Abstract
Introduction
Acute leukemias (AL) are the main types of cancer in children worldwide. In Mexico, they represent one of the main causes of death in children under 20 years of age. Most of the studies on the incidence of AL in Mexico have been developed in the urban context of Greater Mexico City and no previous studies have been conducted in the central-south of the country through a population-based study. The aim of the present work was to identify the general and specific incidence rates of pediatric AL in three states of the south-central region of Mexico considered as some of the marginalized populations of Mexico (Puebla, Tlaxcala, and Oaxaca).
Methods
A population-based study was conducted. Children aged less than 20 years, resident in these states, and newly diagnosed with AL in public/private hospitals during the period 2021-2022 were identified. Crude incidence rates (cIR), standardized incidence rates (ASIRw), and incidence rates by state subregions (ASIRsr) were calculated. Rates were calculated using the direct and indirect method and reported per million children under 20 years of age. In addition, specific rates were calculated by age group, sex, leukemia subtype, and immunophenotype.
Results
A total of 388 cases with AL were registered. In the three states, the ASIRw for AL was 51.5 cases per million (0-14 years); in Puebla, it was 53.2, Tlaxcala 54.7, and Oaxaca de 47.7. In the age group between 0-19 years, the ASIRw were 44.3, 46.4, 48.2, and 49.6, in Puebla, Tlaxcala, and Oaxaca, respectively. B-cell acute lymphoblastic leukemia was the most common subtype across the three states.
Conclusion
The incidence of childhood AL in the central-south region of Mexico is within the range of rates reported in other populations of Latin American origin. Two incidence peaks were identified for lymphoblastic and myeloid leukemias. In addition, differences in the incidence of the disease were observed among state subregions which could be attributed to social factors linked to the ethnic origin of the inhabitants. Nonetheless, this hypothesis requires further investigation.
Keywords: incidence, child, lymphoid leukemia, myeloid leukemia, registries, epidemiology, Latino
1. Introduction
Acute leukemias (AL) are the main types of cancer in children worldwide. In Latin American countries (LAC) high incidence and mortality rates have been reported (1–5). Moreover, for some LAC an increase in leukemia mortality has been predicted by 2030 (6). Mexico is among these populations along with Argentina, Brazil, Chile, Ecuador, Guatemala, Peru, Puerto Rico, and Uruguay. According to data from the National Institute of Statistics, Geography, and Informatics of Mexico (INEGI) in 2019 (the year previous to the COVID-19 pandemic), childhood leukemias ranked first among the leading causes of death in the 5 to 9 years age group, and second in the 10 to 14 years age group, only surpassed by motor vehicle accidents (7). Consequently, the problem of childhood leukemia in Mexico such as another LAC requires effective actions aimed at prevention in order to reduce the incidence and mortality of AL.
To date, few risk factors have been found to be associated with childhood leukemia and explain less than 10% of the causes of the disease (8). One of the regions of Mexico which has been explored further in previous studies is Greater Mexico City (GMC) where it has been reported that the incidence of AL is among the highest in the world (9). Moreover, the relapses and deaths in the early phases of treatment (first year after diagnosis) are at least three times more frequent than in high-income countries despite the use of the same chemotherapy regimens (10, 11). Then, it is evident that each country and regions within countries have their own particularities for considering the study of factors associated with both the etiology and the prognosis of the disease such as the environmental and socioeconomic conditions, lifestyle, and access to health services among others (12–15).
Since January 2021 a population-based leukemia registry was implemented in the States of Puebla, Tlaxcala, and Oaxaca located in the central-south region of Mexico as a first step for investigating for the first time the incidence and mortality rates of AL in the pediatric population, the needs for hospital services, the efficacy of current treatments, the discovering of the factors associated with therapeutic failure and the environmental risks factors associated with the development of the disease.
In the present report, we display the results of AL incidence after two years of the leukemia registry implementation in Puebla, Tlaxcala, and Oaxaca.
2. Materials and methods
Cases with AL were recruited from public and private hospitals of Puebla, Tlaxcala, and Oaxaca from 1 January 2021 to 31 December 2022. Additionally, those patients from these Mexican States who were diagnosed and/or treated in public hospitals of GMC during the study period were registered. In this regard, it is important to highlight that the public hospitals of GMC diagnos and treat patients from almost all the States of the country because of the infrastructure of the Institutions and relatively easy access for some families to reach them. Therefore, as part of the present study, all public hospitals of GMC that in the last 10 years had attended children from Puebla, Tlaxcala, and Oaxaca also participated (See the list of the participating institutions in Table 1 ).
Table 1.
Participating Institutions in the population-based registry of incident cases with childhood acute leukemias in Puebla, Tlaxcala and Oaxaca.
| State | Hospital name/Laboratory name | Healthcare institution |
|---|---|---|
| Oaxaca | Hospital Especializado de la Niñez Oaxaqueña | SS/INSABI |
| Hospital General de Zona 1 “Dr. Demetrio Mayoral Pardo” | IMSS | |
| Laboratorios Juárez | Private | |
| Puebla | Hospital para el Niño Poblano | SS/INSABI |
| UMAE Hospital de especialidades CMN Manuel Ávila Camacho (San José) | IMSS | |
| Hospital Regional de Alta Especialidad | ISSSTE | |
| Instituto de Seguridad y Servicios Sociales de los Trabajadores al Servicio de Los Poderes del Estado de Puebla | ISSSTEP | |
| Hospital General del Sur | INSABI | |
| Hospital Universitario de Puebla | BUAP/Private | |
| Centro de Hematología y Medicina Interna, Clínica Ruiz | Private | |
| Laboratorio de Oncoinmunología and Citómica del Cáncer Infantil | CIBIOR | |
| Centro de Investigación Oncológica Una Nueva Esperanza-UPAEP | UNE-UPAEP | |
| Tlaxcala | Hospital Infantil de Tlaxcala | SS/INSABI |
| Mexico City | UMAE Hospital de Pediatría “Dr. Silvestre Frenk Freund” CMN Siglo XXI | IMSS |
| Centro Médico Nacional 20 de Noviembre | ISSSTE | |
| Instituto Nacional de Pediatría | SS/INSABI | |
| Hospital Infantil de México Federico Gómez | SS/INSABI | |
| Hospital Juárez de México | SS/INSABI |
IMSS, Instituto Mexicano del Seguro Social; SS, Secretaría de Salud; INSABI, Instituto de Salud para el Bienestar; CLUES, Clave Única de Establecimientos de Salud; UMAE, Unidad Médica de Alta Especialidad; CMN, Centro Médico Nacional; ISSSTE, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado; A.C, Asociación Civil; UPAEP, Universidad Popular Autónoma del Estado de Puebla.
2.1. Ethical considerations
The protocol was approved by the National Scientific Research and Ethics Committee of the Mexican Institute of Social Security with the number R-2020-785-022. In addition, authorization was received from the Local Ethics and Research Committees of each participating institution.
2.2. Validity of methods
Trained and standardized personnel were assigned to each participating hospital for case registration, ensuring the identification and follow-up of incident cases of AL. Clinical and demographic data including: sex, age at diagnosis, municipality of residence, socioeconomic level (SES), and immunophenotype were recorded. In addition, face-to-face interviews were conducted with parents and tutors of patients with a confirmed diagnosis of AL in order to validate the information related to the place of residence of the families. Written informed consent was obtained from parents and informed assent was obtained from patients ≥8 years old, when feasible, to be included in the study. In this study, all parents/guardians agreed to participate in the enrollment phase. Therefore, our participation rate was 100%.
The diagnosis was established by pediatric hematologists/oncologists according to clinical features: cell morphology, immunophenotype, and genetics, as defined by the 2008 World Health Organization (WHO) classification of lymphoid neoplasms. According to ICD-O-3 and ICCC-3, the subtype of AL was classified into two groups: a) acute lymphoblastic leukemia (ALL) (9820, 9823, 9826,9827, 9831, 9833-9837, 9940, 9948); and b) acute myeloid leukemia (AML) (9840, 9860, 9861, 9866, 9867, 9870-9874, 9891, 9895-9897, 9910, 9920, 9931) (16, 17). In regard to the immunophenotype, ALL patients were classified into B-cell, T-cell, or acute leukemia of ambiguous lineage (ALAL) according to the WHO.
2.3. Participating institutions
2.3.1. Populations and methods for incidence rates estimations
The states of Puebla, Tlaxcala, and Oaxaca were studied. Population information for these three states was obtained from the 2015-2050 censuses of the National Population Council (CONAPO). The total average annual population <20 years of age (reference population) from Puebla, Tlaxcala, and Oaxaca was 6,092,475.
Incidence rates were calculated and reported per million population under 20 years of age at the state and sub-regional levels.
2.4. Crude incidence rates
The state-level crude incidence rate (cIR) was calculated by dividing the number of incident cases of acute leukemia during the period 2021-2022 by the population under 20 years of age projected by the CONAPO for the years 2021-2022 (18).
This rate was calculated to estimate the global incidence and by subgroups according to: a) demographic variables: sex and age groups (0-4 years, 5-9 years, 10-14 years, 15-19 years, 0-14 years, 0-19 years); b) clinical variables: leukemia subtype (ALL, AML, OL) and immunophenotype (B-cell, T-cell, and ALAL); c) geographic unit of analysis: states (Puebla, Tlaxcala, and Oaxaca); and subregions of the three states, Puebla (Sierra Norte, Sierra Nororiental, Valle de Serdán, Angelópolis, Valle de Atlixco y Matamoros, Mixteca, Tehuacán y Sierra Negra); Tlaxcala (Norte, Oriente, Poniente, Centronorte, Centrosur, Sur); Oaxaca (Cañada, Costa, Istmo, Mixteca Oaxaqueña, Cuenca del Papaloapan, Sierra Norte; Sierra Sur, Valles Centrales de Oaxaca). (19). In addition, the cIR by subregions was calculated using the summation of the population under 20 years of age from the municipalities conforming to each subregion projected by CONAPO for the period 2016-2050 (20).
It is worth mentioning that Puebla, Tlaxcala, and Oaxaca, are comprised of 847 municipalities ranging from 23 to 517,395 inhabitants under 20 years of age per municipality. Therefore, calculating the rates at the municipal level would generate unstable rates, and consequently random fluctuations, and this observation would not be accurate for this disease. For this reason, it was decided to calculate incidence rates by state subregions as smaller geographic units of analysis with the intention of identifying areas with high incidence rates of acute leukemias and reducing this difficulty derived from the scarcity of data at the municipal level (numerous strata with insufficient or no data). (New York State 1999; Washington State Department of Health 2012).
2.5. Standardized incidence rates
Standardized incidence rates (sIR) were calculated using both direct and indirect methods, which were also reported per million children under 20 years of age. The direct method compared age-standardized incidence rates of AL worldwide (ASIRw), with the reference being the world population reported by the WHO for the period 2000-2025 (21). The indirect method was used to calculate standardized incidence rates by geographic subregions. (ASIRsr), being the reference population the sum of the inhabitants under 20 years of age of Puebla, Tlaxcala, and Oaxaca in the 2020 census according to the National Institute of Statistics and Geography (INEGI). This method addressed not only the instability of standardized incidence rates in data-scarce locations but also identified the state subregions with the greatest incidence rates of AL.
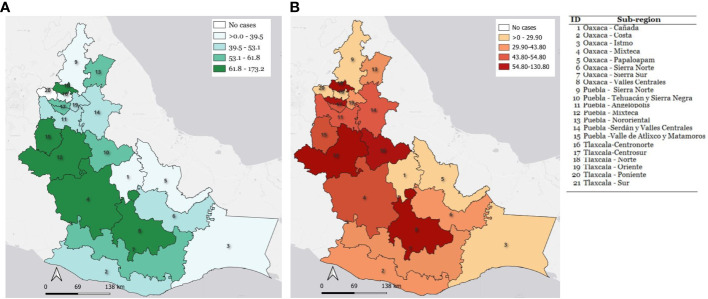
Finally, to know the spatial distribution of the AL incidence in each state subregion, the ASIRsr results were mapped using the QGIS 3.26 software (Open-Source Geospatial Foundation, Beaverton, Oregon, USA, QGIS, RRID : SCR_018507) ( Figure 1 ).
Figure 1.
Choropleth maps representation of standardized incidence rates of childhood acute leukemia reported for each state subregion. (A) Incidence rates by sub-regions in children with AL from 0-14 years of age. (B) Incidence rates by sub-regions in children with AL from 0-19 years of age.
3. Results
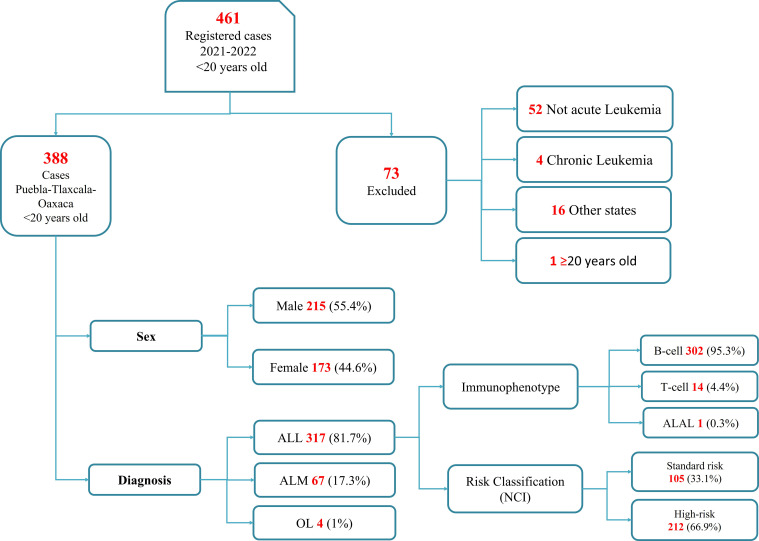
During the period 2021 to 2022, 461 cases with suspected childhood AL were registered in the participant institutions, still, 73 cases were not included in the present analysis because AL was discarded, some patients were from a different state of residence or had an age greater than 20 years old at the moment of diagnosis confirmation ( Figure 2 ). Consequently, a total of 388 cases had a confirmed diagnosis of AL. Among these cases, 55.4% (215) were male. The predominant AL subtype was ALL in 81.7% (n=317), followed by AML with 17.3% (n=67), and finally OL with 1% (n=4). According to the immunophenotype for the ALL subgroup, B-cell leukemias represented 95.3% (n=302), followed by T-cell with 4.4% (n=14) and ALAL with 0.3% (n=1).
Figure 2.
Flowchart of the selection process of children diagnosed with acute leukemia in the states of Puebla, Tlaxcala, and Oaxaca during the period 2021-2022. NCI, National Cancer Institute Classification.
3.1. Incidence rates by age groups
3.1.1. 0 to 14 years
The global AL incidence rates of the three regions in this age group were the following: a cIR of 51.4 and an ASIRw of 51.5 cases per million. Regarding the most frequent subtype of AL, it was ALL with an ASIRw of 41.5; likewise, the most frequent immunophenotype for these states was B-cell, reporting an ASIRw of 39.6. The rest of the crude and standardized rates are displayed in Table 2 .
Table 2.
Incidence rates of acute leukemias in children under 20 years of age from the states of Puebla, Tlaxcala and Oaxaca during the period 2021-2022.
| AL | Sex | Age-specific rate | 0 - 14y | ASIRw 0-14 | 0 - 19y | ASIRw 0 -19 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 - 4 | 5 - 9 | 10 - 14 | 15 - 19 | ||||||||||||
| n | cIR | n | cIR | n | cIR | n | cIR | n | cIR | n | cIR | ||||
| All-AL | Male | 52 | 47.77 | 63 | 56.26 | 71 | 62.39 | 29 | 25.84 | 185 | 55.40 | 55.28 | 215 | 48.11 | 48.17 |
| Female | 57 | 54.26 | 43 | 39.77 | 53 | 48.01 | 20 | 18.17 | 153 | 47.29 | 47.39 | 173 | 39.90 | 40.24 | |
| Total | 109 | 50.96 | 106 | 106.00 | 124 | 55.31 | 49 | 22.04 | 338 | 51.35 | 51.46 | 388 | 44.07 | 44.26 | |
| Subtype | |||||||||||||||
| ALL | Male | 48 | 44.10 | 52 | 46.44 | 56 | 49.21 | 26 | 23.17 | 156 | 46.56 | 46.62 | 182 | 40.73 | 40.83 |
| Female | 47 | 44.74 | 35 | 32.37 | 35 | 31.71 | 18 | 16.35 | 117 | 36.16 | 36.34 | 135 | 31.13 | 31.45 | |
| Total | 95 | 44.41 | 87 | 87.00 | 91 | 40.59 | 44 | 19.79 | 273 | 41.48 | 41.53 | 317 | 36.00 | 36.21 | |
| AML | Male | 4 | 3.67 | 11 | 9.82 | 14 | 12.30 | 3 | 2.67 | 29 | 8.56 | 8.37 | 32 | 7.16 | 7.12 |
| Female | 9 | 8.57 | 8 | 7.40 | 16 | 14.49 | 2 | 1.82 | 33 | 10.20 | 10.13 | 35 | 8.07 | 8.10 | |
| Total | 13 | 6.08 | 19 | 19.00 | 30 | 13.38 | 5 | 2.25 | 62 | 9.27 | 9.33 | 67 | 7.61 | 7.60 | |
| Other | Male | 0 | –––– | 0 | ––– | 1 | 0.88 | 0 | ––– | 1 | 0.29 | 0.30 | 1 | 0.22 | 0.22 |
| Female | 1 | 0.95 | 0 | ––– | 2 | 1.81 | 0 | ––– | 3 | 0.93 | 0.92 | 3 | 0.69 | 0.69 | |
| Total | 1 | 0.47 | 0 | ––– | 3 | 1.34 | 0 | ––– | 4 | 0.61 | 0.60 | 4 | 0.45 | 0.45 | |
| Immunophenotype | |||||||||||||||
| B-cell | Male | 46 | 42.26 | 49 | 43.76 | 52 | 45.69 | 25 | 22.28 | 147 | 43.89 | 43.93 | 172 | 38.49 | 38.60 |
| Female | 47 | 44.74 | 35 | 32.37 | 31 | 28.08 | 17 | 15.45 | 113 | 34.92 | 35.15 | 130 | 29.98 | 30.33 | |
| Total | 93 | 43.48 | 84 | 84.00 | 83 | 37.02 | 42 | 18.89 | 260 | 39.50 | 39.59 | 302 | 34.30 | 34.53 | |
| T-cell | Male | 2 | 1.84 | 3 | 2.68 | 3 | 2.64 | 1 | 0.89 | 8 | 2.38 | 2.39 | 9 | 2.01 | 2.02 |
| Female | 0 | 0.00 | 0 | 0.00 | 4 | 3.62 | 1 | 0.91 | 4 | 1.24 | 1.19 | 5 | 1.15 | 1.12 | |
| Total | 2 | 0.94 | 3 | 3.00 | 7 | 3.12 | 2 | 0.90 | 12 | 1.82 | 1.80 | 14 | 1.59 | 1.58 | |
| ALAL | Male | 0 | ––– | 0 | ––– | 1 | 0.88 | 0 | ––– | 1 | 0.30 | 0.29 | 1 | 0.22 | 0.22 |
| Female | 0 | ––– | 0 | ––– | 0 | ––– | 0 | ––– | 0 | — | ––– | 0 | ––– | ––– | |
| Total | 0 | ––– | 0 | ––– | 1 | 0.45 | 0 | ––– | 1 | 0.15 | 0.15 | 1 | 0.11 | 0.11 | |
AL, acute leukemia; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; ALAL, acute leukemias of ambiguous lineage.
3.1.2. 0 to 19 years
Subsequently, in this age group, the AL cIR was 44.1 cases per million for the three states and an ASIRw of 44.3. The ASIRw for ALL was 36.2, and for the B-cell subtype an ASIRw of 34.5.
3.2. Age incidence peaks by AL main subtypes
Two age incidence peaks for ALL were observed, the first between the ages of three and five years and the second between 13 and 16 years of age. For AML, also two incidence peaks were observed, a first at one year of age and a second at the age of 10 years.
3.3. Incidence rates by age group and states
3.3.1. 0 to 14 years
State of Puebla: The cIR for AL was 53.3 cases per million, and when the rate was standardized, it showed an ASIRw of 53.2. Regarding the AL subtype, again, it was ALL the most common subtype with an ASIRw of 45.2. The B-cell immunophenotype showed an ASIRw of 43.0 ( Supplementary Table 1 ).
State of Tlaxcala: The AL cIR in Tlaxcala was 53.4 cases per million with an ASIRw of 54.7. On the other hand, the ASIRw for the ALL subtype was 41.3 and for the B-cell subtype was 39.9 ( Supplementary Table 2 ).
State of Oaxaca: The observed cIR for AL was 47.5 cases per million, and when analyzing the ASIRw it was 47.7 cases per million. The ALL subtype presented an ASIRw of 35.7; also, the B-cell immunophenotype had an ASIRw of 34.0 ( Supplementary Table 3 ).
3.3.2. 0 to 19 years
State of Puebla: This state showed a cAIR of 46.3 cases per million for AL, and when the rate was standardized, it was observed an ASIRw of 46.4. Regarding the AL subtypes, ALL presented an ASIRw of 39.6, and the B-cell immunophenotype had an ASIRw of 37.7 ( Supplementary Table 3 ).
State of Tlaxcala: The AL cIR for Tlaxcala was 48.0 and an ASIRw of 48.2 per million. On the other hand, the ASIRw for the ALL subtype was 37.1, and the ASIRw for B-cell of 36.0 ( Supplementary Table 2 ).
State of Oaxaca: An AL cIR of 39.3 cases per million was observed for this age group with an ASIRw of 39.6 cases per million. The ALL subtype presented an ASIRw of 30.6; also, the B-cell immunophenotype group had an ASIRw of 28.9 ( Supplementary Table 3 ).
3.4. AL incidence rates by state subregions
The crude and standardized incidence rates of acute leukemia were reported for each subregion and represented on a choropleth map ( Figure 1 ).
In the age group from 0 to 14 years, the Mixteca (Puebla) presented one of the highest rates, reporting an ASIRw of 96.7, followed by three regions with rates above 60 cases per million: the Mixteca Oaxaqueña (ASIRw 69.0), Valles Centrales of Oaxaca (ASIRw 67.0), Valle de Atlixco-Izúcar de Matamoros (ASIRw of 66.0) ( Figure 1 ).
For the age group from 0 to 19 years, three regions stand out for their high rates: the Mixteca (Puebla) with an ASIRw of 88.5 cases per million, followed by the Center-South (Tlaxcala) with an ASIRw of 60.0, and ultimately, the region of Valles Centrales of Oaxaca with an ASIRw of 58.1 ( Figure 1 ).
Remarkably, the North region of Tlaxcala showed an extremely higher rate in both age groups (0-14 and 0-19), with an ASIRw of 173.2 and 130.8, respectively. However, these data should be taken cautiously to avoid the fallacy of small numbers because this region has a low number of populations under 20 years of age, which makes its rates susceptible to random fluctuation.
4. Discussion
To our knowledge, this is the first population-based report on the incidence of childhood AL in the south-central region of Mexico. Although we only report the incidence of two years of registration (2021-2022), we consider this study to be representative of the population since it includes the participation of all hospitals attending children and adolescents with this disease. It is worth mentioning that this study continues with its active registration of incident cases.
The incidences for AL observed in this study for the three states were very relevant, as higher rates were observed in the 0 to 14 years group with 51.5 cases per million than in the 0 to 19 years group with 44.3.
The rates for the 0 to 14 years group were observed slightly above the rates reported for the African regions (0.5-33.6). (1, 22, 23), Asia (30.7-48.2) (24–31), and Central and South America (33.3-49.8) (1, 2, 32). However, these rates are intermediate in comparison to those reported for the European regions (42.1-57.1) (33–41) and Oceania (50.0-53.5) (42–44). They are lower than the rates reported for the North American regions (31.3-65.4) (1, 9, 45–53).
On the other hand, the rates reported for AL in the 0-19 years age group were similar to those reported for the Asian (42.5) (54) and Central and South American (34.8-58.5) regions (4, 32, 55). However, they were lower than those reported in the European regions (51.2-54.1). (56, 57) and North America (26.2-64.8) (58–61).
It has already been described that there are population groups that have a higher incidence of leukemia such as children of Latin American descent (Hispanics), Oceanian Americans, and Pacific Islanders, as their rates range between 54.0-65.4 cases per million for the group of 0-14 years, we consider it relevant to note that the rates reported in this study were lower despite the fact that it is a Latin American ancestry population. (1, 9, 45, 47–50, 53). Similarly, it was observed in the 0-19 age group, which, when compared to the rates of the North American population of Latin American descent, describe rates of 55.0-60.5 cases per million, which are reported to be higher than the rates described in this study (58, 59). When the incidence rates for AL reported in this study were compared with those reported recently in GMC, it was observed that, although the rates are not low, they are not as high as those reported for children in GMC (63.3) (9). Regardless, the rates obtained in the present report could be higher considering several possible factors such as lack of access to diagnosis, poverty, geographic inaccessibility, degree of marginalization of families, and ethnicity, among others. For example, the National Council for the Evaluation of Social Policy and Development (CONEVAL) estimated in 2018 that the lack of access to health services was 20.8% for the population of the state of Puebla, 16% for the population of Oaxaca and, 13.7% in Tlaxcala (62); thus, it is not uncommon to find family histories in these types of regions with long journeys for medical care. These journeys may involve several trips using different types of transportation, including extensive pedestrian travel.
The diagnosis of childhood leukemia requires specialized care, in some cases leading the parents to visit different physicians on multiple occasions because the symptoms of the child persist. All of this may result in economic expenses that low-income families often cannot afford, leaving uncertainty about the child´s diagnosis. This and other social factors become very relevant to take into account when incidence rates of leukemias are reported. Particularly, the incidence rate of AL obtained in the present study for the state of Oaxaca could be underestimated not only as a consequence of the previously mentioned factor. Oaxaca has a lot of municipalities and most of them are far from the center of the state where specialists in hemato-oncological diseases are commonly found (63). It could then be possible that children from these regions of Oaxaca become ill with leukemia and do not have the opportunity to receiving a confirmation of their diagnosis, and leukemia-associated deaths are being attributed to other diseases with similar symptomatology (64).
These situations may also occur in the states of Puebla and Tlaxcala. For example, the Mexican death system reported 1169 deaths that were certified with causes of death of nonspecific signs and symptoms (ICD10 codes, R00-R99), in the three study states, in children under 20 years of age, during the period 2015-2019 (65). This phenomenon has been reported by other investigators who have mentioned that while cancer incidence rates are higher in urban areas, mortality rates are higher in rural areas (66, 67). In addition, it has also been reported that patients in rural areas are frequently diagnosed at later stages, are less likely to receive standard treatments, optimal medical follow-up, or support services, and therefore experience worse health outcomes compared to non-rural patients (68, 69).
Another important aspect to note from the results of the present study is in relation to the biphasic pattern of age peak of incidence observed for ALL and AML. The first peak of presentation for ALL and AML are consistent with that reported in North American and European populations (between 2 to 6, and between 1 to 4 years old, respectively). Importantly, these age peaks have been related to good prognostic factors and specific cytogenic aberrations. (70–72). In ALL, the second age peak was between 9 and 14 years, while for AML it was between 7 and 13 years. These findings are consistent with what has been previously reported in the Mexican population of GMC, 11-14 years for ALL and 10-12 years for AML. (9). Remarkably, in this study, the second peaks of presentation had a longer duration (5 years for ALL and 6 years for AML) than in the study conducted in GMC (3 years for ALL and 2 years for AML) and their peak incidence points were significantly higher: at 13 years of age with a cIR 71 cases per million for ALL and at 10 years of age with a cIR 20 in AML. It is well known that the age at diagnosis of childhood AL is an important predictor of poor outcomes. Then, it would be important to identify the survival rates of adolescents in these country regions which could be lower than in other states. Additionally, it would be relevant to study the environmental factors related to the presentation of the disease during adolescence.
The regions of Puebla, Tlaxcala, and Oaxaca have a multicultural origin since their population has been made up of a mixture of different indigenous populations, as well as European and, to a lesser extent, African peoples (73, 74). Moreover, the region presents significant socioeconomic inequalities based on ethnic origin which results in high poverty rates and marginalization in different areas. Recently, according to official data from Mexico, it was reported that a high proportion of the population in the states of Puebla, Tlaxcala, and Oaxaca live in poverty (62.4%, 59.3%, and 61.7%, respectively) and these frequencies are higher than the national average (36.3%), which, among other aspects, makes these regions to be considered as marginalized populations (75–77).
Mexico does not have a census of indigenous population, the closest indicator being the proportion of households that speak indigenous languages from INEGI’s population census. With this reference, it is known that 6.1% of the Mexican population at the national level speaks an indigenous language, while in Puebla it is 9.9% with 7 native Amerindian ethnic groups, Tlaxcala 2.2% with 2 ethnic groups, and Oaxaca 31.2% with 16 ethnic groups and an important group of Afro-descendant population (4.7%) (78). From the results of the present study, the subregions with the highest incidence rates were located in the center of the study region, in the area connecting the capital cities of Puebla and Oaxaca. The Mixteca region (Puebla) showed an AL incidence rate of 96.7 and 88.5 cases per million, for groups 0-14 and 0-19, respectively. Likewise, the Northern region (Tlaxcala) reports rates of 173.2 and 130. 8 cases per million for the 0-14 and 0-19 age groups, respectively; however, these last rates should be taken with caution, because although they are high, we think that they may also be influenced by the concentration of cases due to the search for medical care between regions; or it is simply a random fluctuation due to the short time of registration along with a low population base of the Northern region (Tlaxcala) (23,000 inhabitants under 20 years of age). Nevertheless, further registration of incident cases is mandatory.
4.1. Study limitations and strengths
One of the possible limitations of this study could be that hospitals in nearby states were not included due to the logistics of the project; this would imply the loss of some cases of resident children who migrated to neighboring states in search of medical attention. However, the observed rates were high despite this limitation, in addition to the fact that we counted the participation of all public and private hospitals in the region that attend to patients with this condition. Additionally, we also have the participation of public hospitals located in GMC. GMC represents the center of the country and is close to the states of Puebla and Tlaxcala. These hospitals have specialists in pediatric hematology and oncology as well as the infrastructure for the diagnosis and treatment of children from these and other states of the country.
The inclusion of death certificates as a supplementary source of information for the registry was unfeasible given the fact that in Mexico the information from death certificates becomes available at least two years after the conclusion of the relevant year of interest. Notwithstanding, death certificate information serves as an additional avenue for identifying incident cases of neoplasms that may be diagnosable in alternative health institutions or laboratories not encompassed within our study. Furthermore, acute leukemias represent pathological entities exclusively diagnosed within highly specialized hospitals or laboratories, akin to the participating institutions in the present research. On the other hand, the methodology employed in the present study entailed an active process carried out by trained personnel consisting of cross-referencing daily hospital admission registries and patient lists within each pediatric hematology and oncology department. This is to ensure the identification and follow-up of all the potential cases with acute leukemia until diagnosis confirmation.
Notably, we consider that a strength of this study was to follow quality control recommendations for the validation of population-based cancer registries: a) comparability, b) internal consistency, c) validity, and d) timeliness (16, 17). In the first instance, to maintain comparability among studies international standard classification and coding systems of neoplasms (ICD-O3 and ICCC-3) were considered in the present research. Additionally, according to the agreed standards about the definition of the incidence date, in the present study, the date of leukemia confirmation through the morphological study of the bone marrow aspirate was used. Secondly, internal consistency was checked. For this purpose, the registrars were standardized before the study initiation, and they were supervised by a local coordinator on a weekly basis by corroborating the information through phone calls, clinical charts, and laboratory data before they were reported in the central database. Likewise, the validity of the information was gained through the active and systematic revision of the morphological study of the bone marrow aspirates, histochemistry staining, and the immunophenotype which are routinely performed in the participant institutions. The percentage of cases with a morphologically verified diagnosis was 100%. Furthermore, the rate of cases with missing data was 0%. In addition, we collected information regarding the cause of death within the study population. Finally, regarding timeliness, in the present investigation rapid reporting was achieved considering that the average time between case confirmation and report in the central database was seven days. Consequently, the data obtained in this study has been collected with sufficient rigor to constitute a first reference of the descriptive epidemiology of childhood acute leukemias in the states of Puebla, Tlaxcala, and Oaxaca.
5. Conclusion
The present work is a robust source of information on the incidence of acute leukemia in the south-central region of the Mexican Republic. These rates are within the range reported in other populations of Latin American origin. Two age peaks of occurrence were observed in the first years of life and a second peak after 7 years of life. Additionally, differences were observed between subregions that could be attributed to social factors linked to the ethnic origin of the populations, but further research is mandatory to elucidate this hypothesis. Finally, we consider this a valuable report for the planning of care and research strategies for acute leukemias in the region.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by National Scientific Research and Ethics Committee of the Mexican Institute of Social Security. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
JF-L: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. AA-L: Conceptualization, Data curation, Formal analysis, Investigation, Supervision, Writing – original draft, Writing – review & editing, Methodology. DD-R: Writing – original draft, Writing – review & editing, Formal analysis, Investigation, Methodology. EA-Ru: Writing – original draft, Writing – review & editing, Formal analysis, Investigation, Methodology. LL-C: Writing – review & editing, Investigation. TS-L: Investigation, Writing – review & editing. MC: Investigation, Writing – review & editing. MB-L: Investigation, Writing – review & editing. DC-A: Investigation, Writing – review & editing. JE-R: Investigation, Writing – review & editing. JL-A: Investigation, Writing – review & editing. MG-H: Investigation, Writing – review & editing. DO-C: Investigation, Writing – review & editing. VT-C: Investigation, Writing – review & editing. KM-J: Investigation, Writing – review & editing. PA-C: Investigation, Writing – review & editing. EA-Ro: Investigation, Writing – review & editing. WH-O: Investigation, Writing – review & editing. GR-A: Investigation, Writing – review & editing. LC-A: Investigation, Writing – review & editing. AM-T: Investigation, Writing – review & editing. LC-C: Investigation, Writing – review & editing. NL-S: Investigation, Writing – original draft. MM-M: Investigation, Writing – review & editing. AR-R: Investigation, Writing – review & editing. LM-P: Investigation, Writing – review & editing. CG-D: Investigation, Writing – review & editing. AM-S: Investigation, Writing – review & editing. MG-R: Investigation, Writing – review & editing. JM-T: Investigation, Writing – review & editing. ER-C: Investigation, Writing – review & editing. VB-M: Investigation, Writing – review & editing. MR-T: Investigation, Writing – review & editing. AC-M: Investigation, Writing – review & editing. GJ-A: Investigation, Writing – review & editing. SP-T: Funding acquisition, Investigation, Resources, Supervision, Writing – review & editing. JR-E: Investigation, Writing – review & editing. MS-A: Investigation, Writing – review & editing. FH-Q: Investigation, Writing – review & editing. AH-D: Investigation, Writing – review & editing. LG-G: Investigation, Writing – review & editing. MM-R: Investigation, Writing – review & editing. AO-S: Investigation, Writing – review & editing. HR-V: Investigation, Writing – review & editing. SJ-M: Investigation, Writing – review & editing. MC-G: Investigation, Writing – review & editing. MÁ-B: Investigation, Writing – review & editing. CD-M: Investigation, Writing – review & editing. RP: Funding acquisition, Investigation, Resources, Supervision, Writing – review & editing. JM-A: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JN-E: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Acknowledgments
The authors thank to "Fundación IMSS, A.C." for the extraordinary support in the administration of the funds received. Additionally, to “Una Nueva Esperanza”, an association for children with cancer, and Laboratorios Juárez Oaxaca, for the facilities given to this work. Furthermore, this population-based project has been possible thanks to the active participation of the following health professionals: Martha Rocío Córtes de la-Barrera, Andrea Huerta-Moreno, Deyanira Córtes-Alva, Raquel Hernández-Ramos, Cynthia Shanat Cruz-Medina, Alvaro José Montiel-Jarquín, Patricia Zagoya-Martínez, Juan Carlos Solís-Poblano, Andrea Huerta-Moreno, Lilia García-Stivalet, María Guadalupe Pérez-Dorantes, Amara Sequeira-Colonnier, Cindy Trinidad Vera-Vicaña, Ana Karen Chamizo-Aguilar, Alejandro Ivan Esquivel-Lú, Adrián Morales-Maravilla, Cynthia Shanat Cruz-Medina, Lourdes Esthela Juan Lien-Chang, Brianda García-Hidalgo, Moises Manuel Gallardo-Pérez, Xochiquetzatl Jiménez-López, Jose Luis Galvez-Romero, Alonso Antonio Collantes-Gutiérrez, Fernando Navarro-Tovar, Mario García-López, Xochiquetzatl Jiménez-López, Flor Lucía Morales-Morales, Claudia Guevara-Espejel, Raquel Hernández-Ramos, Federico Osorio-Antonio, María de Lourdes Flores-Urbina, Raymundo Cuevas-Escalante, Maria Berenice Gónzalez-Romero, Roberto Tepatzi-Carranco, Jessica García-Téllez, María Isabel Martínez-Hernández, Irma Alejandra Hernández-Vicente, Karina Beatriz Martínez-Jose, and Ana Karen Rodriguez-Muñoz. The authors also wish to acknowledge the invaluable contributions and dedication of the PRONAII Childhood Leukemia fieldwork team. Each member played a vital role in advancing the project. Martha Eugenia Juárez Martínez, Alma Itandehui Luna Silva, Juan Carlos Rodríguez Espinosa, César Omar Trejo Pichardo, Keyra Quetzal Ramírez Menes, Diana Patricia Ascencio Gorozpe, Elizabeth Báez Báez, Devaki Meneses Flores, Zenaida Daniela Alatriste Roque, Alberto Antonio Herrera Avendaño, Sayuri Lorelei Zepeda Mendoza, Aldo Daniel Espinosa Espinosa, Javier Alejandro Lima Cervantes, José Froylan Rojas Hernández, Lilia Hernández Gasca, Miriam Carmina Suárez Aguirre, Lizeth Jocelyn Serna Villalobos, José Antonio Hernández Merino, Ricardo David Andrade Espinoza, Aurora Verónica Delgado Gaytan, Saraí Morales Rojas, Ana Berenice Contreras Cuevas, María Monserrat Betanzos Cevallos, Margarita Vargas Huerta, Mitzi Elizabeth Amaro Espinosa, Luisa Daniela Vásquez Gasca, Arianey Aldara Venegas de Jesús, Carmen Paola Nezahual Hernández, Mayra Pérez ángel, Sandra Jessica Olivera Hernández, José Edmundo Balderas Castro, Sebastián Ibarra Zamarrón Guillermo Márquez Carmona, Fernando Cruz Reyna, Anahí Clark Castaño, Laura Tufiño Gutiérrez, Rodrigo Romero González, Liliana Angelica Santana Vergara, Karen Dominique Hernandez Ríos, Magdalena Landa Ortiz, and José Jacinto Vega.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Consejo Nacional de Humanidades, Ciencias y Tecnologías (CONAHCYT) with the following grant number: FORDECYT-PRONACES: 303019 (JN-E); FORDECYT-PRONACES: 302994 (RP), FORDECYT-PRONACES 302941 (SP-T) and to the Instituto Nacional de Medicina Genómica (INMEGEN) (2024-01) for the payment of the publication. The funder had no role in the study design, in the collection and analysis of data, in the writing of the report, and in the decision to submit the article for publication. All researchers have independence from funders.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that authors JN-E, RP and JM-A were all Topic Editors and were members of Frontiers at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1304263/full#supplementary-material
References
- 1. Steliarova-Foucher E, Colombet M, Ries LAG, Moreno F, Dolya A, Bray F, et al. International incidence of childhood cancer 2001–10: A population-based registry study. Lancet Oncol (2017) 18(6):719–31. doi: 10.1016/S1470-2045(17)30186-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moreno F, Loria D, Abriata G, Terracini B. Childhood cancer: incidence and early deaths in Argentina 2000-2008. Eur J Cancer (2013) 49(2):465–735. doi: 10.1016/J.EJCA.2012.08.001 [DOI] [PubMed] [Google Scholar]
- 3. OECD . Survival and mortality for leukaemia in children. Paris: OECD; (2017) p. 126–27. doi: 10.1787/health_glance-2017-42-en [DOI] [Google Scholar]
- 4. Erdmann F, Li T, Luta G, Giddings BM, Alvarado GT, Steliarova-Foucher E, et al. Incidence of childhood cancer in Costa Rica 2000–2014: an international perspective. Cancer Epidemiol (2018) 56(October):21–30. doi: 10.1016/j.canep.2018.07.004 [DOI] [PubMed] [Google Scholar]
- 5. Friestino JKO, Mendonça D, Oliveira P, Oliveira CM, Filho DdeCM. Childhood cancer: incidence and spatial patterns in the city of campinas, Brazil 1996-2005. Salud Colectiva (2018) 14(1):51–635. doi: 10.18294/SC.2018.1200 [DOI] [PubMed] [Google Scholar]
- 6. Torres-Roman JS, Valcarcel B, Guerra-Canchari P, Santos CAD, Barbosa IR, Vecchia CLa, et al. Leukemia mortality in children from latin America: trends and predictions to 2030. BMC Pediatr (2020) 20(1):1–9. doi: 10.1186/S12887-020-02408-Y/TABLES/2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. INEGI . Estadística de Defunciones Registradas (EDR) Enero a Septiembre de 2022. Cifras Preliminares. Aguascalientes, Mexico: Comunicación Social; (2023). Available at: https://www.inegi.org.mx/app/saladeprensa/noticia.html?id=8027. [Google Scholar]
- 8. Wiemels JL, Gallant RE. Infections and acute lymphoblastic leukemia: is the sum worth more than the parts? evidence from birth characteristics. Cancer Epidemiol Biomarkers Prev (2023) 32:292–4. doi: 10.1158/1055-9965.EPI-22-1257 [DOI] [PubMed] [Google Scholar]
- 9. Flores-Lujano J, Duarte-Rodríguez DAldebarán, Jiménez-Hernández E, Martín-Trejo JA, Allende-López A, Peñaloza-González JoséG, et al. Persistently high incidence rates of childhood acute leukemias from 2010 to 2017 in Mexico city: A population study from the MIGICCL. Front Public Health (2022) 10:918921/BIBTEX(September). doi: 10.3389/FPUBH.2022.918921/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Martín-Trejo JA, Núñez-Enríquez JC, Fajardo-Gutiérrez A, Medina-Sansón A, Flores-Lujano J, Jiménez-Hernández E, et al. Early mortality in children with acute lymphoblastic leukemia in a developing country: the role of malnutrition at diagnosis. A multicenter cohort MIGICCL study. Leukemia Lymphoma (2017) 58(4):898–908. doi: 10.1080/10428194.2016.1219904 [DOI] [PubMed] [Google Scholar]
- 11. Núñez-Enríquez JC, Gil-Hernández AE, Jiménez-Hernández E, Fajardo-Gutiérrez A, Medina-Sansón A, Flores-Lujano J, et al. Overweight and obesity as predictors of early mortality in Mexican children with acute lymphoblastic leukemia: A multicenter cohort study. BMC Cancer (2019) 19(1):708. doi: 10.1186/s12885-019-5878-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Petridou ET, Sergentanis TN, Perlepe C, Papathoma P, Tsilimidos G, Kontogeorgi E, et al. Socioeconomic disparities in survival from childhood leukemia in the United States and globally: A meta-analysis. Ann Oncol (2015) 26:589–97. doi: 10.1093/annonc/mdu572 [DOI] [PubMed] [Google Scholar]
- 13. Del Risco Kollerud R, Blaasaas KG, Claussen B. Poverty and the risk of leukemia and cancer in the central nervous system in children: A cohort study in a high-income country. (2015) 43:736–43. doi: 10.1177/1403494815590499 [DOI] [PubMed] [Google Scholar]
- 14. Onyije FM, Olsson A, Baaken D, Erdmann F, Stanulla M, Wollschläger D, et al. Environmental risk factors for childhood acute lymphoblastic leukemia: an umbrella review. Cancers (Basel) (2022) 14:382. doi: 10.3390/CANCERS14020382/S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gupta S, Bonilla M, Fuentes SL, Caniza M, Howard SC, Barr R, et al. Incidence and predictors of treatment-related mortality in paediatric acute leukaemia in El Salvador. Br J Cancer (2009) 100:1026–31. doi: 10.1038/sj.bjc.6604895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Steliarova-Foucher E, Stiller C, Lacour B, Kaatsch P. International classification of childhood cancer, third edition. Cancer (2005) 103(7):1457–675. doi: 10.1002/CNCR.20910 [DOI] [PubMed] [Google Scholar]
- 17. WHO . International classification of diseases for oncology (2013). Available at: https://www.who.int/standards/classifications/other-classifications/international-classification-of-diseases-for-oncology.
- 18. CONAPO . Poblaciones municipales del polígono de estudio en el periodo 2021-2022. In: Proyecciones de la Población de México y de Los Municipios 2016-2050, vol. 2015. Mexico City: Consejo Nacional de Población; (2015). [Google Scholar]
- 19. Honorable Congreso del Estado Libre y Soberano de Oaxaca . Constitución Política Del Estado Libre y Soberano de Oaxaca. Oaxaca, Mexico: Honorable Congreso del Estado Libre y Soberano de Oaxaca; (2009). [Google Scholar]
- 20. Consejo Nacional de Población . Proyecciones de la Población de México y de Las Entidades Federativas 2016-2050. República Mexicana (2019). Available at: http://www.conapo.gob.mx/work/models/CONAPO/Cuadernillos/33_Republica_Mexicana/33_RMEX.pdf.
- 21. Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M, et al. Age standardization of rates: A new WHO standard (2001). Available at: http://www.who.int/healthinfo/paper31.pdf.
- 22. Stefan C, Bray F, Ferlay J, Liu B, Parkin DM. Cancer of childhood in sub-saharan Africa. Ecancermedicalscience (2017) 11(July):755. doi: 10.3332/ecancer.2017.755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Otoo MN, Lubbe MS, Steyn H, Burger JR. Childhood cancers in a section of the South African private health sector: analysis of medicines claims data. Health SA Gesondheid (2020) 25(September):a1382. doi: 10.4102/hsag.v25i0.1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Al-Asadi JN, Ibrahim SJ. Childhood cancer in Basrah, Iraq during 2012-2016: incidence and mortality. Asian Pacific J Cancer Prev (2018) 19(8):2337–415. doi: 10.22034/APJCP.2018.19.8.2337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shabani M, Moghaddam SS, Ataeinia B, Rezaei N, Mohebi F, Mohajer B, et al. Trends of national and subnational incidence of childhood cancer groups in Iran: 1990–2016. Front Oncol (2020) 9:1428(January). doi: 10.3389/fonc.2019.01428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Abood RA, Abdahmed KA, Mazyed SS. Epidemiology of different types of cancers reported in Basra, Iraq. Sultan Qaboos Univ Med J (2020) 20(3):295–3005. doi: 10.18295/squmj.2020.20.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wiangnon S, Jetsrisuparb A, Komvilaisak P, Suwanrungruang K. Childhood cancer incidence and survival 1985-2009, Khon Kaen, Thailand. Asian Pacific J Cancer Prev (2014) 15(18):7989–93. doi: 10.7314/APJCP.2014.15.18.7989 [DOI] [PubMed] [Google Scholar]
- 28. Belgaumi AF, Pathan GQ, Siddiqui K, Ali AA, Al-Fawaz I, Al-Sweedan S, et al. Incidence, clinical distribution, and patient characteristics of childhood cancer in Saudi Arabia: A population-based analysis. Pediatr Blood Cancer (2019) 66(6):e276845. doi: 10.1002/pbc.27684 [DOI] [PubMed] [Google Scholar]
- 29. Akhtar S, Al-Abkal J, Al-Shammari A. Childhood leukaemia incidence and trends in a middle eastern country during 1980–2014: A population-based study. Cancer Causes Control (2020) 31(3):231–405. doi: 10.1007/s10552-020-01267-3 [DOI] [PubMed] [Google Scholar]
- 30. Jastaniah W, Essa MF, Ballourah W, Abosoudah I, Daama SAl, Algiraigri AH, et al. Incidence trends of childhood acute lymphoblastic leukemia in Saudi Arabia: increasing incidence or competing risks? Cancer Epidemiol (2020) 67(August):101764. doi: 10.1016/j.canep.2020.101764 [DOI] [PubMed] [Google Scholar]
- 31. Rahimi Pordanjani S, Kavousi A, Mirbagheri B, Shahsavani A, Etemad K. Temporal trend and spatial distribution of acute lymphoblastic leukemia in Iranian children during 2006-2014: A mixed ecological study. Epidemiol Health (2020) 42:e2020057. doi: 10.4178/epih.e2020057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Oliveira Friestino JK, Mendonça D, Oliveira P, Oliveira CM, de Carvalho Moreira Filho D. Cáncer Infantil: Incidencia y Patrones Espaciales En La Ciudad de Campinas, Brasil 1996-2005. Salud Colectiva (2018) 14(1):51–635. doi: 10.18294/sc.2018.1200 [DOI] [PubMed] [Google Scholar]
- 33. Peris-Bonet R, Salmerón D, Martínez-Beneito MA, Galceran J, Marcos-Gragera R, Felipe S, et al. Childhood cancer incidence and survival in Spain. Ann Oncol (2010) 21(SUPPL.3):iii103–10. doi: 10.1093/annonc/mdq092 [DOI] [PubMed] [Google Scholar]
- 34. AIRTUM Working Group, CCM, and AIEOP Working Group . I tumori in italia - rapporto 2012 I tumori dei bambini e degli adolescenti. In: Epidemiologia e prevenzione, vol. 40. Milan, Italy: Associazione Italiana Registri Tumori; (2016). p. 1–245. [Google Scholar]
- 35. Jakab Z, Juhasz A, Nagy C, Schuler D, Garami M, Hungarian Paediatric Haemato-Oncology Network . Trends and territorial inequalities of incidence and survival of childhood leukaemia and their relations to socioeconomic status in Hungary 1971-2015. Eur J Cancer Prev (2017) 26(September):S183–90. doi: 10.1097/CEJ.0000000000000386 [DOI] [PubMed] [Google Scholar]
- 36. González-García H, Garrote-Molpeceres R, Urbaneja-Rodríguez E, Gutiérrez-Meléndez P, Herráiz-Cristóbal R, Pino-Vázquez MaríaAsunción, et al. Differences in incidence and survival to childhood cancer between rural and urban areas in castilla y león, Spain, (2003–2014). Medicine (2018) 97(41):e12797. doi: 10.1097/MD.0000000000012797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sommer G, Schindler M, Redmond S, Pfeiffer V, Konstantinoudis G, Ammann RA, et al. Temporal trends in incidence of childhood cancer in Switzerland 1985–2014. Cancer Epidemiol (2019) 61(August):157–64. doi: 10.1016/j.canep.2019.06.002 [DOI] [PubMed] [Google Scholar]
- 38. Broccia G, Carter J, Ozsin-Ozler C, Meloni F, Pilia I, Satta G, et al. Haemolymphatic cancer among children in sardinia, Italy: 1974-2003 incidence. BMJ Open (2020) 10(11):371635. doi: 10.1136/bmjopen-2020-037163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Krejci D, Zapletalova M, Svobodova I, Bajciova V, Mudry P, Smelhaus V, et al. Childhood cancer epidemiology in the Czech Republic, (1994–2016). Cancer Epidemiol (2020) 69(December):101848. doi: 10.1016/j.canep.2020.101848 [DOI] [PubMed] [Google Scholar]
- 40. Paapsi K, Baburin A, Mikkel S, Mägi M, Saks K, Innos K. Childhood cancer incidence and survival trends in Estonia, (1970-2016): A nationwide population-based study. BMC Cancer (2020) 20(1):305. doi: 10.1186/s12885-019-6510-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Reedijk AMJ, Kremer LC, Visser O, Lemmens V, Pieters R, Coebergh JWW, et al. Increasing incidence of cancer and stage migration towards advanced disease in children and young adolescents in the Netherlands 1990–2017. Eur J Cancer (2020) 134(July):115–26. doi: 10.1016/j.ejca.2020.04.011 [DOI] [PubMed] [Google Scholar]
- 42. Baade PD, Youlden DR, Valery PC, Hassall T, Ward L, Green AC, et al. Trends in incidence of childhood cancer in Australia 1983-2006. Br J Cancer (2010) 102(3):620–26. doi: 10.1038/sj.bjc.6605503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Holland LR, Bradford NK, Youl P, Cossio D, Dunn N, Tran N, et al. Cancer incidence, mortality, and survival for children, adolescents, and young adults in queensland between 1987 and 2016. J Adolesc Young Adult Oncol (2020) 2(December):16. doi: 10.1089/jayao.2020.0151 [DOI] [PubMed] [Google Scholar]
- 44. Youlden DR, Baade PD, Green AdèleC, Valery PC, Moore AS, Aitken JF. The incidence of childhood cancer in Australia 1983–2015, and projections to 2035. Med J Aust (2020) 212(3):113–20. doi: 10.5694/mja2.50456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fajardo-Gutiérrez A, González-Miranda G, Pachuca-Vázquez A, Allende-López A, Fajardo-Yamamoto LM, Rendón-Macías ME. Cancer incidence and mortality in children in the Mexican social security institute, (1996-2013). Salud Publica Mexico (2016) 58(2):162–705. doi: 10.21149/spm.v58i2.7785 [DOI] [PubMed] [Google Scholar]
- 46. Wilkinson JD, Fleming LE, MacKinnon J, Voti L, Wohler-Torres B, Peace S, et al. Lymphoma and lymphoid leukemia incidence in Florida children. Cancer (2001) 91:1402–8. doi: [DOI] [PubMed] [Google Scholar]
- 47. Services, Texas Department of State Health . Childhood and adolescent cancer. Austin, Texas: Texas Cancer Registry. SEER*Stat Database, 1995-2017 Incidence, Texas Statewide; (2020). Available at: https://www.dshs.state.tx.us/tcr/childhood.shtm. [Google Scholar]
- 48. Mejía-Aranguré JM, Bonilla M, Lorenzana R, Juárez-Ocaña S, Reyes Gde, Pérez-Saldivar MaríaL, et al. Incidence of leukemias in children from El Salvador and Mexico city between 1996 and 2000: population-based data. BMC Cancer (2005) 5(January):33. doi: 10.1186/1471-2407-5-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Fajardo-Gutiérrez A, Juárez-Ocaña S, González-Miranda G, Palma-Padilla V, Carreón-Cruz R, Ortega-Alvárez MC, et al. Incidence of cancer in children residing in ten jurisdictions of the Mexican republic: importance of the cancer registry (a population-based study). BMC Cancer (2007) 7(January):68. doi: 10.1186/1471-2407-7-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Pérez-Saldivar MaríaL, Fajardo-Gutiérrez A, Bernáldez-Ríos R, Martínez-Avalos A, Medina-Sanson A, Espinosa-Hernández L, et al. Childhood acute leukemias are frequent in Mexico city: descriptive epidemiology. BMC Cancer (2011) 11(1):355. doi: 10.1186/1471-2407-11-355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mejía-Aranguré JM, Núñez-Enríquez JC, Fajardo-Gutiérrez A, Rodríguez-Zepeda MDC, Martín-Trejo JA, Duarte-Rodríguez DA, et al. Epidemiología descriptiva de la leucemia mieloide aguda (LMA) en niños residentes de la Ciudad de México: reporte del Grupo Mexicano Interinstitucional para la Identificación de las Causas de la Leucemia en Niños. Gac Med Mex (2016) 152:66–77. Available at: http://www.ncbi.nlm.nih.gov/pubmed/27792718 (Accessed March 5, 2018). [PubMed] [Google Scholar]
- 52. Chen X, Pan J, Wang S, Hong S, Hong S, He S. The epidemiological trend of acute myeloid leukemia in childhood: A population-based analysis. J Cancer (2019) 10:4824–35. doi: 10.7150/jca.32326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Glazer ER, Perkins CI, Young JL, Schlag RD, Campleman SL, Wright WE. Cancer among hispanic children in California 1988-1994: comparison with non-hispanic white children. Cancer (1999) 86(6):1070–79. doi: 10.1097/MPH.0000000000001017 [DOI] [PubMed] [Google Scholar]
- 54. Chen Q, Guo Z, Liu S, Quan P, Cao X, Guo L, et al. The cancer incidence and mortality among children and adolescents during the period of 2010-2014 in Henan Province, China. Cancer Med (2019) 8:814–23. doi: 10.1002/cam4.1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bastos LídiaNV, Silveira JoséC, Luna CF, Lucena-Silva N. Childhood and adolescent cancer in the state of pernambuco, Brazil: incidence, geographical distribution, and association with environmental health indicators. J Pediatr Hematology/Oncology (2018) 40(1):7–145. doi: 10.1097/MPH.0000000000001017 [DOI] [PubMed] [Google Scholar]
- 56. Karim-Kos HE, Hackl M, Mann G, Urban C, Woehrer A, Slavc I, et al. Trends in incidence, survival and mortality of childhood and adolescent cancer in Austria 1994-2011. Cancer Epidemiol (2016) 42(June):72–81. doi: 10.1016/j.canep.2016.03.015 [DOI] [PubMed] [Google Scholar]
- 57. Isaevska E, Manasievska M, Alessi D, Mosso ML, Magnani C, Sacerdote C, et al. Cancer incidence rates and trends among children and adolescents in piedmont 1967–2011. PloS One (2017) 12(7):e01818055. doi: 10.1371/journal.pone.0181805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Giddings BM, Whitehead TP, Metayer C, Miller MD. Childhood leukemia incidence in california: high and rising in the hispanic population. Cancer (2016) 122(18):2867–755. doi: 10.1002/cncr.30129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Barrington-Trimis JL, Cockburn M, Metayer C, Gauderman WJ, Wiemels J, McKean-Cowdin R. Trends in childhood leukemia incidence over two decades from 1992 to 2013. Int J Cancer (2017) 140(5):1000–10085. doi: 10.1002/ijc.30487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Siegel DA, Henley SJ, Li J, Pollack LA, Van Dyne EA, White A. Rates and trends of pediatric acute lymphoblastic leukemia — United States 2001–2014. MMWR. Morbidity Mortality Weekly Rep (2017) 66(36):950–545. doi: 10.15585/mmwr.mm6636a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Moore KJ, Hubbard AK, Williams LA, Spector LG. Childhood cancer incidence among specific asian and pacific islander populations in the United States. Int J Cancer (2020) 147(12):3339–485. doi: 10.1002/ijc.33153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Consejo Nacional de Evaluación de la Política de Desarrollo Social . Evaluación de la Política de Desarrollo Social 2018. Mexico City: Evaluación de la Política Social; (2018). Available at: https://www.coneval.org.mx/Evaluacion/IEPSM/IEPSM/Paginas/IEPDS-2018.aspx. [Google Scholar]
- 63. Secretaría de Gobernación. Consejo Nacional de Población. Instituto Mexicano del Transporte. CentroGeo . Análisis Geoespacial de la Accesibilidad a Centros Urbanos de Las Localidades de México. Mexico City: Documentos Del Consejo Nacional de Población; (2023). Available at: https://www.gob.mx/conapo/documentos/analisis-geoespacial-de-la-accesibilidad-a-centros-urbanos-de-las-localidades-de-Mexico?idiom=es. [Google Scholar]
- 64. López Hernández RC, Velasco AndrésEM, López APHernández. La Salud Urbana de Las Ciudades de Oaxaca y La Reducción de Las Desigualdades Económicas En El Uso de Servicios de Salud. In: Zamora JoséG, E H, Esteves H, editors. Factores Críticos y Estratégicos En La Interacción Territorial Desafíos Actuales y Escenarios Futuros, 1st ed, vol. II . Mexico City: Ciudad de México: Universidad Nacional Autónoma de México y Asociación Mexicana de Ciencias para el Desarrollo Regional A.C, Coeditores; (2020). p. 815–32. [Google Scholar]
- 65. INEGI . Mortalidad Vol. 2022. Aguascalientes, Mexico: Subsistema de Información Demográfica y Social; (2022). Available at: https://www.inegi.org.mx/programas/mortalidad/datos_abiertos. [Google Scholar]
- 66. Levit LA, Byatt L, Lyss AP, Paskett ED, Levit K, Kirkwood K, et al. Closing the rural cancer care gap: three institutional approaches. JCO Oncol Pract (2020) 16(7):422–305. doi: 10.1200/op.20.00174 [DOI] [PubMed] [Google Scholar]
- 67. Henley SJ, Anderson RN, Thomas CC, Massetti GM, Peaker B, Richardson LC. Invasive cancer incidence 2004–2013, and deaths 2006–2015, in nonmetropolitan and metropolitan counties — United States. MMWR. Surveillance Summaries (2023) 66(14):1–13. doi: 10.15585/MMWR.SS6614A1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Chow CJ, Al-Refaie WB, Abraham A, Markin A, Zhong W, Rothenberger DA, et al. Does patient rurality predict quality colon cancer care?: A population-based study. Dis Colon Rectum (2015) 58(4):415–225. doi: 10.1097/DCR.0000000000000173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the case for investment in rural cancer control: an analysis of rural cancer incidence, mortality, and funding trends. Cancer Epidemiol Biomarkers Prev (2017) 26(7):992–75. doi: 10.1158/1055-9965.EPI-17-0092/350815/P/MAKING-THE-CASE-FOR-INVESTMENT-IN-RURAL-CANCER [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Swensen AR, Ross JA, Severson RK, Pollock BH, Robison LL. The age peak in childhood acute lymphoblastic leukemia: exploring the potential relationship with socioeconomic status. Cancer (1997) 79(10):2045–51. doi: 10.1097/01.mph.0000212972.90877.28 [DOI] [PubMed] [Google Scholar]
- 71. Forestier E, Schmiegelow K. The incidence peaks of the childhood acute leukemias reflect specific cytogenetic aberrations. J Pediatr Hematology/Oncology (2006) 28(8):486–955. doi: 10.1097/01.MPH.0000212972.90877.28 [DOI] [PubMed] [Google Scholar]
- 72. Marcotte EL, Spector LG, Mendes-de-Almeida DP, Nelson HH. The prenatal origin of childhood leukemia: potential applications for epidemiology and newborn screening. Front Pediatr (2021) 9:639479/BIBTEX(April). doi: 10.3389/FPED.2021.639479/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Price AL, Patterson N, Yu F, Cox DR, Waliszewska A, McDonald GJ, et al. A genomewide admixture map for latino populations. Am J Hum Genet (2007) 80(6):1024–36. doi: 10.1086/518313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. INEGI . Censo de Población y Vivienda 2020 Vol. 2020. Aguascalientes, Mexico: Censos y Conteos de Población y Vivienda; (2020). Available at: https://www.inegi.org.mx/programas/ccpv/2020/Datos_abiertos. [Google Scholar]
- 75. Consejo Nacional de Evaluación de la Política de Desarrollo Social . Informes de Pobreza y Evaluacion 2022. Puebla: Consejo Nacional de Evaluación de la Política de Desarrollo Social; (2023). Available at: https://www.coneval.org.mx/coordinacion/entidades/Documents/Informes_pobreza_evaluacion_2022/Puebla.pdf. [Google Scholar]
- 76. Consejo Nacional de Evaluación de la Política de Desarrollo Social . Informes de Pobreza y Evaluacion 2022. Tlaxcala: Consejo Nacional de Evaluación de la Política de Desarrollo Social; (2023). Available at: https://www.coneval.org.mx/coordinacion/entidades/Documents/Informes_pobreza_evaluacion_2022/Tlaxcala.pdf. [Google Scholar]
- 77. Consejo Nacional de Evaluación de la Política de Desarrollo Social . Informes de Pobreza y Evaluacion 2022. Oaxaca: Consejo Nacional de Evaluación de la Política de Desarrollo Social; (2023). Available at: https://www.coneval.org.mx/coordinacion/entidades/Documents/Informes_pobreza_evaluacion_2022/Oaxaca.pdf. [Google Scholar]
- 78. Instituto Nacional de los Pueblos Indígenas . Distribución por entidad federativa Vol. 2020. Mexico City: Atlas de Los Pueblos Indígenas de México; (2020). Available at: https://atlas.inpi.gob.mx/distribucion-por-entidad-federativa/. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.