Abstract
Kounis syndrome is an acute coronary syndrome (ACS) caused by an allergic reaction that almost always occurs immediately and simultaneously with allergic symptoms. We present a case of Kounis syndrome type III that developed after complete resolution of contrast-induced anaphylaxis in a 60-year-old man with a coronary stent placed in the proximal left anterior descending (LAD) artery branch for ischemic heart disease. Contrast-enhanced computed tomography revealed anaphylactic shock. Symptoms quickly improved with intramuscular adrenaline injection; however, chest pain appeared after approximately 30 min. ECG revealed ST-wave elevation in the precordial leads. Coronary angiography revealed acute stent thrombosis with total occlusion of the proximal LAD, and percutaneous coronary angioplasty was performed. We diagnosed Kounis syndrome based on the allergic symptoms and ACS. Because some cases of Kounis syndrome develop after anaphylactic symptoms have resolved, it is advisable to follow-up patients with allergic symptoms and pay attention to chest symptoms and ECG changes, especially when they have a history of noted or treated coronary artery disease.
Keywords: anaphylactic shock, contrast-induced anaphylaxis, allergic reaction, iodine contrast media, kounis syndrome, extremely late stent thrombosis, iodinated contrast, anaphylax, kounis case study
Introduction
Acute coronary syndrome (ACS) occurs in conjunction with an allergic reaction in Kounis syndrome [1]. This syndrome is categorized into three types [1,2]: Type I, which is caused by coronary artery spasms without a history of coronary artery disease; Type II, where there is a history of coronary artery disease and spasms lead to plaque erosion or rupture; and Type III, which is caused by thrombosis within a coronary artery stent. While cases of Kounis syndrome caused by contrast agents typically present with ACS immediately following an allergic reaction, we present a case in which Type III Kounis syndrome developed after the complete resolution of anaphylactic symptoms induced by a contrast agent [3,4].
Case presentation
A 60-year-old man with a coronary stent placed in the left anterior descending artery 17 years prior was diagnosed with an aortic aneurysm and underwent a contrast-enhanced computed tomography (CT) scan for evaluation in an outpatient setting. Immediately after the administration of the contrast agent iopamidol, the patient experienced a drop in blood pressure to approximately 70 mmHg and difficulty breathing. Anaphylactic shock was diagnosed, and the patient was treated with an intramuscular injection of adrenaline (0.5 mg) and a rapid infusion of saline. A few minutes later, his vital signs recovered and his symptoms completely disappeared. Although his respiratory and circulatory systems were stable, approximately 30 min after the disappearance of anaphylactic shock symptoms, he suddenly complained of chest discomfort. Electrocardiography showed ST changes (Figure 1), and echocardiography revealed reduced wall motion from the anterior septum to the apex. He was diagnosed with ischemic heart disease and treated with one sublingual tablet of nitropen (nitroglycerin) and a continuous administration of noradrenaline at 0.1 γ to treat his low blood pressure (79/49 mmHg). Emergency coronary catheterization revealed a complete occlusion of the proximal part of the stent in the left anterior descending artery (Figure 2). A percutaneous coronary intervention was performed, and the patient was admitted to the ICU. His condition improved, and he was transferred from the ICU to a general ward; he was then discharged on the 14th day.
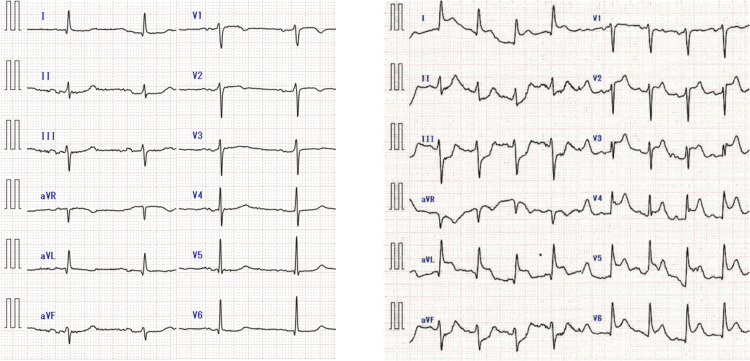
Figure 1. Electrocardiogram (ECG) changes.
A 12-lead ECG in the absence of chest symptoms after anaphylaxis shows no ST change, while a 12-lead ECG after the appearance of chest symptoms shows ST elevation at I, aVL, and V2-6.
Figure 2. Coronary angiography.
Coronary angiography (caudal and right anterior oblique view) revealing left anterior descending (LAD) artery occlusion due to stent thrombosis.
Discussion
Kounis syndrome is a condition in which allergic reactions occur simultaneously with ACS. Mediators released from mast cells during allergic reactions are believed to cause coronary vasoconstriction and acute myocardial infarction. First reported in 1991 by Kounis, it is also referred to as allergic angina [5]. Exposure to various substances such as drugs (antibiotics and nonsteroidal anti-inflammatories), contrast agents, bee stings, and certain foods can trigger mast cell degranulation and induce an allergic reaction, followed by the release of various inflammatory mediators. Kounis syndrome, which is associated with allergic reactions, is caused by the action of these mediators and cytokines, leading to coronary artery spasm, destabilization of coronary artery plaques, rupture, and thrombus formation, ultimately causing coronary blood flow disturbances [6].
Kounis syndrome is classified into three types. Type I occurs in patients with normal coronary arteries where the acute release of inflammatory mediators induces coronary artery spasms. In Type II, spasms in the coronary artery adjacent to an existing atherosclerotic lesion lead to plaque erosion or rupture. Type III is associated with coronary stent thrombosis in patients undergoing stenting. As the acute release of inflammatory mediators induces coronary artery spasms, Types I and II Kounis syndrome, which are primarily caused by coronary spasms, are likely to present with ACS almost simultaneously with allergic symptoms.
Kounis syndrome incidence is often underestimated because it is rare, meaning its actual incidence may be higher than that currently reported. We searched the literature on PubMed up to October 31, 2023, to investigate the relationship between the time from contrast agent administration to the onset of allergic symptoms and from the onset of allergic symptoms to the appearance of chest symptoms suggestive of ACS (Table 1).
Table 1. Summary of reports of contrast agent-related Kounis syndrome.
Delay①: From contrast administration to onset of allergic symptoms. Delay②: From the onset of anaphylaxis to the appearance of ACS-suspected symptoms.
| Authors | Age/Sex | Delay① | Delay② | KS type | Cardiac arrest | Region |
| Wong et al., 2023 [3] | 56/M | Immediately | Immediately | Ⅰ | no | Singapore |
| Prisco et al., 2020 [4] | 53/F | Immediately | Immediately | Ⅰ | yes | USA |
| Xie et al., 2019 [6] | 72/F | 20 min | nr | nr | no | China |
| Xie et al., 2019 [6] | 78/M | 20 min | nr | Ⅱ | no | China |
| Choudhry et al., 2019 [7] | 30/M | Immediately | Immediately, 16 hr | Ⅰ | no | USA |
| Maadarani et al., 2020 [8] | 60/M | 20 min | Immediately, 7 hr | Ⅲ | no | Kuwait |
| Singer et al., 2009 [9] | 57/M | 2 min | Immediately | nr | yes | USA |
| Dauvergne et al., 2009 [10] | 79/M | Immediately | Immediately | Ⅱ | no | Chile |
| Kogias et al., 2010 [11] | 48/M | 10 min | Immediately | Ⅲ | no | Greece |
| Park et al., 2010 [12] | 54/M | 10 min | Immediately | Ⅱ | no | Korea |
| Kocabay et al., 2012 [13] | 51/M | 10 min | Immediately | Ⅱ | no | Turkey |
| Yanagawa et al., 2012 [14] | 62/M | During infusion | Immediately | Ⅰ | yes | Japan |
| Zlojtro et al., 2013 [15] | 46/F | 10 min | Immediately | Ⅱ | no | Croatia |
| Xu et al., 2013 [16] | 71/M | 1 h | Immediately | Ⅰ | no | China |
| Benedetto et al., 2015 [17] | 83/F | During infusion | Immediately | Ⅰ | no | Netherlands |
| Akita et al., 2016 [18] | 70/M | Immediately | Immediately | Ⅰ | yes | Japan |
| Oh et al., 2016 [19] | 74/M | Immediately | Immediately | Ⅰ | yes | Korea |
| Demoulin et al., 2017 [20] | 81/M | Several min | Immediately | Ⅱ | yes | France |
| Tripolino et al., 2018 [21] | 47/M | 30 min | Immediately | Ⅲ | no | Italy |
| Bhaskaran et al., 2018 [22] | 83/M | Immediately | Immediately | Ⅱ | no | Australia |
| Abusnina et al., 2019 [23] | 53/F | Several min | Immediately | Ⅰ | no | USA |
| Dorniak et al., 2019 [24] | 59/F | Within min | Within min | Ⅰ | no | Poland |
| Shibuya et al., 2019 [25] | 60/M | Immediately | Immediately | Ⅱ | no | Japan |
| Tanaka et al., 2019 [26] | 78/M | Immediately | Immediately | Ⅱ | no | Japan |
| Chien et al., 2019 [27] | 81/F | 15 min | Immediately | nr | yes | Taiwan |
| Biagioni et al., 2020 [28] | 45/M | 2 min | Immediately | Ⅰ | yes | Italy |
| Portero-Portaz et al., 2020 [29] | 72/M | Immediately | Several min | Ⅲ | no | Spain |
| Elzeneini et al., 2020 [30] | 76/M | Within min | Immediately | Ⅱ | yes | USA |
| Kangzheng et al., 2021 [31] | 59/M | During infusion | nr | Ⅱ | no | China |
| Lee Chuy et al., 2022 [32] | 59/M | Immediately | Immediately | Ⅰ | no | USA |
| Sagalov et al., 2023 [33] | 51/M | Shortly after | Immediately | Ⅰ | no | USA |
| Singh et al., 2023 [34] | 79/F | Immediately | nr | Ⅱ | no | USA |
| Our case | 76/M | During infusion | 37 min | Ⅲ | no | Japan |
There have been 32 reports of contrast agent-related Kounis syndrome. Except for one case reported by Choudhry et al., chest symptoms occurred almost simultaneously with allergic symptoms or anaphylaxis. Choudhry et al. reported the case of a 35-year-old man who developed allergic symptoms (urticaria, chest tightness, and laryngeal spasm) after the administration of the contrast agent gadobenate dimeglumine [7]. Although the allergic symptoms temporarily improved, severe chest pain reappeared 16 hours later, and the troponin test was positive; however, echocardiography showed no local wall motion abnormalities, and angiography did not reveal any coronary artery stenosis. This was an atypical case of Type I Kounis syndrome.
Our case is a classic example of Type III Kounis syndrome, in which symptoms of anaphylaxis caused by the contrast agent initially completely disappeared; however, 30 min later, complete occlusion near the coronary artery stent was observed. According to previous reports, Kounis syndrome caused by contrast agents typically occurs almost simultaneously with allergic reactions immediately after administration of the contrast agent. Our case is the first reported instance in which typical Type III Kounis syndrome developed after the complete disappearance of allergic symptoms caused by a contrast agent.
Key inflammatory mediators released from mast cells such as histamine, leukotrienes, and prostaglandins initiate an amplifying cascade of blood coagulation, subsequently promoting thrombosis within the blood vessels [1]. In cases where a coronary artery stent is in place, the stent itself, drugs eluted from the stent, and administered antiplatelet drugs can chronically induce an inflammatory state in the stent intima, making it prone to stent thrombosis [35,36]. Coronary artery stent thrombosis, which progresses owing to inflammatory mediators, increases over time, and Kounis syndrome develops when the stent becomes completely occluded. This means that the onset of Type III Kounis syndrome may not occur simultaneously with allergic symptoms but can develop as a delayed reaction.
Maadarani et al. reported the case of a 60-year-old male with a drug-eluting stent who experienced severe chest pain, ST-segment elevation, and decreased wall motion 20 min after administration of a contrast agent [8]. Although thrombolytic therapy temporarily resolved the chest pain and ST elevation, a few hours later the patient presented with severe chest pain, decreased left ventricular wall motion, and extensive ST elevation due to acute stent thrombosis with complete occlusion of the proximal part of the left anterior descending artery. This suggests that thrombus formation driven by the released inflammatory mediators progressed and led to complete stent occlusion hours later. In cases of coronary artery stent implantation, even after the complete disappearance of chest symptoms, attention should be paid to the potential onset of Kounis syndrome.
Conclusions
Kounis syndrome, which is caused by contrast agents, induces ACS almost simultaneously with an allergic reaction. In this case, we report the delayed onset of Type III Kounis syndrome after the allergic symptoms caused by the contrast agent had completely disappeared. Patients with allergic symptoms to contrast agents should be monitored for Kounis syndrome, especially in cases where a coronary stent is in place because delayed Type III Kounis syndrome can occur due to stent thrombosis even after the disappearance of allergic symptoms. Reports on Kounis syndrome induced by contrast agents are limited, and further investigation is necessary to better understand this condition.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Ryuichiro Okuda, Shu Utsumi, Hideki Tanaka, Tatsuo Takama, Yasuyuki Kakihana
Acquisition, analysis, or interpretation of data: Ryuichiro Okuda, Shu Utsumi, Hideki Tanaka, Tatsuo Takama, Yasuyuki Kakihana
Drafting of the manuscript: Ryuichiro Okuda, Shu Utsumi, Hideki Tanaka, Tatsuo Takama, Yasuyuki Kakihana
Critical review of the manuscript for important intellectual content: Ryuichiro Okuda, Shu Utsumi, Hideki Tanaka, Tatsuo Takama, Yasuyuki Kakihana
Supervision: Shu Utsumi, Yasuyuki Kakihana
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Kounis syndrome: an update on epidemiology, pathogenesis, diagnosis and therapeutic management. Kounis NG. Clin Chem Lab Med. 2016;54:1545–1559. doi: 10.1515/cclm-2016-0010. [DOI] [PubMed] [Google Scholar]
- 2.A new classification of Kounis syndrome. Biteker M. Int J Cardiol. 2010;145:553. doi: 10.1016/j.ijcard.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 3.Kounis syndrome after administration of Iopromide-based contrast. Wong SW, Ahmad Hatib A. Acta Cardiol Sin. 2023;39:667–669. doi: 10.6515/ACS.202307_39(4).20230416B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kounis syndrome leading to cardiac arrest after iodinated contrast exposure. Prisco AR, Allen J, Gutierrez A, Zanotto A, Yannopoulos D, Markowitz J, Bartos JA. JACC Case Rep. 2020;2:626–629. doi: 10.1016/j.jaccas.2019.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Histamine-induced coronary artery spasm: the concept of allergic angina. Kounis NG, Zavras GM. https://pubmed.ncbi.nlm.nih.gov/1793697/ . Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 6.Analysis of clinical characteristics of Kounis syndrome induced by contrast media. Wang C, Deng Z, Song L, Sun W, Fang W, Li Z. Am J Emerg Med. 2022;52:203–207. doi: 10.1016/j.ajem.2021.12.036. [DOI] [PubMed] [Google Scholar]
- 7.The unusual suspect: Gadobenate-Dimeglumine induced Kounis syndrome. Choudhry F, Fackler M, Patel M, Patel V, Arnautovic J. Spartan Med Res J. 2019;4 doi: 10.51894/001c.8999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.From Wellens to Kounis syndrome: an unlucky patient. Maadarani O, Bitar Z, Shoeb S, Alsaddah J. Eur J Case Rep Intern Med. 2020;7:1689. doi: 10.12890/2020_001689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Severe adverse drug reaction to gadobenate dimeglumine. Singer BD, Woodrick RS, Pedicano JB. ScientificWorldJournal. 2009;9:363–365. doi: 10.1100/tsw.2009.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.[Coronary spasm secondary to an allergic reaction or Kounis syndrome: report of one case] Dauvergne C, Araya M, Abufhele A. https://pubmed.ncbi.nlm.nih.gov/19746284/ Rev Med Chil. 2009;137:811–814. [PubMed] [Google Scholar]
- 11.Kounis syndrome: a manifestation of drug-eluting stent thrombosis associated with allergic reaction to contrast material. Kogias JS, Papadakis EX, Tsatiris CG, et al. Int J Cardiol. 2010;139:206–209. doi: 10.1016/j.ijcard.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 12.Kounis syndrome captured by coronary angiography computed tomography. Park JM, Cho J, Chung SP, Kim MJ. Am J Emerg Med. 2010;28:640–648. doi: 10.1016/j.ajem.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 13.Myocardial infarction secondary to contrast agent. Contrast effect or type II Kounis syndrome? Kocabay G, Karabay CY, Kounis NG. Am J Emerg Med. 2012;30:255–252. doi: 10.1016/j.ajem.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 14.A case of cardiac arrest with ST elevation induced by contrast medium. Yanagawa Y, Tajima M, Ohara K, Aihara K, Matsuda S, Iba T. Am J Emerg Med. 2012;30:2083–2084. doi: 10.1016/j.ajem.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Kounis syndrome: simultaneous occurrence of an allergic reaction and myocardial ischemia in a 46 year old patient after administration of contrast agent. Zlojtro M, Roginic S, Nikolic-Heitzler V, Babic Z, Kaliterna DM, Marinko A. https://pubmed.ncbi.nlm.nih.gov/24511660/ Isr Med Assoc J. 2013;15:725–726. [PubMed] [Google Scholar]
- 16.Kounis syndrome: allergic acute coronary syndrome. Xu M, Wu XS, Jiang TY, He JQ. https://pubmed.ncbi.nlm.nih.gov/23823844/ Chin Med J (Engl) 2013;126:2591–2592. [PubMed] [Google Scholar]
- 17.Kounis syndrome with cardiogenic shock during transfemoral transcatheter aortic valve replacement. Benedetto D, Agostoni P, de Waal E, Stella PR. Coron Artery Dis. 2015;26:726–727. doi: 10.1097/MCA.0000000000000300. [DOI] [PubMed] [Google Scholar]
- 18.Successful treatment of prolonged cardiopulmonary arrest of Kounis syndrome during coronary angioplasty. Akita T, Kawata M, Sakaguchi A, et al. J Cardiol Cases. 2016;13:47–51. doi: 10.1016/j.jccase.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Successful treatment of Kounis syndrome type I presenting as cardiac arrest with ST elevation. Oh KY, In YN, Kwack CH, Park JS, Min JH, Kang MG, Kim SM. Chin Med J (Engl) 2016;129:626–627. doi: 10.4103/0366-6999.177004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.[Inferior myocardial infarction complicated by complete heart block and cardiac arrest following a gadolinium injection: a case of Kounis syndrome] Demoulin R, Poyet R, Capilla E, et al. Ann Cardiol Angeiol (Paris) 2017;66:319–322. doi: 10.1016/j.ancard.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 21.Acute coronary stent thrombosis: a case of type 3 Kounis syndrome. Tripolino C, Tassone EJ, Morabito G, Grillo P, Missiroli B. J Cardiol Cases. 2019;19:33–35. doi: 10.1016/j.jccase.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Intraprocedure type II Kounis syndrome secondary to radioiodine contrast during coronary angiography. Bhaskaran A, Deshmukh T, Sivagangabalan G. Can J Cardiol. 2018;34:1688–1683. doi: 10.1016/j.cjca.2018.08.029. [DOI] [PubMed] [Google Scholar]
- 23.Kounis syndrome secondary to gadolinium contrast agent. Abusnina W, Shehata M, Abouzid M, Price M, Zeid F. Proc (Bayl Univ Med Cent) 2019;32:253–255. doi: 10.1080/08998280.2019.1581319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Severe left ventricular outflow tract obstruction associated with Kounis syndrome following iodinated contrast administration. Dorniak K, Gałąska R, Fijałkowski M, Pieńkowska J, Łopaciński T, Węsierska M. Pol Arch Intern Med. 2019;129:924–926. doi: 10.20452/pamw.15052. [DOI] [PubMed] [Google Scholar]
- 25.Kounis syndrome induced by contrast media: a case report and review of literature. Shibuya K, Kasama S, Funada R, Katoh H, Tsushima Y. Eur J Radiol Open. 2019;6:91–96. doi: 10.1016/j.ejro.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.An acute adverse reaction with ST elevation induced by magnetic resonance contrast media: Kounis syndrome. Tanaka H, Urushima M, Hirano S, Takenaga M. Intern Med. 2019;58:243–245. doi: 10.2169/internalmedicine.0802-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Contrast media induced Kounis syndrome: a case report. Chien DS, Tsai AP, Lin PC, Yiang GT, Wu MY. Diagnostics. 2019;9:154. doi: 10.3390/diagnostics9040154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Case report of a patient who survived after cardiac arrest and cardiogenic shock by anaphylactic reaction to gadolinium during magnetic resonance imaging. Biagioni E, Coloretti I, Disalvo F, et al. Radiol Case Rep. 2020;15:266–268. doi: 10.1016/j.radcr.2019.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Type III Kounis syndrome after administration of an echocardiography contrast agent. Portero-Portaz JJ, Córdoba-Soriano JG, Gallego-Page JC. Eur Heart J Acute Cardiovasc Care. 2020;9:0–2. doi: 10.1177/2048872616655943. [DOI] [PubMed] [Google Scholar]
- 30.Recurrent lethal allergic coronary vasospasm. Elzeneini M, Aalaei-Andabili SH, Keeley EC. Am J Med. 2020;133:0–2. doi: 10.1016/j.amjmed.2020.04.037. [DOI] [PubMed] [Google Scholar]
- 31.[Kounis syndrome: a case report] Yuan KZ, Wang J, Chang SN, Liao QC. Zhonghua Nei Ke Za Zhi. 2021;60:671–673. doi: 10.3760/cma.j.cn112138-20200918-00827. [DOI] [PubMed] [Google Scholar]
- 32.Recurrent coronary vasospasm: a case of Kounis syndrome from anaphylaxis to contrast dye. Lee Chuy K, Reddy PR, Vij A. Methodist Debakey Cardiovasc J. 2022;18:29–36. doi: 10.14797/mdcvj.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.A rare presentation of Kounis syndrome induced by an echocardiography contrast. Sagalov A, Eggert A, Rimawi A, Hegde S. CJC Open. 2023;5:757–759. doi: 10.1016/j.cjco.2023.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Allergic myocardial infarction (Kounis syndrome)-non-ST elevation MI following Omnipaque contrast. Singh S, Bajaj BS, Chuquin D, Bray Lindsay A. Am J Emerg Med. 2023;67:197–195. doi: 10.1016/j.ajem.2023.03.002. [DOI] [PubMed] [Google Scholar]
- 35.After administration of intravenous epinephrine for bee sting-induced anaphylaxis: Kounis syndrome or epinephrine effect? Kounis NG, Soufras GD, Lianas D, Patsouras N. Chin Med J (Engl) 2016;129:500–501. doi: 10.4103/0366-6999.176081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.The mast cell, contact, and coagulation system connection in anaphylaxis. Guilarte M, Sala-Cunill A, Luengo O, Labrador-Horrillo M, Cardona V. Front Immunol. 2017;8:846. doi: 10.3389/fimmu.2017.00846. [DOI] [PMC free article] [PubMed] [Google Scholar]