Abstract
Ramadan fasting (RF) involves abstaining from food and drink during daylight hours; it is obligatory for all healthy Muslims from the age of puberty. Although sick individuals are exempt from fasting, many will fast anyway. This article explores the impact of RF on individuals with kidney diseases through a comprehensive review of existing literature and consensus recommendations. This study was conducted by a multidisciplinary panel of experts.
The recommendations aim to provide a structured approach to assess and manage fasting during Ramadan for patients with kidney diseases, empowering both healthcare providers and patients to make informed decisions while considering their unique circumstances.
Keywords: Chronic kidney disease, Ramadan fasting, Transplantation, Dialysis, Risk mitigation
Introduction
Fasting during the month of Ramadan constitutes a significant Islamic religious practice, entailing abstinence from food, drinks, and any intentional consumption, such as smoking and medication, from dawn to sunset. Certain individuals, such as prepubertal children, menstruating and pregnant women, breastfeeding mothers, sick people, elderly individuals, and travelers, are exempted from this religious obligation (Surat 2 "Al-Baqarah," Ayat 184–185). However, many within these categories may still choose to fast, seeking to partake in spiritual experiences with their families and peers.
Ramadan falls on the 9th month of the Muslim lunar calendar (Hijra), which comprises 354 days, in contrast to the solar calendar (Gregorian) with 365 days. Consequently, Ramadan occurs 11 days earlier each year and completes a cycle of approximately 33 years. This variation in timing results in a change in the fasting duration based on the year and geographic location. In northern cities, fasting periods can range from just a few hours (less than six hours) during winter Ramadan to over 18 h during summer Ramadan.
Ramadan fasting (RF) involves alternating periods of fasting and refeeding. Understanding its impact on kidney physiology and kidney-related conditions is of utmost importance, particularly when considering the management of chronic kidney disease (CKD) in Muslim patients determined to fast during Ramadan, irrespective of their geographic location.
Few studies have examined the impact of RF on patients with various kidney diseases and the role of diverse risk factors in determining the fasting risk for individual patients with kidney diseases (see Table 1).
Table 1.
Available literature for assessing risks of Ramadan fasting in kidney disease
| Potential Risk Factor | Studies in CKD Pts | Studies in Non CKD Pts |
|---|---|---|
| • Severity of renal insufficiency (eGFR Level) | Limited | |
| • Level of Proteinuria | Very Limited | |
| • Kidney Transplant | ||
| A. First year post transplant | Very Limited | |
| B. After first year post transplant | Limited | |
| • H/o Kidney Stones | Limited | |
| • Hemodialysis | Limited | |
| • Peritoneal dialysis | Very Limited | |
| • Presence of HTN: | ||
| A. Controlled | None | Limited |
| B. Not Controlled | None | None |
| • Heart Diseases: | ||
| A. CAD | None | Limited |
| B. Heart Failure | None | Limited |
| C. Arrhythmia | None | Limited |
| • Duration of Fasting | None | None |
| • Ambient Temperature | None | None |
| • Physical Labor | None | None |
| • Frailty & Age | None | Limited |
| • Liver disease &/or other GI diseases | None | Limited |
| • Pregnancy | None | Limited |
| • Electrolytes abnormalities | None | Limited |
Owing to the obligatory nature of RF, randomized interventional trials are not feasible, as individuals deemed fit to fast must comply, making them ineligible for randomization into non-fasting groups. Consequently, all published studies on RF and the kidney are non-interventional observational studies, predominantly prospective but also include several retrospective analyses. Many of these studies employed fasting individuals as their own controls, whereas others used non-fasting control groups comprising patients who chose not to fast. Moreover, the majority of the studies were conducted at single centers, often involving small patient populations, with absence of studies evaluating the long term effects of Ramadan fasting.
Given the multifaceted functions of the kidneys, the glomerular filtration rate (GFR) serves as an overall assessment of kidney function [1]. However, studies assessing the effects of RF on kidney function have utilized different methods to estimate the GFR. Some studies relied solely on serum creatinine levels as GFR surrogates, while others employed formulas such as Cockcroft-Gault, MDRD, or CKD-Epi. One study used renal DTPA scans.
These factors, among others, contribute to the limited nature of the evidence from existing studies, making it challenging to establish comprehensive fasting recommendations. A task force comprising expert physicians from different countries was assembled to conduct a review of existing literature and reach a consensus. To draw from the extensive expertise of Ramadan and Diabetes (DAR) in this domain, two prominent members of the DaR joined the Ramadan and Kidney Diseases (RaK) task force.
Methodology
The initial concept was conceived by the first three authors who convened in person on three occasions to lay the foundation for the project. Following these initial meetings, an international panel of experts was identified, comprising nephrologists, endocrinologists, and family medicine physicians with expertise in CKD and fasting during the Ramadan.
International experts were invited to participate in a series of virtual meetings held over the course of several months. During these meetings, potential risk factors associated with fasting kidney diseases patients during Ramadan were thoroughly reviewed, and specific tasks were distributed among the group members. The literature relevant to the impact of fasting on kidney function has been extensively reviewed to ensure that the recommendations are evidence-based and comprehensive.
After the literature review, the group conducted several meetings to assess progress and collaboratively drafted the recommendations presented in this consensus statement. The process was characterized by rigorous debate, deliberation, and consensus building among the panel members. The resulting recommendations are the culmination of this multidisciplinary effort intended to provide guidance to healthcare professionals, patients, and researchers in the field of kidney diseases and fasting during Ramadan.
Effect of severity of renal insufficiency
Several studies have investigated the impact of RF on patients with CKD. The majority did not identify significant differences in the kidney function parameters between fasters and non-fasters during Ramadan, or when patients were compared with themselves before and after RF [2–10]. Some studies have suggested that RF might lead to moderate improvement in kidney function [11, 12]. Chowdhury et al. conducted an observational study in the UK with 19 h fasting duration involving stable patients with coexisting CKD Stage 3 and type 2 diabetes. Sixty-eight patients observed the fast, while 71 did not. They found no statistically significant differences in outcome measures or adverse events between the two group [9].
El-Wakil et al. [13] assessed the impact of RF on renal function in a cohort of 15 patients with CKD with an average glomerular filtration rate of 33 ml/min/1.73 m2 in comparison to six healthy controls. While there were no significant differences in the change in GFR between the two groups, they found that CKD patients demonstrated a rise in biomarkers associated with increased tubular cell injury (urinary N-acetyl-B-D- glucosaminidase “NAG”). Another study by Ekinci et al. [4] failed to show any significant differences in urinary neutrophil gelatinase-associated lipocalin (NGAL) between fasting and non-fasting CKD patients.
A limited number of studies have reported worsening renal function in some patients with CKD during RF, primarily observed in those with moderate to severe CKD [14–17]. However, most of these studies lacked a non-fasting control group for comparison purposes. For example, Mbarki et al. reported acute kidney injury (AKI) occurrences in 7 out of 60 patients (11%) with CKD stage 2–4, but without follow-up after Ramadan and lacking a control group [14]. Ansari et al. found worsening kidney function in four patients (14.3%), all of whom were in stage IV and V, although two patients exhibited improvement after Ramadan, resulting in persistent worsening of renal function in only 7% [14].
Baloglu et al. documented AKI in 27 of 117 patients (23%) with CKD stages 2 and 3, but with no follow-up after Ramadan and no control group [16]. Another prospective observational study involving 65 CKD patients fasting in Ramadan with stage 3 or worse CKD demonstrated 22 patients (33.8%) with AKI, as defined by an increase in creatinine of 26.5 umol/L or greater. Among these, 15 patients experienced AKI during Ramadan, 7 patients within three months after Ramadan, 8 patients exhibited subsequent improvement, and 14 continued with persistent reduction in kidney function [17].
A systematic review conducted by Bragazzi [18] identified 26 pertinent studies, of which 5 were specifically focused on CKD non-dialysis and dialysis patients. These studies collectively revealed that RF is generally well tolerated among patients with CKD, albeit with certain caveats. Furthermore, Bragazzi [19] conducted another meta-analysis encompassing six studies involving 350 patients with CKD during Ramadan and monitored changes in eGFR. Of these studies, only two were performed in patients with CKD, and the rest were in transplant recipients. These two meta-analyses were conducted in 2014 and 2015, respectively. More recently, Bello et al. [20] published their protocol for a systemic review in 2019, but the final results have not yet been reported.
In Summery, Available data suggests a progressive increase in the risk of AKI with CKD severity [13, 17]. Stages 1 and 2 show a low risk, stage 3 exhibits a moderate risk, while stages 4 and 5 pose a high risk.
Effect of presence of proteinuria in CKD patients
While some studies have identified the presence of proteinuria as an independent risk factor for renal dysfunction in CKD patients with RF [2], this association has not been consistently confirmed by other studies. Given that these studies were not originally designed for this purpose, we propose considering only nephrotic-range proteinuria as an additional risk factor for CKD in patients with RF.
Effect of Ramadan fasting on pregnant women with CKD
No available study addressed this question. However, observational studies and meta-analyses have assessed the effect of RF on pregnancy without CKD and revealed no harm to pregnant women or their fetuses by RF [21–25].
On the other hand, it is well known that pregnant women with CKD have an increased risk of adverse maternal and infant outcomes in general [26–30], and that pregnancy could cause a flare-up of certain kidney diseases [31].
Taking these data as well as the fact that it is permissible for healthy pregnant and breastfeeding women to break the fast in Ramadan due to concerns about their own health or that of their children [32–35], we recommend that pregnant women with CKD should not fast during Ramadan.
Frailty and cognitive function and Ramadan fasting
Frailty, a syndrome predominantly associated with aging, increases susceptibility to adverse health outcomes [36]. Although we could not find studies specifically assessing the impact of RF in frail CKD patients, the findings from related research are instructive.
Kara et al. observed that advanced age was an independent predictor of renal function deterioration in their study [5]. Bakhit et al. reported through multivariate analysis that more advanced CKD stage, higher baseline systolic blood pressure, and younger age were all independently associated with worsening kidney function [17], which might contradict the results of the study by Kara et al.
Similar to the provision for pregnant women, we advise that frail individuals encounter difficulties in RF to abstain from fasting even in the absence of any underlying medical condition.
Ramadan fasting for kidney transplant recipients
Several studies have investigated the impact of RF on kidney transplant recipients [37–49], and many systematic or mini-reviews have been conducted on the same topic [18, 50–53].
The studies were observational in nature with small sample sizes. Some compared kidney transplant recipients with themselves (pre-Ramadan vs during/post-Ramadan) others had a control group from kidney recipients not fasting during Ramadan. The majority of kidney recipients in these studies had good and stable baseline renal function and fell into CKD stages 1-3T. The risk of acute rejection is generally higher during the first few months post transplantation, and most of these studies excluded kidney recipients who had not completed their first year post-transplantation [40, 42–46]. Only one small study has examined the safety of fasting during the initial year of transplantation. The study included 14 patients who insisted on fasting during Ramadan in 1997, spanning from one to seven months post-transplantation [49]. All patients were on azathioprine and prednisolone and maintained good kidney function (mean plasma creatinine level of 95 ± 15 μmol/L).
These studies (including the last one [49]) as well as the systemic reviews did not reveal any significant changes in kidney function and concluded that RF is safe for patients with stable kidney function.
Ghalib et al. [41] studied whether repeated RF could adversely affect kidney function in kidney transplant recipients. They calculated the eGFR (using the Cockcroft-Gault formula) in 35 transplant patients in the fasting group and 33 in the non-fasting control group both before and after three consecutive Ramadans (2004, 2005, and 2006). They found that RF did not adversely affect kidney function, and no significant change was observed in the eGFR after the third Ramadan compared with the baseline or with the control group. Of interest, five patients in the fasting group had transplants for less than 1 year. Another study yielded similar results and examined kidney transplant recipients with diverse post-transplant periods, including some individuals who had undergone transplantation less than one year prior. However, the study did not provide a precise count of recipients in this particular subgroup. Nevertheless, they did provide the mean post-transplant period, which averaged 2 years, with a range extending from 0.6 to 6.3 years [37].
Based on this limited evidence, we recommend against fasting in the first year after kidney transplant surgery. However, after one year, if a patient exhibits good kidney function (CKD stage I to stage III), fasting does not disrupt their immunosuppressant medication schedule, and has maintained stable kidney function over the previous 3 months, they have the option to decide whether to fast during Ramadan. If a patient chooses to fast, it is crucial to do so with close medical supervision. We recommend monitoring kidney function within the four weeks preceding Ramadan to ensure stability. We also advise repeating the laboratory tests one week after starting fasting to confirm safety. Patients should maintain adequate fluid intake throughout the night, and if they inadvertently forget to take their immunosuppressive medications during the sahoor (pre-dawn meal), it is imperative for them to break their fast on that particular day to take these medications.
Ramadan fasting for patients on dialysis treatment
Ramadan fasting poses notable challenges for patients undergoing dialysis treatment such as hemodialysis or peritoneal dialysis.
In predialysis CKD patients, the primary medical objective is to preserve the remaining kidney function, and other health considerations also play a significant role. However, for dialysis patients already undergoing kidney replacement therapy, where native kidney function is essentially nonexistent or minimal, the focus shifts towards managing other associated health concerns. Notably, the available studies examining the effects of RF on dialysis patients are limited in number and scope.
Maintenance hemodialysis treatment
Studies addressing RF in hemodialysis patients, in general, did not show significant risks [54–61]. However, one Saudi study [59] showed that the fasting group had higher mean interdialytic weight gain (IDWG) by 0.62 kg compared to the non-fasting group. Other studies observed no significant change in dry weight during Ramadan and no increased incidence of pulmonary edema, hypertension, or intradialytic hypotension [55, 56], while a study from Malaysia observed a decrease in IDWG [60].
Another potential risk factor in this group was hyperkalemia. Patients with end-stage kidney disease (ESKD) are more likely than normal controls to develop hyperkalemia after 16 h of fasting. This phenomenon has been attributed to insulinopenia and a diminished response to epinephrine [62]. One study [59] showed that the fasting group exhibited elevated potassium levels when compared to the non-fasting group; however, there was no discernible difference in potassium levels within the fasting group before and during Ramadan. Other studies have found no significant variations in tests in hemodialysis patients during RF [54, 56].
A multicenter, prospective observational study conducted by Adanan et al. [60] revealed a significant improvement in handgrip strength during Ramadan, which continued after Ramadan in patients on maintenance hemodialysis who observed fasting.
Peritoneal dialysis (PD)
We identified a single study conducted by Al Wakeel et al. in Riyadh, Saudi Arabia, during the fasting period of Ramadan in 2009, spanning 14 h in duration [63]. They modified the PD schedule to allow for no fluid exchange during fasting hours. A total 31 PD patients wished to fast. They reported no serious morbidity or mortality and concluded that the most stable patients on PD can fast.
It is important to note that all the studies mentioned above lacked randomization, which is common in research related to RF. This could introduce a significant risk of selection bias since it is probable that healthier and more physically fit patients are more inclined to choose fasting. It is crucial to exercise caution when generalizing the results of these studies to all patients on dialysis. Patients undergoing dialysis typically have a multitude of comorbidities that are likely not adequately represented in these studies. Therefore, we recommend classifying patients on dialysis as high-risk individuals for fasting. This implies that dialysis patients are generally discouraged to fast; if they insist on fast, they should do so under medical supervision. With prior positive fasting experiences, a patient's risk level may shift from high to moderate. This approach prioritizes patient safety given the complexities and risks associated with dialysis and the presence of multiple comorbid conditions in these individuals.
Hypertension in CKD patients who fast during Ramadan
The available literature on this specific topic is limited. We could not find controlled studies specifically aimed at assessing the effects of fasting during Ramadan on CKD patients in the presence or absence of hypertension versus no hypertension. A small prospective self-controlled study from Egypt examining RF encompassed both hypertensive patients with and without CKD. While the mean serum creatinine level increased from 1.06 mg/dL before RF to 1.11 mg/dL post-Ramadan, the level of eGFR did not change significantly. Systolic and diastolic blood pressures (systemic and central) decreased significantly after RF, regardless of CKD status, suggesting that both CKD and non-CKD hypertensive patients can safely observe RF [64].
Other studies have reported in their analysis a significant relationship between the presence of hypertension in CKD patients and the worsening of kidney function during RF [16, 17]. Another study failed to confirm this result [5].
On the other hand, several studies in non-renal hypertensive subjects assessed the influence of RF on blood pressure (BP) control and found no statistical difference between fasting and non-fasting periods in 24 h BP monitoring [65–68]. A large cross-sectional study conducted among 1118 hypertensive patients showed that RF resulted in small but significant improvements in most biochemical parameters [69]. Other studies have reported improved BP control due to RF [70–72]. Two systematic reviews concluded the same [73, 74]. Another meta-analysis suggested beneficial effects of RF on BP independent of changes in weight, total body water, and fat mass, supporting recommendations for some governmental guidelines that describe RF as a safe religious practice with respect to BP [75].
Patients with uncontrolled hypertension were excluded from most studies. However, as they require multiple doses during the daytime, it is recommended that they be counseled against fasting [76].
Ramadan fasting for CKD patients with cardiovascular diseases
There is limited evidence available on the effects of Ramadan fasting in CKD patients with cardiac disease versus those without cardiac disease.
NasrAllah et al. observed adverse cardiovascular events in six patients (11.5%) in the fasting cohort during the month of Ramadan compared with only one patient (1.9%) in the control group (p = 0.036) and were associated with an increase in serum creatinine after one week of fasting and the presence of pre-existing cardiovascular disease [10].
Studies on cardiac patients without CKD have generally found fasting feasible [77–80]. In an observational study, the NYHA functional classification remained unchanged in 92% of the patients who underwent RF [77]. Another study found no significant increase in heart failure hospitalizations during the Ramadan [79]. Two observational studies on patients with chronic coronary syndrome (CAD) [81, 82] found that RF was not associated with increased cardiac mortality or morbidity. The impact of RF on cardiovascular risk factors in patients with stable coronary heart disease is generally favorable [83, 84]. Temizhan et al. [85] found no significant differences in the incidence of acute coronary syndrome (ACS) between the months before, during, and after Ramadan. One study demonstrated that patients who underwent RF within three months of percutaneous coronary intervention had a higher incidence of significant cardiac events than those who did not [86]. Patients with advanced heart failure requiring frequent hospitalization, unstable cardiovascular disease, or arrhythmia need further evaluation prior to fasting, given the risk of complications [76].
Available data regarding CKD patients with cardiac disease are limited, which makes it challenging to establish recommendations. We strongly advocate a thorough evaluation by both nephrologists and cardiologists to collectively determine the safety of RF for these patients.
Ramadan fasting for CKD patients with liver diseases
The influence of RF on individuals with both CKD and concurrent liver disease is complex and understudied. There is an almost complete absence of studies addressing patients with CKD and liver disease during RF.
However, a review of the impact of RF on individuals with liver diseases [87] found that patients with stable liver function and chronic hepatitis B and C can safely fast during Ramadan. For patients with liver cirrhosis, an extensive evaluation is crucial. Patients with Child–Pugh class A liver cirrhosis can participate in fasting, while Child–Pugh class B cirrhosis patients require evaluation based on age and comorbidities. Fasting is generally discouraged in patients with Child–Pugh C liver cirrhosis because of the high risk of complications [88–91]. For non-alcoholic fatty liver disease, RF has shown favorable outcomes in non-alcoholic fatty liver disease [92, 93]. No studies have investigated the effect of fasting on patients with liver cancer [88]. Limited studies have examined the effects of RF on liver transplant recipients [94, 95].
Given the complexity and diversity of liver diseases, it is essential for patients with CKD and liver diseases to undergo a comprehensive evaluation by both nephrologists and gastroenterologists.
The impact of Ramadan fasting during hot summers on CKD patients
Higher ambient temperatures are generally associated with an increased incidence of AKI, which can occur due to hypovolemia or severe heat exposure-induced conditions, such as rhabdomyolysis and inflammation [96–98]. CKD patients observing RF and exposed to a high temperature could be at an increased risk of heat stress, AKI, and stone formation.
The existing literature lacks direct investigation to address this question. Nonetheless, a reasonable conclusion is that CKD patients in hot climates during RF may have an increased risk of kidney complications, depending on the level of temperature and duration of exposure.
The impact of Ramadan fasting on CKD patients with unstable kidney function or acute illness
The existing literature lacks direct investigations addressing this question.
Most studies have excluded CKD patients with acute kidney injury or individuals experiencing acute illnesses, based on the assumption that RF is unsafe for them. We recommend that patients with CKD with unstable kidney function or those currently dealing with acute illnesses refrain from fasting.
The impact of Ramadan fasting on CKD patients with nephrolithiasis
Data from epidemiological and clinical studies have demonstrated that increased urine volume achieved by high fluid intake exerts an efficacious preventive effect on the onset and recurrence of urinary stones [99].
One might presume that RF with no fluid intake during the daytime would predispose susceptible patients to an increased risk of stone formation and renal colic attacks.
The available literature reveals a trend toward RF not increasing the risk of developing urinary stones. However, this remains controversial. Most studies have failed to find a relationship between RF and urinary stones [100–107]. A few studies reported an increased number of renal colic admissions during or after Ramadan [108, 109] There was an association between RF and the incidence of renal colic admissions.
Two recent systematic reviews of the impact of RF on renal stone formation are available. The first (2020) included five studies [110], and the second (2021) identified 10 observational studies [111]. Both studies concluded that RF is unlikely to significantly increase the risk of renal stones.
Owing to limitations in the literature, it is not possible to form a strong opinion on whether fasting during Ramadan affects stone formation. It is also unclear whether RF in summer and hot climate areas adds an additional risk of stone formation.
The impact of Ramadan fasting on patients with diabetes and CKD
In diabetic patients with CKD, managing RF adds complexity. To ensure informed decision-making and enhance patient safety, we strongly advise healthcare providers to utilize the established Diabetes and Ramadan (DAR) risk calculator [112]. This tool considers multiple clinical parameters, including renal function, to evaluate fasting risks and offer personalized recommendations.
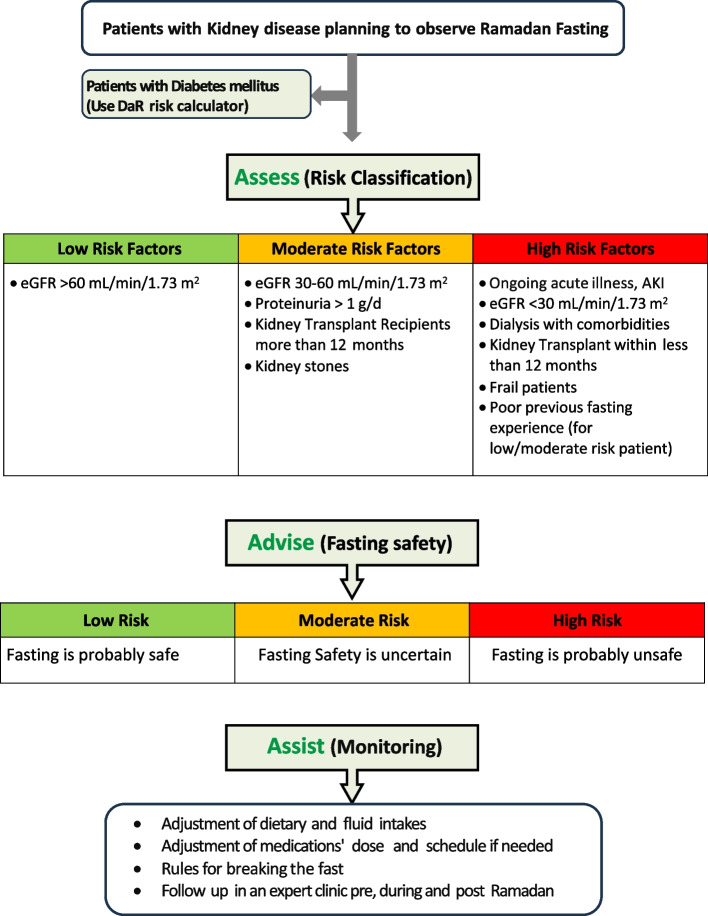
Group recommendations “shown in Fig. 1”
Fig. 1.
RaK clinical assessment tool (3A’s: Assess, Advise & Assist): This figure delineates the RaK recommendations, organized into three steps. The initial step involves the pre-Ramadan assessment to classify the risk of fasting (risk classification), determining whether fasting is advised or not (second step). If a patient, identified with moderate or high risk, chooses to fast, the subsequent step (third) involves assisting them to do it safely, under close monitoring
In light of the review of existing evidence, along with the collective expertise of participating professionals, this task force has developed the first Ramadan and Kidney Disease (RaK) consensus recommendations. These recommendations are designed to provide a structured and as much as possible, evidence-based approach to pre-Ramadan assessment and risk classification, during Ramadan evaluation, and post-Ramadan follow-up for individuals with CKD (Tables 2 and 3). Many social factors could influence these recommendations (availability of air conditioning, patient's profession, housing…) should be taken in consideration. By addressing the challenges and considerations associated with CKD and RF, these recommendations aim to empower both healthcare providers and patients to make informed decisions regarding fasting during the sacred month.
Table 2.
Recommendations for CKD patients planning to fast
| Pre- Ramadan Assessment: | |
| Schedule clinic visit: at 1 to 3 months before Ramadan | - Review previous fasting experience |
| - Evaluate for frailty [113] | |
| - Evaluate clinical and other comorbid conditions | |
| - Assess wellness for fasting and evaluate potential risk factors | |
| - Measure of BP, weight / BMI | |
| - Check basic laboratory investigations: creatinine and electrolytes, eGFR, CBC, blood glucose, calcium, phosphorus levels, protein-to-creatinine ratio, drug levels in patients on tacrolimus or cyclosporine (whenever indicated) | |
|
- Adjust medications to suit fasting hours, detailing the dosing schedule for Ramadan - Substitute short-acting medications with long-acting formulations (e.g., tacrolimus) or patch-based options (eg clonidine), if available - Gradually taper off medications prone to rebound effects (e.g., oral clonidine) if patches aren't an available - Inform the patient about the need to adjust the timing for measuring calcineurin inhibitor (tacrolimus or cyclosporine) trough levels to align with their revised schedule | |
|
- Dietary adjustment and water / fluid intake during Ramadan: - To eat balanced diet that fits patient’s health - To avoid potassium rich food (dried fruits, banana, fruit juice,..) if hyperkalemia is a concern - To break the fast gradually: Begin with a cup of water, followed by light meal, then to have the main meal post Taraweeh prayer - Should not skip Sahoor “pre-dawn meal” - To stay hydrated: to drink at least 1.5 to 2.5 L of water throughout the night, avoiding excessive intake at once. Space out your consumption | |
| - Discuss physical (type and timing) activity during Ramadan | |
| - Refer to other subspecialty clinics for the evaluation of relevant fasting risk factors (nephrology, cardiology, endocrinology, and others), whenever indicated | |
| - Classify patient risk and recommend accordingly. (see Fig. 1) | |
| - Monitoring during Ramadan fasting is advised for all patients | |
| - Discuss the rules for early termination of the fast (Table 3) | |
| During- Ramadan Assessment: | |
| Schedule clinic visit: 1st week of Ramadan for moderate and high-risk patients who opted to fast | - Ask about tolerating fasting and any issues encountered |
| - Check BP, weight / BMI, blood glucose | |
| - Basic laboratory investigations: Creatinine and electrolytes, eGFR, CBC, and drug trough levels in patients on tacrolimus or cyclosporine (be careful about the time of the test) | |
| - Review medications and if patient is following the recommended adjustments | |
| - Advise about dietary adjustment, water / fluid intake | |
| - Review type and timing of physical activity during Ramadan | |
| - Review the rules for early termination of the fast | |
| Post- Ramadan Assessment: | |
| Schedule clinic visit: at 1 then 3 months after Ramadan | - Evaluate the fasting experience and any issues encountered |
| - Measurement of BP, weight / BMI, blood glucose | |
| - Basic laboratory investigations: HbA1c, creatinine, and electrolytes, eGFR, CBC, lipid panel, drug levels in patients on tacrolimus or cyclosporine | |
| - Medications dose adjustment and schedule (resume pre-Ramadan) | |
| - Evaluate the comorbid conditions post Ramadan | |
Table 3.
Rules for early termination of the fast
| ◦ Any acute illness causing (fever, diarrhea, exhaustion, vomiting …) |
| ◦ Any condition requiring hospitalization (trauma, suspected cardiovascular event) |
| ◦ AKI, noted on laboratory investigations |
| ◦ Hyperglycemia Blood glucose > 300 mg/dL (16.6 mmol/L), or hypoglycemia Blood glucose < 70 mg/dL (3.9 mmol/L), even in asymptomatic patients |
| ◦ Kidney transplant patient missed taking his immunosuppression medications at Sohour |
In summary, the RaK Initiative, a collaboration of nephrologists, endocrinologists, and family physicians, sheds light on the intricate relationship between RF and kidney disease. Our recommendations emphasize the importance of pre-Ramadan evaluation, personalized guidance, and risk assessment. We considered factors such as eGFR, proteinuria, transplant status, and comorbidities to help healthcare providers decide on fasting eligibility.
While evidence of RF in the context of kidney disease is limited, our work underscores the need for tailored care and monitoring to ensure that individuals with kidney disease can safely participate in RF and harmonize their spiritual observance with optimal healthcare practices. Further research is needed to expand our understanding and refine our recommendations to prioritize patient safety and well-being.
Recommendations for future research
The road ahead necessitates critical, multidisciplinary collaborations to design and execute high-quality clinical studies delving into the diverse effects of fasting on patients with renal diseases. Standardizing acceptable endpoints and assessment methodologies, coupled with comprehensive details regarding fasting duration, environmental influences, and social factors, could significantly enhance the interpretation of study outcomes.
Presently, there is a notable dearth or extremely limited studies examining the impact of Ramadan fasting on kidney disease patients with various accompanying risk factors (refer to Table 1). For instance, investigations are needed to explore the effects of RF on CKD patients with heart failure, those with ischemic heart disease, individuals with hypertension, among other specific conditions. Expanding research into these specific subgroups within the CKD patient population during RF could provide invaluable insights.
Authors’ contributions
Y. Boobes (YB), as the founder of the RaK initiative, collaborated with B. Afandi (BA) and F. Alkindi (FA) in substantial roles, contributing to the conception, design of the work, data acquisition, analysis, and interpretation. YB authored the main manuscript text; BA, FA, and M. Hassanein (MH) critically reviewed the manuscript, with BA and FA refining the review process. Figure 1 was prepared by FA and A. Tarakji (AT), further reviewed and revised by YB and BA. Table 1 was assembled by YB, Table 2 by FA, then reviewed and modified by YB and BA. BA and MH reviewed literature and analyzed data regarding risk factors of Ramadan fasting in diabetic patients. FA and YB reviewed data related to liver disease and labor work during Ramadan fasting. M. Alrukhaimi and L. AlKetbi reviewed literature and analyzed data concerning Ramadan fasting in relation to pregnancy, frailty, and cognitive function. R. Said and YB reviewed literature and analyzed data on Ramadan fasting in kidney transplant patients. A. Alsuwaida and Y. Abdelhamid reviewed literature and analyzed data on Ramadan fasting and acute kidney injury. N. Attallah and YB reviewed literature and analyzed data on Ramadan fasting in dialysis patients. S.M. Al-Ghamdi and YB reviewed literature and analyzed data on Ramadan fasting in CKD. AT and A. Obaidli reviewed literature and analyzed data on Ramadan fasting and heart diseases (heart failure). A. AlSahow and K. Boubes reviewed literature and analyzed data on Ramadan fasting in relation to the duration of fasting and exposure to heat temperature. J. AlSaid and I. Al Salmi reviewed literature and analyzed data on Ramadan fasting and hypertension. M. Hassan, M. Al Hakim, N. Bashir, and R. Aburahma reviewed literature and analyzed data on risk factors of proteinuria and kidney stones during Ramadan fasting. All authors actively engaged in a series of extensive virtual meetings conducted over several months to evaluate our progress, engage in rigorous debates, deliberate, and collectively formulate the recommendations presented in this consensus statement. All authors read and approved the final manuscript.
Funding
This project did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Inker LA, Titan S. Measurement and estimation of GFR for use in clinical practice: core curriculum 2021. Am J Kidney Dis. 2021;78(5):736–749. doi: 10.1053/j.ajkd.2021.04.016. [DOI] [PubMed] [Google Scholar]
- 2.Dogan I, Eser B, Kayadibi H. The effect of Ramadan fasting on renal functions in patients with chronic kidney disease. Turk J Biochem. 2019;44(2):189–196. doi: 10.1515/tjb-2018-0373. [DOI] [Google Scholar]
- 3.Yousef EA, Atwa MA, Mahmoud MA. Effect of Ramadan fasting on chronic inflammation and body composition in patients with chronic kidney disease. Saudi J Kidney Dis Transpl. 2021;32(4):1013–1018. doi: 10.4103/1319-2442.338274. [DOI] [PubMed] [Google Scholar]
- 4.Ekinci I, Erkoc R, Gursu M, Dogan EE, Kilic E, Cebeci E, et al. Effects of fasting during the month of Ramadan on renal function in patients with autosomal dominant polycystic kidney disease. Clin Nephrol. 2018;89(2):103–112. doi: 10.5414/CN109102. [DOI] [PubMed] [Google Scholar]
- 5.Kara E, Sahin OZ, Kizilkaya B, Ozturk B, Pusuroglu G, Yildirim S, et al. Fasting in Ramadan is not associated with deterioration of chronic kidney disease: a prospective observational study. Saudi J Kidney Dis Transpl. 2017;28(1):68–75. doi: 10.4103/1319-2442.198140. [DOI] [PubMed] [Google Scholar]
- 6.Hassan S, Hassan F, Abbas N, Hassan K, Khatib N, Edgim R, et al. Does Ramadan fasting affect hydration status and kidney function in CKD patients? Ann Nutr Metab. 2018;72(3):241–247. doi: 10.1159/000486799. [DOI] [PubMed] [Google Scholar]
- 7.BaynounaAlKetbi L, Nagelkerke N, AlZarouni A, Al Kuwaiti M, Al Ghafli M, Al Qahtani S, et al. Ramadan fasting outcome among high-risk patients. BMC Nephrol. 2022;23(1):304. doi: 10.1186/s12882-022-02915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al Wakeel JS. Kidney function and metabolic profile of chronic kidney disease and hemodialysis patients during Ramadan fasting. Iran J Kidney Dis. 2014;8:321–328. [PubMed] [Google Scholar]
- 9.Chowdhury A, Khan H, Lasker SS, Chowdhury TA. Fasting outcomes in people with diabetes and chronic kidney disease in East London during Ramadan 2018: the East London diabetes in Ramadan survey. Diabetes Res Clin Pract. 2019;152:166–170. doi: 10.1016/j.diabres.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 10.NasrAllah MM, Osman NA. Fasting during the month of Ramadan among patients with chronic kidney disease: renal and cardiovascular outcomes. Clin Kidney J. 2014;7:348–353. doi: 10.1093/ckj/sfu046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernieh B, Al Hakim MR, Boobes Y, Abu Zidan FM. Fasting Ramadan in chronic kidney disease patients: clinical and biochemical effects. Saudi J Kidney Dis Transpl. 2010;21:898–902. [PubMed] [Google Scholar]
- 12.Karatas A, Canakci E, Arici YK, Kaya M, Sayim B. The effect of fasting during ramadan on the kidney functions of stage III-IV chronic kidney disease patients. Pak J Med Sci. 2021;37(4):972–978. doi: 10.12669/pjms.37.4.3661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Wakil HS, Desoky I, Lotfy N, Adam AG. Fasting the month of Ramadan by Muslims: could it be injurious to their kidneys? Saudi J Kidney Dis Transpl. 2007;18(3):349–354. [PubMed] [Google Scholar]
- 14.Mbarki H, Tazi N, Najdi A, Tachfouti N, Arrayhani M, Sqalli T. Effects of fasting during Ramadan on renal function of patients with chronic kidney disease. Saudi J Kidney Dis Transpl. 2015;26(2):320–324. doi: 10.4103/1319-2442.152494. [DOI] [PubMed] [Google Scholar]
- 15.Ansari FA, Latief M, Manuel S, Shashikiran KB, Dwivedi R, Prasad DK, et al. Impact of fasting during ramadan on renal functions in patients with chronic kidney disease. Indian J Nephrol. 2022;32(3):262–265. doi: 10.4103/ijn.IJN_521_20.Epub2022Mar11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baloglu I, Turkmen K, Kocyigit I, Altunoren O, Demirtas L, Zararsız G, et al. The effect of Ramadan fasting on kidney function in patients with chronic kidney disease. Int Urol Nephrol. 2020;52(7):1337–1343. doi: 10.1007/s11255-020-02506-x. [DOI] [PubMed] [Google Scholar]
- 17.Bakhit AA, Kurdi AM, Wadera JJ, Alsuwaida AO. Effects of Ramadan fasting on moderate to severe chronic kidney disease. A prospective observational study. Saudi Med J. 2017;38(1):48–52. doi: 10.15537/smj.2017.1.17566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bragazzi NL. Ramadan fasting and chronic kidney disease: a systematic review. J Res Med Sci. 2014;19:665–676. [PMC free article] [PubMed] [Google Scholar]
- 19.Bragazzi NL. Ramadan fasting and chronic kidney disease: does estimated glomerular filtration rate change after and before Ramadan? Insights from a mini meta-analysis. Int J Nephrol Renovasc Dis. 2015;8:53–57. doi: 10.2147/IJNRD.S61718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bello AK, Kurzawa J, Osman MA, Olah ME, Lloyd A, Wiebe N, et al. Impact of Ramadan fasting on kidney function and related outcomes in patients with chronic kidney disease: a systematic review protocol. BMJ Open. 2019;9(8):e022710. doi: 10.1136/bmjopen-2018-022710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glazier JD, Hayes DJ, Hussain S, D’Souza SW, Whitcombe J, Heazell AE, et al. The effect of Ramadan fasting during pregnancy on perinatal outcomes: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2018;18(1):1–11. doi: 10.1186/s12884-018-2048-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oosterwijk VNL, Molenaar JM, van Bilsen LA, Kiefte-de Jong JC. Ramadan fasting during pregnancy and health outcomes in offspring: a systematic review. Nutrients. 2021;13(10):3450. doi: 10.3390/nu13103450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hossain N, Samuel M, Mughal S, Shafique K. Ramadan fasting: perception and maternal outcomes during pregnancy. Pak J Med Sci. 2021;37(5):1262–1267. doi: 10.12669/pjms.37.5.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Safari K, Piro TJ, Ahmad HM. Perspectives and pregnancy outcomes of maternal Ramadan fasting in the second trimester of pregnancy. BMC Pregnancy Childbirth. 2019;19(1):128. doi: 10.1186/s12884-019-2275-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parveen R, Khakwani M, Latif M, Tareen AU. Maternal and perinatal outcome after ramadan fasting. Pak J Med Sci. 2020;36(5):894–898. doi: 10.12669/pjms.36.5.2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fink JC, Schwartz SM, Benedetti TJ, Stehman-Breen CO. Increased risk of adverse maternal and infant outcomes among women with renal disease. Paediatr Perinat Epidemiol. 1998;12:277–287. doi: 10.1046/j.1365-3016.1998.00129.x. [DOI] [PubMed] [Google Scholar]
- 27.Jones DC, Hayslett JP. Outcome of pregnancy in women with moderate or severe renal insufficiency [published erratum appears in N Engl J Med 1997;336:739] N Engl J Med. 1996;335:226–232. doi: 10.1056/NEJM199607253350402. [DOI] [PubMed] [Google Scholar]
- 28.Cunningham FG, Cox SM, Harstad TW, Mason RA, Pritchard JA. Chronic renal disease and pregnancy outcome. Am J Obstet Gynecol. 1990;163:453–459. doi: 10.1016/0002-9378(90)91175-C. [DOI] [PubMed] [Google Scholar]
- 29.Trevisan G, Ramos JG, Martins-Costa S, Barros EJ. Pregnancy in patients with chronic renal insufficiency at Hospital de Clinicas of Porto Alegre. Brazil Ren Fail. 2004;26:29–34. doi: 10.1081/JDI-120028540. [DOI] [PubMed] [Google Scholar]
- 30.Fischer MJ, Lehnerz SD, Hebert JR, Parikh CR. Kidney disease is an independent risk factor for adverse fetal and maternal outcomes in pregnancy. Am J Kidney Dis. 2004;43:415–423. doi: 10.1053/j.ajkd.2003.10.041. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez Suarez ML, Kattah A, Grande JP, Garovic V. Renal disorders in pregnancy: core curriculum 2019. Am J Kidney Dis. 2019;73(1):119–130. doi: 10.1053/j.ajkd.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Mabsoot by Al-Sarkhasi, (3/92) “In Arabic Language”.
- 33.Al-Istithkar by Ibn Abd al-Bar, (10/223) “In Arabic Language”.
- 34.Al-Majmoo’ by al-Nawawi, (6/ 267) “In Arabic Language”.
- 35.Al-Mughni by Ibn Qudamah, (3/37) “In Arabic Language”.
- 36.J D Walston, UpToDate, last updated: Nov 05, 2021
- 37.Abdalla AH, Shaheen FA, Rassoul Z, Owda AK, Popovich WF, Mousa DH, et al. Effect of Ramadan fasting on Moslem kidney transplant recipients. Am J Nephrol. 1998;18(2):101–104. doi: 10.1159/000013316. [DOI] [PubMed] [Google Scholar]
- 38.Argani H, Mozaffari S, Rahnama B, Rahbani M, Rejaie M, Ghafari A. Evaluation of biochemical and immunologic changes in renal transplant recipients during Ramadan fasting. Transplant Proc. 2003;35:2725–2726. doi: 10.1016/j.transproceed.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 39.Said T, Nampoory MR, Haleem MA, Nair MP, Johny KV, Samhan M, et al. Ramadan fast in kidney transplant recipients: a prospective comparative study. Transplant Proc. 2003;35:2614–2616. doi: 10.1016/j.transproceed.2003.08.072. [DOI] [PubMed] [Google Scholar]
- 40.Einollahi B, Lessan-Pezeshki M, Simforoosh N, Nafar M, Pour-Reza-Gholi F, Firouzan A, et al. Impact of Ramadan fasting on renal allograft function. Transplant Proc. 2005;37(7):3004–2005. doi: 10.1016/j.transproceed.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 41.Ghalib M, Qureshi J, Tamim H, Ghamdi G, Flaiw A, Hejaili F, et al. Does repeated Ramadan fasting adversely affect kidney function in renal transplant patients? Transplantation. 2008;85(1):141–144. doi: 10.1097/01.tp.0000296841.99263.c2. [DOI] [PubMed] [Google Scholar]
- 42.Boobes Y, Bernieh B, Al Hakim MR. Fasting Ramadan in kidney transplant patients is safe. Saudi J Kidney Dis Transpl. 2009;20(2):198–200. [PubMed] [Google Scholar]
- 43.Einollahi B, Lessan-Pezeshki M, Pourfarziani V, Aghdam B, Rouzbeh J, Ghadiani MH, et al. Ramadan fasting in kidney transplant recipients with normal renal function and with mild-to-moderate renal dysfunction. Int Urol Nephrol. 2009;41:417–422. doi: 10.1007/s11255-008-9476-y. [DOI] [PubMed] [Google Scholar]
- 44.Beladi Mousavi SS, Golzari K, Hayati F, Motemednia F, Beladi Mousavi M. Is Ramadan fasting safe for kidney transplant patients with normal renal function? 5 Case reports. Shiraz E-Med J. 2011;4:203–205. [Google Scholar]
- 45.Qurashi S, Tamimi A, Jaradat M, Al SA. Effect of fasting for Ramadan on kidney graft function during the hottest month of the year (August) in Riyadh. Saudi Arabia Exp Clin Transplant. 2012;10(6):551–553. doi: 10.6002/ect.2012.0139. [DOI] [PubMed] [Google Scholar]
- 46.Hejaili F, Qurashi S, Binsalih S, Jaradt M, Al Sayyari A. Effect of repeated ramadan fasting in the hottest months of the year on renal graft function. Nephrourol Mon. 2014;6(2):e14362. doi: 10.5812/numonthly.14362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ibrahim IA, Hassan EA, Alkhan AM, Hussein MA, Alhabashi AF, Ali TZ, et al. Ramadan fasting in kidney transplant recipients: a single-centre retrospective study. J Transplant. 2018;3(2018):4890978. doi: 10.1155/2018/4890978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arabi ZM, Elhassan EA, Abdalla MI, Farooqui MA, Mateen AA, Kaysi S, et al. Multi national survey of the advice given to muslim kidney graft recipients by muslim nephrologists about lifestyle and religious rituals with potential medical risk. Saudi J Kidney Dis Transpl. 2020;31(5):957–981. doi: 10.4103/1319-2442.301202. [DOI] [PubMed] [Google Scholar]
- 49.Ouziala M, Ouziala S, Bellaoui A, Drif M. Fasting during the first year of transplantation: is it safe? Saudi J Kidney Dis Transpl. 1998;9(4):440–443. [PubMed] [Google Scholar]
- 50.Emami-Naini A, Roomizadeh P, Baradaran A, Abedini A, Abtahi M. Ramadan fasting and patients with renal diseases: A mini review of the literature. J Res Med Sci. 2013;18(8):711–716. [PMC free article] [PubMed] [Google Scholar]
- 51.Binsalih S, Al Sayyari RA, Sheikho M, Hejaili FF, Al Sayyari AA. Effect of fasting the whole month of ramadan on renal function among muslim patients with kidney transplant: a meta-analysis. Exp Clin Transplant. 2019;17(5):588–593. doi: 10.6002/ect.2019.0245. [DOI] [PubMed] [Google Scholar]
- 52.Malik S, Hamer R, Shabir S, Youssouf S, Morsy M, Rashid R, et al. Effects of fasting on solid organ transplant recipients during Ramadan - a practical guide for healthcare professionals. Clin Med (Lond) 2021;21(5):e492–e498. doi: 10.7861/clinmed.2021-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Habas E, Sr, Errayes M, Habas E, Farfar KL, Alfitori G, Habas AE, et al. Fasting Ramadan in Chronic Kidney Disease (CKD), kidney transplant and dialysis patients: review and update. Cureus. 2022;14(5):e25269. doi: 10.7759/cureus.25269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wan Md Adnan WA, Zaharan NL, Wong MH, Lim SK. The effects of intermittent fasting during the month of Ramadan in chronic haemodialysis patients in a tropical climate country. PLoS One. 2014;9(12):e114262. [DOI] [PMC free article] [PubMed]
- 55.Alshamsi S, Binsaleh F, Hejaili F, Karkar A, Moussa D, Raza H, et al. Changes in biochemical, hemodynamic, and dialysis adherence parameters in hemodialysis patients during Ramadan. Hemodial Int. 2016;20(2):270–276. doi: 10.1111/hdi.12369. [DOI] [PubMed] [Google Scholar]
- 56.Imtiaz S, Salman B, Dhrolia MF, Nasir K, Abbas HN, Ahmad A. Clinical and biochemical parameters of hemodialysis patients before and during islamic month of Ramadan. Iran J Kidney Dis. 2016;10(2):75–78. [PubMed] [Google Scholar]
- 57.Tashkandi B, Kaur D, Latifi E, Tallman DA, Chinna K, Daud ZAM, et al. Lipids, lipoprotein distribution and nutritional parameters over the Ramadan period in hemodialysis patients. Nutrients. 2019;11:2225. doi: 10.3390/nu11092225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Megahed AF, El-Kannishy G, Sayed-Ahmed N. Status of fasting in Ramadan of chronic hemodialysis patients all over Egypt: a multicenter observational study. Saudi J Kidney Dis Transpl. 2019;30:339–349. doi: 10.4103/1319-2442.256841. [DOI] [PubMed] [Google Scholar]
- 59.Khazneh E, Qaddumi J, Hamdan Z, Qudaimat F, Sbitany A, Jebrin K, et al. The effects of Ramadan fasting on clinical and biochemical markers among hemodialysis patients: a prospective cohort study. PLoS One. 2019;14(6):e0218745. doi: 10.1371/journal.pone.0218745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Adanan NI, Md Ali MS, Lim JH, Zakaria NF, Lim CTS, Yahya R, et al. Investigating Physical and nutritional changes during prolonged intermittent fasting in hemodialysis patients: a prospective cohort. J Ren Nutr. 2020;30:e15–26. doi: 10.1053/j.jrn.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 61.Adanan NIH, Adnan WAHWM, Khosla P, Karupaiah T, Daud ZAM. Exploring the experiences and perceptions of haemodialysis patients observing Ramadan fasting: a qualitative study. BMC Nephrol. 2021;22(01):48 [DOI] [PMC free article] [PubMed]
- 62.Gifford JD, Rutsky EA, Kirk KA, McDaniel HG. Control of serum potassium during fasting in patient with end stage renal disease. Kidney Int. 1989;35:90–94. doi: 10.1038/ki.1989.12. [DOI] [PubMed] [Google Scholar]
- 63.Al Wakeel J, Mitwalli AH, Alsuwaida A, Al Ghonaim M, Usama S, Hayat A, Shah IH. Recommendations for fasting in Ramadan for patients on peritoneal dialysis. Perit Dial Int. 2013;33(1):86–91. doi: 10.3747/pdi.2010.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Eldeeb AA, Mahmoud MA, Ibrahim AB, Yousef EA, Sabry AA. Effect of Ramadan fasting on arterial stiffness parameters among Egyptian hypertensive patients with and without chronic kidney disease. Saudi J Kidney Dis Transpl. 2020;31(3):582–588. doi: 10.4103/1319-2442.289444. [DOI] [PubMed] [Google Scholar]
- 65.Perk G, Ghanem J, Aamar S, Ben-Ishay D, Bursztyn M. The effect of the fast of Ramadan on ambulatory blood pressure in treated hypertensives. J Hum Hypertens. 2001;15(10):723–725. doi: 10.1038/sj.jhh.1001262. [DOI] [PubMed] [Google Scholar]
- 66.Ural E, Kozdag G, Kilic T, Ural D, Sahin T, Celebi O, et al. The effect of Ramadan fasting on ambulatory blood pressure in hypertensive patients using combination drug therapy. J Hum Hypertens. 2008;22(3):208–810. doi: 10.1038/sj.jhh.1002296. [DOI] [PubMed] [Google Scholar]
- 67.Khosropanah S, Ashraf F, Handjani AM. The effect of one-day Ramadan fast on blood pressure of hypertensive patients. Iran Heart J. 2003;4:39–43. [Google Scholar]
- 68.Zairi I, Bejar MA, Ben Mrad I, Mzoughi K, Kraiem S. Effects of Ramadan fasting on blood pressure in hypertensive patients. Tunis Med. 2021;99(7):727–733. [PMC free article] [PubMed] [Google Scholar]
- 69.Bener A, Al-Hamaq AOAA, Öztürk M, Güllüoğlu S. Does Ramadan fasting have effects on sleep, fatigue and blood pressure among patients with hypertension? Blood Press Monit. 2021;26(2):108–112. doi: 10.1097/MBP.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 70.Aktürk IF, Biyik I, Koşaş C, Yalçın AA, Ertürk M, Uzun F. Effects of Ramadan fasting on blood pressure control, lipid profile, brain natriuretic peptide, renal functions and electrolyte levels in hypertensive patients taking combination therapy. Nobel Medicus. 2013;9:43–46. [Google Scholar]
- 71.Farag HAM, Baqi HR, Qadir SA, El Bilbeisi AH, Hamafarj KK, Taleb M, et al. Effects of Ramadan fasting on anthropometric measures, blood pressure, and lipid profile among hypertensive patients in the Kurdistan region of Iraq. SAGE Open Med. 2020;27(8):2050312120965780. doi: 10.1177/2050312120965780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Demirci E, Çalapkorur B, Celik O, Koçer D, Demirelli S, Şimsek Z. Improvement in blood pressure after intermittent fasting in hipertension: could renin-angiotensin system and autonomic nervous system have a role? Arq Bras Cardiol. 2023;120(5):e20220756. doi: 10.36660/abc.20220756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alinezhad-Namaghi M, Salehi M. Effects of Ramadan fasting on blood pressure in hypertensive patients: a systematic review. J Fast Health. 2016;4(1):17–21. [Google Scholar]
- 74.Luke K, Ferona NA, Anjani HL, Putri S, Harelina T, Jefri Prastyo B, et al. The effect of ramadan fasting to blood pressure in hypertensive patients: a meta analysis. J Commun Med Public Health Res. 2021;2(2):54–60. doi: 10.20473/jcmphr.v2i2.26821. [DOI] [Google Scholar]
- 75.Al-Jafar R, Zografou Themeli M, Zaman S, Akbar S, Lhoste V, Khamliche A, et al. Effect of religious fasting in ramadan on blood pressure: results from LORANS (London Ramadan Study) and a meta-analysis. J Am Heart Assoc. 2021;10(20):e021560. doi: 10.1161/JAHA.120.021560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chamsi-Pasha M, Chamsi-Pasha H. The cardiac patient in Ramadan. Avicenna J Med. 2016;6(2):33–38. doi: 10.4103/2231-0770.179547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Abazid RM, Khalaf HH, Sakr HI, Altorbak NA, Alenzi HS, Awad ZM, et al. Effects of Ramadan fasting on the symptoms of chronic heart failure. Saudi Med J. 2018;39(4):395–400. doi: 10.15537/smj.2018.4.22011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Salam AM, Sulaiman K, Alsheikh-Ali AA, Singh R, Asaad N, Al-Qahtani A, et al. Acute heart failure presentations and outcomes during the fasting month of Ramadan: an observational report from seven Middle Eastern countries. Curr Med Res Opin. 2018;34(2):237–245. doi: 10.1080/03007995.2017.1376629. [DOI] [PubMed] [Google Scholar]
- 79.Al Suwaidi J, Bener A, Hajar HA, Numan MT. Does hospitalization for congestive heart failure occur more frequently in Ramadan: a population-based study (1991–2001) Int J Cardiol. 2004;96(2):217–221. doi: 10.1016/j.ijcard.2003.06.018. [DOI] [PubMed] [Google Scholar]
- 80.Alam S, Hussain S, Abbas J, Raza MH, Rasool WA, Alsubai AK, et al. Clinical outcomes of fasting in patients with chronic heart failure with preserved ejection fraction: a prospective analysis. Ann Med Surg (Lond) 2022;81:104373. doi: 10.1016/j.amsu.2022.104373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Khafaji HA, Bener A, Osman M, Al Merri A, Al SJ. The impact of diurnal fasting during Ramadan on the lipid profile, hs-CRP, and serum leptin in stable cardiac patients. Vasc Health Risk Manag. 2012;8:7–14. doi: 10.2147/VHRM.S22894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mousavi M, Mirkarimi S, Rahmani G, Hosseinzadeh E, Salahi N. Ramadan fast in patients with coronary artery disease. Iran Red Crescent Med J. 2014;16(12):e7887. doi: 10.5812/ircmj.7887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ben Ahmed H, Allouche E, Bouzid K, Zrelli S, Hmaidi W, Molahedh Y, et al. Impact of Ramadan fasting on lipid profile and cardiovascular risk factors in patients with stable coronary artery disease. Ann Cardiol Angeiol (Paris) 2022;71(1):36–40. doi: 10.1016/j.ancard.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 84.Gocer H, Gunday M, Abusharekh M, Unal M. To show the effect of intermittent fasting during Ramadan on endothelial dysfunction via TIMI frame count. Niger J Clin Pract. 2021;24(06):943–947. doi: 10.4103/njcp.njcp_626_19. [DOI] [PubMed] [Google Scholar]
- 85.Temizhan A, Dönderici O, Ouz D, Demirbas B. Is there any effect of Ramadan fasting on acute coronary heart disease events? Int J Cardiol. 1999;70:149–53. doi: 10.1016/S0167-5273(99)00082-0. [DOI] [PubMed] [Google Scholar]
- 86.Amin OA, Alaarag A. The safety of Ramadan fasting following percutaneous coronary intervention. BMC Cardiovasc Disord. 2020;20:489. doi: 10.1186/s12872-020-01784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Emara MH, Soliman HH, Elnadry M, Mohamed Said E, Abd-Elsalam S, Elbatae HE, et al. Egyptian Ramadan fasting, liver diseases interest group”. Ramadan fasting and liver diseases: a review with practice advices and recommendations. Liver Int. 2021;41(3):436–448. doi: 10.1111/liv.14775. [DOI] [PubMed] [Google Scholar]
- 88.Elnadry MH, Nigm IA, Abdel Aziz IM, Elshafee AM, Elazhary SS, Abdel Hafeez MA, et al. Effect of Ramadan fasting on Muslim patients with chronic liver diseases. J Egypt Soc Parasitol. 2011;41(2):337–346. [PubMed] [Google Scholar]
- 89.Elfert AA, AbouSaif SA, Kader NA, AbdelAal E, Elfert AY, et al. A multicenter pilot study of the effects of Ramadan fasting on patients with liver cirrhosis. Tanta Med Sci J. 2011;6:25–33. [Google Scholar]
- 90.Mohamed SY, Emara MH, Hussien HI, Elsadek HM. Changes in portal blood flow and liver functions in cirrhotics during Ramadan in the summer: a pilot study. Gastroenterol Hepatol Bed Bench. 2016;9:180–188. [PMC free article] [PubMed] [Google Scholar]
- 91.Mohamed SY, Emara MH, Gabballah BA, Mostafa EF, Maaly MA. Effects of Ramadan fasting on muslim patients with liver cirrhosis: a comparative study. Govaresh. 2018;23:47–52. [Google Scholar]
- 92.Arabi SM, Hejri Zarifi S, Nematy M, Safarian M. The effect of Ramadan fasting on non-alcoholic fatty liver disease (NAFLD) patients. J Fasting Health. 2015;3:74–80. [Google Scholar]
- 93.Ebrahimi S, Gargari BP, Aliasghari F, Asjodi F, Izadi A. Ramadan fasting improves liver function and total cholesterol in patients with nonalcoholic fatty liver disease. Int J Vitam Nutr Res. 2020;90(1–2):95–102. doi: 10.1024/0300-9831/a000442. [DOI] [PubMed] [Google Scholar]
- 94.Derbala M, Elbadri M, Amer A, AlKaabi S, Mohiuddin S, Elsayad E, et al. Safety and deleterious effect of fasting Ramadan in liver transplant recipients. J Gastroenterol Metabol. 2018;1:203. [Google Scholar]
- 95.Montasser IF, Dabbous H, Sakr MM, Ebada H, Massoud YM, Salaheldin MM, et al. Effect of Ramadan fasting on Muslim recipients after living donor liver transplantation: a single center study. Arab J Gastroenterol. 2020;21(2):76–79. doi: 10.1016/j.ajg.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 96.Borg MA, Bi P. The impact of climate change on kidney health. Nat Rev Nephrol. 2021;17(5):294–295. doi: 10.1038/s41581-020-00365-4. [DOI] [PubMed] [Google Scholar]
- 97.Johnson RJ, Sánchez-Lozada LG, Newman LS, Lanaspa MA, Diaz HF, Lemery J, et al. Climate Change and the Kidney. Ann Nutr Metab. 2019;74(Suppl 3):38–44. doi: 10.1159/000500344. [DOI] [PubMed] [Google Scholar]
- 98.Sasai F, Roncal-Jimenez C, Rogers K, Sato Y, Brown JM, Glaser J, et al. Climate change and nephrology. Nephrol Dial Transplant. 2021;2(2):gfab258. doi: 10.1093/ndt/gfab258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Siener R, Hesse A. Fluid intake and epidemiology of urolithiasis. Eur J Clin Nutr. 2003;57(Suppl 2):S47–51. doi: 10.1038/sj.ejcn.1601901. [DOI] [PubMed] [Google Scholar]
- 100.Al-Hadramy MS. Seasonal variations of urinary stone colic in Arabia. J Pak Med Assoc. 1997;47(11):281–284. [PubMed] [Google Scholar]
- 101.Basiri A, Moghaddam SM, Khoddam R, Nejad ST, Hakimi A. Monthly variations of urinary stone colic in Iran and its relationship to the fasting month of Ramadan. J Pak Med Assoc. 2004;54(1):6–8. [PubMed] [Google Scholar]
- 102.Miladipour AH, Shakhssalim N, Parvin M, Azadvari M. Effect of Ramadan fasting on urinary risk factors for calculus formation. Iran J Kidney Dis. 2012;6(1):33–38. [PubMed] [Google Scholar]
- 103.Cevik Y, Corbacioglu SK, Cikrikci G, Oncul V, Emektar E. The effects of Ramadan fasting on the number of renal colic visits to the emergency department. Pak J Med Sci. 2016;32(1):18–21. doi: 10.12669/pjms.321.8248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Al Mahayni AO, Alkhateeb SS, Abusaq IH, Al Mufarrih AA, Jaafari MI, Bawazir AA. Does fasting in Ramadan increase the risk of developing urinary stones? Saudi Med J. 2018;39(5):481–486. doi: 10.15537/smj.2018.5.22160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shahid S, Akram S, Haroun S. The impacts of fasting in Ramadan on the amount of renal colic visits to the department of emergency. Indo Am J P Sci. 2019;06(5):10706–10710. [Google Scholar]
- 106.Torabi M, Shojaee F, Mirzaee M. Prevalence of renal colic in the emergency departments: a multi-center study. Hosp Pract Res. 2021;6(3):123–126. doi: 10.34172/hpr.2021.23. [DOI] [Google Scholar]
- 107.Taha I. Renal diseases and Ramadan: A review of the literature. Life Science Journal. 2013;10.
- 108.Abdolreza N, Omalbanin A, Mahdieh TS, Mohammad Ali MR, Reza MS, Maryam S, et al. Comparison of the number of patients admitted with renal colic during various stages of peri-Ramadan month. Saudi J Kidney Dis Transpl. 2011;22(6):1199–1202. [PubMed] [Google Scholar]
- 109.Mustafa MN, AlOmran AJ, Raes AA. Frequency of renal colic during the month of Ramadan. Bahrain Med Bull. 2020;42(3):189–191. [Google Scholar]
- 110.Amjadi M, Soleimanzadeh F, Ghamatzadeh H, Hajebrahimi S, Hosseinifard H, SalehiPourmehr H, et al. Ramadan fasting and kidney stones: a systematic review. Urol J. 2020;18(4):364–370. doi: 10.22037/uj.v16i7.6373. [DOI] [PubMed] [Google Scholar]
- 111.Kirubarajan A, Lam ACL, Khan S, Yau M, Golda N, Buckley R. The association between renal stones and fasting: a systematic review. Can Urol Assoc J. 2021;15(03):E169–E174. doi: 10.5489/cuaj.6664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.IDF. Diabetes and Ramadan IDF-DAR Practical Guidelines 2021. Available from: https://www.daralliance.org/daralliance/idf-dar-practical-guidelines-2021/.
- 113.Capurso C, Bellanti F, Lo Buglio A, Vendemiale G. The mediterranean diet slows down the progression of aging and helps to prevent the onset of frailty: a narrative review. Nutrients. 2019;12(1):35. doi: 10.3390/nu12010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.