Abstract
The current study aimed to advance our understanding of the factors that influence mental health diversion in Local Courts in New South Wales, Australia. Logistic regression was used to systematically identify the factors that are correlated with diversion in a cohort of individuals (N = 7283) diagnosed with psychosis. Those with a substance-induced psychotic disorder were less likely to be diverted than those with an affective psychosis or schizophrenia, after adjusting for age, gender, Indigenous status, offence seriousness, violence and criminal history. Unexpectedly, those with psychotic disorders committing violent or serious offences were more likely to be diverted than those committing non-violent, less serious offences. Legal representation should be provided to all individuals with serious mental illnesses facing criminal charges. The State-wide Community and Court Liaison Service should be expanded to more Local Courts. Further research is required into why Aboriginal defendants with a psychotic illness are less likely to be diverted.
Keywords: court diversion, logistic regression, mental health referral, offenders, psychosis, substance-induced psychotic disorder
Introduction
Globally, rates of mental illness within criminal justice settings are consistently higher than in the general population (Al-Rousan et al., 2017; Bebbington et al., 2017; Fazel & Seewald, 2012; Tyler et al., 2019). In Australia, the prevalence of mental illness in incarcerated populations has been shown to be 80%; markedly higher than the community estimate of 31% (Butler et al., 2006). In response to the over-representation of those with mental illness in the criminal justice system, many countries have developed measures designed to divert mentally ill defendants away from the criminal justice system. The United States, for example, introduced Mental Health Courts (MHCs), which are run along similar lines to Drug Courts and are staffed by personnel who attempt to address the problems in offenders’ lives that contribute to the cycle of arrests (Castellano & Anderson, 2013).
Australia has mental health courts in Victoria, Queensland, South Australia, Western Australia and Tasmania, and most operate in a similar manner to MHCs in the United States (Davidson et al., 2017). New South Wales (NSW) does not have a mental health court but magistrates in NSW have the power to dismiss charges and divert mentally ill defendants into treatment (Richardson & McSherry, 2010), based on a mental health assessment. The relevant diversionary legislation in NSW was originally established in Sections 32 and 33 of the Mental Health (Forensic Provisions) Act 1990 (NSW). These sections enabled a magistrate to dismiss the charge or charges and discharge the defendant into the care of a person (Gotsis & Donnelly, 2008). Section 32 applied to ‘mentally disordered’ defendants, including those with cognitive impairments. Section 33 applied to ‘mentally ill’ defendants under the Mental Health Act 2007 (NSW) and permitted a magistrate to order the detention of a defendant in a treatment facility. Sections 32 and 33 were enforceable for up to six months. It should be noted at this point that, while the Mental Health (Forensic Provisions) Act 1990 (NSW) has since been repealed, the powers conferred upon courts under Sections 32 and 33 have since been carried over into Sections 12 and 19 of the new Mental Health and Cognitive Impairment Forensic Provisions Act (MHCIFPA) 2020 (NSW) passed by the NSW Parliament in 2020.
Evidence has recently emerged in Australia indicating that those who are diverted into treatment under the Mental Health Act 2007 (NSW) are less likely to re-offend than similar individuals who are prosecuted and dealt with according to law (Weatherburn et al., 2021). Earlier research, however, has shown that only a fraction of those eligible to be diverted into treatment are in fact diverted. Albalawi et al. (2019), using a dataset of 7743 individuals diagnosed with a psychotic disorder and who subsequently appeared in court charged with a criminal offence, found that only 26% received a treatment order and were diverted from the criminal justice system. Soon et al. (2018) found that, over a seven-year period, only 57.3% of defendants eligible for diversion were diverted by magistrates. An understanding of the factors that impede diversion of mentally ill defendants from the criminal justice system and into treatment is obviously of crucial importance in reducing re-offending. Little research to date, however, has been conducted on mental health diversion and none specifically on diversion under Sections 32 and 33 (or their current equivalents of Sections 12 and 19 of the MHCIFPA). The purpose of this study is to report the results of the first systematic analysis of the factors that influence magistrate decision making under Sections 32 and 33. In the next section of this article we provide further detail on the legal factors that courts are required to consider when exercising their discretion under these sections. We then describe the current study in more detail and report our results.
Relevant case law in NSW
Although Section 32 (and the new s 19 MHCIFPA provision) enables a court to divert a defendant into treatment if they are assessed as suffering from a mental illness or mental health condition, interpretation of the Act is guided by case law. Firstly, a decision must be made whether the defendant is eligible to be dealt with under Section 32 (and the new s 19 MHCIFPA provision) – that is, whether they are suffering from a mental illness or cognitive impairment. Secondly, a decision must be made as to whether (in light of the evidence) it would be ‘more appropriate’ to deal with the defendant in accordance with Section 32 (or the new s 19 MHCIFPA provision), rather than the criminal law (Gotsis & Donnelly, 2008). This second decision is a ‘balancing exercise’, in which the magistrate must consider the purpose of two potentially conflicting public interests: punishment through the ‘full weight of the law’, and diverting the mentally ill away into treatment for the protection of the community (Fernandez, 2007; Gotsis & Donnelly, 2008).
In reaching a decision under Section 32 (and the new s 19 MHCIFPA provision), a magistrate may consider the seriousness and circumstances of the alleged offence(s), the defendant’s criminal history, the existence and content of a treatment plan, the duration of the order and the sentencing options available if the defendant is dealt with according to the law (Gotsis & Donnelly, 2008). While offence seriousness is a relevant consideration in deciding whether or not to issue a Section 32 (or Section 19 MHCIFPA order) order (Gotsis & Donnelly, 2008), serious offences are not barred from diversion, as long as diversion is considered more appropriate than the alternative and more likely to result in a better outcome for the individual and the community (Fernandez, 2007). It is firmly established in case law that ‘clear and effective’ treatment plans must be available to magistrates before making Section 32 (or Section 19 MHCIFPA) decisions (Gotsis & Donnelly, 2008).
Given the tension between the interests of the broader community and the interests of the defendant, it would seem likely that the more serious the offence and the more substantial a defendant’s prior criminal history, the less likely they are to be diverted. Since older offenders and female offenders are less likely to reoffend than younger or male offenders, age and gender may be also likely to be relevant factors when a magistrate is considering whether to dismiss the charges against a defendant and refer him or her to mental health treatment. Finally, given the importance of a ‘clear’ treatment plan and the shortage of treatment services in small regional or remote areas, one might expect diversion to be less likely amongst defendants with a mental illness or cognitive impairment who live in remote areas.
Past research
In an analysis of 8317 individuals assessed as eligible for court diversion via the NSW State-wide Community and Court Liaison Service (SCCLS), Soon et al. (2018) found that, over a seven-year period, only 57.3% of defendants deemed eligible for diversion by clinicians were diverted by magistrates. Of the 57.3% that were diverted, 25% were diverted via Section 32 or 33. Soon et al. found that defendants with a mental illness were more likely to be diverted if they were over the age of 40, female, a non-Aboriginal or a Torres Strait Islander, or if they had a serious mental illness (as opposed to a substance use disorder or a ‘common’ mental disorder, e.g. an anxiety or a personality disorder). The following year Albalawi et al. (2019), in a study designed to assess the effectiveness of diversion under Section 32 in reducing the risk of reoffending, noted that there were differences in the characteristics of those whose charges were dismissed under this section. Albalawi et al. (2019) found that only 26% were diverted and that those diverted included a higher proportion of defendants who were older, non-Indigenous, married, Australian born and a resident in a higher socioeconomic status area at the time of most recent diagnosis, and who had received a diagnosis of schizophrenia (as opposed to an affective or substance-induced psychosis).
The Albalawi et al. (2019) and Soon et al. (2018) studies provide insight into factors magistrates may consider when deciding whether to divert a person charged with a criminal offence into mental health treatment; however, each has limitations for our purposes. Albalawi et al. found that those diverted into treatment tended to be older, non-Indigenous, Australian born and suffering from schizophrenia or an affective psychosis (rather than a substance-induced psychosis). Albalawi et al., however, did not determine which of these factors were unrelated to diversion after controlling for the effects of other factors. Soon et al. did not control for offence seriousness or violence, nor criminal history, which are likely to be important factors in magistrates’ decisions when making Section 32 or 33 orders.
As noted earlier, the current study is the first to systematically examine the factors that influence magistrate decision making under Section 32 and 33 orders. Our aim is to obtain a better understanding of the diversionary process as it affects defendants with a serious mental illness. More specifically, we seek to answer the following questions:
Are Indigenous defendants with a prior diagnosis of psychotic illness less likely to be diverted than non-Indigenous defendants with a psychotic illness?
Are defendants with a prior diagnosis of psychotic illness who are female and/or older more likely to be diverted than male defendants or those who are younger?
Are defendants with a prior diagnosis of psychotic illness less likely to be diverted if they live in an area where it is harder to access mental health treatment?
Are defendants with a prior diagnosis of psychotic illness less likely to be diverted if the charge or charges they face involve violence or a serious offence?
Are defendants with a prior diagnosis of substance-induced psychosis less likely to be diverted than defendants with other forms of psychotic illness?
Method
Sample
We used data from an existing dataset of 7743 individuals diagnosed with a psychotic disorder who were charged with at least one offence following this diagnosis between 2001 and 2012 (see Albalawi et al., 2019). Individuals under 18 years of age and any court cases in the children’s court were removed, as this court operates on different principles than the adult court. This resulted in a total sample of 7546. For the regression analysis, the total sample was 7283 as there were missing data for 263 individuals on one variable (remoteness of the area of residence at time of offence).
Data
An individual’s psychosis diagnosis was based on International Classification of Diseases–9th Revision (ICD–9) and 10th Revision (ICD–10) primary and secondary diagnosis codes (World Health Organization, WHO, 1978, 1992) and was obtained through NSW Ministry of Health’s Admitted Patient Data Collection (APDC) and the Emergency Department Data Collection (EDDC) for the period of 1 July 2001 to 31 December 2012. For admitted patients, the following ICD–9 and ICD–10 codes were used to define psychosis: schizophrenia and related psychoses (F20.1–F20.6, F20.8, F20.9, F22.0, F22.8, F22.9, F23.2, F23.3, F23.9, F25.0–F25.2, F25.9, F29 and 295); affective psychosis (F30.2, F31.2, F31.5, F32.3 F33.3, 296.8 and 296.9); and substance-induced psychotic disorder (F10.5, F13.5, F14.5, F15.5, F16.5, F19.5, 291 and 292). For individuals presenting to emergency departments, the diagnostic codes from the Systemized Nomenclature of Medicine–Clinical Terms (SNOMED–CT) were used, which map onto ICD–9 and ICD–10.
Offending data were obtained from the NSW Bureau of Crime Statistics and Research (BOCSAR) Re-offending Database (ROD; Hua & Fitzgerald, 2006), which provided information on whether the person was given a treatment order under Section 32 or 33 of the Mental Health (Forensic Provisions) Act 1990 NSW. The ROD also contains information on offence type, age, gender, race (Indigenous vs. non-Indigenous) and criminal history, including prior offence type. The health data and the reoffending data were linked via NSW Ministry of Health’s Centre for Health Record Linkage (CHeReL), outlined in more detail in Albalawi et al. (2019).
Dependent variable
The outcome of interest was referral to mental health services under Section 32 or 33 of the Mental Health (Forensic Provisions) Act 1990 NSW, coded ‘1’ if the defendant was diverted and ‘0’ if otherwise. We make no distinction between Section 32 and Section 33 dismissals because, prior to 2004, courts did not specify which section charges were dismissed under.
Independent variables
Offence seriousness was measured using the NSW Bureau of Crime Statistics and Research median severity ranking, or MSR (MacKinnell et al., 2010). The MSR for the most serious offence in the dataset was examined and the median obtained. Offences were divided into ‘less serious’ (an MSR of 85 and below) or ‘more serious’ (an MSR of 86 and above). A dummy variable identifying whether an offence involved violence was also examined as an offence may be serious without necessarily involving violence. The classification of an offence as violent or non-violent was based on the Australian and New Zealand Standard Offence Classification (ANZSOC; Pink, 2011). Violent offences were coded as any offence in Divisions 01–03 or 05–06. Offences under Division 04 ‘Dangerous or negligent acts endangering persons’ were categorised as non-violent, as they include offences such as dangerous driving, which, although they involve injury or harm, do not involve a plan to do harm.
The prior criminal history of the defendant was captured in two variables provided by the ROD. The first involved a count of the number of prior proven court appearances (i.e. court appearances at which at least one offence was found proved). The second involved a dichotomous variable of whether the defendant had previously been imprisoned or not. There was no direct measure of whether the defendant had a treatment plan available. Since mental health treatment may be harder to secure in regional and remote areas, we used a measure of remoteness – the Accessibility and Remoteness Index of Australia (ARIA) – developed by the Australian Bureau of Statistics, as a proxy measure of treatment availability (Commonwealth Department of Health and Aged Care, 2001).
In addition to variables that case law identifies as relevant to Section 32 and 33 determinations, we include several other variables on the grounds that, based on past research, or on a priori grounds, they might also be expected to influence Section 32 and 33 determinations.
The independent variables included in the analysis are:
Age (1 = 18–25, 2 = 26–35, 3 = 36–45, 4 = 46–55).
Gender (male = 0, female =1).
Indigenous status (0 = not Indigenous, 1 = Indigenous, 2 = unknown).
Number of prior court appearances (0 = no prior court, 1 = one prior court appearance, 2 = two to four prior court appearances, 3 = five or more court appearances).
Prior prison episode (0 = no prior prison episode, 1 = prior prison episode).
Remoteness of where the defendant resided at the time of offence (0 = major cities, 1 = inner regional, 2 = outer regional, 3 = remote or very remote).
Whether an offence involved violence or not (0 = non-violent offence, 1 = violent offence).
Seriousness of offence (0 = less serious offence, 1 = more serious offence).
Psychosis type (0 = affective psychosis or schizophrenia, 1 = substance-induced psychosis).
Whether the defendant was legally represented or not (0 = not represented, 1 = represented, 2 = unknown).
Whether the charge or group of charges was heard in a court with the SCCLS or not (0 = not an SCCLS court, 1 = an SCCLS court).
Analysis
All analyses were carried out in Stata 16.0. Firstly, a bivariate analysis was conducted to determine which variables were significantly related to mental health diversion. Then the significant variables in the bivariate analysis were included in a logistic regression to identify those variables that independently affect the odds of diversion. Tests confirmed that the assumption of linearity of the logit was not violated, and no problems of multicollinearity arose (see online Supplementary Material for output of these results). As odds ratios are not directly translatable as predicted probabilities, postestimation was used to generate the predicted probability of diversion for each individual in the study. These predicted probabilities were then averaged to estimate the proportions diverted for different combinations of offence/offender characteristics.
Results
Sample characteristics
The characteristics of the sample are shown in Table 1. Most of the sample were male, and most were non-Indigenous. The most common psychosis type was schizophrenia. Most of the sample lived in major cities. Most offences were non-violent, and just over half of the sample had no prior court appearances. Overall, 73.87% (n = 5574) of the sample were processed according to law (viz. prosecuted), and 26.13% (n = 1972) were granted a mental health dismissal.
Table 1.
Sample description.
| Variable | n (%) |
|---|---|
| Gender | |
| Male | 5509 (73.01) |
| Female | 2037 (26.99) |
| Age group (years) | |
| 18–25 | 1564 (20.73) |
| 26–35 | 2584 (34.24) |
| 36–45 | 2063 (27.34) |
| 46–87 | 1335 (17.69) |
| Indigenous status | |
| Non-indigenous | 5817 (77.09) |
| Indigenous | 498 (6.60) |
| Unknown | 1231 (16.31) |
| Psychosis type | |
| Affective | 768 (10.18) |
| Schizophrenia | 5223 (69.22) |
| Substance-induced | 1555 (20.61) |
| Prior court appearances | |
| No prior court appearances | 3954 (52.4) |
| One prior court appearance | 1388 (18.39) |
| Two to four prior court appearances | 1552 (20.57) |
| Five or more prior court appearances | 652 (8.64) |
| Prior prison | |
| Yes | 518 (93.14) |
| No | 7028 (6.86) |
| Remoteness of area | |
| Major cities | 5072 (69.64) |
| Inner regional | 1694 (23.26) |
| Outer regional | 451 (6.19) |
| Remote/very remote | 66 (0.91) |
| Unknown | 263 (3.49) |
| Legal representation | |
| Not represented | 2253 (29.86) |
| Represented | 4906 (65.01) |
| Unknown | 387 (5.13) |
| Type of offence | |
| Violent | 2645 (35.05) |
| Non-violent | 4901 (64.95) |
| Offence seriousness | |
| More serious | 3949 (52.33) |
| Less serious | 3597 (47.67) |
| Availability of court liaison service | |
| No court liaison service | 3602 (47.73) |
| Court liaison service | 3944 (52.27) |
Note: n = 7546.
Bivariate analysis
Table 2 shows the results of the bivariate comparisons. All covariates were significantly correlated with mental health diversion. Defendants were more likely to be diverted if they were older, were non-Indigenous, did not have a substance-induced psychotic disorder, did not have a prior court appearance, had not been previously imprisoned, lived in a major city or inner regional area or had committed a violent or serious offence. The only variable not significantly associated with mental health diversion was gender.
Table 2.
Bivariate comparisons of variables associated with mental health dismissal.
| Variable | N | MH dismissal (%) | p |
|---|---|---|---|
| Gender | .467 | ||
| Male | 5509 | 26.36 | |
| Female | 2037 | 25.53 | |
| Age group (years) | .001 | ||
| 18–25 | 1564 | 25.26 | |
| 26–35 | 2584 | 25.35 | |
| 36−45 | 2063 | 24.87 | |
| 46–87 | 1335 | 30.64 | |
| Indigenous status | <.001 | ||
| Non-Indigenous | 5817 | 27.63 | |
| Indigenous | 498 | 19.48 | |
| Unknown | 1231 | 21.77 | |
| Psychosis type | <.001 | ||
| Affective | 768 | 30.86 | |
| Schizophrenia | 4953 | 30.42 | |
| Substance-induced | 1555 | 9.39 | |
| Prior court appearances | <.001 | ||
| No prior court appearances | 3954 | 32.57 | |
| One prior court appearance | 1388 | 20.89 | |
| Two to four prior court appearances | 1552 | 17.65 | |
| Five or more prior court appearances | 652 | 18.40 | |
| Prior prison | <.001 | ||
| Yes | 518 | 18.34 | |
| No | 7028 | 26.71 | |
| Remoteness of areaa | <.001 | ||
| Major cities | 5072 | 29.14 | |
| Inner regional | 1694 | 20.84 | |
| Outer regional | 451 | 18.18 | |
| Remote/very remote | 66 | 12.12 | |
| Legal representation | <.001 | ||
| Not represented | 2253 | 5.02 | |
| Represented | 4906 | 36.10 | |
| Unknown | 387 | 22.74 | |
| Type of offence | <.001 | ||
| Violent offence | 2645 | 39.17 | |
| Non-violent offence | 4901 | 19.10 | |
| Offence seriousness | <.001 | ||
| More serious | 3949 | 32.69 | |
| Less serious | 3597 | 18.93 | |
| Availability of court liaison service | <.001 | ||
| No court liaison service | 3602 | 23.90 | |
| Court liaison service | 3944 | 28.17 |
Note: MH = mental health.
aExcluding ‘unknown’.
Multivariate analysis
The results of the logistic regression are shown in Table 3. Controlling for other factors, Indigenous defendants were less likely to be diverted than non-Indigenous defendants, as were those whose Indigenous status was unknown. Age did not appear to affect the likelihood of diversion although the p-value associated with age is close to significance, suggesting that those aged over 45 years are more likely to be diverted than younger defendants. Remoteness of residence had a strong effect on the likelihood of diversion, with the odds of diversion among those in remote or very remote areas being less than half that of those residents in major cities. Having one or more prior appearances in court reduced the odds of diversion but prior imprisonment had no effect, most likely because much of its effect was captured by the prior court variable. Individuals with legal representation had 10 times higher odds of being diverted than those without legal representation.
Table 3.
Correlates of mental health diversion.
| Given a treatment order under Section 32/33 | Odds ratio | Robust SE | p |
95% CI |
|---|---|---|---|---|
| Indigenous status | ||||
| Non-indigenous (reference) | ||||
| Indigenous | 0.714 | 0.093 | .010 | [0.554, 0.923] |
| Unknown | 0.836 | 0.072 | .038 | [0.706, 0.999] |
| Age group, years | ||||
| 18–25 (reference) | ||||
| 26–35 | 1.05 | 0.090 | .592 | [0.885, 1.239] |
| 36–45 | 0.971 | 0.087 | .747 | [0.814, 1.158] |
| 46+ | 1.20 | 0.114 | .055 | [0.996, 1.446] |
| Remoteness of area | ||||
| Major cities (reference) | ||||
| Inner regional | 0.594 | 0.045 | <.001 | [0.512, 0.690] |
| Outer regional | 0.495 | 0.071 | <.001 | [0.373, 0.657] |
| Remote/very remote | 0.382 | 0.151 | .015 | [0.176, 0.829] |
| Prior court | ||||
| No prior court appearance (reference) | ||||
| One prior court appearance | 0.591 | 0.050 | <.001 | [0.501, 0.698] |
| Two to four prior court appearances | 0.481 | 0.042 | <.001 | [0.405, 0.572 |
| Five or more court appearances | 0.534 | 0.074 | <.001 | [0.407, 0.701] |
| Prior prison | 1.00 | 0.151 | .994 | [0.745, 1.344] |
| Legal representation | ||||
| Not represented (reference) | ||||
| Represented | 10.15 | 1.10 | <.001 | [8.20, 12.56] |
| Unknown | 5.375 | 0.866 | <.001 | [3.92, 7.37] |
| Court liaison available at court | 1.251 | 0.079 | <.001 | [1.10, 1.415] |
| Violent offence | 2.038 | 0.126 | <.001 | [1.806, 2.300] |
| More serious offence | 1.436 | 0.089 | <.001 | [1.270, 1.624] |
| Psychosis type | ||||
| Affective/schizophrenia (reference) | ||||
| Substance-induced | 0.217 | 0.022 | <.001 | [0.179, 0.265] |
| Constant | 0.058 | 0.007 | <.001 | [0.045, 0.075] |
Note: CI = confidence interval.
Individuals processed at Local Courts with a court liaison service were significantly more likely to be diverted (odds ratio = 1.25) than those at courts without the SCCLS. Those diagnosed with a substance-induced psychotic disorder were substantially less likely to be diverted, even after controlling for age, gender, Indigenous status, remoteness of residence, legal representation, court liaison service, charge type and seriousness and prior record. The two most surprising findings are that those charged with violent or serious offences were substantially more likely to be diverted than those charged with non-violent or less serious offences (odds ratio of 2.04 and 1.44, respectively).
Predicted probability analysis
Individuals suffering from schizophrenia or depression are known to be at heightened risk of committing violent offences (Cho et al., 2019; Fazel et al., 2015). It is possible that courts take a more lenient view of violence when the defendant is suffering from schizophrenia or depression than when the defendant is suffering from a substance-induced psychotic disorder. If this is true, the difference in diversion rates between those charged with violent offences and those charged with non-violent offences should be smaller among those with an affective/schizophrenia disorder than among those charged with a substance-induced psychotic disorder. A similar interaction might be expected to exist between psychosis type and offence seriousness. To explore this, we calculated the predicted probabilities of diversion for those who commit violent or serious offences, separately for the two types of disorder. The computation proceeded on the basis that the values of all other variables are held at their modal values.
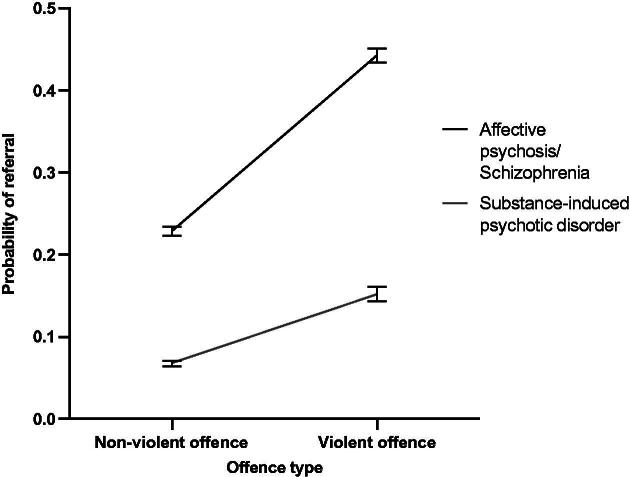
Figure 1 shows the change in the predicted probability of diversion as we move from a non-violent to a violent offence. The top curve shows the effect of this transition on those with an affective/schizophrenia disorder. The bottom curve shows the effect for those with a substance-induced psychotic disorder. There are two important points to take away from this graph. Firstly, even when the charge involves a non-violent offence, those with a substance-induced psychotic disorder are less likely to be diverted than those with an affective psychosis/schizophrenia disorder. Secondly, contrary to expectations, the transition from non-violence to violence has a larger positive effect on the probability of diversion among those with an affective psychosis/schizophrenia disorder than on those with a substance-induced psychosis.
Figure 1.
Predicted probability of diversion for violent and non-violent offenders with psychosis type as a parameter.
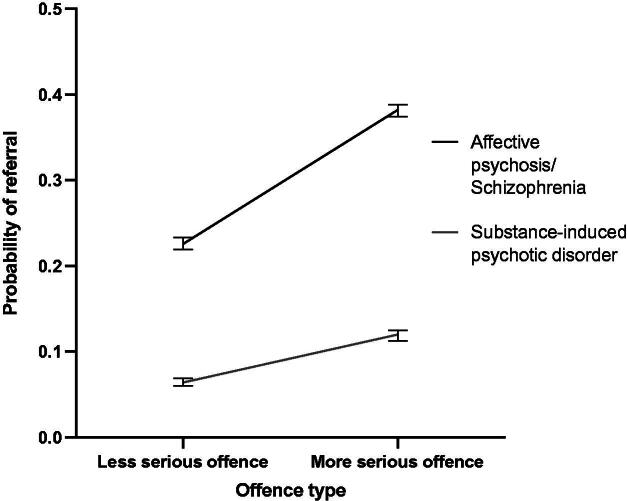
Figure 2 shows the effect of offence seriousness and psychosis type on the probability of diversion. The pattern is the same as that for violence. Regardless of whether the defendant is charged with a serious or a non-serious offence, those with a substance-induced psychotic disorder are substantially less likely to be diverted than those with an affective/schizophrenic psychosis. Furthermore, the effect on the likelihood of diversion of moving from a less to a more serious offence is more pronounced among those with an affective/schizophrenia psychosis than among those with a substance-induced psychotic disorder. The difference in diversion probability for those charged with a serious offence and those charged with a non-serious offence is .16 for those with an affective/schizophrenia disorder but only .06 for those with a substance-induced psychotic disorder.
Figure 2.
Predicted probability of diversion for serious and non-serious offenders with psychosis type as a parameter.
Discussion
This article sought to answer several questions relating to diversion of those with histories of serious mental illness (psychosis) appearing in the magistrates’ courts in New South Wales (Australia) between 2001 and 2012. Several important findings emerged that have implications for the current operations of court diversion services both locally and more broadly.
Firstly, Indigenous defendants were significantly less likely to be diverted than non-Indigenous defendants even after controlling for factors such as age, remoteness of residence, prior contact with the court system, legal representation, the presence or absence of a court liaison service, prior imprisonment, offence seriousness and whether charged with a violent offence. Remoteness of residence has a strong effect on the likelihood of diversion, with the odds of diversion among those in remote or very remote areas being less than half those residing in major cities. Contrary to what might have been expected, those charged with a violent or (otherwise) serious offence are more likely to be diverted than those charged with a non-violent or less serious offence. Finally, those suffering from a drug-related psychosis are much less likely to be diverted than those suffering from affective psychosis or schizophrenic psychosis. This is true regardless of whether the charge is serious or involves violence. In fact, the effect of these last two variables on the likelihood of diversion appears weaker among those with a drug-related psychosis than among those suffering from a mood/schizophrenia disorder.
Given that all Australian Governments have recently committed to reducing Indigenous over-representation in custody by 15% by 2031 (Australian Government, 2020) as part of the Closing the Gap initiative, our findings in relation to Indigeneity are a matter of concern. The negative effect of remoteness on the likelihood of diversion is easier to understand. As noted earlier, ‘clear and effective’ treatment plans must be available to magistrates before making Section 32 decisions (Gotsis & Donnelly, 2008), and this is more likely to be limited in regional and remote areas of Australia than it is in major cities (Van Spijker et al., 2019). The SCCLS, which is the main provider of court advice on whether an individual meets the statutory criteria for diversion and/or requires mental health diversion (Davidson et al., 2016), is only available in 22 NSW Local Courts, with 59% of these being in major cities and the remainder (∼105) in inner regional cities (Justice Health & Forensic Mental Health Network, 2021).
The fact that the odds of diversion were ten times higher for those with legal representation than those without highlights the importance of legal counsel when there is an indication of mental illness. All individuals in the sample had been diagnosed with a psychotic illness, and thus the finding that those with no legal representation were significantly less likely to be diverted underscores the importance of affording legal representation to individuals with serious mental illnesses.
The finding that those with a substance-induced psychotic disorder were less likely to be diverted than those with other forms of functional psychosis is consistent with the observations of Soon et al. (2018). One possible explanation for this result is that the definition of psychosis in this dataset was based on World Health Organization (WHO) ICD codes. Substance-induced psychotic disorder, as defined in the ICD codes, is transient, lasting from 7 to 20 days, but not more than one month. Symptoms lasting more than 30 days would generally be classified as a more chronic psychosis type, such as schizophrenia (World Health Organization, WHO, 1992). To be included in the sample, subjects in the study had to receive a diagnosis of psychosis before they committed at least one offence. Given the observation period was over several years, it is possible that some individuals with a substance-induced psychosis were not experiencing psychotic symptoms at the time of the current offence/s nor during their court appearance, which would preclude them from diversion.
The most significant puzzle to emerge from this study is the higher rate of diversion amongst those facing charges of having committed a violent or otherwise serious offence. Given that decisions in relation to Sections 32 and 33 require the court to balance the public interest in those charged with a criminal offence facing the full weight of the law against the public interest in treating, or regulating to the greatest extent practical, the conduct of individuals suffering from any of the mental conditions referred to in Section 32(1) or mental illness (Section 33), one might have expected that those facing charges of having committed a violent or serious offence would be less likely to be diverted than similar individuals who committed a non-violent or less serious offence. The findings suggest that some other factor, correlated with violence or seriousness but not measured in the current study, is responsible for the surprising result. It may also be that more serious or violent offences suggest a stronger link between the psychotic illness and the offending behaviour than less serious or non-violent offences. It is possible that magistrates see violence as having a biological basis that is treatable with psychotropic medications and are thus amenable to referring this group to mental health services for treatment.
The findings of the current study must be considered in light of its limitations. Crucially, we were unable to determine the time from diagnosis to first offence. This is particularly important for drug-related psychosis because it is, by definition, a transient state. This may be a significant confounder of the results, as some individuals with a substance-induced psychotic disorder in the sample might not have been psychotic at the time of their offence. Finally, although it was known that the individuals in the sample were diagnosed with psychosis, it is unknown whether their legal counsel sought to have the charge or charges dismissed under Section 32 or 33. Individuals could have differed significantly from one another in this respect, and this would have undoubtedly influenced the chances of success in an application to have the charges dismissed under Sections 32 and 33.
Conclusions
The current study provides important new insight into the factors that influence court decision making when deciding whether to dismiss a charge and refer a defendant to treatment on mental health grounds. Further research is clearly required into why Aboriginal defendants are less likely to be diverted on these grounds and why defendants facing violent or other serious charges are more likely to be diverted into treatment than non-violent, non-serious offenders. The finding that those who live in remote areas are less likely to be diverted than those in more urbanised areas also warrants further investigation. If it turns out that the effect is attributable to lack of legal and/or medical resources, those deficits will need to be addressed.
Ethical standards
Declaration of conflicts of interest
Christel Macdonald has declared no conflicts of interest
Don Weatherburn has declared no conflicts of interest
Tony Butler has declared no conflicts of interest
Olayan Albalawi has declared no conflicts of interest
David Greenberg has declared no conflicts of interest
Michael Farrell has declared no conflicts of interest
Supplementary Material
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors. Note that although the study was an analysis of deidentified health and court records, it was not an in vivo experiment with human participants.
References
- Albalawi, O., Chowdhury, N. Z., Wand, H., Allnutt, S., Greenberg, D., Adily, A., Kariminia, A., Schofield, P., Sara, G., Hanson, S., O’Driscoll, C., & Butler, T. (2019). Court diversion for those with psychosis and its impact on re-offending rates: Results from a longitudinal data-linkage study. BJPsych Open, 5(1), 1–9. 10.1192/bjo.2018.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Rousan, T., Rubenstein, L., Sieleni, B., Deol, H., & Wallace, R. B. (2017). Inside the nation’s largest mental health institution: A prevalence study in a state prison system. BMC Public Health, 17(1). 10.1186/s12889-017-4257-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Government. (2020). National agreement on closing the gap. https://www.closingthegap.gov.au/national-agreement
- Bebbington, P., Jakobowitz, S., McKenzie, N., Killaspy, H., Iveson, R., Duffield, G., & Kerr, M. (2017). Assessing needs for psychiatric treatment in prisoners: 1. Prevalence of disorder. Social Psychiatry and Psychiatric Epidemiology, 52(2), 221–229. 10.1007/s00127-016-1311-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler, T., Andrews, G., Allnutt, S., Sakashita, C., Smith, N. E., & Basson, J. (2006). Mental disorders in Australian prisoners: A comparison with a community sample. The Australian and New Zealand Journal of Psychiatry, 40(3), 272–276. 10.1080/j.1440-1614.2006.01785.x [DOI] [PubMed] [Google Scholar]
- Castellano, U., & Anderson, L. (2013). Mental health courts in America. American Behavioral Scientist, 57(2), 163–173. 10.1177/0002764212465616 [DOI] [Google Scholar]
- Cho, W., Shin, W.-S., An, I., Bang, M., Cho, D.-Y., & Lee, S.-H. (2019). Biological aspects of aggression and violence in schizophrenia. Clinical Psychopharmacology and Neuroscience, 17(4), 475–486. 10.9758/cpn.2019.17.4.475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commonwealth Department of Health and Aged Care. (2001). Measuring remoteness: Accessibility/Remoteness Index of Australia (ARIA). Australian Government. [Google Scholar]
- Davidson, F., Heffernan, E., Greenberg, D., Butler, T., & Burgess, P. (2016). A Critical Review of Mental Health Court Liaison Services in Australia: A first national survey. Psychiatry, Psychology and Law, 23(6), 908–921. 10.1080/13218719.2016.1155509 [DOI] [Google Scholar]
- Davidson, F., Heffernan, E., Greenberg, D., Waterworth, R., & Burgess, P. (2017). Mental health and criminal charges: Variation in diversion pathways in Australia. Psychiatry, Psychology, and Law: An Interdisciplinary Journal of the Australian and New Zealand Association of Psychiatry, Psychology and Law, 24(6), 888–898. 10.1080/13218719.2017.1327305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel, S., & Seewald, K. (2012). Severe mental illness in 33 588 prisoners worldwide: systematic review and meta-regression analysis. The British Journal of Psychiatry: The Journal of Mental Science, 200(5), 364–373. 10.1192/bjp.bp.111.096370 [DOI] [PubMed] [Google Scholar]
- Fazel, S., Wolf, A., Chang, Z., Larsson, H., Goodwin, G. M., & Lichtenstein, P. (2015). Depression and violence: a Swedish population study. The Lancet Psychiatry, 2(3), 224–232. 10.1016/S2215-0366(14)00128-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez, L. (2007). Section 32 Mental Health (Criminal Procedure) Act – Summary of principles. Legal Aid NSW. https://www.legalaid.nsw.gov.au/__data/assets/pdf_file/0006/6099/Section-32-Summary-of-Principles-.pdf
- Gotsis, T., & Donnelly, H. (2008). Diverting mentally disordered offenders in the NSW Local Court. Judicial Commission of New South Wales. [Google Scholar]
- Hua, J., & Fitzgerald, J. (2006). Matching court records to measure reoffending. NSW Bureau of Crime Statistics and Research Crime and Justice Bulletin, 1–12. https://www.bocsar.nsw.gov.au/Publications/CJB/cjb95.pdf [Google Scholar]
- Justice Health and Forensic Mental Health Network. (2021). https://www.justicehealth.nsw.gov.au/about-us/health-care-locations/courts
- Mackinnel, I., Poletti, P., & Holmes, M. (2010). Measuring offence seriousness. Crime and Justice Bulletin, (142), 1–12. https://www.bocsar.nsw.gov.au/Publications/CJB/cjb142.pdf
- Pink, B. (2011). Australian and New Zealand standard offence classification (ANZSOC). Australian Bureau of Statistics. https://www.abs.gov.au/statistics/classifications/australian-and-new-zealand-standard-offence-classification-anzsoc/latest-release
- Richardson, E., & McSherry, B. (2010). Diversion down under—programs for offenders with mental illnesses in Australia. International journal of Law and Psychiatry, 33(4), 249–257. 10.1016/j.ijlp.2010.06.007 [DOI] [PubMed] [Google Scholar]
- Soon, Y.-L., Rae, N., Korobanova, D., Smith, C., Gaskin, C., Dixon, C., Greenberg, D., & Dean, K. (2018). Mentally ill offenders eligible for diversion at local court in New South Wales (NSW), Australia: Factors associated with initially successful diversion. The Journal of Forensic Psychiatry & Psychology, 29(5), 705–716. 10.1080/14789949.2018.1508487 [DOI] [Google Scholar]
- Tyler, N., Miles, H. L., Karadag, B., & Rogers, G. (2019). An updated picture of the mental health needs of male and female prisoners in the UK: prevalence, comorbidity, and gender differences. Social psychiatry and Psychiatric Epidemiology, 54(9), 1143–1152. 10.1007/s00127-019-01690-1 [DOI] [PubMed] [Google Scholar]
- Van Spijker, B. A., Salinas-Perez, J. A., Mendoza, J., Bell, T., Bagheri, N., Furst, M. A., Reynolds, J., Rock, D., Harvey, A., Rosen, A., & Salvador-Carulla, L. (2019). Service availability and capacity in rural mental health in Australia: Analysing gaps using an Integrated Mental Health Atlas. The Australian and New Zealand Journal of Psychiatry, 53(10), 1000–1012. 10.1177/0004867419857809 [DOI] [PubMed] [Google Scholar]
- Weatherburn, D., Albalawi, O., Chowdhury, N., Wand, H., Adily, A., Allnutt, S., & Butler, T. (2021). Does mental health treatment reduce recidivism among offenders with a psychotic illness? Journal of Criminology, 54(2), 239–258. 10.1177/0004865821996426 [DOI] [Google Scholar]
- World Health Organization (WHO). (1978). The ninth revision of the international classification of diseases and related health problems (ICD-9). World Health Organization. [Google Scholar]
- World Health Organization (WHO). (1992). The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.