Abstract
Treatment recommendations for cancer patients are carried out according to clinical assessment, type and stage of cancer and treatment guidelines. However, many patients do not accept the recommendations. This raises obstacles in managing of cancers, which not only affects the patients, but also the family and people around the patients. This problem could increase morbidity, mortality and recurrence rate, which might result in lower quality of life. Since this condition is a complex problem, there is necessity to explore and determine various determinants from different levels. The aim of this systematic review was to explore the acceptances of cancer treatments among cancer patients and its associated determinants. Articles published from 2010 to 2023 were searched in four databases: ScienceDirect, Medline, Google Scholar and PubMed. Articles written in English and focussing on three main cancer treatments (surgery, chemotherapy and radiotherapy) were eligible. A narrative approach was used and the data were analysed into selected themes. Data suggest that several factors influence patient acceptance for cancer therapy including sociodemographic, economic and spiritual cultural backgrounds; patient knowledge and perceptions; community support, as well as policy and availability of health facilities. The determinants consist of individual, interpersonal, institutional, community and public policy level and interaction between levels are contributing to cancer treatment acceptance. In conclusion, cancer treatment acceptance remains a problem in particular in low middle income countries. In addition, the data on radiotherapy referral acceptance were limited and needed further study.
Keywords: Cancer, treatment, acceptance, transtheoretical, quality of life
Introduction
Cancer defined as a disease sequence which progressively decreased the control of cell growth. Treatment of cancer in general consists of local therapy (surgery or radiotherapy) which focused on the site of primary tumor and its circumambient glands; and systemic therapy which focused to prevent metastases to distant areas (chemotherapy or radiotherapy). It can be given alone or combination (multimodality) [1]. Therapy of cancer are adjusted to its sensitivity and response to each therapeutic modality, thus, one of the common strategies is tumor resection with surgery followed by radiotherapy and/or chemotherapy [2]. On the other hand, considerations such as the infiltration depth of the primary tumor and the outgrowth distribution into blood vessels or lymph nodes are the determinant of cancer’s therapy with chemotherapy and/or radiotherapy. Surgery was considered as effective as primary choice of therapy if the cancer found at an early stage. Radiotherapy and chemotherapy have its limitation which damaging healthy cells and tissues and causing cancer resistance to drugs. However, as adjuvant therapy, it can reduce morbidity, mortality and cancer recurrence [1].
Treatment recommendations are carried out by physician according to clinical assessment, type and stage of cancer align with therapy guidelines. However, not all patients carry out therapy according to the recommendations that have been given. This raises obstacles in the process of cancer therapy, which not only affects the patient, but also the family and other significant parties. Increased number of morbidities, mortality and recurrence leads to increased length of treatment and costs which results in lower quality of life. Several factors influence patient adherence in carrying out therapy such as sociodemographic, economic, and spiritual-cultural; patient knowledge and perceptions; perception and support from people around the patient; as well as policy and availability of health facilities [3,4].
Overall survival and quality of life can be increased through several determinants such as background factors, perceptions, and encouragement from the patient; family and health worker’s support; and especially the availability of resources to support the implementation of behavior change, namely acceptance. However, there are still few studies that examine patient’s acceptance of the recommended therapy. Previous studies have defined acceptance as an active condition in which an individual can live with an uncomfortable experience, acknowledge, and want to experience all aspects of the current situation, both physically and emotionally, regardless of social pressure and self-will. There are several studies that showed the relation between acceptance and several conditions such cancer or a terminal illness [5].
Acceptance can be based on behavior which the desire to experience and carry out a certain experience or self-regulatory theory which is not too fixated on the problem at hand and focuses more on aspects that are not affected by the problem [6]. This study uses the definition of acceptance as the patient’s willingness to carry out therapy according to their doctor’s recommendations including the psychological, physical, and economic effects that accompany the experience.
Due to the complexity of psychological condition, acceptance is influenced by various factors, both from within the patient and outside influences. The aim of this systematic review was to determine the factors influence patient’s acceptance of therapy recommendations, as well as what efforts have been made to be able to turn barrier variables into patient supports. It is expected that the results could help health workers and policy makers to increase patient’s acceptance in real world.
Methods
Information sources and search strategy
Three databases, PubMed, ScienceDirect and Google Scholar, were searched using the search terms “acceptance of treatment” AND “cancer patients” OR “treatment” OR “radiotherapy” OR “chemotherapy” OR “surgery” up to May 10, 2023. Further terms were used such as “factor influencing treatment option”, “referral to radiotherapy”, “cancer treatment”, “determinant of health”, “cancer therapy accessibility”, “multimodality treatment of cancer”, “cancer treatment access” and “decision making in cancer treatment”. The searches were restricted to 10-year period (2013 to 2023).
Study risk of bias assessment
The searches and risk of bias assessment manually were performed by two independent authors. Each author assessed risk of bias independently and then convened to discuss and review their risk of bias assessments. Literature search using the Preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.
Eligibility criteria
Inclusion criteria of the studies to be included were: (a) studies assessing factors influencing acceptance and choice of therapy for cancer patients, for all types and stages of cancer; (b) qualitative research; (c) published within the last 10 years; (d) studies using single and multimodal therapy; and (e) studies on factors and access that influence actualization of cancer therapy.
Selection and data collection process
Two investigators (RN and AP) used Mendeley citation manager to complete the study selection, and the process was divided into three parts. First, all duplicates and incomplete studies were excluded. Next, the titles and abstracts of all studies were initially reviewed and were graded according to the inclusion criteria. Subsequently, full-texts were read to determine the eligibility of each study based on inclusion criteria and data availability. Data extraction encompassed information from the main articles and supplementary materials when necessary. Additionally, the references were retrieved to find any further studies. Study characteristics such as authors, publication year, study location, and study design were collected. Furthermore, we collected information of study inclusion, study purpose, study groups, and outcomes for each eligible study. All disputes during the study selection process were resolved other two authors (TR and MM).
Synthesis methods
The data were qualitatively analyzed by shifting, charting, coding, and sorting material according to the aims of the study. The results of charting data were summarized into three aspects: demographic of cancer (total sample, type of cancer, median age), objective study, and main associated determinants.
Results
Study selection
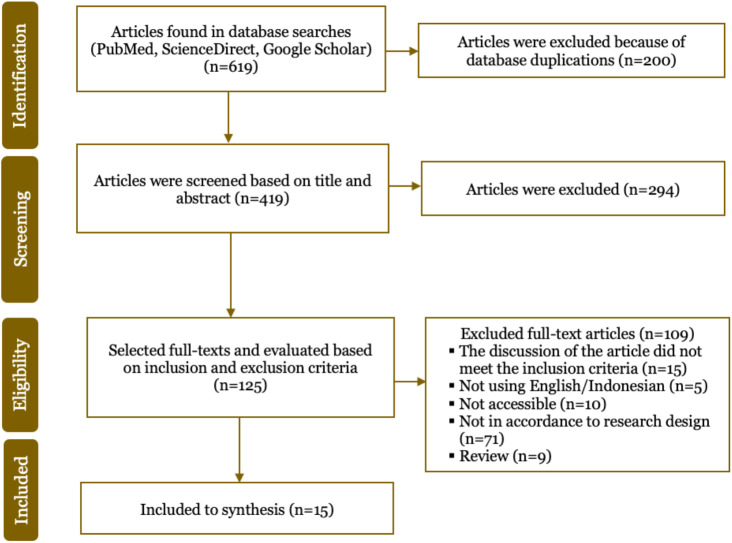
Of the 619 articles yielded from the searches, after selecting abstracts and assessing the contents of the research; duplicates; inclusion and exclusion criteria; appropriateness of the abstract and research content, thus, only 16 articles could be used for this study. A total of 15 literature that met the inclusion criteria and were not included in the exclusion criteria were retrieved and narrated in this review (Figure 1).
Figure 1. PRISMA flow diagram of study selection.
Cancer treatment acceptance and its associated factors
Acceptance of therapy is not easy, especially for cancer patients. Receiving a cancer diagnosis on their own is a difficult thing for patients, mainly due to the patient’s lack of familiarity with cancer. When patients hear that they have been diagnosed with cancer, they tend to feel that the disease is difficult to cure, requires a lot of money, and the side effects of therapy are also severe. Time, cost, and quality of life are the main factors for patient consideration in receiving therapy.
Most results applied acceptance therapy in the subset of gynecological cancer while the least is chronic pain on terminal illness (1/15). Acceptance of cancer and its treatment goes through 5 stages: non-acceptance, passive acceptance, willingness to accept, accepting behavior, and acceptance practice. Acceptance develops over time in therapy. Factors that play a role in refusal of therapy are discomfort due to therapy, fear of side effects, difficulties with transportation. Elderly patients prefer to maintain quality of life rather than prolong their life. The most consistent determinant is doctor’s recommendation, thus, trust in health workers increases expectations and acceptance for therapy (Table 1).
Table 1. Basic characteristics of included studies, acceptance and factors associated with treatment in cancer patients.
| Author, place, and design of study | Total sample, type of cancer, median age | Objective | Main associated determinants |
|---|---|---|---|
| Stoker (2014); Indonesia; cohort Prospective [17] | n=67; nasopharynx cancer; 47-year-old | To describe why the overall time to radiotherapy and the interval from diagnosis to therapy takes longer. | The main reason for absent for radiotherapy session were due to unavailability of the machines. Other reasons include poor patient conditions, national holidays, radiation adjustments, power outages, treatment planning systems that are not operational, factors related to the patient and the type of insurance. |
| Lam (2015); Australia; cross-sectional [9] | n=574; Breast cancer; 63-year-old | To explore the radiotherapy affordability and increase breast conservation therapy (BCT) acceptance rates | Increasing the affordability of radiotherapy by reducing transportation costs does not increase the acceptance of breast conservation therapy (BCT) because the convenience of therapy is the main consideration for patients |
| Calaguas (2016); Southeast Asia; qualitative study [11] | N/A | To explore the accessibility of radiotherapy in Southeast Asia through the socioeconomic perspective of the Philippines, where urban and rural locations affect this condition. | Improving access to radiotherapy is a complex issue in the highly heterogeneous region of Southeast Asia. Not only poverty barriers, but also sociocultural factors that influence health seeking behavior from the community to be noted in cancer therapy. |
| Smith (2017); Australia; cohort prospective [18] | n=21; prostate, breast, gynecological, head and neck cancer, hematology malignancies, and melanoma; 64-year- old | To explore patient perceptions in their involvement in choosing therapy, patient knowledge and understanding regarding therapy, and interaction preferences with health workers | Trust in the radiation oncology specialist, feeling explained about the side effects and benefits of therapy, a treatment team showing concern for the patient, and feeling part of the department make the patient more likely to accept treatment. |
| Egger (2019); Australia; cohort prospective [19] | n=1071; prostate cancer; >40-year-old | To describe the trend of urology specialists in referring high risk prostate cancer patients to radiation oncology specialists 4 months after radical prostatectomy and receiving radiotherapy 6 months after consultation with radiation oncologists. | Only 30% of patients with high-risk features are referred to a radiation oncology specialist. This is influenced by perceptions and referral bias of urology specialists. When patients had seen a radiation oncology specialist, 61% received radiotherapy within 6 months. This demonstrates the importance of eliminating referral bias to increase radiotherapy acceptability |
| Minichsdorfer (2020); Austria; cross-sectional [20] | n=101; pulmonary, breast, and other type of cancer; 56.2-year- old | To assess patient information and expectations when starting their first cancer therapy, and communication satisfaction with healthcare professionals | Patients who do not speak fluent German feel that there is a lack of communication. Poor doctor-patient communication is often the main factor for poor palliative care. A significant number of patients anticipate the adverse side effects of therapy with a more positive approach. |
| Yap (2021); Australia; cohort retrospective [8] | n=267; Metastatic cancer (25% primary lung cancer, 16% colorectal, 10% unknown); 72-year- old | To compare actual and optimal use of radiotherapy | Radiotherapy acceptance is lower, especially in elderly patients and those with more comorbidities. |
| Author, place, and design of study | Total sample, type of cancer, median age | Objective | Main associated determinants |
| Jin (2021); China; Cross-sectional [15] | n=103; breast cancer; 25-75-year-old | To evaluate the stigma and demographic influences, disease- related factors, psychosocial, self-efficacy, and how to adjust to breast cancer survivors. | Stigma from breast cancer survivors is related to breast asymmetry, belief in karma, and financial inadequacy. Support from family, health workers, and peer groups is a strength for cancer survivors. |
| Greer (2022); United States of America; cross-sectional [10] | n=418.754; all type of cancer; all ages range. | To explore the distance to facilities, race and ethnicity and radiotherapy acceptance and mortality | Patients who lived in rural areas must travel 3 times the distance compared to who lived in urban areas thus made them have fewer radiotherapy sessions and increased mortality. |
| Zeilani (2022); Jordan; cross-sectional [21] | n=13; all type of cancer; >18-year-old | To describe the experience of family support from the perspective of a cancer patient | Arabic culture where the family bears the burden of caring for the patient, religious and cultural practitioners give strength to the patient to undergo cancer therapy. |
| Liu (2022); China; cross-sectional [22] | n=16; pulmonary cancer; 36-73-year- old | To explore the factors that influence patient adherence to undergoing oral- targeted therapy | Lung cancer survivors experience many psychosocial pressures, such as stigma and belief in karma. Discomfort due to cancer and side effects of therapy are one of the factors that make patients give up on therapy. Patients need adequate information about therapy, including costs, to be able to make good decisions. |
| Moradi (2022); Canada; experimental [23] | N/A | To improve the schedule of radiotherapy centers and performance indicators | The development of machine algorithms can be carried out to predict the absence and punctuality of patients in the Patient Appointment Schedule (PAS) and prioritize patients with severe illness and delays in therapy |
| Suarilah (2022); Indonesia; cross-sectional [24] | n=15; obstetric and gynecological cancer; 18-65-year-old | To describe the narratives and experiences of Indonesian women diagnosed with obstetric and gynecological cancer in making therapeutic decisions | The majority have a passive role in the therapeutic decision-making process, whereas patients who are working and financially independent are more active in decision-making. Family support can be interpreted negatively by patients and hinder therapy. |
| Mesiti (2023); USA; cross-sectional [12] | n=800; colon cancer; 37-66-year-old | To explore the general public’s acceptance of immediate adjuvant chemotherapy for colon cancer | Individuals with long working hours, high levels of education and male sex have different tendencies in choosing therapy in terms of time, quality of life that is maintained, and side effects that occur. |
| Carmo (2023); Brazil; cross-sectional [16] | n=15; obstetric and gynecological cancer; 18-65-year-old | To describe the narratives and experiences of Indonesian women diagnosed with obstetric and gynecological cancer in making therapeutic decision | Trust in health workers increases expectations and acceptance for therapy. |
Discussion
Not all patients undergoing cancer therapy had accept and are willing to go through all the experiences and pain. Patients who have not experienced acceptance tend to feel hopeless halfway through and do not continue therapy. So that in measuring patient acceptance, it cannot be seen from the number of patients undergoing or receiving referral therapy but must approach psychosocial and in-depth interviews. One of the mechanisms carried out to foster acceptance in patients is through the intervention of acceptance and commitment therapy. Cancer patients have different backgrounds, knowledge, economic abilities, culture and beliefs of the people around them, thus, not all cancer patients have sufficient support from their surroundings to foster acceptance of therapy, so it is important to carry out measurable psychological interventions to encourage this acceptance [5] Acceptance of cancer therapy is a complex psychological reaction that is influenced by various factors that will be discussed in the next following topics.
Patient’s background
Low acceptance of multimodality therapy related to socio-economic factors including the insurance availability, range to the health facilities nearby, geographical factors, low level of education and income [3]. Older age, presence of comorbidities, and pessimistic personality are also barriers to acceptance of therapy. Patients with old age tend to prefer to maintain quality of life rather than prolong life and this is related to patient knowledge regarding the process and side effects of therapy [7]. In patients with lower of activities daily living tends to have a decreasing session on radiotherapy due to the benefits of radiotherapy outweigh the toxicity and uncomfortable side effects [8]. Patients who live in remote areas tend to refuse to undergo therapy due to the limitation of transportation and lodging costs and duration of therapy that interferes with work schedules [9,10]. Challenging geographical and the range to the facility for such patient who lived in rural areas especially who have lower incomes [11]. Patients with higher levels of education and working hours tend to be more likely to accept adjuvant chemotherapy plans that increase their expectancy and quality of life. Patients with high income tend to be more accepting of the possible side effects of adjuvant chemotherapy to increase their expectancy and quality of life [12]. The ability of patients to pay for costs associated with optimal universal health coverage. In Brazil, where 70% of the population depends on public insurance, thus, their radiotherapy units have increased in the last 10 year [13]. Spiritual beliefs can provide strength for patients and families in carrying out therapy, but some religious teachings also put pressure on the patient’s psychology, where the patient believes that he has cancer because of punishment and karma for something he did in the present or past life [14] causing the patient to blame themself [15]. Spiritual beliefs that emphasize the possibility of God’s miracle regardless of the patient’s condition and opportunity, can be a barrier to patient acceptance of palliative therapy, and make patients tend to choose aggressive therapy [16].
Patient’s perception and knowledge
Perception of body’s morphology also influences patients to refuse procedures that are considered damaging to their image, such as mastectomy which causes asymmetry and even loss of breasts in patients with breast cancer [15]. Perception of stigma regarding the causes of certain cancers, such as cervical cancer sufferers who are stigmatized as a disease caused by bad sexual behavior [25]. Patient knowledge about the therapy process, side effects of therapy, cost planning and treatment prognosis is very important to know [7]. The lack of knowledge about disease and therapy causes patients to fear cancer recurrence or the need for additional surgery, to think pain and side effects of therapy reduce quality of life and are disproportionate to the benefits of therapy, to feel too high-risk and not healthy enough to undergo therapy that is considered severe, and to fear Patients will burden their families both financially and physically in caring for patients, especially when they have to experience side effects from therapy [4]. Patients with more positive knowledge and perceptions of therapy think that therapy can increase life expectancy and quality of life, making it easier to cooperate in receiving therapy [12].
The influence from family and health workers
The patient’s tendency to trust the experiences of relatives or those around them who suffer from a similar illness can also affect the patient’s perception [23] especially the recommendations for the use of alternative therapies [21]. This is also influenced by factors of knowledge, culture, and low trust in health workers. Family support in the form of moral, affection, financial and facilities such as having a relative’s house near a therapy facility determines the patient’s preference [25]. Patients with adequate family and friend support tend to be more positive in receiving therapy. Therefore, it is important to provide a community where patients with similar illnesses and treatment plans can share and support one another [26].
Health workers play a major role in influencing patient acceptance of therapy. Both in terms of spiritual support, familiarity in the examination room, and good communication make patients feel comfortable and trust the recommendations of health workers. Patients feel the need to be explained repeatedly and involved in planning therapy by health workers [18]. Clear communication without language barriers, communication that respects the patient as well as explanations regarding the treatment plan and the results that the patient can expect during the therapy process builds trust between doctors and patients so that patients are more likely to accept recommendations from doctors [20]. In addition to communication, the knowledge of health workers regarding the conditions of patients who must be referred to cancer treatment facilities as well as the benefits of the therapy itself causes a referral bias which significantly reduces the number of patients who receive optimal therapy. Therefore, it is important for health workers to have good competence and empathy to foster patient trust [19].
Health policy and health facilities
Policies and provision of health facilities are external factors that influence patient decisions. State policies in providing health insurance, referral systems that make it easier for patients to receive therapy, policies in health facilities related to queuing and patient care capacity can support or even eliminate patient interest in receiving therapy [27].
Cancer therapy is not enough once done, so it takes more time and effort to receive therapy. Factors that affect the total duration of radiotherapy are facilities not operating all the time, where 48% of inactive days are caused by machine breakdown, power outages, and radiation adjustments. Another factor is the patient’s condition due to illness and side effects of therapy which makes it impossible to get radiotherapy on time. The absence of adjustments to the therapy schedule due to the closure of the facility on holidays was also a factor in the long duration of therapy. The number of patients who do not come to the therapy schedule also contributes to the accumulation of queues, but this can be overcome by increasing patient commitment and attention from health workers [17]. In addition to the length of the treatment period, the referral system policy and the number of cancer therapy facilities that have not been optimal are also a factor in the delay in therapy [28,29].
Effort to support patient acceptance
Acceptance is a psychological response that is shaped by a variety of complex factors, it is necessary to evaluate the views and basic conditions of the patient before intervening. However, from several studies that have been carried out, several efforts and suggestions were developed based on the results of the patient assessment in the study. The spiritual belief approach can be carried out by health workers, directing the patient to the necessary therapy involving elements of religion that the patient believes in, one of which is to prioritize spiritual peace in a good quality of life through palliative therapy rather than aggressive therapy [16].
Increasing patient knowledge and reducing patient fear of starting therapy can be done through good communication and treatment plans from health workers. In elderly patients who tend to feel that undergoing therapy has side effects that outweigh the benefits, health workers must be able to explain the safety of therapy. If the patient has high-risk cancer features, a palliative radiotherapy program can be immediately initiated or using single-fraction radiotherapy for palliative bone metastases to ensure that the benefits of radiotherapy outweigh the side effects [19].
The problem of patients not showing up and long queues does not only occur in Indonesia, but also in Canada, so researchers have started to create machine algorithms to determine patient queues. Reducing the duration of therapy can make patients prefer to carry out therapy, so that the number of therapy sessions is no longer a barrier in radiotherapy. Several studies have also begun to look at the use of artificial intelligence to process clinical data into machine algorithms to support diagnosis and treatment plans so as to increase the effectiveness of therapy [23].
The number of facilities that are lacking and difficult access is influenced by state policies. To be able to change state policies, both in procuring health equipment and resources and in improving health insurance, valid data is needed regarding the urgency of needing to change these policies. Research on the number of patients referred from the first health facility and finally receiving appropriate cancer therapy is urgently needed to become basic data for policy making. Lam et al. conducted interventions to increase the affordability of access to radiotherapy by paying for public transportation and providing radiotherapy services at a closer distance to patients [9]. However, in this study the number of patients undergoing therapy did not increase significantly, possibly due to the large influence of the inconvenience of therapy with all its side effects on patient refusal to undergo therapy [9].
Psychological interventions can also be carried out, one of which is with the concept of mindfulness, namely increasing awareness to focus on the present, and accepting all positive and negative experiences that occur. This concept also reduces the patient’s worries about the future and openness in dealing with the moments that occur in life. Patients who can accept all experiences that occur and focus on the present will more easily accept and commit to therapy, improve sleep quality, and quality of life. Because the complaints felt by cancer patients are not entirely from cancer symptoms and side effects of therapy, but also from anxiety and the behavior of patients who tend to avoid them. Therefore, it is important to treat cancer patients holistically, rather than symptom-based interventions [5].
Conclusion
Cancer can be a traumatic experience for the patient. A lot of stigmas about cancer seem to be a death sentence for someone even without a clear cause. Undergoing cancer therapy takes a long time and requires a lot of effort and costs not only for the patient, but also for his family members. As with other traumatic experiences, to be able to deal with cancer, patients must be able to accept the reality and experiences that they will experience, both good and bad. Although many factors influence a patient’s decision to accept cancer therapy, psychological acceptance is an important aspect as a basis for commitment and maintaining the patient’s quality of life while undergoing therapy. Therefore, a holistic approach needs to be applied to increase patient commitment to therapy.
Acknowledgments
The author would like to thank for the distinguished opportunity provided by the advisors of Faculty of Medicine, Universitas Syiah Kuala, Aceh, Indonesia and Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia.
Ethical approval
Not required.
Competing interests
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Underlying data
All data underlying the results are available as part of the article and no additional source data are required
How to cite
Novirianthy R, Syukri M, Gondhowiardjo S, et al. Treatment acceptance and its associated determinants in cancer patients: A systematic review. Narra J 2023; 3 (3): e197 - http://doi.org/10.52225/narra.v3i3.197.
References
- 1.Debela DT, Muzazu SGY, Heraro KD, et al. New approaches and procedures for cancer treatment: Current perspectives. SAGE Open Med 2021;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor S, Yorke J, Tsim S, et al. Impact on quality of life from multimodality treatment for lung cancer: A randomised controlled feasibility trial of surgery versus no surgery as part of multimodality treatment in potentially resectable stage III-N2 NSCLC (the PIONEER trial). BMJ Open Respir Res 2021;8(1):e000846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hao S, Mitsakos A, Irish W, et al. Differences in receipt of multimodality therapy by race, insurance status, and socioeconomic disadvantage in patients with resected pancreatic cancer. J Surg Oncol 2022;126(2):302–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puts MTE, Tapscott B, Fitch M, et al. A systematic review of factors influencing older adults’ decision to accept or decline cancer treatment. Cancer Treat Rev 2015;41(2):197–215. [DOI] [PubMed] [Google Scholar]
- 5.Hulbert-Williams NJ, Storey L, Wilson KG. Psychological interventions for patients with cancer: Psychological flexibility and the potential utility of acceptance and commitment therapy. Eur J Cancer Care (Engl) 2015;24(1):15–27. [DOI] [PubMed] [Google Scholar]
- 6.Lauwerier E, Caes L, Van Damme S, et al. Acceptance: What’s in a name? A content analysis of acceptance instruments in individuals with chronic pain. J Pain 2015;16(4):306–317. [DOI] [PubMed] [Google Scholar]
- 7.Puts MTE, Tapscott B, Fitch M, et al. A systematic review of factors influencing older adults’ decision to accept or decline cancer treatment. Cancer Treat Rev 2015;41(2):197–215. [DOI] [PubMed] [Google Scholar]
- 8.Yap ML, O’Connell DL, Goldsbury DE, et al. Actual versus optimal radiotherapy utilisation for metastatic cancer patients in the 45 and up study cohort, New South Wales. Clin Oncol 2021;33(10):650–660. [DOI] [PubMed] [Google Scholar]
- 9.Lam J, Cook T, Foster S, et al. Examining determinants of radiotherapy access: Do cost and radiotherapy inconvenience affect uptake of breast-conserving treatment for early breast cancer? Clin Oncol 2015;27(8):465–471. [DOI] [PubMed] [Google Scholar]
- 10.Greer MD, Amiri S, Denney JT, et al. Disparities in access to radiation therapy facilities among American Indians/Alaska natives and hispanics in Washington State. Int J Radiat Oncol Biol Phys 2022;112(2):285–293. [DOI] [PubMed] [Google Scholar]
- 11.Calaguas MJC, Gubat JA. South East Asia, Differing socioeconomic factors, differing access to radiotherapy: The Philippines, a microcosm. Semin Radiat Oncol 2017;27(2):176–183. [DOI] [PubMed] [Google Scholar]
- 12.Mesiti AM, Brouwer J, Jafari MD, et al. Assessment of attitudes toward initiation of immediate adjuvant chemotherapy for colon cancer. J Surg Res 2023;283:658–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanna SA, Gouveia AG, Moraes FY, et al. Lessons from the Brazilian radiotherapy expansion plan: A project database study. Lancet Reg Health Am 2022;14:100333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen SQ, Liu JE, Li Z, et al. The process of accepting breast cancer among Chinese women: A grounded theory study. Eur J Oncol Nurs 2017;28:77–85.nal Article [DOI] [PubMed] [Google Scholar]
- 15.Jin R, Xie T, Zhang L, et al. Stigma and its influencing factors among breast cancer survivors in China: A cross-sectional study. Eur J Oncol Nurs 2021;52:101972. [DOI] [PubMed] [Google Scholar]
- 16.dos Santos Carmo B, de Camargos MG, dos Santos Neto MF, et al. Relationship between religion/spirituality and the aggressiveness of cancer care: A scoping review. J Pain Symptom Manage 2023; 65(5):e425–e437. [DOI] [PubMed] [Google Scholar]
- 17.Stoker SD, Wildeman MA, Fles R, et al. A prospective study: Current problems in radiotherapy for nasopharyngeal carcinoma in Yogyakarta, Indonesia. PLoS One 2014;9(1):e85959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith SK, Nathan D, Taylor J, et al. Patients’ experience of decision-making and receiving information during radiation therapy: A qualitative study. Eur J Oncol Nurs 2017;30:97–106. [DOI] [PubMed] [Google Scholar]
- 19.Egger S, Smith DP, Brown B, et al. Urologists’ referral and radiation oncologists’ treatment patterns regarding high-risk prostate cancer patients receiving radiotherapy within 6 months after radical prostatectomy: A prospective cohort analysis. J Med Imaging Radiat Oncol 2020;64(1):134–143. [DOI] [PubMed] [Google Scholar]
- 20.Minichsdorfer C, Zeller O, Kirschbaum M, et al. Expectations and perception of cancer treatment goals in previously untreated patients. The EXPECT trial. Support Care Cancer. 2021. Jul;29(7):3585–3592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeilani RS, Abdalrahim MS, Hamash K, et al. The experience of family support among patients newly diagnosed with cancer in Jordan. Eur J Oncol Nurs 2022;60:102173. [DOI] [PubMed] [Google Scholar]
- 22.Liu T, Li N, Liu C, et al. A qualitative exploration of medication experience and factors contributing to adherence to oral-targeted therapy among lung cancer survivors. Semin Oncol Nurs 2022;38(6): 151352. [DOI] [PubMed] [Google Scholar]
- 23.Moradi S, Najafi M, Mesgari S, et al. The utilization of patients’ information to improve the performance of radiotherapy centers: A data-driven approach. Comput Ind Eng 2022;172. [Google Scholar]
- 24.Suarilah I, Nihayati HE, Wahyudi AS, et al. Treatment decision-making experience among Indonesian women with obstetrics and gynecology-related cancer. Medecine Palliative 2023;22(2):68–76. [Google Scholar]
- 25.Peterson CE, Silva A, Goben AH, et al. Stigma and cervical cancer prevention: A scoping review of the U.S. literature. Prev Med (Baltim) 2021;153. [DOI] [PubMed] [Google Scholar]
- 26.Dijkman BL, Luttik ML, Van der Wal-Huisman H, et al. Factors influencing family involvement in treatment decision-making for older patients with cancer: A scoping review. J Geriatr Oncol 2022;13(4):391–397. [DOI] [PubMed] [Google Scholar]
- 27.Mackenzie P, Vajdic C, Delaney G, et al. Radiotherapy utilisation rates for patients with cancer as a function of age: A systematic review. J Geriatr Oncol 2022;14:101387. [DOI] [PubMed] [Google Scholar]
- 28.Ikatan Dokter Indonesia. Penataan sistem pelayanan kesehatan rujukan. Available from: https://dinkes.jatimprov.go.id/userfile/dokumen/Sistem-Pelayanan-Rujukan.pdf. Accessed: 17 February 2023.
- 29.Octavianus S, Gondhowiardjo S.. Review review radiation therapy in Indonesia: Estimating demand as part of a national cancer control strategy. Appl Rad Oncol 2022;11(1):35–42. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required