Abstract
Diabetes Mellitus is one of the biggest health problems in Indonesia but the research on the disease’s projection is still limited. This study aimed to make a projection model of prevalence and mortality of diabetes in Indonesia based on risk factors and NCD programs. The study was a quantitative non-experimental study through multiple linear regression models and system dynamics. The baseline projection was created by 2018 data and projections until 2045 involved the dynamization of risk factors and programs, population, and case fatality rate. The model was created from 205 districts data. This study used secondary data from Basic Health Research, BPJS Kesehatan, NCD programs, and Ministry of Health. The prevalence of diabetes in Indonesia is estimated to increase from 9.19% in 2020 (18.69 million cases) to 16.09% in 2045 (40.7 million cases). The prevalence will be lower to 15.68% (39.6 million) if interventions of programs were carried out, and to 9.22% (23.2 million) if the programs were added with prevention of risk factors. The projected number of deaths due to diabetes increases from 433,752 in 2020 to 944,468 in 2045. Deaths due to stroke among diabetes increases from 52,397 to 114,092 in the same period. Deaths from IHD among diabetes increase from 35,351 to 76,974, and deaths from chronic kidney disease among diabetes increase from 29,061 to 63,279. Diabetes prevalence and mortality in Indonesia rise significantly in Indonesia and can be reduced by intervention of several programs and risk factors. This study findings could be source of planning and evaluation of Diabetes prevention and control program at national and provincial level in the future related to risk factors control and program development.
Keywords: Diabetes, Projection, Prevalence, Mortality
Subject terms: Diseases, Endocrinology, Health care, Medical research, Risk factors
Introduction
The burden of Diabetes, one of main Non-Communicable Diseases (NCD), in term of prevalence and mortality becomes a serious problem in the word as well as in Indonesia. The prevalence rate of the disease was 5943 per 100.000 population in 2019 worldwide, which rose from 2968 per 100,000 in 1990. Meanwhile, the mortality rate was 20.5 per 100,000 population which increased from 12.37 per 100,000 in 19901. In Indonesia, the prevalence was 5.7% among adults in 2007 became 6.9% in 2013 and 8.5% in 20182–4.
There was common risk factors related to Diabetes such as obesity, smoking, unhealthy diet, lack of physical activity, hypertension, raised in blood glucose, and increase of cholesterol5–7. Similarly, study of Peters et al.8 revealed that unhealthy diet, lack of physical activity, smoking, hypertension, and obesity. The study of Kristianita described that there was a significant relationship between fruit and vegetable consumption, physical activity, and the incidence of type 2 Diabetes. Moreover, the study of Zhang et al.9 stated that overweight, obesity, high triglyceride, and hypertension are risk factors for Diabetes in men and women.
Diabetes becomes part of main disease prevention and control program in Indonesia that is included in the National Medium-Term Development Plan 2020–202410, Strategic Plan of the Ministry of Health 2020–202411, and indicators in the Minimum Service Standards for district government12. Thus, there are several NCD programs developed nationally namely NCD integrated post (Posbindu), NCD integrated Service in Primary Health Center (Pandu), as well as the Chronic Disease Service (Prolanis) program7. Furthermore, there are also screening program including obesity, central obesity, and program of Diabetes standard services in the minimum service standards (SPM) as obligation of district government12. The program might influence the development of diabetes, but information of the influence was still limited.
In order to develop adequate prevention and control programs of diabetes, projection of the diseases, especially morbidity and mortality is needed. Projection of Diabetes prevalence may be developed using risk factors and prevention and control programs. The research of Meng et al.13 included risk factors used for diabetes projection, namely body mass index, smoking, alcohol consumption, physical activity, and meat, fish, and vegetable consumption. Meanwhile, the research of Nai-Arun and Moungmai, used smoking, alcohol consumption, family history of diabetes, family history of hypertension, weight, BMI, blood pressure, age, and sex as predictors of14.
Projection of the prevalence and mortality of diabetes mellitus is still limited in Indonesia. One of the Diabetes burden study in Indonesia was conducted in 1993, which showed that the Diabetes treatment burden in Indonesia reached IDR 1.5 billion per day or IDR 500 billion a year15. Another study was a projection till 2024 by Nurhayati16 that by 2020 the prevalence of Diabetes in Indonesia was 8.71% which rose from 8.13% in 2017 and becomes 9.49% in 2024. This study was a literature review based on Institute of Health Metric and Evaluation (IHME) data. Compared to the existing data, the prevalence of 2017 was lower than 2018 national data (8.5%)4.
Diabetes burden projection research has been conducted in various countries. Research by Tan et al.17 in Singapore on the projection of Diabetes complications in 2050 in the form of acute myocardial infarction is estimated to increase from 9300 in 2019 to 16,400 in 2050. The number of strokes increased from 7300 to 12,800, and the number of end-stage kidney disease from 1700 to 270017. Research by Rowley, et al. (2017) on Diabetes projections in the United States through 2030 shows that Diabetes prevalence increases by 54% or more than 54.9 million population between 2015 and 2030, with Diabetes—related deaths increasing 38% to 385,800 people per year18. Another Diabetes projection study by Boyle et al.19 in the United States shows that the incidence of DM is expected to increase from 8 cases per 1000 in 2008 to 15 by 2050.
Besides influence of the risk factors, influence of prevention and control program to diabetes is not known clearly. The projection is needed to estimate the burden and develop anticipated prevention and control program. The previous projection of diabetes in Indonesia used regression based on risk relative of the risk factors only. Thus, we conducted the study to develop projection of diabetes prevalence and mortality based on risk factors and NCD prevention and control programs in Indonesia. The projection of diabetes using modeling of risk factors and NCD control programs in this manuscript is the first method in Indonesia.
Methods
Study design
The study used a quantitative non-experimental study design through developing projection models with multiple linear regression and system dynamics. The model was based on risk factors and Diabetes prevention and control programs, as well as population size, Diabetes risk factor growth, Diabetes prevention and control program growth, case fatality rate, and population projection. This study used secondary data from Basic Health Research 2007, 2013, 2018, National Health Insurance Body (BPJS) 2016–2020, Directorate of P2PTM Ministry of Health 2016–2020, Center for Data and Information the Ministry of Health (2019–2021), and the Central Bureau of Statistics. Wes use district level as analysis unit. This study used risk factors and program of Diabetes to project the morbidity and mortality of Diabetes which was a new method of analysis in projection of the disease in Indonesia. The previous study in Indonesia used only risk factors and existing cases to project the disease.
Study approval
The study was approved by Universitas Indonesia and the authors confirmed that all methods were performed in accordance with the relevant guidelines and regulations in Universitas Indonesia.
Dependent variable
The dependent variables were diabetes morbidity and mortality. Morbidity means prevalence of diabetes, which was defined as percentage of adult respondent (15 years and above) who had diabetes based on medical doctor diagnosis which was adjusted by the prevalence of diabetes based on blood glucose measurement (8.5%). The mortality was number of deaths due to diabetes, number of death due to stroke among diabetes cases, deaths due to ischemic health disease among diabetes cases, and deaths due to chronic kidney disease among diabetes cases.
Independent variables
There were 10 risk factors and 8 NCD prevention and control programs included in the projection model. The risk factors consisted of prevalence of overweight, obesity, central obesity, sweet food consumption, sugary beverage consumption, fatty food consumption, lack of fruit and vegetable consumption, lack of physical activity, smoking, and hypertension. Meanwhile, the prevention and control programs included Posbindu, village running Posbindu, examination of Posbindu, Pandu, Prolanis, routine checking blood glucose, Minimum standard service (SPM) for Diabetes services and minimum standard services of NCD screening.
Overweight was categorized by body mass index (BMI) for 25–26.9, meanwhile 27 and above for obesity. Central obesity category was waist circumferences 90 cm (males) and 80 and above (females). Sweety food consumption was consumption the food containing excessive sugar/carbohydrate 1 time or more a day and sweety beverage consumption was consumption the drinking water containing excessive sugar 1 time or more a day. Fatty food consumption was consumption excessive fat/fried food 1 or more a day. Lack of fruit and consumption was no consumption of or less than 5 portions of fruit or vegetables a day. Moreover, Lack of physical activity was less 30 min or 150 min moderate physical activity a day. Smoking meant active smoking in the last month. Meanwhile, hypertension was based on blood pressure examination for those who has systole of 140 mmHg or diastole for 90 mmHg.
Posbindu was a community participation on detecting and monitoring NCD risk factors. Village running Posbindu meant village that has active Posbindu. Examination of Posbindu was activity of NCD risk factors detection namely smoking, physical activity, fruit and vegetable consumption, weight and height measurement, blood pressure measurement, and blood measurement. Pandu was an activity of detection of NCD risk factors, detection of NCD cases and standard treatment in primary health centers. Prolanis is a chronic disease management, including diabetes and hypertension, run by primary health center with activities of monthly blood glucose measurement, blood pressure measurement, treatment, physical activity, and counseling.
Coverage of village running Posbindu was percentage of village had Posbindu, coverage of Posbindu examination was percentage of members examined in the Posbindu. Coverage of Pandu is percentage of Primary health center (PHC) developing integrated NCD, coverage of Prolanis was member of Prolanis among people aged 15 years and above. Routine of blood glucose checking was percentage of people who regularly checks blood glucose monthly. Coverage of SPM Diabetes service was percentage of Diabetes patients have standard treatment, and coverage of NCD screening was people aged 15 years and above who have complete screening for NCD risk factors.
Data analysis
Data analysis performed in the study was development of baseline prevalence and mortality projection in 2018 using multiple linear regression and projections till 2045 using system dynamics. Multiple Linear regression was developed through step of bivariate selection, multivariate modelling, and final model development20,21. Bivariate selection was performed by correlation analysis between risk factors and diagnosed Diabetes prevalence, which risk factors that had p value less than 0.25 was inputted into full model20. Based on bivariate analysis, 16 out of 18 predictors were included in the full model. Two risk factors namely sweety food consumption and sweety beverage consumption were excluded.
The multivariate testing used Enter method. Then, the multivariate modelling was performed by excluding variables from full model that had p value more than 0.05. If the variable did not influence R2 and B of other variables for 10%, the variables were kept excluded. The variables excluded from final model were Pandu and lack of fruit and vegetables consumption. So, there were 14 determinants included in the final model. In order to justify the fit of the model, all assumption of multiple linear regression were tested, for existence, independence, linearity, homoscedasticity, normality, and collinearity20,21 After testing, all assumption were complied.
Based on multiple linear regression analysis, there were 9 variables consisting of 4 risk factors and 5 prevention and control programs as predictors of Diabetes prevalence in the final model. With R2 0.571, the model described as Diabetes prevalence = − 1.212 + 0.216 overweight prevalence + 0.017 obesity prevalence + 0.112 central obesity prevalence + 0.019 prevalence of fatty food consumption–0.001 Percentage of villages with PTM Posbindu + 0.003 percentage of Pandu + 1.510 prevalence of routine blood sugar checks−0.012 SPM coverage of DM Diabetes service + 0.008 SPM coverage productive age screening.
In order to make a projection to 2045, we incorporate trend/dynamization of each risk factor and program. Risk factors’ trend based on their trends from 2007 to 2018 based on Basic Health research Data. Trend of the program based on data from 2016 to 2020. Assumption of SPM of Diabetes health services and SPM of productive age screening using random normal based on the average of 3 years (2019–2021) and its standard deviation.
Assumptions of case fatality rate of diabetes and proportion of its complication were based on BPJS data 2016–2020. Case fatality rate of Diabetes was 2.32% for diabetes, proportion of death due to stroke, ischemic heart disease, and chronic kidney disease among Diabetes cases was 12.08%, 8.15%, and 6.7% respectively. Meanwhile, assumption of neuropathy due to diabetes was 53.64%22, retinopathy was 30.7%23, and Diabetes Keto Acidosis (DKA) among diabetes cases was 3,07%24 and its mortality for 72 h was 28.57%25. Projection was made in three scenarios, namely scenario without intervention (scenario 1), scenario with program intervention of village with Posbindu and SPM of Diabetes services each 100% coverage (scenario 2), and scenario with program intervention and halt of the rate of risk factors (overweight, obesity, central obesity, and fatty food consumption) as condition in 2018. The projection results have been declared valid after discussion with experts and have an Absolute Mean Percentage Error (MAPE) of 12% for provincial and national projections and 23% for district/city projections26. For generating maps, Looker Studio software with release date on 20 December 2022 was used in this geographical distribution analysis using results of this study. The software could be accessed at https://lookerstudio.google.com/overview.
Ethics approval and consent to participate
The study was approved by The Research and Community Engagement Ethical Committee Faculty of Public Health Universitas Indonesia No. Ket-438/UN2.F10.D11/PPM.00.02/2022 on June 22nd 2022. The data (aggregate data) used in this study were anonymized before its use. Following The Guideline and Ethical Standard of National Health Research and Development issued by Ethical Board of National Health Research and Development, Ministry of Health (2013), this study did not use informed consent as it used secondary data. The authors had permission to use the data from each secondary data holder, namely Head of Policy and Development Body, Ministry of Health, Director of Non-Communicable Disease Prevention and Control, Ministry of Health, and Director of National Health Insurance (BPJS).
Consent for publication
We, the authors, give our consent for the publication of this paper, which can include detail of tables and figures to be published in Scientific Reports. Data of diabetes prevalence and ant the risk factors 2007 can be accessed at https://labmandat.litbang.kemkes.go.id/adownload/?id=2&lkey=82206a9b1521b38 (closed), 2013 at https://labmandat.litbang.kemkes.go.id/adownload/?id=3&lkey=4c9c023be7c4a12 (closed), and 2018 at https://labmandat.litbang.kemkes.go.id/adownload/?id=4&lkey=8ad2f351fd26042 (closed). Data of Indonesia population can be accessed at https://www.bps.go.id/subject/12/kependudukan.html#subjekViewTab5 (open). Links of diabetes risk factors were granted from Head of Policy and Development Body, Ministry of Health. Data of national NCD programs supplied by Director of Non-Communicable Disease Prevention and Control, Ministry of Health. Data of diabetes mortality was supplied by Director of National Health Insurance (BPJS).
Results
Projection of diabetes prevalence
The prevalence and number of Diabetes cases (total) in Indonesia and in each province is estimated to increase quite high in 2020–2045. Nationally, Diabetes prevalence increased from 9.19% in 2020 (18.69 million cases) to 16.09% in 2045 (40.7 million cases). It rose 75.1% over 25 years, with an average increase of 3% from prevalence per year. The provinces with the highest prevalence in 2045 are Jakarta (23.11%) and the lowest East Nusatenggara province (8.91%) (Fig. 1a, Table 1). Based on seven regions, Java-Bali region had the highest average of Diabetes prevalence (18.27%) and the lowest was Nusatenggara region (10.87%) (Fig. 1b). The most cases in 2045 are in West Java Province (7,170,569 cases) and the lowest in North Kalimantan Province (138,038 cases) (Fig. 1c, Table 2). The microvascular complication of diabetes, namely neuropathy and retinopathy were also projected to rise from 2020 to 2045. Neuropathy increased from 10,028,638 cases to 21,836,747 cases and retinopathy rose from 5,739,732 cases to 12,497,915. The highest cases of 2045 were in West Java province with 3,846,293 cases and 2,201,365 and the lowest was in North Kalimantan Province with 74,044 cases and 42,378 cases for neuropathy and retinopathy, respectively (Tables 3 and 4).
Figure 1.
Projection of Morbidity of Diabetes in Indonesia 2045.
Table 1.
Projection of DIABETES PREVALENCE IN Indonesia, 2020–2045, by province.
| No | Province | Diabetes prevalence projection (%) | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 8.31 | 9.87 | 11.45 | 13.14 | 14.74 | 16.39 |
| 2 | North Sumatera | 8.84 | 10.34 | 11.72 | 13.17 | 14.76 | 15.83 |
| 3 | West Sumatera | 8.42 | 9.99 | 11.53 | 13.35 | 14.94 | 16.55 |
| 4 | Riau | 8.58 | 10.40 | 12.26 | 14.08 | 15.81 | 17.70 |
| 5 | Jambi | 6.77 | 8.09 | 9.51 | 10.83 | 12.43 | 14.28 |
| 6 | South Sumatera | 7.35 | 9.15 | 11.01 | 12.90 | 14.92 | 16.83 |
| 7 | Bengkulu | 7.17 | 8.64 | 9.68 | 10.98 | 12.47 | 14.49 |
| 8 | Lampung | 6.63 | 8.10 | 9.61 | 11.05 | 12.64 | 13.86 |
| 9 | Bangka Belitung Island | 9.66 | 11.07 | 12.69 | 14.23 | 15.52 | 17.16 |
| 10 | Riau Island | 9.54 | 10.91 | 12.29 | 13.73 | 15.15 | 16.47 |
| 11 | Jakarta | 14.30 | 16.09 | 18.12 | 19.60 | 21.40 | 23.11 |
| 12 | West Java | 9.42 | 10.56 | 11.62 | 12.78 | 13.90 | 14.95 |
| 13 | Central Java | 8.99 | 10.44 | 11.73 | 13.23 | 14.50 | 15.86 |
| 14 | Yogyakarta | 12.60 | 14.31 | 16.08 | 17.84 | 19.99 | 21.94 |
| 15 | East Java | 10.07 | 11.55 | 12.86 | 14.08 | 15.51 | 17.01 |
| 16 | Banten | 9.66 | 10.58 | 12.22 | 13.18 | 14.43 | 15.56 |
| 17 | Bali | 10.31 | 12.25 | 13.93 | 15.87 | 17.31 | 19.43 |
| 18 | West Nusa Tenggara | 6.58 | 7.41 | 8.97 | 10.06 | 11.64 | 12.84 |
| 19 | East Nusa Tenggara | 3.89 | 5.10 | 6.10 | 6.90 | 8.09 | 8.91 |
| 20 | West Kalimantan | 7.28 | 8.76 | 9.76 | 11.39 | 13.16 | 14.48 |
| 21 | Central Kalimantan | 7.43 | 8.50 | 9.65 | 10.89 | 12.01 | 12.97 |
| 22 | South Kalimantan | 8.89 | 10.27 | 11.52 | 12.88 | 14.23 | 15.42 |
| 23 | East Kalimantan | 12.36 | 13.70 | 15.23 | 17.01 | 18.58 | 20.25 |
| 24 | North Kalimantan | 14.33 | 14.83 | 15.64 | 16.18 | 16.53 | 17.29 |
| 25 | North Sulawesi | 10.61 | 11.76 | 12.82 | 13.46 | 14.85 | 15.84 |
| 26 | Central Sulawesi | 9.12 | 10.30 | 10.99 | 12.18 | 13.31 | 14.72 |
| 27 | South Sulawesi | 8.62 | 10.64 | 12.25 | 14.37 | 16.07 | 17.99 |
| 28 | Southeast Sulawesi | 8.22 | 9.59 | 10.99 | 12.65 | 14.20 | 15.68 |
| 29 | Gorontalo | 10.62 | 12.26 | 12.85 | 14.57 | 15.88 | 17.03 |
| 30 | West Sulawesi | 7.47 | 9.41 | 11.24 | 13.27 | 15.25 | 17.13 |
| 31 | Maluku | 7.89 | 9.33 | 10.90 | 12.41 | 13.97 | 15.55 |
| 32 | North Maluku | 8.84 | 9.33 | 10.97 | 12.12 | 12.87 | 14.28 |
| 33 | West Papua | 8.89 | 9.83 | 10.99 | 12.30 | 12.98 | 14.28 |
| 34 | Papua | 7.71 | 8.37 | 9.08 | 9.97 | 10.87 | 11.19 |
| Indonesia | 9.19 | 10.61 | 11.89 | 13.37 | 14.79 | 16.09 | |
Table 2.
Projection of diabetes cases in Indonesia, 2020–2045, by province.
| No | Province | Number of diabetes cases projection | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 321,498 | 416,124 | 519,639 | 635,349 | 751,360 | 873,750 |
| 2 | North Sumatera | 943,618 | 1,187,416 | 1,432,263 | 1,688,543 | 1,965,634 | 2,171,341 |
| 3 | West Sumatera | 337,347 | 430,949 | 532,139 | 652,695 | 765,778 | 881,138 |
| 4 | Riau | 422,944 | 577,337 | 749,983 | 930,448 | 1,115,769 | 1,323,481 |
| 5 | Jambi | 182,506 | 232,864 | 288,936 | 343,965 | 408,111 | 480,378 |
| 6 | South Sumatera | 462,350 | 617,245 | 789,789 | 977,323 | 1,181,214 | 1,379,270 |
| 7 | Bengkulu | 107,272 | 138,246 | 163,836 | 195,098 | 229,731 | 274,375 |
| 8 | Lampung | 423,440 | 549,083 | 684,452 | 817,592 | 960,440 | 1,072,210 |
| 9 | Bangka Belitung | 106,364 | 131,390 | 160,724 | 190,355 | 217,009 | 248,833 |
| 10 | Riau Island | 162,291 | 218,131 | 283,507 | 362,349 | 453,336 | 555,171 |
| 11 | Jakarta | 1,170,540 | 1,363,348 | 1,578,110 | 1,746,904 | 1,932,776 | 2,093,705 |
| 12 | West Java | 3,526,676 | 4,247,308 | 4,953,851 | 5,708,318 | 6,456,651 | 7,170,569 |
| 13 | Central Java | 2,425,092 | 2,935,055 | 3,397,962 | 3,902,698 | 4,320,404 | 4,745,282 |
| 14 | Yogyakarta | 393,501 | 476,903 | 568,148 | 667,693 | 791,184 | 916,821 |
| 15 | East Java | 3,184,025 | 3,768,696 | 4,285,593 | 4,769,819 | 5,287,282 | 5,784,386 |
| 16 | Banten | 928,816 | 1,107,764 | 1,375,654 | 1,578,329 | 1,816,134 | 2,039,772 |
| 17 | Bali | 355,352 | 454,496 | 547,063 | 655,054 | 745,547 | 868,706 |
| 18 | West Nusa Tenggara | 250,425 | 306,043 | 399,144 | 478,727 | 584,753 | 673,995 |
| 19 | East Nusa Tenggara | 150,977 | 213,758 | 274,306 | 331,772 | 411,342 | 474,199 |
| 20 | West Kalimantan | 275,238 | 356,041 | 421,828 | 517,757 | 623,131 | 707,526 |
| 21 | Central Kalimantan | 149,556 | 185,747 | 225,840 | 269,995 | 311,710 | 348,806 |
| 22 | South Kalimantan | 279,663 | 348,269 | 418,653 | 494,369 | 569,880 | 639,636 |
| 23 | East Kalimantan | 342,169 | 408,152 | 482,296 | 565,851 | 642,241 | 721,296 |
| 24 | North Kalimantan | 74,716 | 86,172 | 100,094 | 112,312 | 123,511 | 138,038 |
| 25 | North Sulawesi | 204,505 | 237,340 | 268,411 | 289,644 | 324,898 | 349,627 |
| 26 | Central Sulawesi | 206,043 | 250,766 | 286,394 | 336,462 | 386,178 | 445,155 |
| 27 | South Sulawesi | 580,477 | 753,698 | 906,079 | 1,098,762 | 1,257,503 | 1,430,337 |
| 28 | Southeast Sulawesi | 158,586 | 202,326 | 250,555 | 309,283 | 369,209 | 429,852 |
| 29 | Gorontalo | 94,747 | 115,651 | 126,838 | 148,940 | 166,522 | 181,961 |
| 30 | West Sulawesi | 73,876 | 101,234 | 130,401 | 164,058 | 198,693 | 232,765 |
| 31 | Maluku | 101,568 | 128,630 | 159,333 | 190,583 | 223,357 | 257,124 |
| 32 | North Maluku | 79,931 | 91,795 | 116,083 | 136,318 | 152,464 | 177,012 |
| 33 | West Papua | 62,882 | 79,741 | 100,719 | 125,626 | 146,392 | 176,556 |
| 34 | Papua | 190,147 | 224,240 | 260,512 | 302,616 | 344,685 | 367,506 |
| Indonesia | 18,696,194 | 22,990,010 | 27,138,625 | 31,855,207 | 36,449,447 | 40,709,820 | |
Table 3.
Projection of neuropathy due to diabetes in Indonesia, 2020–2045, by province.
| No | Province | Number of diabetes cases projection | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 172,452 | 223,209 | 278,735 | 340,801 | 403,029 | 468,679 |
| 2 | North Sumatera | 506,157 | 636,930 | 768,266 | 905,735 | 1,054,366 | 1,164,707 |
| 3 | West Sumatera | 180,953 | 231,161 | 285,439 | 350,106 | 410,763 | 472,642 |
| 4 | Riau | 226,867 | 309,684 | 402,291 | 499,092 | 598,498 | 709,915 |
| 5 | Jambi | 97,896 | 124,908 | 154,985 | 184,503 | 218,911 | 257,675 |
| 6 | South Sumatera | 248,005 | 331,090 | 423,643 | 524,236 | 633,603 | 739,840 |
| 7 | Bengkulu | 57,541 | 74,155 | 87,882 | 104,651 | 123,227 | 147,175 |
| 8 | Lampung | 227,133 | 294,528 | 367,140 | 438,556 | 515,180 | 575,134 |
| 9 | Bangka Belitung | 57,054 | 70,478 | 86,212 | 102,106 | 116,404 | 133,474 |
| 10 | Riau Island | 87,053 | 117,005 | 152,073 | 194,364 | 243,170 | 297,794 |
| 11 | Jakarta | 627,877 | 731,300 | 846,498 | 937,039 | 1,036,741 | 1,123,063 |
| 12 | West Java | 1,891,709 | 2,278,256 | 2,657,246 | 3,061,942 | 3,463,348 | 3,846,293 |
| 13 | Central Java | 1,300,819 | 1,574,364 | 1,822,667 | 2,093,407 | 2,317,465 | 2,545,369 |
| 14 | Yogyakarta | 211,074 | 255,811 | 304,754 | 358,151 | 424,391 | 491,783 |
| 15 | East Java | 1,707,911 | 2,021,528 | 2,298,792 | 2,558,531 | 2,836,098 | 3,102,745 |
| 16 | Banten | 498,217 | 594,205 | 737,901 | 846,616 | 974,174 | 1,094,134 |
| 17 | Bali | 190,611 | 243,791 | 293,444 | 351,371 | 399,912 | 465,974 |
| 18 | West Nusa Tenggara | 134,328 | 164,161 | 214,101 | 256,789 | 313,662 | 361,531 |
| 19 | East Nusa Tenggara | 80,984 | 114,660 | 147,138 | 177,963 | 220,644 | 254,360 |
| 20 | West Kalimantan | 147,637 | 190,980 | 226,268 | 277,725 | 334,247 | 379,517 |
| 21 | Central Kalimantan | 80,222 | 99,635 | 121,140 | 144,825 | 167,201 | 187,099 |
| 22 | South Kalimantan | 150,011 | 186,811 | 224,565 | 265,180 | 305,684 | 343,101 |
| 23 | East Kalimantan | 183,540 | 218,933 | 258,704 | 303,522 | 344,498 | 386,903 |
| 24 | North Kalimantan | 40,077 | 46,223 | 53,690 | 60,244 | 66,251 | 74,044 |
| 25 | North Sulawesi | 109,696 | 127,309 | 143,976 | 155,365 | 174,275 | 187,540 |
| 26 | Central Sulawesi | 110,522 | 134,511 | 153,622 | 180,478 | 207,146 | 238,781 |
| 27 | South Sulawesi | 311,368 | 404,283 | 486,021 | 589,376 | 674,525 | 767,233 |
| 28 | Southeast Sulawesi | 85,066 | 108,528 | 134,398 | 165,900 | 198,044 | 230,572 |
| 29 | Gorontalo | 50,822 | 62,035 | 68,036 | 79,891 | 89,322 | 97,604 |
| 30 | West Sulawesi | 39,627 | 54,302 | 69,947 | 88,001 | 106,579 | 124,855 |
| 31 | Maluku | 54,481 | 68,997 | 85,466 | 102,228 | 119,809 | 137,921 |
| 32 | North Maluku | 42,875 | 49,239 | 62,267 | 73,121 | 81,782 | 94,949 |
| 33 | West Papua | 33,730 | 42,773 | 54,026 | 67,386 | 78,525 | 94,705 |
| 34 | Papua | 101,995 | 120,282 | 139,738 | 162,323 | 184,889 | 197,130 |
| Indonesia | 10,028,638 | 12,331,842 | 14,557,158 | 17,087,133 | 19,551,483 | 21,836,747 | |
Table 4.
Projection of retinopathy due to diabetes in Indonesia, 2020–2045, by province.
| No | Province | Number of diabetes cases projection | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 98,700 | 127,750 | 159,529 | 195,052 | 230,667 | 268,241 |
| 2 | North Sumatera | 289,691 | 364,537 | 439,705 | 518,383 | 603,450 | 666,602 |
| 3 | West Sumatera | 103,566 | 132,301 | 163,367 | 200,377 | 235,094 | 270,509 |
| 4 | Riau | 129,844 | 177,243 | 230,245 | 285,648 | 342,541 | 406,309 |
| 5 | Jambi | 56,029 | 71,489 | 88,703 | 105,597 | 125,290 | 147,476 |
| 6 | South Sumatera | 141,942 | 189,494 | 242,465 | 300,038 | 362,633 | 423,436 |
| 7 | Bengkulu | 32,932 | 42,442 | 50,298 | 59,895 | 70,527 | 84,233 |
| 8 | Lampung | 129,996 | 168,569 | 210,127 | 251,001 | 294,855 | 329,169 |
| 9 | Bangka Belitung | 32,654 | 40,337 | 49,342 | 58,439 | 66,622 | 76,392 |
| 10 | Riau Island | 49,823 | 66,966 | 87,037 | 111,241 | 139,174 | 170,437 |
| 11 | Jakarta | 359,356 | 418,548 | 484,480 | 536,299 | 593,362 | 642,767 |
| 12 | West Java | 1,082,690 | 1,303,923 | 1,520,832 | 1,752,454 | 1,982,192 | 2,201,365 |
| 13 | Central Java | 744,503 | 901,062 | 1,043,174 | 1,198,128 | 1,326,364 | 1,456,802 |
| 14 | Yogyakarta | 120,805 | 146,409 | 174,421 | 204,982 | 242,893 | 281,464 |
| 15 | East Java | 977,496 | 1,156,990 | 1,315,677 | 1,464,335 | 1,623,196 | 1,775,807 |
| 16 | Banten | 285,147 | 340,084 | 422,326 | 484,547 | 557,553 | 626,210 |
| 17 | Bali | 109,093 | 139,530 | 167,948 | 201,101 | 228,883 | 266,693 |
| 18 | West Nusa Tenggara | 76,880 | 93,955 | 122,537 | 146,969 | 179,519 | 206,916 |
| 19 | East Nusa Tenggara | 46,350 | 65,624 | 84,212 | 101,854 | 126,282 | 145,579 |
| 20 | West Kalimantan | 84,498 | 109,304 | 129,501 | 158,951 | 191,301 | 217,210 |
| 21 | Central Kalimantan | 45,914 | 57,024 | 69,333 | 82,888 | 95,695 | 107,083 |
| 22 | South Kalimantan | 85,856 | 106,919 | 128,526 | 151,771 | 174,953 | 196,368 |
| 23 | East Kalimantan | 105,046 | 125,303 | 148,065 | 173,716 | 197,168 | 221,438 |
| 24 | North Kalimantan | 22,938 | 26,455 | 30,729 | 34,480 | 37,918 | 42,378 |
| 25 | North Sulawesi | 62,783 | 72,863 | 82,402 | 88,921 | 99,744 | 107,335 |
| 26 | Central Sulawesi | 63,255 | 76,985 | 87,923 | 103,294 | 118,557 | 136,663 |
| 27 | South Sulawesi | 178,206 | 231,385 | 278,166 | 337,320 | 386,054 | 439,113 |
| 28 | Southeast Sulawesi | 48,686 | 62,114 | 76,920 | 94,950 | 113,347 | 131,964 |
| 29 | Gorontalo | 29,087 | 35,505 | 38,939 | 45,725 | 51,122 | 55,862 |
| 30 | West Sulawesi | 22,680 | 31,079 | 40,033 | 50,366 | 60,999 | 71,459 |
| 31 | Maluku | 31,182 | 39,490 | 48,915 | 58,509 | 68,571 | 78,937 |
| 32 | North Maluku | 24,539 | 28,181 | 35,637 | 41,850 | 46,807 | 54,343 |
| 33 | West Papua | 19,305 | 24,481 | 30,921 | 38,567 | 44,942 | 54,203 |
| 34 | Papua | 58,375 | 68,842 | 79,977 | 92,903 | 105,818 | 112,824 |
| Indonesia | 5,739,732 | 7,057,933 | 8,331,558 | 9,779,549 | 11,189,980 | 12,497,915 | |
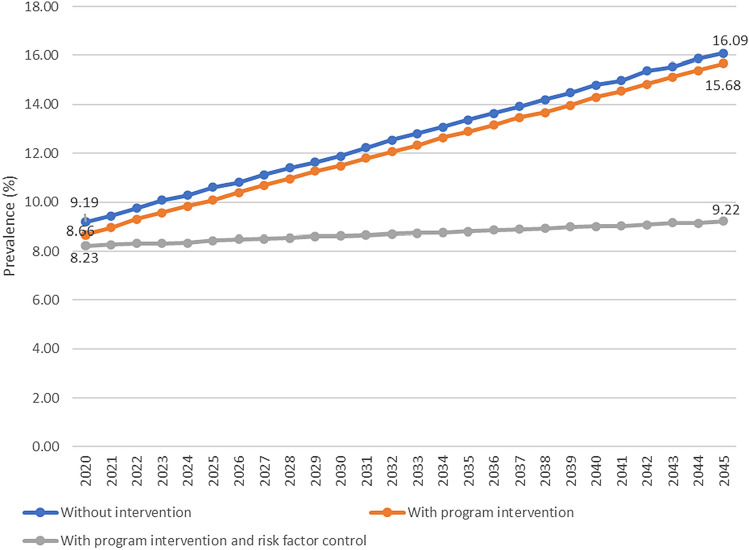
In Fig. 2, it is known that the prevalence of Diabetes is projected at 16.09% in 2045 without intervention and will be lower to 15.68%, or reduced by 5.54%, if the intervention is carried out to increase the coverage of villages with Posbindu and SPM of Diabetes services to 100%. The prevalence will be even lower to 9.22% or reduced by 42.69% if the program intervention is added by preventing the rise of the risk factors (overweight, obesity, central obesity, and consumption of fatty foods).
Figure 2.
Projection of diabetes prevalence in Indonesia in three scenarios, 2020–2045.
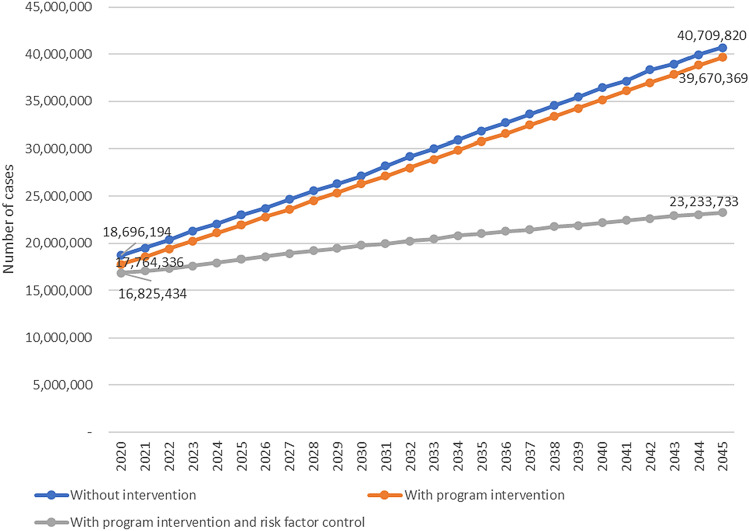
The cases of Diabetes in 2045 is estimated at 40.7 million without intervention. If with the intervention of increasing the program of village with Posbindu and SPM of Diabetes services, the cases are reduced to 39.6 million cases. The cases are even lower if the program is added to halt the increase of risk factors (overweight, obesity, central obesity, consumption of fatty foods), then cases become 23.2 million (Fig. 3).
Figure 3.
Projection of diabetes cases in Indonesia in three scenarios, 2020–2045.
Projection of mortality due to diabetes
The number of deaths due to Diabetes in Indonesia and each province is estimated to increase quite high in 2020–2045. Nationally, the number of deaths due to Diabetes increased from 433,752 in 2020 to 944,468 in 2045 (Fig. 4, Table 5). Stroke deaths among Diabetes cases increased from 52,397 in 2020 to 114,092 in 2045. Deaths from IHD among Diabetes cases increased from 35,351 in 2020 to 76,974 in 2045. Meanwhile, deaths from chronic kidney disease among Diabetes cases rose from 29,061 in 2020 to 63,279 in 2045. Additionally, deaths due to Diabetic Ketoacidosis (DKA) among Diabetes cases rose from 162,382 to 353,576. The number of deaths from Diabetes and its complications increased by 117% over 25 years or an average of 4.7% per year (Tables 6, 7, 8 and 9).
Figure 4.
Projection of number of deaths due to diabetes in Indonesia, 2045.
Table 5.
Projection of deaths due to diabetes in Indonesia, 2020–2045.
| No | Province | Projection of number of deaths due to diabetes | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 7459 | 9654 | 12,056 | 14,740 | 17,432 | 20,271 |
| 2 | North Sumatera | 21,892 | 27,548 | 33,228 | 39,174 | 45,603 | 50,375 |
| 3 | West Sumatera | 7826 | 9998 | 12,346 | 15,143 | 17,766 | 20,442 |
| 4 | Riau | 9812 | 13,394 | 17,400 | 21,586 | 25,886 | 30,705 |
| 5 | Jambi | 4234 | 5402 | 6703 | 7980 | 9468 | 11,145 |
| 6 | South Sumatera | 10,727 | 14,320 | 18,323 | 22,674 | 27,404 | 31,999 |
| 7 | Bengkulu | 2489 | 3207 | 3801 | 4526 | 5330 | 6365 |
| 8 | Lampung | 9824 | 12,739 | 15,879 | 18,968 | 22,282 | 24,875 |
| 9 | Bangka Belitung | 2468 | 3048 | 3729 | 4416 | 5035 | 5773 |
| 10 | Riau Island | 3765 | 5061 | 6577 | 8406 | 10,517 | 12,880 |
| 11 | Jakarta | 27,157 | 31,630 | 36,612 | 40,528 | 44,840 | 48,574 |
| 12 | West Java | 81,819 | 98,538 | 114,929 | 132,433 | 149,794 | 166,357 |
| 13 | Central Java | 56,262 | 68,093 | 78,833 | 90,543 | 100,233 | 110,091 |
| 14 | Yogyakarta | 9,129 | 11,064 | 13,181 | 15,490 | 18,355 | 21,270 |
| 15 | East Java | 73,869 | 87,434 | 99,426 | 110,660 | 122,665 | 134,198 |
| 16 | Banten | 21,549 | 25,700 | 31,915 | 36,617 | 42,134 | 47,323 |
| 17 | Bali | 8244 | 10,544 | 12,692 | 15,197 | 17,297 | 20,154 |
| 18 | West Nusa Tenggara | 5810 | 7100 | 9260 | 11,106 | 13,566 | 15,637 |
| 19 | East Nusa Tenggara | 3503 | 4959 | 6364 | 7697 | 9543 | 11,001 |
| 20 | West Kalimantan | 6386 | 8260 | 9786 | 12,012 | 14,457 | 16,415 |
| 21 | Central Kalimantan | 3470 | 4309 | 5239 | 6264 | 7232 | 8092 |
| 22 | South Kalimantan | 6488 | 8080 | 9713 | 11,469 | 13,221 | 14,840 |
| 23 | East Kalimantan | 7938 | 9469 | 11,189 | 13,128 | 14,900 | 16,734 |
| 24 | North Kalimantan | 1733 | 1999 | 2322 | 2606 | 2865 | 3202 |
| 25 | North Sulawesi | 4745 | 5506 | 6227 | 6720 | 7538 | 8111 |
| 26 | Central Sulawesi | 4780 | 5818 | 6644 | 7806 | 8959 | 10,328 |
| 27 | South Sulawesi | 13,467 | 17,486 | 21,021 | 25,491 | 29,174 | 33,184 |
| 28 | Southeast Sulawesi | 3679 | 4694 | 5813 | 7175 | 8566 | 9973 |
| 29 | Gorontalo | 2198 | 2683 | 2943 | 3455 | 3863 | 4221 |
| 30 | West Sulawesi | 1714 | 2349 | 3025 | 3806 | 4610 | 5400 |
| 31 | Maluku | 2356 | 2984 | 3697 | 4422 | 5182 | 5965 |
| 32 | North Maluku | 1854 | 2130 | 2693 | 3163 | 3537 | 4107 |
| 33 | West Papua | 1459 | 1850 | 2337 | 2915 | 3396 | 4096 |
| 34 | Papua | 4411 | 5202 | 6044 | 7021 | 7997 | 8526 |
| Indonesia | 433,752 | 533,368 | 629,616 | 739,041 | 845,627 | 944,468 | |
Table 6.
Projection of deaths due to stroke among Diabetes cases in Indonesia, 2020–2045.
| No | Province | Projection of number of deaths | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 901 | 1166 | 1456 | 1781 | 2106 | 2449 |
| 2 | North Sumatera | 2645 | 3328 | 4014 | 4732 | 5509 | 6085 |
| 3 | West Sumatera | 945 | 1208 | 1491 | 1829 | 2146 | 2469 |
| 4 | Riau | 1185 | 1618 | 2102 | 2608 | 3127 | 3709 |
| 5 | Jambi | 511 | 653 | 810 | 964 | 1144 | 1346 |
| 6 | South Sumatera | 1296 | 1730 | 2213 | 2739 | 3310 | 3865 |
| 7 | Bengkulu | 301 | 387 | 459 | 547 | 644 | 769 |
| 8 | Lampung | 1187 | 1539 | 1918 | 2291 | 2692 | 3005 |
| 9 | Bangka Belitung | 298 | 368 | 450 | 533 | 608 | 697 |
| 10 | Riau Island | 455 | 611 | 795 | 1016 | 1271 | 1556 |
| 11 | Jakarta | 3281 | 3821 | 4423 | 4896 | 5417 | 5868 |
| 12 | West Java | 9884 | 11,903 | 13,883 | 15,998 | 18,095 | 20,096 |
| 13 | Central Java | 6796 | 8226 | 9523 | 10,938 | 12,108 | 13,299 |
| 14 | Yogyakarta | 1103 | 1337 | 1592 | 1871 | 2217 | 2569 |
| 15 | East Java | 8923 | 10,562 | 12,011 | 13,368 | 14,818 | 16,211 |
| 16 | Banten | 2603 | 3,105 | 3855 | 4423 | 5090 | 5717 |
| 17 | Bali | 996 | 1,274 | 1533 | 1836 | 2089 | 2435 |
| 18 | West Nusa Tenggara | 702 | 858 | 1119 | 1342 | 1639 | 1889 |
| 19 | East Nusa Tenggara | 423 | 599 | 769 | 930 | 1153 | 1329 |
| 20 | West Kalimantan | 771 | 998 | 1182 | 1451 | 1746 | 1983 |
| 21 | Central Kalimantan | 419 | 521 | 633 | 757 | 874 | 978 |
| 22 | South Kalimantan | 784 | 976 | 1173 | 1385 | 1597 | 1793 |
| 23 | East Kalimantan | 959 | 1144 | 1352 | 1586 | 1800 | 2021 |
| 24 | North Kalimantan | 209 | 242 | 281 | 315 | 346 | 387 |
| 25 | North Sulawesi | 573 | 665 | 752 | 812 | 911 | 980 |
| 26 | Central Sulawesi | 577 | 703 | 803 | 943 | 1082 | 1248 |
| 27 | South Sulawesi | 1627 | 2112 | 2539 | 3079 | 3524 | 4009 |
| 28 | Southeast Sulawesi | 444 | 567 | 702 | 867 | 1035 | 1205 |
| 29 | Gorontalo | 266 | 324 | 355 | 417 | 467 | 510 |
| 30 | West Sulawesi | 207 | 284 | 365 | 460 | 557 | 652 |
| 31 | Maluku | 285 | 360 | 447 | 534 | 626 | 721 |
| 32 | North Maluku | 224 | 257 | 325 | 382 | 427 | 496 |
| 33 | West Papua | 176 | 223 | 282 | 352 | 410 | 495 |
| 34 | Papua | 533 | 628 | 730 | 848 | 966 | 1030 |
| Indonesia | 52,397 | 64,431 | 76,058 | 89,276 | 102,152 | 114,092 | |
Table 7.
Projection of deaths due to ischemic heart disease among diabetes cases in Indonesia, 2020–2045.
| No | Province | Projection of number of deaths | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 608 | 787 | 983 | 1201 | 1421 | 1652 |
| 2 | North Sumatera | 1784 | 2245 | 2708 | 3193 | 3717 | 4106 |
| 3 | West Sumatera | 638 | 815 | 1006 | 1234 | 1448 | 1666 |
| 4 | Riau | 800 | 1,092 | 1418 | 1759 | 2110 | 2502 |
| 5 | Jambi | 345 | 440 | 546 | 650 | 772 | 908 |
| 6 | South Sumatera | 874 | 1,167 | 1493 | 1848 | 2233 | 2608 |
| 7 | Bengkulu | 203 | 261 | 310 | 369 | 434 | 519 |
| 8 | Lampung | 801 | 1,038 | 1294 | 1546 | 1816 | 2027 |
| 9 | Bangka Belitung Island | 201 | 248 | 304 | 360 | 410 | 470 |
| 10 | Riau Island | 307 | 412 | 536 | 685 | 857 | 1050 |
| 11 | Jakarta | 2213 | 2578 | 2984 | 3303 | 3654 | 3959 |
| 12 | West Java | 6668 | 8031 | 9367 | 10,793 | 12,208 | 13,558 |
| 13 | Central Java | 4585 | 5550 | 6425 | 7379 | 8169 | 8972 |
| 14 | Yogyakarta | 744 | 902 | 1074 | 1262 | 1496 | 1734 |
| 15 | East Java | 6020 | 7126 | 8103 | 9019 | 9997 | 10,937 |
| 16 | Banten | 1756 | 2095 | 2601 | 2984 | 3434 | 3857 |
| 17 | Bali | 672 | 859 | 1034 | 1239 | 1410 | 1643 |
| 18 | West Nusa Tenggara | 474 | 579 | 755 | 905 | 1106 | 1274 |
| 19 | East Nusa Tenggara | 285 | 404 | 519 | 627 | 778 | 897 |
| 20 | West Kalimantan | 520 | 673 | 798 | 979 | 1178 | 1338 |
| 21 | Central Kalimantan | 283 | 351 | 427 | 511 | 589 | 660 |
| 22 | South Kalimantan | 529 | 659 | 792 | 935 | 1078 | 1209 |
| 23 | East Kalimantan | 647 | 772 | 912 | 1070 | 1214 | 1364 |
| 24 | North Kalimantan | 141 | 163 | 189 | 212 | 234 | 261 |
| 25 | North Sulawesi | 387 | 449 | 508 | 548 | 614 | 661 |
| 26 | Central Sulawesi | 390 | 474 | 542 | 636 | 730 | 842 |
| 27 | South Sulawesi | 1098 | 1425 | 1713 | 2078 | 2378 | 2704 |
| 28 | Southeast Sulawesi | 300 | 383 | 474 | 585 | 698 | 813 |
| 29 | Gorontalo | 179 | 219 | 240 | 282 | 315 | 344 |
| 30 | West Sulawesi | 140 | 191 | 247 | 310 | 376 | 440 |
| 31 | Maluku | 192 | 243 | 301 | 360 | 422 | 486 |
| 32 | North Maluku | 151 | 174 | 219 | 258 | 288 | 335 |
| 33 | West Papua | 119 | 151 | 190 | 238 | 277 | 334 |
| 34 | Papua | 360 | 424 | 493 | 572 | 652 | 695 |
| Indonesia | 35,351 | 43,470 | 51,314 | 60,232 | 68,919 | 76,974 | |
Table 8.
Projection of deaths due to chronic kidney disease among diabetes cases in Indonesia, 2020–2045.
| No | Province | Projection of number of deaths | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 500 | 647 | 808 | 988 | 1168 | 1358 |
| 2 | North Sumatera | 1467 | 1846 | 2226 | 2625 | 3055 | 3375 |
| 3 | West Sumatera | 524 | 670 | 827 | 1015 | 1190 | 1370 |
| 4 | Riau | 657 | 897 | 1166 | 1446 | 1734 | 2057 |
| 5 | Jambi | 284 | 362 | 449 | 535 | 634 | 747 |
| 6 | South Sumatera | 719 | 959 | 1228 | 1519 | 1836 | 2144 |
| 7 | Bengkulu | 167 | 215 | 255 | 303 | 357 | 426 |
| 8 | Lampung | 658 | 853 | 1064 | 1271 | 1493 | 1667 |
| 9 | Bangka Belitung Island | 165 | 204 | 250 | 296 | 337 | 387 |
| 10 | Riau Island | 252 | 339 | 441 | 563 | 705 | 863 |
| 11 | Jakarta | 1819 | 2119 | 2453 | 2715 | 3004 | 3254 |
| 12 | West Java | 5482 | 6602 | 7700 | 8873 | 10,036 | 11,146 |
| 13 | Central Java | 3770 | 4562 | 5282 | 6066 | 6716 | 7376 |
| 14 | Yogyakarta | 612 | 741 | 883 | 1038 | 1230 | 1425 |
| 15 | East Java | 4949 | 5858 | 6662 | 7414 | 8219 | 8991 |
| 16 | Banten | 1444 | 1722 | 2138 | 2453 | 2823 | 3171 |
| 17 | Bali | 552 | 706 | 850 | 1018 | 1159 | 1350 |
| 18 | West Nusa Tenggara | 389 | 476 | 620 | 744 | 909 | 1048 |
| 19 | East Nusa Tenggara | 235 | 332 | 426 | 516 | 639 | 737 |
| 20 | West Kalimantan | 428 | 553 | 656 | 805 | 969 | 1100 |
| 21 | Central Kalimantan | 232 | 289 | 351 | 420 | 485 | 542 |
| 22 | South Kalimantan | 435 | 541 | 651 | 768 | 886 | 994 |
| 23 | East Kalimantan | 532 | 634 | 750 | 880 | 998 | 1121 |
| 24 | North Kalimantan | 116 | 134 | 156 | 175 | 192 | 215 |
| 25 | North Sulawesi | 318 | 369 | 417 | 450 | 505 | 543 |
| 26 | Central Sulawesi | 320 | 390 | 445 | 523 | 600 | 692 |
| 27 | South Sulawesi | 902 | 1172 | 1408 | 1708 | 1955 | 2223 |
| 28 | Southeast Sulawesi | 247 | 314 | 389 | 481 | 574 | 668 |
| 29 | Gorontalo | 147 | 180 | 197 | 232 | 259 | 283 |
| 30 | West Sulawesi | 115 | 157 | 203 | 255 | 309 | 362 |
| 31 | Maluku | 158 | 200 | 248 | 296 | 347 | 400 |
| 32 | North Maluku | 124 | 143 | 180 | 212 | 237 | 275 |
| 33 | West Papua | 98 | 124 | 157 | 195 | 228 | 274 |
| 34 | Papua | 296 | 349 | 405 | 470 | 536 | 571 |
| Indonesia | 29,061 | 35,736 | 42,184 | 49,516 | 56,657 | 63,279 | |
Table 9.
Projection of deaths due to diabetic ketoacidosis among diabetes cases in Indonesia, 2020–2045.
| No | Province | Projection of number of deaths | |||||
|---|---|---|---|---|---|---|---|
| 2020 | 2025 | 2030 | 2035 | 2040 | 2045 | ||
| 1 | Aceh | 2792 | 3614 | 4513 | 5518 | 6526 | 7589 |
| 2 | North Sumatera | 8196 | 10,313 | 12,440 | 14,665 | 17,072 | 18,859 |
| 3 | West Sumatera | 2930 | 3743 | 4622 | 5669 | 6651 | 7653 |
| 4 | Riau | 3673 | 5014 | 6514 | 8081 | 9691 | 11,495 |
| 5 | Jambi | 1585 | 2022 | 2509 | 2987 | 3545 | 4172 |
| 6 | South Sumatera | 4016 | 5361 | 6860 | 8488 | 10,259 | 11,979 |
| 7 | Bengkulu | 932 | 1201 | 1423 | 1694 | 1995 | 2383 |
| 8 | Lampung | 3678 | 4769 | 5945 | 7101 | 8342 | 9312 |
| 9 | Bangka Belitung Island | 924 | 1141 | 1396 | 1653 | 1885 | 2161 |
| 10 | Riau Island | 1410 | 1895 | 2462 | 3147 | 3937 | 4822 |
| 11 | Jakarta | 10,166 | 11,841 | 13,706 | 15,172 | 16,787 | 18,184 |
| 12 | West Java | 30,630 | 36,889 | 43,026 | 49,578 | 56,078 | 62,278 |
| 13 | Central Java | 21,063 | 25,492 | 29,512 | 33,896 | 37,524 | 41,214 |
| 14 | Yogyakarta | 3418 | 4142 | 4935 | 5799 | 6872 | 7963 |
| 15 | East Java | 27,654 | 32,732 | 37,222 | 41,427 | 45,922 | 50,239 |
| 16 | Banten | 8067 | 9621 | 11,948 | 13,708 | 15,774 | 17,716 |
| 17 | Bali | 3086 | 3947 | 4751 | 5689 | 6475 | 7545 |
| 18 | West Nusa Tenggara | 2175 | 2658 | 3467 | 4158 | 5079 | 5854 |
| 19 | East Nusa Tenggara | 1311 | 1857 | 2382 | 2882 | 3573 | 4119 |
| 20 | West Kalimantan | 2391 | 3092 | 3664 | 4497 | 5412 | 6145 |
| 21 | Central Kalimantan | 1299 | 1613 | 1961 | 2345 | 2707 | 3029 |
| 22 | South Kalimantan | 2429 | 3025 | 3636 | 4294 | 4950 | 5555 |
| 23 | East Kalimantan | 2972 | 3545 | 4,189 | 4915 | 5578 | 6265 |
| 24 | North Kalimantan | 649 | 748 | 869 | 975 | 1073 | 1199 |
| 25 | North Sulawesi | 1776 | 2061 | 2331 | 2516 | 2822 | 3037 |
| 26 | Central Sulawesi | 1790 | 2178 | 2487 | 2922 | 3354 | 3866 |
| 27 | South Sulawesi | 5042 | 6546 | 7870 | 9543 | 10,922 | 12,423 |
| 28 | Southeast Sulawesi | 1377 | 1757 | 2176 | 2686 | 3207 | 3733 |
| 29 | Gorontalo | 823 | 1004 | 1102 | 1294 | 1446 | 1580 |
| 30 | West Sulawesi | 642 | 879 | 1133 | 1425 | 1726 | 2022 |
| 31 | Maluku | 882 | 1117 | 1384 | 1655 | 1940 | 2233 |
| 32 | North Maluku | 694 | 797 | 1008 | 1184 | 1324 | 1537 |
| 33 | West Papua | 546 | 693 | 875 | 1091 | 1271 | 1533 |
| 34 | Papua | 1651 | 1948 | 2263 | 2628 | 2994 | 3192 |
| Indonesia | 162,382 | 199,675 | 235,707 | 276,671 | 316,574 | 353,576 | |
At the provincial level, deaths due to Diabetes and its three complications in 2045 are highest in West Java province with 166,357 deaths due to Diabetes, 3,202 deaths from stroke among Diabetes, 13,558 deaths from IHD among Diabetes, and 11,146 deaths from CKD among Diabetes. The lowest mortality was in North Kalimantan province with 3,202 deaths due to Diabetes, 387 deaths from stroke among Diabetes, 261 deaths from IHD among Diabetes, and 215 deaths from CKD among Diabetes Tables 6, 7, 8 and 9).
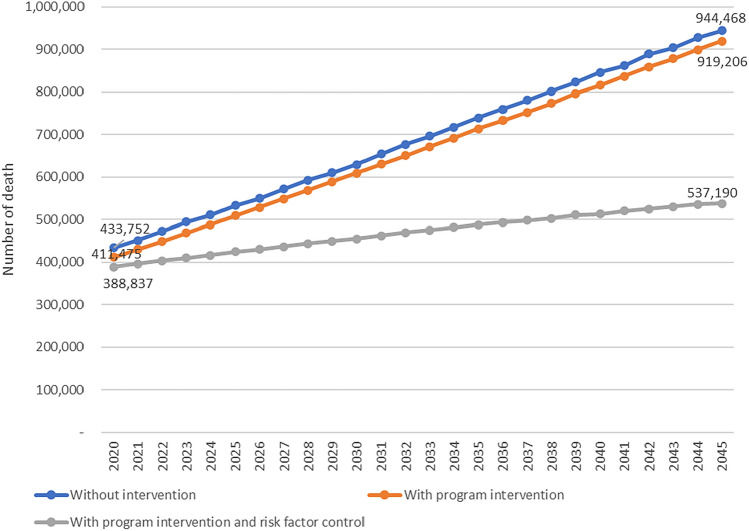
Figure 5 shows that the number of deaths due to Diabetes in 2045 is estimated at 944,468 if without intervention and lower to 919,206 (reduced by 2.67%) if program improvement interventions are carried out and to 537,190 (reduced by 43.12%) if program improvement is added with controlling of the risk factors increase.
Figure 5.
Projection of deaths due to diabetes in three scenarios in Indonesia, 2020–2045.
Discussion
The result of the study shows that the prevalence of Diabetes in Indonesia increased from 9.19% in 2020 (18.69 million cases) to 16.09% in 2045 (40.7 million cases) or an increase of 75.1% over 25 years, or an average of 3% per year. The province with the highest prevalence in 2045 is Jakarta (23.11%) and the lowest is East Nusa Tenggara province (8.91%). The largest number of cases in 2045 is in West Java Province (7,170,569 cases) and the lowest is in North Kalimantan Province (138,038 cases). The results of this study indicate a large increase in the prevalence and number of Diabetes cases in Indonesia, if adequate prevention and control of the NCDs risk factors programs are not carried out. Jakarta Province is an urban area which have higher Diabetes risk factors so that the prevalence is the highest. NTT Province is a rural province with a lower risk of Diabetes, so the prevalence is the lowest. The size of cases corresponds to the magnitude of the prevalence and the number of adult populations. The number of Diabetes cases is according to the prevalence and number of people aged 15 years and over, so provinces with large populations tend to have a larger number of Diabetes cases. West Java Province is the largest province in Indonesia so that the number of cases is the largest, while North Kalimantan province is the province with the smallest population so that the number of Diabetes cases is also the lowest.
The increase in the prevalence of Diabetes in Indonesia is almost the same as the results of other studies. In Indonesia, Nuryati’s research in 201227 shows that the prevalence diabetes among adults in Indonesia 8.04%. This study was a cross sectional study using secondary data from Basic Health Research 2007 with respondents above 18 years using oral glucose tolerance test. Nuryati’s study used the same as this study from Basic Health Research but with different period (2007 and 2018 data) so the prevalence was quite same. But, the projection from this study is higher that projection of Nurhayati16 that by 2020 the prevalence was 8.71% in Indonesia and 9.49% in 2024. Nurhayati’s study used a literature review based on Institute of Health Metric and Evaluation (IHME) data which was based on relative risk modelling using regression analysis. This projection is different from this study which used not only risk factors but also Diabetes programs. It indicates that the programs influence the burden of diabetes in Indonesia.
In Thailand, Mahikul et al.28 reported that Diabetes prevalence is predicted to increase from 6.5% in 2015 to 10.69% in 2035 or an increase of 64.4% over 20 years or 3.2% per year. According to data from the Institute of Health Metric and Evaluation, the prevalence of Diabetes in Indonesia in 2019 is estimated at 3.98% of the entire population or 10.33 million cases1. In China, research of Pan et al.29 in a systematic review 1987–2007 reported that the prevalence of Diabetes in China in 2009 was 3.9% (urban 5.2%, rural 2.9%) and is predicted to increase to 5.4% (urban 6.9%, rural 3.8%) in 2016, or an increase of 38.4% over 7 years or an annual increase of 4.6%. Meanwhile, the number of Diabetes cases is projected to increase from 53.1 million cases in 2009 to 76.1 million cases in 2016. In Sweden, Andersson et al.30 reported that the prevalence of Diabetes increased from 5.8% in 2007 to 6.8% in 2013 (2013) and will rise to 10.4% in 2050 or an increase of 79.3% over 1.8% per year. The number of cases is predicted to increase to 940,000 and every 1% increase in annual incidence will result in an increase of 12.6% prevalence and 1,136 000 cases.
In the United States by Boyle et al.19 where if Diabetes mortality is high, then Diabetes prevalence increases from 14% in 2010 to 21% in 2050 (increase of 50% or 1.25% per year) and to 33% in 2050 (increase of 135%) or 3.3% per year) for 40 years if mortality is low. Rowley et al.18 in the US The prevalence of Diabetes will increase by 54% to more than 54.9 million US population between 2015 and 2030. Diabetes—related annual deaths will rise by 38% to 385,800. Another study by Mainous et al.31 in the United States, projections of Diabetes burden based on individual risk prevalence show that the total burden of Diabetes is estimated at 11.5% (25.4 million) in 2011, 13.5% (32.6 million) in 2021, and 14.5% (37.7 million) in 2031 or an increase of 26% over 20 years with an average increase of 1.3% per year. Wild et al.32 projected that diabetes prevalence is estimated at 2.8% in 2000 and increases to 4.4% by 2030 worldwide, or an increase of 57.1% from the prevalence over 30 years, with an average of 1.9% increase per year. The number of people with diabetes in the world is expected to increase from 171 million cases in 2000 to 366 million cases in 2030.
Based on the scenarios, the results of this study show that the prevalence of Diabetes by 2045 was 16.09% and can be reduced to 15.68%, or reduced by 5.54%, if program intervention namely increase of the coverage of villages with Posbindu and SPM of Diabetes services to 100%. This figure can be lowered again to 9.22% or reduced by 42.69% if the program intervention is added with prevention of risk factors (overweight, obesity, central obesity and consumption of fatty foods). These results show that existing program interventions (Posbindu village and SPM of Diabetes services play a role in reducing the prevalence of Diabetes but not so large. The reduction will be much greater if prevention of the main risk factors for Diabetes are overweight, obesity, central obesity, and consumption of fatty foods.
To reduce Diabetes cases, efforts are needed to control risk factors that positively affect Diabetes projections, namely overweight, obesity, central obesity, and consumption of fatty foods. These control efforts are carried out through increasing education, physical activity, and efforts to change the pattern of consumption of fatty foods into healthy foods (enough fruits and vegetables). Efforts to halt the prevalence rate of these four risk factors can be made through a combination of physical activity and a healthy diet. Intervention targets need to be more specific to at-risk populations. Research by Gregg et al.33 in the United States, shows that by 2030 it is projected that 4.6 million incidences and 3.6 million cases of Diabetes prevalence or reducing the prevalence rate by 14% can be prevented by a combination of prevention strategies. This prevention strategy is developed with structured lifestyle interventions for high-risk (pre-diabetic), moderate-risk, and general populations.
The Ministry of Health of Indonesia needs to make policies and programs to prevent risk factors. The program can be through educational efforts through the Healthy Living Community Movement (GERMAS) and healthy behavior in the community. It is necessary to increase 100% Village with Posbindu. In addition, the achievement of Diabetes health service SPM becomes 100% every year. National Planning Bureau needs to include efforts to control Diabetes risk factors, especially overweight, obesity, central obesity, and unhealthy consumption patterns in health program plans in Indonesia and provide sufficient budget related to Posbindu and Diabetes health service SPM.
The results showed that the projected number of deaths due to Diabetes in Indonesia increased from 433,752 deaths in 2020 to 944,468 in 2045. Stroke deaths in Diabetes increased from 52,397 in 2020 to 114,092 in 2045. Deaths from IHD in Diabetes increased from 35,351 in 2020 to 76,974 in 2045. Meanwhile, deaths from chronic kidney disease in Diabetes increased from 29,061 in 2020 to 63,279 in 2045. The number of deaths from Diabetes and its complications increased by 117% over 25 years or an average of 4.7% per year.
These results indicate that Diabetes is one of the highest causes of death in Indonesia. Based on data from the Institute of Health Metric and Evaluation, deaths from Diabetes in Indonesia in 2019 amounted to 40.98 per 100,000 population or 106,333 deaths. It has the largest increase of all other causes of death for 128.7% from 19901. Meanwhile, based on data from the 2015 Sample Registration System, Diabetes is the third highest cause of death in Indonesia after stroke and ischemic heart disease with a proportion of 7.8%34, an increase from 5.7% in 20072.
In Singapore, research by Tan et al.17 shows that Diabetes complications in 2050 in the form of acute myocardial infarction will increase from 9300 deaths (2019) to 16,400 (2050), the number of stroke increase from 7300 to 12,800, the number of end-stage kidney disease from 1700 to 2700. This number increased by an average of 76.3% over 30 years. In Thailand, Mahikul et al.28 in their study predicted death in undiagnosed Diabetes 10 times greater than undiagnosed Diabetes. The positive screening rate decreased mortality in women aged 15–34 years at 10 years. This indicates the importance of blood sugar screening so that people can be aware of the dangers of diabetes and can make prevention and control efforts independently. Research by Foreman et al.35 shows that deaths from Diabetes in the world amounted to 1,437,000 in 2016 to 2,971,000 in 2040, or an increase of 106.7% over 24 years, with an average increase of 4.4% per year. Deaths from Diabetes -related kidney disease in the world 500,000 in 2016 to 1380 in 2040. Stroke deaths in the world were 5,528,000 in 2016 to 5973 in 2040. The number of ischemic heart disease deaths worldwide was 9,480,000 in 2016 to 10,872,000 in 2040.
Deaths from Diabetes and its complications need to be suppressed with appropriate primary, secondary, and tertiary prevention. Ministry of Health to improve such prevention adequately. On primary prevention to prevent complications in people with diabetes through diet modification and a healthy lifestyle. In secondary prevention, treatment of Diabetes and its complications needs to be provided to all patients using the latest technology. Increased achievement of SPM of Diabetes Health services. In tertiary prevention, rehabilitation for advanced cases such as diabetic foot care needs to be expanded, including home care services.
To reduce the fatality of diabetes due to its complications such as Stroke, Ischemic heart disease, Chronic kidney disease and immediate fatality due to Diabetic Ketoacidosis, interventions of the disease should be enhanced across the regions in Indonesia. Chronic disease management program (Prolanis), number of primary health care facilities providing optimal diabetes services (NCD integrated services), and the participation of healthy life movement (GERMAS) should be strengthened. Meanwhile, achievement of blood glucose targets under Prolanis and the percentage of diabetic patients receiving scheduled screenings and counselling with specialists should be increased.
This study has several limitations in terms of quality and representation of research data. This is due to inconsistent data, missing data, and program coverage data exceeding 100%. For inconsistent data, projections use their mean and standard deviation. For data that exceeds the target of 100%, the data is fulfilled to a maximum of 100%. There are 3.3–34.6% missing data that can reduce data quality in making projections. For these circumstances, the data is filled in using the average province of the district so that the data does not deviate from the actual condition.
Data representation for village with Posbindu, Pandu, and SPM of Diabetes services, and SPM of screening are routine data that is inputted by district government which tends to overestimate, because there is no individual data. However, this data is an official release from the Ministry of Health so it can still be used. The data analyzed in this study is aggregate data at the district level (205 districts/cities out of 514 districts/cities) to estimate the burden of Diabetes at the district, provincial, and national levels. This can cause actual projections to vary more than the results of this study because not all district data are analyzed in the preparation of the model. However, with a provincial MAPE value of 13% that is good at making projections at the provincial level and MAPE at the district / city level, the projection is still quite feasible to estimate conditions in the district/city.
Conclusion
Diabetes morbidity and mortality in Indonesia is projected to rise significantly in Indonesia from 2020 to 2045. The prevalence increases 75.1% over 25 years, with an average of 3% from prevalence per year. The number of deaths from Diabetes and its complications increased by 117% over 25 years or an average of 4.7% per year. Morbidity and mortality can be reduced by intervention of several programs (Village with NCD Post/Posbindu, standard service of diabetes) and risk factors control (overweight, obesity, central obesity, and fatty food consumption). It is recommended to Ministry of Health and health policy makers to use this study result as source of planning and evaluation of diabetes prevention and control program. I need to strengthen the program of risk factor monitoring trough Posbindu, achieve target of minimum standard services of diabetes, and increase healthy lifestyle including physical activity and healthy diet to control overweight and obesity.
Acknowledgements
The authors thank the Head of Policy and Development Body, Ministry of Health, Director of Non-Communicable Disease Prevention and Control, and Director of national Health Insurance (BPJS) who provided data and support this research.
Abbreviations
- DM
Diabetes Mellitus
- MAPE
Absolute Mean Percentage Error
- NCD
Non Communicable Disease
- Pandu
Pelayanan Terpadu (NCD integrated services at Primary Health Center)
- Posbindu
Pos Pembinaan Terpadu (NCD integrated post at community)
- Prolanis
Program pelayanan penyakit kronis (Chronic disease management)
- SPM
Standar Pelayanan Minimal (Minimum Standard Services)
Author contributions
M.W. and A.A. developed the concept and wrote main manuscript. M.W. conducted data acquisition. Data analyze was performed by M.W.B., S.K., and D.K. Data interpretation and result writing were conducted by M.W., A.A.B., S.K., E.R., M.P., S.R., M.N., A.N., and D.K. Discussion writing was performed by M.W., A.A.B., S.K., E.R., M.P., S.R., M.N., and A.N. All authors reviewed and agreed on the final manuscript.
Funding
The research is funded by Universitas Indonesia which is stated in Grant Agreement No NKB-1130/UN2.RST/HKP.05.00/2022.
Data availability
Data of the research is available and can be shared on request to Anhari Achadi at aachadi@gmail.com.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.IHME. Burden of Disease, 2019. Available at https://vizhub.healthdata.org/gbd-compare/ (2020).
- 2.Kemenkes RI. Report on result of national basic health research (Riskesdas) 2007. Available at https://repository.badankebijakan.kemkes.go.id/id/eprint/4386/1/Report%20on%20Result%20of%20National%20Basic%20Health%20Research%202007.pdf (2008).
- 3.Kemenkes RI. Laporan Nasional Riset Kesehatan Dasar (Riskesdas) 2013. Available at https://repository.badankebijakan.kemkes.go.id/id/eprint/4467/1/Laporan_riskesdas_2013_final.pdf (2013).
- 4.Kemenkes RI. Laporan Nasional Riset Kesehatan Dasar (Riskesdas) 2018. Available at https://repository.badankebijakan.kemkes.go.id/id/eprint/3514/1/Laporan%20Riskesdas%202018%20Nasional.pdf (2019).
- 5.WHO . Summary Surveillance of Risk Factors for Noncommunicable Diseases The WHO STEPwise Approach. Geneva; 2001. [Google Scholar]
- 6.Perkeni. Pedoman pengelolaan dan pencegahan diabetes melitus tipe 2 dewasa di Indonesia 2019. Available at https://pbperkeni.or.id/wp-content/uploads/2021/06/Pedoman-Pengelolaan-DM-Tipe-2-Dewasa-di-Indonesia-eBook-PDF.pdf (PB Perkeni, Jakarta, 2019).
- 7.Kemenkes, R. I. Pedoman Umum Pencegahan dan Pengendalian DM Tipe 2 (Jakarta, 2016).
- 8.Peters R, Ee N, Peters J, Beckett N, Booth A, Rockwood K, et al. Common risk factors for major noncommunicable disease, a systematic overview of reviews and commentary: The implied potential for targeted risk reduction. Ther. Adv. Vaccines. 2018;9:259–261. doi: 10.1177/https. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang H, Ni J, Yu C, Wu Y, Li J, Liu J, et al. Sex-based differences in diabetes prevalence and risk factors: A population-based cross-sectional study among low-income adults in China. Front. Endocrinol. (Lausanne) 2019;10:1–8. doi: 10.3389/fendo.2019.00658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Presiden RI . Peraturan Presiden RI Nomor 18 Tahun 2020 Tentang Rencana Pembangunan Jangka Menengah Nasional Tahun 2020 - 2024. Jakarta; 2020. [Google Scholar]
- 11.Kemenkes RI . Peraturan Menteri Kesehatan Republik Indonesia Nomor 21 Tahun 2020 Tentang Rencana Strategis Kementerian Kesehatan Tahun 2020-2024. Jakarta; 2020. [Google Scholar]
- 12.Kemenkes RI . Peraturan Menteri Kesehatan RI Nomor 4 Tahun 2019 tentang Standar Teknis Pemenurhan Mutu Pelayanan Dasar Pada Standar Pelayanan Minimal Bidang Kesehatan. Jakarta; 2019. [Google Scholar]
- 13.Meng XH, Huang YX, Rao DP, Zhang Q, Liu Q. Comparison of three data mining models for predicting diabetes or prediabetes by risk factors. Kaohsiung J. Med. Sci. 2013;29:93–99. doi: 10.1016/j.kjms.2012.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nai-Arun N, Moungmai R. Comparison of classifiers for the risk of diabetes prediction. Procedia Comput. Sci. 2015;69:132–142. doi: 10.1016/j.procs.2015.10.014. [DOI] [Google Scholar]
- 15.Tjokroprawiro A. Diabetes Mellitus di dalam-Masyarakat Indonesia. Bul. Penelit. Kesehat. 1993;1993:21. [Google Scholar]
- 16.Nurhayati, H.-W. Projected number of people with diabetes Indonesia 2017–2024. Available at https://www.statista.com/statistics/1052625/indonesia-diabetes-projection/ (Statista, 2020).
- 17.Tan KW, Dickens BSL, Cook AR. Projected burden of type 2 diabetes mellitus-related complications in Singapore until 2050: A Bayesian evidence synthesis. BMJ Open Diabetes Res. Care. 2020;2020:8. doi: 10.1136/bmjdrc-2019-000928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S. Diabetes 2030: Insights from yesterday, today, and future trends. Popul. Health Manag. 2017;20:6–12. doi: 10.1089/pop.2015.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: Dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul. Health Metr. 2010;8:1–12. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hastono, S. P. Analisis Data. Depok: Fakultas Kesehatan Masyarakat Universitas Indonesia (Depok, 2006).
- 21.Kleinbaum DG, et al. Applied Regression Analysis and Other Multivariable Methods. Duxbury Press; 1998. [Google Scholar]
- 22.Purwata TE. High TNF-alpha plasma levels and macrophages iNOS and TNF-alpha expression as risk factors for painful diabetic neuropathy. J. Pain Res. 2011;4:169–175. doi: 10.2147/JPR.S21751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Halim A, Syumarti S, Rini M, Ratnaningsih N, Iskandar E, Sovani I, et al. Prevalence and associated factors of diabetic retinopathy in people with type 2 diabetes attending community based diabetic retinopathy screening in greater Bandung Indonesia. Int. J. Retin. 2022;5:1. doi: 10.35479/ijretina.2022.vol005.iss001.172. [DOI] [Google Scholar]
- 24.Dewata DGUB, Novida H, Aryati A. Profile of diabetic ketoacidosis patients at regional public hospital Dr. Soetomo in 2017. J. Berk Epidemiol. 2020;8:301. doi: 10.20473/jbe.v8i32020.301-309. [DOI] [Google Scholar]
- 25.Siregar NN, Soewondo P, Subekti I, Muhadi M. Seventy-two hour mortality prediction model in patients with diabetic ketoacidosis: A retrospective cohort study. J. ASEAN Fed. Endocr. Soc. 2018;33:124–129. doi: 10.15605/jafes.033.02.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sterman JD. Business Dinamics: Systems Thinking and Modeling for a Complex World. New York: Irwin McGraw-Hill; 2004. [Google Scholar]
- 27.Nuryati E. Faktor prediksi diabetes melitus tidak terdiagnosis ada usia dewasa di Indonesia Tahun 2011. J. Ilm Kesehat. 2012;2012:1. doi: 10.35952/jik.v1i1.106. [DOI] [Google Scholar]
- 28.Mahikul W, White LJ, Poovorawan K, Soonthornworasiri N, Sukontamarn P, Chanthavilay P, et al. A population dynamic model to assess the diabetes screening and reporting programs and project the burden of undiagnosed diabetes in Thailand. Int. J. Environ. Res. Public Health. 2019;16:1–11. doi: 10.3390/ijerph16122207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pan C, Shang S, Kirch W, Thoenes M. Burden of diabetes in the adult Chinese population: A systematic literature review and future projections. Int. J. Gen. Med. 2010;3:173–179. doi: 10.2147/ijgm.s6343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andersson T, Ahlbom A, Carlsson S. Diabetes prevalence in Sweden at present and projections for year 2050. PLoS One. 2015;10:1–11. doi: 10.1371/journal.pone.0143084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mainous AG, Baker R, Koopman RJ, Saxena S, Diaz VA, Everett CJ, et al. Impact of the population at risk of diabetes on projections of diabetes burden in the United States: An epidemic on the way. Diabetologia. 2007;50:934–940. doi: 10.1007/s00125-006-0528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wild SH, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:2568–2569. doi: 10.2337/diacare.27.10.2568. [DOI] [PubMed] [Google Scholar]
- 33.Gregg EW, Boyle JP, Thompson TJ, Barker LE, Albright AL, Williamson DF. Modeling the impact of prevention policies on future diabetes prevalence in the United States: 2010–2030. Popul. Health Metr. 2013;11:1–9. doi: 10.1186/1478-7954-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kemenkes RI. Indonesia: Sample registration system 2014. Jakarta: Lembaga Penerbitan Balitbangkes; 2015. [Google Scholar]
- 35.Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: Reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet. 2018;392:2052–2090. doi: 10.1016/S0140-6736(18)31694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of the research is available and can be shared on request to Anhari Achadi at aachadi@gmail.com.