Abstract
Background
Persons injured in traffic accidents may have injuries of characteristic types that are of significance for the complex reconstruction of the accident and whose medicolegally sound clinical documentation is highly important. This is of particular relevance for the approximately 55 000 persons who are severely injured in traffic accidents in Germany each year. Gaps in documentation are often disadvantageous for the injured persons.
Methods
This review is based on pertinent publications retrieved by a selective literature review, with additional consideration of relevant textbooks in traffic medicine and legal medicine, as well as the guidelines of the AWMF (Association of the Scientific Medical Societies in Germany).
Results
Injuries in traffic accidents typically differ depending on the mode of participation of the injured person in traffic. They must be examined with a view toward the sequence of events of the accident and documented in medicolegally sound fashion. In particular, because of the different mechanical forces involved, it is important to document the seat that the injured person occupied in the automobile, the nature of the collision (pedestrian vs. automobile; bicycle, e-bike, e-scooter, and motorcycle accidents), and the protective devices that were in use.
Conclusion
The precise documentation of injuries and examination findings, with critical consideration of their plausibility in relation to the sequence of events of the accident as far as it is known, is an important duty of the physician. This documentation serves as the basis for further judicial steps leading to compensation when legally appropriate.
There were approximately 2.3 million traffic accidents in Germany in 2021, according to police records. Some 325 000 people were injured, 55 000 of them seriously, and 2562 people died. Persons riding in cars accounted for most of the injured (N = 161 497), followed by cyclists (N = 83 753) and pedestrians (N = 22 652) (1).
Incidence.
In Germany in 2021, some 325 000 people were injured in traffic accidents, 55 000 of them seriously, and 2,562 people died.
In 2018, approximately 716 000 sentences were handed down by German criminal courts. A sizeable fraction of these, approximately 22%, were for road traffic offenses, including drunk driving (Section 316 StGB), negligent homicide (Section 222 StGB), negligent bodily injury (Section 229 StGB), and endangering road traffic (Section 315 c StGB) (2). Clearly, the medicolegally sound documentation of injuries sustained in road traffic accidents by physicians is an important matter for routine clinical practice, so that the patient can demonstrate the injury sustained in the accident and prove its causality to the court in order to obtain due compensation; this is aside from the further consequences of road accidents in civil law. Mechanisms of injury are harder to reconstruct with incomplete documentation.
In general, although there are some differences across countries owing to local conditions, the most frequently injured body regions in road traffic accidents are the limbs, followed by the head and neck. Serious injuries most commonly involve the head, followed by the chest. There is more than one injury in approximately 40% of cases (3).
Injured regions of the body.
The most frequently injured body regions in road traffic accidents are the limbs, followed by the head and neck. Serious injuries most commonly involve the head, followed by the chest. There is more than one injury in approximately 40% of cases.
The site and severity of an injury depend on a range of intrinsic and extrinsic factors, including the type of transport involved (including the use or non-use of safety devices), the cause of the accident, and the particular vulnerability of the injured person (age, medical history, substance use). Improvements in safety devices have led to a change in injury patterns in recent decades. Nonetheless, the mechanism of the accident is not the sole predictor of the nature of the injury that will result (4).
For persons riding in cars, a collision with a narrow object, such as a tree, is especially dangerous. For pedestrians and cyclists, the most dangerous aspects of accidents involving automobiles are the impact on the hood (usually with the chest) and the impact on the windshield and A pillars (usually with the head) (5). (The A pillars are the pillars to either side of the windshield.) Injured pedestrians and cyclists are, on the average, markedly older than injured car occupants. Accidents with motorized two-wheel vehicles are mainly sustained by men and usually cause the most serious injuries (6).
It is recommended in the current German S3 guideline on the treatment of patients with severe trauma and polytrauma (7) that a shock room team should be alerted whenever a traffic accident involves ejection from a vehicle or a fracture of long tubular bones (Table).
Table. Table of indication criteria for alerting the schock room (S3 guideline) (7).
| Criteria for alerting the shock room | ||
| Pathological findings after trauma | Injuries or measures taken after trauma | Additional criteria for elderly trauma patients |
| A/B problem - respiratory insufficiency (SpO2 < 90 %)/need for airway protection - RR < 10 or > 29 C problem - systolic blood pressure < 90 mm hg - heart rate > 120/min - Shock index > 0.9 - positive eFAST D problem - GCS ≤ 12 E problem - hypothermia < 35.0 °C |
– unstable chest – mechanically unstable pelvic injury – penetrating injuries of the trunk and neck – amputating injury proximal to the hands/feet – sensorimotor deficit after spinal injury – pre-hospital intervention (need for securing the airway, chest decompression procedure, catecholamine administration, pericardiocentesis, or placement of a tourniquet) – fractures of 2 or more proximal large tubular bones – burns > 20% and degree ≥ 2b – fall from more than 3 meters of height – traffic accident with ejection from vehicle or fracture of a long tubular bone – expanded indication for notifying the shock room if the patient is elderly |
– systolic blood pressure < 100 mmhg – known or suspected traumatic brain injury and GCS ≤ 14 – 2 or more injured regions of the body – traffic accident with fracture of one or more long tubular bones |
eFAST, extended focused assessment with sonography in trauma; GCS, Glasgow Coma Scale; RR, respiratory rate;SpO2, oxygen saturation measured by pulse oximetry
The Abbreviated Injury Scale (AIS) is used to classify the severity of injury. It was issued in 1969 and has been repeatedly revised since then; the AIS15 code is the latest version (8). Individual injuries are assigned codes based on their anatomical site, nature, and relative severity. The stated relative severity and probability of survival always refer to the individual injury, i.e., to an otherwise healthy adult with only this particular injury. The AIS code is time-independent: the relative severity does not change over time and is not affected by the consequences of the injury, such as time spent in rehabilitation or inability to work. The coded severity of injury is a useful datum for trauma research; for example, trends in coded severities of injury can be used to document the benefit of a protective measure.
Abbreviated Injury Scale (AIS).
The Abbreviated Injury Scale (AIS) is used to classify the severity of injury; the AIS15 code is its latest version. Individual injuries are assigned codes based on their anatomical site, nature, and relative severity.
The AO classification is an alphanumeric coding system for fractures and dislocations (9). The codes are generally hierarchically arranged, starting with simple fractures and progressing to comminuted fractures. Each code contains information about the site and morphology of the fracture.
AO classification.
The AO classification is used to classify fractures and dislocations. The codes are generally hierarchically arranged, starting with simple fractures and progressing to comminuted fractures. Each code contains information about the site and morphology of the fracture.
The proper forensic documentation of skin injuries after traffic accidents corresponds in its basic features to their documentation after other types of physical violence (10–13). There are many types of injury in road traffic accidents that are of crucial importance for the complex reconstruction of the accident and whose proper forensic documentation is, therefore, essential.
We point out for completeness that, aside from physical injuries, material evidence from the scene of the accident, including damage to vehicles and clothing, is obviously also important for its reconstruction (14). In this article, however, we are concerned only with the characteristic injuries. Damaged clothing should never be discarded, but should remain with the patient.
Proper medicolegal documentation is needed so that the causal relationship between the accident and the injury can be proved by reconstruction of the accident. If this is not established, the injured party cannot be compensated (11).
Learning objetives
In this article, we present the nature and the proper documentation of typical external and internal injuries resulting from various types of accident, as well as their relevance to biomechanical analyses.
The topic is subdivided into the main modes of participation in road traffic.
This article should enable the reader to:
document injuries sustained in road accidents in proper medicolegal fashion;
know the typical injuries depending on the mode of participation in traffic;
be aware of the importance of particular injuries for accident reconstruction.
Methods
This review is based on relevant publications retrieved by a selective search in English and German periodicals and books, including the pertinent AWMF guidelines.
Results
General procedure for the documentation of external injuries
The (at least) informal consent of the injured person is required for the documentation of injuries. If consent is withheld for the taking of photographs, this is to be documented as well, and the injured person should be informed of the potential adverse consequences of purely verbal and thus potentially imprecise documentation (13). If the injured person is unconscious, there can be a presumption of consent, because proper documentation is obviously in his or her best interest (15).
The entire body should be examined (11). In conscious patients, different regions of the body are generally examined in sequence so that full disrobing at one time is unnecessary (10).
Photographic documentation should begin with an incontestably identifiable image of the face. Additional video documentation is sometimes helpful for the visualization of the spatial relationship between injuries (12).
The affected part of the body should be photographed first in its entirety, ideally including a visible anatomical reference point, and then a detailed image of the abnormal finding should be taken, including a scale for distances, a color chart, and the patient’s identifying data. The image should be taken at right angles as far as possible. The reconstruction of the accident is greatly facilitated by the documentation of injuries before they are cared for in any way, and by the at least written documentation of findings that only become evident in the course of care, e.g., tissue bridges, the state of the wound edges, wound depth, and wound cavities (10).
Photographic documentation of (possibly unexpected) negative findings, e.g., lack of a seatbelt mark, and of clothing can also be helpful. The photographs should be stored safely so that they cannot be tampered with by others; there must be no doubt regarding the origin of the dataset. A body diagram can be a useful aid in the presentation of complex or multiple injuries (12).
Documentation of this type, like other medical findings, is subject to the medical confidentiality rule. It may not be shared with the legal authorities or third parties without the patient’s permission (13).
The meticulous documentation of injuries may be helpful or essential for the reconstruction of the road accident that caused them. When examining the patient, the physician should already have the reconstruction of the accident in mind, in order to confirm or refute hypotheses about the predictable direct or indirect effects of the assumed type of accident. The presence of paint, textiles, or material fragments on the patient’s body does not constitute an injury in itself but can also be very important for the reconstruction (16). The wearing of protective clothing or a protective helmet should be documented as well.
Proper medicolegal documentation is not, of course, restricted to the skin and mucous membranes, but concerns the internal organs as well. Internal injuries that are detected by imaging studies or at surgery should also be sufficiently documented (to the extent permitted by the clinical situation) to provide optimal answers to questions that may be asked later about the site of the injury, the edges and base of the wound, and its length, depth, and age. Measurements that are approximate rather than precise, as in an operative note describing an emergency procedure, should be designated as such (e.g., with the abbreviation “ca.”).
The general classification of externally evident consequences of blunt trauma
Traffic accidents other than those involving shrapnel injuries and automobile fires generally cause blunt or blunt-edged trauma, i.e., the transmission of energy to the body over a broad surface rather than at a point. Patterns of injury on the skin are classified into five types (16, 17):
Informal consent.
The (at least) informal consent of the injured person is required for the documentation of injuries. If consent is withheld for the taking of photographs, this is to be documented as well, and the injured person should be informed of the potential adverse consequences of purely verbal and thus potentially imprecise documentation.
Meticulous documentation.
The meticulous documentation of injuries may be helpful or essential for the reconstruction of the road accident that caused them. Proper medicolegal documentation is not restricted to the skin and mucous membranes, but concerns the internal organs as well.
abrasive injuries due to tangential forces, sometimes with epithelial scratches that indicate the direction of the abrasion;
indirect overstretching of the skin, e.g., in the groin of a pedestrian struck from behind;
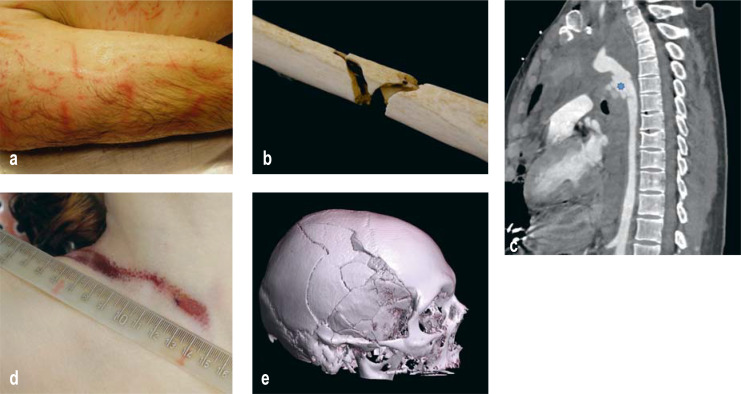
hematomas whose shape may reflect that of the surface that struck the patient, generally in the form of a negative impression (Figure 1a);
lacerations, in which initial compression over a broad surface leads to tearing of the skin and to the classic findings of irregular wound edges, epithelial damage in the immediate vicinity, and tissue bridges in the interior of the wound;
detachment injuries with ultrasonographically demonstrable wound pockets after separation of the skin from the subcutis or fascia, generally seen in rollover injuries on the side of the collision; these can be present without any externally visible structural correlate and can cause marked blood loss.
Figure 1.
(a) negative impression of a tire profile on the patient’s lateral right arm after a rollover injury; (b) tibial Messerer wedge; (c) CT angiogram of a ruptured thoracic aorta after deceleration trauma (* on rupture site); (d) dried seatbelt mark from the shoulder harness of a three-point seatbelt, seen post mortem in a woman killed in an automobile accident; (e) spider web fracture, with focal point overlying the right temporal bone.
The main fracture types
Fractures can be classified as closed or open, as intra-articular, metaphyseal, and diaphyseal, and as either with or without comminution or dislocation. Long-bone fractures can be classified according to the causative trauma (direct, indirect, penetrating, repetitive). Direct and indirect stress are the main mechanisms of fracture in road accidents and can cause various types of fracture (18).
Bending (flexural) fractures can be caused by either direct or indirect stress on a long bone. Direct stress involves compression on the side of the bone that receives the impact and distention on the opposite side; the bone breaks first on the distended side, often causing a wedge-shaped fracture, also known as a Messerer wedge fracture (Figure 1b). Direct and indirect bending fractures can often also be distinguished on the basis of the accompanying soft-tissue injury that is found at the fracture site in direct fractures only (19).
Spiral (twist, torsional) fractures arise when the pedestrian turns around the limb in question at the moment of the collision. This is a type of indirect fracture.
Plastic deformity (20): limbs that are run over may not just be fractured, but may also manifest a plastic deformity, meaning that the fracture ends no longer fit together (20). Direct collisions with automobile bumpers do not cause plastic deformities; in such cases, the fracture ends fit together.
Recognizable consequences of blunt trauma.
abrasions
indirect overstretching of the skin
hematomas
lacerations
detachment injuries
The main fracture types.
Fractures can be classified as closed or open, as intra-articular, metaphyseal, and diaphyseal, and as either with or without comminution or dislocation.
Particular road-accident injury types depending on the mode of participation in traffic, and their special relevance in documentation
Aside from the concrete circumstances of the accident and the particular details of the vehicle involved (21), the type of injury can also depend on the particular seat occupied by the injured person in the automobile. The driver’s seat predisposes to trapping of the injured person in place and to thoracic trauma from the blunt impact of the steering wheel on the chest. Approximately 7% of persons riding in cars who are injured in road accidents were not wearing a seat belt; the figure is appreciably higher among those who are fatally injured. Side collisions are more likely to cause severe and multiple trauma than frontal and rear-end collisions (22, 23), because the safety systems of automobiles provide less protection against them. The reconstruction of a traffic accident often requires interdisciplinary collaboration. Further variations in injury patterns arise from the position of the seat and the passenger’s body posture while sitting in it.
Typical injuries by which the seating position can be identified
The question of who was sitting where in the car arises in particular when multiple passengers refuse to communicate this information, or when a person who has been killed in an accident is falsely said to have been the driver in order to absolve the survivors of responsibility. It may be difficult or impossible to answer this question solely from photographs of the injuries sustained if one or more persons were ejected from the vehicle, if the vehicle rolled over, or, in general, if the accident involved multiple phases. In severe rear-end collisions, the forces acting in equivalent ways on the driver and the passengers may cause very similar injuries that cannot be differentiated (24). The interactions of multiple automobile occupants, at least one of whom is unrestrained, additionally increases the complexity of injury patterns (17).
The determination of seating position.
The question of who was sitting where in the car arises in particular when multiple passengers refuse to give this information, or when a person who has been killed in an accident is falsely said to have been the driver in order to absolve the survivors of responsibility.
In general, both the driver and the passengers tend to be injured on the side nearer the door; superficial glass-fragment injuries on the sides of the face, caused by shattering of the side windows, should be considered in the overall assessment as well (25). Severe craniofacial injuries are usually due to the impact of the face on the steering wheel and are very unusual in restrained passengers (16).
Severe craniofacial injuries.
Severe craniofacial injuries are usually the result of the impact of the face on the steering wheel and are very unusual in restrained passengers
Dashboard injuries can only be sustained by the driver and the front-seat passenger(s). The patella and acetabulum are the most frequently injured bones, although certain portions of the femur can be injured as well. Tall individuals are disproportionately injured (26). Persons with dashboard injuries are less likely to have severe intra-abdominal injuries, presumably because the major portion of the force impact has been absorbed by other regions of the body: odds ratio (OR) 0.25, 95% confidence interval [0.10; 0.62] (27).
In frontal and lateral collisions where the protective effect of the airbags does not suffice, deceleration injuries of the thoracic aorta (Figure 1c) can arise, often in the region of the isthmus (28).
Frontal collisions in which the driver has already initiated a braking response are particularly likely to cause midfoot or ankle dislocations and fractures as well as axial compression injuries of the tibial condyles, usually in the right leg (29, 30). Feet positioned next to the pedals are subject to typical abrasions and degloving injuries in the ankle region. The retarding force of the pedal on the shoe can leave visible traces on the sole of the shoe (24, 16).
The cervical sprains often resulting from unforeseen rear-end collisions are more common in persons who are not protected by headrests, i.e., in rear-seat passengers, but they can be seen in persons sitting anywhere in the car if the headrest was poorly positioned, or as a consequence of “out-of-position” posture of the head.
Demonstration of the use and deployment of safety devices
The introduction of seatbelts is thought to have lessened the risk of dying in an automobile accident by 50% to 60% (32). The importance of seatbelt injuries in insurance law is obvious. There is no implication, however, that safety devices themselves never cause any injuries.
Seatbelt injuries (Figure 1d) are most commonly seen in frontal collisions; clearly, a seatbelt injury can also yield information about where the injured person was sitting, given a known manner of suspension of the shoulder strap (but keep in mind the possibility a seat belt suspension in the middle of the car). These injuries can involve skin marks, subcutaneous hematoma, and intra-abdominal and spinal injuries (Chance fractures of the thoracolumbar junction). Fractures of the clavicle, sternum, or ribs distributed along the course of the seatbelt shoulder strap are seen mainly in elderly persons with osteoporosis (16).
Slipping out from under the seatbelt (“submarining”) increases the risk of injury. This occurs more commonly with obese individuals, soft seats, loosely fastened belts, and markedly reclined position of the seat (34, 35). The absence of a seatbelt mark does not rule out the injured person’s having worn a seat belt (e.g., because of thick clothing) (16).
The introduction of airbags lessened the frequency of AIS level 2 or higher injuries of the head and face by 40% to 70% (36). Airbag-specific injuries include ocular injuries (corneal abrasion, anterior chamber hemorrhage, chemical keratitis, other), injuries of the teeth and temporomandibular joints, and barotrauma (37, 38). Airbags pose particular dangers for persons of small stature, wearers of eyeglasses, and persons sitting out of position (e.g., a child seat in backwards position in front of an airbag) (39, 40).
Pedestrian-against-automobile injuries
Injuries sustained in this type of accident can be classified according to the various accident phases (14, 17), which will be discussed here in temporal sequence:
∙ Impact injuries: this refers to the initial contact of the moving vehicle with the pedestrian, usually in the form of a bumper-lower leg contact (full or partial impact). The so-called Messerer wedge is a bending fracture that indicates the direction of the force applied (the wedge base is on the side of the impact; Figure 1b). The tip of the wedge points in the direction of the vehicle’s velocity vector (e1, e2). To distinguish direct from indirect fractures, any soft tissue injury at the fracture site should be documented, as it indicates the directly applied force by the involved automobile part. The alignment of the Messer wedge tip should be precisely documented, as should the fracture height (measured from the calcaneus), as this may indicate the height of the bumper of the vehicle involved in the accident (e3). Characteristic knee joint injuries may indicate valgus or varus flexion, enabling conclusions to be drawn about the direction of impact. The following types of bone injury should be documented: bone contusions in the central areas of the condyle or under the capsular surface, subsidence of the condyle, condyle fractures. It can generally be assumed that fractures arise on the side facing the impact through compression, while ligament injuries arise on the side opposite to the impact through distension (e4). Skin injuries, too, are usually seen on the side facing the impact. The impact of the bumper against the lower leg can also injure the ankle, aiding in the determination of the underlying mechanism of injury. Injury to the medial malleolus and its ligaments imply pronation and indicate a lateral impact, while lateral injuries imply supination and indicate a medial impact. Transection of the posterior part of the joint capsule and injuries to the anterior edge of the distal tibial epiphysis imply dorsiflexion and indicate an anterior impact; transection of the anterior part of the joint capsule and injuries to the posterior edge of the distal tibial diaphysis imply plantar flexion and indicate a posterior impact (e5). Moreover, fractures of the sacroiliac joint occur on the side facing the impact in lateral collisions, with only rare exceptions (e6). If the front of the vehicle has a large surface area, it may not be possible to delimit the point of impact (e7). The struck pedestrian can easily fall onto the hood secondarily, leading in particular to chest injuries and to head injuries arising from impact of the head against the windshield or an A pillar (Figure e). Fractures of ribs 8–12 commonly result from traffic accidents, but not from cardiopulmonary resuscitation (e8). In countries where driving is on the right side of the road, drivers are less able to react quickly to a pedestrian coming onto the road from the right; thus, the left side of the body is more commonly hit.
∙ Rollover (runover) injuries: impact with a tire is called a runover (Figure 1a) and generally involves shearing forces that cause severe detachment of tissue layers (degloving injury). Fractures and injuries to internal organs are obviously possible depending on the part of the body that is run over. There may also be plastic deformity of the fracture. An individual who lands under a moving automobile without being hit by a tire can also sustain severe injury from the undersurface of the vehicle or from being dragged by it. The pedestrian is more likely to land on top of the automobile in high-speed collisions, and when the impact is below the iliac crest; this depends, in turn, on the size of the individual (more likely in tall persons) and on the configuration of the front of the car.
∙ Injuries resulting from being thrown after a collision with an automobile: this is the final phase of the accident and can cause serious blunt trauma, e.g., in a further collision with road infrastructure (the so-called tertiary accident).
The impact injuries, in particular, are important for reconstruction of the accident, as the subsequent phases are unpredictable owing to the many kinematic degrees of freedom (16).
Injuries of persons riding two-wheeled vehicles
Accidents involving a human-powered or motorized two-wheeled vehicle (e-scooter, bicycle, pedelec, motorcycle, etc.) cause serious injury to the rider relatively often (e9), because such vehicles, unlike an automobile, lack comprehensive protection systems such as a crumple zone, seatbelts, or airbags. As two-wheelers can lower their energy by tipping sideways, they are considered to be inherently unstable around their longitudinal axis (17). Their riders can easily be thrown off of them, and not just in collisions with much heavier automobiles. Thrown riders suffer not only the consequences of the initial impact but also those of the subsequent impact with the ground, a crash barrier, a lamppost, or another object. Accidents involving two-wheelers often cause injuries with an ISS ≥ 16 (e10) despite the use of protective equipment such as protectors and safety clothing. In Germany at present, the law does not require persons riding bicycles/pedelecs or even e-scooters to wear a helmet or special protective clothing (German Road Traffic Regulations, §21a). The injuries sustained may be of unspecific types, but there are also specific injury patterns for each type of vehicle; see Figure 2a–d, eSupplement.
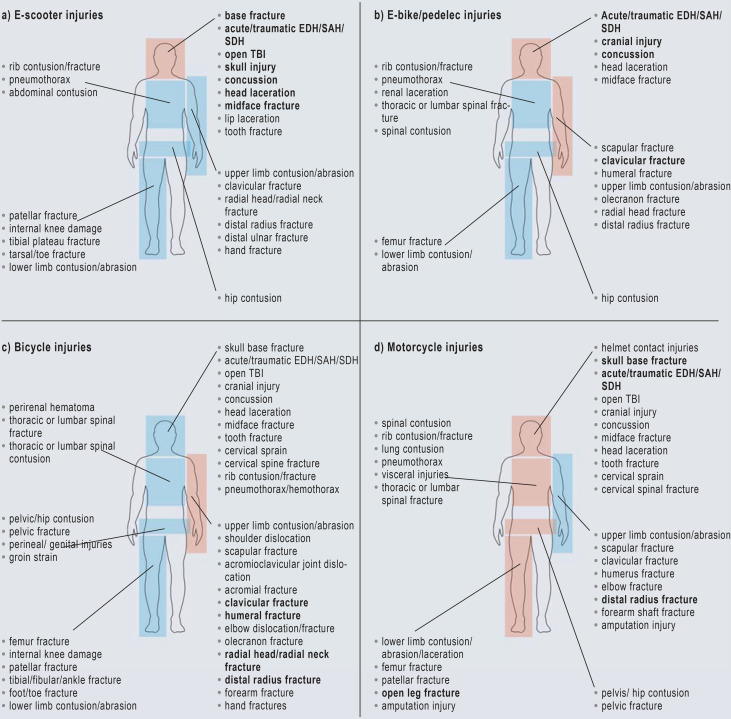
Figure 2.
Non-exhaustive presentation and list of injuries
a) e-scooter accident, b) e-bike/pedelec accident, c) bicycle accident, d) motorcycle accident; more commonly injured body regions are shown in brown; injuries highlighted in bold are more common in the body region in question (e11-e29). For greater clarity, only one limb is labeled in each case.
EDH, epidural hematoma; SAH, subarachnoid hemorrhage; SDH, subdural hematoma; TBI, traumatic brain injury.
Illustration: MaskaRad/stock.adobe.com [m]
E-Supplement.
E-scooter-related injuries
Injuries in e-scooter accidents mainly involve the head, followed by the upper and lower limbs. The most common types of injury are contusions and sprains, followed by fractures. Upper limb injuries usually involve the elbow (radial head/radial neck fractures) and the distal radius (contusions/fractures). The main types of head injury are cranial and midface fractures and intracranial hemorrhages (subdural hematoma, epidural hematoma, and subarachnoid hemorrhage), which may be life-threatening (e11). According to the Federal Statistical Office, there were five deaths from e-scooter accidents in Germany in 2020 (e12). Most e-scooter accidents involve young men in their mid-30s who have drunk alcohol (e11, e13, e14). Collision with the curb is a common accident mechanism (e11).
Bicycle- and pedelec-related injuries
The upper limbs are most commonly injured in bicycle accidents, followed by the head. Fractures of the clavicle, radial head, and radial neck are especially common (e11, e15).
Pedelec riders are a special risk group compared to cyclists and tend to be more severely injured in accidents; the reason, at least in part, is thought to be that they are older on average and thus have a greater burden of medical problems. The head is most commonly injured in pedelec accidents, followed by the upper limbs. The head injuries are mainly intracranial hemorrhages, skull contusions, and concussions; the upper limb injuries are mostly clavicular fractures (e12, e16).
The clavicle is fractured by direct impact in a fall, often over the handlebars. Falls onto the outstretched forearm usually cause radial head and radial neck fractures. Fractures of the lower limbs are less common (e15). Abrasions, lacerations, and contusions are the most common traumatic injuries. Head injuries account for most fatal accidents among cyclists (e17).
Cycling is the most common sport-related activity causing injuries in children aged 5 to 14. In this age group, too, clavicular fracture is the most common injury. Intra-abdominal trauma is regularly observed in children and is caused by falls over the handlebars: organs including the liver, spleen and kidneys can be injured. Chest injuries can include rib contusions/fractures, lung injury, and pneumothorax (e15, e18).
Perineal and genital injuries can be caused by the bicycle frame. The spectrum of injuries ranges from anogenital contusions or lacerations to compression injuries of the genitals (e19).
Another typical bicycle-related injury is foot and ankle trauma caused by bicycle spokes, especially in children. This usually involves an isolated lacerations of the heel with possible involvement of the Achilles tendon or an associated fracture of the distal fibula or tibia (e20).
Injuries related to motorized two-wheeled vehicles
Motorcycle accidents generally cause the most serious two-wheeler-related injuries, mainly in men aged 20 to 30. Most motorcyclists involved in accidents have multiple injuries (e21). These are usually fractures and abrasions but can be much more severe, up to amputation (e22).
The injured rider’s having worn a helmet may be reflected by either non-specific or distinctly shaped scratches, hematomas, or areas of dryness located mainly at the helmet pressure points in the cheek or lower jaw area (so-called helmet contact injuries) or in the strap area (floor of the mouth) (16).
The lower limbs are often injured in motorcycle accidents, with open tibia fractures playing a prominent role. The most common upper limb injury is a distal radial fracture (e23, e24). The abdominal viscera often sustain blunt trauma (e24). Although most motorcyclists wear a helmet as required by law, head injuries also occur and can be fatal (e23, e25). Head injuries with a helmet can resemble those without a helmet, but are much less severe with comparable trauma. The types of head injury range from cranial contusions, concussions, and intracerebral hemorrhages to decapitation (e22, e24, e28, e29).
The pattern and severity of the injury depend on the mechanism of the accident. Collision accidents lead to more severe injuries than single-vehicle accidents due to loss of control (e26).
Motorcyclists can be injured by collisions with objects at the side of the road, or with the road surface. Collisions with roadside objects are more likely to be fatal than collisions with the ground or another motor vehicle. In fatal collisions with roadside object, the chest is the most commonly injured region of the body, followed by the head. Annular skull base fractures are usually due to axial compression but are also seen as a traction injury in motorcyclists, e.g., when they are thrown against a tree (e27). Decapitation injuries can also occur. In all other types of collision, head injuries predominate (e28, e29).
Injuries related to two-wheelers.
Accidents involving a human-powered or motorized two-wheeled vehicle (e-scooter, bicycle, pedelec, motorcycle, etc.) relatively often cause injuries with an ISS ≥ 16, because such vehicles lack comprehensive protection systems such as a crumple zone, seatbelts, or airbags.
No legal requirement for protective clothing.
In Germany at present, the law does not require persons riding bicycles/pedelecs or even e-scooters to wear a helmet or special protective clothing (German Road Traffic Regulations, §21a).
Discussion
The injuries discussed here are among the main ones ensuing from typical collisions affecting automobile occupants, riders of two-wheeled vehicles, and pedestrians. Detecting these injuries and documenting them in a way that will stand up in court is important not only for the health of the injured, but also for just and proper consequences under the law.
Like the obtaining of informed consent for a medical procedure, the documentation of injuries after a traffic accident is harder to carry out (and less rigorously demanded) in the immediate emergency situation than later on, once the danger to life has been eliminated (10). Nonetheless, the untreated skin wound in particular is an important source of information about the accident, provided it is not completely covered in blood.
Seatbelt injuries.
The introduction of seatbelts is thought to have lessened the risk of dying in an automobile accident by 50% to 60% (32). The importance of seatbelt injuries in insurance law is obvious. There is no implication, however, that safety devices themselves never cause any injuries.
Airbag-related injuries.
Airbag-specific injuries include ocular injuries (corneal abrasion, anterior chamber hemorrhage, chemical keratitis, other), injuries of the teeth and temporomandibular joints, and barotrauma
The findings should be critically examined for plausibility in relation to the supposed course of the accident and, if necessary, supplemented by further examinations (16), as long as these are medically feasible.
Accident reconstruction is an interdisciplinary task (17) that requires knowledge of medicine and biomechanics as well as an analysis of the accident based on the damage found at the scene and on the vehicle(s) involved.
Reconstructing the accident that caused the injuries of a person who has already been treated in the hospital is much harder if the need for reconstruction was not considered at the outset, for example, if a Messerer wedge was not designated as such or the direction in which it is pointing was not described.
Injuries of persons riding two-wheeled vehicles.
Accidents involving a human-powered or motorized two-wheeled vehicle (e-scooter, bicycle, pedelec, motorcycle, etc.) relatively often cause severe injury.
Reconstruction of the accident.
Accident reconstruction is an interdisciplinary task that requires knowledge of medicine and biomechanics as well as an analysis of the accident based on the damage found at the scene and on the vehicle(s) involved.
Box. Checklist.
Has consent been obtained for documentation?
Does the dataset begin with a photograph of the face?
Are a scale and a color chart included?
Can the photographed body regions, the person concerned and the date of the photograph be identified beyond any doubt?
Was the entire body viewed, and were positive findings that did not require treatment also documented?
Are any unexpected negative findings documented as well?
Can the documentation be understood by uninvolved persons consulting it after the fact?
Are the injuries consistent with the findings regarding the course of the accident?
Have the photos been stored correctly?
Further information on CME.
Participation in the CME certification program is possible only over the Internet: cme.aerzteblatt.de. This unit can be accessed until 11 January 2025. Submissions by letter, e-mail or fax cannot be considered.
The completion time for all newly started CME units is 12 months. The results can be accessed 4 weeks following the start of the CME unit.Please note the respective submission deadline at: cme.aerzteblatt.de.
This article has been certified by the North Rhine Academy for Continuing Medical Education. CME points can be managed using the “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be stated during registration on www.aerzteblatt.de (“Mein DÄ”) or entered in “Meine Daten,” and consent must be given for results to be communicated. The 15-digit EFN can be found on the CME card (8027XXXXXXXXXXX).
Questions on this article.
Participation is possible at cme.aerzteblatt.de.
The submission deadline is 11 January 2025.
Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
Which of the following statements about seat belt injuries to car occupants is true?
The absence of a seatbelt mark implies no seatbelt was worn.
Obese people are at increased risk of submarining.
Seatbelts never cause direct, fatal injuries.
Chance fractures of the spine are typically found at the lumbosacral junction.
Seatbelt injuries do not enable any inferences about the seating position in the vehicle.
Question 2
Which of the following findings after trauma is pathological and should prompt a shock room alert?
systolic blood pressure = 100 mmHg
respiratory rate = 25/min
heart rate = 110/min
oxygen saturation < 90% by pulse oximetry
body temperature = 35.8 °C
Question 3
Which of the following statements about photographic documentation of injuries after traffic accidents is correct?
Documentation of injuries before they are treated can be especially useful for accident reconstruction.
Negative findings should not be documented.
Patient consent is not needed for medicolegally valid documentation.
The legal presumption of innocence implies that any doubts arising from a lack of documentation are judged for the benefit of the injured party.
The documentation of paint, glass splinters, and textile fragments on the injured person’s body is a matter for the police, rather than the physician.
Question 4
Which injury is typical of an accident in which an airbag is deployed?
Messerer wedge
rib fracture
clavicle fracture
pneumothorax
barotrauma
Question 5
A pedestrian is hit by a car from the front and suffers injuries to the medial malleolus and its ligaments. What is the most likely mechanism of injury?
supination trauma
plantar flexion trauma
pronation trauma
internal rotation trauma
dorsiflexion trauma
Question 6
According to the current guideline, when should a shock room team be alerted after a traffic accident?
in the event of a frontal collision resulting in deformation of the hood by less than 50 cm
in the event of a change in speed by more than 20 km/h
in the event of a traffic accident with ejection from the vehicle
after airbag deployment
if two or more persons are involved in the accident
Question 7
In which type of fracture do the fracture ends often not match?
bending fracture
plastic deformity
spiral fracture
multi-fragment fracture
transverse fracture
Question 8
Which body region is most frequently injured in traffic accidents?
the limbs
the head and neck
the spine
the internal organs
the face
Question 9
By what amount did the introduction of seat belts lower the risk of death after a traffic accident?
10–20%
20–30%
30–40%
40–50%
50–60%
Question 10
Which injury is unlikely in an e-scooter accident?
Rib contusion
Radial head fracture
Distal ulnar fracture
Open fracture of the lower leg
Internal knee injury
Acknowledgments
Acknowledgement
The authors thank Johanna Keschreiter for photographic support in Figure 1b.
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
The authors state that they have no conflict of interest.
References
- 1.Statistisches Bundesamt (Destatis), Gesellschaft und Umwelt. Verkehrsunfälle 2022. www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Verkehrsunfaelle/_inhalt.html#sprg238548 (last accessed on 21 November 2022) 2019 [Google Scholar]
- 2.Jehle JM Bundesministerium der Justiz und für Verbraucherschutz (eds.), editors Strafrechtspflege in Deutschland. Fakten und Zahlen. www.bmj.de/SharedDocs/Downloads/DE/Service/Fachpublikationen/Strafrechtspflege_Deutschland.pdf?__blob=publicationFile&v=15 (last accessed on 22 November 2022) [Google Scholar]
- 3.Calil AM, Sallum EA, Domingues CA, Nogueira LS. Mapping injuries in traffic accident victims: a literature review. Rev Latino AM Enfermagem. 2009;171:20–25. doi: 10.1590/s0104-11692009000100019. [DOI] [PubMed] [Google Scholar]
- 4.Lerner EB, Shah MN, Cushman JT, et al. Does mechanism of injury predict trauma center need? Prehosp Emerg Care. 2011;15:518–525. doi: 10.3109/10903127.2011.598617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Otte D, Pohlemann T, Wiese B, Krettek C. Änderung des Verletzungsmusters Polytraumatisierter in den zurückliegenden 30 Jahren. Unfallchirurg. 2003;106:448–455. doi: 10.1007/s00113-003-0620-y. [DOI] [PubMed] [Google Scholar]
- 6.Malczyk A, Helm M, Hossfeld B, et al. Unfallhergang und Verletzungsmuster schwerstverletzter Verkehrsunfallopfer. Der Notarzt. 2014;30:149–158. [Google Scholar]
- 7.Deutsche Gesellschaft für Unfallchirurgie e.V. S3-Leitlinie Polytrauma/Schwerverletzten-Behandlung (AWMF Registernummer 187-023), Version 4.0 (31.12.2022) https://register.awmf.org/de/leitlinien/detail/187-023 (last accessed on 03 December 2023) 2018 [Google Scholar]
- 8.AAAM. Chicago (IL), USA: Abbreviated Injury Scale: 2015 Revision. [Google Scholar]
- 9.Meinberg E, Agel J, Roberts C, et al. Fracture and dislocation compendium—2018. J Orth Traum. 2018;32(Supplement) doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 10.Ondruschka B, Seifert D, König C, Bayer R. Rechtsmedizinische Expertise in der Notfallmedizin—Klinische Untersuchung Schritt für Schritt. Dtsch Med Wochenschr. 2022;147:923–931. doi: 10.1055/a-1793-0064. [DOI] [PubMed] [Google Scholar]
- 11.Graß HL, Gahr B, Ritz-Timme S. Umgang mit Opfern von häuslicher Gewalt in der ärztlichen Praxis. Anregungen für den Praxisalltag. Bundesgesundheitsbl Gesundheitsforschung Gesundheitsschutz. 2016;59:81–87. doi: 10.1007/s00103-015-2269-4. [DOI] [PubMed] [Google Scholar]
- 12.Grassberger M, Verhoff MA. Klinisch-forensische Fotodokumentation. In: Grassberger M, Yen K, Türk E, editors. Klinisch-forensische Medizin. Wien: Springer; 2013. [Google Scholar]
- 13.Verhoff MA, Kettner M, Lászik A, Ramsthaler F. Digital photo documentation of forensically relevant injuries as part of the clinical first response protocol. Dtsch Arztebl Int. 2012;109:638–642. doi: 10.3238/arztebl.2012.0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahlgrimm J, Nurg H, Dettinger J, Moser A. Fußgängerunfälle. In: Burg H, Moser A, editors. Handbuch Verkehrsunfallrekonstruktion. Wiesbaden: Springer Vieweg; 2017. pp. 391–426. [Google Scholar]
- 15.Parzeller M, Wenk M, Zedler B, Rothschild M. Aufklärung und Einwilligung bei ärztlichen Eingriffen. Dtsch Arztebl. 2007;104:576–586. [Google Scholar]
- 16.Mattern R. Verkehrsunfall. In: Brinkmann B, Madea B, editors. Handbuch Rechtsmedizin 1. Berlin, Heidelberg, New York: Springer; 2004. pp. 1171–1214. [Google Scholar]
- 17.Graw M, Adamec J. Unfallrekonstruktion. In: Haffner HT, Skopp G, Graw M, editors. Begutachtung im Verkehrsrecht. Berlin, Heidelberg: Springer; 2012. pp. 255–301. [Google Scholar]
- 18.Schmitt KU, Niederer PF, Cronin DS, Morrison B, III, Muser MH, Walz F. Berlin: Springer Vieweg; 2020. Trauma-Biomechanik—Einführung in die Biomechanik von Verletzungen. [Google Scholar]
- 19.Hartwig S. Fußgängerunfälle. In: Castro WHM, Becke M, Nugel M, editors. Personenschäden im Straßenverkehr: Unfallanalyse, Medizin und Recht. München: C.H. Beck; 2016. pp. 453–457. [Google Scholar]
- 20.Eubanks JJ, Hill PF. Tuscon (AZ) USA: Lawyers & Judges Publishing Co. Inc; 1998. Pedestrian accident reconstruction and litigation. [Google Scholar]
- 21.Huang H, Chin HC, Haque MM. Severity of driver injury and vehicle damage in traffic crashes at intersections: a Bayesian hierarchical analysis. Accid Anal Prev. 2008;40:45–54. doi: 10.1016/j.aap.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Wunderl M. Universität Ulm; 2022. Untersuchung des Einflusses demographischer und unfalltechnischer Faktoren auf das Verletzungsmuster und die Gesamtverletzungsschwere im Rahmen von PKW-Unfällen. Dissertation. [Google Scholar]
- 23.Laberge-Nadeau C, Bellavance F, Messier S, Vézina L, Pichette F. Occupant injury severity from lateral collisions: a literature review. J Safety Res. 2009;40:427–435. doi: 10.1016/j.jsr.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 24.Becker K, Friedrich K, Rothschild M. Rekonstruktion von Verkehrsunfällen. Rechtsmedizin. 2011;21:561–573. [Google Scholar]
- 25.Curtin E, Langlois NE. Predicting driver from front passenger using only the post-mortem pattern of injury following a motor vehicle collision. Med Sci Law. 2007;47:299–310. doi: 10.1258/rsmmsl.47.4.299. [DOI] [PubMed] [Google Scholar]
- 26.Sochor MR, Faust DP, Wang SC, Schneider LW. Knee, thigh and hip injury patterns for drivers and right front passengers in frontal impacts (No 2003-01-0164) SAE Technical Paper. 2003 [Google Scholar]
- 27.Lee J, Conroy C, Coimbra R, Tominaga GT, Hoyt DB. Injury patterns in frontal crashes: the association between knee-thigh-hip (KTH) and serious intra-abdominal injury. Accid Anal Prev. 2010;42:50–55. doi: 10.1016/j.aap.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 28.Neschis DG, Scalea TM, Flinn WR, Griffith BP. Blunt aortic injury. New Engl J Med. 2008;359:1708–1716. doi: 10.1056/NEJMra0706159. [DOI] [PubMed] [Google Scholar]
- 29.Funk JR, Rudd RW, King RJ, Srinivasan SC, Bailey AM, Crandall JR. Injuries caused by brake pedal loading of the midfoot. Biomed Sci Instrum. 2012;48:134–140. [PubMed] [Google Scholar]
- 30.Smith BR, Begeman PC, Leland R, et al. A mechanism of injury to the forefoot in car crashes. Traffic Injury Prev. 2005;6:156–169. doi: 10.1080/15389580590931635. [DOI] [PubMed] [Google Scholar]
- 31.Wagner S, Renner N, Krause J, Perl M. Distorsion der Halswirbelsäule. Pathophysiologie, Diagnostik, Therapie und Begutachtung. Unfallchirurgie. 2022;125:983–994. doi: 10.1007/s00113-022-01248-y. [DOI] [PubMed] [Google Scholar]
- 32.Rüter G. Köln: 1978. Schutzwirkung von Sicherheitsgurten. Band 2: Literaturanalyse, Forschungsberichte der Bundesanstalt für Straßenwesen. [Google Scholar]
- 33.Masudi T, McMahon HC, Scott JL, Lockey AS. Seat belt-related injuries: a surgical perspective. J Emerg Trauma Shock. 2017;10:70–73. doi: 10.4103/0974-2700.201590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reed MP, Ebert-Hamilton SM, Rupp JD. Effects of obesity on seat belt fit. Traff Inj Prev. 2012;13:364–372. doi: 10.1080/15389588.2012.659363. [DOI] [PubMed] [Google Scholar]
- 35.Beck B, Brown J, Bilston LE. Variations in rear seat cushion properties and the effects on submarining. Traff Inj Prev. 2011;12:54–61. doi: 10.1080/15389588.2010.523099. [DOI] [PubMed] [Google Scholar]
- 36.Wallis LA, Greaves I. Injuries associated with airbag deployment. Emerg Med J. 2002;19:490–493. doi: 10.1136/emj.19.6.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pearlman JA, Au Eong KG, Kuhn F, Pieramici DJ. Airbags and eye injuries: epidemiology, spectrum of injury, and analysis of risk factors. Survey Ophthalmol. 2001;6:234–224. doi: 10.1016/s0039-6257(01)00256-9. [DOI] [PubMed] [Google Scholar]
- 38.Mohamed AA, Banerjee A. Patterns of injury associated with automobile airbag use. Postgrad Med J. 1998;74:455–458. doi: 10.1136/pgmj.74.874.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nightingale RW, Winkelstein BA, Van Ee CA, Myers BS. Injury mechanisms in the pediatric cervical spine during out-of-position airbag deployments. Ann Proceed/AAAM. 1998;42:153–164. [Google Scholar]
- 40.Gault JA, Vichnin MC, Jaeger EA, Jeffers JB. Ocular injuries associated with eyeglass wear and airbag inflation. J Trauma Acute Care Surg. 1995;38:494–497. doi: 10.1097/00005373-199504000-00005. [DOI] [PubMed] [Google Scholar]
- E1.Messerer O. Stuttgart: Verlag der J. G. Cotta’schen Buchhandlung; 1880. Über Elastizität und Festigkeit der menschlichen Knochen. [Google Scholar]
- E2.Messerer O. Über die gerichtlich-medicinische Bedeutung verschiedener Knochenbruchformen. Friedreich’s Blätter gerichtl Med Sanitätspol. 1885;36:81–104. [Google Scholar]
- E3.Chatzaraki V, Thali MJ, Ampanozi G, Schweitzer W. Fatal road traffic vehicle collisions with pedestrian victims. Forensic postmortem computed tomography and autopsy correlation. Am J Forensic Med Pathol. 2018;39:130–140. doi: 10.1097/PAF.0000000000000382. [DOI] [PubMed] [Google Scholar]
- E4.Teresiński G, Mądro R. Knee joint injuries as a reconstructive factors in car-to-pedestrian accidents. Forensic Sci Int. 2001;124:74–82. doi: 10.1016/s0379-0738(01)00569-2. [DOI] [PubMed] [Google Scholar]
- E5.Teresiński G, Mądro R. Ankle joint injuries as a reconstruction parameter in car-to-pedestrian accidents. Forensic Sci Int. 2001;118:65–73. doi: 10.1016/s0379-0738(00)00381-9. [DOI] [PubMed] [Google Scholar]
- E6.Teresiński G, Mądro R. Pelvis and hip joint injuries as a reconstructive factors in car-to-pedestrian accidents. Forensic Sci Int. 2001;124:68–73. doi: 10.1016/s0379-0738(01)00567-9. [DOI] [PubMed] [Google Scholar]
- E7.Dettmeyer R, Veit F, Verhoff M, editors. Rechtsmedizin. Heidelberg: Springer; 2019. Verkehrsmedizin. [Google Scholar]
- E8.Bode G, Joachim H. Zur Differentialdiagnose von Unfall- und Reanimationstraumen. Zeitschr Rechtsmed. 1987;98:19–32. doi: 10.1007/BF00200382. [DOI] [PubMed] [Google Scholar]
- E9.Kent T, Miller J, Shreve C, Allenback G, Wentz B. Comparison of injuries among motorcycle, moped and bicycle traffic accident victims. Traffic Inj Prev. 2022;23:34–39. doi: 10.1080/15389588.2021.2004311. [DOI] [PubMed] [Google Scholar]
- E10.Daniello A, Gabler HC. Fatality risk in motorcycle collisions with roadside objects in the United States. Accid Anal Prev. 2011;43:1167–1170. doi: 10.1016/j.aap.2010.12.027. [DOI] [PubMed] [Google Scholar]
- E11.Meyer HL, Kauther MD, Polan C, et al. E-Scooter, E-Bike- und Fahrradverletzungen im gleichen Zeitraum—eine prospektive Vergleichsstudie eines Level-1-Traumazentrums. Unfallchirurg. 2022;14:1–10. doi: 10.1007/s00113-021-01136-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E12.Statistisches Bundesamt (Destatis) Pressemitteilung Nr. N 021 vom 26. März 2021. www.destatis.de/DE/Presse/Pressemitteilungen/2021/03/PD21_N021_462.html (last access on 15 November 2022) [Google Scholar]
- E13.Mair O, Wurm M, Müller M, et al. E-Scooter-Unfälle und deren Folgen: Erste prospektive Analyse der Verletzungsrate und Verletzungsmuster im urbanen Raum einer deutschen Millionenstadt. Unfallchirurg. 2021;124:382–390. doi: 10.1007/s00113-020-00910-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E14.Kleinertz H, Ntalos D, Hennes F, Nüchtern JV, Frosch KH, Thiesen DM. Accident mechanisms and injury patterns in e-scooter users—a retrospective analysis and comparison with cyclists. Dtsch Arztebl Int. 2021;118:117–121. doi: 10.3238/arztebl.m2021.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E15.Silberman MR. Bicycling injuries. Curr Sports Med Rep. 2013;12:337–345. doi: 10.1249/JSR.0b013e3182a4bab7. [DOI] [PubMed] [Google Scholar]
- E16.Lefarth TL, Poos HPAM, Juhra C, Wendt KW, Pieske O. Pedelec-Fahrer werden bei Unfällen schwerer verletzt als konventionelle Radfahrer. Unfallchirurg. 2021;124:1000–1006. doi: 10.1007/s00113-021-00976-x. [DOI] [PubMed] [Google Scholar]
- E17.Mellion MB. Common cycling injuries. Management and prevention. Sports Med. 19911;1:52–70. doi: 10.2165/00007256-199111010-00004. [DOI] [PubMed] [Google Scholar]
- E18.Cevik M, Boleken ME, Sogut O, Gökdemir MT, Karakas E. Abdominal injuries related to bicycle accidents in children. Pediatr Surg Int. 2013;29:459–463. doi: 10.1007/s00383-013-3279-7. [DOI] [PubMed] [Google Scholar]
- E19.Thompson H, Burdall O, Lakhoo K. Degloving injury to groin, scrotum and penis due to low-velocity handlebar injury. BMJ Case Rep. 2019;25 doi: 10.1136/bcr-2019-231598. e231598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E20.Agarwal A, Pruthi M. J Orthop Surg. Vol. 18. Hong Kong: 2010. Bicycle-spoke injuries of the foot in children; pp. 338–341. [DOI] [PubMed] [Google Scholar]
- E21.Cavalcanti AL, Lucena BM, Rodrigues IS, Silva AL, Lima TT, Xavier AF. Motorcycle accidents: morbidity and associated factors in a city of northeast of Brazil. Tanzan J Health Res. 2013;15:209–215. doi: 10.4314/thrb.v15i4.1. [DOI] [PubMed] [Google Scholar]
- E22.Alghnam S, Alsulaim HA, BinMuneif YA, et al. Injuries following motorcycle crashes at a level-1 trauma center in Riyadh. Ann Saudi Med. 2019;39:185–191. doi: 10.5144/0256-4947.2019.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E23.Wick M, Ekkernkamp A, Muhr G. Motorradunfälle im Strassenverkehr. Eine Analyse von 86 Fällen [Motorcycle accidents in street traffic. An analysis of 86 cases] Unfallchirurg. 1997;100:140–145. doi: 10.1007/s001130050105. [DOI] [PubMed] [Google Scholar]
- E24.Martins RS, Saqib SU, Gillani M, Sania SRT, Junaid MU, Zafar H. Patterns of traumatic injuries and outcomes to motorcyclists in a developing country: across-sectional study. Traffic Inj Prev. 2021;221:62–66. doi: 10.1080/15389588.2020.1856374. [DOI] [PubMed] [Google Scholar]
- E25.Peng Y, Vaidya N, Finnie R, et al. Community preventive services task force. Universal motorcycle helmet laws to reduce injuries: a community guide systematic review. Am J Prev Med. 2017;52:820–832. doi: 10.1016/j.amepre.2016.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E26.Martins RS, Saqib SU, Raja MHR, Gillani M, Zafar H. Collision versus loss-of-control motorcycle accidents: comparing injuries and outcomes. Traffic Inj Prev. 2022;23:255–259. doi: 10.1080/15389588.2022.2052284. [DOI] [PubMed] [Google Scholar]
- E27.Holz F, Birngruber CG, Ramsthaler F, Verhoff MA. Frakturen des Gehirnschädels als Folge stumpfer Gewalt. Rechtsmedizin. 2018;28:229–240. [Google Scholar]
- E28.Bambach MR, Mitchell RJ, Grzebieta RH. The protective effect of roadside barriers for motorcyclists. Traffic Inj Prev. 2013;14:756–765. doi: 10.1080/15389588.2012.752077. [DOI] [PubMed] [Google Scholar]
- E29.Osculati A, Visonà SD, Della Chiesa L, Navarra F, Calbi A, Andrello L. Death due to decapitation in two motorcyclists: a description of a unique case and a brief review of the literature. J Forensic Sci. 2017;62:804–806. doi: 10.1111/1556-4029.13346. [DOI] [PubMed] [Google Scholar]