Abstract
The co-occurrence of Thrombocytopenia with Absent Radius (TAR) syndrome and Langerhans Cell Histiocytosis (LCH) is exceedingly rare, with scant documentation in existing medical literature. This case report aims to shed light on this unique intersection of conditions, emphasizing the diagnostic and therapeutic challenges it presents. A 27-year-old female with a history of TAR syndrome presented with microcytic anemia, hip pain, and gastrointestinal symptoms. Terminal ileum intubation during colonoscopy revealed superficial ulcerations, leading to a biopsy that confirmed LCH. Subsequent radiologic investigations, including CT and MRI, showed multiple osseous lesions in the pelvis, sacrum, and skull. A treatment plan involving IV Cytarabine was initiated due to concerns of CNS involvement, as indicated by mastoid air cell involvement and symptoms of dizziness and ear fullness. The case highlights the diagnostic value of terminal ileum intubation during colonoscopy, which was pivotal in diagnosing LCH in this patient. It also discusses the use of IV cytarabine, a chemotherapy drug that inhibits DNA synthesis, as a suitable treatment option given the suspected CNS involvement. The case adds to the limited literature on the natural history and management of adult patients with LCH, particularly in the context of TAR syndrome. This case report serves as a compelling addition to medical literature, highlighting the diagnostic complexities and treatment considerations in a patient with both TAR syndrome and LCH. It emphasizes the importance of comprehensive diagnostic approaches, including terminal ileum intubation during colonoscopy, and introduces IV cytarabine as a viable treatment option for cases with suspected CNS involvement.
Keywords: Thrombocytopenia with absent radius, Langerhans cell histiocytosis, Colonoscopy, Terminal ileum, Cytarabine, PET
Introduction
Thrombocytopenia with Absent Radius (TAR) syndrome and Langerhans cell histiocytosis (LCH) are both rare medical conditions, each presenting its own set of diagnostic and therapeutic challenges [1]. TAR syndrome is a congenital disorder characterized by the absence of the radius bone in the forearm and a low platelet count, often leading to bleeding tendencies [2]. On the other hand, LCH is a complex disorder involving the proliferation of Langerhans cells, a type of dendritic cell, that affects various organs and systems in the body [3], [4], [5]. While each of these conditions is individually rare and well-documented, the co-occurrence of TAR syndrome and LCH in a single patient is an extraordinary medical anomaly with scant literature to guide clinicians [1].
The rarity of each condition and the unique challenges posed by their coexistence make this case a compelling subject for clinical discussion [1,6]. The diagnosis of LCH, in particular, can be elusive and often requires a multimodal approach involving histopathology, radiology, and sometimes, advanced molecular techniques [7]. The management of LCH is further complicated when it occurs in a patient with an existing complex condition like TAR syndrome, which itself has various hematological and orthopedic implications [1,8].
This case report aims to present a 27-year-old female patient with a known history of TAR syndrome who was subsequently diagnosed with LCH. The report will delve into the diagnostic journey, emphasizing the role of terminal ileum intubation during colonoscopy, which was instrumental in diagnosing LCH. We will also discuss the therapeutic challenges and decisions, including the use of intravenous (IV) cytarabine due to concerns of central nervous system (CNS) involvement.
Case presentation
A 27-year-old female with a pre-existing diagnosis of Thrombocytopenia with Absent Radius (TAR) syndrome presented with multiple concerning symptoms. She reported fatigue, unintentional weight loss of 10 pounds over the past year, and enlarging lymph nodes in her neck and underarm area. Additionally, she had been experiencing dark, tarry stools once a week for the past month. Due to these gastrointestinal symptoms, she was scheduled for an Esophagogastroduodenoscopy (EGD) and colonoscopy.
Concurrently, the patient complained of left hip pain, prompting further imaging. An X-ray of the hip revealed a new lucency at the medial aspect of the left femoral head, which was not present on a previous CT scan (Fig. 1). A subsequent MRI of the pelvis showed multiple osseous lesions, raising concerns for metastatic disease. A CT-guided targeted bone biopsy of the iliac area was performed, confirming the diagnosis of Langerhans Cell Histiocytosis (LCH).
Fig. 1.
X-ray of the left hip: A lucency at the medial aspect of the left femoral head (white dotted circle).
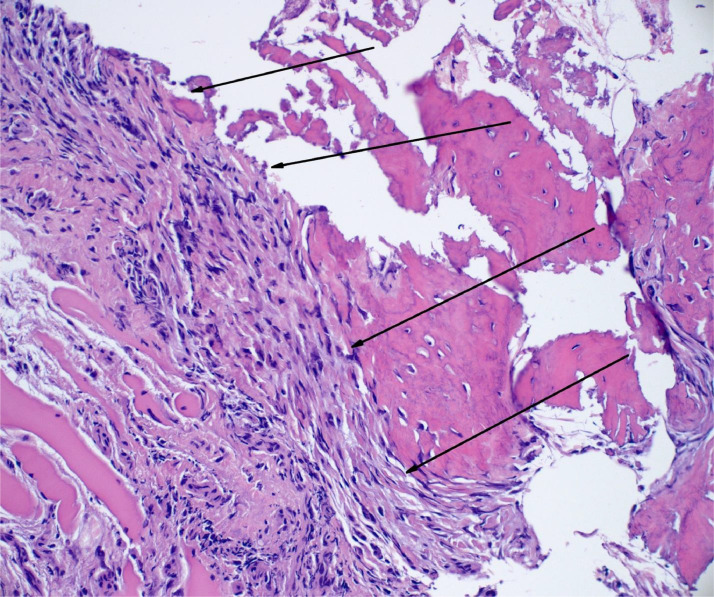
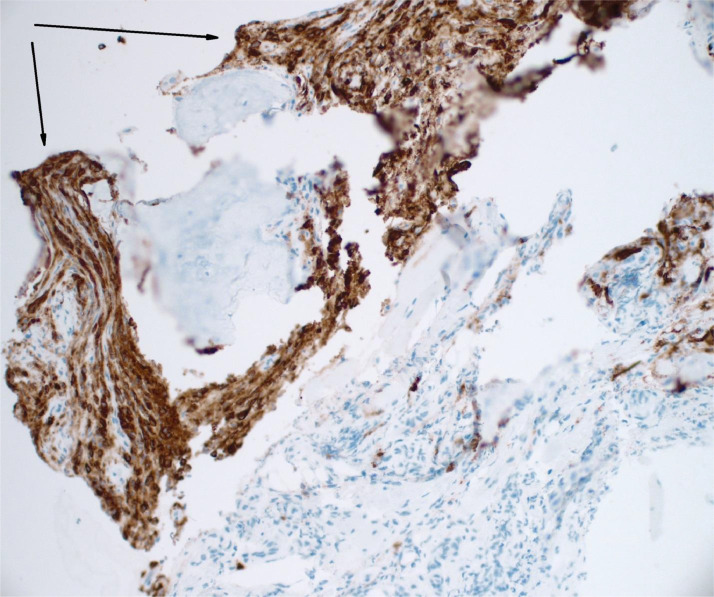
The colonoscopy revealed superficial ulcerations in the terminal ileum. Biopsies from these ulcerations confirmed LCH involvement in the ileal mucosa and submucosa (Figs. 5 and 6). Additional immunohistochemical stains, including CD1a, BRAF, BCL1, and S100, were consistent with LCH.
Fig. 5.
Langerhans histiocytosis (arrows) focally surrounding reactive bone fragment - the Langerhans cells are oval and somewhat crushed with abundant amphophilic cytoplasm. The characteristic nuclear groves are difficult to appreciate in this preparation. H&E stain 200X.
Fig. 6.
Langerin immunohistochemical analysis highlights Langerhans histiocytosis (brown color and arrows) focally surrounding a fragment of reactive bone. Langerin Immunohistochemistry. 200X.
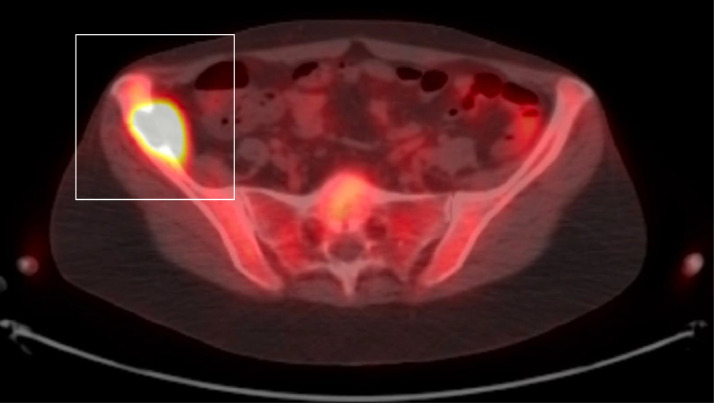
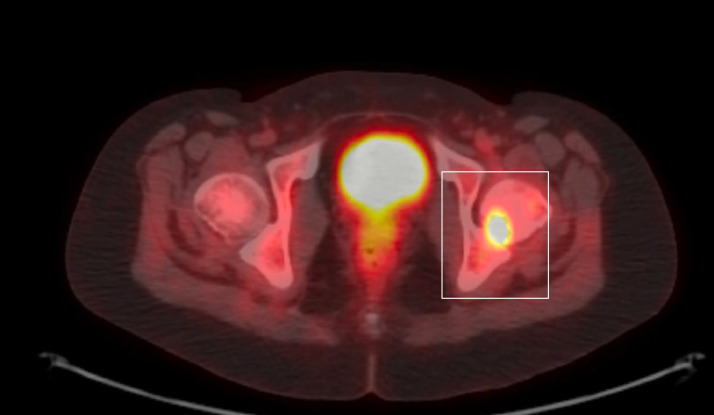
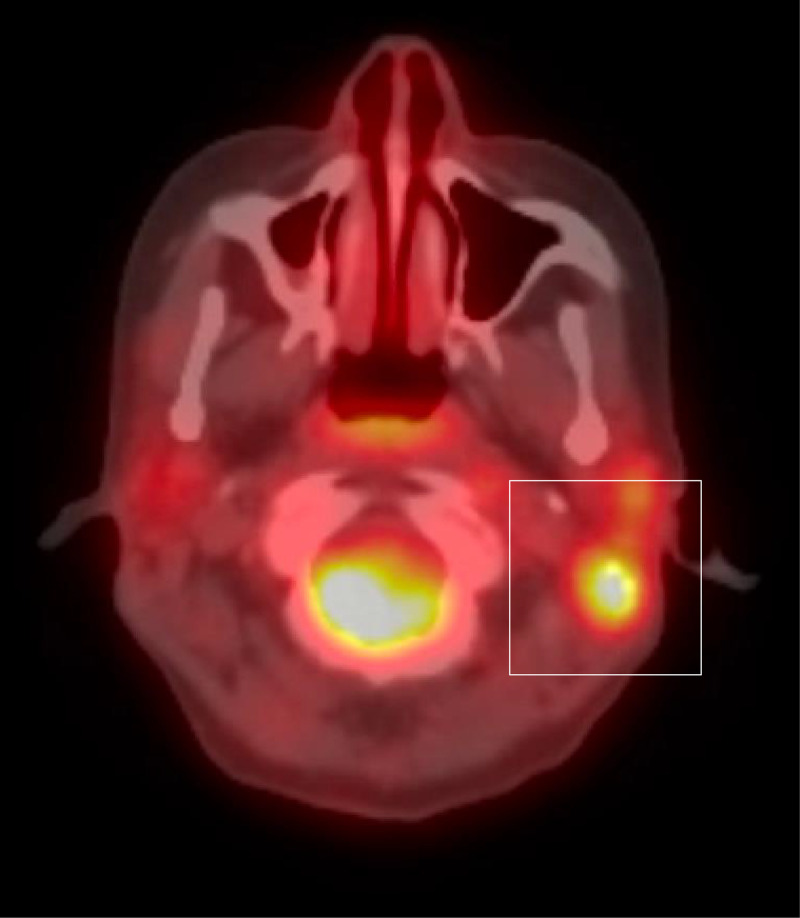
A PET CT scan was also conducted, revealing extensive disease involvement, including the left parietal calvarium, pelvis, and left femoral head, as well as bilateral mastoid air cells and bilateral jugular chain lymph nodes (Fig. 2, Fig. 3, Fig. 4). Given the mastoid involvement and her symptoms of intermittent dizziness and ear fullness, there was concern for potential CNS disease. The treatment plan was formulated to include IV cytarabine, due to the risk of CNS involvement, and IV iron dextran for her microcytic anemia.
Fig. 2.
PET CT shows an expansile lytic lesion in the right iliac wing measuring 2.9 × 3.5 cm with a maximum SUV of 12.3.
Fig. 3.
A lytic lesion in the posterior left femoral head measures 1.7 × 1.3 cm and demonstrates a maximum SUV of 8.5.
Fig. 4.
A lytic lesion in the left mastoid air cells measures maximum SUV of 10.7.
This case was further reviewed at a renowned medical institution, confirming the diagnosis of LCH. The patient's complex and multisystemic case was discussed in a multidisciplinary tumor board to formulate a comprehensive treatment plan.
Discussion
Thrombocytopenia with Absent Radius (TAR) Syndrome is a rare congenital disorder characterized by the absence of the radius bone in the forearm and a significantly reduced platelet count [9,10]. The exact etiology of TAR syndrome remains unknown, but it is believed to have a genetic component, with most cases showing autosomal recessive inheritance [2,9,11]. The diagnosis of TAR syndrome is primarily clinical, based on the characteristic physical findings of bilateral radial aplasia and thrombocytopenia [11]. Management involves addressing the hematological and orthopedic aspects. Platelet transfusions and, in some cases, splenectomy are used to manage thrombocytopenia [9,10]. Orthopedic interventions, including surgical correction and physical therapy, are employed to improve limb function and quality of life [2,11].
The value of intubating the terminal ileum during a colonoscopy cannot be overstated, especially in complex cases with unexplained symptoms [12]. In our patient, this procedure revealed superficial ulcerations that were crucial for diagnosing Langerhans Cell Histiocytosis (LCH), emphasizing the importance of a comprehensive colonoscopic examination.
LCH is a rare myeloid neoplastic disorder characterized by the clonal proliferation of modified dendritic cells with a specific Langerhans cell phenotype [6]. These cells can accumulate in various tissues or organs and are often accompanied by an eosinophil-rich inflammatory background [6,13]. The diagnosis is confirmed through histopathologic examination, which in our patient revealed characteristic neoplastic Langerhans cells with pale eosinophilic cytoplasm and distinctive coffee bean-shaped or cleaved nuclei. Immunohistochemical evidence further supported the diagnosis, with neoplastic cells expressing CD1a, Langerin, and S100.
LCH disease has a broad clinical spectrum, affecting various organs and systems [4]. It can manifest as a single-system or multisystem disease, with bone being the most commonly affected site [14]. In our patient, the involvement was multisystemic, affecting the gastrointestinal tract and bone, among other sites. This case adds to the limited literature on LCH in adults, as the disease is more commonly studied in children [3,8,15].
Treatment of LCH often involves chemotherapy, and in our patient, IV cytarabine was chosen. Cytarabine, also known as Ara-C, is a chemotherapy agent commonly used for acute myeloid leukemia and non-Hodgkin lymphoma [16]. It works by inhibiting DNA synthesis, making it effective against rapidly dividing myeloid cells, which are central to Langerhans Cell Histiocytosis (LCH)[16]. While the drug can cause side effects like myelosuppression and gastrointestinal issues, its potential to penetrate the central nervous system makes it a suitable choice for this case [16]. The patient's mastoid involvement and symptoms like intermittent dizziness suggest possible CNS disease, further supporting the use of cytarabine as a targeted treatment option. The patient was also treated with IV iron dextran for microcytic anemia, given her poor tolerance of oral iron.
Conclusion
This case report presents a unique and complex clinical scenario involving a young adult female with a history of Thrombocytopenia-Absent Radius (TAR) syndrome, who presented with fatigue, hip pain, lymphadenopathy, and gastrointestinal symptoms. The case underscores the diagnostic utility of intubating the terminal ileum during colonoscopy, which led to the identification of superficial ulcerations and subsequent diagnosis of Langerhans Cell Histiocytosis (LCH). The multi-system involvement, including the gastrointestinal tract and osseous lesions, adds another layer of complexity to the case. The use of cytarabine as a treatment option, given its effectiveness against myeloid cells and its ability to penetrate the CNS, highlights the need for a multidisciplinary approach to manage such complex cases.
The case serves as an educational cornerstone for several key points: the importance of thorough diagnostic procedures, including terminal ileum intubation during colonoscopy; the need for a comprehensive approach to pathology to confirm the diagnosis of rare conditions like LCH; and the consideration of tailored treatment options based on the patient's unique presentation and symptoms. It also emphasizes the need for further research and clinical understanding of the natural history of LCH in adults, as most existing literature focuses on pediatric cases. Overall, this case adds valuable insights into the diagnosis and management of LCH in the context of multisystem involvement and coexisting medical conditions.
Patient consent
We confirm that we have obtained written, informed consent from the patient for the publication of this case report. The patient has been thoroughly informed about the details that will be published, and understands the implications of the publication. The written consent is stored securely and is available for review by the editorial team upon request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Giordano P, Cecinati V, Grassi M, Giordani L, De Mattia D, Santoro N. Langerhans cell histiocytosis in a pediatric patient with thrombocytopenia-absent radius syndrome and 1q21.1 deletion: case report and proposal of a rapid molecular diagnosis of 1q21.1 deletion. Immunopharmacol Immunotoxicol. 2011;33(4):754–758. doi: 10.3109/08923973.2011.557077. [DOI] [PubMed] [Google Scholar]
- 2.Cowan J, Parikh T, Waghela R, Mora R. Thrombocytopenia with absent radii (TAR) syndrome without significant thrombocytopenia. Cureus. 2020;12(9):e10557. doi: 10.7759/cureus.10557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abla O, Rollins B, Ladisch S. Langerhans cell histiocytosis: progress and controversies. Br J Haematol. 2019;187(5):559–562. doi: 10.1111/bjh.16099. [DOI] [PubMed] [Google Scholar]
- 4.Bagnasco F, Zimmermann SY, Egeler RM, Nanduri VR, Cammarata B, Donadieu J, et al. Langerhans cell histiocytosis and associated malignancies: A retrospective analysis of 270 patients. Eur J Cancer. 2022;172:138–145. doi: 10.1016/j.ejca.2022.03.036. [DOI] [PubMed] [Google Scholar]
- 5.Gulati N, Allen CE. Langerhans cell histiocytosis: version 2021. Hematol Oncol. 2021;39(Suppl 1):15–23. doi: 10.1002/hon.2857. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Javadi T, Hill C, McLemore ML, Oskouei S, Bahrami A. Adult-onset Langerhans cell histiocytosis of bone: a case series highlighting a rare entity. Ann Diagn Pathol. 2023;66 doi: 10.1016/j.anndiagpath.2023.152171. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez-Galindo C, Allen CE. Langerhans cell histiocytosis. Blood. 2020;135(16):1319–1331. doi: 10.1182/blood.2019000934. [DOI] [PubMed] [Google Scholar]
- 8.Tillotson CV, Anjum F, Patel BC. Langerhans Cell Histiocytosis. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430885. [PubMed]
- 9.Strauss G, Mott K, Klopocki E, Schulze H. Thrombocytopenia absent radius (TAR)-syndrome: from current genetics to patient self-empowerment. Hamostaseologie. 2023;43(4):252–260. doi: 10.1055/a-2088-1801. [DOI] [PubMed] [Google Scholar]
- 10.Petit F, Boussion S, et al. In: GeneReviews(®). University of washington, seattle copyright © 1993-2023. Adam MP, Mirzaa GM, Pagon RA, et al., editors. university of washington; seattle: 1993. Thrombocytopenia Absent Radius Syndrome. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved. [Google Scholar]
- 11.Monteiro C, Gonçalves A, Oliveira J, Salvado R, Tomaz J, Morais S, et al. Thrombocytopenia-Absent Radius Syndrome: Descriptions of Three New Cases and a Novel Splicing Variant in RBM8A That Expands the Spectrum of Null Alleles. Int J Mol Sci. 2022;23(17):9621. doi: 10.3390/ijms23179621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alkhatib AA, Kumar S. Clinical yield of ileal intubation during screening colonoscopy. Cureus. 2022;14(1):e20870. doi: 10.7759/cureus.20870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kobayashi M, Tojo A. Langerhans cell histiocytosis in adults: advances in pathophysiology and treatment. Cancer Sci. 2018;109(12):3707–3713. doi: 10.1111/cas.13817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goyal G, Tazi A, Go RS, Rech KL, Picarsic JL, Vassallo R, et al. International expert consensus recommendations for the diagnosis and treatment of Langerhans cell histiocytosis in adults. Blood. 2022;139(17):2601–2621. doi: 10.1182/blood.2021014343. [DOI] [PubMed] [Google Scholar]
- 15.Leung AKC, Lam JM, Leong KF. Childhood Langerhans cell histiocytosis: a disease with many faces. World J Pediatr. 2019;15(6):536–545. doi: 10.1007/s12519-019-00304-9. [DOI] [PubMed] [Google Scholar]
- 16.Cao XX, Li J, Zhao AL, He TH, Gao XM, Cai HC, et al. Methotrexate and cytarabine for adult patients with newly diagnosed Langerhans cell histiocytosis: A single arm, single center, prospective phase 2 study. Am J Hematol. 2020;95(9):E235–E238. doi: 10.1002/ajh.25864. [DOI] [PubMed] [Google Scholar]