Abstract
Introduction:
South Africa has one of the highest incidences of HIV among adolescent girls and young women (AGW), ages 15–24, and recent research has focused on developing interventions for HIV prevention. However, the South African National Health Act requires those under 18 years of age to obtain a guardian’s permission to participate in research. Limiting research enrolment to AGYW who can obtain guardian consent may lead to non-representative findings. Therefore, innovative, inclusive consent approaches that protect AGYW from the risks of research are needed.
Methods:
This report details the development and implementation of an approach called the in loco parentis (in place of parent) consent procedure. In loco parentis consent provides a vehicle for adolescent participation that protects adolescents from potential social harms. The in loco parentis consent procedure does not seek to obtain independent minor consent but seeks to obtain permission for the minor to participate in research from a trusted adult who is not a minor’s parent or legal guardian. This report also qualitatively explores the experiences of 31 AGYW who were recruited into a behavioral HIV prevention study using this method.
Results:
Findings suggest that the in loco parentis consent procedure is a feasible and acceptable method to inclusively AGYW in HIV research.
Conclusions:
The in loco parentis procedure may provide a more inclusive strategy to recruit AGYW for HIV research to increase the generalizability of findings.
Keywords: Regulations, Consent, Assent, HIV, Substance use, Ethics
Adolescent girls and young women (AGYW) represent 25% of new HIV infections in South Africa (Joint United Nations Programme on HIV/AIDS, 2016a). Recently, research has focused on reaching AGYW to develop and disseminate biobehavioral interventions, including preexposure prophylaxis (PrEP) for HIV prevention (Celum et al., 2019; JointUnited Nations Programme on HIV/AIDS, 2016b). However, Section 71 of the South African National Health Act requires those under 18 years of age to consent as well as obtain guardian consent to participate in research, excluding some AGYW from research participation (Parliament of South Africa, 2004).
Limiting trial enrollment to AGYW who obtain guardian consent may lead to non-representative findings about the safety, acceptability, and feasibility of HIV prevention methods (Fisher & Mustanski, 2014). For example, there may be differences (e.g., familial support) between AGYW whose guardians will consent to their participation in an HIV prevention trial and those whose guardians will not (Liu, Cox, Washburn, Croff, & Crethar, 2017). Therefore, findings may be biased toward AGYW with more family support, thus missing the opportunity to identify challenges that may be represented by AGYW who may not have these supports (Bekker, Slack, Lee, Shah, & Kapogiannis, 2014; Fisher, Arbeit, Dumont, Macapagal, & Mustanski, 2016; Fisher et al., 2013). Much of HIV research among AGYW in South Africa has excluded AGYW who are under 18 years of age or cannot obtain guardian consent (Celum et al., 2019). Therefore, the generalizability of these findings may be limited. Fortunately, there is an opportunity for future research, such as the development of the dual purpose prevention modalities for HIV and pregnancy prevention, to use consent methods that include and protect all AGYW (Minnis and Juliana, 2019).
South African consent laws present a legal-ethical dilemma when attempting to engage AGYW in HIV research (Parliament of South Africa, 2004). Researchers must obey the law, but also respect adolescents’ developing autonomy (Fisher, 2004; Fisher et al., 2016; Hill, 2012; Mustanski, 2011; Strode, Slack, & Essack, 2010). Furthermore, the National Health Act is not aligned with the national ethical guidelines, which allow a broader range of consent processes, or the Children’s Act, which enables youth 12 or older to consent for sexual and reproductive health services without guardian consent (Children’s Act 38 of 2005, 2005; Slack, Strode, Fleischer, Gray, & Ranchod, 2007b; Strode, Singh, Slack, & Wassenaar, 2018). This could be problematic for HIV research with health services goals. Requiring guardian consent for HIV prevention research is also likely to disclose AGYW’s engagement in sexual behaviors, which may result in consequences ranging from stigmatization to violence (Fisher et al., 2016). These factors underscore the importance of identifying informed consent procedures that can protect the autonomy, rights, and welfare of AGYW who may not be able to secure guardian consent to participate in HIV research (Shah et al., 2018).
Youth who are at least 14 years of age may be capable of consenting for research participation, however, their lack of experience and deference to authority can create consent vulnerabilities (Behrman & Field, 2004; Fisher, in press; Fisher et al., 2016; Shah et al., 2018). Given the complexities of adolescent consent, South African ethics review boards have the authority to waive guardian permission for research participation minors under certain circumstances (Fisher et al., 2016; Slack et al., 2007b; Strode & Slack, 2011). Circumstances that may justify the waiving of guardian consent include research that is related to sensitive topics; is minimal risk; and/or may not be feasible without the recruitment of adolescents who might unable or unwilling to participate due to parent consent (Republic of South Africa, 2004). The complexities of the ethical and legal guidelines have been highlighted (Essack, Slack, & Strode, 2008; Jaspan et al., 2008; Slack, Strode, Fleischer, Gray, & Ranchod, 2007a; Strode et al., 2010; Strode & Slack, 2015); however, recommendations for addressing them is scarce (Strode et al., 2018; Strode & Slack, 2011).
In loco parentis consent (in place of parent (“Gott v. Berea College et al., " 1913); provides a vehicle for adolescent consent that protects minors from potential social harms resulting from disclosure of their risk behavior to family members. The In loco parentis consent procedure does not seek to obtain independent minor consent but to obtain permission for the minor to participate in research from a trusted adult who is not a minor’s parent or legal guardian. The in loco parentis procedure addresses the need for the inclusion of socially vulnerable AGYW since the adolescent can obtain permission to participate in research from a trusted adult who they select or an adult identified by community stakeholders and the research team, without disclosing their behavior to their parents. The procedure may have the potential to be used as an alternative consent procedure and increase the reach and impact of HIV research among AGYW in South Africa. However, information on the effectiveness of the procedure is needed to help researchers implement the in loco parentis procedure appropriately and to help ethics review boards evaluate the potential risks and benefits of using the procedure.
There is increasing recognition that HIV research involving vulnerable populations should engage representatives as advisers that can provide valuable insights into their perceptions of procedures (Emanuel, Wendler, Killen, & Grady, 2004; Essack et al., 2008). Therefore, the current study drew on the perspectives of AGYW who have undergone the in loco parentis consenting procedure to inform future methods of obtaining consent for South African AGYW.
Our research team has used the in loco parentis consent procedure to successfully recruit and retain AGYW over the last five years across three trials funded by the NIH (Carney et al., 2019; Wechsberg et al., 2018, 2020). The current report details the development and implementation of the in loco parentis procedure that was used in a behavioral HIV prevention study in Cape Town, South Africa. We also qualitatively explore the experiences of AGYW participants who were enrolled using this procedure (Wechsberg et al., 2018).
1. The development of the in loco parentis procedure
The in loco parentis procedure detailed in this report was initially developed by RTI International’s Office of Research Protection, as a solution to address challenges related to the enrollment of AGYW who were between 16 and 17 years of age into a behavioral HIV prevention study. The in loco parentis procedure was first implemented in a pilot study that was funded by the National Institutes of Health (NIH) to examined the efficacy of a developmentally tailored intervention to seek, test, treat and retain AGYW for HIV testing and services in 2014 (Carney et al., 2019). The eligibility criteria for the initial pilot study were as follows: (1) female, (2), between 16 and 21 years old, (3) is currently out of school having dropped out for at least 6 months, (4) has not completed matric (i.e., high school), (5) has used at least two drugs (one of which can be alcohol) weekly or more in the last 90 days, (6) has a boyfriend/male partner, (7) reports unprotected sex with a male partner in the last 90 days, (8) is able to provide informed consent or assent to participate, and (9) lives in the targeted communities. At the time the consent procedures were developed, the South African Government had enacted the South African National Health Act, which required guardian consent for those under 18 years of age to participate in research. In response to this change in policy, the team requested a waiver of parental consent, which was denied. However, after considering the potential for social harms related to involving parents in a study related to the sexual and substance use behaviors of their children, it was decided that an alternative consent method would be most appropriate. Therefore, the in loco parentis consent procedure was proposed to the ethics review boards at South African Medical Research Council (SAMRC) and RTI to consent those who were under 18 years of age that was aligned with both the legal and ethical guidelines of South Africa.
The research team and the collaborating IRBs evaluated the appropriateness of the in loco parentis procedure based on Section 3.2.2.4 of the South African National Department of Health’s Ethics in Health Research Guidelines (Republic of South Africa, 2004). These guidelines outline the circumstances and justification required for ethics review committees to consider a minor’s independent consent and guided the decision-making process of the team and ethics review board. Although the study team was not seeking approval for independent consent of a minor or parental waiver, we used these guidelines as a framework to develop the in loco parentis procedure (see Table 1). Specifically, the research team was concerned about possible social harms that may occur if guardian consent procedures inadvertently informed parents of their daughters’ substance use or sexual activity, as research suggests that youth’s fear of rejection from family may impact HIV testing (Duby et al., 2020). Given the concentration of new infections among AGYW and current low linkage to care, the inclusion of young women ages 16–17 in the study was critical to inform the development of interventions that would improve AGYW’s linkages to HIV testing and treatment. Lastly, adolescents can seek HIV testing and treatment in South Africa without guardian consent from the age of 12, according to Section 130 of the Children’s Act (Children’s Act 38 of 2005, 2005).
Table 1.
Application of South African and RTI ethical guidelines to assess the appropriateness for the In Loco Parentis consent procedure.
| Requirement of Ethical Guidelines | Application of In loco Parentis |
|---|---|
| Circumstances for Waiver of Guardian Consent | |
| In particular circumstances, e.g. for reasons of sensitivity, like discussions about sexual activities, substance abuse, etc., it may be desirable and ethically justifiable for minors (especially older minors, i.e., 16 years or older) to choose independently i.e. without parental assistance, whether to participate in research. | The study involved assessing (i.e., interviewing) and addressing (i.e., group-based intervention) sexual risk behaviors and substance use among young women 16–21 years old. The study also involved pregnancy testing, substance use screening, HIV testing, and linkage to HIV and/or substance use treatment if needed. |
| Generally, only minimal risk research is suitable for independent consent by minors. | This study was considered minimal risk. There were no physical or substantial psychological, social, or legal risks noted. However, minimal psychological, social, or legal risks included the possible disclosure of confidential information; possible mental discomfort associated with issues raised during interviews and intervention sessions; and potential psychological/social/legal consequences of gaining knowledge of HIV test results and/or potential interactions with alcohol and other drug use and their antiretroviral medications. However, all risks were adequately addressed with the proper protections. |
| Reasons supporting the desirability of independent consent may include recruiting sufficient numbers of minors who otherwise would not be willing to participate if they must tell their parents about the nature of the research to obtain parental permission. | Young women who use substances and engage in sexual intercourse are highly vulnerable to stigma and are unlikely to request permission from their parents and guardians for participation in an HIV and substance use-focused study for fear of negative repercussions. The research teams’ prior research in the same region demonstrated that one of the major barriers to seeking treatment for substance use disorders among young people was fear of negative repercussions from their parents.(Morojele, 2013) Therefore, it would be challenging to recruit a representative sample of young women if they had to obtain guardian consent. |
| Components of Justification for Waiver of Guardian Consent | |
| Prior engagement with participating community role players, the principal investigator (PI) can request (and justify explicitly) research ethics committee approval of a waiver of the parent (or substitute) permission requirement. Engagement could include outreach to relevant role players such as canvassing the opinion of a representative body of parents via schools. | The research team also consulted with a long-standing Community Advisory Board (CAB, which includes community members, substance use treatment providers, and local government officials, to discuss the appropriateness of waiving guardian consent as well as the implementation of the in loco parentis procedure. This discussion included the identification of respected women living in the communities where the study was taking place who could serve as consenters. |
| Factual evidence of such engagement must form part of the PI’s justification in the protocol. Factual evidence may be in the form of a letter from a relevant role player (like a community leader, school principal, or a CAB) that confirms the view that independent consent is acceptable to the parents. | The CAB provided feedback on the development of the in loco parentis procedure and provided their support. Specifically, they helped to identify trusted women in the community to serve as in loco parentis representatives. However, the research team did not submit a letter to the ethic boards because we were not requesting independent consent of a minor. |
| If the research ethics committee accepts the ethical justification and the factual evidence of parental support for independent choice by their minor children, then the research ethics committee may grant a waiver of the requirement of written parental permission and must document the process carefully. | The decision of each ethics review board to allow in loco parentis consenting was recorded in writing via the approval of the research protocol application by both SAMRC and RTI International. |
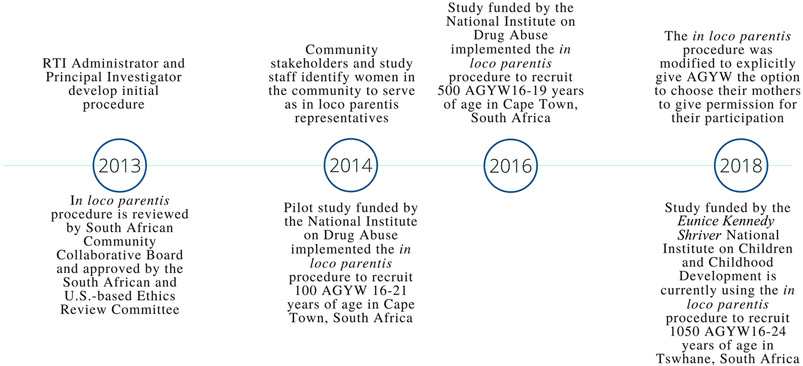
The in loco parentis consenting procedure that emerged out of the collaboration between the research team was approved by ethics review committees of the SAMRC and RTI International. The in loco parentis procedure was implemented in a pilot study from 2014 to 2016 (Carney et al., 2019) and has been modified and utilized across two trials with AGYW (see Fig. 1; (Wechsberg et al., 2018; Wechsberg et al., 2020). Overall, the in loco parentis consent procedures involves requiring any AGYW under 18 years old to receive permission from their parent; an older (25 years or older), trusted women who they identified (including a caregiver, as defined in the Children’s Act) (Republic of South Africa, 2005); or a woman in the community selected by community stakeholders and the research team who will provide consent in place of their parent. Any woman who consents in place of AGYW’s parent was referred to as the “in loco parentis representative”. Table 1 illustrates how our research team applied the South African ethical guidelines to the in loco parentis procedure.
Fig. 1.
Timeline of in loco parentis development and implementation.
2. The in loco parentis procedure
To date, the in loco parentis procedure has been used in three studies recruiting AGYW in South Africa to assess the efficacy of a behavioral HIV prevention intervention to reduce substance use, sexual risk, and gender-based violence among AGYW as well as link them to substance use treatment and sexual and reproductive healthcare services (Carney et al., 2019; Wechsberg et al., 2018, 2020). Below we describe the in loco parentis procedure as it was implemented in the trial that recruited 500 AGYW to assess the efficacy of a behavioral HIV prevention trial in Cape Town, South Africa. We have chosen to use this study as an exemplar because it represents the largest of our completed studies that have used the in loco parentis procedure.
Project staff recruited AGYW from underserved communities in the Western Cape of South Africa. After staff screened AGYW for the study and identified that they were eligible, those who were under 18 years old had the opportunity to identify an older woman who they trust to serve as the in loco parentis representative and provide permission for their participation if they were not comfortable with their mother or female guardian providing consent. Staff members then met with the in loco parentis representatives identified by AGYW to assess their appropriateness to represent the potential participants. Staff received manualized training to assess the mental capacity of the in loco parentis representative and also knew how to check for incapacity due to substance use, if needed. If the adolescent could not identify a trusted woman but was still interested in participating, research staff asked the AGYW’s permission to introduce them to a trusted woman who could serve as their in loco parentis representative. This woman was identified by the project staff with guidance from the study’s Community Advisory Board or a gatekeeper in the community. If the AGYW agreed to meet the in loco parentis representative, staff scheduled a time convenient for the AGYW and the representative to meet in person to be introduced and establish rapport. Of note, in loco parentis representatives were limited to women, with no distinction made between cis or transgender women, given the sensitive nature of sexual behavior among AGYW to reduce the possibility of social harms related to the engendered power dynamics that have been documented among AGYW and older men in southern Africa (Leclerc-Madlala, 2008; Mabaso et al., 2021).
The role of the in loco parentis representative was to act as a responsible adult who is familiar with the study and can make an informed decision about whether AGYW are appropriate for the general study activities. At the study site, the in loco parentis representative and the AGYW sat together while a member of the research staff explained the study. Both the AGYW and the in loco parentis representative were given the opportunity to ask questions and research staff addressed their questions. The in loco parentis representative and the AGYW were also given the opportunity to discuss the study. If they agreed, the in loco parentis representative then signed a permission form to allow the AGYW to participate in the study as well as a confidentiality agreement that they would not disclose the identity of the adolescent for whom they were acting as the in loco parentis representative. In a private session, the staff member then re-screened participants to ensure eligibility criteria, discussed the study with only the prospective participant in the room, and asked the adolescent to provide her assent separately to prevent coercion and ensure that consent is voluntary. The in loco parentis procedure was only used during the initial enrolment visit where all the study activities, including the repeated data collection points, were explained. AGYW were reconsented before each data collection follow-up appointment. Overall, this in loco parentis consent procedure, which were approved by both U.S. and South African-based IRBs represents an attempt to engage AGYW in HIV research, while respecting the potential limits of their consent capacity, and operating within the South Africa Law and Health Research Guidelines.
3. A study of AGYW’s perspectives of the in loco parentis procedure
Understanding the ethically relevant perspectives of AGYW recruited to participate in HIV prevention research can provide valuable insights to ensure that consent requirements are acceptable to participants, developmentally appropriate, and aligned with local laws (Emanuel et al., 2004). Therefore, we conducted post-study focus group discussions with a subsample of the 500 AGYW who participated in a behavioral HIV prevention trial in Cape Town, South Africa to understand AGYW’s experiences of the in loco parentis consent procedure.
4. Methods
AGYW who underwent the in loco parentis procedure to enroll in a behavioral HIV prevention trial were recruited from communities in Cape Town, South Africa. As described above, this trial sought to evaluate an intervention to reduce substance use and sexual risk as well as increase access to healthcare services among young women 16–19 years old who had discontinued school in Cape Town, South Africa.
Participants.
AGYW were eligible if they met the following criteria: (1) were 16–17 years of age at enrollment into the behavioral HIV prevention study (and therefore were consented using the in loco parentis procedure), (2) were currently 18 years of age or older at the time of the focus group discussion, (3) were assigned to the intervention arm of the main behavioral HIV prevention trial, (4) had completed the behavioral HIV prevention trial (i.e. were no longer eligible for data collection and did not withdraw from the study), (5) spoke and understood English, and (6) had indicated that they would like to be re-contacted for future research during their last trial appointment.
Research staff contacted AGYW who met inclusion criteria to ask if they would be interested in participating in a post-study focus group discussion to talk about their experiences in the larger trial. Interested participants were invited to participate in the focus group discussion and given a date and time for the appointment. AGYW were rescreened in-person on the day of the focus group discussion to ensure that they met the eligibility criteria and provided written informed consent.
Procedures.
Four focus group discussions were conducted with 31 AGYW. Two focus groups were conducted with participants who were isiXhosa-speaking (i.e., identified as Black African; n = 13) and two were conducted with those who were Afrikaans-speaking (i.e., identified as Coloured [an Apartheid-era racial category to indicate mixed-race ancestry]; n = 18). Focus group discussions were conducted by the first author, the South African Co-Project Director (who spoke Afrikaans), and/or the Principal Investigator of the larger trial. All facilitators were trained psychologists with experience in qualitative research methods. While groups were conducted in English, some translations were necessary during the group discussions. The South African Co-Project Director served as the translator during the focus group discussions with Afrikaans-speaking AGYW. Another project staff member served as the translator during focus group discussions with isiXhosa-speaking AGYW. Focus group discussions were conducted using a semi-structured focus group guide. The focus group discussion assessed participants’ perspectives on the risks and benefits of participating in the larger trial, including the in loco parentis procedure. Participants were asked about: (a) the risks and benefits of having an adult woman who was not their parent provide permission for them; (b) their perceived willingness to participate in research if guardian permission had been required; and (c) their level of parental disclosure regarding their participation in the study. Focus group discussions were digitally recorded and notes were taken. To protect their privacy, participants were asked not to use their names or the name of anyone else during the group. Instead, participants used pseudonyms to refer to themselves and others. After the focus group discussion, participants were reimbursed with a grocery voucher for ZAR 100 for their time (USD 7). All procedures were approved by the RTI Office of Human Protections (IRB Number 13790; MOD000000430) and the South African Medical Research Council Human Research Ethics Committee (Protocol ID: EC006-3/2016).
5. Analysis
We used a thematic approach to guide the analysis. We began by reading transcripts and interview notes to familiarize ourselves with the data. We developed a codebook combining inductive concepts based on the focus group guide and concepts observed during transcript review. Intercoder reliability was assessed using Cohen’s Kappa (15). One analyst applied codes to excerpts from one transcript and the other coded the same transcript blinded to the first analyst’s codes. Analysts then met several times to compare coding, refine code definitions, and resolve disagreements. Upon reaching high agreement (Kappa = .84), the remaining transcripts were double coded by two analysts. Coded data were summarized in tables to identify themes within and across Afrikaans and isiXhosa focus group discussions. Findings presented here specifically focus on participants’ experience with the in loco parentis consent procedure.
6. Results
Sample Characteristics.
The majority of AGYW (55%) were 18 years old at the time of the focus group discussions, 38% were 19 years old, and 6% were 20 years old (all were either 16 or 17 at the time of enrollment in the larger trial). Approximately 58% of AGYW were Afrikaans-speaking. AGYW participating in the focus group discussions were recruited from 7 different underserved communities across the Western Cape. More detailed demographic information for AGYW included in the trial are reported elsewhere (Bonner et al., 2021).
7. Key themes reflecting participant perspectives
The thematic analysis identified the following key themes illustrating AGYW’s experiences of the in loco parentis procedure: (1) Variety of AGYW-identified women chosen to be in loco parentis representatives; (2) Trust and confidentiality related to the women serving as the study-identified in loco parentis representative; (3) Diversity of AGYW’s attitudes toward sharing research participation information with parents; (4) AGYW’s privacy concerns; and (5) Freedom of AGYW to disclose their research-related information. These themes are organized into three categories: (1) AGYW’s perspectives on in loco parentis permission and assent procedures, (2) AGYW’s perceived impact of guardian consent on research participation; and (3) AGYW’s disclosure to guardians about research participation.
8. AGYW’s perspectives on in loco parentis permission and assent procedures
8.1. Variety of AGYW-identified women chosen to be in loco parentis representatives
AGYW identified a number of types of women to act as in loco parentis representatives for them. As illustrated below some asked family members (e.g., sisters, aunties) to serve as their in loco parentis representative and grant them permission. However, others relied upon other women who were not relatives but with whom they had a relationship (e.g., neighbors).
“I came with my sister.”
- isiXhosa-speaking AGYW, FGD3
“It is a big sister of one of the girls I came with … No, I did not mind because I know her and she knows me too.”
- isiXhosa-speaking AGYW, FGD3
“My aunt signed for me. She was interested that I join the study group because she did not approve that I was dropping out of school …”.
- isiXhosa-speaking AGYW, FGD3
“My aunty, my aunty did come to sign for me. Yes[I was okay with the aunty signing]. I go ask her.”
– Afrikaans-speaking AGYW, FGD1
“My neighbour.”
- isiXhosa-speaking AGYW, FGD4
Some participants could not identify a trusted woman to serve as their in loco parentis representative and therefore study-identified representative granted them permission. Some of the AGYW recognized the study-identified in loco parentis representative as a respected member of the community. As one participant said,
“I remember I think she lived close to where I live. She was a very helpful person. I think I know her like that and she was like community-wise, man. If there’s like maybe some issue she tries to solve it. She cannot be 100% right about things, but she tries to reach out to the community and so forth.
– Afrikaans-speaking AGYW, FGD2
Other AGYW were less familiar with the study-identified representative, but reported that they felt that she was friendly and helpful during the consent process.
“I do not know the name … she explained things more openly so we can understand what is happening here and … ja [yes] she was so friendly though.”
– isiXhosa-speaking AGYW, FGD4
8.2. Trust and confidentiality related to the women serving as the study-identified in loco parentis representative
Regardless of who served as the in loco parentis representative, participants reported that they understood and accepted that their representative would not know about the specific content of their study responses or the specific nature of study activities in which they engaged.
“I felt comfortable because she was … it is not like family or anything. But she was fine with what I am doing here …”
Afrikaans-speaking AGYW, FGD1
“We did mind at first but she will not know what we do here. She will just have to sign the consent form that is all. She will not know.”
- isiXhosa-speaking AGYW, FGD4
8.3. Integrity of the informed consent and assent process
Participants reported that the informed consent and assent process was clear and transparent. Participants reported that staff were responsive to the questions of the in loco parentis representative and explained the study in a way that the representative could understand. According to one participant said,
“She [in loco parentis representative] was comfortable because she was easy because they explained for her about how the process was going to be so she understands and she signed and so there was no complaining and so. And also she did ask questions, yes, and they answer her that is why she understands. That is why she is signed.”
– Afrikaans-speaking AGYW, FGD1
After participants received consent from the in loco parentis, they provided assent. AGYW reported that their questions about the study were answered clearly by research staff and that they believed their participation was voluntary. There was consensus across groups that research staff made sure that they understood the study activities. Overall, AGYW indicated that they felt autonomous in their decision to participate in the study.
“They [study staff] told us there are going to be workshops that we do here and tests but if you do not want to do tests it is your choice.”
– isiXhosa-speaking AGYW, FGD3
“Ja [yes], I did ask questions because they told us that I was going to be tested. Like okay they will do tests. Do test, what tested us for and wanted to know why and all that, ja?..They explained things openly like how they operate here and all that and that is when I could completely see how things goes.”
– isiXhosa-speaking AGYW, FGD4
9. AGYW’s perceived impact of guardian consent on research participation
Participants often contrasted the in loco parentis procedure to having their guardians, particularly their mothers, sign on their behalf. There were mixed perspectives on whether they believed they would still have participated in the intervention if guardian permission was required – highlighting the unique parental relationship of each AGYW. Young women who had open relationships with their guardians, in which they talked about sex and drugs, were more likely to respond that they would still participate even if guardian consent was required. Participants who held these views expressed that they did not want to hide anything from their guardians and that their guardians were aware of some of their behaviors. This relationship dynamic was highlighted by a participant who stated the following:
“I also talk open with my mom. I can talk anything with her. I do not feel like I must hide anything from her.”
- Afrikaans-speaking AGYW, FGD2
Others reported that they did not talk about sex or substance use with their mothers and they would fear that their guardian would want to know about their responses to survey questions and test results. Nevertheless, some AGYW said that they would still participate in the study, even if guardian permission was required. As illustrated by one participant.
“… And she will be on my case like nobody’s business but in the same time, I will be coming, ja.”
- isiXhosa-speaking AGYW, FGD4
Opposite to this, some AGYW stated that they did not believe that their guardians would have consented for them at all.
“My parents will not come here for me.”
– Afrikaans-speaking AGYW, FGD 2
Collectively, AGYW demonstrated the diversity of perspectives related to the implications or consequences of obtaining guardian permission for research participation. These diverse points of view were highlighted by a participant’s statement:
“Because all mothers is [are] not the same. You talk now here and you get there at home she is going to shout at you”
- Afrikaans-speaking AGYW, FGD 2
10. AGYW’s disclosure to guardians about research participation
10.1. AGYW’s privacy concerns
As described above, some AGYW would be hesitant to have their guardians sign for them. This hesitation seemed to be grounded in concerns about their privacy being violated by their guardians. Participants described these concerns as follow:
“… if my mother would have signed for me I would be like why do you need to know all my details, you know. I do not like sharing things with my mother, so.”
- Afrikaans-speaking AGYW, FGD 2
“Because mostly the thing that freaked me out, ja [yes] before I came here, ja [yes] my mother … I did not usually go to clinic and check out for myself you see? So, the first time I was coming here, okay, my mom is going to be involved here and what if I am [HIV] positive? What if I am too much in alcohol?..”
- isiXhosa-speaking AGYW, FGD4
Other AGYW noted their concerns about the consequences related to their guardians’ knowledge of their private information. Specifically, some participants were concerned about the social harms related to their guardians finding out about their tests results. In addition, AGYW spoke to the potential for wider dissemination of their private information through gossip.
“Or otherwise she [mother] will tell you “get out of my house!” and so.”
- Afrikaans-speaking AGYW, FGD 1
“Or she [mother] will go talk with her girlfriends about it … And her friends can tell other friends about it.”
- Afrikaans-speaking AGYW, FGD 1
“She [mother] will shout in the street!”
- Afrikaans-speaking AGYW, FGD 1
10.2. Freedom of AGYW to disclose information about the study
Due to the nature of the in loco parentis procedure, participants had more control of what they disclosed to their parents. Most participants reported that they had disclosed that they were in a health study to their parents. However, participants differed in the extent to which they discussed details related to their participation and the nature of the study. Some AGYW informed their parents about the study in detail-sharing information about the sexual health and substance use topics that were discussed.
“I told what we learned about sex, the tests and whatever … everything.”
– isiXhosa-speaking AGW, FGD4
Other participants were more selective about the details that they shared with their parents. For example, some AGYW provided details about the substance use components of the study, while leaving other details about the sexual health information that was discussed undisclosed.
“Yes, [I talk with parents] about the abuse and the drugs and all that, but not like I tried a condom on, like that stuff. I did not tell them that because I do not feel comfortable to tell like I do maar [just] that and so.”
- Afrikaans-speaking AGYW, FGD 2
Other participants reported that they only disclosed vague descriptions of the project such as the fact that it was a health study.
“I did not tell them anything. I just told them like ja, I was here by a thingy here and we are doing a lot of stuff to learn about like school stuff and so. That’s what I told them. We are learning that is all.”
– Afrikaans- speaking AGYW, FGD2
These differing reports indicate that the in loco parentis procedure did not prohibit all adolescent girls from sharing information with parents and illustrates the importance of allowing AGYW to control what and to whom they disclose information about the research study.
11. Conclusions
HIV prevention research among South African AGYW is a major priority, but may be limited by South African legal policies requiring parental permission for research participation of those younger than 18 (Joint United Nations Programme on HIV/AIDS, 2016b). (Parliament of South Africa, 2004) in addition, a number of AGYW may also not be comfortable discussing their substance use with their main caregivers or guardians. While much research has highlighted the tension between the laws and ethical guidelines related to adolescents’ participation in research in South Africa, there is a paucity of examples and recommendations for how to ethically consent AGYW. The current report meets this need by describing the in loco parentis consent procedure, which was developed to protect the rights and welfare of South African AGYW when researching sensitive topics such as sexual behavior and substance use. Our findings suggest that the in loco parentis was well-received by AGYW who underwent this procedure. Therefore, it may be an alternative or supplementary method of reaching and engaging the most vulnerable in AGYW in HIV prevention, if permitted.
Our findings suggest that AGYW obtained consent from a variety of women, including female family members, neighbors, and study-identified in loco parentis representative. While AGYW who obtained consent from the study-identified in loco parentis representative were initially apprehensive, most agreed that the representative was a respected community member. AGYW reported that they felt positively about the in loco parentis procedure, irrespective of the relationship with their guardian. Most AGYW reported that they would prefer to use the in loco parentis consent procedure to having to obtain guardian permission, citing that the limited relationship with the representative protected their privacy. Contrary to this, some AGYW stated that they would still participate in the study even if they had to obtain guardian permission. Others indicated their parent would refuse to grant them permission to participate. Many AGYW reported that they believe that it would be difficult to protect their privacy if guardian permission was required for study participation. Specifically, they feared that their mothers would ask them about the results of their pregnancy, HIV, and drug tests and that there would be adverse social consequences for a positive test result.
The diversity of perspectives regarding the extent to which AGYW would have participated if parental permission was required demonstrates the utility of the in loco parentis procedure to enhance the population validity of study findings by including those who would not participate if guardian permission was required. AGYW’s responses illustrate that the in loco parentis procedure provides a means for adult protection for adolescent consent to research, while also protecting their privacy rights.
The perspectives from the AGYW also highlighted that the in loco parentis procedure supported girls’ autonomy, by giving them a choice of what to share with their guardian. AGYW disclosed their participation to their guardians to varying degrees. The extent to which participants disclosed their participation and the nature of the study activities appeared to be related to the general level of open communication they had with their guardians. Therefore, guardian consent may be appropriate when AGYW have open communication with their guardians. However, the in loco parentis consent procedure may be an alternative to engage AGYW who have concerns about obtaining guardian permission to participate an in HIV-related study. Collectively, these findings indicate that the in loco parentis consent procedure was well-received by AGYW participating in this HIV prevention trial and that it may be an ethical and feasible alternative or adjunct to guardian consent procedures for researchers to use to engage AGYW in research.
This paper also illustrates the importance of obtaining participant perspectives in the design of research ethics procedures involving vulnerable populations (Fisher, 2015). Through retrospective data collection related to study procedures, researchers can ensure procedures are sensitive to the challenges facing adolescents. For example, based on the focus group findings, the in loco parentis procedure in our most recent research trial with AGYW made the option for AGYW to receive consent from their mother more explicit by providing a different consent form for guardians and in loco parentis representatives.
This article has important implications for alternative consent models for key populations of AGYW to participate in research. Our experience in developing and implementing the in loco parentis procedure, as well as the inclusion of the perspectives of the AGYW who assented and participated in the study, illustrates the feasibility, utility, ethical considerations. What about the ethics of using alternative consent procedures. The in loco parentis consent procedure may provide a comparative advantage over independent adolescent consent (i.e., parental waiver) when ethics review boards or researchers feel that the risk of the research warrants consent from an adult, but disclosure of adolescents’ engagement in sexual or other risk behavior to their guardians may confer additional risks. Future alternative consent procedures may consider using the most appropriate national guidelines during development to facilitate ethical review and approval. We also encourage the collection and presentation of data related to the consent process (e.g., concerns about social harms or desire for alternative consent models). This data may inform the development of alternative consent methods and help ethics review boards with decision-making.
The findings of this study should be viewed in light of their limitations. The small convenience sample had participated in the intervention arm of an on-going behavioral HIV prevention trial. Consequently, they may not be representative of AGYW who were lost to follow-up during the larger study or those who lived in the communities randomized to the control condition of the larger study. For example, this sample’s perspectives may be more positive than those who did not complete the study. In future studies, researchers should consider recruiting completers as well as those who do not complete the protocol to obtain the most balanced view of the research procedures. Focus group discussions were also conducted approximately a year after enrollment into the larger study. Therefore, there is also the risk of recall bias present and we recommend that future research obtain the perspectives of research participants shortly after they complete the study protocol. The in loco parentis procedure was only implemented among AGYW who were 16 or 17 years of age due to the mandatory reporting law requiring researchers and clinicians to report sexual behavior among those 15 years of age or younger (Republic of South Africa, 2007). Therefore, our findings may not be relevant for consent procedures for younger adolescents. Future research should examine how reporting laws may impact the inclusion of younger adolescents into HIV research; consider how alternative consent procedures may intersect with issues of capacity for younger adolescents; and develop alternative consent procedures to address these issues. In addition, we purposely recruited both isiXhosa and Afrikaans-speaking AGYW from different communities in the Western Cape to ensure representativeness across language/racial categories and communities. However, screening, consent, and focus group discussions were conducted in English, with translators available, which is not ideal given the importance of language justice in research (Ghanbarpour, Noguez Mercado, & Palotai, 2020) and limits the representativeness of our findings to those who are English-speaking. Future research should ensure that they obtain AGYW’s perspectives in a language that is most comfortable for them to improve the representativeness of findings. Lastly, this study did not seek the perspectives of the women who served as in loco parentis representatives. Other research using alternative consent procedures may consider exploring the experiences of in loco parentis representatives to obtain a better understanding of the perspectives of all the key stakeholders involved, including the potential need for and implications of researchers providing on-going support for the relationship between AGYW and community-identified representatives.
Limitations notwithstanding, our findings provide empirical evidence related to the potential utility of the in loco parentis consent procedure – which has not been available until now. These findings are particularly relevant for on-going and future HIV prevention and treatment research as well as other high-stakes research to prevent infectious diseases that affect adolescents such as COVID-19. Trials are currently being conducted in Southern Africa to develop multiple delivery methods for PrEP and are focusing on AGYW and requiring participants to obtain parental consent (Bunge et al., 2020; Microbicide Trials Network, 2017). Those who cannot obtain parental consent, who may represent a key population to target from HIV prevention, are excluded. Parental consent may be necessary for therapeutic research presenting greater than minimal risk, such as safety and efficacy testing of biomedical interventions (i.e., Phase 1 trials). However, the in loco parentis procedure may provide a strategy to include a more representative sample of AGYW during demonstration projects to increase the generalizability of findings related to the feasibility and real-world implementation of these new HIV prevention methods.
Acknowledgments
We would like to acknowledge the contributions of the project staff and the young women who participated in the study. We especially want to acknowledge and thank Jamia Bachrach, JD from the RTI Office of Research Protection.
Funding
This work was supported by the National Institute on Drug Abuse under grant numbers R01DA041227-S1 and R25DA03160. The funding source had no role in the analysis of the data, in writing the report, or in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
List of abbreviations
- AGYW
Adolescent girls and young women
- CAPRISA
Centre for the AIDS Programme of Research in South Africa
- CHAMPS
Choices for adolescent prevention methods for South Africa
- DREAMS
Determined, resilient, empowered, AIDS-free, mentored and safe
- FGD
Focus group discussion
- EMPOWER
Enhancing methods of prevention and options for women exposed to risk
- HIV
Human immunodeficiency virus
- HPTN
HIV Prevention Trials Network
- NIH
National Institutes of Health
- POWER
The prevention options for women evaluation research
- PrEP
Preexposure prophylaxis
- SAMRC
South African Medical Research Council
Footnotes
Ethics approval and consent to participate
The research conducted for this report was approved by the RTI Office of Human Protections (IRB Number 13790; MOD000000430) and the South African Medical Research Council Human Research Ethics Committee (Protocol ID: EC006-3/2016). Written consent was obtained from all young women who participated in the focus group discussion.
Availability of data and materials
The qualitative data analyzed for the current report are available from the corresponding author on reasonable request.
Declaration of competing interest
The authors declare that they have no competing interests.
References
- Behrman RE, & Field MJ (2004). Ethical conduct of clinical research involving children. National Academies Press. [PubMed] [Google Scholar]
- Bekker L-G, Slack C, Lee S, Shah S, & Kapogiannis B (2014). Ethical issues in adolescent HIV research in resource-limited countries. JAIDS Journal of Acquired Immune Deficiency Syndromes, 65, S24–S28. 10.1097/qai.0000000000000036 [DOI] [PubMed] [Google Scholar]
- Bonner CP, Carney T, Browne FA, Ndirangu JW, Howard BN, & Wechsberg WM (2021). Substance use and depressive and anxiety symptoms among out-of-school adolescent girls and young women in Cape Town, South Africa. South African Medical Journal, 111111(1So1), 40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunge KE, Levy L, Szydlo DW, Zhang J, Gaur AH, Reirden D, … Squires KE (2020). Brief report: Phase IIa safety study of a vaginal ring containing dapivirine in adolescent young women. Journal of Acquired Immune Deficiency Syndromes, 83(2), 135–139. 10.1097/qai.0000000000002244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney T, Browne FA, Myers B, Kline TL, Howard B, & Wechsberg WM (2019). Adolescent female school dropouts who use drugs and engage in risky sex: Effects of a brief pilot intervention in Cape Town, South Africa. AIDS Care, 31(1), 77–84. 10.1080/09540121.2018.1500008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celum CL, Delany-Moretlwe S, Baeten JM, van der Straten A, Hosek S, Bukusi EA, … Bekker LG (2019). HIV pre-exposure prophylaxis for adolescent girls and young women in Africa: From efficacy trials to delivery. Journal of the International AIDS Society, 22, Article e25298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Children’s Act 38 of 2005, (2005).
- Duby Z, Jonas K, Appollis TM, Maruping K, Dietrich J, Vanleeuw L, & Mathews C (2020). “There is no fear in me…well,that little fear is there ”:dualistic views towards HIV testing among South African adolescent girls and young women. African Journal of AIDS Research, 1–8. 10.2989/16085906.2020.1799232 [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Wendler D, Killen J, & Grady C (2004). What makes clinical research in developing countries ethical? The benchmarks of ethical research. The Journal of Infectious Diseases, 189(5), 930–937. 10.1086/381709 [DOI] [PubMed] [Google Scholar]
- Essack Z, Slack CM, & Strode AE (2008). Toward s roadmap: Summary of idenitified ethical-legal complexities in adolescent HIV vaccine and microbicide research. Retrieved from. [Google Scholar]
- Fisher CB (2004). Informed consent and clinical research involving children and adolescents: Implications of the revised APA ethics code and HIPAA. Journal of Clinical Child and Adolescent Psychology, 33(4), 832–839. [DOI] [PubMed] [Google Scholar]
- Fisher CB (2015). Enhancing the responsible conduct of sexual health prevention research across global and local contexts: Training for evidence-based research ethics. Ethics & Behavior, 25(2), 87–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher CB, Arbeit MR, Dumont MS, Macapagal K, & Mustanski B (2016). Self-consent for HIV prevention research involving sexual and gender minority youth: Reducing barriers through evidence-based ethics. J Empir Res Hum Res Ethics, 11(1), 3–14. 10.1177/1556264616633963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher CB, Brunnquell DJ, Hughes DL, Liben LS, Maholmes V, Plattner S, … Susman EJ (2013). Preserving and enhancing the responsible conduct of research involving children and youth: A response to proposed changes in federal regulations and commentaries. Social Policy Report, 27(1), 1–23. [Google Scholar]
- Fisher CB, & Mustanski B (2014). Reducing health disparities and enhancing the responsible conduct of research involving LGBT youth. Hastings Center Report, 44, S28–S31. 10.1002/hast.367, 0 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher CB, :uri LI, Macapagal K & Mustanski B . (in press). Competence to consent to oral and injectable PrEP trials among adolescent males who have sex with males. AIDS and behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanbarpour S, Noguez Mercado AP, & Palotai A (2020). a language justice framework for culturally responsive and equitable evaluation. New Directions for Evaluation, 2020(166), 37–47. 10.1002/ev.20412 [DOI] [Google Scholar]
- Gott v. Berea College et al. , 156 376 (Kentucky Court of Appeals; 1913). [Google Scholar]
- Hill BJ (2012). Medical decision making by and on behalf of adolescents: Reconsidering first principles. Journal of Health Care Law and Policy, 15, 37. [Google Scholar]
- Jaspan HB, Soka NF, Strode AE, Mathews C, Mark D, Flisher AJ, … Bekker LG (2008). Community perspectives on the ethical issues surrounding adolescent HIV vaccine trials in South Africa. Vaccine, 26(45), 5679–5683. 10.1016/j.vaccine.2008.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2016a). Global AIDS update 2016. Geneva, Switzerland. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2016b). HIV prevention among adolescent girls and young women. Retrieved from Geneva, Switzerland. [Google Scholar]
- Leclerc-Madlala S. (2008). Age-disparate and intergenerational sex in southern Africa: The dynamics of hypervulnerability. AIDS, 22(Suppl 4), S17–S25. 10.1097/01.aids.0000341774.86500.53 [DOI] [PubMed] [Google Scholar]
- Liu C, Cox RB, Washburn IJ, Croff JM, & Crethar HC (2017). The effects of requiring parental consent for research on adolescents’ risk behaviors: A meta-analysis. Journal of Adolescent Health, 61(1), 45–52. 10.1016/j.jadohealth.2017.01.015 [DOI] [PubMed] [Google Scholar]
- Mabaso M, Mlangeni L, Makola L, Oladimeji O, Naidoo I, Naidoo Y, … Simbayi L (2021). Factors associated with age-disparate sexual partnerships among males and females in South Africa: A multinomial analysis of the 2012 national population-based household survey data. Emerging Themes in Epidemiology, 18(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Microbicide Trials Network. (2017). MTN-034 A Phase 2a crossover trial evaluating the safety of and adherence to a vaginal matrix ring containing dapivirine and oral emtricitabine/tenofovir disoproxil fumarate in an adolescent and young adult female population. National Institutes of Health. [Google Scholar]
- Minnis AE, & Juliana. (2019). MTN-045 dual purpose prevention (DPP) product preferences among couples. [Google Scholar]
- Morojele N, Myers B, Townsend L, Lombard C, Plüddemann A, Carney T, et al. (2013). Survey on substance use, risk behaviour and mental health among Grade 8-10 learners in Western Cape provincial schools, 2011. Cape Town. South Africa: South African Medical Research Council. [Google Scholar]
- Mustanski B. (2011). Ethical and regulatory issues with conducting sexuality research with LGBT adolescents: A call to action for a scientifically informed approach. Archives of Sexual Behavior, 40(4), 673. [DOI] [PubMed] [Google Scholar]
- Parliament of Republic of South Africa, 2004. National Health Act 2004 (South Africa) s 71.
- Republic of South Africa. (2004). Ethics in health research: Principles, Structures, and processes. Retrieved from http://www.mrc.ac.za/ethics/DOHEthics.pdf.
- Shah SK, Allison SM, Kapogiannis BG, Black R, Dawson L, & Erbelding E (2018). Advancing independent adolescent consent for participation in HIV prevention research. Institute of Medical Ethics. [DOI] [PubMed] [Google Scholar]
- Slack C, Strode A, Fleischer T, Gray G, & Ranchod C (2007a). Enrolling adolescents in HIV vaccine trials: Reflections on legal complexities from South Africa. BMC Medical Eihics, 8. 10.1186/1472-6939-8-5, 5–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slack C, Strode A, Fleischer T, Gray G, & Ranchod C (2007b). Enrolling adolescents in HIV vaccine trials: Reflections on legal complexities from South Africa. BMC Medical Ethics, 8(1), 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strode A, Singh P, Slack C, & Wassenaar D (2018). Research ethics committees in a tight spot: Approving consent strategies for child research that are prima facie illegal but are ethical in terms of national guidelines. South African Medical Journal, 108(10), 828–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strode AE, & Slack CM (2011). Using the concept of ‘parental responsibilities and rights’ to identify adults able to provide proxy consent to child research in South Africa. South African Journal of Bioethics and Law, 4(2), 69–73. [Google Scholar]
- Strode AE, & Slack CM (2015). Child research in South Africa: How do the new regulations help? South African Medical Journal, 105(11), 899–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strode A, Slack C, & Essack Z (2010). Child consent in South African law: Implications for researchers, service providers and policy-makers. SAMJ: South African Medical Journal, 100(4), 247–249. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Browne FA, Carney T, Myers B, Minnis A, MacDonald R, … Rodman N (2018). The Young Women’s Health CoOp in Cape Town, South Africa: Study protocol for a cluster-randomised trial for adolescent women at risk for HIV. BMC Public Health, 18(1), 859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsberg WM, Browne FA, Ndirangu J, Bonner CP, Minnis AM, Nyblade L, … Ahmed K (2020). The PrEPARE pretoria project: Protocol for a cluster-randomized factorial-design trial to prevent HIV with PrEP among adolescent girls and young women in Tshwane, South Africa. BMC Public Health, 20, 1403. 10.1186/s12889-020-09458-y [DOI] [PMC free article] [PubMed] [Google Scholar]