Abstract
BACKGROUND
Chondrosarcoma is an uncommon spinal tumor that can present as an extraskeletal mass. Rarely, these tumors present as dumbbell tumors through the neural foramina, mimicking schwannomas or neurofibromas.
OBSERVATIONS
A 46-year-old female presented with 2 years of worsening right-arm radiculopathy. Magnetic resonance imaging of the thoracic spine revealed a peripherally enhancing extramedullary mass through the right T1 foramen and compressing the spinal cord. Computed tomography showed the mass to be partially calcified. She underwent C7–T2 laminectomy and C6–T3 posterior instrumented fusion with gross-total resection of an extradural mass. Pathology revealed a grade I chondrosarcoma. Her symptoms improved postoperatively, with some residual right-arm radicular pain.
LESSONS
Intraspinal extradural dumbbell conventional chondrosarcoma is rare, with only 9 cases, including ours, reported. Patient ages range from 16 to 72 years old, and male sex is more common in these cases. The most common location is the thoracic spine, and our case is the only reported one in the cervicothoracic junction. These tumors often mimic schwannomas on imaging, but chondrosarcoma should remain in the differential diagnosis, because management of these tumors differs. Chondrosarcoma may benefit from more aggressive resection, including en bloc resection, and may require adjuvant radiotherapy.
KEYWORDS: intraspinal, spinal tumor, extradural, chondrosarcoma, cervicothoracic junction, schwannoma, case report
ABBREVIATION: MRI = magnetic resonance imaging
Chondrosarcoma is a rare malignant tumor of bone that forms cartilage.1,2 The incidence of chondrosarcoma is only 3 cases per 1 million persons per year,3 and these tumors arise from the spine in 2%–12% of cases.4 An extraskeletal soft tissue origin is possible, and these lesions can present as an intraspinal mass.5 Chondrosarcomas can be histologically classified into conventional, clear cell, mesenchymal, or dedifferentiated, with a variable prognosis depending on lesion subtype.1,4 Many reported cases of intraspinal chondrosarcoma have been of the mesenchymal subtype.5,6 We present the case of an extradural dumbbell-shaped conventional chondrosarcoma at the cervicothoracic junction causing spinal cord compression, and we review the current literature on intraspinal dumbbell chondrosarcoma.
Illustrative Case
A 46-year-old female with a past medical history of anxiety and depression presented to a neurosurgeon with a 2-year history of right-arm pain, numbness, and subjective weakness that was progressively worsening. The pain and numbness were worse in the medial arm in a classic T1 dermatome and were beginning to spread to her left arm. On physical examination, she had trace intrinsic hand weakness on the right but otherwise had full strength with no abnormal objective sensation and normal reflexes throughout.
She had an extensive work-up, including electromyography testing, which was remarkable for right C5 radiculopathy, and magnetic resonance imaging (MRI) of the cervical and thoracic spine as well as the right arm. The MRI of her thoracic spine with and without contrast revealed a heterogeneous, peripherally enhancing extramedullary mass on the right side of the spinal canal and extending into and expanding the right T1 foramen (Fig. 1). Computed tomography of the chest revealed this mass to be partially calcified (Fig. 2). The mass was believed most likely to be a schwannoma or neurofibroma on the basis of imaging characteristics. MRI of the right humerus also revealed a 3.7 × 2.4 × 2.1–cm mass lesion that was believed to be a benign hemangioma or lymph venous malformation. She was monitored while on pain management for her chronic arm pain, and she had a cervical epidural steroid injection, which relieved her symptoms for 1 day.
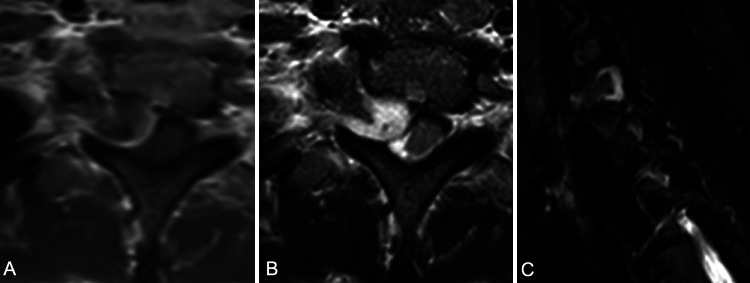
FIG. 1.
Axial T1-weighted postcontrast (A) and T2-weighted (B) MRI of the thoracic spine revealing a peripherally enhancing dumbbell tumor displacing the spinal cord and extending through the right T1 neural foramen anteriorly and laterally, causing scalloping of the surrounding bony structures. Sagittal short tau inversion recovery image (C) shows the ventral extent of the tumor and the right T1 foramen expanded by the tumor.
FIG. 2.

Axial computed tomography of the chest without contrast, revealing calcification of the mass centrally (black arrow) exiting the right T1 neural foramen.
Because of her intractable pain and spinal cord compression, she was offered surgery. She underwent a C7–T2 laminectomy for tumor resection and C6–T3 posterior instrumented fusion. Intraoperatively, the mass was found to be extradural, and gross-total resection was achieved. The tumor itself was white, scaly/partially calcified, and nonvascular. Surgery went well without any complications, and estimated blood loss was 80 mL. There were no neuromonitoring changes. Postoperatively, she was neurologically intact on examination, but at the 2-month follow-up, she continued to have subjective pain and weakness of the right arm. Postoperative MRI at 2 months showed gross-total resection and resolution of the spinal cord compression (Fig. 3). Her incision healed appropriately. Pathology revealed a conventional grade I chondrosarcoma. Low-power histological examination revealed abnormal cartilage tissue with increased cellularity (Fig. 4A), and a higher-power view showed abnormal nuclei with increased mitosis (Fig. 4B and C). She was referred to oncology for further work-up and management of the chondrosarcoma; given the low-grade tumor with gross-total resection, she was offered close surveillance instead of adjuvant chemotherapy or radiotherapy.
FIG. 3.

Postoperative axial postcontrast T1-weighted MRI of the thoracic spine showing gross-total resection of the mass, a fully decompressed spinal cord, and the hemilaminectomy and facetectomy required for the tumor resection.
FIG. 4.

Histological slides of the grade I chondrosarcoma. At low power (A), there was abnormal cartilaginous tissue with increased cellularity. Higher power (B and C) revealed abnormal nuclei and binucleated cells with increased mitosis. Hematoxylin and eosin, original magnification ×10 (A), ×40 (B and C).
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
Intraspinal chondrosarcoma is a rare spine tumor, especially when arising from the meninges instead of the bone, although chondrosarcoma can present as a paraspinal mass with calcification.7 Much of the literature on intraspinal chondrosarcoma is limited to case reports.5,6,8
Obuchowicz et al.5 described a case of a 14-year-old boy with a large intraspinal tumor at the C1–2 level, which was thought to be a hemangiopericytoma after initial biopsy and was first treated with chemotherapy and radiotherapy. After disease progression about 14 months after initial treatment, the patient was taken for resection of the tumor, which was then diagnosed as mesenchymal chondrosarcoma and again treated with chemotherapy and radiation therapy. Their literature review revealed 24 cases of intraspinal mesenchymal chondrosarcoma in patients 21 years or younger, and 40% of the cases were located in the thoracic spine and only 1 case was in the cervicothoracic junction.5
Chen et al.6 reported a case of a dumbbell-shaped intraspinal mesenchymal chondrosarcoma in a 26-year-old female. As in our case, the initial differential diagnosis favored a classic intradural extramedullary tumor such as schwannoma or meningioma. Their patient was treated with resection and, after 5 months, experienced a recurrence requiring reoperation followed by radiotherapy. They found 6 prior reported cases of dumbbell-shaped intraspinal mesenchymal chondrosarcomas, all arising from the thoracic or lumbar spine. Four of the 7 cases in their report and literature review were exclusively extradural.6 In 2022, Chen and Lai9 reported on another dumbbell intradural and extradural mesenchymal chondrosarcoma tumor from T12 to L2 in a 19-year-old male, who was treated with excision alone.
A more recent case report and literature review from 2020 described a 17-year-old male with a T10–11 intradural extramedullary mesenchymal chondrosarcoma.10 He was treated with initial resection, followed by a second surgery for wide excision of surrounding tissues after the diagnosis of mesenchymal chondrosarcoma was made. He then received adjuvant radiotherapy and chemotherapy. These authors reported on 20 prior case reports of intradural extramedullary mesenchymal chondrosarcomas, none of which were located in the cervicothoracic junction, although some were noted to be in multiple locations.10
Myxoid chondrosarcoma has also been described as occurring intraspinally in the literature.11,12 Ricci et al.11 reported on a 55-year-old male with a dumbbell tumor at T5–7 that was resected via a T5–7 laminectomy and a separate thoracotomy; the tumor was found to be an extradural myxoid chondrosarcoma. Rao et al.12 more recently described a case of a 29-year-old male with T4–5 lesion causing back pain and lower-extremity numbness. He was taken for a T4–5 laminectomy, and the tumor was found to be extradural and densely adherent to the dura. The initial diagnosis was meningioma, but the lesion was later confirmed as a myxoid chondrosarcoma. The patient did not receive any adjuvant therapy and was asymptomatic 12 months after surgery.12
Reports of intraspinal well-differentiated chondrosarcoma are less common than mesenchymal chondrosarcoma. Moghamis et al.13 reported on a 40-year-old male with an L5 extradural lesion that was found to be a grade 1 chondrosarcoma arising from osteochondroma. The patient underwent hemilaminectomy with complete resection and a one-level instrumented fusion; he remained free of recurrence and symptoms at 3 years. He did not require chemotherapy or radiation.
A case series by Kilic et al.14 described 3 posterior mediastinal tumors with dumbbell extension into the lower thoracic spine, 2 of which were chondrosarcoma. A 32-year-old male had a grade II chondrosarcoma resected via an anterior approach and afterward was treated with radiotherapy. These authors also treated a 31-year-old male with a grade I chondrosarcoma via a laminectomy followed by a second-stage thoracotomy and radiotherapy.14 Dernevik and Larsson15 similarly reported on their series of dumbbell tumors, one of which included a chondrosarcoma in a 20-year-old male at T5–6. In their case, as in ours, the tumor was preoperatively thought to be a schwannoma and during laminectomy was found to be entirely extradural. The patient also had second-stage thoracotomy and radiotherapy postoperatively. One year after the initial operation, he developed tumor recurrence requiring reoperation, and he died after 16 months.15 In 1996, McCormick16 published his series of 12 dumbbell thoracic and lumbar spine tumors requiring a lateral extracavitary approach, one of which was a chondrosarcoma. The patient in that case was a 72-year-old male with a T8 tumor, which was resected en bloc via the lateral extracavitary approach. He received no adjuvant treatment and was found to have a local recurrence at 24 months.16
Ciappetta et al.17 encountered a 16-year-old girl with a large chondrosarcoma from the right chest wall entering the spine from T7 to T9. She underwent a thoracotomy followed by a T6–10 laminectomy, revealing an entirely extradural tumor that could be fully resected. She had some symptomatic improvement 1 week later on discharge and did not receive adjuvant therapy.17 Zibis et al.18 reported on a series of unusual pathologies causing neural foraminal widening, including one chondrosarcoma. The patient was a 41-year-old female with a dumbbell tumor through the right C6–7 neural foramen, which was found to be a high-grade chondrosarcoma. She had a tumor recurrence shortly after resection. Another report by Yünten et al.19 described an 18-year-old male with a large dumbbell mass through the left C5–6 foramen. He underwent resection, and pathology confirmed a low-grade chondrosarcoma. Table 1 summarizes the 9 existing cases of extradural dumbbell conventional chondrosarcoma, including our case. The majority (66.7%) were in the thoracic spine, including our case, which is the only case in the cervicothoracic junction. Cervical (22.2%) and lumbar (11.1%) locations were less common. There is a male predominance, with two-thirds of cases arising in males. The age range is 16–72 years, with most arising in middle age, which mimics the demographics of chondrosarcoma overall. Instrumented fusion was performed in only 2 cases, including our own. The decision to instrument depends on tumor location, bony erosion/destruction, the amount of bone removed during surgery, and signs of instability. Metallic implants cause artifacts on MRI, which can interfere with surveillance imaging postoperatively. In our case, the junctional level and amount of facet needed to be taken necessitated instrumented fusion. The right T1 and T2 screws were left out of the construct, and a minimal resection cavity artifact was seen on MRI (Fig. 3).
TABLE 1.
Literature summary of extradural dumbbell conventional chondrosarcoma cases
| Case No. | Authors & Year | Age (yrs) | Sex | Tumor Location | Surgical Approach | Treatment | Length of FU (mos) | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 |
Present case |
41 |
F |
T1 |
Laminectomy & instrumented fusion |
GTR |
2 |
Symptomatic improvement, no recurrence |
| 2 |
Moghamis et al., 202213 |
37 |
M |
L5 |
Hemilaminectomy & instrumented fusion |
STR |
36 |
Symptomatic resolution, no progression |
| 3 |
Kilic et al., 200614 |
32 |
M |
T8–9 |
Pediculotomy, pst thoracotomy |
STR, RT |
11 |
No recurrence |
| 4 |
Kilic et al., 200614 |
31 |
M |
T10–12 |
Laminectomy, pst thoracotomy |
STR, RT |
18 |
No recurrence |
| 5 |
Dernevik & Larsson, 199015 |
20 |
M |
T5–6 |
Laminectomy, thoracotomy |
STR, RT |
16 |
Deceased, reop for recurrence |
| 6 |
McCormick, 199616 |
72 |
M |
T8 |
Lat extracavitary approach |
GTR |
37 |
Local recurrence at 24 mos |
| 7 |
Ciappetta et al., 198217 |
16 |
F |
T7–9 |
Laminectomy, posterolat thoracotomy |
GTR |
10 days |
Symptomatic improvement |
| 8 |
Zibis et al., 200018 |
41 |
F |
C6–7 |
NA |
NA |
NA |
Tumor recurrence |
| 9 | Yünten et al., 199719 | 18 | M | C5–6 | NA | GTR | NA | NA |
FU = follow-up; GTR= gross-total resection; NA = not available; pst = posterior; RT = radiotherapy; STR = subtotal resection.
Lessons
Intraspinal extradural dumbbell chondrosarcoma, although rare, should be included in the differential diagnosis for dumbbell tumors of the spine. Chondrosarcoma should be considered especially when there are atypical radiographic features, including focal calcification, abnormal enhancement pattern, or evidence of tumor arising from the vertebrae. Treatment options are different from those for benign lesions such as schwannoma or meningioma, because a wide resection with margins is often recommended in chondrosarcoma when possible, and adjuvant radiotherapy can be advised. When chondrosarcoma is in the preoperative differential diagnosis, the surgeon may consider planning for en bloc resection when feasible. If the preoperative radiographic diagnosis is questionable and en bloc or aggressive resection would greatly alter the surgical plan, preoperative biopsy can be entertained, although this would require a safe and feasible biopsy target and carries with it the risk of tumor seeding.20 Tumors with significant anterior extension may require costotransversectomy or a lateral extracavitary approach. Thoracic or oncological surgeons are needed if thoracotomy or a transthoracic approach is used for aggressive resection. The decision whether to perform an instrumented fusion depends on the goals of surgery and whether there is any instability, but metallic instrumentation can introduce an MRI artifact, which can interfere with surveillance imaging or adjuvant radiotherapy. Most reported cases of intraspinal dumbbell chondrosarcoma are of the mesenchymal subtype, but conventional chondrosarcoma or the myxoid subtype is also noted to occur. Prognosis varies between these subtypes and depends on tumor grading.
Author Contributions
Conception and design: Houten. Acquisition of data: Carr, Pain, Kay. Analysis and interpretation of data: Carr, Pain. Drafting the article: Houten, Carr. Critically revising the article: Carr. Reviewed submitted version of manuscript: Carr, Pain. Approved the final version of the manuscript on behalf of all authors: Houten. Administrative/technical/material support: Pain, Kay. Study supervision: Houten.
References
- 1. McLoughlin GS, Sciubba DM, Wolinsky JP. Chondroma/chondrosarcoma of the spine. Neurosurg Clin N Am. 2008;19(1):57–63. doi: 10.1016/j.nec.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 2. Chow WA. Update on chondrosarcomas. Curr Opin Oncol. 2007;19(4):371–376. doi: 10.1097/CCO.0b013e32812143d9. [DOI] [PubMed] [Google Scholar]
- 3. Chow WA. Chondrosarcoma: biology, genetics, and epigenetics. F1000Res. 2018;7:F1000 Faculty Rev-1826. [Google Scholar]
- 4. Katonis P, Alpantaki K, Michail K, et al. Spinal chondrosarcoma: a review. Sarcoma. 2011;2011:378957. doi: 10.1155/2011/378957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Obuchowicz AK, Szumera-Ciećkiewicz A, Ptaszyński K, et al. Intraspinal mesenchymal chondrosarcoma in a 14-year-old patient: diagnostic and therapeutic problems in relation to the review of literature. J Pediatr Hematol Oncol. 2012;34(5):e188–e192. doi: 10.1097/MPH.0b013e318257a421. [DOI] [PubMed] [Google Scholar]
- 6. Chen S, Wang Y, Su G, Chen B, Lin D. Primary intraspinal dumbbell-shaped mesenchymal chondrosarcoma with massive calcifications: a case report and review of the literature. World J Surg Oncol. 2016;14(1):203. doi: 10.1186/s12957-016-0963-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sundaresan N, Rosen G, Boriani S. Primary malignant tumors of the spine. Orthop Clin North Am. 2009;40(1):21–36, v. doi: 10.1016/j.ocl.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 8. Bae GS, Choi SW, Youm JY, Kim SH. Primary spinal dumbbell-shaped mesenchymal chondrosarcoma located intradurally and extradurally. J Korean Neurosurg Soc. 2011;50(5):468–471. doi: 10.3340/jkns.2011.50.5.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen M, Lai Q. Primary intra- and extradural extramedullary mesenchymal chondrosarcoma with isolated punctate calcification: case report and literature review. BMC Neurol. 2022;22(1):112. doi: 10.1186/s12883-022-02645-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gopakumar S, Steele WJ, Muir M, Bhogani Z, Britz G. Intraspinal mesenchymal chondrosarcoma: an argument for aggressive local resection and adjuvant therapy based on review of the literature. Surg Neurol Int. 2020;11:95. doi: 10.25259/SNI_130_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ricci C, Rendina EA, Venuta F, Pescarmona EO, Gagliardi F. Diagnostic imaging and surgical treatment of dumbbell tumors of the mediastinum. Ann Thorac Surg. 1990;50(4):586–589. doi: 10.1016/0003-4975(90)90194-b. [DOI] [PubMed] [Google Scholar]
- 12. Rao P, Colen RR, Bruner JM, Meis JM. Extraskeletal myxoid chondrosarcoma presenting as an intradural spinal mass: report of a rare clinical presentation with an emphasis on differential diagnostic considerations. Rare Tumors. 2014;6(4):5586. doi: 10.4081/rt.2014.5586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moghamis IS, Alamlih MI, Alhardallo MA, Al Hyassat S, Abdelsalam S, Baco A. Rare presentation of intra-spinal extradural grade 1 chondrosarcoma: a case report. Int J Surg Case Rep. 2022;94:106985. doi: 10.1016/j.ijscr.2022.106985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kilic D, Erdogan B, Sener L, Sahin E, Caner H, Hatipoglu A. Unusual dumbbell tumours of the mediastinum and thoracic spine. J Clin Neurosci. 2006;13(9):958–962. doi: 10.1016/j.jocn.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 15. Dernevik L, Larsson S. Management of dumbbell tumours. Reports of seven cases. Scand J Thorac Cardiovasc Surg. 1990;24(1):47–51. doi: 10.3109/14017439009101823. [DOI] [PubMed] [Google Scholar]
- 16. McCormick PC. Surgical management of dumbbell and paraspinal tumors of the thoracic and lumbar spine. Neurosurgery. 1996;38(1):67–75. doi: 10.1097/00006123-199601000-00017. [DOI] [PubMed] [Google Scholar]
- 17. Ciappetta P, Delfini R, Riccardelli R. Intrathoracic and intraspinal chondrosarcoma. Neurochirurgia (Stuttg). 1982;25(1):24–26. doi: 10.1055/s-2008-1053951. [DOI] [PubMed] [Google Scholar]
- 18. Zibis AH, Markonis A, Karantanas AH. Unusual causes of spinal foraminal widening. Eur Radiol. 2000;10(1):144–148. doi: 10.1007/s003300050022. [DOI] [PubMed] [Google Scholar]
- 19. Yünten N, Calli C, Zileli M, Ustün EE, Sener RN. Chondrosarcoma causing cervical neural foramen widening. Eur Radiol. 1997;7(7):1028–1030. doi: 10.1007/s003300050246. [DOI] [PubMed] [Google Scholar]
- 20. Pennington Z, Ehresman J, Pittman PD, et al. Chondrosarcoma of the spine: a narrative review. Spine J. 2021;21(12):2078–2096. doi: 10.1016/j.spinee.2021.04.021. [DOI] [PubMed] [Google Scholar]