Abstract
Aim
The aim of this study was to verify the clinical feasibility of tele‐proctoring using our ultra‐low latency communication system with shared internet access.
Methods
Connections between two multiple remote locations at various distances were established through the TELEPRO® tele‐proctoring system. The server records the latency between the two locations for tele‐proctoring using the annotations. Questionnaires were administered to the surgeons, assistants, and medical staff. Respondents rated the quickness and quality of communication in terms of latency and disturbances in the audio, video, and usefulness of the live telestrations with annotation.
Results
Seven hospitals tele‐proctored with Sapporo Medical University between January 2021 and September 2022. The median latency of annotation between the two locations ranged from 24.5 to 48.5 ms. No major technological problems occurred, such as streaming interruption, loss of video or audio, poor resolution. The video encoding time was 10 ms, and its decoding time was 0.8 ms. The total latency positively correlated with the distance between two locations (R = 0.55, p < 0.01). The quality of communication regarding latency, disturbance, and surgical education with intraoperative annotative instructions showed similar trends, with perfectly fine being the most common response. No significant differences in surgical quality, educational effect, or social impact were observed between the latency ≥30 and <30 ms groups for whether the size of latency affects surgical education.
Conclusion
The feasibility of the tele‐proctoring system is expected to be a sustainable approach to help education for young surgeons and surgical supports in rural areas, thereby reducing disparities in health care.
Keywords: disparities in health care, education, latency, minimally invasive surgery, surgical supports, tele‐proctoring
One‐to‐one tele‐proctoring using shared internet access is clinically applicable and extremely useful. This study is a major step toward the realization and dissemination of tele‐proctoring in surgical education

1. INTRODUCTION
With the advancement of surgical care, the number of issues has also increased both domestically and internationally. One such issue is the chronic shortage of surgeons within Japan. The current educational system has led to a concentration of young physicians in urban areas and a serious decline in the number of young surgeons. For these reasons, there is an overall shortage of surgeons, as well as a significant regional distribution of surgeons, 1 , 2 with the number of surgeons per 100 000 people in rural areas considerably lower than that in urban areas. Regarding medical care for cancer, which is a life‐threatening disease in Japan, the problem of uneven distribution of medical care for surgery, which plays a central role in cancer treatment, must be solved as soon as possible. The survival rate of patients with colorectal cancer, which is currently the most common site‐specific cancer among Japanese, the second most common cause of death among male patients, and the most common cause of death among female patients, is low in regions and countries with inadequate medical services. 3 , 4 In Japan, the number of physicians continues to increase, and the proportion of female physicians also continues to grow. However, internationally, Japan still ranks last in the OECD in the proportion of female physicians, and the number of female surgeons remains low. 5 It is an urgent issue to improve diversity and inclusion in the Japanese medical field. In particular, it takes a great deal of effort and time to master surgical techniques, and it is an important issue to optimize the work‐life balance of young or female surgeons.
There is an urgent need to materialize ICT in healthcare as one of the components of SDGs in Society 5.0. There are many social issues that can be supported by tele medicine, such as the shortage of surgeons, geographical bias in healthcare services, and career support for female or young surgeons.
The realization of tele‐proctoring within tele‐medicine would provide the following benefits 6 , 7 , 8 : (1) correcting the disparity in surgical skills between facilities and promoting the standardization of surgery; (2) increasing the spread of minimally invasive surgery internationally, especially in countries with limited medical industries; (3) reducing long‐distance travel (and the associated time and costs); and (4) career support for female surgeons. The development of a low‐latency communication system using an existing communication infrastructure, shared internet access (SIA), is necessary for the increased adoption of tele‐proctoring; however, SIA exhibits a noticeable latency and is not clinically applicable. 9 Thus, we successfully developed a communication system based on SIA with a latency lower than the maximum allowable latency for tele‐proctoring. 10 Now that the infrastructure for a low‐latency communication system using SIA has been completed, the feasibility of tele‐proctoring between hospitals needs to be verified. Therefore, this study aimed to verify the feasibility of the clinical application of tele‐proctoring using SIA.
2. MATERIALS AND METHODS
We evaluated whether tele‐proctoring using SIA was clinically applicable from the viewpoint of low latency and low disturbance. Objective data were obtained by measuring latency between two locations, and subjective data were obtained by answering a questionnaire about latency and disturbance.
2.1. Participating institutions
Seven hospitals implemented tele‐proctoring with Sapporo Medical University between January 2021 and September 2022 and were included in the study (i.e., Mombetsu General Hospital, Keio University Hospital, Yamanashi University, Red Cross Hospital Osaka, Kyushu University, Nagasaki University, the University of the Ryukyus). Keio University, Yamanashi University, Kyushu University, Nagasaki University, and the University of the Ryukyus were connected to Sapporo Medical University by SINET5 (Science Information NETwork), 11 SINET5 is a non‐commercial science information network designed and operated by the National Institute of Informatics that provides a nationwide 400 Gbps backbone for about 1000 universities and research institutes throughout Japan. Mombetsu General Hospital and Red Cross Hospital Osaka were connected by a commercial internet line (Appendix S1). The line between the doctor's office and the edge switch is a 100 Mbps line, which is the rate‐limiting point. All cases in this study were proctored by an experienced expert in this area who is a board‐certified surgeon in gastroenterology and qualified surgeon of endoscopic surgical skill qualification system, and the proctee at each hospital were gastroenterological surgeons with 8–15 years of experience. All surgeries were laparoscopic colorectal resections, the details of which are described in Table 1.
TABLE 1.
Implemented tele‐proctoring with Sapporo Medical University between January 2021 and September 2022.
| Distance between two points | Network | Band (Mbps) | Bandwidth compression (Mbps) | Encoding time (ms) | Decoding time (ms) | Total latency (median, IQR) (ms) | ||
|---|---|---|---|---|---|---|---|---|
| Sapporo Medical University | Mombetsu general hospital | 270 km | FTTB | 100 | 24 → 3.0 | 10.0 | 1.0 | 37.5 (35.0–43.0) |
| Sapporo Medical University | Keio University | 1150 km | FTTB | 100 | 24 → 3.0 | 10.0 | 1.0 | 24.5 (23.0–27.0) |
| Sapporo Medical University | Yamanashi University | 1250 km | FTTB | 100 | 24 → 3.0 | 10.0 | 1.0 | 29.0 (26.5–31.5) |
| Sapporo Medical University | Red Cross Hospital Osaka | 1650 km | FTTB | 100 | 24 → 3.0 | 10.0 | 1.0 | 27.5 (25.5–29.0) |
| Sapporo Medical University | Kyushu University | 2000 km | FTTB | 100 | 24 → 3.0 | 10.0 | 1.0 | 29.5 (25.5–31.5) |
| Sapporo Medical University | Nagasaki University | 2150 km | FTTB | 100 | 24 → 3.0 | 10.0 | 1.0 | 34.0 (32.0–36.0) |
| Sapporo Medical University | University of the Ryukyus | 3200 km | FTTB | 100 | 24 → 3.0 | 10.0 | 1.0 | 48.5 (43.5–54.5) |
| Diagnosis | cStage | Operation | Lymphadenectomy | Operative time (min) | Blood loss (ml) |
|---|---|---|---|---|---|
| Sigmoid colon cancer | IIa | Laparoscopic sigmoid colon resection | D3 | 178 | 3 |
| Sigmoid colon cancer | IIIb | Laparoscopic sigmoid colon resection | D3 | 219 | 5 |
| Sigmoid colon cancer | IIa | Laparoscopic sigmoid colon resection | D3 | 212 | 5 |
| Sigmoid colon cancer | I | Laparoscopic sigmoid colon resection | D3 | 184 | 5 |
| Sigmoid colon cancer | IIa | Laparoscopic sigmoid colon resection | D3 | 210 | 5 |
| Recto‐sigmoid cancer | IIIb | Laparoscopic high anterior resection | D3 | 318 | 5 |
|
Sigmoid colon cancer Descending colon cancer |
IIa I |
Laparoscopic left colectomy | D3 | 464 | 100 |
Abbreviations: FTTB, fiber to the building; IQR, interquartile range.
2.2. Measuring latency
We conducted an experiment involving two remote locations using an ultra‐low latency communication system for remote medical education (TELEPRO®, Tenmashimon Co. Ltd.; patent pending in Japan). The entire system involves the proctor's and proctee's sides being connected to a wide‐area network through the internet via the TELEPRO® server. From a remote location, the proctor can communicate using a microphone, speaker, and web camera and can draw annotation lines on a touch panel monitor that shows the images as well as audio (Figure 1). Camera images from both proctor's and proctee's sides are received and connected to the TELEPRO® server to achieve interactive communication between two locations (Videos S1 and S2). The server also records the latency between the two remote locations by detecting the use of the annotation pen on the touch monitor's surface. Hundreds of annotations were performed at each hospital, and the latency of each was measured. Also, encoding time, the sum of camera latency and encode latency, and decoding time, the sum of decode latency and monitor latency, were measured to verify the distance dependence of line latency (Figure 2). Starting with tele‐proctoring with a hospital in Hokkaido, the distance between two locations was gradually extended.
FIGURE 1.
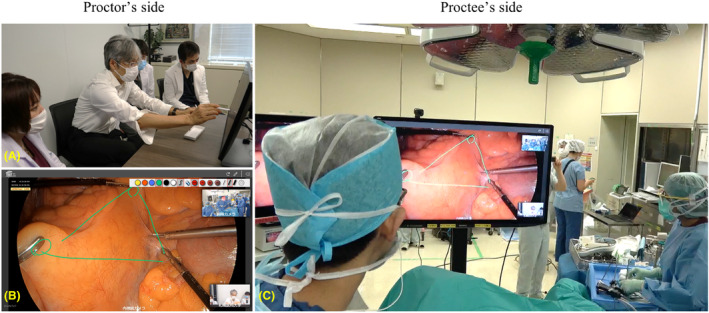
Tele‐proctoring from Sapporo Medical University to University of the Ryukyus. A scene in showing the formation of a “triangulation” in the mesentery at the monitor of doctor's office at Sapporo Medical University (Figure 2A,B) and the operating room in University of the Ryukyus (Figure 2C).
FIGURE 2.
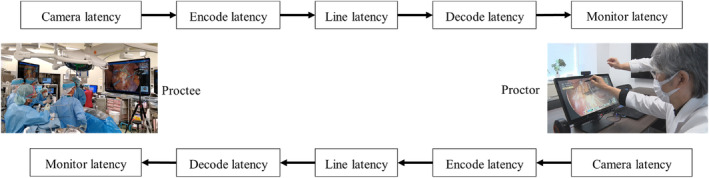
Each component of latency in this study.
2.3. An ultra‐low latency communication system
A view of the internal and operating field was captured by laparoscope and a web camera with two sets of wireless microphones on the proctee's side, which was then sent to the proctor's side (Figure 3). The two locations were connected via the internet and shared 100 Mbps maximum at best effort. The quality of the camera was set at maximum quality (720 p). Return input included a face camera, web microphone, and the annotation lines drawn on a touch panel monitor. All devices were USB‐connected to the proctor's computer. The TELEPRO MENTEE Workstation in the operating room is used to encode and decode audio and video data (Figure 3). The resolution of each camera was automatically downgraded to 720 p (or 1080 p) for any higher display resolution (e.g., 4 K, full high definition, and 1080 p), depending on the maximum internet speed. 10 We purposefully limited the band to 100 Mbps at Sapporo Medical University's doctor's office so that the verified applicability can hold up even in facilities where dedicated internet access lines cannot be installed because of financial, geographical, and infrastructural reasons (Appendix S1).
FIGURE 3.
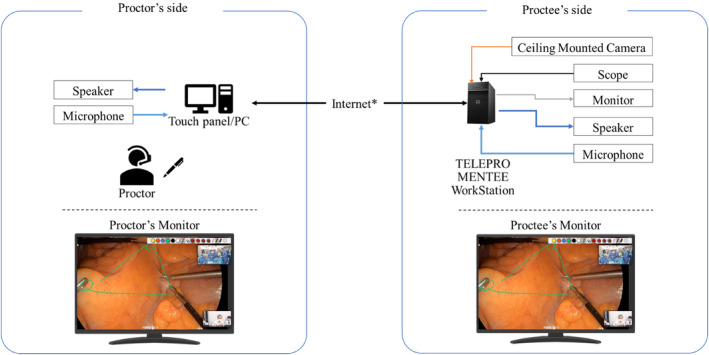
Equipment for tele‐proctoring‐assisted procedures between proctor's side and proctee's side through tele‐proctoring system TELEPRO® (Tenmashimon Co. Ltd.).
2.4. Briefing sheet
Thorough briefings should be conducted to ensure that surgeons are not interrupted by complications, livestream device‐related issues, and/or unstable internet connections. Briefing sheets serve as a reminder of the briefings. Medical professionals should be comprehensively aware of the possible risks of real‐time internet communication during surgery in advance. The briefings should also be done in the presence of information technology experts both within the operating room and the proctor's office. Briefing sheets should include the items listed below: (1) a detailed schedule; (2) personnel in charge of operation room staff, an information system officer, and brand representatives of modalities and live‐streaming staff; (3) details of the configuration and input–output wiring of modalities and communication devices; (4) a secure internet protocol between the operating room and the proctor's facility; (5) knowledge of the possible issues that could occur during live streaming and their solutions. A thorough briefing and the associated briefing sheets shared online can familiarize the staff with the streaming plan and allow them to adapt faster to unexpected situations.
2.5. Questionnaires
Questionnaires were administered to doctors (e.g., proctees, assistants, and medical staff attending the surgery) at eight hospitals. The questionnaire was generated using a Google form and distributed via email (Appendix S2). First, the respondents were asked to rate the quickness and quality of communication in terms of latency and disturbances in audio, video, and live telestrations on a scale of 0 (perfectly fine) to 10 (extremely bad). They were also asked to rate the usefulness of surgical education with intraoperative linguistic and annotative instructions from 0 (extremely bad) to 10 (perfectly fine). The research protocol has been approved by a suitably constituted Ethics Committee of Sapporo Medical University, and it conforms to the provisions of the Declaration of Helsinki (Committee of Sapporo Medical University, Approval No. 4‐1‐68).
2.6. Statistical analysis
Mann–Whitney U test was used to analyze continuous variables and questionnaire scores. Spearman's rank correlation was used to evaluate the correlations between the distance between two hospitals and the latency of annotation. All p‐values were two‐sided, and p‐values ≤ 0.05 were considered statistically significant. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University), 12 a graphical user interface for R (The R Foundation for Statistical Computing) that is a modified version of the R commander designed to add statistical functions frequently used in biostatistics.
3. RESULTS
The total latency between the doctor's office at Sapporo Medical University and the operating room at Mombetsu General Hospital was 37.5 ms. Similarly, the total latency between the Sapporo Medical University and Keio University was 24.5 ms, Yamanashi University was 29.0 ms, Red Cross Hospital Osaka was 27.5 ms, Kyushu University was 29.5 ms, Nagasaki University was 34.0 ms, and the University of the Ryukyus was 48.5 ms (Table 1). The total latency positively correlated with the distance between two locations (R = 0.55, p < 0.01; Figure 4). Encoding time was about 10 ms, and decoding time was about 1 ms, almost constant regardless of location (Appendix S3).
FIGURE 4.
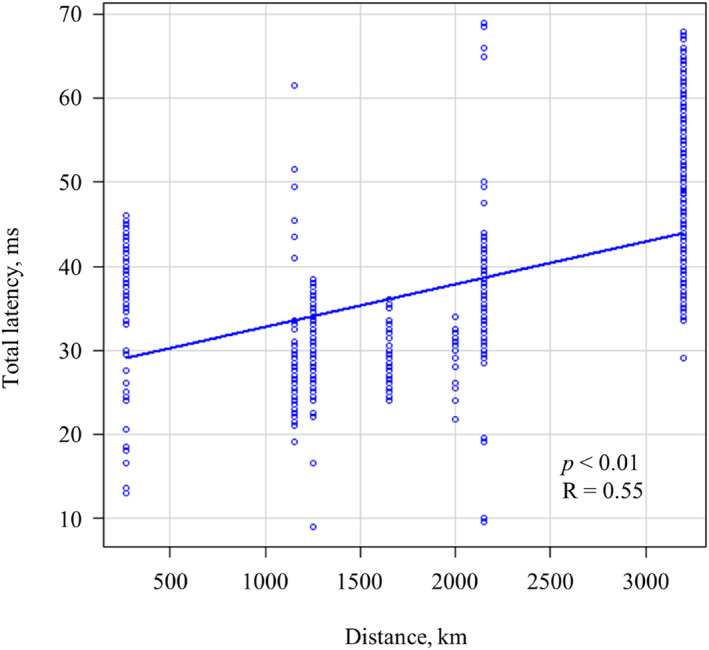
Verification of correlation between the distance of two locations and total latency.
For the items regarding the quality of communication, about half of the respondents chose “0” (perfectly fine) for latency and disturbance for each audio, video, and annotation (Figure 5A–C). In the items of surgical education with intraoperative linguistic and annotative instructions, the respondents were asked about surgical quality, “anatomical recognition, surgical tactics (e.g., reducing operative time), avoidance or recovery of unexpected complications” (Figure 5D), educational effect “education effects for proctees, education effects for colleagues or workers on‐site other than proctees, review of the surgical videos including audio and annotations” (Figure 5E), social impact “tele‐communication in a disaster or a pandemic (e.g., COVID‐19), and application for the proctoring system in any robotic surgeries” (Figure 5F). Responses to all options showed a similar trend, and 10 (perfectly fine) was the most common response, indicating mostly positive responses about the usefulness of tele‐proctoring. However, “anatomical recognition,” “avoidance or recovery of unexpected complications,” and “reducing operative time” were negative responses that scored ≤4 in a few cases. In examining whether the size of latency affects surgical education, there were no significant differences in surgical quality, educational effect, or social impact between the latency ≥30 ms group and the latency <30 ms group (Table 2).
FIGURE 5.
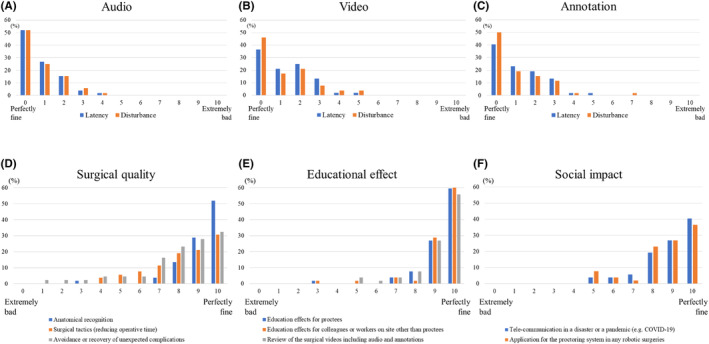
The questionnaire about the quality of communication and surgical education with annotative instructions. The respondents were asked about latency and disturbance for each of audio (A), video (B), and annotation (C). The respondents were asked about surgical quality (D), educational effect (E), and social impact (F).
TABLE 2.
The effect of latency on the results of the surgical education questionnaire.
| Score | p Value | ||
|---|---|---|---|
| Latency (≥30 ms) n = 14 | Latency (<30 ms) n = 38 | ||
| Surgical quality | |||
| Anatomical recognition | 9 (3–10) | 10 (7–10) | 0.06 |
| Surgical tactics (reducing operative time) | 8 (4–10) | 9 (4–10) | 0.32 |
| Avoidance or recovery of unexpected complications | 8 (3–10) | 9 (1–10) | 0.56 |
| Educational effect | |||
| Educational effects for proctees | 10 (3–10) | 10 (7–10) | 0.81 |
| Educational effects for colleagues or workers on site other than proctees | 10 (3–10) | 10 (5–10) | 0.60 |
| Review of the surgical videos including audio and annotations | 10 (5–10) | 10 (7–10) | 0.80 |
| Social impact | |||
| Tele‐communication in a disaster or a pandemic (e.g., COVID‐19) | 9 (5–10) | 9 (5–10) | 0.23 |
| Application for the proctoring system in any robotic surgeries | 9 (5–10) | 9 (5–10) | 0.11 |
4. DISCUSSION
In tele‐proctoring, a latency of up to 200–250 ms is generally considered acceptable, and longer latency might be a major obstacle. 13 , 14 , 15 The recommendation provided by SAGES requires a latency of less than 450 ms for tele‐proctoring. 16 Currently, communication latency has become a problem for tele‐proctoring using SIA (Latency; 425–1500 ms). 6 , 17 , 18 , 19 In our previous report, the median latency between Sapporo and Tokyo (1150 km) was 27.5 ms, 10 and the same latency was measured in tele‐proctoring with a hospital in Tokyo. Moreover, even between two locations with the longest distance of 3200 km, the median latency was 48.5 ms, representing a significant reduction in latency. These results identify a positive correlation between the distance of two locations and total latency since the line latency increases as the number of line transfers increases, so the speed of the optical fiber cable is constant at 200 km/ms (i.e., 2/3 of the speed of light 300 km/ms). Further, the distance dependence of line latency is due to shortened encoding and decoding time. The time required for encoding and decoding was similar regardless of location, suggesting that TELEPRO®'s improved processing power helped achieve low‐latency communication. The results in this study are well below the acceptable latency for tele‐proctoring on both commercial lines and SINET routes. Recently, 5G‐assisted tele‐proctoring has been reported; however, the latency was 146–202 ms, suggesting that time other than line latency is still required, although no mention is made of encoding or decoding time. 20 Additionally, the high frequency, short flying distance, and non‐bending nature of 5G require installing many antennas, and its high cost means that it will take some time before it is widely used. 5G may be one method for the expected bandwidth expansions to spread tele‐proctoring, and its future development is desirable.
Tele‐proctoring effectively educated the participants, especially in anatomical recognition and surgical education for proctees, assistants, and medical staff. These results may be due to the two‐way communication of tele‐proctoring and the ability to provide annotation guidance in real‐time. Surgical education using annotation was shown to be useful with da Vinci surgery. 21 , 22 , 23 As illustrated by the questionnaire results, surgical quality, educational effect, and social impact all received positive responses, and the educational effect of tele‐proctoring seems to be very promising. Verifying the differences in the questionnaire results between large and small latency—although there was a positive correlation between the distance between two locations and total latency—revealed no significant differences in the questionnaire results between the two groups for all latencies measured in this study. For a median latency of either ≥30 ms or <30 ms, the latency around 30 ms was difficult to recognize subjectively and had no effect on surgery. Thus, this study indicates that one‐to‐one tele‐proctoring could achieve low latency communication in the Japanese archipelago regardless of location. While “anatomical recognition,” “avoidance or recovery of unexpected complications,” and “reducing operative time” were negative responses that scored ≤4 in a few cases. This is thought to be due to the difference in educational systems and policy between proctors and proctees—for example, the differences between D3 lymphadenectomy in Japan and complete mesocolic excision overseas, and whether the arterial dissection position is high tie or low tie, the starting position of the medial approach. This limitation of “education” may be due to differences in facilities rather than systems, suggesting the importance of prior briefing. By popularizing tele‐proctoring, we hope to reduce the disparities in surgical skills between facilities and promoting the standardization of surgery, and career support for female surgeons. Therefore, we believe that tele‐proctoring can be applied in other departments where laparoscopic or robotic surgery is performed, for example respiratory surgery, urology, and gynecology.
The feasibility of tele‐proctoring using SIA was verified while ensuring patient safety. In the future, we hope to improve Japanese medical standards by applying tele‐proctoring using this system to young surgeons and female surgeons.
This study has several limitations. First, although low latency communication was achieved, this system has only been proven to work for small 1:1 communication. If it is to be applied to larger‐scale communications in the future, expanding the bandwidth and stability of communications accordingly via network infrastructure development at the national level is necessary. 7 , 20 , 24 Second, compared to on‐site proctoring, tele‐proctoring requires a system that can respond to troubleshooting. The proctor requires extremely advanced educational skills such as standardizing surgical techniques and communicating in a common language, as well as quickly recognizing micro anatomy. In this study, the feasibility of tele‐proctoring by proctor with extensive experience in many surgical training programs who advocate the necessity of such skills was verified. In the future, it will be necessary to consider how to acquire such advanced educational skills. We consider that proctors are important from the viewpoint of future tele‐proctoring and the proctoring system for robotic surgery established by the Japan Society for Endoscopic Surgery (JSES). 25 While there are guidelines promoted by Agency for Medical Research and Development for tele‐surgery, developing guidelines specific to tele‐proctoring would be desirable in the future. From these perspectives, the addition of incentives must also be considered. One factor contributing to the lack of widespread adoption of tele‐proctoring is the legal limitations, such as personal information protection and responsibility. Confidentiality is an issue when using electronic systems, and special measures must be taken to prevent the improper communication of medical data. 26 , 27
5. CONCLUSIONS
One‐to‐one tele‐proctoring using SIA is clinically feasible and expected to be a sustainable approach to help education for young surgeons and surgical supports in rural areas. This study is a major step toward reducing disparities in health care.
AUTHOR CONTRIBUTIONS
All the authors participated in designing the study. Ichiro Takemasa, Koichi Okuya, Kenji Okita, and Korai Takahiro wrote the manuscript. All authors have read and approved the final version of the manuscript.
FUNDING INFORMATION
This research did not receive any grant from funding agencies in the public, commercial, or not‐for‐profit sectors.
CONFLICT OF INTEREST STATEMENT
Eiji Oki, Susumu Eguchi, Daisuke Ichikawa, Yuko Kitagawa, Masaki Mori, and Ichiro Takemasa are members of the Editorial Board of Annals of Gastroenterological Surgery.
ETHICS STATEMENT
Approval of the research protocol: The protocol for this research project has been approved by a suitably constituted Ethics Committee of Sapporo Medical University and it conforms to the provisions of the Declaration of Helsinki (Committee of Sapporo Medical University, Approval No. 4‐1‐68).
Informed consent: N/A.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Supporting information
Appendix S1.
Appendix S2.
Appendix S3.
Video S1.
Video S2.
Takemasa I, Okuya K, Okita K, Akizuki E, Miyo M, Ishii M, et al. Tele‐proctoring for minimally invasive surgery across Japan: An initial step toward a new approach to improving the disparity of surgical care and supporting surgical education. Ann Gastroenterol Surg. 2024;8:356–364. 10.1002/ags3.12750
DATA AVAILABILITY STATEMENT
The dataset supporting our conclusions is included within the article.
REFERENCES
- 1. Ministry of Health, Labour and Welfare . [Internet]. Japan: Ministry of Health, Labour and Welfare [updated Mar 2022]. 2022. Available from: https://www.mhlw.go.jp/toukei/saikin/hw/ishi/18/index.html
- 2. Hakamada K, Mori M. The changing surgical scene: from the days of Billroth to the upcoming future of artificial intelligence and telerobotic surgery. Ann Gastroenterol Surg. 2021;5:268–269. 10.1002/ags3.12466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD‐3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population‐based registries in 71 countries. Lancet. 2018;391:1023–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ward ZJ, Scott AM, Hricak H, Abdel‐Wahab M, Paez D, Lette MM, et al. Estimating the impact of treatment and imaging modalities on 5‐year net survival of 11 cancers in 200 countries – a simulation‐based analysis. Lancet Oncol. 2020;21:1077–1088. 10.1016/S1470-2045(20)30317-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. OECD Health Statistics . [Internet]. France: OECD org [updated Oct 2022]. 2022. Available from: https://www.oecd.org/health/health‐data.htm
- 6. Huang EY, Knight S, Guetter CR, Davis CH, Moller M, Slama E, et al. Telemedicine and telementoring in the surgical specialties: a narrative review. Am J Surg. 2019;218(4):760–766. 10.1016/j.amjsurg.2019.07.018 [DOI] [PubMed] [Google Scholar]
- 7. Thomsen ASS, Saleh GM. Telementoring and remote training in the present era. Acta Ophthalmol. 2021;99(4):e617–e618. 10.1111/aos.14581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Artsen AM, Burkett LS, Duvvuri U, Bonidie M. Surgeon satisfaction and outcomes of tele‐proctoring for robotic gynecologic surgery. J Robot Surg. 2022;16(3):563–568. 10.1007/s11701-021-01280-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sterbis JR, Hanly EJ, Herman BC, Marohn MR, Broderick TJ, Shih SP, et al. Transcontinental telesurgical nephrectomy using the da Vinci robot in a porcine model. Urology. 2008;71(5):971–973. 10.1016/j.urology.2007.11.027 [DOI] [PubMed] [Google Scholar]
- 10. Korai T, Okita K, Okuya K, Hamabe A, Miyo M, Akizuki E, et al. Development and success of an ultra‐low latency communication system using a shared internet access: a contribution to the spread of telemedicine. Surg Today. 2023;53:522–525. 10.1007/s00595-022-02602-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kurimoto T, Urushidani S, Yamada H, Yamanaka K, Nakamura M, Abe S, et al. SINET5: a low‐latency and high‐bandwidth backbone network for SDN/NFV Era. In: IEEE International Conference on Communications (ICC) 2017. 10.1109/ICC.2017.7996843 [DOI]
- 12. Kanda Y. Investigation of the freely available easy‐to‐use software “EZR” (easy R) for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. 10.1038/bmt.2012.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim T, Zimmerman PM, Wade MJ, Weiss CA 3rd. The effect of delayed visual feedback on telerobotic surgery. Surg Endosc. 2005;19(5):683–686. 10.1007/s00464-004-8926-6 [DOI] [PubMed] [Google Scholar]
- 14. Korte C, Nair SS, Nistor V, Low TP, Doarn CR, Schaffner G. Determining the threshold of time‐delay for teleoperation accuracy and efficiency in relation to telesurgery. Telemed J E Health. 2014;20(12):1078–1086. 10.1089/tmj.2013.0367 [DOI] [PubMed] [Google Scholar]
- 15. Xu S, Perez M, Yang K, Perrenot C, Felblinger J, Hubert J. Determination of the latency effects on surgical performance and the acceptable latency levels in telesurgery using the dV‐trainer(®) simulator. Surg Endosc. 2014;28(9):2569–2576. 10.1007/s00464-014-3504-z [DOI] [PubMed] [Google Scholar]
- 16. Bogen EM, Schlachta CM, Ponsky T. White paper: technology for surgical telementoring—SAGES project 6 technology working group. Surg Endosc. 2019;33(3):684–690. 10.1007/s00464-018-06631-8 [DOI] [PubMed] [Google Scholar]
- 17. Yeray TL, Mario DTH, Stefanie CM. Telementoring of in‐home real‐time laparoscopy using Whatsapp messenger: an innovative teaching tool during the COVID‐19 pandemic. A cohort study. Ann Med Surg (Lond). 2021;62:481. 10.1016/j.amsu.2021.01.085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dehlela S, Nihal A, Jhasketan P, Trinh M, Balakrishnan S, Kurer M, et al. Towards development of a tele‐mentoring framework for minimally invasive surgeries. Int Med Robot. 2021;17(5):e2305. 10.1002/rcs.2305 [DOI] [PubMed] [Google Scholar]
- 19. Treter S, Perrier N, Sosa JA, Roman S. Telementoring: a multi‐institutional experience with the introduction of a novel surgical approach for adrenalectomy. Ann Surg Oncol. 2013;20(8):2754–2758. 10.1245/s10434-013-2894-9 [DOI] [PubMed] [Google Scholar]
- 20. Lacy AM, Bravo R, Otero‐Piñeiro AM, Pena R, de Lacy FB, Menchaca R, et al. 5G‐assisted telementored surgery. Br J Surg. 2019;106(12):1576–1579. 10.1002/bjs.11364 [DOI] [PubMed] [Google Scholar]
- 21. Goonewardene SS, Brown M, Challacombe B. Single‐versus dual‐console robotic surgery: dual improves the educational experience for trainees. World J Urol. 2016;34(9):1337–1339. 10.1007/s00345-016-1762-1 [DOI] [PubMed] [Google Scholar]
- 22. Jarc AM, Shah SH, Adebar T, Hwang E, Aron M, Gill IS, et al. Beyond 2D telestration: an evaluation of novel proctoring tools for robot‐assisted minimally invasive surgery. J Robot Surg. 2016;10(2):103–109. 10.1007/s11701-016-0564-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yamamoto M, Ashida K, Hara K, Sugezawa K, Uejima C, Tanio A, et al. Initial experience in rectal cancer surgery for the next generation of robotic surgeons trained in a dual console system. Yonago Acta Med. 2021;64:240–248. 10.33160/yam.2021.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zheng J, Wang Y, Zhang J, Guo W, Yang X, Luo L, et al. 5G ultra‐remote robot‐assisted laparoscopic surgery in China. Surg Endosc. 2020;34(11):5172–5180. 10.1007/s00464-020-07823-x [DOI] [PubMed] [Google Scholar]
- 25. Shibasaki S, Suda K, Kadoya S, Ishida Y, Nakauchi M, Nakamura K, et al. The safe performance of robotic gastrectomy by second‐generation surgeons meeting the operating surgeon's criteria in the Japan Society for Endoscopic Surgery guidelines. Asian J Endosc Surg. 2022;15(1):70–81. 10.1111/ases.12967 [DOI] [PubMed] [Google Scholar]
- 26. Săceanu SM, Angelescu C, Valeriu S, Patrașcu A. Telesurgery and robotic surgery: ethical and legal aspect. J Commun Med Health Educ. 2015;5(3):355. 10.4172/2161-0711.1000355 [DOI] [Google Scholar]
- 27. St Julien J, Perrier ND. Video telementoring to accelerate learning of new surgical techniques. JAMA Surg. 2016;151(7):671–672. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1.
Appendix S2.
Appendix S3.
Video S1.
Video S2.
Data Availability Statement
The dataset supporting our conclusions is included within the article.


