 |
| (US$85.5) | 440.32 | (US$90.3) | 469.15 | (US$4.8) | |
Discussion
Currently, many high- and middle-income countries are instituting programs to vaccinate children against COVID-19; however, there is insufficient information regarding parents’ will to accept. WTP can be seen as an indicator of the overall acceptance of the COVID-19 vaccination program and the inclination to vaccinate the children. Even if vaccines are subsidized by the government, there may be other financial and time-cost factors in obtaining a vaccination [40].
This study found slightly over half of the parents were willing to pay for a COVID-19 vaccine for their children. A similar finding was observed in a study from Kuwait that demonstrated a low willingness of parents to vaccinate their children [41]. Inadequate vaccination coverage among children increases vulnerability to COVID-19, especially when attending schools and following parents to crowded public places. Adults, who are more susceptible to severe COVID-19, especially those with low antibody response after vaccination, may be at risk if children serve as carriers of the virus [42,43]. This study indicated that financial subsidies would be essential to motivate and maintain adequate childhood vaccination coverage. These subsidies, whether provided by the government, insurance, or private companies, can help mitigate economic barriers to self-funded vaccines.
This study found that the estimated WTP for children COVID-19 vaccine in Malaysia ranged between RM344.74 (US$82.5) and RM399.64 (US$95.6) during March 2021 and from RM377.55 (US$90.3) to RM444.33 (US$106.3) in June 2021. The increase in WTP from March to June was possibly influenced by a marked surge in the daily incidence of cases in the country from 1,828 on 1st March to 7,105 on 1st June, and an increase in deaths from 5 to 71 [44]. Another study performed in the USA showed that WTP for childhood COVID-19 vaccines was almost three times higher, i.e., US$243–US$321, compared to this study [20]. However, the mean WTP for COVID-19 vaccination in China was lower, i.e. US$36.8 [45]. The observed differences may be influenced by disparities in average income levels among different countries.
In Malaysia, health insurance can be either acquired personally or obtained as an employee work benefit. This may reflect the importance of health protection by ensuring health insurance coverage and indirectly by warranting health protection for their children through purchasing the COVID-19 vaccine as a preventive measure [45]. Despite possessing private health insurance, they may access both private and public health services which provide primary and outpatient centers, hospitalization, diagnostic laboratories, and pharmaceuticals including vaccines. This study demonstrated a significant relationship among parents having health insurance with WTP for the COVID-19 vaccine for their children which aligns with studies for Zika and chikungunya vaccines in Brazil [46,47]. There are also consistent positive effects between having health insurance and the quality of health life of parents which would indirectly apply to attentiveness to their children’s well-being by vaccination [48,49].
Although several factors above have an impact on the WTP of the parents, this study showed an increase in parental age was associated with a lower WTP for a vaccine. This finding was parallel to a previous study in Indonesia in which older participants were less willing to pay compared to their younger counterparts for a dengue vaccine [50].
Several limitations of this study should be noted when generalizing the findings. First, these studies included the possibility of bias among the participants selected from social media platforms as reported previously [51]. This could produce sampling bias where the results were less representative of individuals who are not active on social media or lack internet access. Second, this study asked about the WTP based on a hypothetical vaccine with fever as the only side effect. There could be other considerations of the vaccine profile, including specific preferences for certain brands. Third, during the movement control order throughout the COVID-19 pandemic, some parents lost their jobs, affecting monthly income, which may influenced their set of priorities. Last, this study included cross-sectional data which cannot estimate causal relationships. The bidding game approach may introduce bias.
Conclusion
The availability of COVID-19 vaccines for children presents an opportunity to vaccinate a larger proportion of the population, thereby increasing herd immunity and preventing transmission within children. However, parents’ low willingness to obtain or pay for a COVID-19 vaccine could limit the distribution of the vaccine among children. This study found potential differences in WTP by age and insurance status, therefore, implementing subsidies or free vaccinations is considerable.
Acknowledgments
We appreciate the work of Mengdi Ji and Kaitlyn Akel in preparing the datasets.
Ethical approval
The Scientific and Ethical Review Committee of Universiti Tunku Abdul Rahman (U/SERC/17/2020) and the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (HUM00180096) approved the study protocol.
Competing interests
The authors declare that there is no conflict of interest.
Funding
This project was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number K01AI137123.
Underlying data
Derived data supporting the findings of this study are available from the corresponding author on request.
How to cite
Rajamoorthy Y, Wagner AL, Kumaran VV, et al. Parents’ willingness to pay for COVID-19 vaccination for children in Malaysia using the contingent valuation method. Narra J 2023; 3 (3): e187 - http://doi.org/10.52225/narra.v3i3.187.
References
- 1.World Health Organization. 2021. Available fromml: https://covid19.who.int/. Accessed: 22 December 2021.
- 2.Ministry of Health Malaysia. 2021. Available fromml: https://covidnow.moh.gov.my/. Accessed: 22 December 2021.
- 3.Rampal L, Liew BS. Malaysia’s third COVID-19 wave - a paradigm shift required. The Med J Malays 2021;76(1):1–4. [PubMed] [Google Scholar]
- 4.Opel DJ, Diekema DS, Ross LF. Should we mandate a COVID-19 vaccine for children? JAMA Pediatr 2021;175(2):125–126. [DOI] [PubMed] [Google Scholar]
- 5.Mathieu E, Ritchie H, Rodés-Guirao L, et al. 2020. Coronavirus Pandemic (COVID-19). Available fromml: https://ourworldindata.org/coronavirus. Accessed: 22 December 2021.
- 6.Muhamad Khair NK, Lee KE, Mokhtar M.. Community-based monitoring in the new normal: A strategy for tackling the COVID-19 pandemic in Malaysia. Int J Environ Res Public Health 2021;18(13):6712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castagnoli R, Votto M, Licari A, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: A systematic review. JAMA Pediatr 2020;174(9):882–889. [DOI] [PubMed] [Google Scholar]
- 8.Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr 2020;109(6):1088–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Preston LE, Chevinsky JR, Kompaniyets L, et al. Characteristics and disease severity of US children and adolescents diagnosed with COVID-19. JAMA Netw Open 2021;4(4):e215298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buonsenso D, Munblit D, De Rose C, et al. Preliminary evidence on long COVID in children. Acta Paediatr 2021;110(7):2208–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ludvigsson JF. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr 2021;110(3):914–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldstein LR, Tenforde MW, Friedman KG, et al. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA 2021;325(11):1074–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu D. Children’s immunity at risk. New Sci 2021;250(3332):8–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Straits Times. PM Muhyiddin receives first Covid-19 vaccine as Malaysia kicks off mass inoculation campaign. https://www.straitstimes.com/asia/se-asia/pm-muhyiddin-receives-first-covid-19-vaccine-as-malaysia-kicks-off-mass-inoculation. Accessed 22 December 2021.
- 15.FDA. FDA authorizes Pfizer-BioNTech COVID-19 vaccine for emergency use in children 5 through 11 years of age. https://www.fda.gov/news-events/press-announcements/fda-authorizes-pfizer-biontech-covid-19-vaccine-emergency-use-children-5-through-11-years-age. Accessed 22 December 2021.
- 16.Nordin MH, Ismail Z, Rusli MF. COVID-19 vaccines are safe and work for children. Available fromml: https://codeblue.galencentre.org/2022/03/22/malaysias-child-covid-19-vaccination-stalls-at-under-40/. Accessed 14 October 2023.
- 17.Cheah FC, Thong MK, Zulkifli I, et al. COVID-19 vaccination for children in Malaysia - A position statement by the College of Paediatrics, Academy of Medicine of Malaysia. Malays J Pathol 2022;44(2):177–185. [PubMed] [Google Scholar]
- 18.Wong L-P, Lee H-Y, Alias H, AbuBakar S.. Malaysian parents’ willingness to vaccinate their children against COVID-19 infection and their perception of mRNA COVID-19 vaccines. Vaccines 2022;10(11):1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CodeBlue. Khairy: Children’s Covid-19 vaccines only arriving end June. https://codeblue.galencentre.org/ 2021/11/22/khairy-childrens-covid-19-vaccines-only-arriving-end-june/. Accessed 22 December 2021.
- 20.Catma S, Reindl D.. Parents’ willingness to pay for a COVID-19 vaccine for themselves and their children in the United States. Hum Vaccin Immunother 2021;17(9):2919–2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.AlHajri B, Alenezi D, Alfouzan H, et al. Willingness of parents to vaccinate their children against influenza and the novel coronavirus disease-2019. J Pediatr 2021;231:298–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bell S, Clarke R, Mounier-Jack S, et al. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020;38(49):7789–7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davis MM, Zickafoose JS, Halvorson AE, Patrik SW. Parents’ likelihood to vaccinate their children and themselves against COVID-19. medRxiv 2020:1–9.
- 24.Goldman RD, Marneni SR, Seiler M, et al. Caregivers’ willingness to accept expedited vaccine research during the COVID-19 pandemic: a cross-sectional survey. Clin Ther 2020;42(11):2124–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hetherington E, Edwards SA, MacDonald SE, et al. Covid-19 vaccination intentions among Canadian parents of 9–12 year old children: Results from the All Our Families longitudinal cohort. medRxiv 2020:1–13.
- 26.Yigit M, Ozkaya-Parlakay A, Senel E.. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J 2021;40(4):e134–e136. [DOI] [PubMed] [Google Scholar]
- 27.Yılmazbaş NP. Did covid-19 pandemic changed parents’ approach to vaccination? Erciyes Med J 2020;43:130–134. [Google Scholar]
- 28.Jeffs E, Lucas N, Walls T.. COVID-19: Parent and caregiver concerns about reopening New Zealand schools. J Paediatr Child Health 2021;57(3):403–408. [DOI] [PubMed] [Google Scholar]
- 29.Akarsu B, Canbay Ozdemir D, Ayhan Baser D, et al. While studies on COVID-19 vaccine is ongoing, the public’s thoughts and attitudes to the future COVID-19 vaccine. Int J Clin Pract 2021;75(4):e13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yılmaz M, Sahin MK. Parents’ willingness and attitudes concerning the COVID-19 vaccine: A cross-sectional study. Int J Clin Pract 2021;75(9):e14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skjefte M, Ngirbabul M, Akeju O, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: Results of a survey in 16 countries. Eur J Epidemiol 2021;36(2):197–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akel, Kaitlyn B, Grace A.et al. A Study of COVID-19 Vaccination in the US and Asia: The Role of Media, Personal Experiences, and Risk Perceptions. PLOS Global Public Health 2022;2(7):e0000734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nguyen KH, Nguyen K, Corlin L, et al. Changes in COVID-19 vaccination receipt and intention to vaccinate by socioeconomic characteristics and geographic area, United States, January 6–March 29, 2021. Ann Med 2021;53(1):1419–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kyprianidou M, Fakonti G, Tzira E, et al. Associations between socio-demographic characteristics and maternal attitudes towards childhood vaccination in Cyprus—A cross-sectional survey. COVID 2023;3(7):1042–1051. [Google Scholar]
- 35.Zhang F, Shih S-F, Harapan H, et al. Changes in COVID-19 risk perceptions: Methods of an internet survey conducted in six countries. BMC Res Notes. BioMed Central 2021;14(1):148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldman RD, Yan TD, Seiler M, et al. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020;38(48):7668–7673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang KC, Fang Y, Cao HE, et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: Cross-sectional online survey. JMIR Pediatr Parent 2020;3(2):e24827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lopez-Feldman A. Introduction to contingent valuation using Stata. (2012). Available fromml: https://www.econpapers.repec.org/paper/pramprapa/41018.htm. Accessed 3 September 2021.
- 39.Sarasty O, Carpio CE, Hudson D, et al. The demand for a COVID-19 vaccine in Ecuador. Vaccine 2021;38(51):8090–8098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thomson A, Robinson K, Vallée-Tourangeau G.. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine 2016;34(8):1018–1024. [DOI] [PubMed] [Google Scholar]
- 41.AlHajri B, Alenezi D, Alfouzan H, et al. Willingness of parents to vaccinate their children against influenza and the novel coronavirus disease-2019. J Pediatr 2021;231:298–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levin EG, Lustig Y, Cohen C, et al. Waning immune humoral response to BNT162b2 Covid-19 vaccine over 6 months. NEJM 2021;385(24):e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Müller L, Andrée M, Moskorz W, et al. Age-dependent immune response to the Biontech/Pfizer BNT162b2 COVID-19 vaccination. MedRxiv 2021;73(11):2065–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Coronavirus cases. Available fromml: https://www.worldometers.info/coronavirus/country/malaysia/. Accessed: 22 October 2021.
- 45.Wang J, Lyu Y, Zhang H, et al. Willingness to pay and financing preferences for COVID-19 vaccination in China. Vaccine 2021;39(14):1968–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muniz Junior RL, Godói IP, Reis EA., et al. Consumer willingness to pay for a hypothetical Zika vaccine in Brazil and the implications. Expert Rev Pharmacoecon Outcomes Res 2019;19(4):473–482. [DOI] [PubMed] [Google Scholar]
- 47.Sarmento TTR, Godói IP, Reis EA, et al. Consumer willingness to pay for a hypothetical chikungunya vaccine in Brazil and the implications. Expert Rev Pharmacoecon Outcomes Res 2019;22(3):513–520. [DOI] [PubMed] [Google Scholar]
- 48.Gebru T, Lentiro K.. The impact of community-based health insurance on health-related quality of life and associated factors in Ethiopia: A comparative cross-sectional study. Health Qual Life Outcomes 2018;16(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fan H, Yan Q, Coyte PC, Yu W.. Does public health insurance coverage lead to better health outcomes? Evidence from Chinese adults. Inquiry 2019;56:0046958019842000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hadisoemarto PF, Castro MC. Public acceptance and willingness-to-pay for a future dengue vaccine: A community-based survey in Bandung, Indonesia. PLoS Negl Trop Dis 2013;7(9):e2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sallam M, Anwar S, Yufika A, et al. Willingness-to-pay for COVID-19 vaccine in ten low-middle-income countries in Asia, Africa and South America: A cross-sectional study. Narra J. 2022;2(1):e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Derived data supporting the findings of this study are available from the corresponding author on request.