Abstract
Context:
The importance of mental health among athletes is becoming more recognized and valued. Athletes experience symptoms of depression, anxiety, and related mental health disorders at rates similar to those of the general population, but because athletes face unique cultural and environmental pressures, such disorders are exacerbated in the context of an injury. Furthermore, we review the less well-known evidence that mental health disorders in athletes are associated with an increased risk of injury. We discuss the increasing awareness of the deficiencies in mental health support for athletes, which has been especially highlighted during the COVID-19 pandemic as well as in prominent professional and Olympic athletes, and describe both internal and external barriers to appropriate care.
Evidence Acquisition:
We searched PubMed for pertinent peer-reviewed studies.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
There is a known psychological response to injury that can prolong recovery from musculoskeletal injury; conversely, mental health disorders in athletes are not only associated with an increased injury risk but also portend poorer outcomes subsequently, including prolonged recovery times, increased rates of injury recurrence, decreased rates of return to sport, and reduced performance upon return. Because of inherent barriers to appropriate care of athletes, including identification, stigma, and resource availability, there are currently various ongoing efforts nationally to create and implement initiatives regarding athlete mental health screening, support systems, and directed interventions to address the inextricably linked physical and mental health of athletes.
Conclusion:
Athletic injury negatively impacts the mental health of athletes. Likewise, mental health can and does influence athletic performance and is also intimately tied to the risk of athletic injury, thus creating a complex cycle with inability to separate physical and mental health.
Keywords: athlete, injury, mental health, psychology, sport
Elite athletes competing at the collegiate, professional, and Olympic levels face obstacles similar to those of athletes of any tier, including performance plateaus, injuries, lengthy recoveries, and multiple challenges to their mental health. Any elite athlete, regardless of competitive level, can face struggles with mental health, as the path to elite competition often involves major physical and mental hardships and sacrifices. It is important to differentiate between mental health disorders, diagnosed through strict clinical criteria, and mental health symptoms, such as social withdrawal, irritation, and mood disruptions, even in the absence of a diagnosed condition. However, both are relevant to athletes and are differentiated in the research where appropriate.
Mental health disorders are prevalent among athletes of all sports and levels of competition; some evidence suggests a greater prevalence than within the general population. 54 Not only can athletic injuries cause or worsen mental health disorders but mental health disorders can, conversely, prolong injury recovery,1,13 decrease the likelihood of returning to play, 5 and lead to poorer athletic performance. 3
In the present study, we review recent research suggesting that athletes with mental illness may experience an increased risk of injury in the subsequent season. There is well-documented evidence regarding the impact that mental health has on athletic performance; here, we present a sample of the growing body of research demonstrating that mental health conditions are a risk for injury.
Epidemiology
Prevalence of Mental Health Disorders and Symptoms in Athletes
Elite athletes experience nearly the same rate of diagnosis of mental health disorders as the general population 54 ; this has been observed in collegiate as well as in internationally ranked athletes,19,30,61 and some report they may be at greater risk than nonathletes. 69 Athletes must also consider unique cultural and environmental factors, such as competition, performance pressure, injury risk, concern for long-term health, unwanted media attention, and transition out of sport. Decreases in performance that result from any combination of these elements can conflict with an athlete’s perception of self-worth and disrupt his or her identity. 51
The true prevalence of mental health disorders in athletes is difficult to assess accurately because of large variations in age, physical demand of sport, and level of competition. This was highlighted in a Swedish study of 471 professional soccer players, in which the prevalence of mental health symptoms differed significantly across player positions (eg, defensive back, striker) and was higher in male players younger than 21 years. 30 There is also great concern that athlete mental health conditions are underrecognized, underreported, and undertreated; a 2006 report from the National Collegiate Athletic Association (NCAA) showed that 21% of athletes showed symptoms of depression, as measured by the Center for Epidemiologic Studies Depression Scale (CES-D), but that only 4% of athletes reported a history of clinically diagnosed depression. 71 In addition, in the German First League, approximately 40% of sampled injured soccer players surveyed wanted psychiatric support during their tenure 49 ; this cohort of players had significantly higher mean depression scores, yet only 10% reported receiving psychiatric intervention during their career. 49 These concerns have also been highlighted in high school students. Although there is limited evidence comparing mental health disorders in athletes at the secondary level, the Centers for Disease Control 8 reports that the rate of students exhibiting symptoms of depression increased from 26% to 36% between 2009 and 2019. Because of the high rate of athletic involvement and, as the average age of average onset for certain mental health disorders is between 11 and 14 years, 42 there is concern that many student-athletes at the secondary level have symptoms and disorders that are not being identified. Regardless of athletic level, the reasons for underdiagnosis or undertreatment of mental health conditions in athletes are unknown, but possible explanations include physician reluctance to diagnose or refer, athlete resistance to seeking care, and stigma regarding mental health as a weakness. 7
Associated Risk Factors
Mental health disorders in athletes are not limited to depression and anxiety. Research has shown that collegiate male athletes have a higher prevalence of risky behaviors than male student-nonathletes, 33 and similar results were observed when analyzing substance abuse by male athletes. 33 Compared with control groups in the general population, elite athletes have been found to have higher rates of bipolarity, 12 impulsivity, 12 obsessive-compulsive disorder (OCD), 10 and eating disorders.40,62 In addition, in 2015, a 9-year analysis of NCAA athletes revealed the suicide rate to be approximately 1 per 100,000 student-athletes per year, lower than previously reported national rates among the college-age population (7.5 per 100,00). 51 Even though it has been reported that athletic participation may provide a protective effect against suicide, 6 there are certain cases within the NCAA athlete population that have a higher suicide risk, including men, African Americans, football players, and Division I athletes across all sports, the latter category suggesting that competition level may be a factor. 51
Roles of Sex, Gender, and Sexual Orientation
Even within the elite athlete population, there are disparities in the prevalence of mental health disorders across biological sex and sexual orientation. In a 2006 report investigating prevalence of depression of NCAA Division I athletes, 71 female sex and freshman class were significantly associated with depression. This association was further validated in a New Zealand study showing that female athletes reported higher rates of life stressors than competitively equivalent male athletes. 5 Similar findings have been demonstrated for eating disorders. 62
An analysis of nearly 200,000 undergraduate students who completed the American College Health Association’s National College Health Assessment from 2008 to 2012 showed that male athlete sexual minorities (nonhetero-normative sexual preferences) had a significantly higher risk of experiencing mental health symptoms than other athletes. 35 Prevalence of substance abuse was greater among sexual minorities of both sexes, and substance use was significantly associated with negative symptoms (eg, depression, hopelessness, anxiety, suicidal thoughts). Despite these studies, an analysis of collegiate athletes linking preseason anxiety to subsequent injury risk demonstrated that findings were unrelated to athlete sex. 38 Regardless of sex or sexual orientation, it is clear that disparities exist in mental health disorders for athletes who identify as a sexual minority, and this should be recognized in the clinical setting.
Pandemic Effect
Adding insult to injury, the COVID-19 pandemic has compromised the psychological well-being of athletes. Rates of mental health symptoms, such as sleep difficulties or depressed mood, within NCAA athletes were 150% to 250% higher than historically reported, 41 and increased prevalence of uncertainty of athletic future and social isolation have been documented in professional and Olympic athletes.20,50
Effect of Mental Health Conditions on Athletes
Athletic Performance
The physical performance and mental health of elite athletes are closely linked. This was highlighted after the 2012 Summer Olympics, when 50 Canadian swimmers who had qualified for the upcoming Olympic and World Championship trials were studied before and after their competitions. 21 Before competing, 68% reported having had a major depressive episode at least once during the 36 months preceding the trials; this percentage was significantly higher in female athletes, and the prevalence doubled among athletes ranking in the top 25%. Depression was significantly associated with performance failure at the competition; performance was quantified as the actual swim time/score compared with personal best as well as change in national ranking as a result of the competition. A similar study demonstrated that 80% of a sample of 50 elite athletes who exhibited performance failure experienced ≥1 major depressive episode during the 12 months after the Olympic trials. 4 Before the Summer Olympics in Brazil, 221 Australian Olympic athletes from 11 sports completed various health questionnaires during their training to assess risk factors for physical and mental illness. 11 Depressive symptoms and/or perceived stress were significantly associated with future sports incapacity (defined as time lost) because of illness. Furthermore, mental illness was associated with a greater number of physical ailments and worse performance. Disordered eating behaviors displayed a strong association with physical (nutritional) deficiencies and mental health disorders, resulting in impaired athletic performance. 40
Physical Injuries Sustained by Athletes
Mental health disorders have been associated not only with effects on athletic performance but with an increased risk of injury in athletes. The NCAA estimates that approximately 6 student-athlete injuries occur per 1000 athletic-exposures. 32 The extent to which mental health disorders affect this number is unknown. Analysis of the effects of mental health on injuries has shown that symptoms such as competitive anxiety and tension are more related to injury frequency, whereas the degree of tension/anxiety, anger/hostility, and total negative mood state are related to injury severity. 37 A 2017 study showed a significant relationship between anxiety and/or depressive symptoms preseason and subsequent risk of injury to the athlete, with nearly 75% of all injuries associated with these symptoms. 38 Preseason anxiety was still significantly associated with higher injury rates for both sexes (rate ratio, 2.3; 95% CI, 2.0-2.6) after adjusting for number of athletic-exposures, age, race, body mass index, history of injury, and university attended. Although history of injury is known to increase the risk of future injury, even after adjusting for this variable, depression was still independently associated with injury likelihood. 70 Football players with depression at the time of undergraduate enrollment were less likely to remain injury-free than those without depression. 70
The association between mental illness and the risk of injury has been corroborated internationally. 59 An 8-month study of 108 Norwegian junior-level soccer players found that the risk of injury could be predicted successfully in 67% of athletes using 4 factors 27 : life stress, anxiety, mistrust, and ineffective coping were associated with an increased risk of injury. Repeating this analysis in senior-level soccer players showed similar results. 23 A cohort study of 307 participants in the 2015 International Association of Athletics Federations World Championships in Beijing, China, showed that athletes who reported a physical illness symptom that caused anxiety were 5 times more likely to sustain an injury during the events (odds ratio, 5.6; 95% CI, 1.3-23). 63 Competitive climate, high levels of stress, and mood disorders have all been demonstrated as significant predictors of injury.14,59
To characterize this relationship further, researchers required Swedish Premiere League soccer players to complete weekly surveys throughout a season. 25 Trait anxiety (inherent anxiety as part of personality type), stress from significant life-events, and daily hassle (distressing aspects of everyday life) were significant predictors of injury. Specifically, daily hassle was positively correlated with injury frequency, and negative-life-event stress was positively correlated with daily hassle; further analysis demonstrated a significant indirect correlation of negative-life-event stress with injury frequency, suggesting an acute-on-chronic approach to injury prediction. A pair of meta-analyses on psychosocial factors in sports injuries reinforced that stressors and the athlete’s response to stressors have strong associations with, and appear to predict, injury rates, even suggesting that injury rates are lower in groups that receive treatment focused on stress-relief compared with control groups.24,28 It has also been suggested that insufficient sleep increases the propensity for sports-related injuries. 45 This is a reasonable conjecture, as accidents and injuries among sleep-deprived pilots and automobile drivers have been well-documented and led to systematic changes within the respective industries.16,22
There is growing evidence that mental health contributes to the risk of, as well as prolongs recovery from, sports-related concussion. There is an increased risk of concussion in athletes with preinjury aggression and psychoticism; furthermore, there is an increased risk of persistent postconcussive symptoms in those with baseline depression, anxiety, and irritability. 64 Attention-deficit/hyperactivity disorder (ADHD) has been associated with increased risks of concussion and delayed recovery from concussion. An NCAA Division I study found that 50% of 139 athletes surveyed with a diagnosis of ADHD reported a history of ≥1 concussion, compared with only 14% of those without ADHD. 1
A Vicious Cycle
To compound this association between mental health and injury in athletes, there is substantial evidence in the literature that injuries can lead to the development or further exacerbation of mental health disorders. This establishes a complex relationship between an athlete’s mental and physical health, such that neither can be viewed independently. Negative outcomes in one have a demonstrable impact on the other, and the athletes may enter the cycle from either point. A study of elite Australian athletes suggested that rates of symptoms of depression and generalized anxiety disorder were significantly higher in those who had sustained an injury than in noninjured athletes. 19 Chronically injured athletes score in the same range on the Impact of Event Scale as people traumatized by natural disasters. 56 Chronic injuries, or those with extended recovery times, cause mood alterations in athletes compared with college students in a normative group. 57 Athletic injury and failure to succeed significantly increased the risk of suicidal behavior in student-athletes. 51 Furthermore, rehabilitation and return-to-sport rates are negatively affected by preinjury stress in athletes. 66
From a surgical perspective, preoperative scores on both the mental and physical component summaries of the Short-Form Health Survey (SF-12) were predictive of return-to-play after anterior cruciate ligament (ACL) reconstruction. 9 Likewise, “psychological readiness” was identified as a positive influence on return-to-sport after ACL reconstruction. 2 These findings are not limited to the ACL. Patients with preoperative symptoms of psychological distress had higher pain scores and worse range of motion 3 months after rotator cuff repair than a control group, even after controlling for age, sex, tear size, and preoperative range of motion. 46 A significant association between mental health and athlete injury has been found in all extremities and in the axial skeletal system. 55
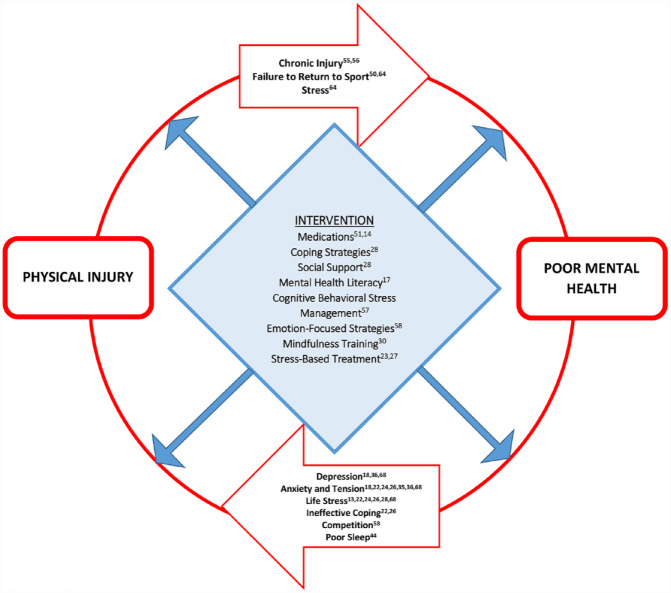
Thus, a cycle (Figure 1) exists in which poor mental health increases the risk of injury and injury increases the risk of poor mental health. Improving the identification and intervention of at-risk athletes at any point in this cycle can prevent potentially detrimental consequences.
Figure 1.
A vicious cycle. Diagram depicting the relationship between mental health and physical injury, also demonstrating areas in which identification and intervention can improve care of the athlete.
Identification of at-Risk Athletes
Theories Explaining the Relationship Between Mental and Physical Health in the Athlete
Stress-Injury Model
One of the most cited theories and earliest explanations of this relationship is from the late 1980s, when partners Williams and Andersen 67 developed the stress-injury model. This model seeks to explain the relationship between stress and injury as nature versus nurture seeks to explain human behavior. On one side is the person, who is the product of personality, genetic predispositions, and perceptions of his or her environment. On the other are external factors, including the concept of intervention - coping resources, grounding factors, and the social infrastructure surrounding that person. The stress response can be seen as representing the physiological effect as a result of the summative forces from both sides.
Within the framework of the stress-response theory, no single stressful event plays a substantial role in the physiologic stress response unless the tendencies of the person are not matched by supportive intervention. The magnitude and extent of the stress response depends on various factors that span the athlete’s life. The authors retested the applicability of their model and found that, of the studies they reviewed analyzing injury in athletes, 85% showed a positive correlation between stress of life events faced by the athlete and subsequent risk of injury. 27
Physiological Theories
Expanding on their model, Williams and Andersen 67 theorized that athletes experience peripheral narrowing of their visual fields when experiencing psychological stress, which can limit focus on their environment and impede the athlete’s ability to avoid risky situations.
Another theory suggests that certain mental health conditions can lead to physiologic responses that make tissue more vulnerable to injury. For example, several neuropsychologic diseases, including ADHD, have manifested features of reduced axonal integrity as well as reduced coordination. 1 Because concussions are associated with axonal shearing, and reduced coordination may be a risk factor for concussion, it is theorized that the physiologic effects of ADHD are the cause of its association with concussion. Symptoms of anxiety and depression can create a dysfunctional psychophysiologic process wherein the disturbance of attention results in changes in arousal and muscle tension, thereby affecting the athlete’s normal physiologic response in a competitive environment and potentially reducing naturally protective measures. 38 Athletes experiencing negative mental health symptoms have exhibited poor risk management in decision-making because of insufficient apprehension of potential risk - a concept supported by the evidence of risky behaviors observed in athletes. 33 OCD has also been analyzed, 10 with a group of 269 collegiate athletes reporting a 17% positive screening rate for OCD. Certain traits of OCD, such as superstitions, rituals, and repetitive behaviors, could be advantageous to the competitive athlete by establishing consistency and emulating the ingame experience. However, athletes who were awarded “all-conference” honors screened positive for OCD less frequently than their peers, 10 suggesting an eventual negative association with performance. One could posit that elite athletes have a better balance of positive and negative symptoms associated with OCD, although this has not been formally studied.
Internal and External Barriers to Appropriate Care
Internal Barriers
Barriers to Appropriate Care Intrinsic in the Athlete
Elite athletes may experience perceived obstacles to seeking and obtaining care for their mental health. A literature review in 2000 noted that major life-event stressors were positively correlated with injuries in football, gymnastics, and track and field, 29 and revealed some important commonalities: injured players were found to have fewer coping mechanisms, the athlete’s degree of social support was inversely related to severity of injury, and competitive anxiety was positively correlated with risk of injury. These fit within the stress-injury model and provide tangible areas for programs and athletic personnel to focus on and improve regarding mental health in athletes.
Another barrier to identification of the at-risk athlete is separating certain psychological conditions from socially acceptable or common behaviors of elite athletes. Athletes with major depressive disorder are frequently misdiagnosed as overtraining. 52 In this setting, laboratory evaluation along with counseling on sleep and nutrition may assist the medical staff in delineating symptoms common to both mental health conditions and overtraining syndrome. Likewise, OCD in athletes is commonly observed as over-responsibility, perfectionism, calorie obsession, and even superstitious behavior. In a field in which rituals are normalized, and even valued, it can be difficult for staff to notice warning signs in an athlete’s behavior.
Even if the athlete overcomes these obstacles to seeking mental health care, there are a multitude of obstacles regarding obtaining appropriate treatment, particularly regarding medication. A systematic review showed that elite athletes have great concern about unknown performance effects, safety, and governing bodies’ policies of using medication to treat mental health conditions. 52 For example, the International Archery Foundation banned a wide array of performance-enhancing drugs, including, but not limited to, many common medications used to treat diagnosed mental health disorders (eg, certain antidepressants and mood stabilizers). 52 This dilemma has been especially complicated by the use of stimulant therapy to treat ADHD in athletes, but there is disparity in terms of medication approval for many common mental health conditions. 15 All these factors contribute to the difficulty that athletes experience when seeking mental health care.
External Barriers
Stigma Regarding Mental Health
Athletes face unique obstacles regarding the diagnosis and treatment of mental health conditions, among which is the associated stigma. A qualitative study found that the stigma surrounding mental health was the single most important barrier to seeking care for elite athletes 18 ; a lack of mental health literacy and negative past experiences with health care providers were also barriers, and these findings have been corroborated. 48
A US study of standardized encounters with 152 athletic support personnel showed that, compared with female athletes with depression, female athletes with anorexia nervosa were viewed as significantly more difficult to communicate with, more likely to be using their disorder to gain attention, personally responsible for their condition, and less likely to recover. 39 Another qualitative study highlighted the following factors contributing to underutilization of mental health resources 47 : denial of emotional problems, counter-dependence (unconscious development of dependence on athletic services), and availability of social support via teammates. This last factor illustrates the concept that athletic teams can provide a sense of friendship and identification during stressful times, effectively eliminating an athlete’s desire to seek help elsewhere. Furthermore, sharing mental health information may influence a coach’s or team’s perspective on an athlete and negatively impact playing time or performance.
Barriers to Appropriate Care Intrinsic to Athletic Infrastructure
Resources for the management of mental health disorders vary according to the sport, level of competition, and individual athlete. One obstacle involves the lack of appropriately trained clinical staff. The field of sports psychiatry is still developing; general clinicians have traditionally been treating athletes. 52 For example, the strongest predictor of an athletics department’s having a written mental health screening plan is the presence of an employed clinical psychologist. 34 As of 2016, team physicians and head athletic trainers across NCAA universities had reported that only 39% of programs have an official written plan related to identifying student-athletes with mental health concerns. 34 Less than half of programs report using a screening method (verbal or written) to identify risk factors for athletes with disordered eating behaviors (44%), depression (32%), or anxiety (37%). A 2015 report indicates that the percentage of athletes identified to have clinically depressive symptoms has not changed significantly over the last several decades and was reported most recently to be approximately one-quarter (24%) of all collegiate athletes, as identified using the CES-D. 68 Because of recent efforts on the part of national governing bodies,61,65 sports medicine physicians, or those acting as the primary care physician to sports organizations, have been encouraged to screen widely for symptoms of depression. As these screening methods are not athlete specific, recent research has focused on developing early distress screening instruments such as the Athlete Psychological Strain Questionnaire. 53 Similar questionnaires have been built to assess sleep quality, 26 which can be administered easily as part of a collective screening protocol. Sports medicine professionals must establish an infrastructure that provides an organized and systematic approach to identifying mental health disorders and promoting psychological wellness.
Ongoing and Potential Interventions
Ongoing Efforts
National governing bodies across athletic levels are aware of the increasing need for identification and intervention of mental health disorders and have made official statements promoting such change.42,43 The NCAA has released a consensus document on the best practices for promoting mental health in student-athletes, including measures to promote screening, incorporating a licensed mental health practitioner, and collaboration of medical records. 43 However, recent evidence suggests that 88% of 137 polled mental health clinicians who treat student-athletes document their findings in a separate medical record, 61 and 72% report using a general student counseling center not affiliated with the athletic department. This highlights the complexity of maintaining mental health records in terms of achieving a balance between the confidentiality of a student-athlete and the desire to decrease stigma and improve communication. Findings show that a stronger relationship between campus health services and athletic staff strengthens care for student-athletes 34 ; this relationship would likely benefit from a developed psychological referral system or mental health emergency action plan.
The National Football League has responded similarly in promoting mental health wellness by launching the Total Wellness Initiative in 2012, establishing a system that orients players toward common mental health practices, mandatory psychoeducational modules, and optional free counseling. 44
The American Medical Society for Sports Medicine released a 2020 consensus statement in which recommendations were made to identify psychological factors, such as stress, as risk factors for poor outcomes after athletic injury. 9 This statement calls for preparticipation examinations and advocates for mental health care to be provided closer to athletic facilities. In a survey of 659 NCAA athletic trainers, nearly 50% believed that better mental care happens in the training room; yet, only 20% reported that a mental health provider could be available in the training room.61,72 Furthermore, higher satisfaction rates were reported when mental health professionals had advanced education specific to the field of athletics, owing to a sense of athletic cultural competency; unfortunately, only a small number of mental health professionals have this type of background and experience. Approximately 70% of athletic trainers who used sport psychologists during the injury-rehabilitation process reported positive experiences that directly complemented their work, including improved coping skills and anxiety management for the student-athletes. 72
Athletic personnel and national organizations generally agree that improving mental health care in athletes involves inclusion of the appropriate sports clinician and integrating health services.
Future Efforts
Questions on how best to improve the diagnosis and treatment of elite athletes remain unanswered. In a 2021 report, the International Olympic Committee described 2 tools specific to elite athletes for the identification of mental health symptoms and disorders. 17 Application and analysis of the efficacy of these tools in future Olympic games may enable improved diagnosis. Psychological interventions using cognitive behavioral stress management, 58 for example, reduced the number of illness and injury days experienced by Olympic athletes compared with a control group. Additional emphasis on coping strategies, 29 in particular, emotion-focused strategies, 59 mindfulness training, 31 and stress-based treatment,24,28 may help reduce injury burden. Further assessment and demonstration of similar interventions across other competition levels are needed.
Obtaining data on the effect of medications on athletes is either impossible because of restrictions by governing bodies or limited by methodology stemming from concerns about impairing an athlete’s performance. 52 Studies that span a season can help to determine the degree to which mental health is impacted. 38 Advanced studies can include criteria to control for other injury confounders, such as biomechanical risk factors. 27 For example, a 2020 systematic review on cognition in athletes demonstrated that lower performance measures of cognition were associated with the development of biomechanical patterns that increased the risk of musculoskeletal injury. 3 When examining the system-level impact of addressing mental health in athletes, the financial burden of expanding access to mental health care can be daunting; for example, a 1998 study projected that adolescents required US$12 billion in medical costs related to mental health. 60 Because of insurance variability and lack of records on out-of-pocket expenses, estimating total cost of certain mental health interventions has proven difficult. However, the NCAA has suggested that hiring outside consultants is an effective way to incorporate mental health professionals while limiting potential costs. 36 As cost remains a concern, athletic governing bodies must provide resources to programs seeking to add appropriate staff, such as clinical psychologists.
Conclusion
Improved mental health resources for athletes are needed. Athletes across all ages and competitive levels experience mental health symptoms at rates similar to the general population, but unique cultural factors pertinent to competitive sports, such as athletic identity, performance expectations, stigma, and injury risks, must be considered for the athlete. Although injuries can lead to mental health disorders in athletes, recent evidence suggests that mental health disorders can be risk factors for injury. Furthermore, mental health disorders lead to poorer outcomes in injured athletes, including prolonged recovery times, increased rates of injury recurrence, decreased rates of return to sport, and reduced performance upon return. The athlete’s mental and physical health are intimately linked, and inappropriate management in either can lead to a tumultuous cycle for both aspects. It is imperative that identification and management of mental health disorders in athletes involve the coordination of an interdisciplinary sports medicine team, including athletic staff, trainers, coaches, and medical providers, to develop evidence-based, standardized methods. Continued research is needed to investigate the association of mental health with the risk of injury, to discover safe and effective treatment options for the athletic population, and to adapt the approach of mental health care to the unique culture of athletics.
Acknowledgments
For their editorial assistance, the authors thank Denise Di Salvo, MS, and Rachel Box, MS, in the Editorial Services group of The Johns Hopkins Department of Orthopaedic Surgery.
Footnotes
The following authors declared potential conflicts of interest: G.D. has received speaking fees from Rowan University. M.T. has received research funding from Fujifilm, consulting fees from Johnson & Johnson, and honorarium from AO North America.
References
- 1. Alosco ML, Fedor AF, Gunstad J. Attention deficit hyperactivity disorder as a risk factor for concussions in NCAA Division-I athletes. Brain Inj. 2014;28(4):472-474. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613-1619. [DOI] [PubMed] [Google Scholar]
- 3. Avedesian JM, Forbes W, Covassin T, Dufek JS. Influence of cognitive performance on musculoskeletal injury risk: a systematic review. Am J Sports Med. 2021;50(2):363546521998081. [DOI] [PubMed] [Google Scholar]
- 4. Baillie PHF, Davis H, Ogilvie BC. Working with elite athletes. In: Van Raalte JL, Brewer BW, eds. Exploring Sport and Exercise Psychology. 3rd ed. Washington DC: American Psychological Association; 2014:401-425. [Google Scholar]
- 5. Beable S, Fulcher M, Lee AC, Hamilton B. SHARPSports Mental health awareness research project: prevalence and risk factors of depressive symptoms and life stress in elite athletes. J Sci Med Sport. 2017;20(12):1047-1052. [DOI] [PubMed] [Google Scholar]
- 6. Brown DR, Blanton CJ. Physical activity, sports participation, and suicidal behavior among college students. Med Sci Sports Exerc. 2002;34(7):1087-1096. [DOI] [PubMed] [Google Scholar]
- 7. Castaldelli-Maia JM, Gallinaro JG de M e, Falcão RS, et al. Mental health symptoms and disorders in elite athletes: a systematic review on cultural influencers and barriers to athletes seeking treatment. Br J Sports Med. 2019;53(11):707-721. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention/National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Adolescent and School Health (DASH) | CDC/Youth Risk Behavior Survey Data Summary & Trends Report 2009-2019. Centers for Disease Control and Prevention. https://www.cdc.gov/healthyyouth/index.htm. Accessed January 17, 2023 [Google Scholar]
- 9. Chang C, Putukian M, Aerni G, et al. Mental health issues and psychological factors in athletes: detection, management, effect on performance and prevention: American Medical Society for Sports Medicine Position Statement - Executive Summary. Br J Sports Med. 2020;54(4):216-220. [DOI] [PubMed] [Google Scholar]
- 10. Cromer L, Kaier E, Davis J, Stunk K, Stewart SE. OCD in college athletes. Am J Psychiatry. 2017;174(6):595-597. [DOI] [PubMed] [Google Scholar]
- 11. Drew MK, Vlahovich N, Hughes D, et al. A multifactorial evaluation of illness risk factors in athletes preparing for the Summer Olympic Games. J Sci Med Sport. 2017;20(8):745-750. [DOI] [PubMed] [Google Scholar]
- 12. Dudek D, Siwek M, Jaeschke R, et al. A web-based study of bipolarity and impulsivity in athletes engaging in extreme and high-risk sports. Acta Neuropsychiatr. 2016;28(3):179-183. [DOI] [PubMed] [Google Scholar]
- 13. Ford IW, Eklund RC, Gordon S. An examination of psychosocial variables moderating the relationship between life stress and injury time-loss among athletes of a high standard. J Sports Sci. 2000;18(5):301-312. [DOI] [PubMed] [Google Scholar]
- 14. Galambos S, Terry P, Moyle G, Locke S, Lane A. Psychological predictors of injury among elite athletes. Br J Sports Med. 2005;39(6):351-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Garner AA, Hansen AA, Baxley C, Ross MJ. The use of stimulant medication to treat attention-deficit/hyperactivity disorder in elite athletes: a performance and health perspective. Sports Med. 2018;48(3):507-512. [DOI] [PubMed] [Google Scholar]
- 16. Goode JH. Are pilots at risk of accidents due to fatigue? J Safety Res. 2003;34(3):309-313. [DOI] [PubMed] [Google Scholar]
- 17. Gouttebarge V, Bindra A, Blauwet C, et al. International Olympic Committee (IOC) Sport Mental Health Assessment Tool 1 (SMHAT-1) and Sport Mental Health Recognition Tool 1 (SMHRT-1): towards better support of athletes’ mental health. Br J Sports Med. 2021;55(1):30-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gulliver A, Griffiths KM, Christensen H. Barriers and facilitators to mental health help-seeking for young elite athletes: a qualitative study. BMC Psychiatry. 2012;12:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gulliver A, Griffiths KM, Mackinnon A, Batterham PJ, Stanimirovic R. The mental health of Australian elite athletes. J Sci Med Sport. 2015;18(3):255-261. [DOI] [PubMed] [Google Scholar]
- 20. Håkansson A, Jönsson C, Kenttä G. Psychological distress and problem gambling in elite athletes during COVID-19 restrictions - a web survey in top leagues of three sports during the pandemic. Int J Environ Res Public Health. 2020;17(18):6693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hammond T, Gialloreto C, Kubas H, Hap Davis H, IV. The prevalence of failure-based depression among elite athletes. Clin J Sport Med. 2013;23(4):273-277. [DOI] [PubMed] [Google Scholar]
- 22. Harris W. Fatigue, circadian rhythm, and truck accidents. In: RR Mackie, ed. Vigilance: Theory, Operational Performance, and Physiological Correlates. NATO Conference Series. New York: Springer US; 1977:133-146. [Google Scholar]
- 23. Ivarsson A, Johnson U. Psychological factors as predictors of injuries among senior soccer players. A prospective study. J Sports Sci Med. 2010;9(2):347-352. [PMC free article] [PubMed] [Google Scholar]
- 24. Ivarsson A, Johnson U, Andersen MB, Tranaeus U, Stenling A, Lindwall M. Psychosocial factors and sport injuries: meta-analyses for prediction and prevention. Sports Med. 2017;47(2):353-365. [DOI] [PubMed] [Google Scholar]
- 25. Ivarsson A, Johnson U, Podlog L. Psychological predictors of injury occurrence: a prospective investigation of professional Swedish soccer players. J Sport Rehabil. 2013;22(1):19-26. [DOI] [PubMed] [Google Scholar]
- 26. Jansson-Fröjmark M, Harvey AG, Lundh L-G, Norell-Clarke A, Linton SJ. Psychometric properties of an insomnia-specific measure of worry: the anxiety and preoccupation about sleep questionnaire. Cog Behav Ther. 2011;40(1):65-76. [DOI] [PubMed] [Google Scholar]
- 27. Johnson U, Ivarsson A. Psychological predictors of sport injuries among junior soccer players. Scand J Med Sci Sports. 2011;21(1):129-136. [DOI] [PubMed] [Google Scholar]
- 28. Johnson U, Ivarsson A. Psychosocial factors and sport injuries: prediction, prevention and future research directions. Curr Opin Psychol. 2017;16:89-92. [DOI] [PubMed] [Google Scholar]
- 29. Junge A. The influence of psychological factors on sports injuries. Am J Sports Med. 2000;28(5 Suppl):10-15. [DOI] [PubMed] [Google Scholar]
- 30. Junge A, Feddermann-Demont N. Prevalence of depression and anxiety in top-level male and female football players. BMJ Open Sport Exerc Med. 2016;2(1):e000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kaiseler M, Poolton JM, Backhouse SH, Stanger N. The relationship between mindfulness and life stress in student-athletes: the mediating role of coping effectiveness and decision rumination. Sport Psychol. 2017;31(3):288-298. [Google Scholar]
- 32. Kerr ZY, Marshall SW, Dompier TP, Corlette J, Klossner DA, Gilchrist J. College sports-related injuries - United States, 2009-10 through 2013-14 academic years. MMWR Morb Mortal Wkly Rep. 2015;64(48):1330-1336. [DOI] [PubMed] [Google Scholar]
- 33. Kokotailo PK, Henry BC, Koscik RE, Fleming MF, Landry GL. Substance use and other health risk behaviors in collegiate athletes. Clin J Sport Med. 1996;6(3):183-189. [DOI] [PubMed] [Google Scholar]
- 34. Kroshus E. Variability in institutional screening practices related to collegiate student-athlete mental health. J Athl Train. 2016;51(5):389-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kroshus E, Davoren AK. Mental health and substance use of sexual minority college athletes. J Am Coll Health. 2016;64(5):371-379. [DOI] [PubMed] [Google Scholar]
- 36. Kroshus E, Reynon A, Goehlert A, Seifert C. Mind, Body and Sport: Understanding and Supporting Student-Athlete Mental Wellness. National Collegiate Athletic Association. https://www.naspa.org/images/uploads/events/Mind_Body_and_Sport.pdf. Accessed January 17, 2023. [Google Scholar]
- 37. Lavallée L, Flint F. The relationship of stress, competitive anxiety, mood state, and social support to athletic injury. J Athl Train. 1996;31(4):296-299. [PMC free article] [PubMed] [Google Scholar]
- 38. Li H, Moreland JJ, Peek-Asa C, Yang J. Preseason anxiety and depressive symptoms and prospective injury risk in collegiate athletes. Am J Sports Med. 2017;45(9):2148-2155. [DOI] [PubMed] [Google Scholar]
- 39. McArdle S, Meade MM, Burrows E. Service providers’ attitudes toward athletes with eating disorders. Clin J Sport Med. 2018;28(1):51-55. [DOI] [PubMed] [Google Scholar]
- 40. Melin A, Torstveit MK, Burke L, Marks S, Sundgot-Borgen J. Disordered eating and eating disorders in aquatic sports. Int J Sport Nutr Exerc Metab. 2014;24(4):450-459. [DOI] [PubMed] [Google Scholar]
- 41. National Collegiate Athletic Association. NCAA student-athlete well-being study. https://www.ncaa.org/sports/2020/5/22/ncaa-student-athlete-well-being-study.aspx. Accessed April 2, 2021
- 42. Neal TL, Diamond AB, Goldman S, et al. Inter-association recommendations for developing a plan to recognize and refer student-athletes with psychological concerns at the collegiate level: an executive summary of a consensus statement. J Athl Train. 2013;48(5):716-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Neal TL, Diamond AB, Goldman S, et al. Interassociation recommendations for developing a plan to recognize and refer student-athletes with psychological concerns at the secondary school level: a consensus statement. J Athl Train. 2015;50(3):231-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. NFL launches new comprehensive total wellness program for current and former NFL players. NFL Player Engagement. https://nfl-pe-stage.azurewebsites.net/news-and-media/press/nfl-launches-new-comprehensive-total-wellness-program-for-current-and-former-nfl-players/. Accessed March 4, 2019
- 45. Owens JA, Weiss MR. Insufficient sleep in adolescents: causes and consequences. Minerva Pediatr. 2017;69(4):326-336. [DOI] [PubMed] [Google Scholar]
- 46. Park JH, Rhee S-M, Kim HS, Oh JH. Effects of anxiety and depression measured via the hospital anxiety and depression scale on early pain and range of motion after rotator cuff repair. Am J Sports Med. 2021;49(2):314-320. [DOI] [PubMed] [Google Scholar]
- 47. Pinkerton RS, Hinz LD, Barrow JC. The college student-athlete: psychological considerations and interventions. J Am Coll Health. 1989;37(5):218-226. [DOI] [PubMed] [Google Scholar]
- 48. Plateau CR, Arcelus J, Leung N, Meyer C. Female athlete experiences of seeking and receiving treatment for an eating disorder. Eat Disord. 2017;25(3):273-277. [DOI] [PubMed] [Google Scholar]
- 49. Prinz B, Dvořák J, Junge A. Symptoms and risk factors of depression during and after the football career of elite female players. BMJ Open Sport Exerc Med. 2016;2(1):e000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ramos e, Côrte AC, Camargo-Junior F, Chalhub T, et al. COVID-19 and its effect on Olympic sport: the importance of studying social isolation and the harm it causes, in order to minimize it. Rev Bras Med Esporte. 2020;26(5):371-377. [Google Scholar]
- 51. Rao AL, Asif IM, Drezner JA, Toresdahl BG, Harmon KG. Suicide in National Collegiate Athletic Association (NCAA) athletes: a 9-year analysis of the NCAA resolutions database. Sports Health. 2015;7(5):452-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Reardon CL, Factor RM. Sport psychiatry. Sports Med. 2010;40(11):961-980. [DOI] [PubMed] [Google Scholar]
- 53. Rice S, Olive L, Gouttebarge V, et al. Mental health screening: severity and cut-off point sensitivity of the Athlete Psychological Strain Questionnaire in male and female elite athletes. BMJ Open Sport Exerc Med. 2020;6(1):e000712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Rice SM, Purcell R, De Silva S, Mawren D, McGorry PD, Parker AG. The mental health of elite athletes: a narrative systematic review. Sports Med. 2016;46(9):1333-1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sarac N, Sarac B, Pedroza A, Borchers J. Epidemiology of mental health conditions in incoming Division I collegiate athletes. Phys Sportsmed. 2018;46(2):242-248. [DOI] [PubMed] [Google Scholar]
- 56. Shuer ML, Dietrich MS. Psychological effects of chronic injury in elite athletes. West J Med. 1997;166(2):104-109. [PMC free article] [PubMed] [Google Scholar]
- 57. Smith AM, Milliner EK. Injured athletes and the risk of suicide. J Athl Train. 1994;29(4):337-341. [PMC free article] [PubMed] [Google Scholar]
- 58. Smyth EA, Newman P, Waddington G, Weissensteiner JR, Drew MK. Injury prevention strategies specific to pre-elite athletes competing in Olympic and professional sports - a systematic review. J Sci Med Sport. 2019;22(8):887-901. [DOI] [PubMed] [Google Scholar]
- 59. Steffen K, Pensgaard AM, Bahr R. Self-reported psychological characteristics as risk factors for injuries in female youth football. Scand J Med Sci Sports. 2009;19(3):442-451. [DOI] [PubMed] [Google Scholar]
- 60. Sturm R, Ringel JS, Bao Y, et al. Mental health care for youth: who gets it? How Much does it cost? Who pays? Where does the money go? RAND Corporation. https://www.rand.org/pubs/research_briefs/RB4541.html. Accessed January 17, 2023 [Google Scholar]
- 61. Sudano LE, Miles CM. Mental health services in NCAA Division I athletics: a survey of head ATCs. Sports Health. 2016;9(3):262-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sundgot-Borgen J, Torstveit MK. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med. 2004;14(1):25-32. [DOI] [PubMed] [Google Scholar]
- 63. Timpka T, Jacobsson J, Bargoria V, et al. Preparticipation predictors for championship injury and illness: cohort study at the Beijing 2015 International Association of Athletics Federations World Championships. Br J Sports Med. 2017;51(4):271-276. [DOI] [PubMed] [Google Scholar]
- 64. Trinh LN, Brown SM, Mulcahey MK. The influence of psychological factors on the incidence and severity of sports-related concussions: a systematic review. Am J Sports Med. 2020;48(6):1516-1525. [DOI] [PubMed] [Google Scholar]
- 65. Trojian T. Depression is under-recognised in the sport setting: time for primary care sports medicine to be proactive and screen widely for depression symptoms. Br J Sports Med. 2016;50(3):137-139. [DOI] [PubMed] [Google Scholar]
- 66. Wiese-Bjornstal DM. Psychology and socioculture affect injury risk, response, and recovery in high-intensity athletes: a consensus statement. Scand J Med Sci Sports. 2010;20(Suppl 2):103-111. [DOI] [PubMed] [Google Scholar]
- 67. Williams JM, Andersen MB. Psychosocial antecedents of sport injury: review and critique of the stress and injury model. J Appl Sport Psychol. 1998;10(1):5-25. [Google Scholar]
- 68. Wolanin A, Hong E, Marks D, Panchoo K, Gross M. Prevalence of clinically elevated depressive symptoms in college athletes and differences by gender and sport. Br J Sports Med. 2016;50(3):167-171. [DOI] [PubMed] [Google Scholar]
- 69. Xanthopoulos MS, Benton T, Lewis J, Case JA, Master CL. Mental health in the young athlete. Curr Psychiatry Rep. 2020;22(11):63. [DOI] [PubMed] [Google Scholar]
- 70. Yang J, Cheng G, Zhang Y, Covassin T, Heiden EO, Peek-Asa C. Influence of symptoms of depression and anxiety on injury hazard among collegiate American football players. Res Sports Med. 2014;22(2):147-160. [DOI] [PubMed] [Google Scholar]
- 71. Yang J, Peek-Asa C, Corlette JD, Cheng G, Foster DT, Albright J. Prevalence of and risk factors associated with symptoms of depression in competitive collegiate student athletes. Clin J Sport Med. 2007;17(6):481-487. [DOI] [PubMed] [Google Scholar]
- 72. Zakrajsek RA, Martin SB, Wrisberg CA. National Collegiate Athletic Association Division I Certified athletic trainers’ perceptions of the benefits of sport psychology services. J Athl Train. 2016;51(5):398-405. [DOI] [PMC free article] [PubMed] [Google Scholar]