Abstract
Background and aims:
Alcohol use disorder (AUD) is one of the strongest predictors of suicidal behavior. Here, we measured risk of suicide attempt and death as a function of AUD typologies.
Design:
We used AUD typologies from previous latent class analysis: (i) externalizing subtype (characterized by externalizing symptomatology and early age of onset; individuals in this group have lower education and higher familial/social difficulties); (ii) subtype described by minimal psychopathology; and (iii) internalizing subtype (characterized by internalizing symptomatology and later age of onset; individuals in this group have higher education). We used class membership to predict distal outcomes (attempt and death) and performed regressions to evaluate whether differences in suicidal behavior were explained by the group characteristics (sex, age of onset, number and type of AUD registrations, familial/genetic risk for AUD, externalizing and internalizing behaviors, socio-economic indicators, marital status and childhood family status). We also evaluated the effect of suicide attempt prior to AUD.
Setting and participants:
Based on longitudinal Swedish registry data, we included 217 074 individuals with AUD born 1950–80.
Measurements:
Suicide attempts were identified using medical registers and deaths using the mortality register.
Findings:
Individuals with the externalizing subtype had higher risks of suicidal behavior than other groups [attempt: externalizing versus minimal psychopathology: odds ratio (OR) = 1.35, 95% confidence interval (CI) = 1.35, 1.35; externalizing versus internalizing: OR = 1.47, 95% CI = 1.46, 1.48; death: externalizing versus minimal psychopathology: OR = 1.57, 95% CI = 1.57, 1.58; externalizing versus internalizing: OR = 1.99, 95% CI = 1.93, 2.06]. Individuals with minimal psychopathology had higher risks than those with internalizing symptomatology (attempt: OR = 1.09, 95% CI = 1.08, 1.10, death: OR = 1.26, 95% CI = 1.23, 1.30). These differences were explained by age at registration and were related to the number of registrations, sex, education, family disruption and suicide attempt prior to AUD.
Conclusions:
Among people in Sweden, considering alcohol use disorder (AUD) heterogeneity appears to be a meaningful way to evaluate suicide risk. The highest risk of suicide attempt and death occurs in the externalizing subtype of AUD, followed by the minimal psychopathology subtype, and then the internalizing subtype.
Keywords: alcohol use disorder, externalizing behaviors, heterogeneity, internalizing behaviors, non-fatal suicide attempt, suicide death, typology
INTRODUCTION
Suicidal behavior has long been studied in the context of psychiatric illness and is particularly associated with substance use disorders, personality disorders and depression [1, 2]. The associations between substance use disorders and suicidal behavior have been reported in many studies [3-6], with evidence of a possible causal pathway from alcohol use disorder (AUD) to suicide attempt and death [7-9]. Recently, research focused upon individuals with substance use disorders implicated specific factors related to a higher risk of non-fatal suicide attempt in this population. Results reveal the roles of family disruption (e.g. having lived in a non-intact family before age 15 years) and low educational attainment, as well as genetic liability for both AUD and suicide attempt [10].
For several decades, however, researchers and clinicians have asserted that AUD is not homogeneous and that parsing its heterogeneity is crucial for intervention [11, 12]. Numerous studies have been interested in the heterogeneity of AUD and describe different subtypes according to sex, age of onset, genetic factors, environment, personality traits and comorbid psychiatric disorders [13-17]. The most consistent typologies found in the literature contrast a subtype with a later AUD onset and fewer psychological impairments to an early-onset subtype associated with psychological vulnerability and personality disturbances [12]. Recently, latent class analyses were conducted in Swedish registry-based samples to further explore AUD heterogeneity [18, 19]. Using types of AUD registration (outpatient, medical, prescription and criminal), the first study identified a four-class solution, with two groups potentially reflecting prior typologies characterized by comorbid externalizing versus internalizing disorders [19]. Capitalizing on prior clinical works [12], the second study used sex, age at registration and externalizing and internalizing symptomatology and showed a three-class solution characterized by (i) externalizing disorders, (ii) minimal psychopathology and (iii) internalizing disorders [18]. These subgroups are consistent with prior typologies, some of which were derived in clinical/treatment-seeking samples [16, 17], whereas the Swedish study used a population-based cohort, perhaps explaining the addition of a group with AUD and minimal psychopathology. These subtypes are supported by differences in characteristics and external validators. The externalizing subtype of AUD is characterized by a predominance of males, early age of onset, a greater family disruption, lower educational attainment, more AUD registrations, more criminal behaviors, the highest proportion of individuals on social welfare and higher genetic liability for externalizing behaviors. The minimal psychopathology subtype is the most common, described by low rates of externalizing and internalizing disorders before AUD onset. The internalizing subtype of AUD is characterized by the highest prevalence of females, later age of onset, higher educational attainment and genetic liability for internalizing behaviors [18]. The three-class solution was very robust (mean posterior probabilities for class membership > 90%) and reproduced in additional analyses conducted on a random split half of the sample.
While AUD is a strong risk factor for suicidal behavior, it is unclear whether this risk differs across AUD typologies. Some of the factors associated with suicide attempt within individuals with substance use disorders (e.g. family disruption and low education) [10] seem to characterize the subgroup with AUD and externalizing disorders. Therefore, examining whether this group would be more at risk of engaging in suicidal behavior is of interest. Moreover, relying upon well-defined AUD typologies could help to more clearly understand which characteristics of these typologies drive the association with suicidal behavior.
In the current study, we aimed to follow-up on the Swedish population-based findings reported previously by exploring how the heterogeneity of AUD may be related to differential risk of suicidal behavior. We chose to use the typologies found by Kendler and colleagues [18], as these are in line with previous clinical works [11]. First, we evaluated how the variables characterizing those typologies are related to suicidal behavior within the entire population of individuals registered for AUD. Then, we focused upon each of the three subtypes of AUD (externalizing disorders, minimal psychopathology and internalizing disorders) and compared their risks of non-fatal suicide attempt and suicide death. Finally, we investigated whether distinct risks of suicide attempt and death across AUD typologies were related to specific confounding factors such as AUD characteristics (age of onset and number of registrations), family status, education or genetic risks, as these were identified as good external validators between AUD typologies [18] and risk factors that explained suicide attempt among individuals with substance use disorders [10] and suicide death [20]. We also accounted for suicide attempt prior to AUD, as this is a strong predictor of further attempts and death [21, 22].
METHOD
We analyzed information on individuals from Swedish population-based registers with national coverage. The registers were linked using each person’s unique identification number replaced by a serial number to preserve confidentiality. We secured ethical approval from the Regional Ethical Review Board in Lund (no. 2008/409 and later amendments).
We based this analysis on data from 217 074 individuals born in Sweden from 1950 to 1980 and registered with AUD (Supporting information, Table S1). We relied upon prior results from a latent class analysis to determine AUD typologies [18]. We used the same database and expanded it with information on non-fatal suicide attempt and suicide death during follow-up time [time from AUD registration to suicide attempt, death, emigration or end of follow-up (31 December 2018)]. In addition, we included several variables that might confound the association between the three AUD typologies and suicidal behavior. The variables we included were sex, age at AUD registration, suicide attempt prior to AUD, year of birth, educational attainment, number of AUD registrations, type of AUD registration (prescription, medical and criminal; Supporting information, Table S1), information on early retirement (similar to long-term disability in the United States), unemployment status, social welfare receipt, neighborhood deprivation, marital status and family status during childhood (i.e. intact family is defined as residing with both parents from ages 0 to 15 years). We also included three familial genetic risk scores (FGRS) for AUD and externalizing and internalizing behaviors (Supporting information, Tables S1 and S2). The FGRS are calculated from morbidity risks for disorders in first- to fifth-degree relatives, controlling for cohabitation effects, and thus arise from phenotypes in extended pedigrees within the whole Swedish population, not from molecular genetic data. Recent evidence indicates FGRS as a good indicator of genetic liability [23]. See Supporting information for a definition of registers and variables. To account for potential differences in data availability across cohorts, variables related to AUD characteristics and socio-economic status have been standardized by year of birth.
Statistical analysis
First, we explored how the variables characterizing AUD typologies (both the variables used to create the classes and the external validators) were related to suicidal behavior by conducting univariable logistic regression models. We estimated the association between the predictor variables and non-fatal suicide attempt/suicide death in the whole population of individuals with AUD (n = 217 074), and reported odds ratios (ORs) and 95% confidence intervals (CI).
Secondly, we compared the risk of non-fatal suicide attempt/suicide death among AUD typologies (externalizing disorders, minimal psychopathology and internalizing disorders) using the Bolck, Croon, Hagenaars (BCH) method [24]. Prior simulations using this method show that BCH outperforms other methods that predict auxiliary outcomes because it avoids shifts in latent class in the final stage of the analysis. It also takes into account uncertainty in the probability of belonging to a specific class, which is important when trying to predict distal outcomes based on class membership. The BCH method is utilized to predict the distal outcomes (suicide attempt/death) in the three latent classes obtained in Kendler et al. [18] and requires two steps. In the first step, we estimated the latent class measurement model and saved the weights that reflect the measurement error of the latent class variable. In the second step, we evaluated class-specific regressions of suicide attempt/death on the predictor variables. We present BCH weighted ORs and 95% CI. The three ORs compare the odds for suicide attempt/death in the three classes (AUD typologies).
Finally, to investigate if the risk of suicidal behavior in these groups was related to specific confounding factors, we used the ORs from the previous model (BCH) and controlled them for the predictor variables. The predictor variables were entered one at a time in univariate regression models with suicide attempt/death as outcomes. To evaluate the change in group differences between models, we used a relative measure that informs about the percentage of change in the ORs [25]. The percentage of change was measured on the log odds scale. For all calculations we used the Mplus software version 7.31 [26]. This project was not pre-registered on a publicly available platform, and analysis and results should be considered exploratory.
RESULTS
Descriptive analyses
Standardized group characteristics are reported in Table 1; unstandardized data are available by 10-year birth cohort in the Supporting information. We found a small proportion of missing data (7.5%) for the neighborhood deprivation variable and performed imputation based on similar covariates (Supporting information).
TABLE 1.
Description of the subgroups with alcohol use disorder (AUD).
| AUD externalizing n = 68 866 |
AUD minimal psychopathology n = 99 324 |
AUD internalizing n = 48 881 |
|
|---|---|---|---|
| Suicide attempt | 22% | 17.6% | 16.7% |
| Suicide death | 5.3% | 3.5% | 2.9% |
| Mean or % | Mean or % | Mean or % | |
| Sex (% females) | 9.0% | 28.5% | 52.2% |
| Age at AUD registration | −0.42 | −0.23 | 0.96 |
| Suicide attempt prior to AUD | 7.2% | 3.4% | 18.2% |
| Year of birth | 1.06 | 0.97 | 1.25 |
| Educational attainment | 10.6 | 11.7 | 12.0 |
| Family genetic risk scores | |||
| FGRSAUD | 0.783 | 0.409 | 0.497 |
| FGRSIB | 0.233 | 0.122 | 0.412 |
| FGRSEB | 0.678 | 0.208 | 0.293 |
| Number of registrations | 0.22 | −0.08 | −0.09 |
| Type of AUD registration | |||
| Criminal versus medical | 54.4% | 33.7% | 8.5% |
| Prescription versus medical | 27.4% | 30.4% | 56.6% |
| Early retirement | 0.00 | −0.14 | 0.28 |
| Unemployment | 0.97 | 0.62 | 0.53 |
| Social welfare | 0.28 | −0.19 | −0.01 |
| Neighborhood deprivation | 0.61 | 0.13 | 0.29 |
| Marital status (married) | 1.34 | 2.57 | 2.47 |
| Intact family during childhood | 50.6% | 67.6% | 62.4% |
Age at AUD registration, FGRS, number of registrations, early retirement and social welfare are standardized values with mean of 0 and standard deviation (SD) of 1. FGRS are standardized based on the general population (mean = 0); scores higher than 0 in this AUD population-based sample reflect higher genetic risk than the general population. Unemployment, neighborhood deprivation and marital status represent the mean number of years during follow-up time.
AUD = alcohol use disorder, FGRS = family genetic risk score.
The mean age in our sample [standard deviation (SD)] for suicide attempt was 36.4 (12.2) years and the mean age for suicide death was 40.4 (11.3) years. The outcomes had to occur after the first AUD registration: we thus evaluated the risk of non-fatal suicide attempt after AUD; suicide attempts that occurred prior to the first AUD registration were accounted for analytically.
In individuals classified with the externalizing subtype of AUD, the prevalence of suicide attempt was 22% and the prevalence of suicide death was 5.3%. Among AUD with the minimal psychopathology subtype, 17.6% of individuals attempted suicide and 3.5% died by suicide. In individuals classified with the internalizing subtype of AUD, the prevalence was 16.7% for suicide attempt and 2.9% for suicide death.
Risk for non-fatal suicide attempt
First, we explored whether the factors characterizing AUD typologies were positively or negatively associated with suicide attempt, using the full sample of individuals with AUD. Results are presented in Table 2 and showed that being married, having lived in an intact family during childhood, higher educational attainment and early retirement were related to lower risk of suicide attempt.
TABLE 2.
Univariable regressions for risk of suicidal behavior (non-fatal suicide attempt and suicide death) in the entire sample of individuals with alcohol use disorder (AUD; n = 217 071).
| Mean or % | Suicide attempt OR (95% CI) |
Suicide death OR (95% CI) |
|
|---|---|---|---|
| Sex (females versus males) | 27.7 | 1.72 (1.69, 1.77) | 0.87 (0.83, 0.92) |
| Age at AUD registration | −0.02 | 0.57 (0.56, 0.58) | 0.59 (0.58, 0.61) |
| Suicide attempt prior to AUD | 8.0% | 2.90 (2.80, 2.99) | 2.28 (2.15, 2.42) |
| Year of birth | 1.06 | 1.08 (1.06, 1.09) | 0.65 (0.63, 0.67) |
| Educational attainment | 11.4 | 0.92 (0.91, 0.92) | 0.90 (0.89, 0.91) |
| Family genetic risk scores | |||
| FGRSAUD | 0.55 | 1.16 (1.15, 1.17) | 1.06 (1.05, 1.08) |
| FGRSinternalizing | 0.22 | 1.18 (1.17, 1.19) | 1.07 (1.05, 1.09) |
| FGRSexternalizing | 0.38 | 1.23 (1.22, 1.24) | 1.11 (1.08, 1.13) |
| Number of registrations | 0.00 | 1.67 (1.65, 1.69) | 0.99 (0.97, 1.01) |
| Type of AUD registration | |||
| Criminal versus medical | 34.6% | 0.97 (0.95, 1.00) | 0.76 (0.73, 0.80) |
| Prescription versus medical | 35.3% | 0.99 (0.97, 1.02) | 0.38 (0.36, 0.41) |
| Early retirement | 0.00 | 0.98 (0.97, 0.99) | 0.88 (0.86, 0.90) |
| Unemployment | 0.71 | 1.06 (1.06, 1.08) | 0.96 (0.94, 0.98) |
| Social welfare | 0.00 | 1.15 (1.14, 1.16) | 1.04 (1.01, 1.06) |
| Neighborhood deprivation | 0.32 | 1.10 (1.09, 1.11) | 1.08 (1.06, 1.09) |
| Marital status (married) | 2.18 | 0.92 (0.92, 0.92) | 0.89 (0.88, 0.89) |
| Intact family during childhood | 61.0% | 0.72 (0.70, 0.74) | 0.69 (0.66, 0.72) |
FGRS are standardized based on the general population (mean = 0); scores higher than 0 in this AUD population-based sample reflect higher genetic risk than the general population.
AUD = alcohol use disorder, CI = confidence intervals, FGRS = family genetic risk score, OR = odds ratio.
Results also implicated characteristics associated with an increased risk of suicide attempt among individuals with AUD: being female, having a suicide attempt prior to AUD registration, younger age at AUD registration, higher number of AUD registrations; higher FGRS for AUD, internalizing behaviors, externalizing behaviors; and socio-economic difficulties (unemployment, social welfare and neighborhood deprivation).
Comparison between AUD typologies
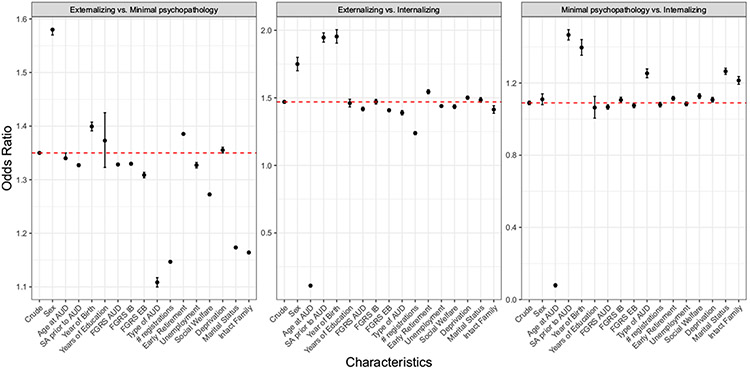
Results are depicted in Figure 1 and Supporting information, Table S3.
FIGURE 1.
Risk of non-fatal suicide attempt across alcohol use disorder (AUD) typologies. The y-axes depict the odds ratios for the group difference in risk for non-fatal suicide attempt. The y-axes are on the linear scale for a better interpretation of the differences in effect sizes. The first point represents the crude association (extended by the dashed red horizontal line) and the subsequent points represent the odds ratios for the group difference controlled for a specific predictor (mentioned in the x-axes). FGRS, family genetic risk score; IB, internalizing behaviors; EB, externalizing behaviors; # registrations, number of AUD registrations; Deprivation, neighborhood deprivation.
Externalizing versus minimal psychopathology
Risk for suicide attempt was higher among individuals having externalizing compared to minimal psychopathology subtypes of AUD (OR = 1.35, 95% CI = 1.35, 1.35). We explored how specific factors drove this difference (change in OR; see Figure 1), and found that controlling for type of AUD registration (e.g. medical versus criminal) or number of AUD registrations explained more than 50% of the increased odds in those with the externalizing subtype (Supporting information, Table S3). This may be due to the higher rates of criminal registration and number of AUD registrations in this group. We found other factors with a high explanatory power for this group difference: having lived in an intact family during childhood (OR = 1.16, 95% CI = 1.16, 1.17) and being married (OR = 1.17, 95% CI = 1.17, 1.18) explained 49.4 and 46.7%, respectively, of the odds among individuals with AUD from the externalizing subtype; that is, controlling for those factors attenuated the magnitude of difference in risk for suicide attempt.
Externalizing versus internalizing
Results showed that individuals having the externalizing subtype of AUD were at higher risk for suicide attempt than individuals having the internalizing subtype (OR = 1.47, 95% CI = 1.46, 1.48). Accounting for suicide attempt prior to AUD registration reinforced this difference, leading to 72.9% increase in the odds of suicide attempt in the externalizing subtype (Supporting information, Table S3). However, controlling for group characteristics reduced the group difference. The most significant variations were observed for AUD-related variables: number of AUD registrations decreased the OR (OR = 1.24, 95% CI = 1.23, 1.25) and age at AUD registration led to an inversion of the effect, such that the odds for suicide attempt were much lower in externalizing than internalizing subtypes (OR = 0.11, 95% CI = 0.10, 0.11).
Minimal psychopathology versus internalizing
Risk for suicide attempt was higher among individuals having AUD with minimal psychopathology compared to the internalizing subtype (OR = 1.09, 95% CI = 1.08, 1.10), and this difference was strengthened when accounting for various risk and protective factors; that is, suicide attempt prior to AUD, type of AUD registration, being married and having lived in an intact family during childhood which led to higher ORs. However, accounting for age at AUD registration led to an OR < 1, suggesting lower suicide attempt risk in the minimal psychopathology than in the internalizing subtype (OR = 0.08, 95% CI = 0.07, 0.08).
Risk for suicide death
Primary analyses indicated that type of AUD registration, having lived in an intact family during childhood, being a woman, being married, early retirement and having higher education were related to lower risk of suicide death (Table 2).
Results also implicated the following risk factors for suicide among individuals with AUD: having a suicide attempt prior to AUD registration, a younger age at AUD registration; higher FGRS for AUD, internalizing behaviors, externalizing behaviors; and socio-economic difficulties (unemployment, social welfare and neighborhood deprivation).
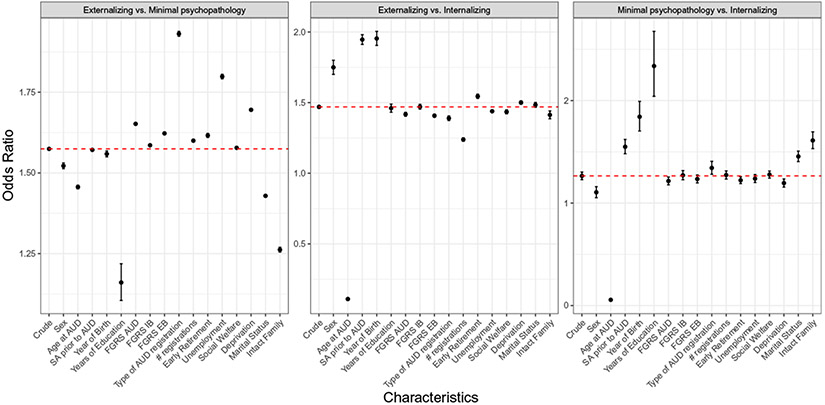
Comparison between AUD typologies
Results are depicted in Figure 2 and Supporting information, Table S4.
FIGURE 2.
Risk of suicide death across alcohol use disorder (AUD) typologies. The y-axes depict the odds ratios for the group difference in risk for suicide death. The y-axes are on the linear scale for a better interpretation of the differences in effect sizes. The first point represents the crude association (extended by the dashed red horizontal line) and the subsequent points represent the odds ratios for the group difference controlled for a specific predictor (mentioned in the x-axes). FGRS, family genetic risk score; IB, internalizing behaviors; EB, externalizing behaviors; # registrations, number of AUD registrations; Deprivation, neighborhood deprivation.
Externalizing versus minimal psychopathology
Results showed that individuals with the externalizing subtype of AUD were at higher risk for suicide death than individuals with the minimal psychopathology subtype (OR = 1.57, 95% CI = 1.57, 1.58). We also investigated how specific factors explained this difference (Figure 2), and found that it was reinforced by socio-economic variables and group characteristics, with type of AUD registration (OR = 1.93, 95% CI = 1.92, 1.94) showing the strongest increase (change in OR for suicide death of 44.9%; Supporting information, Table S4), probably due to the higher rates of criminal registrations in the externalizing subgroup. Moreover, we found that accounting for potentially protective factors decreased this group difference: educational attainment (OR = 1.16, 95% CI = 1.11, 1.22) and having lived in an intact family during childhood (OR = 1.26, 95% CI = 1.25, 1.27) explained, respectively, 67.2 and 48.7% of the increased odds of death in individuals with the externalizing subtype of AUD.
Externalizing versus internalizing
Risk of suicide death was higher among individuals having externalizing compared to internalizing subtype of AUD (OR = 1.99, 95% CI = 1.93, 2.06). We explored the roles of specific factors and found that group characteristics strengthened this difference, especially educational attainment (OR = 2.71, 95% CI = 2.49, 2.96, change in OR for suicide = 44.8%). Sex decreased the group difference (Supporting information, Table S5), whereas age at AUD registration inverted the OR to below 1 (OR = 0.08, 95% CI = 0.07, 0.09).
Minimal psychopathology versus internalizing
Results showed a higher risk of suicide death in individuals with the minimal psychopathology than the internalizing subtype of AUD (OR = 1.26, 95% CI = 1.23, 1.30). Accounting for potential protective factors led to a more pronounced difference: educational attainment (OR = 2.34, 95% CI = 2.04, 2.68), intact family during childhood (OR = 1.61, 95% CI = 1.53, 1.70) and being married (OR = 1.45, 95% CI = 1.40, 1.51) increased the odds of those with minimal psychopathology by more than 50% (Supporting information, Table S5). Some group characteristics also reduced the difference: age at AUD registration led to an OR < 1 (OR = 0.06, 95% CI = 0.05, 0.06), indicating a lower suicide risk in the minimal psychopathology subgroup, while sex decreased the group difference with a change in OR for suicide of 56.4% (OR = 1.11, 95% CI = 1.05, 1.16).
DISCUSSION
The current study evaluates the risk of suicidal behavior as a function of AUD typologies. Individuals with AUD have higher risks of suicide attempt and death compared to population-based samples [8], but also relative to populations with other psychiatric disorders [1]. AUD is described as a heterogenous syndrome, and consistent classifications have been proposed to account for personal and drinking-related differences [12]. We capitalized on recent typologies from a latent class analysis in a Swedish cohort of individuals with AUD [18] to evaluate the risks of suicide attempt and death among three subgroups with AUD (externalizing symptomatology, minimal psychopathology and internalizing symptomatology). We also investigated which characteristics of these subgroups explain the differential risk of suicidal behavior.
Our findings indicate a higher prevalence of suicide attempt and death in the externalizing subtype of AUD compared to minimal psychopathology and internalizing subtypes. These results underscore that individuals with AUD who are characterized by criminal behaviors, multiple AUD registrations, high genetic risks for externalizing disorders and AUD, low education and family disruption [18] have a higher risk of suicidal behavior. This observation is consistent with prior evidence obtained in individuals with substance use disorders [10], while we expand this to specific comparisons between AUD typologies for suicidal behaviors (non-fatal attempt and death). The focus upon AUD typologies also further informs about the importance of externalizing behaviors, suggesting the role of potential etiological factors that are common to externalizing symptomatology and suicidal behavior; for example, impulsivity [27]. Previous studies demonstrate a shared genetic and environmental etiology between substance use disorders and suicidal behavior [28, 29], whereas genetic correlations have been found between suicidal behavior and characteristics of externalizing behaviors such as risk-taking [30], disinhibition [31] and impulsivity [32].
In addition, we observed that individuals with AUD characterized by minimal psychopathology had higher risks of suicide attempt and death than those with internalizing disorders. This may seem unexpected, because of prior associations between depression and suicidal behavior [2, 33]. However, a recent meta-analysis of studies conducted in general populations indicates that these associations were weak to modest [34]. Moreover, individuals with AUD and internalizing symptomatology are characterized by higher educational attainment, which is an important and potentially causal protective factor for suicidal behavior [35, 36]. Individuals in this subgroup also have a later age of AUD onset, suggesting that AUD might be a consequence of internalizing disorders whereas, in other groups, AUD is hypothesized as a causal factor for suicidal behavior [7, 8]. Two other points are worth mentioning: first, while it did not explain the whole difference between groups, the rate of suicide attempts prior to AUD is higher in those with internalizing symptomatology than in other groups. Secondly, although significant, the difference in the prevalence of suicide attempt between internalizing and minimal psychopathology subtypes is 1.1%.
In a second analysis, we evaluated whether specific factors may explain the risks of suicide attempt and death among AUD subgroups. There are several points of interest in these results. First, accounting for the number of AUD registrations attenuated the magnitude of increased risk in the externalizing subtype compared to other groups. This suggests that the number of registrations is strongly related to suicidal behavior in individuals with AUD and externalizing disorders, consistent with the hypothesis that this group is characterized by elevated impulsivity (e.g. more hospitalizations for alcohol intoxications, more criminal behaviors, potentially more relapses). Secondly, controlling for sex intensified the higher magnitude of suicide attempt risk in the externalizing subtype (which is male-preponderant) compared to other groups. This was not observed for suicide death, which may reflect the sex difference previously described in suicidal behavior [37]. Thirdly, accounting for suicide attempt prior to AUD registration reinforced the group differences with the internalizing subtype of AUD; that is, lowering their risk of suicide attempt compared to other groups. This might be explained by the fact that individuals are older in the internalizing group [18] and may have engaged in suicidal behavior prior to their AUD registration. These findings support previous suicide attempts as a risk factor for further attempts [21, 38]; however, in line with recent findings suggesting that suicidal behaviors are not on a continuum of liability [39, 40], we did not observe a role of prior attempts in relation to the group differences for suicide death.
Fourthly, age at AUD registration inverted the group differences, suggesting that the higher risk of suicidal behavior in subtypes with externalizing symptomatology and minimal psychopathology was mainly related to a younger age of AUD onset. Younger age at AUD registration was associated with increased risks of suicide attempt and death in our primary analyses. When looking at the group differences, after controlling for age at AUD registration, individuals classified with the internalizing subtype were at greater risk for suicidal behavior than others. Although previous studies conducted in general populations indicate that people with externalizing disorders have a higher risk for suicidal behavior [1], this study focused upon a sample of individuals with AUD in which comorbid internalizing symptomatology may add to the risk of an externalizing disorder (i.e. AUD). It is worth noting, however, that age at registration could be an index of overall liability and/or genetic risk for AUD and other externalizing disorders [41-44]. Age of onset of substance use is also related to low education [42, 45] and suicidal behavior [44, 46]. Controlling for age at registration may thus account for various externalizing traits. Moreover, no individuals classified with the internalizing subtype of AUD have an age of onset below age 25 years [18], which may explain the modification in group differences, especially compared to those with minimal psychopathology.
These findings should be viewed in the context of potential limitations. First, we relied upon medical registries to evaluate suicide attempt. Although it constitutes an objective evaluation, it means that all the attempts included in this study came to the attention of medical workers and thus probably reflect medically serious attempts. As the characteristics of suicide attempts (e.g. impulsivity and severity) [47] might differ among our subgroups, confirmation of our findings is needed in future studies where such details are available. Secondly, consistent with previous studies [39, 40, 48, 49], our definition of suicide included undetermined intent deaths (i.e. certification of deaths under undetermined circumstances). Recent results suggest that the inclusion of undetermined intent deaths should be defined according to the research question [20]. We balanced two primary concerns in making our decision: (1) our research was conducted in a subpopulation of individuals with AUD. Although we evaluated subgroups with externalizing versus internalizing disorders, this was conducted within the context of AUD, thus limiting the impact of potential distinct etiologies between these deaths; and (2) the exclusion of undetermined intent deaths has been associated with a reduced estimation of suicidal behavior in previous studies [50]. Nonetheless, our estimates should be considered conservative. Thirdly, to minimize cohort and register effects, the variables related to AUD characteristics and socio-economic status were standardized by birth year. Nevertheless, the availability of other variables, such as suicide attempts prior to AUD, might also differ between cohorts. It is possible that considering age of onset on a time scale (rather than standardized) would lower its effect size. As age at registration appears to be the main explanatory variable in our results, the robustness of its effect needs to be replicated in future studies. Fourthly, one socio-economic indicator (neighborhood deprivation) had a small proportion of missing data and was imputed based on other covariates. Finally, we used logistic regression models to evaluate the role of group characteristics, as recommended with the BCH method. However, further research could improve these results by using survival analyses. It is also worth noting that we conducted post-hoc analyses to evaluate whether the group differences were explained by specific characteristics, but because of correlations between our predictors these analyses have not been controlled for multiple comparisons.
To conclude, this research represents an additional contribution to help understanding of the risk of suicidal behavior in AUD. Our results support the high prevalence of suicide attempt and death in this population. Capitalizing on recent findings [18] to account for AUD heterogeneity, we found differential risk of suicidal behavior across AUD typologies. Individuals whose AUD is characterized by comorbidity with externalizing disorders had the highest risks of non-fatal suicide attempt and suicide death. This effect was mainly explained by their age at registration for AUD, which may constitute a proxy for externalizing behaviors. When controlling for age at registration, individuals with AUD and internalizing disorders appeared to have the highest risk of suicidal behavior. Considering AUD characteristics through well-validated typologies could be a clinically meaningful way to improve risk assessment for suicidal behavior. In particular, this study emphasizes the importance of variables that can be easily accessible to clinicians (age of onset, sex, age, education, prior suicide attempts, externalizing and internalizing behaviors), thus offering concrete and reliable targets to assess the risk of suicidal behavior among patients with AUD.
Supplementary Material
ACKNOWLEDGEMENTS
This project was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA, grant numbers: AA027522 and AA023534), and funding from the Swedish Research Council (2020-01175) and ALF (Region Skåne).
Footnotes
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
DATA AVAILABILITY STATEMENT
Data from the Swedish registers are not publicly available.
REFERENCES
- 1.Barak-Corren Y, Castro VM, Javitt S, Hoffnagle AG, Dai Y, Perlis RH, et al. Predicting suicidal behavior from longitudinal electronic health records. Am J Psychiatry. 2017;74:154–62. [DOI] [PubMed] [Google Scholar]
- 2.Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry. 1996;153:1001–8. [DOI] [PubMed] [Google Scholar]
- 3.Lynch FL, Peterson EL, Lu CY, Hu Y, Rossom RC, Waitzfelder BE, et al. Substance use disorders and risk of suicide in a general US population: a case control study. Addict Sci Clin Pract. 2020;15:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hesse M, Thylstrup B, Seid AK, Skogen JC. Suicide among people treated for drug use disorders: a Danish national record-linkage study. BMC Public Health. 2020;20:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017;112:1193–201. [DOI] [PubMed] [Google Scholar]
- 6.Colbert SMC, Hatoum AS, Shabalin A, Li QS, Coon H, Nelson EC, et al. Exploring the genetic overlap of suicide-related behaviors and substance use disorders. Am J Med Genet B Neuropsychiatr Genet. 2021;186:445–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards AC, Ohlsson H, Moscicki E, Crump C, Sundquist J, Kendler KS, et al. Alcohol use disorder and non-fatal suicide attempt: findings from a Swedish national cohort study. Addiction. 2022;117:96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edwards AC, Ohlsson H, Sundquist J, Sundquist K, Kendler KS. Alcohol use disorder and risk of suicide in a Swedish population-based cohort. Am J Psychiatry. 2020;177:627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lannoy S, Ohlsson H, Sundquist J, Sundquist K, Edwards AC. Roles of alcohol use disorder and resilience in risk of suicide attempt in men: a Swedish population-based cohort. Suicide Life Threat Behav. 2022;52:341–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lannoy S, Ohlsson H, Stephenson M, Kendler KS, Sundquist J, Sundquist K, et al. Risk of non-fatal suicide attempt in individuals with substance use disorder: the roles of aggregate genetic liability and environmental exposures in a Swedish population-based cohort. Addiction. 2022;117:2943–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leggio L, Kenna GA, Fenton M, Bonenfant E, Swift RM. Typologies of alcohol dependence. From Jellinek to genetics and beyond. Neuropsychol Rev. 2009;19:115–29. [DOI] [PubMed] [Google Scholar]
- 12.Babor TF. The classification of alcoholics. Typology theories from the 19th century to the present. Alcohol Health Res World. 1996;20:6–14. [PMC free article] [PubMed] [Google Scholar]
- 13.Cloninger RC, Bohman M, Sigvardsson S. Inheritance of alcohol abuse. Arch Gen Psychiatry. 1981;38:861–8. [DOI] [PubMed] [Google Scholar]
- 14.Cloninger RC, Sigvardsson S, Bohman M. Type I and type II alcoholism: an update. Alcohol Health Res World. 1996;20:18–23. [PMC free article] [PubMed] [Google Scholar]
- 15.Moss H, Chen CM, Yi H. Subtypes of alcohol dependence in a nationally representative sample. Drug Alcohol Depend. 2007;91:149–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Babor TF, Dolinsky ZS, Meyer RE, Hesselbrock M, Hofmann M, Tennen H. Types of alcoholics: concurrent and predictive validity of some common classification schemes. Br J Addict. 1992;87:1415–31. [DOI] [PubMed] [Google Scholar]
- 17.Windle M, Scheidt DM. Alcoholic subtypes: are two sufficient? Addiction. 2004;99:1508–19. [DOI] [PubMed] [Google Scholar]
- 18.Kendler KS, Ohlsson H, Sundquist J, Sundquist K. The typology of alcohol use disorder: latent class analyses of a population-based Swedish sample. J Stud Alcohol Drugs. 2022;83:672–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Long EC, Ohlsson H, Sundquist J, Sundquist K, Kendler KS. Different characteristics and heritabilities of alcohol use disorder classes: a population-based Swedish study. Alcohol Alcohol. 2019;54:647–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards AC, Ohlsson H, Moscicki EK, Sundquist J, Crump C, Kendler KS, et al. Genetic differences between suicide deaths and deaths of undetermined intent. Suicide Life Threat Behav. 2022;53:100–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beghi M, Rosenbaum JF. Risk factors for fatal and nonfatal repetition of suicide attempt: a critical appraisal. Curr Opin Psychiatry. 2010;23:349–55. [DOI] [PubMed] [Google Scholar]
- 22.Lannoy S, Ohlsson H, Kendler KS, Sundquist J, Sundquist K, Edwards AC. Examining common and distinct contributions to the etiology of suicide attempt and reattempt. J Psychopathol Clin Sci. 2023;132:165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kendler KS, Ohlsson H, Sundquist J, Sundquist K. Risk for mood, anxiety, and psychotic disorders in individuals at high and low genetic liability for bipolar disorder and major depression. JAMA Psych. 2022;79:1102–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asparouhov T, Muthen B. Auxiliary variables in mixture modeling: using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes. 2021;21:1–22. [Google Scholar]
- 25.Agresti A. Categorical Data Analysis Hoboken, NJ: Wiley; 2012. [Google Scholar]
- 26.Muthen LK, Muthen BO. Mplus User’s Guide Los Angeles, CA: Muthen & Muthen; 1998–2012. [Google Scholar]
- 27.Dougherty DM, Mathias CW, Marsh DM, Moeller FG, Swann AC. Suicidal behaviors and drug abuse: impulsivity and its assessment. Drug Alcohol Depend. 2004;76:S93–S105. [DOI] [PubMed] [Google Scholar]
- 28.Edwards AC, Ohlsson H, Lannoy S, Stephenson M, Crump C, Sundquist J, et al. Shared genetic and environmental etiology between substance use disorders and suicidal behavior. Psychol Med. 2022;53:2380–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deak JD, Levey DF, Wendt FR, Zhou H, Galimberti M, Kranzler HR, et al. Genome-wide investigation of maximum habitual alcohol intake in US veterans in relation to alcohol consumption traits and alcohol use disorder. JAMA Netw Open. 2022;5:e2238880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mullins N, Kang J, Campos A, Coleman JRI, Edwards AC, Galfalvy H, et al. Dissecting the shared genetic architecture of suicide attempt, psychiatric disorders and known risk factors. Biol Psychiatry. 2021;91:313–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Docherty AR, Shabalin AA, DiBlasi E, Monson E, Mullins N, Adkins DE, et al. Genome-wide association study of suicide death and polygenic prediction of clinical antecedents. Am J Psychiatry. 2020;177:917–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stephenson M, Lannoy S, Edwards AC. Shared genetic liability for alcohol consumption, alcohol problems, and suicide attempt: evaluating the role of impulsivity. Transl Psychiatry. 2023;13:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hawton K, Casanas ICC, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147:17–28. [DOI] [PubMed] [Google Scholar]
- 34.Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. 2018;212:279–86. [DOI] [PubMed] [Google Scholar]
- 35.Lannoy S, Ohlsson H, Kendler KS, Sundquist J, Sundquist K, Edwards AC. The causal effect of education and cognitive performance on risk for suicide attempt: a combined instrumental variable and co-relative approach in a Swedish national cohort. J Affect Disord. 2022;305:115–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosoff DB, Kaminsky ZA, McIntosh AM, Davey SG, Lohoff FW, Educational attainment reduces the risk of suicide attempt among individuals with and without psychiatric disorders independent of cognition: a bidirectional and multivariable Mendelian randomization study with more than 815,000 participants. Transl Psychiatry. 2020;10:388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miranda-Mendizabal A, Castellvi P, Pares-Badell O, Alayo I, Almenara J, Alonso I, et al. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health. 2019;64:265–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans, and attempts. Br J Psychiatry. 2009;192:98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kendler KS, Ohlsson H, Sundquist J, Sundquist K, Edwards AC. The sources of parent-child transmission of risk for suicide attempt and deaths by suicide in Swedish national samples. Am J Psychiatry. 2020;177:928–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edwards AC, Ohlsson H, Moscicki E, Crump C, Sundquist J, Lichtenstein P, et al. On the genetic and environmental relationship between suicide attempt and death by suicide. Am J Psychiatry. 2021;178:1060–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karlsson LR, Mallard TT, Barr PB, Sanchez-Roige S, Madole JW, Driver MN, et al. Multivariate analysis of 1.5 million people identifies genetic associations with traits related to self-regulation and addiction. Nat Neurosci. 2021;24:1367–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kendler KS, Ohlsson H, Sundquist K, Sundquist J. Prediction of drug abuse recurrence: a Swedish national study. Psychol Med. 2018;48:1367–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kendler KS, Ohlsson H, Edwards A, Sundquist J, Sundquist K. The clinical features of alcohol use disorders in biological and step-fathers that predict risk for alcohol use disorders in offspring. Am J Med Genet B Neuropsychiatr Genet. 2017;174:779–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DuRant RH, Smith JH, Kreiter SR, Krowchuk DP. The relationship between early age of onset of initial substance use and engaging in multiple health risk behaviors among young adolescents. Arch Pediatr Adolesc Med. 1999;153:86–291. [DOI] [PubMed] [Google Scholar]
- 45.Grant JD, Scherrer JF, Lynskey MT, Agrawal A, Duncan AE, Haber JR, et al. Associations of alcohol, nicotine, cannabis, and drug use/dependence with educational attainment: evidence from cotwin-control analyses. Alcohol Clin Exp Res. 2012;36:1412–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ahuja M, Awasthi M, Records K, Lamichhane RR. Early age of alcohol initiation and its association with suicidal behaviors. Subst Use Misuse. 2021;56:1332–8. [DOI] [PubMed] [Google Scholar]
- 47.Lopez-Castroman J, Nogue E, Guillaume S, Picot MC, Courtet P. Clustering suicide attempters: impulsive-ambivalent, well-planned, or frequent. J Clin Psychiatry. 2016;77:e711–8. [DOI] [PubMed] [Google Scholar]
- 48.von Borczyskowski A, Lindblad F, Vinnerljung B, Reintjes R, Hjern A. Familial factors and suicide: an adoption study in a Swedish national cohort. Psychol Med. 2011;41:749–58. [DOI] [PubMed] [Google Scholar]
- 49.Crump C, Sundquist K, Sundquist J, Winkleby MA. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychol Med. 2014;44:279–89. [DOI] [PubMed] [Google Scholar]
- 50.Chang SS, Sterne JA, Lu TH, Gunnell D. ‘Hidden’ suicides amongst deaths certified as undetermined intent, accident by pesticide poisoning and accident by suffocation in Taiwan. Soc Psychiatry Psychiatr Epidemiol. 2010;45:143–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from the Swedish registers are not publicly available.