Abstract
Vaccine hesitancy is considered as one of the greatest challenges to control the ongoing coronavirus disease 2019 (COVID-19) pandemic. A related challenge is the unwillingness of the general public to pay for vaccination. The objective of this study was to determine willingness-to-pay (WTP) for COVID-19 vaccine among individuals from ten low- middle-income countries (LMICs) in Asia, Africa, and South America. Data were collected using an online questionnaire distributed during February - May 2021 in ten LMICs (Bangladesh, Brazil, Chile, Egypt, India, Iran, Nigeria, Pakistan, Sudan, and Tunisia). The major response variable of in this study was WTP for a COVID-19 vaccine. The assessment of COVID-19 vaccine hesitancy was based on items adopted from the World Health Organization (WHO) Strategic Advisory Group of Experts (SAGE) vaccine hesitancy scale constructs. In this study, 1337 respondents included in the final analysis where the highest number of respondents was from India, while the lowest number was from Egypt. A total of 88.9% (1188/1337) respondents were willing to pay for the COVID-19 vaccination, and 11.1% (149/1337) were not. The average WTP for COVID-19 vaccination was 87.9 US dollars ($), (range: $5-$200). The multivariate model analysis showed that the country, monthly household income, having a history of respiratory disease, the agreement that routine vaccines recommended by health workers are beneficial and having received the flu vaccination within the previous 12 months were strongly associated with the WTP. Based on the country of origin, the highest mean WTP for COVID-19 vaccine was reported in Chile, while the lowest mean WTP for the vaccine was seen among the respondents from Sudan. The availability of free COVID-19 vaccination services appears as a top priority in the LMICs for successful control of the ongoing pandemic. This is particularly important for individuals of a lower socio- economic status. The effects of complacency regarding COVID-19 extends beyond vaccine hesitancy to involve less willingness to pay for COVID-19 vaccine and a lower value of WTP for the vaccine.
Keywords: COVID-19, SARS-CoV-2, acceptance, hesitancy, value, WHO SAGE
Introduction
Two years have passed since the declaration of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), as a global pandemic [1,2]. Besides the noticeable devastating health effects of COVID-19, the pandemic resulted in a negative impact on various aspects of life, including a drop in economic growth, exposed vulnerabilities in healthcare systems and adverse psychological and social impacts all over the world [3–5].
An important noticeable feature of the ongoing COVID-19 pandemic is the continuous emergence of SARS-CoV-2 variants, attributed mainly to the swift genetic changes in the spike gene of the virus [6–8]. Subsequently, the emergence of highly transmissible variants and the selection of variants with immune escape properties appear as an expected outcome [9,10].
Vaccination to protect from SARS-CoV-2 infection and/or COVID-19 illness has been advocated as the safest and most efficient approach to prevent virus transmission and to reduce morbidity and mortality from COVID-19 [11,12]. Various COVID-19 vaccines have been approved for use and until recently, the World Health Organization (WHO) has recommended nine different types of vaccine that are both safe and effective [11,13–15]. Despite the successful role of various COVID-19 vaccines in reducing SARS-CoV-2 transmission, as well as its helpful role in reducing morbidity and mortality from the disease, a major concern is the continuous emergence of virus variants, with reduce efficacy of the currently approved COVID-19 vaccines towards such variants [9,16–19].
The effectiveness of COVID-19 vaccination in real-world setting depends on the level of vaccine uptake. In turn, the vaccine uptake is multifactorial, with psychologic, social, religious, ethical and economic factors determining the acceptance, hesitancy or rejection of vaccination [20-23]. The economic factors appear of extreme importance in the context of COVID-19 pandemic, due to the pandemic's discernible negative impact on the economic activities and the reduced employment in different regions worldwide [24,25]. The detrimental economic effect of COVID-19 is more pronounced among low-income countries with subsequent limited resources allocated for vaccine purchasing and manufacturing [26].
For SARS-CoV-2, experts estimate that 70% to 90% of the population needs to be immune to achieve population immunity [27,28]. Despite the fact that COVID-19 vaccination has been proven safe and effective, not everyone has shown willingness to receive it, a phenomenon known as COVID-19 vaccine hesitancy [29,30]. This phenomenon appears more profound if people have to pay to get vaccinated [31,32]. A previous study from China has shown that 79% of the participants expressed a willingness to get vaccinated against COVID-19; nevertheless, almost 50% were unwilling to pay more than 100 yuan (USD ($)15.78) for vaccination [33]. Another recent study from Nigeria showed that out of 1,767 participants, only 26% were willing to pay for COVID-19 vaccination [34].
Several studies on the willingness-to-pay (WTP) for COVID-19 vaccine have been conducted in various countries worldwide, including in the US, China, Chile, India, Malaysia, Ecuador, Nigeria and Indonesia, with WTP for vaccination being associated with participants of higher-income groups [32-40]. However, gaps in knowledge regarding WTP for COVID-19 vaccination still exist, especially in low-middle-income countries (LMICs) in Asia, Africa, and South America. Previous studies have shown that a majority of people in some LMICs are still hesitant to get vaccinated against COVID-19, particularly in the Middle East and North Africa [29,41,42]. The rising number of unemployed people due to COVID-19 can complicate this problem, further reducing the number of people willing to pay for the vaccine. In addition, if the government does not provide subsidies, the possibility of willing to pay for vaccination will diminish subsequently leading to augmented vaccine hesitancy and rejection. Therefore, the objective of this study was to assess the WTP for COVID-19 vaccine, defined by the maximum amount of money that individual is willing to pay for a product or service, and its associated determinants in ten LMICs in Asia, Africa, and South America. The findings of this study are expected to be used by governments not just in these nations, but also in other LMICs, to develop proper strategies for dealing with the problem of vaccination financing in the future. The results may also be utilized to take make the required effort to promote COVID-19 vaccination.
Methods
Study setting and instrument
Between February to May 2021, an online survey was conducted in four Asian countries (Bangladesh, India, Iran, and Pakistan), four African countries (Egypt, Nigeria, Sudan, and Tunisia), and two South American countries (Brazil and Chile). All the countries are classified as LMICs. The survey was hosted by SurveyMonkey and to recruit the participants, invitations to participate in the survey were distributed on three social media and instant messaging platforms: Facebook, Twitter and WhatsApp. The survey comprised several sections as follows: the first introductory section provided information about the study and an item for electronic informed consent. Only those who agreed to participate could open the next section. The following sections comprised items to assess the demographic characteristics of the participant, current health condition, economic disruption during COVID-19 pandemic and experience for influenza vaccination during the past 12 years. It required approximately 10-15 minutes to complete the survey.
Response variables
The response variable of the study was WTP for a COVID-19 vaccine. To assess the WTP, the respondents were provided with a scenario: “Imagine that a new COVID-19 vaccine has just been developed. It has received the same testing as the adult influenza vaccine. The COVID-19 vaccine has 95% effectiveness level and a 5% chance of side effects like fever or local pain. Would you like to buy the vaccine and get vaccinated if the price of the vaccine is [US dollar ($) 5, 12.5, 25, 50, 100 and 200]”. The bid was randomly assigned, for example if a respondent was willing to pay at $25, then the bid was increased to $50; while if unwilling to pay, the bid was reduced to $12.5. In some countries, the bids were given in the local currency. The possible responses for each bid were “Yes” or “No” and the highest bid where the participant responded “Yes” was defined as the WTP. If the participant responded “No” at the lowest bid ($5), then this respondent was classified as not willing to pay for the vaccine. If the respondent agreed to pay at the highest bid ($200), the follow-up question asking the highest vaccine price that would be paid by the respondent was given and this price was defined as the WTP.
Explanatory variables
Some possible explanatory variables were collected and assessed. Demographic characteristics were collected and grouped for statistical proposes: age (≤ 20, 21-30, 31-40, 41-50 and > 51 years), sex, urbanicity (rural vs. urban), monthly household income ($500, 500-999, 1,000-1,999, 2,000-2,999, 3,000-4,999, 5,000-7,999 and ≥8,000), religion (Islam, Protestant Christian (Protestant/Methodist/Lutheran/Baptist), Catholic, Hindu, and others (Mormon, Greek or Russian Orthodox, Jewish, and Buddhist) and atheist or agnostic, type of job (healthcare-related sector and non-healthcare-related sector), and type of occupation (self- employed, employed for wages, out of work for less or more than one year, homemaker, student and retired or unable to work). Respondents were also asked whether they had comorbidities such as hypertension, diabetes mellitus, cardiopulmonary disease and whether they had received a flu vaccination in the previous 12 months.
We also inquired about the economic disruption experience of the respondents by asking two questions: “How much has your work changed as a result of the COVID-19 pandemic?” and “How much has your salary changed as a result of the COVID-19 pandemic?“ The possible answers for the first question were: “I work fewer hours”, “No change or not applicable (not working)”, “I work more hours“ and “I was let go from my job”. Three possible responses were provided for the last question: “I am getting paid less”, “I am getting paid more” or “No change”.
In addition, the attitude towards the benefit of vaccination and social distancing were assessed. To assess COVID-19 vaccine hesitancy, five questions belonging to lack of vaccination benefits construct from the World Health Organization (WHO) Strategic Advisory Group of Experts (SAGE) Vaccine Hesitancy Scale were used [43]: (1) “Vaccines are important for my health”; (2) “All routine vaccines recommended by the healthcare workers are beneficial”; (3) “New vaccines carry more risks than older vaccines”; (4) “The information I receive about vaccines from the government is reliable and trustworthy”; and (5) “Getting vaccines is a good way to protect me from disease”. The possible responses for each statement were in 5-Likert scale from “Strongly agree”, Strongly agree”, “Neither agree nor disagree”, “Disagree” and “Strongly disagree”. For statistical purpose, the responses of the individual were classified as “Disagree” (those who answered disagree and strongly disagree), “Neutral” (neither agree nor disagree) and “Agree” (those who responded agree or strongly agree).
Statistical analysis
In determining associated factors affecting WTP, a linear regression model was employed. First, diagnostic analyses were performed to examine multicollinearity, heteroscedasticity, and residual normality assumptions. To assess multicollinearity assumption, the Variance Inflation Factor (VIF) was used. A VIF lower than 10 indicates there is no substantial multicollinearity between determinants in the model [44]. Heteroscedasticity and residual normality assumptions were examined using Glejser test and Kolmogorov–Smirnov test [45,46]. For both tests, a p value greater than 0.05 indicated that the residuals have a constant variance (homoscedasticity) and are distributed normally. The initial diagnostic assessments showed that the model with WTP as dependent variable did not fulfill all assumptions. Moreover, the distribution of WTP data was right skewed. The WTP data as a dependent variable were therefore converted using log transformation, which is widely accepted and have been previously [47-52]. In performing linear regression analysis, all independent variables were translated into dummy indicators where one of the categories was designated as the reference category. In the initial model, all determinants were included. Only determinants with p<0.05 in the initial model were included in the final model. The mean of the estimated WTP and its confidence interval were calculated as described previously [47,48]. The formula of was used to estimate the mean of WTP, where the and were estimated regression coefficients and the mean squared error (MSE) of the regression model, respectively [53,54].
Results
Characteristics of the study respondents
Out of 1,337 respondents from ten LMICs, a total of 1,188 (88.9%) were willing to pay for a COVID-19 vaccine and were included in final analysis. The highest number of respondents was from India (n=256, 21.5%), while the lowest number was from Egypt (n=71, 6.0%) (Table 1). Overall, there was a slight female predominance (n=670, 56.4%), and the majority of the respondents aged between 21-40 years (n=876, 73.7%). A total of 202 respondents (17.0%) came from rural areas and the majority of respondents were Muslims (n=607, 51.1%). Regarding occupation, students dominated among the study respondents (n=694, 58.4%), followed by employees for wages (n=295, 24.8%). A small minority of respondents reported a comorbidity such as hypertension, diabetes mellitus, heart disease, or respiratory disease (5.9%, 3.5%, 3.3%, and 5.5% respectively). The vast majority of respondents strongly agreed or agreed that vaccines are important for health (n=1071, 90.2%); nevertheless, only 22.1% of the respondents reported flu vaccine uptake during the previous 12 months. The detailed characteristics of the respondents are presented in (Table 1).
Table 1. Demographic characteristics of the participants who were willing to pay for COVID-19 vaccination (n=1,188).
| Variable | Number (%) |
|---|---|
| Country | |
| Pakistan | 149 (12.5) |
| Brazil | 97 (8.2) |
| Chile | 100 (8.4) |
| Egypt | 71 (6.0) |
| India | 256 (21.5) |
| Iran | 100 (8.4) |
| Nigeria | 108 (9.1) |
| Bangladesh | 98 (8.2) |
| Sudan | 117 (9.8) |
| Tunisia | 92 (7.7) |
| Age group (year) | |
| ≤20 | 188 (15.8) |
| 21-30 | 692 (58.2) |
| 31-40 | 184 (15.5) |
| 41-50 | 80 (6.7) |
| >50 | 44 (3.7) |
| Sex | |
| Male | 518 (43.6) |
| Female | 670 (56.4) |
| Urbanicity | |
| Rural | 202 (17.0) |
| Urban | 986 (83.0) |
| Monthly household income (USD) | |
| <500 | 418 (35.2) |
| 500-999 | 240 (20.2) |
| 1,000-1,999 | 160 (13.5) |
| 2,000-2,999 | 116 (9.8) |
| 3,000-4,999 | 95 (8.0) |
| 5,000-7,999 | 76 (6.4) |
| ≥8,000 | 83 (7.0) |
| Religion | |
| Islam | 607 (51.1) |
| Christian (Protestant/Methodist/Lutheran/Baptist) | 124 (10.4) |
| Catholic | 104 (8.8) |
| Hindu | 196 (16.5) |
| Atheist or agnostic | 119 (10.0) |
| Others | 38 (3.2) |
| Healthcare-related job | |
| No | 639 (53.8) |
| Yes | 549 (46.2) |
| Having hypertension | |
| No | 810 (68.2) |
| Yes | 67 (5.6) |
| Do not know | 311 (26.2) |
| Having diabetes mellitus | |
| No | 878 (73.9) |
| Yes | 37 (3.1) |
| Do not know | 273 (23.0) |
| Having heart disease | |
| No | 809 (68.1) |
| Yes | 31 (2.6) |
| Do not know | 348 (29.3) |
| Having respiratory disease | |
| No | 771 (64.9) |
| Yes | 64 (5.4) |
| Do not know | 353 (29.7) |
| Occupation | |
| Self-employed | 111 (9.3) |
| Employed for wages | 295 (24.8) |
| Out of work | 52 (4.4) |
| Homemaker | 21 (1.8) |
| Student | 694 (58.4) |
| Retired or unable to work | 15 (1.3) |
| Has how much your work changed as a result of the COVID-19 pandemic? | |
| I work fewer hours | 198 (16.7) |
| No change and not applicable (not working) | 728 (61.3) |
| I work more hours | 229 (19.3) |
| I was let go from my job | 33 (2.8) |
| Has how much your salary changed as a result of the COVID-19 pandemic? | |
| I am getting paid less | 335 (28.2) |
| I am getting paid more | 83 (7.0) |
| No changes | 770 (64.8) |
| Vaccines are important for my health | |
| Disagree or strongly disagree | 12 (1.0) |
| Neither agree nor disagree | 105 (8.8) |
| Agree or strongly agree | 1071 (90.2) |
| All routine vaccines recommended by the healthcare workers are beneficial | |
| Disagree or strongly disagree | 35 (2.9) |
| Neither agree nor disagree | 159 (13.4) |
| Agree or strongly agree | 994 (83.7) |
| New vaccines carry more risks than older vaccines | |
| Agree or strongly agree | 411 (34.6) |
| Neither agree nor disagree | 478 (40.2) |
| Disagree or strongly disagree | 299 (25.2) |
| The information I receive about vaccines from the government is reliable and | |
| Disagree or strongly disagree | 185 (15.6) |
| Neither agree nor disagree | 368 (31.0) |
| Getting vaccines is a good way to protect me from disease | |
| Disagree or strongly disagree | 19 (1.6) |
| Neither agree nor disagree | 107 (9.0) |
| Agree or strongly agree | 1062 (89.4) |
| Received influenza vaccination during the previous 12 months | |
| No | 925 (77.9) |
| Yes | 263 (22.1) |
Willingness-to-pay for COVID-19 vaccine and its explanatory variables
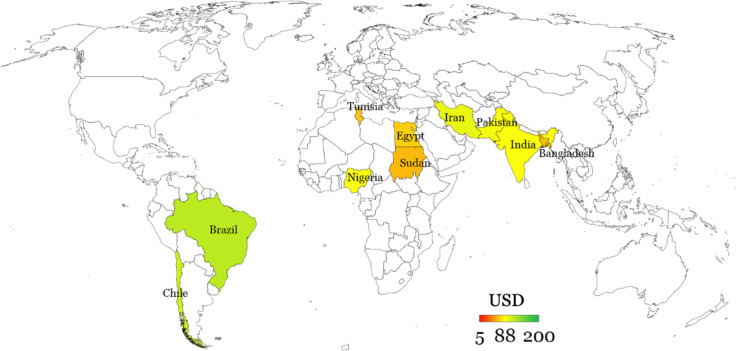
The analysis included 1,337 participants who provided complete information. A total of 1,188 (88.9%) respondents were willing to pay for the COVID-19 vaccine while 11.1% (149/1,337) of the participants were not willing to pay for the vaccine, which does not imply unwillingness to get the vaccine if it is provided for free. The average WTP the participants were willing to spend for COVID-19 vaccination was $87.9. Based on the country of origin, the highest WTPs came from Brazil while the lowest was from Sudan with $119.02 and $64.33, respectively (Figure 1).
Figure 1.
The mean value in US dollars that the respondents were willing to spend for COVID-19 vaccine (n=1,188).
The initial linear regression model revealed that the country, monthly household income, health-related occupation, having a history of respiratory disease, the agreement that routine vaccines recommended by health workers are beneficial, and having received the flu vaccination within the previous 12 months were correlated with WTP (p<0.05) (Table 2). All of these explanatory variables were included in the final linear regression model.
Table 2. Initial multivariable linear regression model showing factors associated with the willingness to pay for COVID-19 vaccination (n=1,188).
| Variable | Unstandardized coefficients | US dollar ($) estimate | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| B | 95% CI of B | MSE | Mean | 95% CI | ||||
| Lower | Upper | Lower | Upper | |||||
| Country (Pakistan) | ||||||||
| Brazil | 0.168 | -0.225 | 0.561 | 0.200 | 2.005 | -0.011 | 4.020 | 0.403 |
| Chile | 0.226 | -0.163 | 0.615 | 0.198 | 2.124 | 0.108 | 4.140 | 0.255 |
| Egypt | -0.181 | -0.495 | 0.133 | 0.160 | 1.415 | -0.601 | 3.430 | 0.258 |
| India | -0.156 | -0.497 | 0.184 | 0.174 | 1.450 | -0.566 | 3.465 | 0.368 |
| Iran | -0.081 | -0.393 | 0.231 | 0.159 | 1.563 | -0.452 | 3.579 | 0.611 |
| Nigeria | 0.128 | -0.229 | 0.484 | 0.182 | 1.926 | -0.089 | 3.942 | 0.482 |
| Bangladesh | -0.257 | -0.554 | 0.040 | 0.151 | 1.311 | -0.705 | 3.326 | 0.089 |
| Sudan | -0.555 | -0.851 | -0.260 | 0.151 | 0.973 | -1.043 | 2.989 | <0.001 |
| Tunisia | -0.481 | -0.796 | -0.165 | 0.161 | 1.048 | -0.968 | 3.064 | 0.003 |
| Age group (year) (<20) | ||||||||
| 21-30 | -0.129 | -0.319 | 0.061 | 0.097 | 1.490 | -0.525 | 3.506 | 0.184 |
| 31-40 | -0.069 | -0.343 | 0.204 | 0.139 | 1.582 | -0.434 | 3.598 | 0.621 |
| 41-50 | 0.112 | -0.222 | 0.446 | 0.170 | 1.895 | -0.121 | 3.911 | 0.512 |
| >51 | 0.245 | -0.158 | 0.648 | 0.205 | 2.165 | 0.150 | 4.181 | 0.233 |
| Gender (Male) | ||||||||
| Female | 0.041 | -0.089 | 0.171 | 0.066 | 1.767 | -0.249 | 3.783 | 0.532 |
| Urbanicity (Rural) | ||||||||
| Urban | 0.018 | -0.149 | 0.185 | 0.085 | 1.726 | -0.290 | 3.742 | 0.832 |
| Monthly household income (USD) (<500) | ||||||||
| 500-999 | -0.077 | -0.250 | 0.096 | 0.088 | 1.569 | -0.447 | 3.585 | 0.381 |
| 1,000-1,999 | 0.231 | 0.032 | 0.430 | 0.101 | 2.136 | 0.120 | 4.152 | 0.023 |
| 2,000-2,999 | -0.060 | -0.290 | 0.170 | 0.117 | 1.596 | -0.420 | 3.612 | 0.607 |
| 3,000-4,999 | 0.124 | -0.121 | 0.369 | 0.125 | 1.920 | -0.096 | 3.935 | 0.319 |
| 5,000-7,999 | 0.117 | -0.151 | 0.385 | 0.137 | 1.906 | -0.110 | 3.922 | 0.391 |
| ≥8,000 | 0.268 | 0.001 | 0.535 | 0.136 | 2.215 | 0.200 | 4.231 | 0.049 |
| Religion (Islam) | ||||||||
| Christian/Protestant/Methodist/Lutheran/Baptist | -0.250 | -0.531 | 0.030 | 0.143 | 1.320 | -0.696 | 3.336 | 0.080 |
| Catholic | -0.316 | -0.637 | 0.005 | 0.164 | 1.236 | -0.780 | 3.252 | 0.054 |
| Hindu | -0.022 | -0.317 | 0.272 | 0.150 | 1.658 | -0.358 | 3.673 | 0.881 |
| Atheist or agnostic | -0.181 | -0.464 | 0.103 | 0.144 | 1.415 | -0.601 | 3.431 | 0.211 |
| Others | -0.258 | -0.629 | 0.113 | 0.189 | 1.309 | -0.706 | 3.325 | 0.172 |
| Healthcare-related job (No) | ||||||||
| Yes | 0.140 | 0.002 | 0.278 | 0.070 | 1.949 | -0.066 | 3.965 | 0.047 |
| Have hypertension (No) | ||||||||
| Yes | -0.062 | -0.355 | 0.232 | 0.150 | 1.594 | -0.422 | 3.610 | 0.680 |
| Do not know | -0.013 | -0.207 | 0.180 | 0.099 | 1.673 | -0.343 | 3.688 | 0.893 |
| Have diabetes (No) | ||||||||
| Yes | 0.002 | -0.385 | 0.389 | 0.197 | 1.698 | -0.317 | 3.714 | 0.992 |
| Do not know | -0.086 | -0.295 | 0.123 | 0.106 | 1.556 | -0.460 | 3.572 | 0.421 |
| Have heart disease (No) | ||||||||
| Yes | 0.106 | -0.308 | 0.520 | 0.211 | 1.885 | -0.131 | 3.900 | 0.616 |
| Do not know | 0.123 | -0.102 | 0.348 | 0.115 | 1.916 | -0.099 | 3.932 | 0.285 |
| Have pulmonary disease (No) | ||||||||
| Yes | 0.220 | -0.065 | 0.504 | 0.145 | 2.111 | 0.096 | 4.127 | 0.130 |
| Do not know | -0.280 | -0.504 | -0.055 | 0.115 | 1.282 | -0.734 | 3.297 | 0.015 |
| Occupation (Self-employed) | ||||||||
| Employed for wages | -0.043 | -0.279 | 0.193 | 0.121 | 1.624 | -0.392 | 3.640 | 0.722 |
| Out of work | 0.169 | -0.185 | 0.524 | 0.181 | 2.008 | -0.008 | 4.024 | 0.349 |
| Homemaker | -0.141 | -0.643 | 0.361 | 0.256 | 1.472 | -0.544 | 3.488 | 0.581 |
| Student | -0.176 | -0.416 | 0.064 | 0.122 | 1.421 | -0.594 | 3.437 | 0.150 |
| Retired or unable to work | -0.090 | -0.662 | 0.483 | 0.292 | 1.550 | -0.466 | 3.566 | 0.759 |
| Has how much your work changed as a result of the COVID-19 pandemic? (I work fewer hours) | ||||||||
| No change and not applicable (not working) | 0.001 | -0.172 | 0.174 | 0.088 | 1.696 | -0.319 | 3.712 | 0.993 |
| I work more hours | 0.015 | -0.190 | 0.220 | 0.105 | 1.721 | -0.295 | 3.737 | 0.886 |
| I was let go from my job | 0.162 | -0.237 | 0.561 | 0.203 | 1.994 | -0.022 | 4.010 | 0.425 |
| Has how much your salary changed as a result of the COVID-19 pandemic? (I am getting paid less) | ||||||||
| I am getting paid more | 0.070 | -0.194 | 0.335 | 0.135 | 1.819 | -0.197 | 3.835 | 0.601 |
| No changes | 0.079 | -0.068 | 0.226 | 0.075 | 1.835 | -0.181 | 3.850 | 0.292 |
| Vaccines are important for my health (Disagree or strongly disagree) | ||||||||
| Neither agree nor disagree | -0.332 | -1.008 | 0.343 | 0.344 | 1.216 | -0.800 | 3.232 | 0.335 |
| Agree or strongly agree | -0.241 | -0.898 | 0.417 | 0.335 | 1.332 | -0.683 | 3.348 | 0.473 |
| All routine vaccines recommended by the healthcare workers are beneficial (Disagree or strongly disagree) | ||||||||
| Neither agree nor disagree | 0.423 | 0.026 | 0.819 | 0.202 | 2.587 | 0.571 | 4.603 | 0.037 |
| Agree or strongly agree | 0.713 | 0.337 | 1.088 | 0.191 | 3.458 | 1.442 | 5.473 | <0.001 |
| New vaccines carry more risks than older vaccines (Agree or strongly agree) | ||||||||
| Neither agree nor disagree | -0.034 | -0.175 | 0.108 | 0.072 | 1.639 | -0.377 | 3.655 | 0.640 |
| Disagree or strongly disagree | 0.100 | -0.067 | 0.267 | 0.085 | 1.873 | -0.142 | 3.889 | 0.242 |
| The information I receive about vaccines from the government is reliable and trustworthy (Disagree or strongly disagree) | ||||||||
| Neither agree nor disagree | -0.101 | -0.298 | 0.096 | 0.100 | 1.532 | -0.483 | 3.548 | 0.315 |
| Agree or strongly agree | 0.125 | -0.070 | 0.319 | 0.099 | 1.920 | -0.096 | 3.936 | 0.209 |
| Getting vaccines is a good way to protect me from disease (Disagree or strongly disagree) | ||||||||
| Neither agree nor disagree | -0.057 | -0.614 | 0.500 | 0.284 | 1.602 | -0.414 | 3.617 | 0.841 |
| Agree or strongly agree | 0.103 | -0.433 | 0.639 | 0.273 | 1.879 | -0.136 | 3.895 | 0.706 |
| Having flu vaccination during the past 12 months (No) | ||||||||
| Yes | 0.225 | 0.066 | 0.384 | 0.081 | 2.123 | 0.107 | 4.139 | 0.006 |
| MSE | 1.056 | |||||||
| F-value (p<0.001) | 3.818 | |||||||
| R2 | 0.159 | |||||||
CI: Confidence interval; MSE: Mean squared error
The results of the multivariate model analysis on the previously included variables showed that the country, monthly household income, having a history of respiratory disease, the agreement that routine vaccines recommended by health workers are beneficial and having received the flu vaccination within the previous 12 months were strongly associated with the WTP (p<0.05) (Table 3). Participants with income ≥$8,000 and having a history of respiratory disease had a higher WTP compared to those with income <$500 and those who reported had no history of respiratory disease, approximately $2.21 and $1.99, respectively. Participants who agreed that routine vaccines recommended by health workers are beneficial and had the flu vaccination within the previous 12 months had a higher WTP approximately $3.62 and $2.21, respectively compared to those who disagreed that routine vaccines are beneficial and who had no flu vaccination within last year (Table 3).
Table 3. Final model multivariable linear regression model showing factors associated with the willingness to pay for COVID-19 vaccination (n=1,188).
| Variable | Unstandardized coefficients | US dollar ($) estimate | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| B | 95% CI of B | SE | Mean | 95% CI | ||||
| Lower | Upper | Lower | Upper | |||||
| Country (Pakistan) | ||||||||
| Brazil | 0.022 | -0.259 | 0.304 | 0.143 | 1.746 | -0.284 | 3.775 | 0.878 |
| Chile | 0.060 | -0.218 | 0.338 | 0.142 | 1.813 | -0.216 | 3.843 | 0.671 |
| Egypt | -0.263 | -0.565 | 0.039 | 0.154 | 1.313 | -0.717 | 3.342 | 0.087 |
| India | -0.168 | -0.400 | 0.064 | 0.118 | 1.443 | -0.586 | 3.473 | 0.155 |
| Iran | -0.060 | -0.335 | 0.215 | 0.140 | 1.608 | -0.421 | 3.637 | 0.669 |
| Nigeria | 0.050 | -0.215 | 0.315 | 0.135 | 1.795 | -0.234 | 3.824 | 0.711 |
| Bangladesh | -0.301 | -0.573 | -0.029 | 0.139 | 1.264 | -0.765 | 3.293 | 0.030 |
| Sudan | -0.549 | -0.822 | -0.276 | 0.139 | 0.986 | -1.043 | 3.016 | <0.001 |
| Tunisia | -0.509 | -0.791 | -0.226 | 0.144 | 1.027 | -1.003 | 3.056 | <0.001 |
| Monthly household income (USD) (<500) | ||||||||
| 500-999 | 0.153 | -0.026 | 0.321 | 0.086 | 1.990 | -0.039 | 4.019 | 0.760 |
| 1,000-1,999 | 0.224 | 0.281 | 0.420 | 0.100 | 2.137 | 0.107 | 4.166 | 0.005 |
| 2,000-2,999 | -0.261 | -0.012 | -0.036 | 0.115 | 1.315 | -0.714 | 3.344 | 0.919 |
| 3,000-4,999 | 0.373 | 0.173 | 0.615 | 0.123 | 2.480 | 0.451 | 4.509 | 0.159 |
| 5,000-7,999 | 0.754 | 0.175 | 1.016 | 0.133 | 3.628 | 1.599 | 5.658 | 0.191 |
| ≥8,000 | 0.260 | 0.325 | 0.522 | 0.134 | 2.214 | 0.185 | 4.243 | 0.015 |
| Healthcare-related job (No) | ||||||||
| Yes | 0.153 | 0.021 | 0.285 | 0.067 | 1.990 | -0.039 | 4.019 | 0.024 |
| Have pulmonary disease (No) | ||||||||
| Yes | 0.224 | -0.044 | 0.492 | 0.137 | 2.137 | 0.107 | 4.166 | 0.101 |
| Do not know | -0.261 | -0.397 | -0.126 | 0.069 | 1.315 | -0.714 | 3.344 | <0.001 |
| All routine vaccines recommended by the healthcare workers are beneficial (Disagree or strongly disagree) | ||||||||
| Neither agree nor disagree | 0.373 | -0.011 | 0.758 | 0.196 | 2.480 | 0.451 | 4.509 | 0.057 |
| Agree or strongly agree | 0.754 | 0.400 | 1.108 | 0.180 | 3.628 | 1.599 | 5.658 | <0.001 |
| Having flu vaccination during the past 12 months (No) | ||||||||
| Yes | 0.260 | 0.105 | 0.415 | 0.079 | 2.214 | 0.185 | 4.243 | 0.001 |
| MSE | 1.070 | |||||||
| F-value (p<0.001) | 7.671 | |||||||
| R2 | 0.121 | |||||||
CI: Confidence interval; MSE: Mean squared error
Discussion
In light of the economic negative impact of COVID-19 pandemic, the economic determinants of vaccine acceptance and the possible need for booster doses of COVID-19 vaccination to protect from SARS-CoV-2 variants, the current study aimed to assess the willingness to pay for COVID-19 vaccine in ten LMICs. The major findings of this study included the observation that a majority of respondents (89%) showed willingness to pay for COVID-19 vaccine; albeit with variability in the mean and maximum values depending on country of origin, monthly income, occupation, and previous uptake of flu vaccination in the past 12 months. Another major result of this study entailed the finding that the mean value the respondents were willing to pay for COVID-19 vaccine was $87.9 with a range of $5 up to $200.
Several factors influence the public's WTP for vaccination in general and for COVID-19 vaccination in particular, such as general protection level and duration, possible side effects, and socioeconomic factors reflected in income level among others [32,47,48,55,56]. Among the most important of these factors is the general belief that the vaccine can prevent transmission and minimize the risks associated with infection [31,57,58].
According to the findings of this study, only 11% (149/1337) of the respondents showed unwillingness to pay for COVID-19 vaccination, whereas the majority of those who responded to our survey were willing to pay for the vaccine. Although it is unclear how much they must pay, considering the current status of free availability of vaccines in many countries, the findings of this study showed that the respondents were willing to pay up to $87.9 on average. Similarly, a study that was conducted in China soon after the declaration of COVID-19 as a pandemic showed the willingness of a majority (81%) of the general public to pay for the vaccine in the country [59]. However, the rate of willingness to pay for the vaccine was much lower in a recent study from Nigeria with only 26% of the participants showing willingness to pay a fee for COVID-19 vaccination, which highlights the importance of free vaccination services in resource- limited settings [60].
To put the results of this study into a broader perspective, a few studies with similar objectives were conducted recently; nevertheless, these studies were conducted at a country level contrary to our approach of investigating this aim in ten LMICs. One of the earliest studies to tackle willingness of the general public to pay for COVID-19 vaccine was conducted in Chile by García and Cerda [61], which found that WTP was $185, in line with our results which showed that respondents from Chile were more willing to pay for the vaccine. Additionally, the previously mentioned study showed the association of willingness to pay for the vaccine with the existence of chronic disease and income level which is consistent with our results [61].
An early study from Malaysia also showed the importance of income level as a determinant for willingness to pay for COVID-19 vaccine; even though the study by Wong et al showed that the average WTP for the vaccine was lower ($31) compared to our study [62]. Such a result highlights the continuous need for the investigation of WTP for COVID-19 vaccines in various countries, particularly in LMICs. A similar pattern of correlation between the high income and more inclination to pay for COVID-19 vaccine was also seen in a study from Indonesia, with an average WTP value of $57 [32]. A higher average value for willingness to pay for the vaccine ($86) was reported from Vietnam in early 2020 [63], while a much higher mean value for WTP ($319) for the vaccine that was seen in a study from the United States, given the vaccine provides a 3-year protection at a 95% efficacy [64]. This discrepancy can be related mainly to classification of different countries based on the income level, and is supported by generally low mean and median values that respondents from LMICs were willing to pay for COVID-19 vaccine (mean WTP of $5 in Ethiopia, median WTP of $7 in Bangladesh, WTP of $50-68 in Kenya, mean WTP of $15 for an 80% effective vaccine in Iran, and a maximum WTP of $60 in Lebanon) [65-69].
The observation that individuals with low-income levels have displayed lower levels of WTP for COVID-19 vaccination can be attributed to a variety of factors, including the lack of funds, other pressing issues, or holding the belief that it is the governments’ responsibility to provide the vaccines for free. In line with this result, previous research has also shown that individuals with higher income were willing to pay more for the COVID-19 vaccination than those with lower income [33,35,70].
In this study, the results indicated that the respondents with a history of respiratory disease were also more willing to pay for COVID-19 vaccination than those without such a comorbidity. This can be explained by the fact that COVID-19 is a respiratory disease; therefore, those who have a history of chronic respiratory illnesses appear more vulnerable to experience severe consequences of COVID-19 [71-73]. Recent evidence has also shown that individuals who are at high risk of infection or who are easily infected are more likely to receive the COVID-19 vaccine due to low levels of complacency [74-76]. In addition, a previous study from Indonesia has demonstrated that individuals who believe that there is a > 60% chance of being infected with SARS-CoV-2 were more willing to pay for COVID-19 vaccination [32].
Additionally, it has been shown that knowledge of COVID-19 has an association with WTP for vaccination, besides the sociodemographic and socioeconomic factors [32]. In this study, the participants in the health worker group, those who believed that "all routine vaccines recommended by healthcare workers are beneficial," and those who have received the flu vaccine in the previous 12 months were WTP more for COVID-19 vaccination. This is consistent with findings of study in Kuwait [77]. Thus, the finding of a link between willingness to pay for COVID-19 vaccine with actions of health behavior in this study such as the previous uptake of flu vaccination, as well as the healthcare-related occupation appears fathomable considering the frontline position of healthcare workers in fighting the pandemic with higher risk of virus exposure, with subsequently higher possibility of vaccine acceptance among this group compared to the general public [41,78].
Of note, a recent comprehensive systematic review that investigated the determinants of willingness to pay for health services including COVID-19 vaccination showed the importance of the following factors: sociodemographic features (including income/wealth), perceived benefits, barriers and threats, all of which should be considered in the future policies for vaccine allocation and subsidization [79].
Our study found that the average WTP for COVID-19 vaccines was significantly different among the countries included in this study. The explanation of this findings can be related to variable levels of wages in different LMICs, which was shown in a previous study from Nigeria, which showed the discrepancy between COVID-19 vaccine acceptance and the willingness to pay for the vaccine, highlighting the importance of monthly income on affordability of paying for the vaccine [80].
The current study had a few limitations which should be considered as follows: first, the cross-sectional nature inevitably leading to susceptibility to non-response bias and recall bias [81]. Second, the online distribution of the survey can lead to selection bias considering the possibility of poor access to internet and social media platforms in some subpopulations of the LMICs. Third, the analysis in the current study was done by comparing WTPs with only one country (Pakistan); therefore, it would be preferable if each country included in the study was compared with each other so that the results of each country's ability could be seen clearly and validly. Finally, the unequal distribution of the study respondents from different countries could have resulted in selection bias as well.
Conclusion
The current study can help in providing important insights to achieve effective COVID-19 vaccination strategies and policies in the LMICs. In particular, the continuous availability of free COVID-19 vaccination services appears of utmost importance in the LMICs despite the finding that WTP was relatively high in this study. Moreover, subsidizing the COVID-19 vaccine should be prioritized for individuals with a lower socio-economic status particularly in Sudan, Tunisia and Pakistan. Our results showed that the mean value that individuals were willing to pay for COVID-19 vaccine varied based on country of origin, besides the income level, history of respiratory disease, and previous uptake of flu vaccine. Our results can be helpful to guide the vaccination is a plausible scenario with continuous emergence of viral variants with vaccine escape properties.
Acknowledgments
We would like to thank Universitas Syiah Kuala that funded the study. We would like to thank Narra Studio Jurnal Indonesia for assistant during the manuscript preparation.
Ethics approval
This study was approved by the Institutional Review Board of the Universitas Syiah Kuala & Zainoel Abidin Hospital (129/EA/FK-RSUDZA/2021) and National Health Research and Development Ethics Commission (KEPPKN) of the Ministry of Health of the Republic of Indonesia (#1171012P).
Conflict of interest
The authors declare no competing interest.
Funding
This study was funded by Universitas Syiah Kuala (Kementerian Pendidikan dan Kebudayaan) - Penelitian H-Indeks Tahun Anggaran 2021 (169/UN11/SPK/PNBP/2021).
Underlying data
Derived data supporting the findings of this study are available from the first author on request.
How to cite
Sallam M, Anwar S, Yufika A, et al. Willingness-to-pay for COVID-19 vaccine in ten low-middle- income countries in Asia, Africa and South America: A cross-sectional study. Narra J 2022; 2(1): e74 - http://doi.org/10.52225/narra.v2i1.74.
References
- 1.Cascella M, Rajnik M, Aleem A, et al. https://www.ncbi.nlm.nih.gov/books/NBK554776/ Features, evaluation, and treatment of coronavirus (COVID-19). StatPearls Publishing. Available from: (Accessed: 13 February 2022). [PubMed]
- 2.World Health Organization (WHO) . WHO Director-General’ s opening remarks at the media briefing on COVID-19- 11 March 2020: Geneva, Switzerland. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (Accessed: 13 February 2022).
- 3.Kaye AD, Okeagu CN, Pham AD, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol 2021; 35(3):293-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schippers MC. For the greater good? the devastating ripple effects of the Covid-19 crisis. Front in Psych. 2020:11:577740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saladino V, Algeri D, Auriemma V. The psychological and social impact of Covid-19: New Perspectives of well-being. Front in Psych. 2020;11: 577684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) . Tracking SARS-CoV-2 variants. Available from: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (Accessed: 13 February 2022).
- 7.Perez-Gomez R. The development of SARS-CoV-2 variants: The gene makes the disease. J Develop Bio 2021; 9(4):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallam M, Ababneh NA, Dababseh D, et al. Temporal increase in D614G mutation of SARS-CoV-2 in the Middle East and North Africa. Heliyon 2021; 7(1): e06035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harvey WT, Carabelli AM, Jackson B, et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Micro 2021; 19(7): 409-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bushman M, Kahn R, Taylor BP, et al. Population impact of SARS-CoV-2 variants with enhanced transmissibility and/or partial immune escape. Cell. 2021;184(26):6229-42.el8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization (WHO) . COVID-19 advice for the public: Getting vaccinated. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice (Accessed: 13 february 2022). [Google Scholar]
- 12.Macchia A, Ferrante D, Angeleri P, et al. Evaluation of a COVID-19 vaccine campaign and SARS-CoV-2 infection and mortality among adults aged 60 years and older in a middle-income country. JAMA Network Open 2021; 4(10): e2130800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu S, Huang R, Sy LS, et al. COVID-19 vaccination and Non-COVID-19 mortality risk—seven integrated health care organizations, United States, December 14, 2020-July 31, 2021. Morbidity and Mortality Weekly Report 2021; 70(43): 1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xing K, Tu XY, Liu M, et al. Efficacy and safety of COVID-19 vaccines: a systematic review. Zhongguo dang dai er ke za zhi =. Chinese J of Contemporary Pediatrics. 2021;23(3):221-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pormohammad A, Zarei M, Ghorbani S, et al. Efficacy and safety of COVID-19 Vaccines: A systematic review and meta-analysis of randomized clinical trials. Vaccines 2021; 9(5):467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubin R. COVID-19 Vaccines vs variants—determining how much immunity is enough. JAMA 2021; 325(13): 1241.-1243. [DOI] [PubMed] [Google Scholar]
- 17.Liu Y, Liu J, Xia H, et al. Neutralizing activity of BNT162b2-elicited serum. New England J Med 2021; 384(15): 1466.-1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krause PR, Fleming TR, Longini IM, et al. SARS-CoV-2 variants and vaccines. New England J Med 2021; 385(2): 179.-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malik JA, Ahmed S, Mir A, et al. The SARS-CoV-2 mutations versus vaccine effectiveness: New opportunities to new challenges. J Infection Pub Health 2022; 15(2): 228-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cerda AA, Garcia LY. Hesitation and refusal factors in individuals' decision-making processes regarding a coronavirus disease 2019 vaccination. Front in Pub Health 2021; 9:626852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akther T, Nur T. A model of factors influencing COVID-19 vaccine acceptance: A synthesis of the theory of reasoned action, conspiracy theory belief, awareness, perceived usefulness, and perceived ease of use. PLOS ONE 2022; 17(1): e0261869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brewer NT, Chapman GB, Rothman AJ, et al. Increasing vaccination: Putting psychological science into action. Psych Sci in the Public Interest 2017; 18(3): 149-207. [DOI] [PubMed] [Google Scholar]
- 23.Betsch C, Schmid P, Heinemeier D, et al. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLOS ONE 2018; 13(12): e0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Su C-W, Dai K, Ullah S, Andlib Z. COVID-19 pandemic and unemployment dynamics in European economies. Eco Res-Ekonomska Istrazivanja 2021; 1-13. [Google Scholar]
- 25.Josephson A, Kilic T, Michler JD. Socioeconomic impacts of COVID-19 in low-income countries. Nat Human Behaviour 2021; 5(5): 557-565. [DOI] [PubMed] [Google Scholar]
- 26.Tagoe ET, Sheikh N, Morton A, et al. COVID-19 vaccination in lower-middle income countries: national stakeholder views on challenges, barriers, and potential solutions. Front in Pub Health 2021; 9: 709127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McDermott A. Core Concept: Herd immunity is an important-and often misunderstood-public health phenomenon. Proc Natl Acad SciU S A 2021;118(21):e2107692118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubin R. Difficult to determine herd immunity threshold for COVID-19. JAMA 2020; 324(8):732. [DOI] [PubMed] [Google Scholar]
- 29.Sallam M, Al-Sanafi M, Sallam M. A global map of COVID-19 vaccine acceptance rates per country: An updated concise narrative review. J of Multidisciplinary Healthcare 2022; 15: 21-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines 2021; 9(2):160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patwary MM, Bardhan M, Disha AS, et al. Determinants of COVID-19 vaccine acceptance among the adult population of bangladesh using the health belief model and the theory of planned behavior model. Vaccines 2021; 9(12): 1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harapan H, Wagner AL, Yufika A, et al. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Human Vaccines & Immunotherapeutics 2020; 16(12): 3074-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qin W, Wang E, Ni Z. Chinese consumers’ willingness to get a COVID-19 vaccine and willingness to pay for it. PLOS ONE 2021; 16(5): e0250112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adigwe OP. COVID-19 vaccine hesitancy and willingness to pay: Emergent factors from a cross-sectional study in Nigeria. Vaccine: X 2021; 9: 100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cerda AA, Garcia LY. Willingness to pay for a COVID-19 vaccine. App Health Econ and Health Policy 2021; 19(3): 343-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J, Lyu Y, Zhang H, et al. Willingness to pay and financing preferences for COVID-19 vaccination in China. Vaccine 2021; 39(14): 1968-1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Das U, Rathore U, Pal R. On willingness to pay for Covid-19 vaccines: a case study from India. Hum Vaccin Immunother 2021: 1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarasty O, Carpio CE, Hudson D, et al. The demand for a COVID-19 vaccine in Ecuador. Vaccine 2020; 38(51): 8090.-8098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Azzeri A, Laziz NAA, Ithnin M, Jaafar H. Ability to pay and willingness to pay for covid-19 vaccination: are we ready? Malaysian J Pub Health Med 2021; 21(1): 347-355. [Google Scholar]
- 40.Harapan H, Anwar S, Yufika A, et al. Vaccine hesitancy among communities in ten countries in Asia, Africa, and South America during the COVID-19 pandemic. Pathogens Global Health 2021: 1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sallam M, Dababseh D, Eid H, et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: A study in Jordan and Kuwait among other arab countries. Vaccines 2021; 9(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosiello DF, Anwar S, Yufika A, et al. Acceptance of COVID-19 vaccination at different hypothetical efficacy and safety levels in ten countries in Asia, Africa, and South America. Narra J 2021; l(3):e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Butler R, MacDonald NE. Diagnosing the determinants of vaccine hesitancy in specific subgroups: The guide to tailoring immunization programmes (TIP). Vaccine 2015; 33(34): 4176-479. [DOI] [PubMed] [Google Scholar]
- 44.O’ brien RM. A Caution Regarding rules of thumb for variance inflation factors. Quality & Quantity 2007; 41(5): 673.-690. [Google Scholar]
- 45.Glejser H. A new test for heteroskedasticity. J American Statistical Association 1969; 64(325): 316-323. [Google Scholar]
- 46.Yap BW, Sim CH. Comparisons of various types of normality tests. J Statistical Computation Simulation 2011; 81(12): 2141-2155. [Google Scholar]
- 47.Harapan H, Anwar S, Bustamam A, et al. Willingness to pay for a dengue vaccine and its associated determinants in Indonesia: A community-based, cross-sectional survey in Aceh. Acta Trop 2017; 166: 249-256. [DOI] [PubMed] [Google Scholar]
- 48.Harapan H, Mudatsir M, Yufika A, et al. Community acceptance and willingness-to-pay for a hypothetical Zika vaccine: A cross-sectional study in Indonesia. Vaccine 2019; 37(11): 1398-1406. [DOI] [PubMed] [Google Scholar]
- 49.Mudatsir M, Anwar S, Fajar JK, et al. Willingness-to-pay for a hypothetical Ebola vaccine in Indonesia: A crosssectional study in Aceh. FlOOORes 2019; 8: 1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Birhane MG, Miranda MEG, Dyer JL, et al. Willingness to Pay for dog rabies vaccine and Registration in llocos Norte, Philippines (2012). PLOS Neglected Trop Dis 2016; 10(3): e0004486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sauerborn R, Gbangou A, Dong H, et al. Willingness to pay for hypothetical malaria vaccines in rural Burkina Faso. Scand J Public Health 2005; 33(2): 146-150. [DOI] [PubMed] [Google Scholar]
- 52.Hansen KS, Pedrazzoli D, Mbonye A, et al. Willingness-to-pay for a rapid malaria diagnostic test and artemisinin- based combination therapy from private drug shops in Mukono District, Uganda. Health Policy Plan 2013; 28(2): 185-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Feng C, Wang H, Lu N, et al. Log-transformation and its implications for data analysis. Shanghai Arch Psychiatry 2014; 26(2): 105-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang Jing. Interpreting Regression coefficients for logtransformed variables. Available from: https://www.cscu.cornell.edu/news/archive.php (Accessed: 13 February 2022).
- 55.Slunge D. The willingness to pay for vaccination against tick-borne encephalitis and implications for public health policy: Evidence from Sweden. PLOS ONE 2015; 10(12): e0143875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wong CKH, Man KKC, Ip P, et al. Mothers’ Preferences and willingness to pay for human papillomavirus vaccination for their daughters: A discrete choice experiment in Hong Kong. Value in Health 2018; 21(5): 622-629. [DOI] [PubMed] [Google Scholar]
- 57.Banik R, Islam MS, Pranta MUR, R, et al. Understanding the determinants of COVID-19 vaccination intention and willingness to pay: findings from a population-based survey in Bangladesh. BMC Infectious Diseases 2021; 21(1): 892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Caserotti M, Girardi P, Rubaltelli E, et al. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med 2021; 272: 113688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Y, Luo X, Ma ZF. Willingness of the general population to accept and pay for COVID-19 vaccination during the early stages of COVID-19 pandemic: a nationally representative survey in mainland China. Hum Vaccin Immunother 2021; 17(6): 1622-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Adigwe OP. COVID-19 vaccine hesitancy and willingness to pay: Emergent factors from a cross-sectional study in Nigeria. Vaccine: X 2021; 9: 100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Garcia LY, Cerda AA. Contingent assessment of the COVID-19 vaccine. Vaccine 2020; 38(34): 5424-5429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wong LP, Alias H, Wong P-F, et al. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccines & Immuno 2020; 16(9): 2204-2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vo NX, Nguyen TTH, Van Nguyen P. , et al. Using contingent valuation method to estimate adults' willingness to pay for a future coronavirus 2019 vaccination. Value in Health Regional Issues 2021; 24: 240-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Catma S, Varol S. Willingness to pay for a hypothetical COVID-19 vaccine in the United States: A contingent valuation approach. Vaccines 2021; 9(4): 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kabir R, Mahmud I, Chowdhury MTH, et al. COVID-19 vaccination intent and willingness to pay in Bangladesh: A cross-sectional study. Vaccines 2021; 9(5): 416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carpio CE, Sarasty O, Hudson D, et al. The demand for a COVID-19 vaccine in Kenya. Hum Vaccin Immunother 2021;17(10):3463-3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shitu K, Wolde M, Handebo S, Kassie A. Acceptance and willingness to pay for COVID-19 vaccine among school teachers in Gondar City, Northwest Ethiopia. Tropical Med Health 2021; 49(1): 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Meshkani Z, Zarei L, Hajimoladarvish N, et al. Private demand for Covid-19 vaccine: A contingent assessment from a low-and middle-income country. IJPR 2021; 20(3): 223-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Karam MM, Baki JA, Al-Hajje A, et al. Willingness to pay for a coronavirus vaccine and its associated determinants in Lebanon. Value Health Reg Issues 2022; 30: 18-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Catma S, Varol S. Willingness to pay for a hypothetical COVID-19 vaccine in the United States: A contingent valuation approach. Vaccines 2021; 9(4):318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmunity 2020; 109: 102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA 2020; 324(8): 782-793. [DOI] [PubMed] [Google Scholar]
- 73.Harapan H, Itoh N, Yufika A, et al. Coronavirus disease 2019 (COVID-19): A literature review. J Infection and Public Health 2020; 13(5): 667-673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Harapan H, Wagner AL, Yufika A, et al. Acceptance of a COVID-19 vaccine in Southeast Asia: A cross-sectional study in Indonesia. Front Public Health 2020; 8:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bongomin F, Olum R, Andia-Biraro I, et al. COVID-19 vaccine acceptance among high-risk populations in Uganda. TherAdv Infect Dis. 2021;8:20499361211024376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mohamed NA, Solehan HM, Mohd Rani MD, et al. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLOS ONE 2021; 16(8): e0256110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Alqudeimat Y, Alenezi D, AlHajri B, et al. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract 2021; 30(3): 262-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Al-Sanafi M, Sallam M. Psychological determinants of COVID-19 vaccine acceptance among healthcare workers in Kuwait: A cross-sectional study using the 5C and Vaccine conspiracy beliefs scales. Vaccines 2021; 9(7):701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Steigenberger C, Flatscher-Thoeni M, Siebert U, Leiter AM. Determinants of willingness to pay for health services: A systematic review of contingent valuation studies. Eur J Health Econ 2022: 1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ilesanmi O, Afolabi A, Uchendu O. The prospective COVID-19 vaccine: Willingness to pay and perception of community members in Ibadan, Nigeria . Peer J 2021; 9: elll53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang X, Cheng Z. Cross-Sectional studies: Strengths, weaknesses, and recommendations. Chest 2020; 158(1, Supplement): S65-S71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Derived data supporting the findings of this study are available from the first author on request.