Abstract
BACKGROUND
Intracranial aneurysms are prevalent, particularly with advancing age. De novo aneurysms, occurring independently from the initial lesion, pose a unique challenge because of their unpredictable nature. Although risk factors such as female sex, smoking history, and hypertension have been proposed, the mechanisms underlying de novo aneurysm development remain unclear.
OBSERVATIONS
A 79-year-old female developed a de novo saccular aneurysm within a year after management of a ruptured vertebral artery dissecting aneurysm. Her complex clinical course involved subarachnoid hemorrhage with diffuse vasospasm, stent occlusion of a dissecting aneurysm, discovery of a right 7- to 8-mm de novo middle cerebral artery aneurysm at the 1-year magnetic resonance angiography follow-up, and successful coil embolization.
LESSONS
This rare occurrence challenges established timelines, as most de novo aneurysms manifest over a longer interval. Studies have attempted to identify risk factors, yet consensus remains elusive, particularly regarding the influence of treatment modality on de novo formation rates.
This unique case urges reconsideration of posttreatment surveillance protocols, proposing shorter intervals for imaging and more vigilant follow-up strategies to detect asymptomatic de novo aneurysms. Timelier identification could significantly impact patient outcomes by averting potential ruptures. This emphasizes the need for further research to delineate effective monitoring and preventive measures for these enigmatic lesions.
KEYWORDS: de novo aneurysm, dissecting aneurysm, intracranial aneurysm
ABBREVIATIONS: CT = computed tomography, MCA = middle cerebral artery, MR = magnetic resonance
Intracranial aneurysms are relatively common, with their incidence increasing with age.1–3 First described by Graf and Hamby,4 de novo aneurysms, those occurring secondary to an initial aneurysm, are anatomically unrelated to the initial lesion and occur at rates of 0.28% to 1.8% per year.2,5 Although little is known about the underlying mechanisms of the development of de novo aneurysms, risks such as female sex, a history of smoking, and hypertension have been suggested.1,6 The age at onset of de novo aneurysms remains controversial; however, some studies have reported that an age <40 years is highly correlated with an increased risk,1,6 whereas others have reported that risk increases with advanced age (>40 years).7,8
The interval between presentation of an initial aneurysm and the second admission for the de novo aneurysm has been between 3 and 29 years,7 and monitoring for risks of de novo aneurysms is key, particularly as the incidence of subarachnoid hemorrhage from ruptured a de novo aneurysm is approximately five times the risk for intracranial aneurysms in general.9 Here, we present the case of a patient who developed a large de novo saccular aneurysm within a year after management of a ruptured vertebral artery dissecting aneurysm.
Illustrative Case
A 79-year-old right-handed female presented to the emergency department with a severe posterior headache and neck pain. The patient was taking 81 mg of aspirin daily. She had a medical history of hypertension, hyperlipidemia, and chronic obstructive pulmonary disease but no history of smoking or illicit drug use.
Upon her arrival, her blood pressure was elevated to 162/63. On examination, she was lethargic but had no focal neurological deficits. Her Glasgow Coma Scale score was 15. She had a Hunt and Hess grade of 3. Computed tomography (CT) of the head demonstrated extensive subarachnoid hemorrhage in the premedullary, prepontine, suprasellar, and sylvian cisterns along with intraventricular hemorrhage (Fig. 1), consistent with a modified Fisher grade IV. CT angiography of the head was negative for any vascular abnormalities.
FIG. 1.
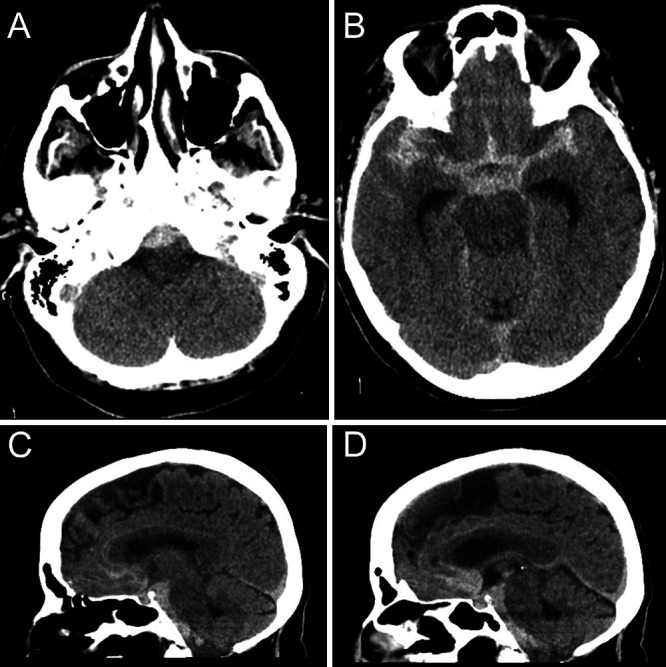
Head CT without contrast obtained during initial presentation, showing extensive subarachnoid hemorrhage within the premedullary (A), prepontine (C and D), suprasellar, and bilateral sylvian (B) cisterns.
The patient was intubated because of a deteriorating mental status, and an external ventricular drain was placed for worsening hydrocephalus. Magnetic resonance (MR) angiography performed on hemorrhage day 1 was concerning for a possible dissecting aneurysm within the right vertebral artery (Fig. 2A). No other vascular abnormalities were observed (Fig. 2B and C). Diagnostic cerebral angiography on hemorrhage day 2 confirmed the presence of a right vertebral artery dissecting aneurysm proximal to the posterior inferior cerebellar artery (Fig. 2D). No other vascular abnormalities were seen (Fig. 2E). A self-expanding Atlas stent was used to secure the aneurysm.
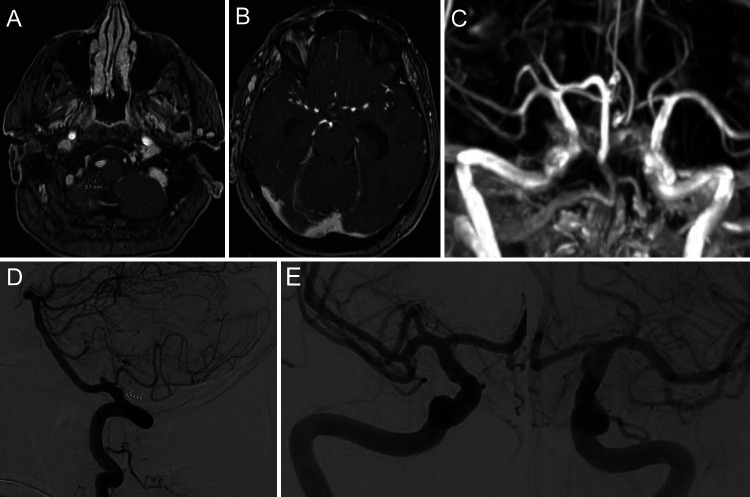
FIG. 2.
Initial vascular imaging. MR angiography (A) showing a right vertebral artery dissecting aneurysm. No additional vascular abnormalities were seen in the anterior circulation on time of flight (B) or maximum intensity projection (MIP; C) sequences. Diagnostic right vertebral artery angiogram (D), lateral view, with an arrow pointing to the dissecting aneurysm in the vertebral artery just proximal to the posterior inferior cerebellar artery. Right and left internal carotid artery injection angiograms (E), anteroposterior view, showing no additional vascular abnormalities.
The patient’s hospital course was complicated by vasospasm and multiple ischemic infarcts. The patient was eventually discharged on posthemorrhage day 14.
Repeat MR angiography at 2 months showed a patent right vertebral artery and no new vascular abnormalities (Fig. 3). However, at the 1-year follow-up, MR angiography revealed a de novo saccular aneurysm near the right middle cerebral artery (MCA) trifurcation, measuring 7 to 8 mm in diameter (Fig. 4). This was confirmed with a repeat diagnostic cerebral angiogram (Fig. 5A). Of note, the patient’s hypertension during the follow-up period was well controlled, with systolic blood pressure ranging from 97 to 122 mm Hg.
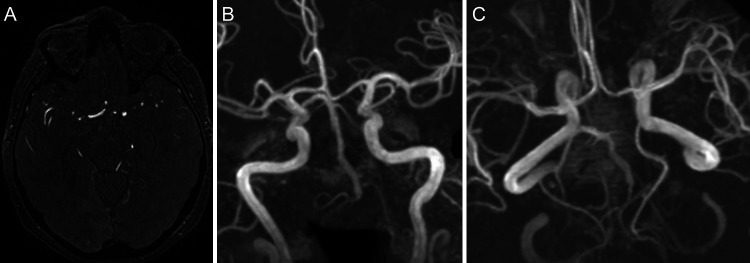
FIG. 3.
MR angiography at 2 months posthemorrhage. Time of flight (A) and MIP (B and C) sequences show no new vascular abnormalities.
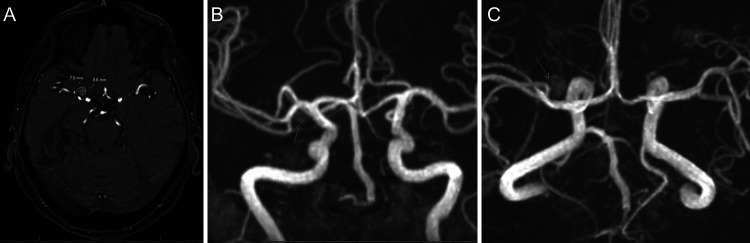
FIG. 4.
MR angiography performed at 1-year posthemorrhage. Axial view (A) showing a de novo right MCA aneurysm that is 7.0 mm × 8.6 mm in diameter. Coronal (B) and axial (C) MIP sequences showing the de novo aneurysm (arrow) near the MCA trifurcation.
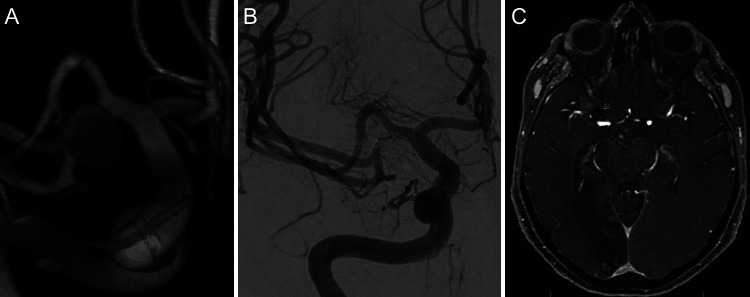
FIG. 5.
A: Three-dimensional reconstruction of right internal carotid artery (ICA) injection on repeat cerebral angiogram. There is a de novo aneurysm originating from one of the trifurcating branches of the right MCA. B: Anteroposterior view of right ICA injection after coil embolization of the right de novo MCA aneurysm. C: Axial MR angiography performed 2 months after coil embolization. Arrow indicates the embolized de novo aneurysm.
The patient elected to undergo endovascular management with coil embolization and had immediate angiographic occlusion of the aneurysm (Fig. 5B). Follow-up MR angiography at 2 months confirmed complete occlusion of the aneurysm (Fig. 5C).
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Observations
Our illustrative case demonstrates the rare presentation of a de novo aneurysm after management of a ruptured vertebral artery dissecting aneurysm. The incidence of ruptured intracranial aneurysms is approximately 10.5 cases in 100,000 persons,10 and the occurrence rate for the formation of de novo aneurysms is only between 0.28% and 1.8%,2,5 further depicting the rarity of the lesion. Although certain studies have reported de novo aneurysm formations in less than 5 years after presentation of an initial unruptured aneurysm (notably, Obray et al.6 at 6 and 22 months), there have been, to our knowledge, no reports of a de novo aneurysm presenting within 1 year of the initial ruptured aneurysm. Studies and meta-analyses that have investigated the occurrence of de novo aneurysms have demonstrated a mean incidence between 3% and 7.7%, with a follow-up interval of around 8 years.11,12
In addition, studies have reported the potential risk factors associated with de novo aneurysm formation, including female sex, history of smoking, hypertension, and multiplicity and localization of the aneurysm.7,12–14 However, a study of 130 patients conducted by Vourla et al.12 revealed that the aforementioned factors were not statistically associated with de novo aneurysm formation. There is also a lack of consensus regarding the relative risk of de novo formation after surgical clipping (3.3%)15 versus endovascular coiling (2.5%)16 for the treatment of intracranial aneurysms.
There is also the possibility that the de novo aneurysm may have been present at the onset of the subarachnoid hemorrhage presentation. If the lesion auto-thrombosed, the diagnostic cerebral angiogram may not have demonstrated the MCA aneurysm after the subarachnoid hemorrhage, which can occur in 6% to 30% of patients, only to be found on a later repeat angiogram.17 However, in our case, the patient had MR angiography studies on hemorrhage day 1 and at 2 months posthemorrhage, which did not demonstrate any vascular abnormalities within the right MCA territory.
Lessons
Most de novo aneurysms are discovered at more than 5 years of follow-up. In our case, this occurred within a year of rupture. Although this report represents only one example of a rapidly forming de novo aneurysm, it should provide reason for pause when formulating a follow-up plan after endovascular management of a spontaneous intracranial dissecting aneurysm. We propose that follow-up imaging, with either CT or MR angiography, be conducted at shorter intervals in order to assess risk of de novo aneurysm formation, which can present asymptomatically, and to improve the morbidity and mortality associated with aneurysm rupture.
Author Contributions
Conception and design: Bulsara, Diaz. Acquisition of data: all authors. Analysis and interpretation of data: all authors. Drafting the article: all authors. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Bulsara. Administrative/technical/material support: Diaz, Shin. Study supervision: Bulsara.
References
- 1. Hu S, Yu N, Li Y, Hao Z, Liu Z, Li MH. A meta-analysis of risk factors for the formation of de novo intracranial aneurysms. Neurosurgery. 2019;85(4):454–465. doi: 10.1093/neuros/nyy332. [DOI] [PubMed] [Google Scholar]
- 2. Cheong JJY, Ghinea N, van Gelder JM. Estimating the annual rate of de novo multiple aneurysms: three statistical approaches. Neurosurg Focus. 2004;17(5):E8. doi: 10.3171/foc.2004.17.5.8. [DOI] [PubMed] [Google Scholar]
- 3. Thompson BG, Brown RD, Jr, Amin-Hanjani S, et al. Guidelines for the management of patients with unruptured intracranial aneurysms: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(8):2368–2400. doi: 10.1161/STR.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 4. Graf CJ, Hamby WB. Report of a case of cerebral aneurysm in an adult developing apparently de novo. J Neurol Neurosurg Psychiatry. 1964;27(2):153–156. doi: 10.1136/jnnp.27.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. David CA, Vishteh AG, Spetzler RF, Lemole M, Lawton MT, Partovi S. Late angiographic follow-up review of surgically treated aneurysms. J Neurosurg. 1999;91(3):396–401. doi: 10.3171/jns.1999.91.3.0396. [DOI] [PubMed] [Google Scholar]
- 6. Obray R, Clatterbuck R, Olvi A, Tamargo R, Murphy KJ, Gailloud P. De novo aneurysm formation 6 and 22 months after initial presentation in two patients. AJNR Am J Neuroradiol. 2003;24(9):1811–1813. [PMC free article] [PubMed] [Google Scholar]
- 7. Rahmah NN, Horiuchi T, Kusano Y, Sasaki T, Hongo K. De novo aneurysm: case reports and literature review. Neurosurgery. 2011;69(3):E761–E767. doi: 10.1227/NEU.0b013e3182196489. [DOI] [PubMed] [Google Scholar]
- 8. Kemp WJ, 3rd, Fulkerson DH, Payner TD, et al. Risk of hemorrhage from de novo cerebral aneurysms. J Neurosurg. 2013;118(1):58–62. doi: 10.3171/2012.9.JNS111512. [DOI] [PubMed] [Google Scholar]
- 9. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol. 2011;10(7):626–636. doi: 10.1016/S1474-4422(11)70109-0. [DOI] [PubMed] [Google Scholar]
- 10. Tonn J, Hoffmann O, Hofmann E, Schlake HP, Sörensen N, Roosen K. “De novo” formation of intracranial aneurysms: who is at risk? Neuroradiology. 1999;41(9):674–679. doi: 10.1007/s002340050823. [DOI] [PubMed] [Google Scholar]
- 11. Giordan E, Lanzino G, Rangel-Castilla L, Murad MH, Brinjikji W. Risk of de novo aneurysm formation in patients with a prior diagnosis of ruptured or unruptured aneurysm: systematic review and meta-analysis. J Neurosurg. 2018;131(1):14–24. doi: 10.3171/2018.1.JNS172450. [DOI] [PubMed] [Google Scholar]
- 12. Vourla E, Filis A, Cornelius JF, et al. Natural history of de novo aneurysm formation in patients with treated aneurysmatic subarachnoid hemorrhage: a ten-year follow-up. World Neurosurg. 2019;122:e291–e295. doi: 10.1016/j.wneu.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 13. Juvela S, Poussa K, Porras M. Factors affecting formation and growth of intracranial aneurysms: a long-term follow-up study. Stroke. 2001;32(2):485–491. doi: 10.1161/01.str.32.2.485. [DOI] [PubMed] [Google Scholar]
- 14. Sakaki T, Tominaga M, Miyamoto K, Tsunoda S, Hiasa Y. Clinical studies of de novo aneurysms. Neurosurgery. 1993;32(4):512–517. doi: 10.1227/00006123-199304000-00004. [DOI] [PubMed] [Google Scholar]
- 15. Burkhardt JK, Chua MHJ, Weiss M, Do ASS, Winkler EA, Lawton MT. Risk of aneurysm residual regrowth, recurrence, and de novo aneurysm formation after microsurgical clip occlusion based on follow-up with catheter angiography. World Neurosurg. 2017;106:74–84. doi: 10.1016/j.wneu.2017.06.110. [DOI] [PubMed] [Google Scholar]
- 16. Yeon EK, Cho YD, Yoo DH, et al. De novo intracranial aneurysms detected on imaging follow-up of coiled aneurysms in a Korean population. Korean J Radiol. 2019;20(9):1390–1398. doi: 10.3348/kjr.2018.0914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Inamasu J, Nakamura Y, Saito R, et al. “Occult” ruptured cerebral aneurysms revealed by repeat angiography: result from a large retrospective study. Clin Neurol Neurosurg. 2003;106(1):33–37. doi: 10.1016/j.clineuro.2003.09.002. [DOI] [PubMed] [Google Scholar]