Abstract
Introduction:
Urological surgeries are a significant part of surgical services. The need for these services varies regionally and globally. Knowledge of the local need is important for prioritisation of resources.
Objectives:
To describe the urological procedures done in our hospital for effective utilisation of the already scarce resource in this region.
Patients and Methods:
This was a retrospective one-year study of the urosurgical cases done in a Nigerian Teaching Hospital. The main theatre register was used to collate data. Data collected included age, sex, operation done and anaesthesia employed.
Results:
One hundred and twenty-two male and three female patients were included with a male-to-female ratio of 41:1. The mean age of the patients was 56.6 ± 19.89 years. Elective cases accounted for 102 (81.6%) of surgeries. Regional anaesthesia was the most common form of anaesthesia accounting for 105 (84%) followed by local anaesthesia in 16 (12.8%). Day cases accounted for 77 (61.6%) of procedures. More than 80% of the study population was 50 years and older. Overall, the three most common performed surgeries were digital-guided prostate biopsy 47 (37.6%), suprapubic cystostomy 16 (12.8%) and open prostatectomy 9 (7.2%). In male patients, the three most common procedures were prostate biopsy 47 (38.5%), suprapubic cystostomy 16 (13.1 %), open prostatectomy 9 (7.4%) whereas nephrectomy, pyeloplasty and stent removal each accounted for 33.3% each of procedures in female patients. Endourological procedures accounted for 5 (4%) of cases.
Conclusion:
Open surgeries accounted for the majority of these cases done with prostate-related procedures being the most common procedures. Few endourological procedures were performed.
Keywords: Endourology, Nigeria, procedure, surgery, urology
Introduction
The populations of the sub-Saharan Africa have limited access to surgical intervention.[1] The urological surgeries routinely performed vary regionally. This is representative of the commonly encountered diseases. In Nigeria, as in Sub-Saharan Africa (SSA), prostate pathology, male infertility and urethral stricture disease are common and as such this should represent the bulk of urological interventions.[2,3,4]
Whereas endoscopy for the management of urological diseases has been widely accepted in developed countries, in Nigeria, as in other SSA countries, open surgeries are commonly performed.[5] The use of this technology in Nigeria is evolving, with majority of the minimally invasive surgeries being carried out in private facilities.[6,7,8] This difference in use of endoscopy between high- and low-income countries revolves around physical availability of trained specialists, lack of basic facilities such as water, electricity to use these instruments and lack of funding of the hospitals.[5,9,10]
The practice of surgery and urology in sub-Saharan Africa is marred by numerous challenges. These range from lack of basic infrastructure to cater for these patients, political instability, poverty and illiteracy to poor funding and equipping of these institutions.[9,10,11] Furthermore, these patients present late leaving the surgeons with few options to treat these patients.[12,13] These challenges alter the patterns of urological disease presentation, and hence the choice of available treatments.
This paper aimed to enumerate the urological procedures carried out in a tertiary hospital in South-Eastern Nigeria over a year period with a view to recommending to the hospital management and relevant authority appropriate mode of allocation of scarce resources to cater for the urologic needs.
Patients and Methods
This was a retrospective hospital-based study of the all the urological cases done over a one-year period from January 2021 to December 2021 in Alex-Ekwueme Federal University Teaching Hospital, Abakaliki, Ebonyi Sate, South East Nigeria. Ethical approval was obtained from the hospital ethical committee (AE-FUTHA/REC/VOL3/2022/137). The hospital is a 720-bedded hospital. The hospital serves the state and neighbouring states of Benue, Enugu, Imo and Cross River states. It is the only referral centre in the state. The hospital has a modular theatre with five suites for different surgical specialties. The elective patients were seen in the outpatient clinic, optimised and were admitted in the wards about two days before surgery. They were reviewed by anaesthetists on the ward. The day cases were admitted on the day-of-surgery and were discharged the same day. The main theatre and emergency theatre records were used to retrieve data. Two theatre session days are allocated to the urology unit per week. Data collated were transferred into a pro forma. This was analysed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, New York). Continuous variables were summarised as means and standard deviation, whereas categorical variables were presented in frequencies and percentages. Statistical significance was set at P < 0.05.
Results
A total of 148 surgeries were performed out during the period of study. Twenty-three cases had incomplete data and were excluded, leaving 125 cases for analysis. One hundred and twenty-two patients were males (97.6%) whereas 3 (2.4%) patients were females with a male to female ratio of 41:1. The mean age of the patients was 56.6 ± 19.89 years with a range of 18–92 years as shown in Figure 1. Elective cases accounted for 102 (81.6%) of surgeries done. Day cases accounted for 77 (61.6%) of procedures. Regional anaesthesia was the most common form of anaesthesia that was employed accounting for 105 (84%) followed by local anaesthesia in 16 (12.8%). More than 80% of the study population was 50 years and older. Overall, the three most common performed surgeries were prostate biopsy 47 (37.6%), suprapubic cystostomy 16 (12.8%) and open prostatectomy 9 (7.2%) as shown in Table 1. In male patients, the three most common procedures performed were digital-guided prostate biopsy 47 (38.5%), suprapubic cystostomy 16 (13.1%), and open prostatectomy 9 (7.4%) whereas nephrectomy, pyeloplasty and stent removal each accounted for 33.3% of procedures in female patients. Endourological procedures accounted for 5 (4%) of cases done.
Figure 1.
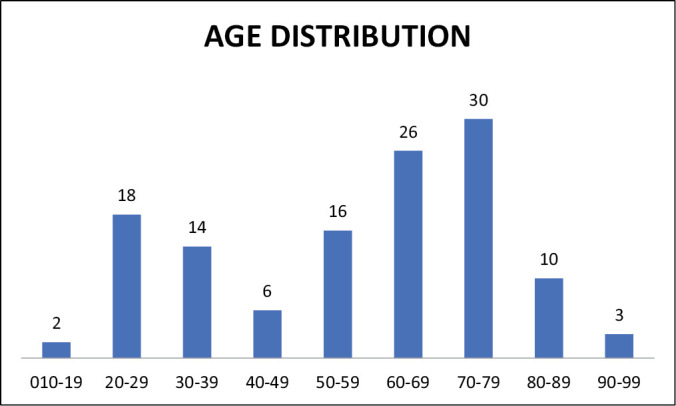
Bar chart showing the age distribution of the patients (n = 125)
Table 1.
Distribution of the cases done during the study period
| Procedure | Frequency | Age (mean ± SD) | Percentage |
|---|---|---|---|
| Prostate biopsy | 47 | 65.34 ± 12.64 | 37.6 |
| Varicocelectomy | 8 | 33.38 ± 9.02 | 6.4 |
| Wound debridement | 5 | 41.4 ± 28.53 | 4.0 |
| Open SPC | 16 | 62.69 ± 18.35 | 12.8 |
| Urethroplasty | 8 | 45.13 ± 16.24 | 6.4 |
| Incision and drainage of scrotal abscess | 1 | 23.0 | 0.8 |
| Orchidectomy (for cancer of the prostate) | 8 | 73 ± 10.76 | 6.4 |
| Hydrocelectomy | 4 | 51.50 ± 11.56 | 3.2 |
| TURP | 4 | 66.75 ± 2.87 | 3.2 |
| Herniorraphy | 1 | 44.0 | 0.8 |
| Orchiopexy for intermittent torsion | 8 | 25.63 ± 837 | 6.4 |
| Open prostatectomy | 9 | 66.67 ± 10.46 | 7.2 |
| Scrotoplasty | 2 | 60 ± 45.25 | 1.6 |
| Nephrectomy | 1 | 26.0 | 0.8 |
| Pyeloplasty | 1 | 26.0 | 0.8 |
| Stent removal of JJ stent (postpyeloplasty) | 1 | 35.0 | 0.8 |
| Bladder exploration | 1 | 30.0 | 0.8 |
| Total | 125 | 100.0 |
Discussion
Despite the huge burden of surgical disease in low and middle income countries (LMIC), they have limited access to surgical care.[1]
The 125 operations performed in this study is a small number for some obvious reasons. Firstly, during the period of study, the Nigerian Association of Resident Doctors (NARD) embarked on a two-month industrial action. Another factor is the peculiarity of the region; poverty is endemic and majority of the populace fund their health care out-of-pocket with the National Health Insurance Scheme (NHIS) covers the civil servants which is a small per cent of our study population.[14] The patients may not be able to afford surgical bills and may opt to cancel the surgery. This has been our experience. In our earlier study, as much as 47% of patient-related reason for day-of-surgery cancellation were fund-related.[15] Poor record keeping has been noted in this subregion and this may also explain this number of cases recorded in this study.[16,17] Lastly, illiteracy may also play a part.[18] This pattern of low patient turnout was seen in a tertiary hospital in North Eastern Nigeria where over a two-year period, 185 urological surgeries were performed.[4]
The high male-to-female ratio in this study is similar to the findings of earlier authors.[2,19]
The mean age of 56.6 years in this study is the age of prostate-related pathologies.[20,21,22] 68% of the study population were 50 years and older This explains the overall mean age in this study.
Improvement in anaesthesia and the development of new surgical techniques led to uptake of day case surgeries.[23] This has led to a reduction in cost of patient care and increased patient turnover.[23] Despite these advantages, most centres in Nigeria lack a dedicated day surgery unit.[4,24,25] In this study, as much as 61% of surgeries were day cases. This is similar to the findings in Lagos and Ibadan both in Nigeria where day cases accounted for as 62%–68% of the surgeries carried out.[24,26]
Endourology comes with the advantages of less functional impairment of target organs, shorter in patient stays and early return.[5] As low as 4% of the procedures in this study were endourological with transurethral resection of the prostate (TURP) accounting for more than 80%. This is similar to the description of earlier authors in various regions of the country.[2,19] There has been a steady increase in the number of endourological procedures being done in the country in recent times. These have ranged from lower to upper tract procedures. The vast majority of such cases are being treated in private facilities around the country.[6,7,8,27] Many challenges are responsible for this ranging from a lack of political goodwill to fund the tertiary hospitals with state-of-the-art endourology sets to a lack of maintenance culture and lack of trained manpower to operate these equipment.[9,10]
Prostate-related procedures were the most common. This is because prostate-related pathologies account for a majority of the clinic and emergency presentations in this region.[10,28,29] Prostate biopsies were the most common performed procedure accounting for 36%. This was similar to the findings of earlier authors in Nigeria.[24,30] Digitally guided biopsy was the most common procedure as most patients meet the criteria for biopsy and the unavailability of ultrasound guided-biopsy machine. This is, however, higher than the seven per cent reported by Aisuodionoe-Shadrach[19] in Abuja. The reason for this wide difference was not evident.
Open prostatectomy is a common urological procedure for the management of benign prostatic enlargement in this sub region.[3,5,31] In this study as much as 7.5% had open prostatectomy. This is similar to the rates reported in Benue and Yobe states Nigeria.[4,30]
In high income countries, TURP is commonly done for this disease because the cost of TURP is cheaper than open prostatectomy unlike in LMIC where the irrigation fluid and hard wares for TURP is more expensive than the surgical blades and few sutures required for open prostatectomy.[5] Patients who opt for TURP in this sub region are persons who can afford them.[5]
Regional anaesthesia which was the most common anaesthesia employed in this study is similar to the findings of earlier authors.[30] This is because the most common procedures performed in this study revolve around the prostate which most of the time require regional anaesthesia.[3]
Conclusion
Prostate-related surgeries, suprapubic cystostomies and urethral surgeries were common in this study. Open surgeries accounted for the majority of these cases. Endourological procedures did not feature commonly. There is a need for the federal government of Nigeria, through the hospital management board to procure equipment related to the above procedures particularly as related to endourology as this is the current trend.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author contribution
Chike John Okeke—Substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, drafting the article, revising it critically for important intellectual content and final approval of the version to be published.
Rufus Wale Ojewola—Analysis and interpretation of data, drafting the article, revising it critically for important intellectual content, and final approval of the version to be published.
Chinonso Odo—Analysis and interpretation of data, drafting the article, revising it critically for important intellectual content, and final approval of the version to be published.
Ugbede Emmanuel Oyibo—Analysis and interpretation of data, drafting the article, revising it critically for important intellectual content, and final approval of the version to be published.
Anselm Okwudili Obi—Substantial contributions to conception and design, analysis and interpretation of data, drafting the article, revising it critically for important intellectual content, and final approval of the version to be published.
Uzodimma Ugochukwu Nnadozie—Acquisition of data, analysis and interpretation of data, drafting the article, revising it critically for important intellectual content and final approval of the version to be published.
Acknowledgement
This work is in memoriam of Late Dr. Charles Azuwike Odoemene who passed away on March 7, 2022.
References
- 1.Shrime MG, Bickler SW, Alkire BC, Mock C. Global burden of surgical disease: An estimation from the provider perspective. Lancet Glob Health. 2015;3:S8–9. doi: 10.1016/S2214-109X(14)70384-5. [DOI] [PubMed] [Google Scholar]
- 2.Eke N, Sapira M, Echem R. Spectrum of urological procedures in University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria. Niger J Clin Pract. 2007;10:74–8. [PubMed] [Google Scholar]
- 3.Salako AA, Badmus TA, Owojuyigbe AM, David RA, Ndegbu CU, Onyeze CI. Open prostatectomy in the management of benign prostate hyperplasia in a developing economy. Open J Urol. 2016;6:179–89. [Google Scholar]
- 4.Tela UM, Mainasara R. Spectrum of urological procedures in Yobe State University Teaching Hospital: An initial experience in a young West African Hospital. Int Surg J. 2021;8:455–8. [Google Scholar]
- 5.Watson G, Niang L, Chandresekhar S, Natchagande G, Payne SR. The feasibility of endourological surgery in low-resource settings. BJU Int. 2022;130:18–25. doi: 10.1111/bju.15770. [DOI] [PubMed] [Google Scholar]
- 6.Ijah RF, Ray-Offor E, Igwe PO, Ekeke ON, Okoro PE, Nyengidiki TK, et al. Minimally invasive surgery in Port Harcourt, Nigeria: Progress so far. Cureus. 2022;14:e32049. doi: 10.7759/cureus.32049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alabi T, Jeje E, Ogunjimi M, Ojewola R. Endoscopic management of ureteric stones: Our initial experience. Niger J Surg. 2019;25:26–9. doi: 10.4103/njs.NJS_20_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin I, Sadiq A, Abayomi A, Olalekan O, Monica O. Spectrum of endo-urological procedures performed at a Nigerian kidney transplant centre. Yen Med J. 2020;2:74–9. [Google Scholar]
- 9.Olapade-Olaopa EO, Onawola KA. Challenges for urology in sub-Saharan Africa in 2006. J Men’s Health Gender. 2006;3:109–16. [Google Scholar]
- 10.Olapade-Olaopa EO, Adebayo SA, Ajamu O, Ukachukwu A, Shittu O, Okeke L. British training and urological practice in sub-Saharan Africa. BJU Int. 2010;105:1353–5. doi: 10.1111/j.1464-410X.2010.09261.x. [DOI] [PubMed] [Google Scholar]
- 11.Ogunbiyi OJ. Impact of health system challenges on prostate cancer control: Health care experiences in Nigeria. Infect Agent Cancer. 2011;6:2–5. doi: 10.1186/1750-9378-6-S2-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Badmus TA, Adesunkanmi ARK, Yusuf BM, Oseni GO, Eziyi AK, Bakare TIB, et al. Burden of prostate cancer in Southwestern Nigeria. Urology. 2010;76:412–6. doi: 10.1016/j.urology.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 13.Ajape A, Ibrahim KOO, Fakeye JA, Abiola OO. An overview of cancer of the prostate diagnosis and management in Nigeria: The experience in a Nigerian tertiary hospital. Ann Afr Med. 2010;9:113–7. doi: 10.4103/1596-3519.68353. [DOI] [PubMed] [Google Scholar]
- 14.Uzochukwu B, Ughasoro M, Okwuosa C, Onwujekwe O, Envuladu E, Etiaba E. Health care financing in Nigeria: Implications for achieving universal health coverage. Niger J Clin Pract. 2015;18:437–44. doi: 10.4103/1119-3077.154196. [DOI] [PubMed] [Google Scholar]
- 15.Okeke CJ, Obi AO, Tijani KH, Eni UE, Okorie CO. Cancellation of elective surgical cases in a Nigerian teaching hospital. Niger J Clin Pract. 2020;23:965–9. doi: 10.4103/njcp.njcp_650_19. [DOI] [PubMed] [Google Scholar]
- 16.Okeke CJ, Ogunjimi MA, Jeje EA, Obi AO, Uzoma C. Urinary catheter documentation in a Nigerian teaching hospital: Are we recording enough? J West Afr College Surg. 2023;13:45–8. doi: 10.4103/jwas.jwas_288_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ko I, Adamu A, Jiya FB, Yusuf T, Sani UM, Jiya NM, et al. Quality of hospital admission documentation: A study in an emergency paediatric unit of a tertiary hospital in Nigeria. Afr J Med Health Sci. 2019;18:25–30. [Google Scholar]
- 18.UNESCO. International Literacy Statistics: A Review of Concepts, Methodology and Current Data. Montreal, Canada: UNESCO-UIS; 2008. [Google Scholar]
- 19.Aisuodionoe-Shadrach O. Range of urologic surgical procedures in two district tertiary care hospitals in Abuja, Nigeria. Afr J Urol. 2011;17:92–6. [Google Scholar]
- 20.Ezeanyika L, Ejike C, Obidoa O, Elom S. Prostate disorders in an apparently normal Nigerian population 1: Prevalence. Biokemistri. 2010;18:127–32. [Google Scholar]
- 21.Chokkalingam AP, Yeboah ED, DeMarzo A, Netto G, Yu K, Biritwum RB, et al. Prevalence of BPH and lower urinary tract symptoms in West Africans. Prostate Cancer Prostatic Dis. 2011;15:170–6. doi: 10.1038/pcan.2011.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A systematic review and meta-analysis. Sci Rep. 2017;7:1–10. doi: 10.1038/s41598-017-06628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Appleby J. Day case surgery: A good news story for the NHS. BMJ. 2015;351:1–4. doi: 10.1136/bmj.h4060. [DOI] [PubMed] [Google Scholar]
- 24.Ogunjimi MA, Ojewola RW, Fatuga AL, Tijani KH, Jeje EA, Okeke CJ, et al. Urologic day case surgery at a Nigerian tertiary hospital: A 5-year experience MA. Niger J Clin Pract. 2021;24:1380–4. doi: 10.4103/njcp.njcp_671_20. [DOI] [PubMed] [Google Scholar]
- 25.Dakum N, Ramyil V, Misauno M, Ojo E, Ogwuche E, Sani A. Reasons for cancellations of urologic day care surgery. Niger J Surg Res. 2010;8:30–3. [Google Scholar]
- 26.Takure AO, Shittu OB, Okeke LI, Olapade-Olaopa EO, Adebayo SA. Daycase urology at Ibadan, Nigeria: A ten year review. Pan Afr Med J. 2010;6:13. [PMC free article] [PubMed] [Google Scholar]
- 27.Raphael JE, Ezenta C. Percutaneous nephrolithotomy, pneumatic and holmium laser lithotripsy for urinary calculi: Adopting the paradigm shift in stone management in Southern Nigeria. Am J Clin Med Res. 2022;10:10–6. [Google Scholar]
- 28.Okeke CJ, Obi AO, Odoemene CA, Ojewola RW, Afogu EN, Odo C, et al. Urological emergencies in a Nigerian teaching hospital: Epidemiology and treatment. Niger J Clin Pract. 2021;24:400–5. doi: 10.4103/njcp.njcp_393_20. [DOI] [PubMed] [Google Scholar]
- 29.Mungadi I, Khalid A. Spectrum of urological cases in a West African Tertiary Hospital. Ann Afr Med. 2021;20:14–8. doi: 10.4103/aam.aam_7_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Efu ME, Ogwuche EI, Ojo BA, Eke BA. Anesthetic techniques for urological surgeries in Benue State University Teaching Hospital (BSUTH), Makurdi, Nigeria. Eur J Med Health Sci. 2020;2:1–4. [Google Scholar]
- 31.Obi AO, Okeke CJ, Ulebe AO, Ogbobe UU. The modified suprapubic prostatectomy technique is associated with improved hemostasis and decline in blood transfusion rate after open suprapubic prostatectomy compared to the Freyers technique. Niger J Clin Pract. 2022;25:432–8. doi: 10.4103/njcp.njcp_1391_21. [DOI] [PubMed] [Google Scholar]


