Abstract
The study aimed to evaluate the immediate effects of a dry needling (DN) therapy session on biomechanical properties, muscle power, perfusion, and pressure pain threshold of the gastrocnemius muscle with latent trigger points. Twenty mixed martial arts athletes (MMA) were randomly divided into two groups: experimental (eDN, n = 10) and sham (qDN, n = 10) to undergo one session of DN either with a real or a qazi needle. The measurements were taken at rest, 1-5 minutes after the DN (Post1-5min) and 24h after the DN (Post24h). DN significantly increased the muscle perfusion (Post1-5min and Post24h, p < 0.001), reduced its tone (Post1-5min and Post24h, p < 0.001) and stiffness (Post1-5min, p < 0.05; Post24 h, p < 0.001), and improved its elasticity (Post1-5min and Post24h, p < 0.001). DN also caused a significant increase in pressure pain threshold (Post1-5min, p < 0.001; Post24h, p < 0.05) and in muscle power (Post24h, p < 0.01). The DN session increased the blood perfusion and improved the biomechanical properties of the gastrocnemius muscle, which led to improved muscle power. The DN also had an analgesic effect. These effects were maintained at 24 h, which suggests that DN could facilitate muscle recovery in a post-exercise period of MMA athletes.
Key points.
Latent trigger points in skeletal muscles reduce their functionality, increasing the risk of injury and impairing the sports performance of martial arts athletes.
A single dry needling session improves the microcirculation in the gastrocnemius muscle with latent trigger points acutely and for at least 24 hours.
A session of dry needling also improves the biomechanical properties of the muscle and its power.
Dry needling shows an analgesic effect.
Dry needling seems to be effective in facilitating muscle regeneration, improving athletic performance, and most importantly, it is safe, so mixed martial arts athletes can use it after training sessions and before competition.
MyotonPro is a reliable tool for measuring biomechanical properties of skeletal muscles.
Key words: Latent trigger point, mixed martial arts, myotonometry, blood perfusion
Introduction
Trigger point(s) TrP adversely affects muscles’ function, increasing its stiffness and reducing muscle strength (Albin et al., 2020; Ballyns et al., 2012; Fernández-de-las-Peñas and Dommerholt, 2018; Simons et al., 2002). TrP is an overly sensitive area in a tense band of the skeletal muscle fibers, characterized by referred pain and sometimes a local twitch response (LTR) (Kelly et al., 2018). The most accepted definition describes the muscle TrP as "a hypersensitive point in skeletal muscles associated with a hypersensitive palpable node in a taut band. The site is painful with manual pressure and may cause referred pain, tenderness, motor dysfunction, and autonomy phenomena " (Fernández-de-las-Peñas and Dommerholt, 2018). TrP can be latent or active and usually develops in response to chronic muscle fatigue but also to acute or chronic damage of a muscle, tendon, ligament, joint, or nerve (Ding et al., 2018). The diagnostic criteria and etiology of TrP are still unclear. TrP may have one or more over-sensitive locus/loci characterized by a greater concentration of nociceptors. These loci tend to mainly occur in the vicinity of the motor end plate; nevertheless, they can also be found in other areas of the muscle (Jiménez-Sánchez et al., 2018; Rivers et al., 2015). Sensitive loci have a specific EMG pattern consisting of spontaneous low-amplitude superimposed by high-amplitude discharges. This phenomenon is the end-plate noise (EPN) (Domingo et al., 2013).
Dry needling (DN) is one of the therapeutic methods used to alleviate TrP; its actual mechanisms have not yet been established (Liu et al., 2015). DN beneficially affects the muscles’ biomechanical properties, including reduction of muscle tone and stiffness, as well as increases in its elasticity (Albin et al., 2020; Kelly et al., 2021). The American Physical Therapy Association (APTA) has defined DN as "a skilled intervention using a fine needle to penetrate the skin that stimulates TrP, muscles, and connective tissue to treat neuromusculoskeletal disorders" (Dos Santos et al., 2021; Fernández-de-las-Peñas and Dommerholt, 2018). Despite its utilization in sports rehabilitation, DN has not been sufficiently studied (Boyles et al., 2015; Gattie et al., 2017; Kietrys et al., 2013; Mansfield et al., 2019). It is also worth mentioning that DN still raises some concerns among coaches and their athletes, as it has been suggested that DN can intensify exercise-induced muscle pain and impair athletic performance (Martín-Pintado-Zugasti et al., 2018).
Previous studies have shown that the effects of DN on the latent TrP include reducing muscle pain (Mansfield et al., 2019), modify the muscle tissue hyperemia (Sandberg et al., 2003, 2005) and improve mobility of the musculoskeletal system (Gattie et al., 2017; Zarei et al., 2020) and regeneration (Albin et al., 2020; Bandy et al., 2017; Dos Santos et al., 2021). However, there is a research gap in the scientific literature describing the impact of DN on muscle biomechanical changes and their correlations with tissue perfusion; in particular, there are no studies in the group of martial arts athletes.
The nature of mixed martial arts (MMA) fights places high physiological demands on the fighters. MMA differs from other martial arts in requiring high muscle strength (James et al., 2016). The rules of MMA allow the use of strikes and holds both in a standing position and on the ground. The fight itself involves many explosive actions, such as kicks and punches, the effectiveness of which is often crucial to the final result of the competition (Andrade et al., 2019). The energy systems that an MMA fighter activates during a fight are the same as those that enable repeated sprinting effort (Zebrowska et al., 2019). Excessive static and dynamic exercise leads to myocytes’ membrane damage, activation of inflammatory processes, muscle soreness, local ischemia, and unfavorable changes in the muscle biomechanical properties, including increased muscle tone and stiffness and decreased elasticity (Albin et al., 2020; Albracht and Arampatzis, 2013; Ballyns et al., 2012; Enoka and Duchateau, 2008).
Such changes will make the skeletal muscles more susceptible to fatigue and injury during exercise (Konrad et al., 2023), hinder their regeneration (Albin et al., 2020; Konrad et al., 2023), and over time may lead to the development of trigger point(s) (TrP). TrP adversely affects muscles’ function, increasing its stiffness and reducing muscle strength (Albin et al., 2020; Ballyns et al., 2012; Fernández-de-las-Peñas and Dommerholt, 2018; Simons et al., 2002).
It seems crucial to evaluate the methods used to assess changes in biomechanical properties of skeletal muscles in response to exercise (Ding et al., 2018; Hansen et al., 2010; Simons et al., 2002). Myotonometry and laser Doppler flowmetry (LDF) are well-documented methods assessing muscles’ biomechanical properties, such as tone, stiffness, elasticity (myotonometry), and hyperemia (LDF) (Kvandal et al., 2006; Liana et al., 2009; Szyguła et al., 2020), which is indicative of changes in the muscle tissue induced by exercise (Szyguła et al., 2020). In myotonometry, a probe applies a mechanical impulse to the muscle tissue, eliciting oscillations of the muscles to measure the biomechanical properties of the muscle (Bartsch et al., 2023a; Chen et al., 2019a; Kisilewicz et al., 2020; Melo et al., 2022). LDF is a method comparable with capillaroscopy and thermographic methods (Kvandal et al., 2006a). Although it is popular in sports medicine, it would be an innovative method for assessing changes induced by a therapy called dry needling (Szyguła et al., 2020).
The objective of the current study was to assess the immediate effects of a DN session on the biomechanical properties (muscle tone, stiffness, elasticity), power, pressure pain threshold, and blood perfusion of the gastrocnemius muscles in mixed martial arts (MMA) athletes. We hypothesized that DN within latent TrP can beneficially affect the biomechanical properties of the muscle, reduce muscle pain, and increase muscle power. Our study findings will contribute to a better understanding of the relationship between biomechanical properties of the muscle and local ischemia causing latent TrP and their adverse effect on athletic performance of MMA athletes.
Methods
Participants
Twenty MMA fighters (n = 20) were enrolled in the study according to the following inclusion criteria: subjects aged 18-40 years, with a minimum of 3 years of training experience, training at least four times per week, and with a documented record (data of professional fights on tapology.com, amateur fights on mmapolska.org) of amateur or professional fights. The exclusion criteria were as follows: elevated blood pressure at rest (blood pressure > 140/90 mm Hg), musculoskeletal system injuries, skin lesions and a tattoo close to the procedure site (inability to interpret tissue perfusion), needle phobia, fever, infection, allergy to nickel, extreme fatigue. Participants were asked to refrain from consuming ergogenic drinks for 4 hours before the test and abstain from training 48 hours before the study, which could affect the blood perfusion measurement. All participants were informed that they could withdraw from the study without giving reasons. Signed informed consent was obtained from each subject.
The research study was approved by the ethics committee at the National Council of Physiotherapists (consent No. 26/2022 of January 12, 2023) and registered as a clinical trial (ISRCTN10378682). The study was carried out by the Declaration of Helsinki.
Study design
In this single-blind randomized controlled trial, participants were randomly assigned (simple randomization 1:1 using randomizer.org) to either the experimental (eDN; n = 10) or placebo (qDN; n = 10) group (Figure 1- flow chart). Fourteen days before the study, each participant was familiarized with the DN method (familarization intervention). The DN procedure was carried out by the safety rules, which included disinfecting the puncture site. DN was performed in a standardized prone position with feet hanging freely off the table. In the eDN group, sterile soma needles 0.30x50 mm were used (Figure 2). Each puncture was made with one needle for one TrP, and an LTR was monitored for. TrP was defined as palpable tenderness in a taut band approximately four fingers below the popliteal fossa in the medial head of the gastrocnemius muscle of both legs. An experienced clinician, also a DN instructor, performed an average of 3 to 5 punctures in the area of the TrP without removing the needle from the skin. If LTR was not observed after five punctures, the clinician changed the needle and a puncture site about 5 cm away from the initial puncture site. The procedure was repeated for each gastrocnemius muscle (Albin et al., 2020; Fernández-de-las-Peñas and Dommerholt, 2018). In case of no LTR, insertions were discontinued. The entire procedure lasted from 15 to 30 seconds for one TrP. If the patient was experiencing a burning sensation during the process or a different adverse reaction, the procedure was discontinued (this applied to one subject). After the DN, a 5-second ischemic compression was performed to reduce the unpleasant sensations due to LTR. In the qDN group, a quasi-needle that did not pierce the skin was used instead. The quasi needle contained a spring, which, along with a unique technique, enabled to produce a similar sensation to that by the needle used in DN (telescopic needle - sham therapy- Figure 3) (Braithwaite et al., 2019). Additionally, due to the prone position, the participants could not see the used needle.
Figure 1.
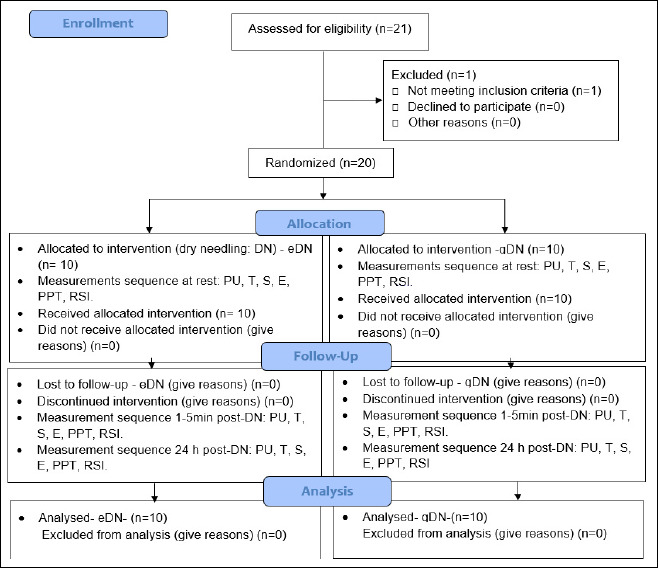
Consort diagram.
Figure 2.

Dry needling in the experimental group (eDN). DN application in the experimental group
Figure 3.

Dry needling in the placebo (qDN) group using a telescopic needle (sham therapy).
The following measurements were taken at rest (Rest), 1-5 minutes after the DN therapy (Post1-5min) and at the 24th hour after the DN (Post24h): blood perfusion described in non-reference units (PU), muscle tone (T - [Hz]), dynamic stiffness (S - [N/m]), elasticity (E- [arb- relative arbitrary unit]), pressure pain threshold (PPT - [N/cm] ), and muscle power based on relative strength index (RSI = jump height/contact time [m/s]. The measurements were taken by trained students and physiotherapists in the following order: (1) PU, (2) T, (3) S, (4) E, (5) PPT and (6) RSI. All participants were tested between 10 am and 12 pm at the Provita Medical Center in Poland.
Measurement- perfusion unit (PU)
To analyze the PU, the LDF was used (Szyguła et al., 2020). After clinically determining the site (Albin et al., 2020) and marking it with a special pen, the wave reflected from the erythrocytes was measured (Szyguła et al., 2020). The LDF was performed using a Perimed apparatus (Sweden 2004). The measurement depth was 2.5 mm, the volume was 1 mm3, and the procedure lasted 2 minutes. The LDF method, due to its repeatability, high sensitivity, and non-invasiveness, allows for a precise assessment of microcirculation at rest and in response to a physical stimulus. The standardized LDF test proposed by Liana et al. (Liana et al., 2009) was used to assess augmented in response to DN skin microcirculation. Laser Doppler flowmetry (LDF) is a standard technology to access microcirculatory function in vivo (Rodrigues et al., 2019). Better sensors and more effective wireless communication cause great interest among scientists and clinicians in using LDF. LDF is the gold standard in assessing microcirculatory reactions, demonstrating great sensitivity and repeatability of measurements (Kvandal et al., 2006).
Measurement- myotonometry
The gastrocnemius muscles T, S, and E were assessed using a myotonometer - MyotonPRO (AS, Myoton Ltd, Estonia 2021), which is a digital palpation device consisting of a body and an indentation probe (Ø 3 mm). The MyotonPro employs the Mechanical Dynamic Response method, which consists of a mechanical precision impulse, the recording of dynamic tissue response in the form of physical displacement and oscillation acceleration signal, and the subsequent computation of parameters characterizing T, S, and E. Its reliability and repeatability have been confirmed in scientific literature. (Bartsch et al., 2023; Melo et al., 2022). Pre-pressure (0.18 N) is first applied through the probe to the surface, compressing the tissue underneath. The device then releases a mechanical impulse (0.4 N, 15 ms), deforming the tissue for a short time (Melo et al., 2022). The device evaluates the resting T state based on a muscle's oscillation frequency in resting state (silent EMG signal) (Bartsch et al., 2023). The S assessed by myotonometry characterizes the resistance of the muscle to contraction (Chen et al., 2019). Muscle E, defined as the muscle's ability to regain its original shape after deformation, was measured as a logarithmic decrement that characterizes the dampening of tissue oscillation. The faster the tissue oscillation fades, the higher the dissipation of mechanical energy induced by the measurement impulse. The decrement of tissue natural oscillation inversely describes elasticity (Bartsch et al., 2023).
Measurement- pressure pain threshold (PPT)
The PPT was measured with an algesimeter (FDIX, Wagner Instruments, Greenwich, CT, USA 2013). The participants were subjected to three compression tests with a probe (parameters: r = 4 mm) in a tissue area (mm). The force value (in kg or N/cm 2) was calculated as the average of the three measurements and displayed digitally. In case of a significant deviation in the measured value, the device signaled the need to repeat the test. The pressure force was increased until a stimulus was unpleasant for the participant (Suzuki et al., 2022). Pressure algometers have been widely used in clinical practice for almost one hundred years (Park et al., 2011). This instrument is widely used to assess myofascial pain syndrome and various musculoskeletal diseases, demonstrating high repeat measurement reliability (Fernández-Lao et al., 2010).
Measurement – muscle power - reactive strength index (RSI)
A primary goal in exercise science is to evaluate the degree to which training affects performance. Therefore, we rely on empirical data for comparisons and conclusions as sports scientists, coaches, physicians, or trainers. To ensure that the interpretation of the results and inferences drawn from these data are correct, it is essential to perform accurate measurements that are highly reproducible, that the tests can detect small changes in performance, and that the changes found in performance are fundamental and not due to error or measurement noise(Venegas-Carro et al., 2022). The RSI index is one such test for assessing muscle strength, confirmed in scientific literature (Markwick et al., 2015).
The final measurement was the muscle power based on the reactive strength index (RSI). RSI describes an individual's ability to change quickly from eccentric to concentric muscle contraction and is intended to assess the athlete's reactive strength - muscle power. RSI was determined using a drop jump using the Force Decks platform (Vald Performance Australia 2012). The drop jump is reliable for assessing RSI and associated kinematic performance (Healy et al., 2018). The athletes had to perform a drop jump from a 55 cm platform and perform a maximal vertical jump as soon as they landed. Before the test, participants warmed up by doing ten squats and passive stretches of the lower leg muscles for one minute. A research assistant instructed All athletes on the jump technique and made three attempts before the measurements were taken (Gervasi et al., 2022; Markwick et al., 2015). The test involved two different drop heights and assessed how high an athlete can raise their center of gravity. To calculate an RSI for each participant, we used the following equation: RSI = jump height [m]/contact time [s].
Statistical analysis
The standard statistical procedures were selected to calculate the means and standard deviations (SD). The normality and homogeneity of variance were confirmed using Shapiro-Wilk’s and Levene’s tests. The compound symmetry, or sphericity, was assessed by Mauchley’s test. When the assumption of sphericity was not met, the significance of F-ratios was adjusted according to the Greenhouse- Geisser procedure. The evaluation of the effects of the applied DN on the variables PU, T, S, E, PPT, and RSI was performed using a two-factor analysis of variance with repeated measures. The two factors were the study group (eDN vs. qDN) and the time of measurements (Rest and Post-DN: Post1-5 min and Post24 h.
To determine the intragroup and intergroup differences, the post hoc Bonferroni tests were used. The level of significance was set at p ≤ 0.05. Partial eta squared (η 2 p) for ANOVA was used to estimate an effect size with the classifications small (0.01), medium (0.06), and large (0.14) (Cohen, 1992). Also, the percentage change of variables between Rest and Post (1-5 min or 24 h) was calculated as Δ (%): (Post - Rest) / Rest × 100) for each study group. The magnitudes of all effects were assessed using the standardized effect sizes (ES), where thresholds representing trivial, small, moderate, and significant effects were respectively given by < 0.2, 0.2-0.6, 0.6-1.2, and 2-4 times the combined between- subject baseline standard deviation (SD). The most minor worthwhile change in all variables was calculated by multiplying the standard deviation for results obtained at rest measures by a small effect size (i.e., 0.2) to screen for positive and negative responders within the sample. A priori power analysis was conducted with the program G*Power (Faul et al., 2007). The repeated measure ANOVA between interactions with an effect size of at least 0.25, α = 0.05, and 1-β = 0.95 gave a statistical power of 97.37% and a minimum sample size of 16 subjects.
Results
The results of the variance analysis are presented in Table 1. The analysis revealed significant differences between the groups and the time (Rest vs Post1-5 min and Rest vs Post24 h) for PU, T, E, PPT, and RSI (for S, only a significant effect of the time was found) in response to the DN session.
Table 1.
Blood perfusion, biomechanical properties, pressure pain threshold and reactive strength index (muscle power) of the gastrocnemius muscle in the experimental and sham group during Rest and Post-DN period (1-5 min and 24 h).
| Variables | groups | Rest | Post 1-5 minutes | Post 24 hours | ES ηp 2 | Groups effect | Time effect | time × group effect |
|---|---|---|---|---|---|---|---|---|
| PU | eDN | 7.91 ± 0.73 | 12.41 ± 0.93 ‡c | 9.39 ± 1.37 †b | 0.685 | 65.054 <.001 |
39.01 <.001 |
39.198 <.001 |
| qDN | 7.58 ± 0.65 | 7.62 ± 0.83 | 7.8 ± 0.8 | |||||
| T [Hz] | eDN | 18.15 ± 1.87 | 16.13 ± 1.52 ‡a | 14.77 ± 1.09 ‡c | 0.583 | 12.991 .002 |
23.446 <.001 |
25.149 <.001 |
| qDN | 19.42 ± 2.51 | 19.45 ± 2.66 | 19.48 ± 2.05 | |||||
| S [N/m] | eDN | 326.6 ± 57.75 | 303.4 ± 54.79* | 280.8 ± 47.61 ‡ | 0.365 | 3.083 .096 |
13.088 <.001 |
10.356 <.001 |
| qDN | 354.7 ± 78.49 | 355.2 ± 77.04 | 352 ± 69.9 | |||||
| E | eDN | 0.96 ± 0.1 | 0.91 ± 0.13 | 0.84 ± 0.1 ‡a | 0.465 | 5.052 .037 |
3.632 0.037 |
15.649 <.001 |
| qDN | 0.97 ± 0.08 | 1.01 ± 0.08 | 1.01 ± 0.11 | |||||
| PPT [N/cm] | eDN | 112.94 ± 5.93 | 128.52 ± 5.67 ‡c | 136.15 ± 8.24 ‡c | 0.788 | 28.168 <.001 |
58.631 <.001 |
67.073 <.001 |
| qDN | 107.33 ± 11.16 | 104.25 ± 7.95 | 107.19 ± 11.50 | |||||
| RSI [m/s] | eDN | 2.10 ± 0.21 | 2.24 ± 0.24* | 2.35 ± 0.15 ‡b | 0.414 | 10.323 .005 |
5.924 .006 |
11.659 <.001 |
| qDN | 1.98 ± 0.2 | 1.92 ± 0.24 | 1.94 ± 0.22 |
eDN – experimental group; qDN – quasi group; PU – perfusion unit; T- uscle tone; S – stiffness; E – elasticity; PPT - pressure pain threshold; RSI - reactive strength index.
*, †, ‡: significant difference between Post 1-5min- or 24h vs. Rest measures (p < .05; p < .01; p < .001 – respectively);
a, b, c: significant difference between groups (p < .05; p < .01; p < .001 – respectively).
DN led to a significant increase in the PU at the Post1-5 min period (p < 0.001). At the Post-24h, PU decreased, but it was still significantly more significant compared to the resting values (p < 0.01). The analysis of variance revealed statistically significant effects of the main factors, i.e., Group (F = 65.054; p < 0.001), Time (F = 39.01; p < 0.001) and Time × Group interaction (F = 39.198; p < 0.001) on the PU. Based on the percentage differences in the PU between rest and post-DN calculated for each of the subjects (Figure 4A), an increase of 58% (ES = significant) and 20% (ES = moderate) in the eDN group (differences between Post1-5 min vs. Rest and Post24 h vs. Rest, respectively), with slight changes (ES = trivial) in the qDN group were observed.
Figure 4.
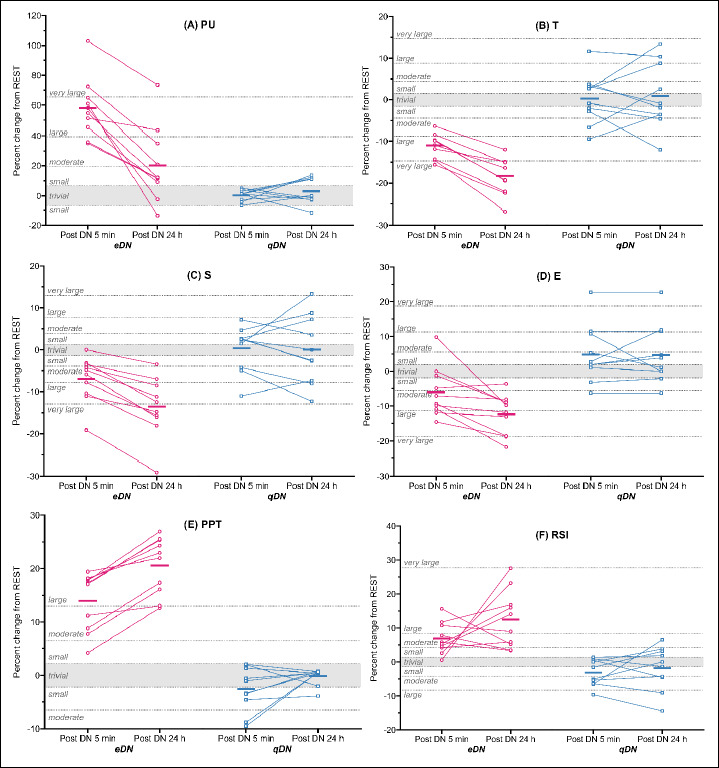
Percent changes in the analyzed indices after 1-5 min and 24 h of DN. eDN - experimental group; qDN – sham group; A: blood perfusion (PU), B: muscle tone (T), C: dynamic stiffness (S), D: elasticity, E: pressure pain threshold (PPT) and F: reactive strength index (RSI) / muscle power. Data are adjusted group means (solid dash), plus unadjusted individual percent changes. The trivial region was determined from the smallest worthwhile change for each variable (0.2 × combined between-subject baseline SD).
In the eDN group, the T decreased significantly by 11% (ES = large) and 18% (ES = very large) at the Post1-5min and Post24 period (p < 0.001), respectively, while no changes (ES = trivial) were observed in the qDN (Figure 4B). There was a statistically significant difference in the T between the studied groups at the Post1-5min (p < 0.05) and Post24h (p < 0.001), which was confirmed by a statistically significant interaction effect of Time × Group (F = 25.149; p < .001) on this variable.
The variance analysis revealed a significant effect of the main factors (Group, Time) and an interaction effect of Time × Group (F = 10.356; p < 0.001) on the S. The DN led to a decrease in the S by 7% (ES = moderate) (p < 0.05) and 14% (ES = very large) (p < 0.001) at the Post1-5min and Post24h, respectively, in the eDN group, while no changes (ES = trivial) in the S were found in the qDN group (Figure 4C).
Statistically significant effects of the main factors (Group, Time) and the Time × Group interaction (F= 15.649; p < 0.001) on the E were found. In the eDN group, a 6% (ES = moderate) and 12% (ES = large) (p < 0.001) decrease in the E at the Post1-5 min vs Rest and Post24 h vs Rest, respectively was found. A slight increase in muscle E in the qDN group (5% - ES = small) was also noted (Figure 4D). Logarithmic decrement of the muscle’s natural oscillation equates to increased muscle elasticity due to its inversely proportional relationship to muscle decrement (Cohen, 1992).
The analysis of variance also revealed statistically significant effects of the main factors (Group, Time) and their interaction Time × Group (F = 67.073; p < 0.001) on the PPT. In the eDN group, a statistically significant (p < 0.001) 14% and 21% (ES = large) increase in PPT at the Post1-5 min and Post24h, respectively, was observed. A slight decrease in PPT (-3%) at 1-5 min after DN (Figure 4E) in the qDN group was also found.
Statistically significant effects of the main factors (Group, Time) and their interaction Time × Group (F = 11.659; p < 0.001) on the RSI were revealed. In the eDN group, a statistically significant 7% (ES = moderate) (p < 0.05) and 12% (ES = large) (p < 0.01) increase in the RSI at the Post1-5min and Post24h, respectively was observed (Figure 4F). Only small (ES = small) changes in the RSI were found in the qDN group.
Discussion
Our findings confirm the effectiveness of DN in alleviating latent TrPs by enhancing blood perfusion (PU), increasing RSI and PPT, as well as improving all biomechanical properties of the gastrocnemius muscle–muscle tone and stiffness (decreased after DN) and elasticity (increased after DN). The DN-induced beneficial changes were maintained for at least 24 hours. It is especially noteworthy that DN significantly increased the muscle perfusion, reduced its tone and stiffness, and improved its elasticity immediately after using the method, i.e. for 1-5 minutes, which may suggest the possibility of using DN between exercises.
The DN effects on blood perfusion have not been studied well. Here, we observed statistically significant changes in PU, indicating that DN augmented blood perfusion in the treated area. The development of novel methods (e.g., near-infrared spectroscopy, NIRS, nuclear magnetic resonance, NMR) combined with high-fidelity measurement (spatial and temporal) mathematical and kinetic modeling approaches have better resolved the physiology of elite athletes (Joyner and Casey, 2015). The scientific literature suggests that increasing the microcirculatory response in contracting muscles is necessary to provide adequate conditions for continued exercise and recovery (Tan et al., 2021). Blood flow to contracting skeletal muscles has a remarkable ability to adapt to changes in the oxygen content in arterial blood, which directly affects the efficiency of muscle work and regeneration (Brunt et al., 2016). Researchers suggest that this increase in muscle blood flow can minimize the mismatch between oxygen demand and supply and promote metabolite clearance in the exercised muscle tissues. Locally released metabolites and ions are believed to have a dominant contribution to inducing and controlling the post-exercise blood flow response (Tan et al., 2021).
Various mechanisms of the DN-induced blood flow have been suggested, and the release of vasoactive substances, such as calcitonin gene-related peptide and substance P, upon activation of the A-δ and C fibers via the axonal reflex is one of them (Cagnie et al., 2013; Ohkubo et al., 2009). The release of vasoactive substances causes vasodilation of small vessels and improvement in blood flow. The reflex vasodilation can also be triggered by an activation of nociceptors (Simons et al., 2002), which can be stimulated by DN. Cagnie et al. (2013) also demonstrated that one session of DN augmented the blood flow and oxygen saturation in the trapezius muscle of healthy participants, and the DN-induced changes persisted throughout the 15-minute recovery period. There was no change in blood perfusion in the regions distant from the DN site (Cagnie et al., 2013). Similarly, Ohkubo et al. (2009) found an increase in oxygenation of the DN-treated region of the trapezius muscle, thus with no blood perfusion changes in the region 3 cm away from the DN site. On the contrary, Sandberg et al. (2003) found a transient significant increase in blood perfusion in the contralateral region of the DN-stimulated trapezius muscle. However, the increase was much less than in the DN-stimulated muscle and was observed only during the initial stage of the post-DN. The authors suggested that this short-lived improvement in blood perfusion in the contralateral region could have been a consequence of a sympathetic stress response, which is consistent with the previously observed short-duration increases in sympathetic nerve activity during needle manipulation (acupuncture) in healthy participants (Liu et al., 2015). It has been shown that blood circulation within TrP is impaired and leads to local hypoxia and reduced transport of the metabolic products (e.g., CO2, H+, lactate), consequently leading to muscle fatigue, also increasing the risk of injury during exercise (Bueno et al., 2022). Hence, our finding of the improved PU in the latent TrP area seems to be of significant importance for individuals training in MMA, where facilitated regeneration and less likelihood of an injury will be crucial for optimal athletic performance.
We observed a positive effect of DN on muscles T, S, and E, which has been demonstrated elsewhere (Gattie et al., 2017; Kietrys et al., 2013; Fernández-De-Las-Peñas et al., 2021). On the contrary, Baraja-Vegas et al.(2019) noticed an increase in stiffness (as measured by tensiomyography) and intramuscular edema in the gastrocnemius muscle. We found that a decrease in response to DN gastrocnemius muscle stiffness contributed to the improvement in RSI measured by a drop jump. The relationship between stiffness and drop jump performance was presented in the study by Gervasi et al. (2022). The authors demonstrated that the greater the stiffness (assessed with MyotonPro as in the current study) of the patellar and Achilles tendons and quadriceps, gastrocnemius, and rectus femoris muscles at rest, the lower the RSI and drop jump performance of young male basketball players aged 12-18 years was. The authors also observed that tendons and muscles stiffness increased with age in the adolescents and suggested that the extensive training experience of the players could have affected the level of stiffness. Nevertheless, due to the lack of an untrained control group, a separate effect of exercise training and maturation could not be assessed (Gervasi et al., 2022). In another study, Bandy et al. (2017) evaluated the effects of a single DN therapy session on the double-leg vertical jumping ability of healthy asymptomatic (no muscle pain) college students randomly assigned to an experimental (DN) or a sham group. Likewise, the DN led to a significant increase in the vertical jump height compared to the sham group. Athletic performance improvement in response to DN was observed in other studies. Haser et al. (2017) found that DN augmented maximal strength of the knee extensors in soccer players. Additionally, DN significantly increased their muscular endurance and a range of flex motion in the hip, which was maintained for four weeks after the treatment. Schneider et al. (2022) observed that applying DN to latent TrP within the gluteus medius muscle significantly increased the gluteal muscle strength immediately after the intervention in males and females aged 18-50 years not experiencing muscle pain (asymptomatic). The DN also reduced the level of electromyographic muscle activation required during force production testing. The authors concluded that latent TrPs have an adverse effect on the strength of the gluteus medius and its contraction efficiency (Schneider et al., 2022).
Many athletes and their coaches are concerned about potential DN-induced micro-damages in the skeletal muscles and nerve fibers. Hence, the therapy is often avoided, especially in the period between sports competitions. Although there are still no clear protocols for the use of DN as to the number of injections (Fernández-De-Las-Peñas and Nijs, 2019), it should be noted that even needle penetrations exceeding the norm (greater than 5 for one TrP) do not cause clinically significant damage.
Domingo et al. (2013) observed that the nerve-ending injury caused by 15 repeated punctures of the muscle of studied mice regenerated in the post-treatment period. The authors noted that the reinnervation was completed on the third-day post-DN and concluded that the repeated muscle punctures with DN did not interfere with the various stages of muscle regeneration in mice. In our study, the DN technique consisted of fever punctures (i.e., five vs fifteen used by Domingo et al. (2013) per one TrP as performed elsewhere (Albin et al., 2020; Fernández-de-las-Peñas and Dommerholt, 2018). We did not observe any signs and symptoms indicating a micro-injury, and DN had a beneficial effect on the biomechanical properties of the gastrocnemius muscles, including the improvement of RSI.
Also, the PPT increased in response to DN, which could have been a consequence of a localized contractile response that often occurs post-DN, interrupting the motor endplate noises and producing an analgesic effect (Domingo et al., 2013; Mansfield et al., 2019). There are many hypotheses describing the mechanisms of the DN-induced analgesic reactions, with another being the DN-stimulated release of endogenic opioids (Chou et al., 2014). An improvement in pain perception is one of the most commonly reported benefits of DN (Kietrys et al., 2013); however, the duration of analgesic effect varies (Baraja-Vegas et al., 2019). The beneficial changes in pain perception and pressure pain threshold confirm clinically significant effects induced by DN (Mansfield et al., 2019; Tsai et al., 2010).
With our findings of the improvement in PU, biomechanical properties of the muscles, and pressure pain threshold in response to DN, we suggest that special attention should be given to the role of microcirculation in the deactivation of pain perception and changes in the biomechanical properties of muscles (Uemoto et al., 2013).
Limitations
Although the measurement tools used in our study objectify the assessment of DN-induced changes, they have their limitations. Firstly, the measurement methods did not have reference values, making interpretation of the observed DN-induced changes challenging. Secondly, the LDF method is susceptible and requires following strict procedures. Not adhering to these may lead to misinterpretation of the observed changes. Thirdly, a placebo effect cannot be ruled out, as some individuals overly favor the DN therapy, and their expectations of the effects may impact the results. Also, we did not control for the muscle damage biomarkers (CK, LDH) to assess the subjects' muscle fatigue level. Another limitation is that the subjects were young, without evident muscle pain, with latent TrP. Therefore, the results of the study cannot be directly generalized to other groups, e.g., older or sick. Finally, our group consisted only of twenty MMA fighters.
Perspective studies
Future studies should focus on comparing the effects of DN versus other methods concerned with muscle regeneration on muscle stiffness, resting tension, or flexibility of a larger group of participants of different ages, levels of fitness, and training in various sports disciplines would be interesting to study.
Practical implications
Our results suggest that using DN during inter-exercise periods should not pose any concerns for coaches and athletes. It is common knowledge that DN is a suitable method of eliminating muscle pain, but using this method as inter-exercise regeneration is not recommended. We confirmed that a single session can change the biomechanical parameters of the muscles, directly improving sports performance, which should encourage coaches and physiotherapists to include DN in the recovery processes. Additionally, it should be noted that DN is relatively the fastest method of affecting the muscles and is important in optimizing recovery. Unfortunately, the scientific literature still lacks clear protocols for the use of DN for specific TrPs in regeneration, and we would rather use protocols related to the treatment of muscle pain(Fernández-De-Las-Peñas and Nijs, 2019).
Conclusion
We demonstrated that DN leads to an increase in blood perfusion of the treated latent TrP site and causes beneficial changes in the biomechanical properties of the gastrocnemius muscle, i.e., muscle tone, dynamic stiffness, and elasticity, increasing muscle power and, hence, athletic performance during a drop jump. In addition, DN has an immediate analgesic effect and, in our opinion, can be used as a therapy between training sessions. The DN effects were maintained at 24 h, which suggests that DN could facilitate muscle recovery in a post-exercise period of MMA athletes. MyotonPRO has been proven to be a reliable tool to measure the biomechanical properties of the gastrocnemius muscle in MMA athletes in a non-invasive way.
Acknowledgements
The experiments comply with the current laws of the country in which they were performed. The authors have no conflict of interest to declare. The datasets generated and analyzed during the current study are not publicly available, but are available from the corresponding author who was an organizer of the study.
Biographies
Robert TRYBULSKI
Employment
Medical Depart. Wojciech Korfanty Upper Silesian Academy, Katowice, Poland
Degree
PhD
Research interests
Strength training, exercise physiology, recovery in sports
E-mail: rtrybulski@o2.pl
Arkadiusz STANULA
Employment
Laboratory of Sport Performance Analysis, Inst. of Sport Sciences, The Jerzy Kukuczka Academy of PE in Katowice, Poland
Degree
Professor
Research interests
Statistical methods in sports, training theory, exercise physiology
E-mail: a.stanula@awf.katowice.pl
Aleksandra ŻEBROWSKA
Employment
Depart. of Physiology, School of Physiological-Medical Sciences, The Jerzy Kukuczka Academy of PE in Katowice, Poland
Degree
Professor
Research interests
Training theory, exercise physiology, kinesiology in sports
E-mail: a.zebrowska@awf.katowice.pl
Mieszko PODLEŚNY
Employment
“Salus” Health Center, Słupsk, Poland
Degree
Msc
Research interests
Sports medicine, physiotherapy in sports
E-mail: mieszko.podlesny@gmail.com
Barbara HALL
Employment
Depart. of Physiology, School of Physiological-Medical Sciences, The Jerzy Kukuczka Academy of PE in Katowice, Poland
Degree
PhD
Research interests
Training theory, exercise physiology, kinesiology in sports
E-mail: b.hall@awf.katowice.pl
References
- Albin S. R., Koppenhaver S. L., MacDonald C. W., Capoccia S., Ngo D., Phippen S., Pineda R., Wendlandt A., Hoffman L. R. (2020) The effect of dry needling on gastrocnemius muscle stiffness and strength in participants with latent trigger points. Journal of Electromyography and Kinesiology 55, 102479. https://doi.org/10.1016/J.JELEKIN.2020.102479 10.1016/J.JELEKIN.2020.102479 [DOI] [PubMed] [Google Scholar]
- Albracht K., Arampatzis A. (2013) Exercise-induced changes in triceps surae tendon stiffness and muscle strength affect human running economy. European Journal of Applied Physiology 113(6), 1605-1615. https://doi.org/10.1007/S00421-012-2585-4 10.1007/S00421-012-2585-4 [DOI] [PubMed] [Google Scholar]
- Andrade A., Flores M. A., Andreato L. V., Coimbra D. R. (2019) Physical and training characteristics of mixed martial arts athletes: Systematic review. Strength and Conditioning Journal 41(1), 51-63. https://doi.org/10.1519/SSC.0000000000000410 10.1519/SSC.0000000000000410 [DOI] [Google Scholar]
- Ballyns J. J., Turo D., Otto P., Shah J. P., Hammond J., Gebreab T., Gerber L. H., Sikdar S. (2012) Office-based elastographic technique for quantifying mechanical properties of skeletal muscle. Journal of Ultrasound in Medicine : Official Journal of the American Institute of Ultrasound in Medicine 31(8), 1209-1219. https://doi.org/10.7863/JUM.2012.31.8.1209 10.7863/JUM.2012.31.8.1209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandy W. D., Nelson R., Beamer L. (2017) Comparison of dry needling vs. Sham on the performance of vertical jump. International Journal of Sports Physical Therapy 12(5), 747. https://doi.org/10.26603/ijspt20170747 10.26603/ijspt20170747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baraja-Vegas L., Martín-Rodríguez S., Piqueras-Sanchiz F., Faundez-Aguilera J., Bautista I. J., Barrios C., Fernández-De-Las-Peñas C. (2019) Localization of Muscle Edema and Changes on Muscle Contractility After Dry Needling of Latent Trigger Points in the Gastrocnemius Muscle. Pain Medicine (Malden, Mass.) 20(7), 1387-1394. https://doi.org/10.1093/PM/PNY306 10.1093/PM/PNY306 [DOI] [PubMed] [Google Scholar]
- Bartsch K., Brandl A., Weber P., Wilke J., Bensamoun S. F., Bauermeister W., Klingler W., Schleip R. (2023) Assessing reliability and validity of different stiffness measurement tools on a multi-layered phantom tissue model. Scientific Reports 13(1), 1-10. https://doi.org/10.1038/s41598-023-27742-w 10.1038/s41598-023-27742-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyles R., Fowler R., Ramsey D., Burrows E. (2015) Effectiveness of trigger point dry needling for multiple body regions: a systematic review. The Journal of Manual & Manipulative Therapy 23(5), 276-292. https://doi.org/10.1179/2042618615Y.0000000014 10.1179/2042618615Y.0000000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite F. A., Walters J. L., Li L. S. K., Moseley G. L., Williams M. T., McEvoy M. P. (2019) Blinding Strategies in Dry Needling Trials: Systematic Review and Meta-Analysis. Physical Therapy 99(11), 1461-1480. https://doi.org/10.1093/PTJ/PZZ111 10.1093/PTJ/PZZ111 [DOI] [PubMed] [Google Scholar]
- Brunt V. E., Howard M. J., Francisco M. A., Ely B. R., Minson C. T. (2016) Passive heat therapy improves endothelial function, arterial stiffness and blood pressure in sedentary humans. Journal of Physiology 594(18), 5329-5342. https://doi.org/10.1113/JP272453 10.1113/JP272453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueno J. C. A., Faro H., Lenetsky S., Gonçalves A. F., Dias S. B. C. D., Ribeiro A. L. B., da Silva B. V. C., Filho C. A. C., de Vasconcelos B. M., Serrão J. C., Andrade A., Souza-Junior T. P., Claudino J. G. (2022) Exploratory Systematic Review of Mixed Martial Arts: An Overview of Performance of Importance Factors with over 20,000 Athletes. Sports (Basel, Switzerland) 10(6) https://doi.org/10.3390/sports10060080 10.3390/sports10060080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagnie B., Dewitte V., Barbe T., Timmermans F., Delrue N., Meeus M. (2013) Physiologic effects of dry needling. Current Pain and Headache Reports 17(8) https://doi.org/10.1007/S11916-013-0348-5 10.1007/S11916-013-0348-5 [DOI] [PubMed] [Google Scholar]
- Chen G., Wu J., Chen G., Lu Y., Ren W., Xu W., Xu X., Wu Z., Guan Y., Zheng Y., Qiu B. (2019) Reliability of a portable device for quantifying tone and stiffness of quadriceps femoris and patellar tendon at different knee flexion angles. Plos One 14(7) https://doi.org/10.1371/JOURNAL.PONE.0220521 10.1371/JOURNAL.PONE.0220521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou L. W., Hsieh Y. L., Kuan T. S., Hong C. Z. (2014) Needling therapy for myofascial pain: recommended technique with multiple rapid needle insertion. BioMedicine 4(2), 39-46. https://doi.org/10.7603/S40681-014-0013-2 10.7603/S40681-014-0013-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1992) Statistical Power Analysis. Current Directions in Psychological Science 1(3), 98-101. https://doi.org/10.1111/1467-8721.EP10768783 10.1111/1467-8721.EP10768783 [DOI] [Google Scholar]
- Ding C. L., Ma Y. T., Huang Q. M., Liu Q. G., Zhao J. M. (2018) Effect of Dry Needling Stimulation of Myofascial Trigger Point on Sample Entropy of Electromyography of Gastrocnemius Injured Site in Rats. Acupuncture Research 43(2), 127-132. https://doi.org/10.13702/j.1000-0607.170155 10.13702/j.1000-0607.170155 [DOI] [PubMed] [Google Scholar]
- Domingo A., Mayoral O., Monterde S., Santafé M. M. (2013) Neuromuscular damage and repair after dry needling in mice. Evidence-Based Complementary and Alternative Medicine. https://doi.org/10.1155/2013/260806 10.1155/2013/260806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dos Santos W. Y. H., Aidar F. J., de Matos D. G., Van den Tillaar R., Marçal A. C., Lobo L. F., Marcucci-Barbosa L. S., Machado S. da C., de Almeida-Neto P. F., Garrido N. D., Reis V. M., Vieira É. L. M., Cabral B. G. de A. T., Vilaça-Alves J., Nunes-Silva A., da Silva, Júnior W. M. (2021) Physiological and Biochemical Evaluation of Different Types of Recovery in National Level Paralympic Powerlifting. International Journal of Environmental Research and Public Health 18(10). https://doi.org/10.3390/IJERPH18105155 10.3390/IJERPH18105155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enoka R. M., Duchateau J. (2008) Muscle fatigue: what, why and how it influences muscle function. The Journal of Physiology 586(Pt 1), 11. https://doi.org/10.1113/JPHYSIOL.2007.139477 10.1113/JPHYSIOL.2007.139477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A. G., Buchner A. (2007) G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 39(2), 175-191. https://doi.org/10.3758/BF03193146 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- Fernández-de-las-Peñas C., Dommerholt J. (2018) International Consensus on Diagnostic Criteria and Clinical Considerations of Myofascial Trigger Points: A Delphi Study. Pain Medicine 19(1), 142-150. https://doi.org/10.1093/PM/PNX207 10.1093/PM/PNX207 [DOI] [PubMed] [Google Scholar]
- Fernández-De-Las-Peñas C., Nijs J. (2019) Trigger point dry needling for the treatment of myofascial pain syndrome: current perspectives within a pain neuroscience paradigm. Journal of Pain Research 12, 1899-1911. https://doi.org/10.2147/JPR.S154728 10.2147/JPR.S154728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-De-Las-Peñas C., Plaza-Manzano G., Sanchez-Infante J., Gómez-Chiguano G. F., Cleland J. A., Arias-Buría J. L., López-De-Uralde-Villanueva I., Navarro-Santana M. J. (2021) Is Dry Needling Effective When Combined with Other Therapies for Myofascial Trigger Points Associated with Neck Pain Symptoms? A Systematic Review and Meta-Analysis. Pain Research and Management. https://doi.org/10.1155/2021/8836427 10.1155/2021/8836427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Lao C., Cantarero-Villanueva I., Fernández-De-Las-Peñas C., Del-Moral-Ávila R., Arendt-Nielsen L., Arroyo-Morales M. (2010) Myofascial trigger points in neck and shoulder muscles and widespread pressure pain hypersensitivtiy in patients with postmastectomy pain: evidence of peripheral and central sensitization. The Clinical Journal of Pain 26(9), 798-806. https://doi.org/10.1097/AJP.0B013E3181F18C36 10.1097/AJP.0B013E3181F18C36 [DOI] [PubMed] [Google Scholar]
- Gattie E., Cleland J. A., Snodgrass S. (2017) The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: A systematic review and meta-analysis. In Journal of Orthopaedic and Sports Physical Therapy 47(3), 133-149. https://doi.org/10.2519/jospt.2017.7096 10.2519/jospt.2017.7096 [DOI] [PubMed] [Google Scholar]
- Gervasi M., Benelli P., Venerandi R., Fernández-Peña E. (2022) Relationship between Muscle-Tendon Stiffness and Drop Jump Performance in Young Male Basketball Players during Developmental Stages. International Journal of Environmental Research and Public Health 19(24), 17017. https://doi.org/10.3390/IJERPH192417017 10.3390/IJERPH192417017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen A. H., Nielsen J. J., Saltin B., Hellsten Y. (2010) Exercise training normalizes skeletal muscle vascular endothelial growth factor levels in patients with essential hypertension. Journal of Hypertension 28(6), 1176-1185. https://doi.org/10.1097/HJH.0B013E3283379120 10.1097/HJH.0B013E3283379120 [DOI] [PubMed] [Google Scholar]
- Haser C., Stöggl T., Kriner M., Mikoleit J., Wolfahrt B., Scherr J., Halle M., Pfab F. (2017) Effect of Dry Needling on Thigh Muscle Strength and Hip Flexion in Elite Soccer Players. Medicine and Science in Sports and Exercise 49(2), 378-383. https://doi.org/10.1249/MSS.0000000000001111 10.1249/MSS.0000000000001111 [DOI] [PubMed] [Google Scholar]
- Healy R., Kenny I. C., Harrison A. J. (2018) Reactive Strength Index: A Poor Indicator of Reactive Strength? International Journal of Sports Physiology and Performance 13(6), 802-809. https://doi.org/10.1123/IJSPP.2017-0511 10.1123/IJSPP.2017-0511 [DOI] [PubMed] [Google Scholar]
- James L. P., Haff G. G., Kelly V. G., Beckman E. M. (2016) Towards a Determination of the Physiological Characteristics Distinguishing Successful Mixed Martial Arts Athletes: A Systematic Review of Combat Sport Literature. Sports Medicine (Auckland, N.Z.) 46(10), 1525-1551. https://doi.org/10.1007/S40279-016-0493-1 10.1007/S40279-016-0493-1 [DOI] [PubMed] [Google Scholar]
- Jiménez-Sánchez C., Ortiz-Lucas M., Bravo-Esteban E., Mayoral-Del Moral O., Herrero-Gállego P., Gómez-Soriano J. (2018) Myotonometry as a measure to detect myofascial trigger points: an inter-rater reliability study. Physiological Measurement 39(11) https://doi.org/10.1088/1361-6579/AAE9AA 10.1088/1361-6579/AAE9AA [DOI] [PubMed] [Google Scholar]
- Joyner M. J., Casey D. P. (2015) Regulation of increased blood flow (hyperemia) to muscles during exercise: a hierarchy of competing physiological needs. Physiological Reviews 95(2), 549-601. https://doi.org/10.1152/PHYSREV.00035.2013 10.1152/PHYSREV.00035.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J. P., Koppenhaver S. L., Michener L. A., Kolber M. J., Cleland J. A. (2021) Immediate decrease of muscle biomechanical stiffness following dry needling in asymptomatic participants. Journal of Bodywork and Movement Therapies 27, 605-611. https://doi.org/10.1016/j.jbmt.2021.04.014 10.1016/j.jbmt.2021.04.014 [DOI] [PubMed] [Google Scholar]
- Kelly J. P., Koppenhaver S. L., Michener L. A., Proulx L., Bisagni F., Cleland J. A. (2018) Characterization of tissue stiffness of the infraspinatus, erector spinae, and gastrocnemius muscle using ultrasound shear wave elastography and superficial mechanical deformation. Journal of Electromyography and Kinesiology : Official Journal of the International Society of Electrophysiological Kinesiology 38, 73-80. https://doi.org/10.1016/J.JELEKIN.2017.11.001 10.1016/J.JELEKIN.2017.11.001 [DOI] [PubMed] [Google Scholar]
- Kietrys D. M., Palombaro K. M., Azzaretto E., Hubler R., Schaller B., Schlussel J. M., Tucker M. (2013) Effectiveness of dry needling for upper-quarter myofascial pain: A systematic review and meta-analysis. Journal of Orthopaedic and Sports Physical Therapy 43(9), 620-634. https://doi.org/10.2519/jospt.2013.4668 10.2519/jospt.2013.4668 [DOI] [PubMed] [Google Scholar]
- Kisilewicz A., Madeleine P., Ignasiak Z., Ciszek B., Kawczynski A., Larsen R. G. (2020) Eccentric Exercise Reduces Upper Trapezius Muscle Stiffness Assessed by Shear Wave Elastography and Myotonometry. Frontiers in Bioengineering and Biotechnology 8. https://doi.org/10.3389/FBIOE.2020.00928 10.3389/FBIOE.2020.00928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Tilp M., Mehmeti L., Mahnič N., Seiberl W., Paternoster F. K. (2023) The Relationship Between Lower Limb Passive Muscle and Tendon Compression Stiffness and Oxygen Cost During Running. Journal of Sports Science & Medicine 22(1), 28-35. https://doi.org/10.52082/JSSM.2023.28 10.52082/JSSM.2023.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvandal P., Landsverk S. A., Bernjak A., Stefanovska A., Kvernmo H. D., Kirkebøen K. A. (2006a) Low-frequency oscillations of the laser Doppler perfusion signal in human skin. Microvascular Research 72(3), 120-127. https://doi.org/10.1016/J.MVR.2006.05.006 10.1016/J.MVR.2006.05.006 [DOI] [PubMed] [Google Scholar]
- Liana R., Chudański M., Katedra I. P. (2009) Standarisation of laser Doppler flowmetry - own standards. Clinical Diabetology 10(2), 58-64. https://journals.viamedica.pl/clinical_diabetology/article/view/8426 [Google Scholar]
- Liu L., Huang Q. M., Liu Q. G., Ye G., Bo C. Z., Chen M. J., Li P. (2015) Effectiveness of dry needling for myofascial trigger points associated with neck and shoulder pain: A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation 96(5), 944-955. https://doi.org/10.1016/j.apmr.2014.12.015 10.1016/j.apmr.2014.12.015 [DOI] [PubMed] [Google Scholar]
- Mansfield C. J., Vanetten L., Willy R., Di Stasi S. P. P. D. O., Magnussen R., Briggs M. (2019) The Effects of Needling Therapies on Muscle Force Production: A Systematic Review and Meta-analysis. The Journal of Orthopaedic and Sports Physical Therapy 49(3), 154-170. https://doi.org/10.2519/JOSPT.2019.8270 10.2519/JOSPT.2019.8270 [DOI] [PubMed] [Google Scholar]
- Markwick W. J., Bird S. P., Tufano J. J., Seitz L. B., Haff G. G. (2015) The intraday reliability of the Reactive Strength Index calculated from a drop jump in professional men’s basketball. International Journal of Sports Physiology and Performance 10(4), 482-488. https://doi.org/10.1123/IJSPP.2014-0265 10.1123/IJSPP.2014-0265 [DOI] [PubMed] [Google Scholar]
- Martín-Pintado-Zugasti A., Mayoral del Moral O., Gerwin R. D., Fernández-Carnero J. (2018) Post-needling soreness after myofascial trigger point dry needling: Current status and future research. Journal of Bodywork and Movement Therapies 22(4), 941-946. https://doi.org/10.1016/J.JBMT.2018.01.003 10.1016/J.JBMT.2018.01.003 [DOI] [PubMed] [Google Scholar]
- Melo A. S. C., Cruz E. B., Vilas-Boas J. P., Sousa A. S. P. (2022) Scapular Dynamic Muscular Stiffness Assessed through Myotonometry: A Narrative Review. Sensors (Basel, Switzerland) 22(7). https://doi.org/10.3390/S22072565 10.3390/S22072565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohkubo M., Niwayama M., Murase N., Osada T., Kime R., Kurosawa Y., Sakamoto A., Katsumura T., Hamaoka T. (2009) Local increase in trapezius muscle oxygenation during and after acupuncture. Dynamic Medicine 8(1). https://doi.org/10.1186/1476-5918-8-2 10.1186/1476-5918-8-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park G., Kim C. W., Park S. B., Kim M. J., Jang S. H. (2011) Reliability and Usefulness of the Pressure Pain Threshold Measurement in Patients with Myofascial Pain. Annals of Rehabilitation Medicine 35(3), 412. https://doi.org/10.5535/ARM.2011.35.3.412 10.5535/ARM.2011.35.3.412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivers W. E., Garrigues D., Graciosa J., Harden R. N. (2015) Signs and Symptoms of Myofascial Pain: An International Survey of Pain Management Providers and Proposed Preliminary Set of Diagnostic Criteria. Pain Medicine 16(9), 1794-1805. https://doi.org/10.1111/PME.12780 10.1111/PME.12780 [DOI] [PubMed] [Google Scholar]
- Rodrigues L. M., Rocha C., Ferreira H., Silva H. (2019) Different lasers reveal different skin microcirculatory flowmotion - data from the wavelet transform analysis of human hindlimb perfusion. Scientific Reports 9(1). https://doi.org/10.1038/S41598-019-53213-2 10.1038/S41598-019-53213-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg M., Larsson B., Lindberg L. G., Gerdle B. (2005) Different patterns of blood flow response in the trapezius muscle following needle stimulation (acupuncture) between healthy subjects and patients with fibromyalgia and work-related trapezius myalgia. European Journal of Pain (London, England) 9(5), 497. https://doi.org/10.1016/J.EJPAIN.2004.11.002 10.1016/J.EJPAIN.2004.11.002 [DOI] [PubMed] [Google Scholar]
- Sandberg M., Lundeberg T., Lindberg L. G., Gerdle B. (2003) Effects of acupuncture on skin and muscle blood flow in healthy subjects. European Journal of Applied Physiology 90(1-2), 114-119. https://doi.org/10.1007/S00421-003-0825-3 10.1007/S00421-003-0825-3 [DOI] [PubMed] [Google Scholar]
- Schneider E., Moore E. S., Stanborough R., Slaven E. (2022) Effects of Trigger Point Dry Needling on Strength Measurements and Activation Levels of the Gluteus Medius: A Quasi-Experimental Randomized Control Study. International Journal of Sports Physical Therapy 17(7). https://doi.org/10.26603/001C.55536 10.26603/001C.55536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons D. G., Hong C. Z., Simons L. S. (2002) Endplate potentials are common to midfiber myofacial trigger points. American Journal of Physical Medicine and Rehabilitation 81(3), 212-222. https://doi.org/10.1097/00002060-200203000-00010 10.1097/00002060-200203000-00010 [DOI] [PubMed] [Google Scholar]
- Suzuki H., Tahara S., Mitsuda M., Izumi H., Ikeda S., Seki K., Nishida N., Funaba M., Imajo Y., Yukata K., Sakai T. (2022) Current Concept of Quantitative Sensory Testing and Pressure Pain Threshold in Neck/Shoulder and Low Back Pain. Healthcare 10(8). https://doi.org/10.3390/HEALTHCARE10081485 10.3390/HEALTHCARE10081485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szyguła R., Wierzbicka M., Sondel G. (2020) Influence of 8-Week Aerobic Training on the Skin Microcirculation in Patients with Ischaemic Heart Disease. Journal of Aging Research. https://doi.org/10.1155/2020/4602067 10.1155/2020/4602067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan Q., Wang Y., Li Z., Wang D., Lam W. K., Wong D. W. C., Peng Y., Zhang G., Zhang M. (2021) Spectral Analysis of Muscle Hemodynamic Responses in Post-Exercise Recovery Based on Near-Infrared Spectroscopy. Sensors (Basel, Switzerland) 21(9). https://doi.org/10.3390/S21093072 10.3390/S21093072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai C. T., Hsieh L. F., Kuan T. S., Kao M. J., Chou L. W., Hong C. Z. (2010) Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. American Journal of Physical Medicine and Rehabilitation 89(2), 133-140. https://doi.org/10.1097/PHM.0b013e3181a5b1bc 10.1097/PHM.0b013e3181a5b1bc [DOI] [PubMed] [Google Scholar]
- Uemoto L., Nascimento De Azevedo R., Almeida Alfaya T., Nunes Jardim Reis R., Depes De Gouvêa C. V., Cavalcanti Garcia M. A. (2013) Myofascial trigger point therapy: laser therapy and dry needling. Current Pain and Headache Reports 17(9). https://doi.org/10.1007/S11916-013-0357-4 10.1007/S11916-013-0357-4 [DOI] [PubMed] [Google Scholar]
- Venegas-Carro M., Kramer A., Moreno-Villanueva M., Gruber M. (2022) Test-Retest Reliability and Sensitivity of Common Strength and Power Tests over a Period of 9 Weeks. Sports (Basel, Switzerland) 10(11). https://doi.org/10.3390/SPORTS10110171 10.3390/SPORTS10110171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarei H., Bervis S., Piroozi S., Motealleh A. (2020) Added Value of Gluteus Medius and Quadratus Lumborum Dry Needling in Improving Knee Pain and Function in Female Athletes With Patellofemoral Pain Syndrome: A Randomized Clinical Trial. Archives of Physical Medicine and Rehabilitation 101(2), 265-274. https://doi.org/10.1016/J.APMR.2019.07.009 10.1016/J.APMR.2019.07.009 [DOI] [PubMed] [Google Scholar]
- Zebrowska A., Trybulski R., Roczniok R., Marcol W. (2019) Effect of Physical Methods of Lymphatic Drainage on Postexercise Recovery of Mixed Martial Arts Athletes. Clinical Journal of Sport Medicine : Official Journal of the Canadian Academy of Sport Medicine 29(1), 49-56. https://doi.org/10.1097/JSM.0000000000000485 10.1097/JSM.0000000000000485 [DOI] [PubMed] [Google Scholar]


