Abstract
Introduction:
High-quality epidemiological data on hemorrhagic stroke (HS) and its subtypes, intracerebral hemorrhage (ICH) and subarachnoid hemorrhage (SAH), remains limited in Asian ethnicities. We investigated the trends in HS incidence and 30-day mortality from 2005 to 2019 in a multi-ethnic Asian population from a national registry.
Patients and methods:
Data on all stroke cases from the Singapore Stroke Registry from 2005 to 2019 were collected. Cases were defined using centrally adjudicated review of diagnosis codes. Death outcomes were obtained by linkage with the national death registry. Incidence (per 100,000 people) and 30-day mortality (per 100 people) were measured as crude and age-standardized rates. Trends were analyzed using linear regression.
Results:
We analyzed 19,017 cases of HS (83.9% ICH; 16.1% SAH). From 2005 to 2019, age-standardized incidence rates (ASIR) for HS remained stable from 34.4 to 34.5. However, age-standardized mortality rates (ASMR) decreased significantly from 29.5 to 21.4 (p < 0.001). For ICH, ASIR remained stable while ASMR decreased from 30.4 to 21.3 (p < 0.001); for SAH, ASIR increased from 2.7 to 6.0 (p = 0.006) while ASMR remained stable. In subgroup analyses, HS incidence increased significantly in persons <65 years (from 18.1 to 19.6) and Malays (from 39.5 to 49.7).
Discussion:
From 2005 to 2019, ASIR of HS remained stable while ASMR decreased. Decreasing ASMR reflects improvements in the overall management of HS, consistent with global trends.
Conclusion:
Population health efforts to address modifiable risk factors for HS in specific demographic subgroups may be warranted to reduce incidence and mortality of HS.
Keywords: Hemorrhagic stroke, epidemiology, incidence, mortality, intracerebral hemorrhage, subarachnoid hemorrhage
Graphical abstract.
Introduction
Globally, hemorrhagic stroke (HS) represents approximately 37.6% of all stroke cases. 1 There is a need for high-quality epidemiological studies on HS, particularly those including specific subgroups of intracerebral hemorrhage (ICH) and subarachnoid hemorrhage (SAH). 2 Worldwide, the age-standardized incidence rates (ASIR) of ICH and SAH were 41.81 and 14.46 per 100,000 people in 2019, respectively. 1 The age-standardized morality rates (ASMR) of ICH and SAH were 36.04 and 4.66 per 100,000 people, respectively. 1 The global incidence and mortality rates of both HS subtypes showed a declining trend from 1990 to 2019. 1
Considerable geographical variations in HS incidence and mortality have been reported,1,3 with several studies indicating a higher risk of HS in individuals of Asian ethnicity compared to non-Asians.4–7 For ICH and SAH, both incidence and mortality rates decreased in Asia and its subregions from 1990 to 2019, with the exception of a 40.2% increase in the ASIR of SAH in high-income Asia Pacific countries, and a 15.4% increase in the ASMR of SAH in Central Asia. 1 In country-specific studies from Asia, trends in HS incidence were variable,8–12 while mortality trends were more homogeneous, with decreasing ASMR of both ICH and SAH reported in Japan (1961–2009), 13 China (1990–2019), 9 Taiwan (2004–2011), 10 Korea (2012–2020), 14 and Malaysia (2008–2016). 12 Despite these findings, some were not based on primary data, 9 were not nationally representative,8,13,15 or only investigated incidence 8 or mortality13,14 but not both within the same cohort. None of the studies were based on data from a national stroke registry,8–15 and several lacked data from the last decade.10,11,13 Notably, the 2021 Global Burden of Diseases study highlighted that up-to-date, country-specific data by stroke subtype were scarce, with a lack of original, good-quality stroke epidemiological studies for most countries, 1 particularly in Asia 3 and for HS (including ICH and SAH). 14 This underscores the need for epidemiological studies on HS in Asian populations to drive improvements in patient care and clinical outcomes.
Evaluation of HS epidemiology by ethnicity is also important to aid in the prioritization of health system funding and research for vulnerable populations. 6 Most epidemiological studies on HS in Asia have been conducted based on geographical region without stratification of by ethnicity.9,12 Given its multi-ethnic population, Singapore was uniquely positioned to contribute to the understanding of inter-ethnic trends in stroke incidence and mortality in Asia.
In 2016, the first nationwide hospital-based stroke registry study from Singapore was published, showing declining trends in stroke incidence and case fatality from 2006 to 2012, especially in women, older age groups, and ischemic stroke. 16 However, no significant trends were identified specifically for patients with HS. Thus, we aimed to investigate the trends in HS incidence and mortality, and conduct subgroup analyses according to age, sex, race, and HS subtype from 2005 to 2019 in a multi-ethnic Asian population.
Methods
Setting
The study population was the population of Singapore. Singapore is a heavily urbanized, densely populated island city-state in Southeast Asia, with a population of 5.7 million over a land area of 725.7 km2 (population density 7810 per km2). 17 During the study period, seven restructured general hospitals managed more than 95% of HS patients, with the remaining 5% managed by private hospitals. 18
Study population and outcome data
The annual number of stroke cases were obtained from the Singapore Stroke Registry (SSR), 19 which received stroke case notifications from all public healthcare institutions via hospital inpatient discharge summaries, medical claim listings, and the national death registry, capturing both inpatient and out-of-hospital fatal stroke cases. The International Classification of Diseases (ICD) diagnosis codes were used to identify stroke cases, comprising ICD-9 codes 430–437 (excluding 432.1 and 435) prior to 2012, and ICD-10 codes I60 to I68 (excluding I62.0, I62.1) from 2012 onward. Registry coordinators confirmed the diagnosis of HS by assessing patients’ medical records before extracting detailed individual-level clinical data.
All cases were diagnosed as HS by a medical practitioner, defined as the presence of neurological deficit lasting >24 h, supported by CT brain imaging diagnosis of hemorrhagic stroke. We included all cases of HS aged ⩾15 years in Singapore from 1 January 2005 to 31 December 2019 from the SSR. The date of presentation to hospital was taken as the event date for patients admitted due to stroke, while the date of onset of stroke symptoms was taken as the event date for patients admitted due to other conditions prior to stroke. Data collected by the SSR include age, sex, and race (Chinese, Malay, Indian, or other races, defined by linkage with the national registration identity card (NRIC) number), and HS subtype (ICH or SAH). Data from the SSR were subject to annual audits for accuracy and inter-rater reliability. Outlier and illogical data were flagged for review and consensus among registry coordinators.
The incidence rate in each year was calculated by taking the number of stroke episodes that occurred in a year, divided by the number of Singapore residents in the same year. The annual Singapore resident population used (as denominators) to calculate incidence rates were obtained from the Singapore Department of Statistics, which compiles population data from birth, death and migration and publishes Singapore’s mid-year population annually. 17
Death data was obtained from the Registry of Births and Deaths, which records all deaths occurring within Singapore and its territorial waters under the Registration of Births and Deaths Act, 20 hence capturing all deaths due to stroke in Singapore. Death data was merged with SSR data to retrieve the survival status of all stroke patients, and the cause and date of death of patients who died during the study period. Primary cause of death was defined according to the World Health Organization definition as “the disease or injury which initiated the train of morbid events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury.” 21 The 30-day mortality rate in each year was calculated by taking the number of deaths with stroke as the primary cause of death that occurred within 30 days from onset of stroke, divided by the number of stroke patients in the same year.
The Centralised Institutional Review Board granted approval for this study with a waiver of patient consent (CIRB Ref: 2017/2380).
Statistical analysis
Baseline characteristics of all included cases were presented using frequency with proportion for categorical variables and median with interquartile range (IQR) for continuous variables. Chi-squared test and Wilcoxon rank-sum test were used to compare the baseline characteristics by survival status at 30 days after stroke. Trends in incidence and 30-day mortality were reported using annual crude incidence rates (CIR), age-standardized incidence rates (ASIR), crude mortality rates (CMR), and age-standardized mortality rates (ASMR). Incidence rates were calculated by dividing the number of stroke cases in a calendar year by the resident population in the same year, while mortality rates were calculated by dividing the number of stroke patients who died within 30 days after stroke in a calendar year by the number of stroke patients in the same year. ASIR and ASMR were directly standardized using the World Health Organization standard population 22 and stroke patients in Singapore in 2005 respectively. Incidence rates were presented as per 100,000 Singapore resident population, and mortality rates as per 100 stroke patients. Linear regression was used to determine if changes in logarithmic CIR, ASIR, CMR, and ASMR over time were significant. Subgroup analyses were performed by age, sex, race, and HS subtype. Statistical analyses were performed using STATA/SE 13 (StataCorp, College Station, Texas). Two-tailed p-values < 0.05 were considered statistically significant.
Results
Baseline characteristics of patients with HS between 2005 and 2019
There were 19,017 cases of HS aged ⩾15 years between 2005 and 2019. The median age was 64.4 years (IQR = 54.1–75.7) and 10,429 cases (54.8%) were male. Majority were Chinese (79.8%), followed by Malay (14.3%), Indian (4.2%), and other ethnicities (1.7%); this was similar to the ethnic composition of the Singapore resident population of Chinese (76.0%), Malays (15.0%), Indians (7.5%), and other ethnicities (1.5%) as of June 2019. 23 15,957 cases (83.9%) were ICH, while 3060 (16.1%) were SAH. About 4895 cases (25.7%) died within 30 days after onset of HS. Baseline characteristics of the study cohort are presented in Table 1.
Table 1.
Baseline characteristics of hemorrhagic stroke patients by 30-day mortality.
| Overall n = 19,017 | 30-day mortality | p-Value | ||
|---|---|---|---|---|
| No n = 14,122 (74.3%) | Yes n = 4895 (25.7%) | |||
| Demographics | ||||
| Age, median (IQR) | 64.4 (54.1–75.7) | 62.6 (53.1–73.6) | 70.3 (57.7–80.7) | <0.001 |
| ⩾65 years, n (%) | 9239 (48.6) | 6233 (44.1) | 3006 (61.4) | <0.001 |
| Male, n (%) | 10,429 (54.8) | 7875 (55.8) | 2554 (52.2) | <0.001 |
| Race, n (%) | ||||
| Chinese | 15,179 (79.8) | 11,238 (79.6) | 3941 (80.5) | 0.015 |
| Malay | 2722 (14.3) | 2079 (14.7) | 643 (13.1) | |
| Indian | 800 (4.2) | 584 (4.1) | 216 (4.4) | |
| Others | 316 (1.7) | 221 (1.6) | 95 (1.9) | |
| Stroke subtype | ||||
| ICH | 15,957 (83.9) | 12,001 (85.0) | 3956 (80.8) | <0.001 |
| SAH | 3060 (16.1) | 2121 (15.0) | 939 (19.2) | |
IQR: interquartile range; ICH: intracerebral hemorrhage; SAH: subarachnoid hemorrhage.
Trends in incidence of HS between 2005 and 2019
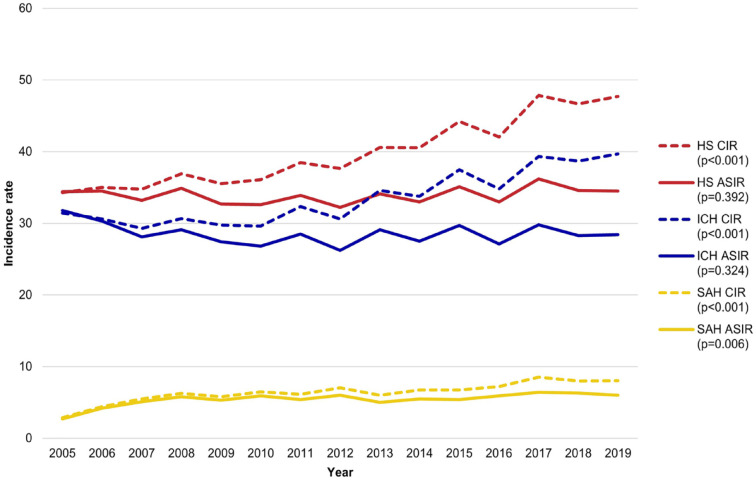
The trends in yearly CIR and ASIR for HS and subtypes of ICH and SAH are shown in Figure 1 and Table 2. From 2005 to 2019, CIR of HS increased from 34.3 (32.2–36.6) to 47.7 (45.4–50.1) (p < 0.001), while ASIR remained stable at 34.4 (32.2–36.7) in 2005 and 34.5 (32.8–36.2) in 2019. For HS subtypes, CIR of ICH increased (p < 0.001) while ASIR remained stable; and both CIR and ASIR of SAH increased (CIR p < 0.001; ASIR p = 0.006) (Table 2).
Figure 1.
Crude incidence rates (CIR) and age-standardized incidence rates (ASIR) of hemorrhagic stroke (HS) (2005–2019). p-values for trend are indicated.
ICH: intracerebral hemorrhage; SAH: subarachnoid hemorrhage.
Table 2.
Crude and age-standardized incidence rates of hemorrhagic stroke from 2005 to 2019.
| Incidence rate, per 100,000 persons (95% CI) | p-Value | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | ||
| HS and subtypes | ||||||||||||||||
| HS CIR | 34.3 (32.2–36.6) | 35.0 (32.9–37.3) | 34.7 (32.6–37.0) | 36.9 (34.8–39.2) | 35.6 (33.5–37.7) | 36.1 (34.0–38.3) | 38.5 (36.3–40.7) | 37.7 (35.6–39.9) | 40.6 (38.4–42.8) | 40.5 (38.4–42.8) | 44.2 (42.0–46.5) | 42.0 (39.9–44.3) | 47.8 (45.5–50.2) | 46.7 (44.4–49.0) | 47.7 (45.4–50.1) | <0.001 |
| HS ASIR | 34.4 (32.2–36.7) | 34.5 (32.4–36.8) | 33.2 (31.1–35.3) | 34.9 (32.9–37.1) | 32.7 (30.8–34.7) | 32.6 (30.7–34.6) | 33.9 (32.0–35.9) | 32.2 (30.4–34.1) | 34.1 (32.2–36.0) | 33.0 (31.2–34.9) | 35.1 (33.3–36.9) | 33.0 (31.3–34.8) | 36.2 (34.5–38.1) | 34.6 (32.9–36.4) | 34.5 (32.8–36.2) | 0.392 |
| ICH CIR | 31.4 (29.4–33.6) | 30.6 (28.6–32.7) | 29.3 (27.3–31.3) | 30.7 (28.7–32.7) | 29.7 (27.8–31.7) | 29.6 (27.7–31.6) | 32.4 (30.4–34.4) | 30.6 (28.7–32.6) | 34.6 (32.6–36.6) | 33.8 (31.8–35.8) | 37.5 (35.4–39.6) | 34.8 (32.8–36.9) | 39.3 (37.2–41.5) | 38.7 (36.6–40.8) | 39.7 (37.6–41.8) | <0.001 |
| ICH ASIR | 31.8 (29.4–33.6) | 30.3 (28.1–32.1) | 28.1 (26.3–30.2) | 29.1 (27.1–30.9) | 27.4 (25.9–29.6) | 26.8 (25.2–28.8) | 28.5 (27.1–30.7) | 26.2 (24.8–28.2) | 29.1 (27.5–31.0) | 27.5 (26.1–29.5) | 29.7 (28.7–32.2) | 27.1 (25.9–29.2) | 29.8 (28.5–31.9) | 28.3 (27.0–30.3) | 28.4 (27.3–30.5) | 0.324 |
| SAH CIR | 2.9 (2.3–3.6) | 4.4 (3.7–5.2) | 5.5 (4.7–6.4) | 6.3 (5.4–7.2) | 5.8 (5.0–6.7) | 6.5 (5.6–7.4) | 6.1 (5.3–7.0) | 7.0 (6.2–8.0) | 6.0 (5.2–6.9) | 6.7 (5.9–7.7) | 6.7 (5.9–7.7) | 7.2 (6.3–8.2) | 8.5 (7.6–9.6) | 8.0 (7.1–9.0) | 8.0 (7.1–9.0) | <0.001 |
| SAH ASIR | 2.7 (2.3–3.6) | 4.2 (3.6–5.2) | 5.1 (4.5–6.2) | 5.8 (5.1–6.9) | 5.3 (4.7–6.4) | 5.9 (5.2–6.9) | 5.4 (4.9–6.6) | 6.0 (5.5–7.2) | 5.0 (4.6–6.1) | 5.5 (5.1–6.7) | 5.4 (4.9–6.4) | 5.9 (5.4–7.1) | 6.4 (6.1–7.7) | 6.3 (5.8–7.5) | 6.0 (5.5–7.1) | 0.006 |
| By ethnicity | ||||||||||||||||
| Chinese CIR | 36.2 (33.7–38.8) | 36.6 (34.1–39.3) | 36.1 (33.6–38.6) | 38.3 (35.8–40.9) | 37.1 (34.7–39.7) | 37.8 (35.4–40.4) | 39.8 (37.4–42.5) | 40.4 (37.9–43.0) | 42.3 (39.8–45.0) | 43.0 (40.4–45.7) | 46.9 (44.3–49.7) | 44.6 (42.0–47.3) | 50.7 (47.9–53.5) | 50.1 (47.4–52.9) | 49.8 (47.1–52.6) | <0.001 |
| Chinese ASIR | 34.6 (33.7–38.8) | 34.4 (33.4–38.4) | 32.5 (32.1–37.0) | 34.2 (33.4–38.2) | 32.0 (31.9–36.5) | 31.9 (31.8–36.3) | 33.0 (33.0–37.6) | 32.4 (32.3–36.8) | 33.4 (33.2–37.7) | 32.8 (32.9–37.3) | 35.1 (35.5–40.0) | 32.8 (32.9–37.3) | 35.9 (36.3–40.7) | 34.9 (35.1–39.4) | 33.5 (33.7–37.8) | 0.398 |
| Malay CIR | 32.4 (26.7–38.9) | 34.7 (28.9–41.3) | 41.8 (35.5–49.0) | 41.0 (34.7–48.0) | 40.6 (34.5–47.5) | 42.7 (36.5–49.7) | 46.8 (40.3–54.1) | 42.9 (36.8–49.8) | 47.5 (41.0–54.6) | 46.6 (40.2–53.6) | 50.9 (44.3–58.2) | 48.4 (42.0–55.5) | 53.4 (46.7–60.7) | 48.7 (42.4–55.7) | 55.6 (48.8–63.0) | <0.001 |
| Malay ASIR | 39.5 (26.7–38.9) | 40.5 (28.4–40.6) | 48.6 (34.1–47.1) | 47.5 (32.6–45.2) | 44.0 (32.6–45.0) | 47.8 (33.5–46.0) | 50.2 (35.9–48.4) | 45.0 (33.0–45.1) | 47.0 (34.2–46.0) | 45.8 (35.1–47.7) | 49.2 (36.5–48.8) | 46.5 (35.2–47.6) | 50.3 (38.3–51.0) | 44.9 (33.7–45.5) | 49.7 (39.2–52.2) | 0.034 |
| Indian CIR | 17.1 (12.1–23.5) | 21.5 (16.0–28.4) | 14.5 (10.1–20.1) | 20.7 (15.5–27.2) | 20.9 (15.8–27.1) | 18.7 (13.9–24.6) | 22.1 (16.9–28.4) | 13.6 (9.6–18.7) | 20.6 (15.7–26.7) | 16.2 (11.9–21.6) | 20.3 (15.4–26.2) | 18.7 (14.1–24.4) | 22.7 (17.5–28.8) | 20.7 (15.9–26.6) | 25.6 (20.1–32.0) | 0.172 |
| Indian ASIR | 19.0 (12.1–23.5) | 25.1 (16.1–28.5) | 16.9 (10.2–20.3) | 23.2 (15.8–27.8) | 25.6 (15.5–26.8) | 22.5 (13.2–23.5) | 24.4 (16.3–27.5) | 15.5 (9.0–17.6) | 21.6 (13.7–23.6) | 17.0 (9.8–18.2) | 19.9 (13.2–22.8) | 18.0 (11.9–21.2) | 20.6 (13.5–22.6) | 18.9 (12.3–21.1) | 23.1 (15.4–24.9) | 0.512 |
| By age group | ||||||||||||||||
| <65 years CIR | 19.8 (18.1–21.6) | 18.8 (17.2–20.6) | 21.4 (19.7–23.3) | 21.6 (19.8–23.4) | 22.2 (20.5–24.0) | 21.9 (20.2–23.8) | 23.6 (21.8–25.5) | 23.5 (21.8–25.4) | 23.8 (22.0–25.7) | 24.0 (22.2–25.9) | 26.8 (24.9–28.8) | 26.0 (24.2–27.9) | 27.3 (25.4–29.3) | 26.4 (24.6–28.4) | 26.2 (24.3–28.1) | <0.001 |
| <65 years ASIR | 18.1 (18.1–21.6) | 16.8 (16.9–20.3) | 18.7 (18.9–22.4) | 18.6 (18.7–22.1) | 18.6 (19.1–22.5) | 18.1 (18.5–21.8) | 19.0 (19.6–23.0) | 18.6 (19.2–22.5) | 18.7 (19.3–22.6) | 18.7 (19.4–22.7) | 20.7 (21.7–25.1) | 20.2 (20.8–24.2) | 20.8 (21.6–25.0) | 19.9 (20.6–24.0) | 19.6 (20.4–23.8) | <0.001 |
| ⩾65 years CIR | 163.7 (149.0–179.4) | 174.9 (160.1–190.6) | 147.9 (134.6–162.2) | 166.0 (152.1–180.9) | 146.3 (133.6–160.0) | 152.3 (139.4–166.0) | 156.6 (143.8–170.2) | 142.7 (130.9–155.2) | 157.9 (145.9–170.6) | 149.0 (137.7–161.0) | 151.8 (140.8–163.5) | 135.8 (125.6–146.5) | 161.4 (150.6–172.7) | 152.0 (141.9–162.7) | 153.3 (143.4–163.8) | 0.138 |
| ⩾65 years ASIR | 164.8 (149.0–179.4) | 175.5 (160.7–191.3) | 148.7 (134.9–162.6) | 165.3 (151.0–179.5) | 144.7 (131.8–157.9) | 148.5 (135.1–160.9) | 153.2 (140.4–166.3) | 140.3 (127.7–151.5) | 156.5 (144.0–168.5) | 147.3 (135.4–158.3) | 149.7 (138.3–160.9) | 134.7 (123.8–144.7) | 159.6 (148.5–170.4) | 151.6 (140.9–161.7) | 152.7 (142.1–162.3) | 0.118 |
| By sex | ||||||||||||||||
| Male CIR | 36.9 (33.7–40.3) | 38.3 (35.1–41.7) | 37.5 (34.4–40.8) | 41.8 (38.5–45.2) | 40.7 (37.6–44.1) | 40.7 (37.5–44.0) | 43.9 (40.7–47.4) | 42.4 (39.3–45.8) | 45.8 (42.6–49.3) | 45.0 (41.7–48.4) | 50.8 (47.3–54.4) | 48.9 (45.6–52.4) | 52.0 (48.6–55.6) | 53.1 (49.7–56.8) | 53.4 (49.9–57.0) | <0.001 |
| Male ASIR | 38.7 (33.7–40.3) | 40.5 (34.4–40.8) | 37.3 (33.0–39.2) | 41.6 (36.3–42.7) | 38.8 (35.0–41.1) | 38.3 (34.1–40.1) | 40.0 (36.3–42.3) | 37.4 (33.9–39.7) | 39.9 (36.2–42.1) | 38.3 (34.5–40.2) | 41.8 (39.0–45.1) | 40.1 (36.3–42.0) | 40.9 (37.7–43.4) | 41.3 (38.0–43.7) | 40.6 (37.6–43.3) | 0.117 |
| Female CIR | 31.8 (28.9–34.9) | 31.9 (29.0–34.9) | 32.1 (29.3–35.1) | 32.3 (29.5–35.3) | 30.6 (27.9–33.4) | 31.7 (29.0–34.6) | 33.2 (30.5–36.2) | 33.1 (30.4–36.0) | 35.5 (32.7–38.5) | 36.3 (33.4–39.3) | 38.0 (35.1–41.0) | 35.5 (32.8–38.5) | 43.9 (40.8–47.1) | 40.5 (37.6–43.6) | 42.4 (39.4–45.5) | <0.001 |
| Female ASIR | 30.1 (28.9–34.9) | 29.5 (28.6–34.4) | 29.2 (28.3–34.0) | 28.8 (27.9–33.4) | 26.9 (26.2–31.4) | 27.3 (26.5–31.7) | 28.3 (27.5–32.7) | 27.3 (26.5–31.5) | 28.6 (27.7–32.7) | 28.0 (27.8–32.7) | 28.4 (28.1–32.9) | 26.3 (26.2–31.0) | 31.6 (31.3–36.3) | 28.1 (27.7–32.4) | 28.5 (28.1–32.7) | 0.605 |
HS: hemorrhagic stroke; ICH: intracerebral hemorrhage; SAH: subarachnoid hemorrhage; CIR: crude incidence rate; ASIR: age-standardized incidence rate; CI: confidence interval.
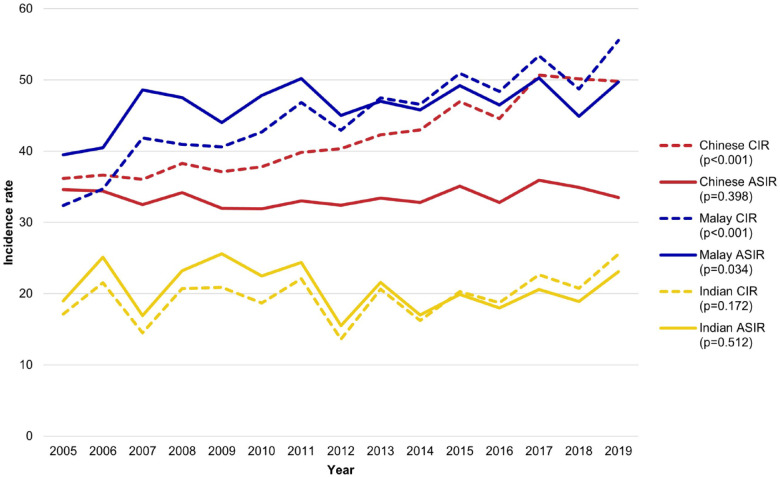
Figure 2 shows the trends in yearly CIR and ASIR for HS stratified by ethnicity. From 2005 to 2019, Chinese had an increase in CIR (p < 0.001) while ASIR remained stable; Malays had an increase in both CIR (p < 0.001) and ASIR (p = 0.034); and Indians had fluctuating CIR and ASIR (Table 2).
Figure 2.
Crude incidence rates (CIR) and age-standardized incidence rates (ASIR) of hemorrhagic stroke by ethnicity. p-values for trend are indicated.
When stratified by age group (<65 years vs ⩾65 years), CIR and ASIR of those <65 years increased from 2005 to 2019 (p < 0.001), while CIR and ASIR of those ⩾65 years fluctuated over the years. When stratified by sex, CIR of both males and females increased from 2005 to 2019 (p < 0.001), while ASIR of both groups remained stable. (Table 2; Supplemental Figure S1).
Trends in 30-day mortality of HS between 2005 and 2019
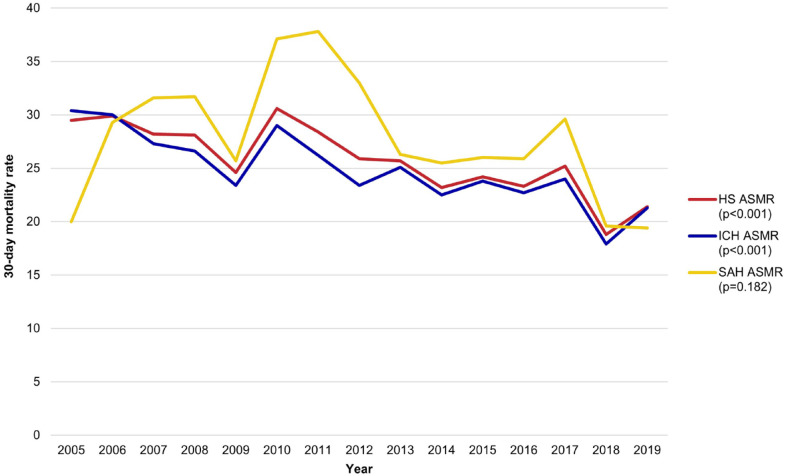
The trends in yearly CMR and ASMR for HS and subtypes of ICH and SAH are shown in Figure 3 and Table 3. From 2005 to 2019, CMR of HS decreased from 29.5 (26.2–33.2) to 22.9 (20.6–25.3) (p < 0.001), and ASMR decreased from 29.5 (26.2–33.2) to 21.4 (19.3–23.8) (p < 0.001). For HS subtypes, CMR and ASMR of ICH decreased (CMR p = 0.001; ASMR p < 0.001); while CMR and ASMR of SAH remained stable (Table 3).
Figure 3.
Age-standardized mortality rates (ASMR) of hemorrhagic stroke (HS) (2005–2019). p-values for trend are indicated.
ICH: intracerebral hemorrhage; SAH: subarachnoid hemorrhage.
Table 3.
Crude and age-standardized 30-day mortality rates of hemorrhagic stroke from 2005 to 2019.
| 30-day mortality rate, per 100 persons (95% CI) | p-Value | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | ||
| HS and subtypes | ||||||||||||||||
| HS CMR | 29.5 (26.2–33.2) | 30.3 (27.0–33.9) | 28.2 (25.1–31.7) | 28.2 (25.1–31.5) | 24.2 (21.4–27.3) | 30.7 (27.5–34.1) | 28.1 (25.2–31.3) | 25.9 (23.1–28.9) | 26.0 (23.3–28.9) | 24.1 (21.5–26.8) | 24.6 (22.1–27.3) | 23.6 (21.1–26.3) | 26.1 (23.7–28.7) | 19.6 (17.5–22.0) | 22.9 (20.6–25.3) | <0.001 |
| HS ASMR | 29.5 (26.2–33.2) | 29.9 (26.6–33.6) | 28.2 (25.0–31.8) | 28.1 (25.1–31.5) | 24.6 (21.7–27.8) | 30.6 (27.4–34.0) | 28.4 (25.5–31.6) | 25.9 (23.0–29.0) | 25.7 (23.0–28.6) | 23.2 (20.7–25.9) | 24.2 (21.8–26.9) | 23.3 (20.8–26.0) | 25.2 (22.9–27.8) | 18.8 (16.7–21.0) | 21.4 (19.3–23.8) | <0.001 |
| ICH CMR | 30.4 (26.9–34.3) | 30.3 (26.7–34.2) | 26.9 (23.6–30.7) | 26.6 (23.3–30.1) | 22.7 (19.7–26.0) | 29.1 (25.8–32.8) | 25.8 (22.8–29.1) | 23.4 (20.5–26.7) | 25.4 (22.5–28.5) | 23.4 (20.6–26.4) | 23.8 (21.2–26.7) | 23.1 (20.4–26.0) | 24.9 (22.3–27.7) | 18.8 (16.5–21.3) | 22.5 (20.1–25.2) | 0.001 |
| ICH ASMR | 30.4 (26.9–34.3) | 30.0 (26.4–33.9) | 27.3 (23.8–31.2) | 26.6 (23.4–30.3) | 23.4 (20.3–26.8) | 29.0 (25.6–32.7) | 26.2 (23.1–29.6) | 23.4 (20.4–26.7) | 25.1 (22.2–28.2) | 22.5 (19.8–25.5) | 23.8 (21.1–26.7) | 22.7 (20.0–25.7) | 24.0 (21.4–26.8) | 17.9 (15.7–20.3) | 21.3 (18.9–23.9) | <0.001 |
| SAH CMR | 20.0 (11.4–32.5) | 30.4 (21.5–41.7) | 35.2 (26.6–45.7) | 36.0 (27.9–45.7) | 32.0 (24.3–41.5) | 37.6 (29.6–47.1) | 40.4 (31.9–50.4) | 36.4 (29.0–45.2) | 29.9 (22.7–38.6) | 27.3 (20.8–35.1) | 28.8 (22.2–36.8) | 26.1 (20.1–33.4) | 31.7 (25.5–38.9) | 23.9 (18.4–30.5) | 24.6 (19.1–31.2) | 0.365 |
| SAH ASMR | 20.0 (11.4–32.4) | 29.3 (20.0–41.5) | 31.6 (22.7–42.6) | 31.7 (23.5–41.5) | 25.7 (18.5–34.6) | 37.1 (28.3–47.5) | 37.8 (28.8–48.5) | 33.0 (25.5–42.0) | 26.3 (19.1–35.1) | 25.5 (18.8–33.6) | 26.0 (19.2–34.2) | 25.9 (19.1–34.1) | 29.6 (23.2–37.3) | 19.6 (14.3–26.0) | 19.4 (14.1–26.0) | 0.182 |
| By ethnicity | ||||||||||||||||
| Chinese CMR | 30.0 (26.3–34.1) | 30.2 (26.5–34.3) | 27.8 (24.3–31.7) | 27.8 (24.4–31.5) | 23.8 (20.6–27.3) | 29.6 (26.2–33.4) | 28.5 (25.2–32.1) | 26.2 (23.1–29.6) | 27.2 (24.1–30.6) | 23.8 (20.9–26.9) | 25.4 (22.6–28.4) | 23.0 (20.3–26.0) | 26.6 (23.8–29.6) | 20.0 (17.6–22.5) | 24.6 (22.0–27.5) | 0.003 |
| Chinese ASMR | 30.0 (26.3–34.1) | 29.8 (26.1–33.9) | 27.9 (24.3–31.9) | 27.6 (24.2–31.3) | 24.1 (20.9–27.7) | 29.8 (26.3–33.7) | 28.7 (25.3–32.4) | 26.3 (23.1–29.8) | 26.8 (23.8–30.2) | 22.6 (19.8–25.6) | 24.7 (21.9–27.7) | 22.6 (19.9–25.5) | 25.7 (23.0–28.6) | 18.9 (16.6–21.4) | 22.7 (20.2–25.4) | 0.001 |
| Malay CMR | 30.7 (21.4–42.7) | 28.0 (19.5–38.9) | 28.6 (20.8–38.4) | 26.6 (19.1–36.1) | 21.2 (14.6–29.7) | 32.9 (24.8–42.9) | 26.9 (20.0–35.4) | 20.8 (14.6–28.8) | 19.6 (13.9–26.9) | 22.8 (16.6–30.6) | 25.7 (19.4–33.5) | 24.8 (18.4–32.6) | 22.2 (16.5–29.2) | 17.5 (12.3–24.1) | 15.6 (11.0–21.4) | 0.002 |
| Malay ASMR | 30.7 (21.4–42.7) | 25.2 (16.8–36.4) | 29.6 (20.2–41.7) | 26.5 (18.1–37.5) | 22.4 (14.8–32.4) | 36.0 (26.4–47.6) | 29.5 (21.3–39.7) | 20.4 (13.8–29.0) | 20.7 (13.4–30.2) | 24.3 (16.7–33.8) | 22.8 (16.4–30.7) | 24.0 (16.9–32.8) | 23.1 (16.6–31.2) | 16.7 (11.0–24.3) | 16.6 (10.7–24.3) | 0.003 |
| Indian CMR | 23.7 (10.8–45.0) | 32.0 (18.3–52.0) | 34.3 (17.7–59.9) | 34.6 (20.5–54.7) | 39.3 (24.6–59.5) | 35.3 (20.9–55.8) | 23.0 (12.5–38.5) | 36.8 (20.1–61.8) | 25.9 (14.5–42.7) | 32.6 (18.3–53.8) | 12.1 (4.9–24.9) | 22.2 (11.5–38.8) | 28.8 (17.3–45.0) | 19.7 (10.2–34.4) | 17.1 (9.1–29.3) | 0.033 |
| Indian ASMR | 23.7 (10.8–44.6) | 26.5 (13.5–46.2) | 41.4 (11.3–95.1) | 39.4 (20.3–67.4) | 26.1 (13.9–46.2) | 27.5 (10.4–55.9) | 21.9 (10.3–39.9) | 29.6 (13.1–56.0) | 18.0 (7.7–35.2) | 21.1 (7.9–44.6) | 12.4 (4.6–26.9) | 16.6 (6.0–35.9) | 25.7 (14.0–42.5) | 16.4 (7.1–31.4) | 19.1 (5.7–42.7) | 0.009 |
| By age group | ||||||||||||||||
| <65 years CMR | 23.1 (19.1–27.8) | 24.4 (20.2–29.3) | 22.4 (18.7–26.7) | 22.5 (18.8–26.8) | 17.6 (14.4–21.3) | 24.9 (21.1–29.2) | 20.9 (17.5–24.7) | 19.6 (16.4–23.3) | 19.9 (16.7–23.6) | 15.3 (12.5–18.6) | 18.3 (15.4–21.6) | 18.4 (15.4–21.7) | 20.3 (17.2–23.7) | 12.2 (9.8–14.9) | 15.1 (12.5–18.2) | 0.001 |
| <65 years ASMR | 23.1 (19.1–27.8) | 24.3 (20.0–29.2) | 21.7 (18.1–26.1) | 22.6 (18.8–26.9) | 17.5 (14.4–21.2) | 25.2 (21.4–29.7) | 20.7 (17.4–24.6) | 19.1 (15.9–22.8) | 19.7 (16.5–23.4) | 15.0 (12.2–18.3) | 18.1 (15.2–21.4) | 18.3 (15.4–21.7) | 19.8 (16.8–23.2) | 12.3 (9.9–15.2) | 14.7 (12.1–17.8) | 0.001 |
| ⩾65 years CMR | 36.5 (31.1–42.4) | 35.7 (30.8–41.3) | 35.4 (30.1–41.3) | 34.4 (29.5–39.8) | 32.5 (27.6–38.0) | 37.5 (32.4–43.2) | 36.8 (31.9–42.2) | 33.5 (28.8–38.8) | 32.4 (28.2–37.2) | 33.3 (29.0–38.1) | 31.5 (27.5–36.0) | 29.5 (25.5–33.9) | 31.5 (27.8–35.6) | 26.4 (23.0–30.1) | 29.4 (25.9–33.2) | <0.001 |
| ⩾65 years ASMR | 36.5 (31.1–42.4) | 36.0 (30.9–41.7) | 35.2 (29.9–41.1) | 34.1 (29.2–39.5) | 32.3 (27.4–37.8) | 36.3 (31.3–41.9) | 36.7 (31.8–42.2) | 33.1 (28.4–38.4) | 32.1 (27.8–36.8) | 31.9 (27.8–36.6) | 30.8 (26.8–35.2) | 28.6 (24.7–33.0) | 31.1 (27.4–35.1) | 25.7 (22.4–29.4) | 28.6 (25.2–32.3) | <0.001 |
| By sex | ||||||||||||||||
| Male CMR | 26.2 (22.0–31.1) | 26.4 (22.2–31.1) | 28.2 (23.9–33.1) | 25.9 (22.1–30.3) | 23.9 (20.1–28.1) | 31.9 (27.6–36.6) | 26.7 (22.9–30.9) | 26.1 (22.4–30.3) | 24.6 (21.1–28.5) | 21.6 (18.4–25.3) | 22.6 (19.5–26.2) | 23.3 (20.0–26.9) | 25.1 (21.8–28.7) | 19.0 (16.2–22.1) | 21.2 (18.3–24.5) | 0.004 |
| Male ASMR | 26.2 (22.0–31.1) | 25.4 (21.3–30.2) | 28.9 (24.2–34.2) | 25.1 (21.3–29.5) | 24.3 (20.5–28.7) | 31.3 (27.0–36.1) | 26.8 (22.9–31.2) | 26.0 (22.1–30.6) | 24.6 (21.0–28.6) | 20.7 (17.4–24.4) | 22.2 (19.1–25.8) | 22.4 (19.2–26.0) | 24.7 (21.4–28.5) | 18.3 (15.6–21.4) | 19.8 (17.0–22.9) | 0.003 |
| Female CMR | 33.3 (28.1–39.0) | 34.8 (29.6–40.6) | 28.3 (23.7–33.5) | 30.9 (26.2–36.3) | 24.7 (20.4–29.6) | 29.2 (24.6–34.3) | 29.9 (25.5–34.9) | 25.6 (21.5–30.2) | 27.8 (23.7–32.4) | 26.9 (22.9–31.4) | 27.1 (23.2–31.4) | 24.0 (20.3–28.2) | 27.2 (23.7–31.2) | 20.5 (17.3–24.1) | 24.8 (21.4–28.7) | 0.001 |
| Female ASMR | 33.3 (28.1–39.0) | 35.2 (29.8–41.3) | 28.0 (23.4–33.2) | 30.7 (25.9–36.1) | 25.2 (20.7–30.3) | 29.4 (24.7–34.6) | 30.6 (26.0–35.8) | 25.7 (21.5–30.5) | 27.5 (23.4–32.1) | 25.7 (21.8–30.0) | 26.0 (22.1–30.3) | 23.7 (19.9–27.9) | 26.4 (22.9–30.4) | 19.2 (16.1–22.7) | 23.0 (19.7–26.6) | <0.001 |
HS: hemorrhagic stroke; ICH: intracerebral hemorrhage; SAH: subarachnoid hemorrhage; CMR: crude mortality rate; ASMR: age-standardized mortality rate; CI: confidence interval.
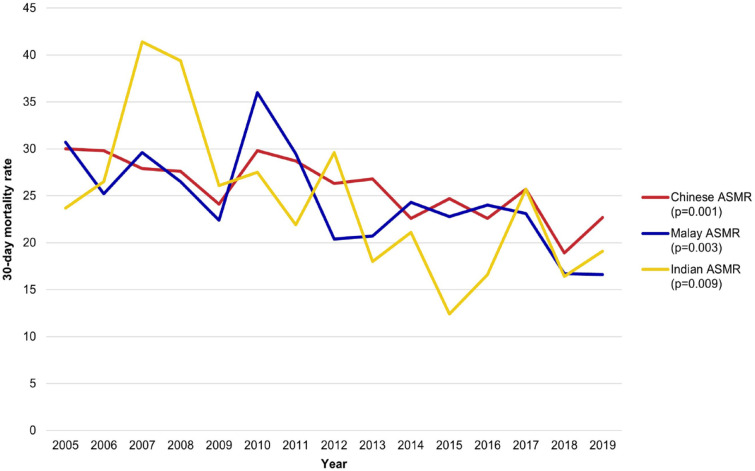
Figure 4 shows the trends in yearly CMR and ASMR for HS stratified by ethnicity. All ethnicities had a decrease in CMR and ASMR from 2005 to 2019 (all p < 0.04) (Table 3).
Figure 4.
Age-standardized mortality rates (ASMR) of hemorrhagic stroke by ethnicity. p-values for trend are indicated.
When stratified by age group (<65 years vs ⩾65 years), CMR and ASMR of both groups decreased from 2005 to 2019 (all p ⩽ 0.001). When stratified by sex, CMR and ASMR of both males and females decreased from 2005 to 2019 (all p < 0.005) (Table 3; Supplemental Figure S2).
Discussion
In a national multi-ethnic urban Asian population of 19,017 cases of HS aged ⩾15 years between 2005 and 2019, we showed that CIR of HS increased by approximately 39.1% while ASIR remained stable, and both CMR and ASMR decreased by approximately 22.4% and 27.5% respectively. Singapore is a developed country and these trends were largely consistent with recently reported global and Asian trends in HS incidence and mortality.1,8–15
We hypothesize that the increase in CIR of HS with stable ASIR was due to the aging population in Singapore. The median age of the Singapore resident population rose from 35.8 years in 2005 to 42.0 years in 2019, and the proportion of older adults was increasing rapidly. 17 Incidence of HS increased sharply with age, 24 and was therefore expected to increase as the population aged. Hence, preventive measures targeting modifiable risk factors of HS would be an essential component of contemporary public health strategies to reduce the incidence of HS.
ASMR decreased from 2005 to 2019 in all subgroup analyses. We hypothesize that these trends of decreasing ASMR reflect improvements in the overall management of HS from 2005 to 2019, and were consistent with recently reported global trends. 1 In particular, in the last decade, a substantial decrease of stroke incidence, mortality, and DALYs has been achieved in high-income countries, most likely due to improvements in primary and secondary prevention, acute stroke treatment, and neurorehabilitation. 25 In Singapore, evidence-based clinical practice guidelines have been rigorously formulated to address the assessment, investigations, immediate management, secondary prevention, and rehabilitation for stroke, 26 contributing to improved service delivery and patient care.
ASIR of ICH remained stable from 2005 to 2019, while ASMR of ICH decreased significantly by approximately 30.0%. Conversely, although ASIR of SAH increased by approximately 122.2%, ASMR of SAH remained stable. The 2021 Global Burden of Disease study showed decreasing incidence and mortality rates of both subtypes of HS worldwide. 1 In our population, the decrease in ICH mortality parallels overall HS and global trends, and was likely a reflection of advances in stroke treatment and prevention. The reasons for an increase in SAH incidence were less clear, although this trend coincided with pooled data from high-income Asia Pacific countries (which include Singapore, Japan, Korea, etc.), which showed that ASIR of SAH rose by 40.2% from 1990 to 2019. 1 Other country-specific studies, such as from the United States, reported similar results. 27 Improved case detection may also have contributed to the apparent increase in SAH incidence. SAH mortality remained stable, and further research to improve treatment outcomes for SAH may be warranted.28,29 It has been suggested that premature withholding or withdrawal of support without offering a trial of aggressive early resuscitation may be a potent determinant of mortality after SAH. 30 Lantigua et al. advocated for an initial trial of full support, including aneurysm treatment and ventriculostomy, to be offered to all eligible poor-grade SAH patients if consistent with their wishes. 28
In subgroup analyses, we showed that ASIR of those aged <65 years increased significantly by 8.3% from 2005 to 2019 compared to those aged ⩾65 years. Increases in ASIR amongst those aged <65 years reflect an increasing incidence of patients with young stroke, especially those with SAH. This corresponds with recent data from Western countries.31,32 Several hypotheses have been postulated for the rising incidence of stroke among the younger age group, including the increase in modifiable risk factors especially hypertension among younger and middle-aged adults, and/or suboptimal control of these risk factors in this age group. Two large-scale studies in Singapore found that younger individuals with hypertension were more likely to be unaware of their diagnosis, with higher likelihood of untreated hypertension.33,34 This could contribute to the risk of HS in the younger demographic. This bears important implications for public health, as the burden of HS among younger and middle-aged adults translates to longer-lasting disability, increased healthcare costs, and potential loss of economic productivity.
Our study also reported on the inter-ethnic differences in HS trends, with an increased ASIR from 2005 to 2019 in Malays, but increased risk for mortality in Indians after adjusting for other demographic factors. We hypothesize that these trends in stroke could be due to adverse trends in risk factors such as hypertension, diabetes mellitus, and smoking among the Malay and Indian population in Singapore, as supported by recently published population health data, which consistently reported higher rates of hypertension and diabetes in Malays and Indians compared to the Chinese.35–37 Specifically, from 2007 to 2019, the Malay ethnic group in Singapore showed the greatest increase in the prevalence of both hypertension and diabetes among the three ethnic groups. 35 The prevalence of smoking also remained high with no decline in Malays at 23.0% from 2007 to 2019, as opposed to a decrease in both Chinese (from 12.0% in 2007 to 8.6% in 2019) and Indians (from 11.1% in 2007 to 10.9% in 2019). 35 These trends warrant further investigation of stroke risk factors in these ethnic groups in Singapore.
Our study had several strengths. The SSR captured nationwide data of all stroke cases admitted to public hospitals in Singapore, where most stroke patients (approximately 95%) were managed. Furthermore, the source of mortality data in the SSR was the national death registry, which recorded all deaths in Singapore. Such national registries ensured recording of high-quality epidemiologic data, with a large and comprehensive sample comprising nearly the entirety of the population. Rigorous methodology was also applied, with standardized definitions and case report forms used, supported by thorough quality assurance procedures. To our knowledge, this was the first study to demonstrate trends over more than 10 years in HS incidence and mortality in a multi-ethnic Asian population with comparisons across ethnic groups. However, patients treated in private hospitals, non-tertiary hospitals, or outpatient clinics were not included in this study, although this constituted a very small proportion of the national caseload of HS patients. Lastly, though the stroke registry captures clinical data beyond baseline demographics and stroke subtypes, data completeness was low and hence we were unable to account for other clinical confounders of mortality in our study.
In conclusion, in a highly urbanized multi-ethnic Asian population, we showed that from 2005 to 2019, there was a stable ASIR and decreasing ASMR of HS. ICH had stable ASIR and significant decrease in ASMR, while SAH showed significant increase in ASIR with stable ASMR from 2005 to 2019. In subgroup analyses, we showed an increased incidence of HS in younger adults and those of Malay ethnicity. Overall, targeting modifiable risk factors of HS such as hypertension, metabolic syndrome, and smoking in specific demographic subgroups may be warranted to overcome population disparities and reduce the future burden of HS both in Singapore and internationally.
Supplemental Material
Supplemental material, sj-docx-1-eso-10.1177_23969873231202392 for Trends in hemorrhagic stroke incidence and mortality in a National Stroke Registry of a multi-ethnic Asian population by Mervyn Jun Rui Lim, Huili Zheng, Zheting Zhang, Ching Hui Sia, Benjamin Yong-Qiang Tan, Marcus Eng Hock Ong, Vincent Diong Weng Nga, Tseng Tsai Yeo and Andrew Fu Wah Ho in European Stroke Journal
Supplemental material, sj-docx-2-eso-10.1177_23969873231202392 for Trends in hemorrhagic stroke incidence and mortality in a National Stroke Registry of a multi-ethnic Asian population by Mervyn Jun Rui Lim, Huili Zheng, Zheting Zhang, Ching Hui Sia, Benjamin Yong-Qiang Tan, Marcus Eng Hock Ong, Vincent Diong Weng Nga, Tseng Tsai Yeo and Andrew Fu Wah Ho in European Stroke Journal
Acknowledgments
None.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the Centralised Institutional Review Board (CIRB Ref: 2017/2380).
Informed consent: A waiver of patient consent was granted for this study as it involved minimal risks to subjects.
Guarantor: MJRL
Contributorship: MJRL designed the study, performed data analysis and the main writing of the manuscript. HZ performed data analysis and contributed to the writing of the manuscript. ZZ, CHS, BYQT, MEHO, VDWN, and TTY contributed to the writing of the manuscript. AFWH contributed to the study design and the writing of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
ORCID iD: Zheting Zhang  https://orcid.org/0009-0004-0797-8439
https://orcid.org/0009-0004-0797-8439
Supplemental material: Supplemental material for this article is available online.
References
- 1. Feigin VL, Stark BA, Johnson CO. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021; 20: 795–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Caplan LR. Caplan's stroke: a clinical approach. Cambridge: Cambridge University Press, 2016. [Google Scholar]
- 3. Venketasubramanian N, Yoon BW, Pandian J, et al. Stroke epidemiology in South, East, and South-East Asia: a review. J Stroke 2017; 19: 286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van Asch CJ, Luitse MJ, Rinkel GJ, et al. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 2010; 9: 167–176. [DOI] [PubMed] [Google Scholar]
- 5. Shen AY, Yao JF, Brar SS, et al. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol 2007; 50: 309–315. [DOI] [PubMed] [Google Scholar]
- 6. Khan NA, McAlister FA, Pilote L, et al. Temporal trends in stroke incidence in South Asian, Chinese and white patients: a population based analysis. PLoS One 2017; 12: e0175556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bako AT, Pan AP, Potter T, et al. Demographic characteristics and clinical outcomes of Asian American and Pacific Islander patients with primary intracerebral hemorrhage. JAMA Netw Open 2021; 4: e2138786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li J, Imano H, Kitamura A, et al. Trends in the incidence of stroke and its subtypes from 1963 to 2018 in Japanese urban and rural communities: the Circulatory Risk in Communities Study (CIRCS). Int J Stroke 2023; 18: 657–662. [DOI] [PubMed] [Google Scholar]
- 9. Sun T, Chen S, Wu K, et al. Trends in incidence and mortality of stroke in China from 1990 to 2019. Front Neurol 2021; 12: 759221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tsai CF, Wang YH, Teng NC, et al. Incidence, subtypes, sex differences and trends of stroke in Taiwan. PLoS One 2022; 17: e0277296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim JY, Kang K, Kang J, et al. Executive Summary of Stroke Statistics in Korea 2018: a report from the Epidemiology Research Council of the Korean Stroke Society. J Stroke 2019; 21: 42–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hwong WY, Ang SH, Bots ML, et al. Trends of stroke incidence and 28-day all-cause mortality after a stroke in Malaysia: a linkage of national data sources. Glob Heart 2021; 16: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hata J, Ninomiya T, Hirakawa Y, et al. Secular trends in cardiovascular disease and its risk factors in Japanese: half-century data from the Hisayama Study (1961-2009). Circulation 2013; 128: 1198–1205. [DOI] [PubMed] [Google Scholar]
- 14. Cho KC, Kim H, Suh SH. Trends in mortality from hemorrhagic stroke in Korea from 2012 to 2020. Neurointervention 2022; 17: 87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li B, Lou Y, Gu H, et al. Trends in incidence of stroke and transition of stroke subtypes in rural Tianjin China: a population-based study from 1992 to 2012. PLoS One 2015; 10: e0139461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tan CS, Müller-Riemenschneider F, Ng SHX, et al. Trends in stroke incidence and 28-day case Fatality in a nationwide stroke registry of a multiethnic Asian population. Stroke 2015; 46: 2728–2734. [DOI] [PubMed] [Google Scholar]
- 17. Singapore Department of Statistics. Population and population structure, https://www.singstat.gov.sg/find-data/search-by-theme/population/population-and-population-structure/latest-data (2023, accessed May 23, 2023).
- 18. Venketasubramanian N. Stroke care services in Singapore during COVID-19 pandemic - a national perspective. Front Neurol 2020; 11: 780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Venketasubramanian N, Chang HM, Chan BPL, et al. Countrywide stroke incidence, subtypes, management and outcome in a multiethnic Asian population: the Singapore Stroke Registry—methodology. Int J Stroke 2015; 10: 767–769. [DOI] [PubMed] [Google Scholar]
- 20. Parliament of Singapore. Registration of births and deaths act. Singapore: Singapore Statutes, 2021. [Google Scholar]
- 21. World Health Organization. Cause of death, https://www.who.int/standards/classifications/classification-of-diseases/cause-of-death (2023, accessed August 19, 2023).
- 22. World Health Organization. World (WHO 2000-2025) standard, https://seer.cancer.gov/stdpopulations/world.who.html (2013, accessed June 16, 2023).
- 23. Singapore Department of Statistics. Population in Brief 2019. Singapore: Singapore Department of Statistics, 2019. [Google Scholar]
- 24. Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke 2022; 53: e282–e361. [DOI] [PubMed] [Google Scholar]
- 25. Katan M, Luft A. Global burden of stroke. Semin Neurol 2018; 38: 208–211. [DOI] [PubMed] [Google Scholar]
- 26. Venketasubramanian N, Pwee KH, Chen CP. Singapore ministry of health clinical practice guidelines on stroke and transient ischemic attacks. Int J Stroke 2011; 6: 251–258. [DOI] [PubMed] [Google Scholar]
- 27. Xia C, Hoffman H, Anikpezie N, et al. Trends in the incidence of spontaneous subarachnoid hemorrhages in the United States, 2007-2017. Neurology 2023; 100: e123–e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lantigua H, Ortega-Gutierrez S, Schmidt JM, et al. Subarachnoid hemorrhage: who dies, and why? Crit Care 2015; 19: 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Komotar RJ, Schmidt JM, Starke RM, et al. Resuscitation and critical care of poor-grade subarachnoid hemorrhage. Neurosurg 2009; 64: 397–410. [DOI] [PubMed] [Google Scholar]
- 30. Kowalski RG, Chang TR, Carhuapoma JR, et al. Withdrawal of technological life support following subarachnoid hemorrhage. Neurocrit Care 2013; 19: 269–275. [DOI] [PubMed] [Google Scholar]
- 31. Bako AT, Pan A, Potter T, et al. Contemporary trends in the nationwide incidence of primary intracerebral hemorrhage. Stroke 2022; 53: e70–e74. [DOI] [PubMed] [Google Scholar]
- 32. Li L, Scott CA, Rothwell PM. Association of younger vs older ages with changes in incidence of stroke and other vascular events, 2002-2018. JAMA 2022; 328: 563–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wu Y, Tai ES, Heng D, et al. Risk factors associated with hypertension awareness, treatment, and control in a multi-ethnic Asian population. J Hypertens 2009; 27: 190–197. [DOI] [PubMed] [Google Scholar]
- 34. Liew SJ, Lee JT, Tan CS, et al. Sociodemographic factors in relation to hypertension prevalence, awareness, treatment and control in a multi-ethnic Asian population: a cross-sectional study. BMJ Open 2019; 9: e025869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Epidemiology & Disease Control Division and Policy, Research & Surveillance Group Ministry of Health and Health Promotion Board. National Population Health Survey 2021. Singapore: Epidemiology & Disease Control Division and Policy, Research & Surveillance Group Ministry of Health and Health Promotion Board, 2021. [Google Scholar]
- 36. Porhcisaliyan VD, Wang Y, Tan NC, et al. Socioeconomic status and ethnic variation associated with type 2 diabetes mellitus in patients with uncontrolled hypertension in Singapore. BMJ Open Diabetes Res Care 2021; 9: e002064. DOI: 10.1136/bmjdrc-2020-002064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tan KHX, Tan LWL, Sim X, et al. Cohort profile: the Singapore multi-ethnic cohort (MEC) study. Int J Epidemiol 2018; 47: 699–699. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-eso-10.1177_23969873231202392 for Trends in hemorrhagic stroke incidence and mortality in a National Stroke Registry of a multi-ethnic Asian population by Mervyn Jun Rui Lim, Huili Zheng, Zheting Zhang, Ching Hui Sia, Benjamin Yong-Qiang Tan, Marcus Eng Hock Ong, Vincent Diong Weng Nga, Tseng Tsai Yeo and Andrew Fu Wah Ho in European Stroke Journal
Supplemental material, sj-docx-2-eso-10.1177_23969873231202392 for Trends in hemorrhagic stroke incidence and mortality in a National Stroke Registry of a multi-ethnic Asian population by Mervyn Jun Rui Lim, Huili Zheng, Zheting Zhang, Ching Hui Sia, Benjamin Yong-Qiang Tan, Marcus Eng Hock Ong, Vincent Diong Weng Nga, Tseng Tsai Yeo and Andrew Fu Wah Ho in European Stroke Journal