Abstract
Bilateral traumatic dissections of the cervical internal carotid artery (ICA) are rare complications of polytrauma. A thorough literature review was performed, and data from selected studies were analyzed to assess the trends in clinical presentation, modes of trauma, management protocols, and clinical outcomes. The reported outcomes were categorized and graded into optimal, intermediate, and poor outcomes. We describe a rare case of bilateral dissection of ICA in a 31-year-old woman who was involved in a motor vehicle accident. She had a Glasgow Coma Scale score of 9 and right-sided hemiparesis. Radiological findings revealed left upper ICA dissection, arterial intramural thrombus, and stenosis of the upper segment of the right ICA. She improved on conservative management and had a good clinical outcome at a three-month follow-up. Emergency physicians must be knowledgeable about such cases, as more than half of these trauma victims are initially asymptomatic on initial presentation. Specific diagnostic and therapeutic modalities should be implemented based on low threshold clinical suspicion to avoid missing these potentially disabling injuries and reduce morbidity and mortality. Computed tomographic angiography is recommended in cases with atypical clinical presentations, unexplained neurological deficits, or delayed-onset clinical deterioration. While antiplatelet and anticoagulant therapies are the mainstays of conservative management, endovascular and surgical management are only used in severe cases when medical treatment has failed, the artery has been completely transected, or there is active bleeding. Generally, good outcomes were reported in about two-thirds of those patients.
Keywords: dissections, vascular dissection, traumatic brain injury, internal carotid artery, cervical
Introduction
Carotid artery dissection is a relatively rare condition, as the prevalence is between 2.5 and three per 100,000/year [1]. The segment of the internal carotid artery (ICA), which is located between the bifurcation of the common carotid artery and the base of the skull, is referred to as the cervical ICA [2]. Even though the ICA's location places it at a significant risk for injury due to its mobility and susceptibility to stretching, the majority of carotid artery dissections occur spontaneously, and only 4% of the reported dissections of the ICA are related to severe trauma [3,4]. The most common type of trauma is blunt trauma, which is typically caused by accidents involving motor vehicles and can disrupt one or more of the layers of the ICA [5,6]. Research studies have demonstrated that almost 1% to 2% of patients who suffered blunt trauma had extracranial traumatic vascular injuries, while the incidence of ICA injuries was between 0.08% and 0.33%. However, fortunately, 52%-79% of these injuries did not manifest any symptoms [7,8].
In most patients with ICA dissection, conservative medical treatment is sufficient for effective management [9]. However, on the other hand, endovascular and surgical interventions are required in a relatively small percentage of cases. The diagnosis of traumatic dissection of the ICA is frequently challenging and may be delayed because the presenting symptoms may be overlooked in the initial clinical assessment, particularly in the presence of other injuries [3]. Blunt bilateral traumatic dissections of the ICA are a very uncommon entity, as evidenced by the limited number of published case reports and series in the medical literature. However, highlighting such injuries is essential to improving the awareness of clinicians and the involved healthcare team, as it can effectively aid in increasing the suspicion index for diagnostic and treatment strategies, which in turn can reduce the associated morbidity and mortality of trauma patients. We report a rare case of bilateral dissection of ICA in a 31-year-old woman. Additionally, we compare the findings of our reported case with those of the 40 patients who were reported in 26 different papers in the literature to signify the importance of such injuries in terms of presentation, diagnosis, and management [10-36]. These studies from the literature were retrieved after conducting an intensive review and analysis of the available literature.
Case presentation
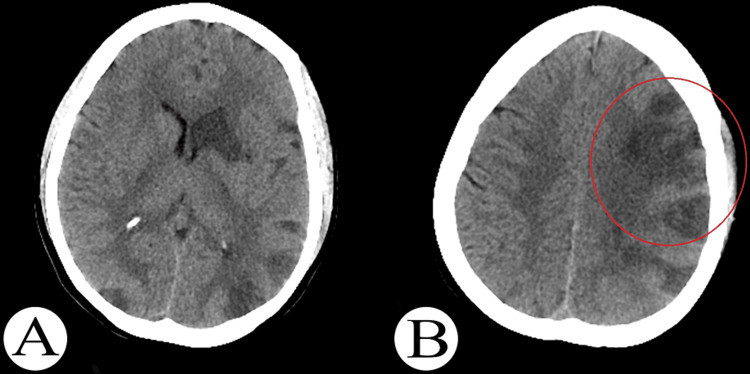
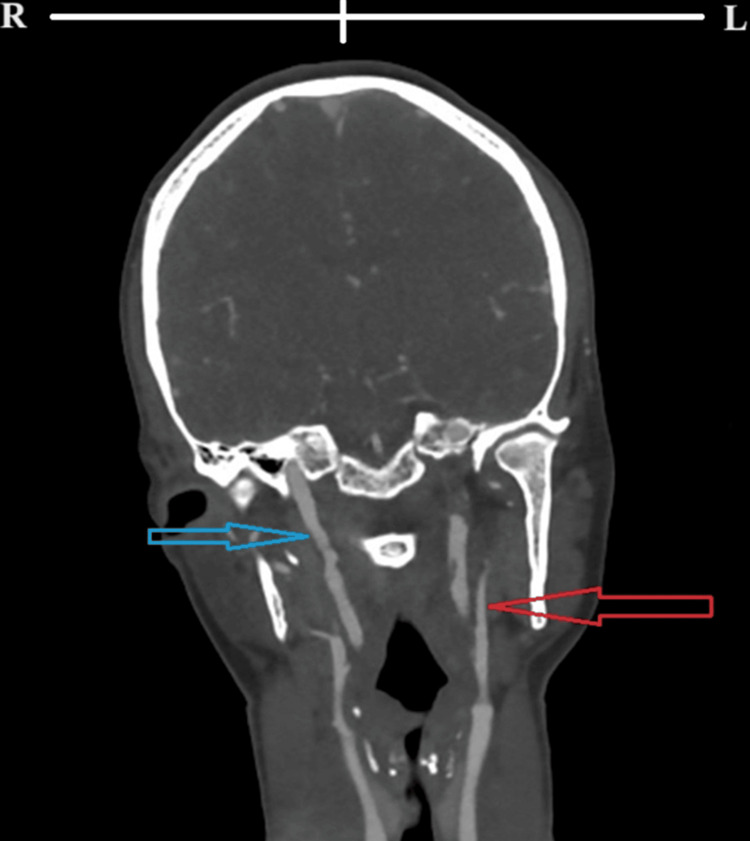
A 31-year-old woman was involved in a motor vehicle collision and was referred to our facility by a nearby hospital 24 hours after the incident. The patient's medical history was unremarkable, and she did not take any regular medications. On arrival, her vital signs were stable, and she had a Glasgow Coma Scale (GCS) score of 9/15. She was localizing to pain, opening her eyes in response to speech, and demonstrating no verbal response. She had grade 3 right-sided hemiparesis on the Medical Research Council scale for motor power. Cranial nerves were grossly intact. In addition, distal arterial pulsations were normal, and there were no signs of arterial ischemia in any of the extremities. Due to the patient's atypical presentation and unexplained neurological deficits, we proceeded from plain brain computed tomography (CT) to CT angiography, magnetic resonance imaging, and magnetic resonance arteriography. The images revealed left upper ICA dissection, arterial intramural thrombus, and stenosis of the upper segment of the right ICA. The skeletal examination revealed stable sacral and pubic rami fractures, and the abdomen CT scan revealed a low-grade liver injury (Figures 1A, 1B, 2).
Figure 1. (A, B) Initial post-traumatic axial computed tomography of the brain showing multiple bilateral hemispheric hypodense area multiple strokes (red circle).
Figure 2. Initial coronal computed tomography angiogram of the neck showing left upper cervical ICA dissection (red arrow) and evidence of arterial intramural thrombus, in addition to stenosis of the upper segment of right ICA (blue arrow) .
R: right side; L: left side; ICA: internal carotid artery
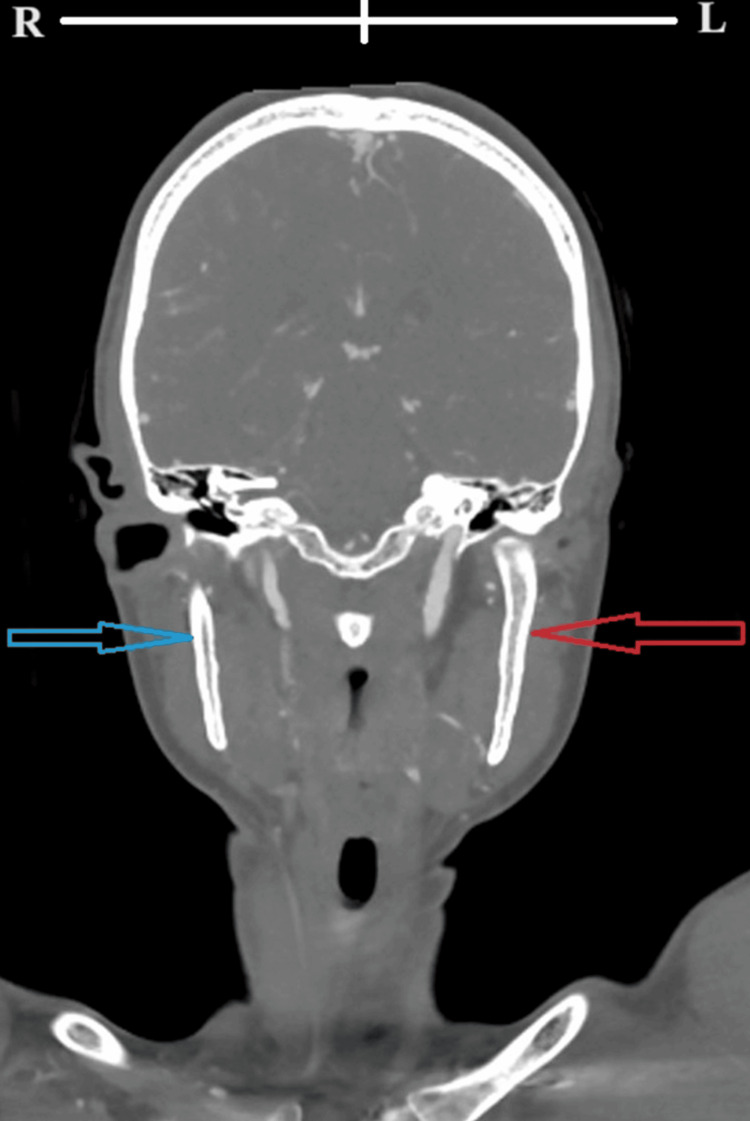
Antiplatelet therapy with aspirin 81 mg once daily and therapeutic subcutaneous doses of enoxaparin 6,000 IU twice daily for three months was initiated. Liver injury and fractures of the sacral and pubic rami were treated conservatively without complications. The patient's condition gradually improved under conservative care until she became fully awake, conscious, and verbally responsive. Both aphasia and right-sided hemiparesis improved gradually. She was discharged two weeks following admission. Before discharge, follow-up CT angiography revealed the disappearance of filling defects in the left internal artery and the persistence of stenosis in the upper right ICA (Figure 3). On a three-month follow-up, the patient showed no residual neurological deficits.
Figure 3. A follow-up coronal computed tomography angiogram of the neck showing normal left internal carotid artery (red arrow) and mild residual right internal carotid stenosis (blue arrow).
R: right; L: left
Discussion
The majority of ICA dissections are spontaneous [3]; however, there is limited clinical data on ICA dissections caused by trauma. Moreover, the bilateral occurrence of traumatic ICA dissections is exceedingly uncommon, and our current case is therefore regarded as an important addition to the current literature on this rare vascular disorder [37]. Our comprehensive review yielded information including clinical presentation, diagnosis, management strategies, and clinical outcomes.
While studying age and gender distribution among our study cases, we identified that four patients were under the age of 18 at the time of injury, 29 patients were between the ages of 18 and 40, and seven patients were older than 40 years. The average age of the patients studied was 31 years. Twenty-three of the patients in the study were female. Cranial nerve palsies, alone or in combination, were observed in 12 patients. The cranial nerve palsies most frequently reported were facial nerve palsy (nine patients), oculomotor nerve palsy (two patients), and glossopharyngeal nerve palsy (one patient).
Motor vehicle accidents were the leading cause of injury in almost 80% of 32 cases. Other causes reported of trauma were domestic violence (7.5%) and one case each of horse kicks, falling from a height, neck strangulation injury, chiropractic manipulation, and a private aircraft accident. Cronlein et al. reported that the sudden deceleration of motor vehicles is likely the cause of traumatic ICA dissections in restrained passengers [21]. While activation of the coagulation cascade, cerebral arterial dissection increases the risk of developing a thrombus as well as cerebral thromboembolism and ischemia [3,38,39]. The clinical presentation of observed cases was marked by substantial variation and discordance from being asymptomatic, having early neurological deficits, or having a clinical presentation with a delayed onset.
The group of asymptomatic patients, however, is quite challenging and is frequently identified by accident or overlooked. Patients typically exhibit no neurological deficits. Findings from our review of the literature revealed that almost 55% (22 patients) were initially asymptomatic, and among them, 17 were aged between 18 and 40 years. In seven asymptomatic patients, symptoms started between six and 12 hours; in nine patients, symptoms started between one and seven days; and in five patients, symptoms started one to six months following trauma. One patient had a delayed onset of symptoms, but the duration was not specified.
In the group of patients who presented with early symptoms, there were 18 patients (45%) with immediate post-traumatic symptoms or impairments. Hemiparesis (n = 15), pupillary changes, visual field cuts, cranial nerve palsies (n = 15), aphasia (n = 10), and coma (n = 4) were among the presenting symptoms. Headache, dizziness, neck pain, amaurosis fugax, pronator drift, hemi-hypoesthesia, Horner's syndrome, and incoordination were also reported as less frequent manifestations. The initial and delayed presentation of cases is demonstrated in Table 1.
Table 1. Initial and delayed presentation of cases.
| Author and year | Case No. | Initial clinical presentation | Delayed clinical presentation | Time between initial and delayed presentation |
| Malek AM, 2000 [10] | 1 | Asymptomatic | Rt hand & arm paresis, Dysphasia | 3months |
| 2 | Asymptomatic | Lt hand & arm paresis, Pronator drift | 3months | |
| 3 | Asymptomatic | Coma, Bilateral sensorimotor dysfunction, Aphasia | 6 months- 1 year | |
| Chang C, 2017 [11] | 4 | Asymptomatic | Hemiparesis, and Aphasia | 1week |
| Agarwal A, 2020 [12] | 5 | Asymptomatic | Lt sided weakness | 2week |
| Taoussi N, 2017 [13] | 6 | Asymptomatic | Motor dysphasia, Rt upper limb paresis | 8hours |
| Ballard JL, 1992 [14] | 7 | Asymptomatic | Rt (Facial palsy, Hemiparesis) and expressive aphasia | Few hours |
| Gabriel SA, 2019 [15] | 8 | Severe headache, Dizziness, Cervical pain, and Rt amaurosis fugax | Lt Hemiplegia, Aphasia, Dysphagia and Rt facial palsy | 48hours |
| Bajkó Z, 2016 [16] | 9 | Asymptomatic | hemiplegia, Hemi hypoesthesia | 12hours |
| Gioia S, 2019 [17] | 10 | Asymptomatic | Restless, Disorientation and aphasia | 1week |
| Thie A, 1993 [18] | 11 | Asymptomatic | Aphasia, Rt hemiparesis, Lt Horner’s syndrome | 7days |
| 12 | Asymptomatic | Left hemiparesis | 2days | |
| 13 | Coma, Midbrain syndrome | never recovered | 4hours | |
| 14 | Asymptomatic | Upper limb weakness | . | |
| 15 | Asymptomatic | Lt hemiparesis | 7hours | |
| 16 | Coma | Rt hemiparesis | 2days | |
| 17 | Asymptomatic | 9th nerve palsy | 1months | |
| 18 | Coma, Midbrain syndrome | Rt hemiparesis | 1months | |
| 19 | Asymptomatic | Upper limb weakness | 6days | |
| 20 | Coma | Lt hemiparesis | 12hours | |
| 21 | Asymptomatic | Iatrogenic coma with minor lateralizing signs | 2days | |
| Fanelli F, 2004 [19] | 22 | Hemiplegia | . | . |
| Chomel A, 2002 [20] | 23 | Asymptomatic | Lt hemiplegia | 1day |
| 24 | Asymptomatic | Drowsiness, Rt hemiparesis, Clonic convulsion of Rt upper limb, and Rt Horner syndrome | 6days | |
| Crönlein M, 2015 [21] | 25 | Severe headache | . | . |
| Duncan MA, 2000 [22] | 26 | Homonymous hemianopia, Hemiplegia and facial palsy | . | . |
| Petetta C, 2019 [23] | 27 | Traumatic shock condition, vital signs: pulse: 120 beats/min; blood pressure:60/40 mm Hg; and SpO2, 70%. | Mixed aphasia | 1week |
| Pittock SJ, 2001 [24] | 28 | facial palsy, Hemiparesis, Hemineglect syndrome | . | . |
| Yong RL and Heran NS, 2005 [25] | 29 | Dilated pupil | . | 48hours |
| Watridge CB, 1989 [26] | 30 | Aphasia and hemiparesis | . | . |
| Stringer LW, 1980 [27] | 31 | Asymptomatic | Confusion, Aphasia | 8hours |
| Storrow AB and Smith BA, 1995 [28] | 32 | Asymptomatic | Rt hemiparesis, Expressive aphasia | 12hours |
| Scherman BM, 1982 [29] | 33 | Asymptomatic | Hemiparesis | 6hours |
| Malin J-P, 1985 [30] | 34 | Asymptomatic | Rt hemiplegia and facial nerve paresis, Aphasia, Agraphia and dyslexia | 5months |
| Molacek J, 2010 [31] | 35 | Dilated pupils | Tonic-clonic seizure | 13days |
| Nadgir RN, 2003 [32] | 36 | Rt ptosis, Lt Facial palsy and paresthesia | Loss of coordination, hypoesthesia and involuntary movement of U and L limb and dysarthria | . |
| Robinson RG and Gwynne JF, 1978 [33] | 37 | Unconscious with right-sided weakness, Partial left ptosis | Deterioration of symptoms | 4days |
| de Borst GJ, 2006 [34] | 38 | Unconscious | Facial palsy, paralysis, hemianopia | Few days later |
| Friedenberg MJ, 1973 [35] | 39 | Hypotensive, Agitated, and confused with constricted pupils | . | . |
| Fukuda I, 1989 [36] | 40 | Shock, and cyanotic extremities | . | . |
There are numerous diagnostic imaging modalities for assessing vessel dissection [21]. CT scans and CT angiography are primarily used to diagnose cerebral vascular pathologies in emergencies. String signs, lupus constrictions, and arterial hypertension are regarded as indirect indicators of an artery dissection [38]. In the reported cases, various diagnostic techniques were utilized to confirm the diagnosis. In 17 cases, carotid angiography was the most frequently used imaging modality, followed by CT angiography in 15 cases (Table 2).
Table 2. Neurovascular imaging findings in the reviewed articles.
DSA: Digital Subtraction Angiography; CT: Computed tomography; MRA: Magnetic resonance angiography; ICA: Internal carotid artery
| Author and year | Case No. | Brain images findings | Vascular image types- findings |
| Malek AM, 2000 [10] | 1 | Hemispheric embolic infarction | Digital Subtraction Angiography (DSA)-Bilateral symmetrical focal stenoses in ICA at C2-C3 level |
| 2 | Opercular infarction | Digital Subtraction Angiography (DSA)-Bilateral symmetrical focal stenosis in ICA at C2-3 level | |
| 3 | Bilateral frontal infarctions watershed distribution | Digital Subtraction Angiography (DSA)-Lt: extracranial ICA occlusion; Rt: extracranial ICA chronic dissection | |
| Chang C, 2017 [11] | 4 | Sub insular cortex and lentiform nucleus infarction | MRA-Bilateral extracranial internal carotid artery dissections with aneurysms formation |
| Agarwal A, 2020 [12] | 5 | caudate nucleus, Insula, and parietal lobes infarction | CTA-Dissection of bilateral distal cervical ICA |
| Taoussi N, 2017 [13] | 6 | Frontal lobe infarction | CTA-Bilateral occlusion of the ICA |
| Ballard JL, 1992 [14] | 7 | Posterior fronto-parietal infarction | Carotid Angiography-Bilateral ICA dissections above bifurcations and extending to skull base |
| Gabriel SA, 2019 [15] | 8 | corona radiata infarction | Carotid Angiography-String sign in the distal Rt and Lt internal carotid arteries |
| Bajkó Z, 2016 [16] | 9 | MCA infarction | Ultrasound examination of the carotid arteries-Rt ICA: a high-resistance flow signal, without stenotic lesions at the proximal level, suggestive of significant distal stenosis or occlusion, Lt ICA: irregular stenosis caused by a hypoechoic mural thickening, suggestive of a mural hematoma secondary to dissection |
| Gioia S, 2019 [17] | 10 | Cortical-subcortical infarction | CTA-Bilateral dissection of the extracranial internal carotid arteries |
| Thie A, 1993 [18] | 11 | . | Angiography-Bilateral carotid artery stenosis |
| 12 | . | Angiography-Bilateral aneurysm at base of the skull | |
| 13 | . | Angiography-Bilateral stenosis of extracranial internal carotid | |
| 14 | . | Angiography-Rt stenosis at C1/C2, Lt not done; filling of left anterior cerebral artery from right ICA raised suspicion of left ICA lesion | |
| 15 | . | Angiography-Rt stenosis at C2, Lt occlusion at C2. | |
| 16 | . | Angiography-Rt stenosis at the base of the skull, Lt aneurysm | |
| 17 | . | Angiography-Bilateral carotid artery stenosis | |
| 18 | . | Angiography-Bilateral carotid artery stenosis | |
| 19 | . | Angiography-Bilateral carotid artery stenosis | |
| 20 | . | Angiography- Rt: Occlusion at base of the skull, Lt: stenosis and two aneurysms at base of the skull | |
| 21 | . | Angiography-Rt: tapering occlusion at C2, Lt: occlusion and aneurysm at base of the skull | |
| Fanelli F, 2004 [19] | 22 | Hemispheric infarction | DSA-Rt: dissection and obstruction of the right ICA with its reconstitution at the level of the intracranial tract, Lt: pseudoaneurysm associated with the dissection of the left ICA. |
| Chomel A, 2002 [20] | 23 | Frontal, Peduncular and capsular infarction. | CTA-Rt internal carotid dissection up to the entrance in the carotid channel, and Lt internal carotid dissection with pseudoaneurysm |
| 24 | Caudate nucleus infarction | CTA-Lt: dissection of the left ICA with extension to the intracranial segment, Rt: dissection of the right ICA just below the petrosal bone with false aneurysm. | |
| Crönlein M, 2015 [21] | 25 | Bi-hemispheric, mainly left-sided infarction | CTA-Bilateral internal carotid artery dissection |
| Duncan MA, 2000 [22] | 26 | parietal lobe infarction | CTA-bilateral ICA dissection, fibromuscular dysplasia of the ICAs and thrombus in Rt ICA |
| Petetta C, 2019 [23] | 27 | Multiple extensive ischemic areas in the frontal region and circumscribed lesions in the parietal region bilaterally, in the left occipital region, and in the left thalamic site. | CTA-Bilateral internal carotid artery dissection |
| Pittock SJ, 2001 [24] | 28 | Anterior cerebral artery territory infarction | Digital Subtraction Angiography (DSA)-Bilateral internal carotid artery dissection |
| Yong RL and Heran NS، 2005 [25] | 29 | Bi-cerebellar hemispheres infarction, Rt parietal, and Lt frontal subcortical white matter infarction. | CTA-Bilateral internal carotid artery dissection |
| Watridge CB, 1989 [26] | 30 | Normal | CTA-Bilateral internal carotid artery dissection |
| Stringer LW, 1980 [27] | 31 | Normal | CTA-Bilateral internal carotid artery dissection |
| Storrow AB and Smith BA, 1995 [28] | 32 | Parietal region infarction | CTA-Bilateral internal carotid artery dissection |
| Scherman BM, 1982 [29] | 33 | . | Carotid Arteriography-Bilateral internal carotid artery dissection |
| Malin J-P, 1985 [30] | 34 | Hemispheric infarction | Carotid angiography-Bilateral internal carotid artery dissection |
| Molacek J, 2010 [31] | 35 | . | CTA-Bilateral internal carotid artery dissection |
| Nadgir RN, 2003 [32] | 36 | Thalamic infarction | MRA-Bilateral internal carotid artery dissection |
| Robinson RG and Gwynne JF, 1978 [33] | 37 | Parietal and occipital areas, Internal capsule, and basal ganglia infarction | Arteriogram-Bilateral ICAs were thrombosed from about 2 cm above the common carotid artery bifurcations. |
| de Borst GJ, 2006 [34] | 38 | Cerebral hemisphere and anterior cerebral artery infarction | CTA-Bilateral stenosis of extracranial internal carotid artery |
| Friedenberg MJ, 1973 [35] | 39 | . | Angiogram-Bilateral internal carotid arteries occlusion |
| Fukuda I, 1989 [36] | 40 | Frontal and occipital lobe infarction | CTA and DSA-Bilateral internal carotid artery dissection |
Anticoagulants and antiplatelet medications were used to treat most patients [3,40], eight underwent endovascular procedures, and three underwent surgery after medical treatment failed (Tables 3, 4). Cerebrovascular dissections can be treated with open surgical methods like microvascular suturing, extracranial-intracranial bypass, and thromboendarterectomy, or endovascular methods like stenting, stent-assisted intravascular thrombolysis, and thrombectomy [3,38]. Surgical and endovascular alternatives are used in the most severe and critical clinical situations [40], in cases with complete arterial transactions, and after medical treatment fails [41].
Table 3. Summary of the medical and surgical interventions of 40 patients in the reviewed articles.
| Type of management | Specified management | Frequency | Percent | |
| Medical management | Antiplatelets / Anticoagulant | 29 | 72.5 | |
| Not mentioned | 11 | 27.5 | ||
| Surgical interventions | Endovascular intervention | 8 | 20 | |
| Emergency operation | 3 | 7.5 | ||
Table 4. Management details and clinical outcomes of 40 patients in the reviewed articles.
| Author and year | Case No. | Management (Medical) | Management (Intervention) | Time of last follow up | Radiological outcome | Clinical outcome |
| Malek AM, 2000 [10] | 1 | Clopidogrel (75 mg daily) or ticlopidine hydrochloride-before the procedure, and daily aspirin. | Angioplasty and stent placement | 8months | Persistent patency of the stented Lt ICA with no evidence of intimal hyperplasia or mismatch with the native artery | Sustained retroperitoneal hemorrhage |
| 2 | Clopidogrel (75 mg daily) or ticlopidine hydrochloride-before the procedure, and daily aspirin. | Percutaneous Balloon Angioplasty | 20months | . | Asymptomatic, no further neurological deficits. | |
| 3 | Anticoagulation therapy consisting of heparin, later changed to warfarin. | . | 3monhs | . | Persistent paralyzed right upper extremity and weak left U & L extremity, mild dysphasia. | |
| Chang C, 2017 [11] | 4 | Aspirin initially | Carotid Wallstent endoprostheses | 1week | . | Recovered |
| Agarwal A, 2020 [12] | 5 | Antiplatelets (aspirin, clopidogrel) and physiotherapy | . | 2week | . | Improved MRC 3/5 |
| Taoussi N, 2017 [13] | 6 | Clexane and LMWH, warfarin after 7 days and continued for 6 months | . | . | . | Improvement with minor dysphasia |
| Ballard JL, 1992 [14] | 7 | Heparin | Rt side revascularization, Autologous right, ICA bypass | 15months | Widely patent Rt graft and return the intracerebral flow to normal | Recovered |
| Gabriel SA, 2019 [15] | 8 | Antiplatelets (aspirin) , therapeutic intravenous heparin followed by warfarin for 6 months | . | . | . | Improvement with minor dysphasia and dyslalia |
| Bajkó Z, 2016 [16] | 9 | Aspirin and LMWH as prophylactic doses (initially, and 3 weeks following emergency decompressive craniotomy due to ischemic event) | . | . | . | Improved |
| Gioia S, 2019 [17] | 10 | Heparin then followed by warfarin | . | . | . | Recovered |
| Thie A, 1993 [18] | 11 | 2 Patients received anticoagulant drugs during the acute phase | . | . | . | hemiparesis |
| 12 | . | . | . | . | hemiparesis | |
| 13 | . | . | . | . | Death | |
| 14 | . | . | . | . | No deficits | |
| 15 | . | . | . | . | Death | |
| 16 | . | . | . | . | Death | |
| 17 | . | . | . | . | No deficits | |
| 18 | . | . | . | . | hemiparesis | |
| 19 | . | . | . | . | No deficits | |
| 20 | . | . | . | . | hemiparesis | |
| 21 | . | . | . | . | Slight cognitive impairment | |
| Fanelli F, 2004 [19] | 22 | Heparin before procedure, discharge on ticlopidine and LMWH | Carotid Wallstent endoprostheses | 13months | Good recanalization of the right ICA | Mild Lt arm weakness |
| Chomel A, 2002 [20] | 23 | Anticoagulant: 2 weeks of heparin, followed by LMWH as prophylactic use. Ten days later, antiplatelet drugs were introduced. | . | 1month | Persistent, localized stenosis of the right internal carotid with a false aneurysm. The left internal carotid was normal. | hemiplegia |
| 24 | Anticoagulant: 2 weeks of heparin, followed by LMWH (Therapeutic)+ 10 days of preventive use of LMWH, and long-term antiplatelet | . | . | Normalization of the left internal carotid artery | Recovered | |
| Crönlein M, 2015 [21] | 25 | Heparin | Angioplasty | 6months | Improved | Improved |
| Duncan MA, 2000 [22] | 26 | Aspirin, then heparin which changed to warfarin | . | . | . | faciobrachial palsy |
| Petetta C, 2019 [23] | 27 | Therapeutic enoxaparin | . | 1year | . | hemiparesis |
| Pittock SJ, 2001 [24] | 28 | IV heparin, Oral warfarin | . | 1year | . | Improved |
| Yong RL and Heran NS, 2005 [25] | 29 | Heparin infusion followed by warfarin | . | 1year | Improved | Recovered |
| Watridge CB, 1989 [26] | 30 | Heparin | . | 6months | Recanalization of the dissected left internal carotid artery and near-normal healing of the right internal carotid artery. | Mildly hand weakness and mild expressive aphasia |
| Stringer LW, 1980 [27] | 31 | Heparin started and replaced gradually with warfarin | . | <1year | . | Recovered |
| Storrow AB and Smith BA, 1995 [28] | 32 | Warfarin | . | . | Slight improvement in both internal carotid narrowing. | Recovered |
| Scherman BM, 1982 [29] | 33 | Heparin | Endovascular (Fogarty catheter) | . | . | Death |
| Malin J-P, 1985 [30] | 34 | . | . | 5months | Improved | Recovered |
| Molacek J, 2010 [31] | 35 | . | Stents insertion into both ICAs | 22days | Improved | Recovered |
| Nadgir RN, 2003 [32] | 36 | Heparin, discharged coumadin and aspirin. | . | Few weeks later | Improved | Recovered |
| Robinson RG and Gwynne JF, 1978 [33] | 37 | . | Rt mid-temporal burr hole was made under local anesthesia, there was no hematoma, the brain was not under tension, and when the left temporal horn of the ventricle was tapped, the fluid was clear and at low pressure. | . | No difference | Death |
| de Borst GJ, 2006 [34] | 38 | LMWH for 1 week, followed by antiplatelet therapy (carbasalate calcium) | . | 6months | Improved | Recovered |
| Friedenberg MJ, 1973 [35] | 39 | Heparin, Digitalis, followed by coumadin | . | 53days | Improved | Recovered |
| Fukuda I, 1989 [36] | 40 | Heparin | Emergency operation including vessels occlusion and ligation | 6months | Improved | Recovered |
We reviewed the available literature and classified the reported clinical outcomes as good outcomes when there had been complete recovery or only mild neurological deficits, intermediate outcomes when there was hemiparesis, and poor outcomes when there were severe permanent deficits or death. Overall, among all 40 patients assessed, optimal, intermediate, and poor outcomes were observed in 25, eight, and seven patients, respectively, and in total, seven mortalities were noted (Table 4). Among 22 initially asymptomatic patients, optimal, intermediate, and poor outcomes were reported in 14, five, and three patients, respectively. In this group, one mortality was observed. On the other hand, among 18 initially symptomatic patients, optimal, intermediate, and poor outcomes were encountered in 11, three and four patients, respectively, and in this cohort, four mortalities were reported. In our case, we observed optimal clinical and radiological outcomes.
Conclusions
Bilateral traumatic dissections of the extracranial cervical ICA occur in polytraumatized patients, and more than half of these cases are initially asymptomatic on initial presentation. Specific diagnostic and therapeutic modalities should be implemented based on low threshold clinical suspicion in order to avoid missing these potentially disabling injuries and reduce morbidity and mortality. CT angiography is recommended in cases with atypical clinical presentations, unexplained neurological deficits, or delayed-onset clinical deterioration. Antiplatelet and anticoagulant therapies are the mainstays of conservative management. Endovascular and surgical management are only used in severe cases when medical treatment has failed, the artery has been completely transected, or there is active bleeding. Generally, optimal outcomes were reported in about two-thirds of those patients. A multidisciplinary management approach is mandatory in this rare type of injury.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Alshaymaa Arishy, Yahya H. Khormi, Atheer I. Darraj, Seham O. Abuzahirah, Mostafa Atteya
Acquisition, analysis, or interpretation of data: Alshaymaa Arishy, Yahya H. Khormi, Atheer I. Darraj, Seham O. Abuzahirah, Mostafa Atteya
Drafting of the manuscript: Alshaymaa Arishy, Yahya H. Khormi, Atheer I. Darraj, Seham O. Abuzahirah, Mostafa Atteya
Critical review of the manuscript for important intellectual content: Alshaymaa Arishy, Yahya H. Khormi, Atheer I. Darraj, Seham O. Abuzahirah, Mostafa Atteya
Supervision: Alshaymaa Arishy, Yahya H. Khormi, Atheer I. Darraj, Seham O. Abuzahirah, Mostafa Atteya
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Rare case of bilateral traumatic internal carotid artery dissection. Jenkins JM, Norton J, Hampton T, Weeks R. BMJ Case Rep. 2016;2016:0. doi: 10.1136/bcr-2016-217262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Endovascular treatment of blunt injury of the extracranial internal carotid artery: the prospect and dilemma. Wang G, Li C, Piao J, Xu B, Yu J. Int J Med Sci. 2021;18:944–952. doi: 10.7150/ijms.50275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blunt traumatic extracranial cerebrovascular injury and ischemic stroke. Foreman PM, Harrigan MR. Cerebrovasc Dis Extra. 2017;7:72–83. doi: 10.1159/000455391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Traumatic dissection of the carotid artery: challenges for diagnostics and therapy illustrated by a case example (Article in German) Jansen G, Popp J, Dietrich U, Mertzlufft F, Bach F. Anaesthesist. 2013;62:817–823. doi: 10.1007/s00101-013-2243-1. [DOI] [PubMed] [Google Scholar]
- 5.What are the expected findings on follow-up computed tomography angiogram in post-traumatic patients with blunt cerebrovascular Injury? Elbanna KY, Mohammed MF, Choi JI, et al. Can Assoc Radiol J. 2018;69:266–276. doi: 10.1016/j.carj.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Blunt cerebrovascular injury in elderly fall patients: are we screening enough? Anto VP, Brown JB, Peitzman AB, et al. World J Emerg Surg. 2018;13:30. doi: 10.1186/s13017-018-0188-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.An update in imaging of blunt vascular neck injury. Abu Mughli R, Wu T, Li J, et al. Can Assoc Radiol J. 2020;71:281–292. doi: 10.1177/0846537120909468. [DOI] [PubMed] [Google Scholar]
- 8.Blunt traumatic vascular injuries of the head and neck in the ED. George E, Khandelwal A, Potter C, Sodickson A, Mukundan S, Nunez D, Khurana B. Emerg Radiol. 2019;26:75–85. doi: 10.1007/s10140-018-1630-y. [DOI] [PubMed] [Google Scholar]
- 9.Endovascular stenting for the treatment of traumatic internal carotid injuries: expanding experience. DuBose J, Recinos G, Teixeira PG, Inaba K, Demetriades D. J Trauma. 2008;65:1561–1566. doi: 10.1097/TA.0b013e31817fd954. [DOI] [PubMed] [Google Scholar]
- 10.Patient presentation, angiographic features, and treatment of strangulation-induced bilateral dissection of the cervical internal carotid artery. Report of three cases. Malek AM, Higashida RT, Halbach VV, et al. J Neurosurg. 2000;92:481–487. doi: 10.3171/jns.2000.92.3.0481. [DOI] [PubMed] [Google Scholar]
- 11.Traumatic dissections of bilateral internal carotid artery with aneurysms formation. Chang C, Tsai I, Liang C, et al. Hong Kong J Emerg Med. 2016;23:285–288. [Google Scholar]
- 12.Delayed bilateral internal carotid artery dissection following motor vehicle accident: time to make its screening a part of trauma protocol? Agarwal A, Yadav D, Gupta A, et al. QJM. 2020;113:672–673. doi: 10.1093/qjmed/hcaa037. [DOI] [PubMed] [Google Scholar]
- 13.Traumatic bilateral dissection of cervical internal carotid artery in the wake of a car accident: a case report. Taoussi N, Alghamdi AJ, Bielewicz J, Luchowski P, Rejdak K. Neurol Neurochir Pol. 2017;51:432–438. doi: 10.1016/j.pjnns.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Bilateral traumatic internal carotid artery dissections: case report. Ballard JL BT, Fitzpatrick B, Malone JM. J Vasc Surg. 1992;15:431–435. [PubMed] [Google Scholar]
- 15.Bilateral traumatic internal carotid artery dissection after crossfit training. Gabriel SA, Beteli CB, Aluize de Menezes E, et al. Ann Vasc Surg. 2019;61:466–465. doi: 10.1016/j.avsg.2019.04.028. [DOI] [PubMed] [Google Scholar]
- 16.Malignant middle cerebral artery infarction secondary to traumatic bilateral internal carotid artery dissection. A case report. Bajkó Z, Bălaşa R, Moţăţăianu A, Bărcuţean L, Stoian A, Stirbu N, Maier S. J Crit Care Med (Targu Mures) 2016;2:135–141. doi: 10.1515/jccm-2016-0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.A case of bilateral extracranial internal carotid artery dissection due to the helmet strap after motorcycle crash. Gioia S, Franceschetto L, Lancia M, Bacci M, Suadoni F. Am J Forensic Med Pathol. 2019;40:153–155. doi: 10.1097/PAF.0000000000000458. [DOI] [PubMed] [Google Scholar]
- 18.Bilateral blunt traumatic dissections of the extracranial internal carotid artery: report of eleven cases and review of the literature. Thie A, Hellner D, Lachenmayer L, et al. Cerebrovascul Dis. 1993;3:295–303. [Google Scholar]
- 19.Stent repair of bilateral post-traumatic dissections of the internal carotid artery. Fanelli F, Salvatori FM, Ferrari R, Pacella S, Rossi P, Passariello R. J Endovasc Ther. 2004;11:517–521. doi: 10.1583/04-1207.1. [DOI] [PubMed] [Google Scholar]
- 20.Traumatic bilateral dissections of the internal carotid artery: an infrequent diagnosis not to be missed. Chomel A, Vernet M, Lile A, Messant I, Combes JC, Freysz M. J Neurosurg Anesthesiol. 2002;14:309–312. doi: 10.1097/00008506-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Traumatic bilateral carotid artery dissection following severe blunt trauma: a case report on the difficulties in diagnosis and therapy of an often overlooked life-threatening injury. Crönlein M, Sandmann GH, Beirer M, Wunderlich S, Biberthaler P, Huber-Wagner S. Eur J Med Res. 2015;20:62. doi: 10.1186/s40001-015-0153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Traumatic bilateral internal carotid artery dissection following airbag deployment in a patient with fibromuscular dysplasia. Duncan MA, Dowd N, Rawluk D, Cunningham AJ. Br J Anaesth. 2000;85:476–478. doi: 10.1093/bja/85.3.476. [DOI] [PubMed] [Google Scholar]
- 23.Forensic and clinical issues in a case of motorcycle blunt trauma and bilateral carotid artery dissection. Petetta C, Santovito D, Tattoli L, Melloni N, Bertoni M, Di Vella G. Ann Vasc Surg. 2020;64:409–406. doi: 10.1016/j.avsg.2019.10.049. [DOI] [PubMed] [Google Scholar]
- 24.Traumatic bilateral carotid dissection with concomitant cerebral infarction. Pittock SJ, Moroney JT, Alexander M, et al. J Emerg Med. 2001;20:33–38. doi: 10.1016/s0736-4679(00)00284-5. [DOI] [PubMed] [Google Scholar]
- 25.Traumatic carotid cavernous fistula with bilateral carotid artery and vertebral artery dissections. Yong RL, Heran NS. Acta Neurochir (Wien) 2005;147:1109–1113. doi: 10.1007/s00701-005-0604-5. [DOI] [PubMed] [Google Scholar]
- 26.Traumatic carotid artery dissection: diagnosis and treatment. Watridge CB, Muhlbauer MS, Lowery RD. J Neurosurg. 1989;71:854–857. doi: 10.3171/jns.1989.71.6.0854. [DOI] [PubMed] [Google Scholar]
- 27.Traumatic dissection of the extracranial internal carotid artery. Stringer WL, Kelly DL Jr. Neurosurgery. 1980;6:123–130. doi: 10.1227/00006123-198002000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Traumatic bilateral carotid dissection. Storrow AB, Smith BA. J Emerg Med. 1995;13:169–174. doi: 10.1016/0736-4679(94)00138-3. [DOI] [PubMed] [Google Scholar]
- 29.Bilateral traumatic thrombosis of the internal carotid arteries in the neck: a case report with review of the literature. Scherman BM, Tucker WS. Neurosurgery. 1982;10:751–753. doi: 10.1227/00006123-198206010-00014. [DOI] [PubMed] [Google Scholar]
- 30.Bilateral traumatic extracranial aneurysms of the internal carotid artery with delayed brain infarction. Malin JP, Becker H, Abicht J. J Neurol. 1985;232:314–317. doi: 10.1007/BF00313873. [DOI] [PubMed] [Google Scholar]
- 31.Bilateral post-traumatic carotid dissection as a result of a strangulation injury. Molacek J, Baxa J, Houdek K, Ferda J, Treska V. Ann Vasc Surg. 2010;24:1133–1111. doi: 10.1016/j.avsg.2010.02.042. [DOI] [PubMed] [Google Scholar]
- 32.Simultaneous bilateral internal carotid and vertebral artery dissection following chiropractic manipulation: case report and review of the literature. Nadgir RN, Loevner LA, Ahmed T, Moonis G, Chalela J, Slawek K, Imbesi S. Neuroradiology. 2003;45:311–314. doi: 10.1007/s00234-003-0944-x. [DOI] [PubMed] [Google Scholar]
- 33.Bilateral internal carotid artery thrombosis after closed head injury. Robinson RG, Gwynne JF. Acta Neurochir (Wien) 1978;44:137–142. doi: 10.1007/BF01401637. [DOI] [PubMed] [Google Scholar]
- 34.Bilateral traumatic carotid artery dissection in a child. de Borst GJ, Slieker MG, Monteiro LM, Moll FL, Braun KP. Pediatr Neurol. 2006;34:408–411. doi: 10.1016/j.pediatrneurol.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 35.Bilateral incomplete traumatic occlusion of internal carotid arteries. Friedenberg MJ, Lake P, Landau S. Am J Roentgenol Radium Ther Nucl Med. 1973;118:546–549. doi: 10.2214/ajr.118.3.546. [DOI] [PubMed] [Google Scholar]
- 36.Traumatic disruption of bilateral vertebral arteries and internal carotid arteries: case report. Fukuda I, Meguro K, Matsusita S, Shigeta O, Oohashi N, Nakata Y. J Trauma. 1989;29:263–266. doi: 10.1097/00005373-198902000-00025. [DOI] [PubMed] [Google Scholar]
- 37.Juvenile stroke: cervical artery dissection in a patient after a polytrauma. Marschner-Preuth N, Warnecke T, Niederstadt TU, Dittrich R, Schäbitz WR. Case Rep Neurol. 2013;5:21–25. doi: 10.1159/000347001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Current optimal assessment and management of carotid and vertebral spontaneous and traumatic dissection. Mohan IV. Angiology. 2014;65:274–283. doi: 10.1177/0003319712475154. [DOI] [PubMed] [Google Scholar]
- 39.Traumatic dissection of the internal carotid artery following whiplash injury. Diagnostic workup and therapy of an often overlooked but potentially dangerous additional vascular lesion (Article in German) Lenz M, Bula-Sternberg J, Koch T, Bula P, Bonnaire F. Unfallchirurg. 2012;115:369–376. doi: 10.1007/s00113-011-2130-7. [DOI] [PubMed] [Google Scholar]
- 40.Long-term outcomes of internal carotid artery dissection. Rao AS, Makaroun MS, Marone LK, Cho JS, Rhee R, Chaer RA. J Vasc Surg. 2011;54:370–374. doi: 10.1016/j.jvs.2011.02.059. [DOI] [PubMed] [Google Scholar]
- 41.Traumatic dissection of the common carotid artery after blunt injury to the neck. Okada Y, Shima T, Nishida M, et al. Surg Neurol. 1999;51:513–519. doi: 10.1016/s0090-3019(98)00102-5. [DOI] [PubMed] [Google Scholar]