ABSTRACT
Invasive primary Candida surgical site infections (IP-SSIs) are a common complication of liver transplantation, and targeted antifungal prophylaxis is an efficient strategy to limit their occurrence. We performed a retrospective single-center cohort study among adult single liver transplant recipients at Duke University Hospital in the period between 1 January 2015 and 31 December 2020. The study aimed to determine the rate of Candida IP-SSI according to the peri-transplant antifungal prophylaxis received. Of 470 adult single liver transplant recipients, 53 (11.3%) received micafungin prophylaxis, 100 (21.3%) received fluconazole prophylaxis, and 317 (67.4%) did not receive systemic antifungal prophylaxis in the peri-transplant period. Ten Candida IP-SSIs occurred among 5 of 53 (9.4%) micafungin recipients, 1 of 100 (1.0%) fluconazole recipients, and 4 of 317 (1.3%) recipients who did not receive antifungal prophylaxis. Our study highlights the limitations of antifungal prophylaxis in preventing invasive Candida IP-SSI after liver transplant surgery. We hypothesize that pathogen, host, and pharmacokinetic-related factors contributed to the occurrence of Candida IP-SSI despite antifungal prophylaxis. Our study reinforces the need for a risk-based, multi-pronged approach to fungal prevention, including targeted antifungal administration in patients with risks for invasive candidiasis and close monitoring, especially among patients with surgically complex procedures, with timely control of surgical leaks.
KEYWORDS: micafungin, prophylaxis, transplant, liver
INTRODUCTION
As Candida is part of the gastrointestinal microbiome, it can translocate into the peritoneal cavity at the time of liver transplantation and cause invasive surgical site infections. This contributes to the high rate of invasive Candida infections reported in the liver transplant population and the need for antifungal prophylaxis at the time of surgery for liver transplant candidates at an increased risk for invasive Candida infections (1, 2). The American Society of Transplantation (AST) recognizes re-transplantation, re-operation, renal failure requiring hemodialysis, transfusion of ≥40 units of cellular blood products, choledochojejunostomy, and Candida colonization in the perioperative period as risk factors for Candida infection among liver transplant recipients and recommends antifungal prophylaxis for 2–4 weeks following transplantation in this setting (2). While no final recommendation regarding the preferred antifungal agent in high-risk liver transplant recipients is provided, the AST guidelines suggest similar performance of echinocandins and fluconazole in the prevention of Candida infections after liver transplant surgery (2). Of note, however, more recent studies questioned the efficacy of echinocandin prophylaxis after transplant surgery, given concerns about the tissue penetration of echinocandins, particularly into the pleural space (3). In this study, we assessed the epidemiology and outcomes of invasive Candida surgical site infections among adult liver transplant recipients according to the peri-transplant antifungal prophylaxis received over a 6-year period at a major US transplant center.
MATERIALS AND METHODS
Study design
We performed an observational single-center retrospective cohort study of all adult patients who underwent a single liver transplant between 1 January 2015 and 31 December 2020 at Duke University Hospital (Durham, North Carolina), a high-volume solid organ transplant center that has been performing adult and pediatric solid organ transplants since 1965. This study was approved by the Duke University Health System Institutional Review Board (IRB number: Pro00104142). Inform consent of study participants was waived by the IRB.
Study population
Eligible patients were 18 years of age or older and met all the following criteria: (i) single-liver transplant performed at Duke University Hospital during the 6-year study period and (ii) at least 12-month post-transplant clinical follow-up available, unless death occurred before the 12-month mark.
Definitions and adjudication process for invasive primary surgical site infections
Using the Centers for Disease Control and Prevention—National Healthcare Safety Network definitions for surgical site infections, surgical site infections needed to occur within 3 months after the transplant procedure (4). Deep incisional and organ/space infections involving the primary surgical incision were considered invasive primary surgical site infections (IP-SSIs). Additional details on the adjudication process for IP-SSI are described in our previous publication (5).
Other study definitions
Antifungal prophylaxis was defined as any systemic prophylactic antifungal administered within 24 hours of surgical incision. Antifungal prophylaxis regimens were categorized into three groups: micafungin prophylaxis, fluconazole prophylaxis, and no antifungal prophylaxis. The institutional antifungal prophylaxis protocol is reported in Table 1: while fluconazole was the recommended antifungal agent, micafungin prophylaxis was used in the case of prior infections with non-albicans isolates, prior prolonged azole exposure, or contraindications to use fluconazole (including prolonged QTc or prior hypersensitivity reaction). The duration of antifungal prophylaxis was calculated in days as interval from the time of transplant until the discontinuation of prophylactic antifungal agent. For those patients receiving antifungal prophylaxis at the time of Candida IP-SSI diagnosis, the duration of antifungal prophylaxis was calculated in days as the interval from the time of transplant until the diagnosis of Candida IP-SSI. Candida antifungal susceptibility testing was performed by the Duke Microbiology Laboratory in accordance with the Clinical and Laboratory Standards Institute (CLSI) methods, breakpoints, and interpretative categories. Length of hospital stay was defined as the number of days from the admission date to the date of discharge during the index transplant hospitalization. In-hospital mortality was defined as all-cause mortality during the index transplant hospitalization. One-year mortality was defined as all-cause mortality from the time of transplant to 365 days after transplant (5).
TABLE 1.
Perioperative antifungal (excluding Pneumocystis jiroveci) prophylaxis protocol for adult liver transplant surgery at Duke University Hospital in the period between 1 January 2015 and 31 December 2020a
| Antifungal prophylaxis protocol |
|---|
| Standard |
| Clotrimazole 10 mg q12h (for 3 months) |
| Fulminant liver failure |
| Fluconazole 400 mg q24hb assuming estimated creatinine clearance >50 mL/min (for 5 days or as clinically indicated) |
| Split liver |
| Fluconazole 400 mg q24h assuming estimated creatinine clearance >50 mL/min (for 2 days or as clinically indicated) |
| History of Candida infection in donor or recipient |
| Individualized antifungal prophylaxis |
Starting in 2018, in the case of intraoperative transfusion requirement of ≥40 units of blood products, fluconazole prophylaxis was administered (for 5 days or as clinically indicated). When micafungin was used as an antifungal prophylactic agent, 100 mg q24h was administered.
q24h, every 24 hours.
Study objectives
The primary aim of this study was to determine the rate of Candida IP-SSIs during the study period among adult liver transplant recipients according to the peri-transplant antifungal prophylaxis received. Secondary aims included (i) determining the clinical outcomes in each antifungal prophylaxis group and (ii) evaluating the reasons behind antifungal prophylaxis failure in cases of Candida IP-SSI occurring in patients who received systemic antifungal prophylaxis.
Statistical analysis
Continuous variables were calculated as means with standard deviation. Categorical variables were calculated based on frequencies and percentages of the specified group. Comparisons between groups were made with the chi-square test, Fisher exact test, or independent t-test as appropriate. A two-sided P value of <0.05 was considered statistically significant. Candida IP-SSI rates were calculated based on the total number of single liver transplants (denominator) and the total number of Candida IP-SSI (numerator) in each prophylaxis group. Statistical analyses were performed using IBM SPSS Statistics (version 29.0; IBM, Armonk, New York).
RESULTS
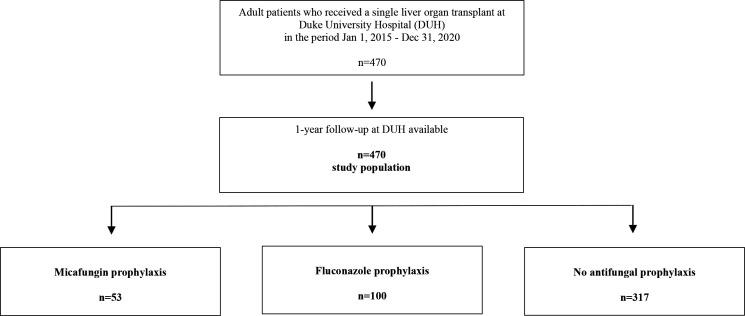
Between 1 January 2015 and 31 December 2020, 470 adult single liver transplants were performed at Duke University Hospital (Durham, North Carolina). A 12-month post-transplant clinical follow-up was available for all the patients transplanted, and compliance with institutional prophylaxis recommendations was observed in 96.4% of the cases. Of the 470 adult single liver transplant recipients, 53 (11.3%) received micafungin prophylaxis, 100 (21.3%) fluconazole prophylaxis, and 317 (67.4%) did not receive systemic antifungal prophylaxis in the peri-transplant period (Fig. 1). The duration of antifungal prophylaxis was similar in the fluconazole and micafungin groups (4.1 vs 4.3 days, P = 0.56).
Fig 1.
Study population.
Antifungal prophylaxis groups: baseline characteristics
When comparing the adult single liver transplant recipients who received systemic antifungal prophylaxis with those recipients who did not receive systemic antifungal prophylaxis in the peri-transplant setting, several statistically significant differences were noted (Table 2). This was expected given the targeted antifungal prophylaxis approach in place at our institution during the study period. Patients who did not receive systemic antifungal prophylaxis were older (P < 0.01) and had a lower model for end-stage liver disease scores (P < 0.01). The underlying disease leading to transplant differed significantly in these study groups (P < 0.01). In addition, patients who did not receive systemic antifungal prophylaxis were less likely to be on immunosuppressive therapy (P < 0.01) and have end-stage renal disease (P < 0.01), ascites (P < 0.01), or prior hepatobiliary surgery (P = 0.01) in the pre-transplant period. The duration of hospitalization before the transplant was also shorter for patients who did not receive systemic antifungal prophylaxis in the peri-transplant setting (P < 0.01). The duration of hospitalization before transplant was also shorter for patients who received fluconazole prophylaxis than for recipients who received micafungin prophylaxis (4.2 vs 8.2 days, P < 0.01) (Table 2). The longer pre-transplant hospitalization among those who received micafungin was often due to acute (or chronic) liver failure requiring inpatient management.
TABLE 2.
Baseline characteristics of adult patients who underwent a single liver transplant at Duke University Hospital in the period between 1 January 2015 and 31 December 2020 stratified by antifungal prophylaxis regimena
| Micafungin prophylaxis n = 53 | Fluconazole prophylaxis n = 100 | P-value (micafungin prophylaxis vs fluconazole prophylaxis) | No antifungal prophylaxis n = 317 | P-value (micafungin and fluconazole prophylaxis vs no prophylaxis) | |
|---|---|---|---|---|---|
| Male gender, n (%) | 36 (67.9) | 57 (57.0) | 0.23 | 227 (71.6) | 0.02 |
| Race, n (%) | 0.16 | 0.02 | |||
| Caucasian | 41 (77.4) | 72 (72.0) | 275 (86.8) | ||
| African American | 4 (7.5) | 18 (18.0) | 27 (8.5) | ||
| Asian | 3 (5.7) | 3 (3.0) | 5 (1.6) | ||
| American Indian or Alaska Native | 3 (5.7) | 1 (1.0) | 2 (0.6) | ||
| Other | 0 (0.0) | 3 (3.0) | 3 (0.9) | ||
| Declined | 2 (3.8) | 3 (3.0) | 5 (1.6) | ||
| Age (years), mean (standard deviation) | 52.6 (12.8) | 53.7 (10.0) | 0.54 | 57.7 (10.8) | <0.01 |
| BMI, mean (standard deviation) | 29.2 (5.0) | 30.7 (5.7) | 0.11 | 30.2 (5.5) | 0.97 |
| Underlying disease leading to transplant, n (%) | 0.40 | <0.01 | |||
| Drug-induced acute hepatic necrosis | 1 (1.9) | 1 (1.0) | 1 (0.3) | ||
| Acute hepatic necrosis other | 3 (5.7) | 4 (4.0) | 1 (0.3) | ||
| Cirrhosis biliary (primary and secondary) | 3 (5.7) | 5 (5.0) | 7 (2.2) | ||
| Cirrhosis alcoholic | 12 (22.6) | 17 (17.0) | 55 (17.4) | ||
| Cirrhosis autoimmune | 5 (9.4) | 4 (4.0) | 4 (1.3) | ||
| Cirrhosis cryptogenic | 3 (5.7) | 2 (2.0) | 19 (6.0) | ||
| Cirrhosis NASH | 5 (9.4) | 24 (24.0) | 68 (21.5) | ||
| Cirrhosis HBV related | 1 (1.9) | 4 (4.0) | 2 (0.6) | ||
| Cirrhosis HCV related | 6 (11.3) | 11 (11.0) | 43 (13.6) | ||
| Hepatocellular carcinoma | 2 (3.8) | 11 (11.0) | 79 (24.9) | ||
| Cholangiocarcinoma | 0 (0.0) | 1 (1.0) | 3 (0.9) | ||
| Hepatic epithelioid hemangioendothelioma | 1 (1.9) | 0 (0.0) | 3 (0.9) | ||
| Primary sclerosing cholangitis | 6 (11.3) | 11 (11.0) | 23 (7.3) | ||
| Alpha 1 anti-trypsin deficiency | 1 (1.9) | 1 (1.9) | 5 (1.6) | ||
| Hemochromatosis | 0 (0.0) | 0 (0.0) | 1 (0.3) 3 (0.9) | ||
| Other | 4 (7.5) | 3 (3.0) | |||
| Pre-transplant immunosuppressive therapy, n (%) | 10 (18.9) | 11 (11.0) | 0.22 | 15 (4.7) | <0.01 |
| Pre-transplant diabetes, n (%) | 11 (20.8) | 31 (31.0) | 0.19 | 110 (34.7) | 0.14 |
| Pre-transplant end-stage renal disease, n (%) | 7 (13.2) | 6 (6.0) | 0.14 | 7 (2.2) | <0.01 |
| Antibiotic use in the 4 months prior to transplant, n (%) | 38 (71.7) | 82 (82.0) | 0.15 | 229 (72.2) | 0.18 |
| Ascites, n (%) | 41 (77.4) | 70 (70.0) | 0.45 | 182 (57.4) | <0.01 |
| Prior hepatobiliary surgery, n (%) | 20 (37.7) | 36 (36.0) | 0.86 | 80 (25.2) | 0.01 |
| Days admitted before transplant, mean (standard deviation) | 8.2 (7.5) | 4.2 (6.5) | <0.01 | 1.8 (5.9) | <0.01 |
| MELD score at transplant, mean (standard deviation) | 28.3 (9.6) | 25.5 (9.8) | 0.09 | 18.1 (7.4) | <0.01 |
| Donor status, n (%) | 0.56 | <0.01 | |||
| - Brain death | 49 (92.5) | 87 (87.0) | 305 (96.2) | ||
| - Cardiac death | 2 (3.8) | 8 (8.0) | 12 (3.8) | ||
| - Living donor | 2 (3.8) | 5 (5.0) | 0 (0.0) | ||
| Repeat transplantation, n (%) | 6 (11.3) | 4 (4.0) | 0.10 | 2 (0.6) | <0.01 |
| Split liver, n (%) | 4 (7.5) | 12 (12.0) | 0.58 | 2 (0.6) | <0.01 |
| Cold ischemic time (minutes), mean (standard deviation) | 326 (126.2) | 318 (118.8) | 0.72 | 313.9 (113.7) | 0.52 |
| Warm ischemic time (minutes), mean (standard deviation) | 37 (6.6) | 39 (6.4) | 0.12 | 40 (41.0) | 0.53 |
| Primary closure, n (%) | 48 (90.6) | 94 (94.0) | 0.52 | 313 (98.7) | <0.01 |
| Transplant surgery >8 hours, n (%) | 15 (28.3) | 26 (26.0) | 0.85 | 26 (8.2) | <0.01 |
| Roux en Y biliary anastomosis, n (%) | 17 (32.1) | 20 (20.0) | 0.11 | 37 (11.7) | <0.01 |
| Bacterial contamination due to entry into GI tract, n (%) | 4 (7.5) | 1 (1.0) | 0.05 | 0 (0.0) | <0.01 |
| Units PRBC required during surgery, mean (standard deviation) | 7.4 (7.1) | 7.0 (8.7) | 0.79 | 3.1 (3.5) | <0.01 |
| >6 units PRBC required during surgery, n (%) | 18 (34.0) | 36 (36.0) | 0.86 | 43 (13.6) | <0.01 |
| Anastomotic leak, n (%) | 6 (11.3) | 10 (10.0) | 0.79 | 11 (3.5) | <0.01 |
| Post-transplant renal replacement therapy, n (%) | 17 (32.1) | 25 (25.0) | 0.35 | 17 (5.4) | <0.01 |
| Return to the OR for abdominal surgery within 3 months of transplant, n (%) | 22 (41.5) | 36 (36.0) | 0.60 | 48 (15.1) | <0.01 |
| Duration of antifungal prophylaxis, mean (standard deviation) | 4.3 (1.7) | 4.1 (1.8) | 0.56 | − | − |
| Candida IP-SSI, n (%) | 5 (9.4) | 1 (1.0) | 0.02 | 4 (1.3) | 0.09 |
BMI, body mass index; NASH, non-alcoholic steatohepatitis; HBV, hepatitis B virus; HCV, hepatitis C virus; MELD, model for end-stage liver disease; GI, gastrointestinal; PRBC, packed red blood cells; OR, operating room.
Patients who did not receive systemic antifungal prophylaxis in the peri-transplant setting also had less complex surgical courses with fewer patients in this group requiring operative time above 8 hours (P < 0.01), Roux-en-Y biliary anastomosis (P < 0.01), extensive use of intra-operative blood products (P < 0.01), delayed closure of the abdominal cavity (P < 0.01), repeat transplantation (P < 0.01), or split liver procedures (P < 0.01). Similarly, surgical (peritoneal contamination due to accidental intestinal tract injury or anastomotic leak) and post-surgical (need for renal replacement therapy and abdominal surgery within 3 months of liver transplant) complications were uncommon among patients who did not receive systemic antifungal prophylaxis in the peri-transplant setting when compared to patients who received antifungal prophylaxis (P < 0.01). Peritoneal contamination due to accidental intestinal tract injury was more common among patients who received micafungin than patients who received fluconazole (7.5% vs 1.0%, P =0.05; Table 2).
Candida IP-SSI rate
During the study period, 10 Candida IP-SSIs occurred among 5 of 53 (9.4%) micafungin recipients, 1 of 100 (1.0%) fluconazole recipients, and 4 of 317 (1.3%) recipients who did not receive antifungal prophylaxis. Fourteen Candida strains were isolated among the 10 patients with Candida IP-SSI (Table 4). Candida albicans accounted for 5 (35.7%) of the isolates. Among non-albicans species, Candida glabrata, Candida tropicalis, and Candida kefyr were identified. Candida glabrata accounted for 7 (77.7%) of the non-albicans isolates. All C. glabrata isolates were fluconazole susceptible dose-dependent. Of note, 8 of 10 Candida IP-SSI were polymicrobial and were characterized by the concomitant detection of bacterial pathogens and Candida (one monomicrobial infection was reported in the micafungin group and one in the no antifungal prophylaxis group).
Candida IP-SSI outcomes
Patients who did not receive systemic antifungal prophylaxis at the time of liver transplant surgery had more favorable clinical outcomes than patients who received antifungal prophylaxis: while no difference in 1-year mortality was observed (P = 0.07), their index hospitalization was shorter (P < 0.01), and their in-hospital and 30-day mortality rates were lower (P = 0.04) (Table 3). Clinical outcomes were similar in the micafungin and fluconazole prophylaxis groups (Table 3).
TABLE 3.
Outcomes of adult patients who underwent a single liver transplant at Duke University Hospital in the period between 1 January 2015 and 31 December 2020 stratified by antifungal prophylaxis regimen
| Micafungin prophylaxis, n = 53 |
Fluconazole prophylaxis, n = 100 |
P-value (micafungin prophylaxis vs fluconazole prophylaxis) |
No antifungal prophylaxis, n = 317 |
P-value (micafungin and fluconazole prophylaxis vs no prophylaxis) |
|
|---|---|---|---|---|---|
| Length of hospital stay (days), mean (standard deviation) | 32.4 (27.5) | 22.7 (32.4) | 0.07 | 12.8 (14.8) | <0.01a |
| In-hospital mortality, n (%) | 1 (1.9) | 3 (3.0) | 1.00 | 1 (0.3) | 0.04 |
| 30-day mortality, n (%) | 1 (1.9) | 4 (4.0) | 0.66 | 2 (0.6) | 0.04 |
| 1-year mortality, n (%) | 5 (9.4) | 7 (7.0) | 0.75 | 11 (3.5) | 0.07 |
Statistically significant values are presented in bold.
Antifungal prophylaxis failures
Of the 10 Candida IP-SSI diagnosed during the study period, 6 occurred in liver transplant recipients who received systemic antifungal prophylaxis in the peri-transplant period and constituted prophylaxis failures (Table 5). Micafungin prophylaxis failure occurred in five patients: two patients received a short duration of prophylaxis (3 days) and developed IP-SSI 6 and 10 days, respectively, after antifungal discontinuation, while three patients developed intra-abdominal candidiasis despite longer courses of prophylaxis, including two that occurred while the drug was still being administered. Also notable, three of the five Candida IP-SSIs occurred in the setting of surgical complications (i.e., anastomotic or enteric leaks). Failure of fluconazole prophylaxis was reported in only one patient: in this case, failure occurred on day 3 of prophylaxis with an isolate that was fluconazole susceptible dose-dependent (likely representing microbiologic failure).
DISCUSSION
This study sheds light on the limitations of antifungal prophylaxis in preventing Candida IP-SSI among adult liver transplant recipients at Duke University Hospital over a recent 6-year period (2015–2020).
Antifungal prophylaxis in adult liver transplant surgery
In line with international recommendations, targeted antifungal prophylaxis was administered at Duke University Hospital in the period of 2015–2020 for adult liver transplant recipients at an increased risk for invasive Candida infections (2). Specifically, fulminant liver failure, split liver procedures, and prior Candida infections were considered risk factors associated with an increased risk for Candida IP-SSI warranting antifungal prophylaxis at the time of surgery. Of note, while re-transplantation, re-operation, renal failure requiring hemodialysis, transfusion of ≥40 units of cellular blood products, and choledochojejunostomy are historically recognized as Candida risk factors, their identification did not trigger the deployment of antifungal prophylaxis at our center during the study period (2). Deploying targeted antifungal prophylaxis in the presence of re-transplantation, re-operation, renal failure requiring hemodialysis, transfusion of ≥40 units of cellular blood products, and choledochojejunostomy would have potentially prevented two of the four Candida IP-SSIs documented among patients who did not receive systemic antifungal prophylaxis. That said, the low rate (1.3%; 4/317) of Candida IP-SSI among patients who did not receive systemic antifungal prophylaxis confirms the overall appropriateness of our targeted strategy, striking the balance between antifungal stewardship and infection prevention.
Of 470 adult single liver transplants performed, 153 (32.6%) were considered at increased risk for invasive Candida infections per our protocol and received antifungal prophylaxis. Fluconazole was the recommended antifungal prophylaxis agent and was used in 100 (21.3%) transplant procedures, while micafungin was used in 53 (11.3%). Six Candida IP-SSIs occurred among patients who received antifungal prophylaxis. There was a higher rate of Candida IP-SSIs (9.4% vs 1.0%, P = 0.02) among patients who received micafungin prophylaxis than among those who received fluconazole.
Possible explanations for the failure of antifungal prophylaxis
Factors influencing the efficacy of antifungal prophylaxis may be related to the pathogen, host, and the drug used.
Pathogen-related factors
In the fluconazole group, we documented one prophylaxis failure related to a C. glabrata isolate with dose-dependent susceptibility to fluconazole. Isolates in the susceptible dose-dependent category require higher doses of fluconazole to achieve clinical success. Failure in this case was thus likely related to resistance in the isolate and suboptimal fluconazole dosing as prescribed for prophylaxis. While mutations in the FKS1 and FKS2 genes that encode the β-1,3-glucan synthase enzyme complex among Candida isolates are associated with echinocandin resistance (6, 7), none of the Candida isolates identified in the liver transplant recipients who developed a Candida IP-SSI in our study population were micafungin resistant based on CLSI breakpoints (Table 4). Thus, echinocandin resistance in the pathogens was not likely the reason for the failure of micafungin prophylaxis.
TABLE 4.
Candida isolates identified among 10 adults who received a single liver transplant at Duke University Hospital in the period between 1 January 2015 and 31 December 2020 and developed a Candida spp. IP-SSIa
| Pathogens recovered | Micafungin prophylaxis n = 53 patients (five Candida IP-SSI cases) |
Fluconazole prophylaxis n = 100 patients (one Candida IP-SSI) |
No antifungal prophylaxis n = 317 patients (four Candida IP-SSIs) |
Total n = 470 patients (10 Candida IP-SSIs) |
|---|---|---|---|---|
| Candida albicans | 2 | − | 3 | 5 |
| Fluconazole susceptible dose-dependent | 0 | 0 | 0 | |
| Fluconazole resistant | 0 | 0 | 0 | |
| Micafungin resistant | 0 | 0 | 0 | |
| Candida glabrata | 3 | 1 | 3 | 7 |
| Fluconazole susceptible dose-dependent | 3 | 1 | 3 | 7 |
| Fluconazole resistant | 0 | 0 | 0 | 0 |
| Micafungin resistant | 0 | 0 | 0 | 0 |
| Candida tropicalis | 1 | − | − | 1 |
| Fluconazole susceptible dose-dependent | 0 | 0 | ||
| Fluconazole resistant | 1 | 1 | ||
| Micafungin resistant | 0 | 0 | ||
| Candida kefyr | 1 | − | − | 1 |
| Fluconazole susceptible dose-dependent | 0 | 0 | ||
| Fluconazole resistant | 0 | 0 | ||
| Micafungin resistant | 0 | 0 |
Data stratified by antifungal prophylaxis regimen.
Host-related factors
Immunosuppression, prolonged antibacterial exposure, and lack of source control are well-recognized factors promoting the failure of antifungal prophylaxis (8). Furthermore, prompt intervention to control sources has been associated with successful clinical outcomes in prior studies on intra-abdominal candidiasis (9, 10). Of the five cases of Candida IP-SSI that occurred despite micafungin prophylaxis, three developed in the setting of anastomotic leaks wherein recognition and surgical intervention were not immediate (Table 5). Lack of early intervention may have, therefore, contributed to micafungin failure in these patients. However, it is also worth noting that anastomotic leaks and abdominal surgery within 3 months of liver transplant were equally encountered among patients who received micafungin prophylaxis and patients who received fluconazole prophylaxis, suggesting that prompt intervention and control of leaks were not the sole factor leading to micafungin prophylaxis failure. Other host-related factors may also have been at play. For example, more patients who received micafungin suffered unintentional breaches of the intestinal mucosa during the transplant procedure compared with those who received fluconazole. The relatively small number of patients receiving prophylaxis may have limited our ability to distinguish other important differences between the groups that posed an increased risk for invasive candidiasis.
TABLE 5.
Candida spp. IP-SSIs: clinical detailsa
| Pathogens (sample) |
Antifungal prophylactic drug (dose) | Systemic antifungal indicated per 2015–2020 prophylaxis protocol | Candida IP-SSI risk factors |
Candida IP-SSI diagnosis after transplant (days) |
Candida IP-SSI clinical presentation |
Systemic antifungal prophylaxis at diagnosis of Candida IP-SSI | Antifungal prophylaxis before Candida IP-SSI diagnosis (days) | Possible explanation for prophylaxis failure |
|---|---|---|---|---|---|---|---|---|
|
C. glabrata (peritoneal fluid) |
Micafungin (100 mg) |
Yes (micafungin chosen over fluconazole given prior C. glabrata infection) |
5, 6 | 13 | Candida peritonitis Sepsis |
No | 3 | Premature discontinuation of micafungin (micafungin discontinued on post-transplant day 3) |
|
C. albicans C. glabrata (peritoneal fluid) |
Micafungin (100 mg) |
Yes (micafungin chosen over fluconazole given prior C. glabrata infection) |
5, 6 | 9 | Candida peritonitis secondary to biliary leak Septic shock |
No | 3 | Premature discontinuation of micafungin (micafungin discontinued on post-transplant day 3) and source control (anastomotic bile leak identified on post-transplant day 8) |
| C. glabrata (peritoneal fluid) | Micafungin (100 mg) |
Yes (micafungin chosen over fluconazole given prior C. glabrata infection) |
3, 6 | 6 | Candida peritonitis secondary to biliary leak Asymptomatic, isolated leukocytosis |
Yes | 6 | Source control (anastomotic bile leak identified on post-transplant day 6) |
|
C. tropicalis (peritoneal fluid) |
Micafungin (100 mg) |
Yes (micafungin chosen over fluconazole given prior C. glabrata infection) |
5, 6 | 9 | Candida peritonitis secondary to enteric leak Asymptomatic, isolated leukocytosis | Yes | 9 | Source control (enteric leak identified on post-transplant day 9) |
|
C. albicans C. kefyr (peri-hepatic abscess) |
Micafungin (100 mg) |
Yes (micafungin chosen over fluconazole given recurrent cholangitis in the pre-transplant period) |
1, 3, 5, 7 | 26 | Candida peri-hepatic abscess Asymptomatic, isolated leukocytosis | No | 17 | Source control (intra-abdominal abscess identified on post-transplant day 26) |
|
C. glabrata (blood) |
Fluconazole (400 mg) |
No (fluconazole used per surgeon’s decision given complicated transplant surgery with Roux anastomosis) | 5 | 3 | Candidemia and peritonitis Multifactorial shock (septic and hemorrhagic) | Yes | 3 | Microbiological failure (C. glabrata fluconazole susceptible dose-dependent) |
|
C. glabrata (intra-abdominal abscess and blood) |
No | No | 3 | 7 | Candida intra-abdominal abscess Fever and leukocytosis |
− | − | |
|
C. albicans C. glabrata (peri-hepatic abscess and peritoneal fluid) |
No | No | 5 | 14 | Candida peri-hepatic abscess and peritonitis Asymptomatic, isolated leukocytosis | − | − | |
|
C. albicans (peritoneal fluid) |
No | No | − | 13 | Candida peritonitis secondary to biliary leak Asymptomatic | − | − | |
|
C. albicans C. glabrata (peritoneal fluid and blood) |
No | No | − | 4 | Candida peritonitis Sepsis | − | − |
Candida risk factors: (i) re-transplantation; (ii) re-operation; (iii) renal failure requiring hemodialysis; (iv) transfusion of ≥40 units of cellular blood products; (v) choledochojejunostomy; (vi) Candida colonization in the perioperative period; (vii) fulminant liver failure; and (viii) split liver.
Antifungal therapy-related factors
In two of the five patients who developed Candida IP-SSI despite micafungin prophylaxis, micafungin was discontinued on day 3 post-transplant. The shorter course of antifungal coverage possibly contributed to the development of Candida IP-SSI. These cases potentially reinforce the need for a longer duration of antifungal prophylaxis, as suggested by the AST guidelines (2), particularly in patients with surgical complications. Alternatively, one such liver recipient developed a peri-hepatic Candida abscess despite 17 days of micafungin prophylaxis. Prior studies also suggest that echinocandin delivery to intra-abdominal sites may be insufficient to achieve concentrations capable of eliminating Candida (11–15). Yamada and colleagues analyzed the distribution of micafungin in the ascitic fluid of one patient with an invasive fungal infection and observed that the steady-state concentration of micafungin in the ascitic fluid was only 15% of that in plasma (12). Grau and colleagues performed a population pharmacokinetic study for micafungin in critically ill adult patients with proven or suspected intra-abdominal fungal infection and showed moderate to low penetration of micafungin into the peritoneal fluid with a median area under the concentration-time curve peritoneal fluid-plasma ratio of 0.3 after the first dose and at steady state (13). Zhao and colleagues investigated the tissue spatial and quantitative distribution of micafungin in a murine model and found that at steady state, micafungin diffused into hepatic abscesses at just under 5 μg/g, which was below the reported minimal concentrations that inhibit Candida drug-susceptible subpopulations (14). Welte and his team analyzed the concentrations of anidulafungin in the ascitic fluid of seven critically ill patients: anidulafungin concentrations in the ascitic fluid were lower than the simultaneous levels in plasma and below the MIC values for several pathogenic Candida strains (15). Taken together, these studies suggest the distribution of micafungin in the abdominal compartment may be limited and concentrations are suboptimal to prevent infection. While two studies have shown similar efficacy of echinocandins and fluconazole in the prevention of invasive fungal infections among high-risk liver transplant recipients (16, 17), Breitkopf and colleagues reported a high incidence (16.0%) of invasive Candida infections breaking through echinocandin prophylaxis among adults undergoing first-time liver transplant and receiving echinocandin prophylaxis (micafungin or anidulafungin) for a minimum of 7 days after transplant (18). Finally, no firm conclusions on the efficacy of echinocandin prophylaxis among high-risk liver transplant recipients can be drawn based on the randomized non-inferiority clinical trial performed by Saliba and colleagues wherein liver transplant recipients were randomized to receive prophylaxis with either micafungin or standard of care (caspofungin, fluconazole, or liposomal amphotericin B). While micafungin was determined to be non-inferior to the standard of care in the prevention of invasive fungal infections, the heterogenicity of the standard of care group prohibited definitive conclusions (19).
Study limitations
This study has multiple limitations. Based on its retrospective design, this study is prone to selection and information bias, and the external validity of this study is hampered by its single-center design. Data generated by this study reflect the epidemiology, outcomes, and management practices associated with Candida IP-SSI among adult liver transplant recipients at Duke University Hospital in the period of 2015–2020. Although we observed a statistically significant difference in the rate of Candida IP-SSIs among patients who received micafungin prophylaxis compared to patients who received fluconazole prophylaxis, our study was not randomized nor was it powered to adjust for potential confounders. Thus, the association between higher failure rates in the micafungin group compared to the fluconazole group does not provide evidence of superiority. Finally, our study lacks pharmacokinetic data regarding the distribution of micafungin in the intra-abdominal compartment.
Conclusions
In conclusion, our refined approach to antifungal prophylaxis in the adult liver transplant population successfully identified recipients at low risk for invasive Candida infections. Furthermore, our findings highlight the limitations of antifungal prophylaxis in preventing Candida IP-SSIs among patients at high risk for candidiasis after liver transplant surgery. We hypothesize that pathogen, host, and drug-associated pharmacokinetic factors contributed to the occurrence of Candida IP-SSIs despite antifungal prophylaxis. Given the complexity of liver transplant surgery, our findings reinforce the need for a risk-based, multi-pronged approach to fungal prevention, including targeted antifungal administration in patients with risks for invasive candidiasis in conjunction with close monitoring, especially among patients with complex procedures and surgical complications, with timely intervention/control of surgical leaks. Finally, further investigation into the intraabdominal pharmacokinetics and efficacy of echinocandins for preventing intraabdominal candidiasis following liver transplantation is needed.
Contributor Information
M. Carugati, Email: manuela.carugati@duke.edu.
Andreas H. Groll, University Children's Hospital Münster, Münster, Germany
DATA AVAILABILITY
All study data were maintained on a secured REDCap platform offered by the Duke Office of Clinical Research and are available upon request (20).
REFERENCES
- 1. Andes DR, Safdar N, Baddley JW, Alexander B, Brumble L, Freifeld A, Hadley S, Herwaldt L, Kauffman C, Lyon GM, Morrison V, Patterson T, Perl T, Walker R, Hess T, Chiller T, Pappas PG, TRANSNET Investigators . 2016. The epidemiology and outcomes of invasive Candida infections among organ transplant recipients in the United States: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Transpl Infect Dis 18:921–931. doi: 10.1111/tid.12613 [DOI] [PubMed] [Google Scholar]
- 2. Aslam S, Rotstein C, AST Infectious Disease Community of Practice . 2019. Candida infections in solid organ transplantations: guidelines from the American society of transplantation infectious diseases community of practice. Clin Transplant 33:e13623. doi: 10.1111/ctr.13623 [DOI] [PubMed] [Google Scholar]
- 3. Baker AW, Maziarz EK, Arnold CJ, Johnson MD, Workman AD, Reynolds JM, Perfect JR, Alexander BD. 2020. Invasive fungal infections after lung transplantation: epidemiology in the setting of antifungal prophylaxis. Clin Infect Dis 70:30–39. doi: 10.1093/cid/ciz156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Surgical site infection event. CDC-NHSN Website. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf. Accessed 01 March 2021 [Google Scholar]
- 5. Carugati M, Arif S, Sudan DL, Collins BH, Haney JC, Schroder JN, Reynolds JM, Lewis SS, Yarrington ME, Miller RA, Alexander BD. 2022. Epidemiology of surgical site infections after solid organ transplants in the period 2015-2019: a single-center retrospective cohort study. Am J Transplant 22:3021–3030. doi: 10.1111/ajt.17189 [DOI] [PubMed] [Google Scholar]
- 6. Pfeiffer CD, Garcia-Effron G, Zaas AK, Perfect JR, Perlin DS, Alexander BD. 2010. Breakthrough invasive candidiasis in patients on micafungin. J Clin Microbiol 48:2373–2380. doi: 10.1128/JCM.02390-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alexander BD, Johnson MD, Pfeiffer CD, Jiménez-Ortigosa C, Catania J, Booker R, Castanheira M, Messer SA, Perlin DS, Pfaller MA. 2013. Increasing echinocandin resistance in Candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis 56:1724–1732. doi: 10.1093/cid/cit136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cornely OA, Hoenigl M, Lass-Flörl C, Chen S-A, Kontoyiannis DP, Morrissey CO, Thompson GR, Mycoses Study Group Education and Research Consortium (MSG-ERC) and the European Confederation of Medical Mycology (ECMM) . 2019. Defining breakthrough invasive fungal infection. Position paper of the mycoses study group education and research consortium and the European confederation of medical mycology. Mycoses 62:716–729. doi: 10.1111/myc.12960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vergidis P, Clancy CJ, Shields RK, Park SY, Wildfeuer BN, Simmons RL, Nguyen MH. 2016. Intra-abdominal candidiasis: the importance of early source control and antifungal treatment. PLoS ONE 11:e0153247. doi: 10.1371/journal.pone.0153247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Viehman JA, Clancy CJ, Clarke L, Shields RK, Silveira FP, Kwak EJ, Vergidis P, Hughes C, Humar A, Nguyen MH. 2016. Surgical site infections after liver transplantation: emergence of multidrug-resistant bacteria and implications for prophylaxis and treatment strategies. Transplantation 100:2107–2114. doi: 10.1097/TP.0000000000001356 [DOI] [PubMed] [Google Scholar]
- 11. Howard SJ, Livermore J, Sharp A, Goodwin J, Gregson L, Alastruey-Izquierdo A, Perlin DS, Warn PA, Hope WW. 2011. Pharmacodynamics of echinocandins against Candida glabrata: requirement for dosage escalation to achieve maximal antifungal activity in neutropenic hosts. Antimicrob Agents Chemother 55:4880–4887. doi: 10.1128/AAC.00621-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yamada N, Kumada K, Kishino S, Mochizuki N, Ohno K, Ogura S. 2011. Distribution of micafungin in the tissue fluids of patients with invasive fungal infections. J Infect Chemother 17:731–734. doi: 10.1007/s10156-011-0240-3 [DOI] [PubMed] [Google Scholar]
- 13. Grau S, Luque S, Campillo N, Samsó E, Rodríguez U, García-Bernedo CA, Salas E, Sharma R, Hope WW, Roberts JA. 2015. Plasma and peritoneal fluid pharmacokinetics of micafungin in post-surgical patients with severe peritonitis. J Antimicrob Chemother 70:2854–2861. doi: 10.1093/jac/dkv173 [DOI] [PubMed] [Google Scholar]
- 14. Zhao Y, Prideaux B, Nagasaki Y, Lee MH, Chen P-Y, Blanc L, Ho H, Clancy CJ, Nguyen MH, Dartois V, Perlin DS. 2017. Unraveling drug penetration of echinocandin antifungals at the site of infection in an intra-abdominal abscess model. Antimicrob Agents Chemother 61:e01009-17. doi: 10.1128/AAC.01009-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Welte R, Eller P, Lorenz I, Joannidis M, Bellmann R. 2018. Anidulafungin pharmacokinetics in ascites fluid and pleural effusion of critically ill patients. Antimicrob Agents Chemother 62:e02326-17. doi: 10.1128/AAC.02326-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Winston DJ, Limaye AP, Pelletier S, Safdar N, Morris MI, Meneses K, Busuttil RW, Singh N. 2014. Randomized, double-blind trial of anidulafungin versus fluconazole for prophylaxis of invasive fungal infections in high-risk liver transplant recipients. Am J Transplant 14:2758–2764. doi: 10.1111/ajt.12963 [DOI] [PubMed] [Google Scholar]
- 17. Fortún J, Muriel A, Martín-Dávila P, Montejo M, Len O, Torre-Cisneros J, Carratalá J, Muñoz P, Fariñas C, Moreno A, Fresco G, Goikoetxea J, Gavaldá J, Pozo JC, Bodro M, Vena A, Casafont F, Cervera C, Silva JT, Aguado JM, Grupo de Estudio de Infección en Pacientes Trasplantados-Grupo de Estudio de Micología Médica (Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica), and Red Española de Investigación en Patología Infecciosa . 2016. Caspofungin versus fluconazole as prophylaxis of invasive fungal infection in high-risk liver transplantation recipients: a propensity score analysis. Liver Transpl 22:427–435. doi: 10.1002/lt.24391 [DOI] [PubMed] [Google Scholar]
- 18. Breitkopf R, Treml B, Senoner T, Bukumirić Z, Rajsic S. 2023. Invasive fungal breakthrough infections under targeted echinocandin prophylaxis in high-risk liver transplant recipients. J Fungi (Basel) 9:272. doi: 10.3390/jof9020272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Saliba F, Pascher A, Cointault O, Laterre P-F, Cervera C, De Waele JJ, Cillo U, Langer RM, Lugano M, Göran-Ericzon B, Phillips S, Tweddle L, Karas A, Brown M, Fischer L, TENPIN (Liver Transplant European Study Into the Prevention of Fungal Infection) Investigators, TENPIN Liver Transplant European Study Into the Prevention of Fungal Infection Investigators . 2015. Randomized trial of micafungin for the prevention of invasive fungal infection in high-risk liver transplant recipients. Clin Infect Dis 60:997–1006. doi: 10.1093/cid/ciu1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Carugati M, Arif S, Miller RA, Alexander BD. 2023. Data from ‘Duke University surgical site infection in solid organ transplants (SSI-SOT) database’. Database maintained on a secured REDCap platform offered by the duke office of clinical research. Database available upon request
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All study data were maintained on a secured REDCap platform offered by the Duke Office of Clinical Research and are available upon request (20).