Abstract
Tuberculum sellae meningiomas commonly present as bitemporal hemianopia and loss of visual acuity due to optic nerve compression. Two female patients (48 and 58 years old) presented with a small scotoma at the lower visual field center due to tuberculum sellae meningioma (25 and 10 mm, respectively). Despite the fact that their visual field defect was not very large, daily activities, including walking or reading were hindered. By the total removal of the tumors in both patients, the scotoma was cured and daily activities recovered. When patients exhibit visual deficits, especially in the lower center fields, surgical removal should be considered even if the tumors are small and visual deficits are limited because improvement of both vision and daily activities can be achieved.
Keywords: removal, scotoma, tuberculum sellae meningioma, visual disturbance
Introduction
Tuberculum sellae meningiomas commonly present bitemporal hemianopia and loss of visual acuity, of which 60%-80% can be improved by surgical removal.1-4) Meanwhile, the surgical outcome of central visual deficits as atypical visual symptoms is largely unknown. To date, only three studies have reported central visual deficits due to tuberculum sellae meningiomas.5-7) Among them, visual outcome, which was unfavorable, was described only in one patient in a Japanese article.6) Here we report the surgical outcome of two patients with tuberculum sellae meningiomas who presented with scotoma at the lower visual field center.
Case Report 1
A 48-year-old female experienced difficulty in walking and reading words on her cellular phone, which progressed over three months. After visiting a nearby ophthalmologist, she was referred to our department because of her visual field deficits. Goldman visual field test revealed a scotoma at the lower visual field center in her right eye (Fig. 1A and B). Brain magnetic resonance imaging (MRI) revealed tuberculum sellae meningioma (Fig. 1C and D). The tumor size was 25 mm and grew symmetrically to compress the bilateral optic nerves. Intraoperative finding via the interhemispheric approach was that the tumor widely compressed the bilateral optic nerves and chiasm, and no adhesion was found between them. Since dissection of the bilateral falciform ligaments revealed no tumor invasion inside the optic canal, the canal was not opened. The tumor was completely removed (Simpson grade II) using an interhemispheric approach (Fig. 2A and B). Her scotoma was cured postoperatively (Fig. 2C and D), and she recovered to work soon. The pathological diagnosis was meningothelial meningioma.
Fig. 1.
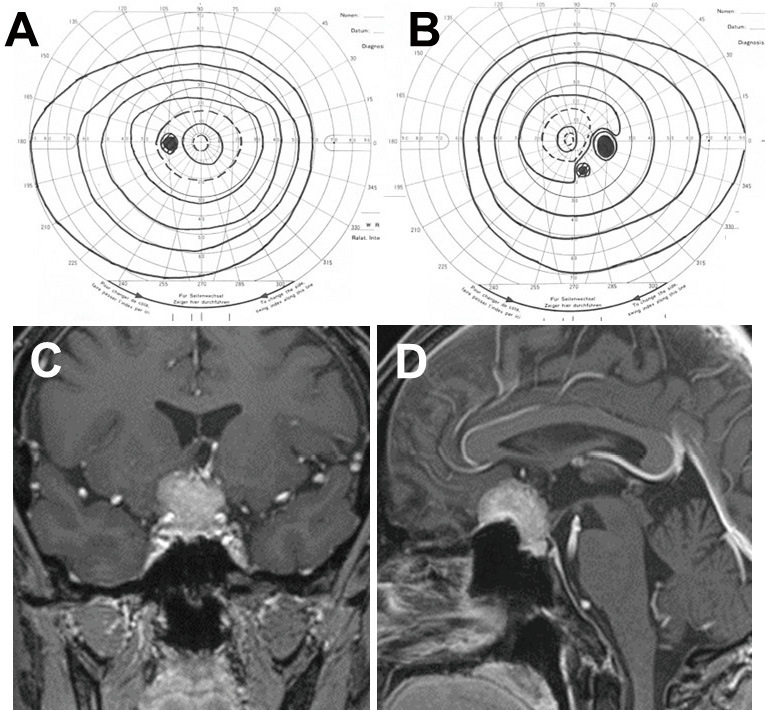
Preoperative left (A) and right (B) visual field of case 1 showing scotoma at the lower visual field center in the right eye. Coronal (C) and sagittal (D) contrast-enhanced T1-weighted magnetic resonance images showing tuberculum sellae meningioma.
Fig. 2.
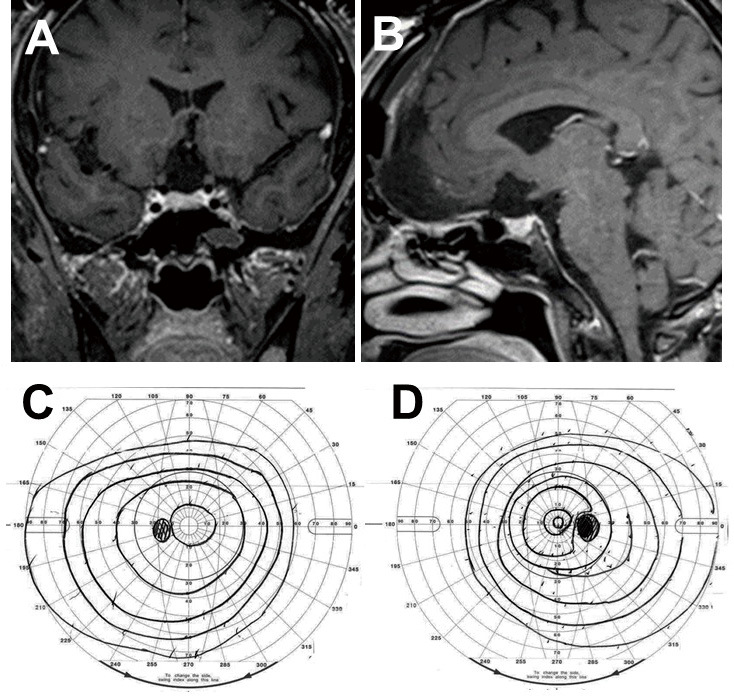
Postoperative coronal (A) and sagittal (B) contrast-enhanced T1-weighted magnetic resonance images of case 1 showing total tumor removal. Left (C) and right (D) visual field showing a cured scotoma after surgery.
Case Report 2
A 58-year-old female presented to the ophthalmology department of our institute complaining of blurred vision in the lateral visual field of her left eye since one year ago. Goldman visual field test revealed a small scotoma at the lower center in the left eye and upper lateral area near the center of the right eye (Fig. 3A and B). A small meningioma (10 mm in size) at the left tuberculum sellae was found after brain MRI and was referred to our department (Fig. 3C and D). The tumor compressed the inferior medial aspect of the left optic nerve. Despite the small size of the tumor, the patient was eager to undergo surgical removal because her daily activities, including walking or reading, were hindered by her visual disturbance. Intraoperative finding via the left pterional approach was that the tumor compressed the left optic nerve from the medial, and inferior aspects. The arachnoid layer was absent around the tumor, and the lesion was strongly adhered to the left optic nerve. To avoid nerve injury, a small amount of the tumor capsule was left unremoved. Since the tumor involved the optic canal, the tumor was extensively removed by opening the optic canal (Fig. 4A and B). The scotoma was cured (Fig. 4C and D). The pathological diagnosis was meningothelial meningioma.
Fig. 3.
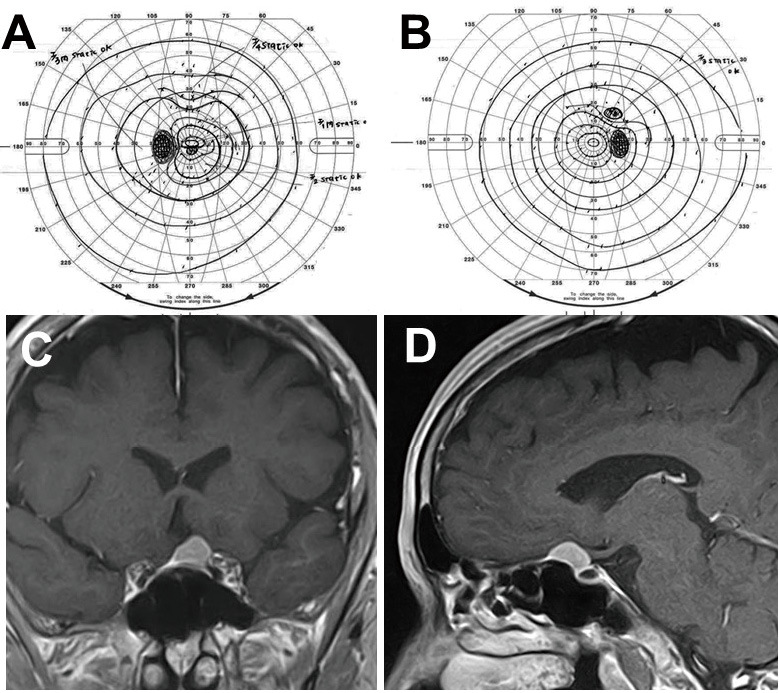
Preoperative left (A) and right (B) visual field of case 2 showing a small scotoma at the lower center in the left eye. Coronal (C) and sagittal (D) contrast-enhanced T1-weighted magnetic resonance images showing a small tuberculum sellae meningioma.
Fig. 4.
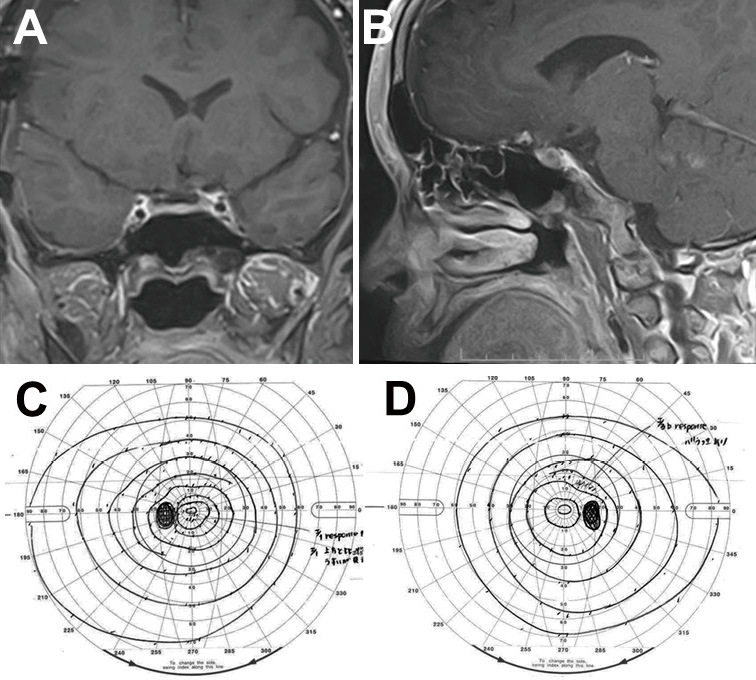
Postoperative coronal (A) and sagittal (B) contrast-enhanced T1-weighted magnetic resonance images of case 2 showing total tumor removal. Left (C) and right (D) visual field showing a cured scotoma after surgery.
Visual deficits in both patients were relatively limited, but their difficulty in daily activities recovered immediately after surgical removal, and they were fully satisfied with the surgical results.
Discussion
Despite the small scotoma at lower visual field center, the tuberculum sellae meningiomas in two patients were successfully removed because of the strong desire of the patients. The patients' visual function recovered well immediately after surgical removal, and they were completely satisfied. Deficits at the central visual field can be caused by the lesion in the macula of the retina, posterior area of the occipital lobe, center of the optic chiasm, and the unilateral optic nerve near the optic chiasm.8) The latter two regions might be attributable to the visual symptoms in our patients. In our first case, the tumor widely compressed the bilateral optic nerves and chiasm. Central scotoma may be due to the compression of the center of the optic chiasm, rather than the unilateral optic nerve near the optic chiasm. In our second case, the central scotoma may have been due to the compression of the unilateral optic nerve near the optic chiasm. Another possible mechanism would be junctional scotoma, which could be caused by compression of the anterior of the optic chiasm.9,10)
Although visual defects in both patients were not so wide, their symptoms affected their daily activities. This would be because the lower center visual field is particularly important in walking and reading.11) Therefore, visual deficits in the lower center fields may cause large obstacles,12) and the patients' daily activities was considered to be strongly affected. The mean size for the removal of the tuberculum sellae meningiomas has been reported to be 20-40 mm.1,13,14) Tumor size in our patients was 10 and 25 mm, respectively. The size in the first patient was relatively small, and visual field deficits were relatively limited. However, strong hope for surgery of the patient to relieve her symptoms forced us to perform surgery, which consequently led to immediate symptom relief.
According to past studies, the following factors were related to favorable visual outcomes after surgical removal of the tuberculum sellae meningiomas: younger age, shorter period of visual symptoms, less severe visual impairment, the presence of the arachnoid membrane around the lesion, predominantly vertical growth, the presence of a significant peri-tumoral edema, and extensive removal.4,7,15-18) In view of these facts, the following conditions were considered to be related to favorable visual outcomes in our patients; relatively young age, mild and short duration of visual symptoms, absence of peri-tumoral edema, and success in extensive removal. Hence, we found that even if relatively small tumors cause relatively limited visual deficits, patient symptoms can be immediately relieved by appropriate removal, and patient satisfaction can be achieved by improving patient's daily activities. In addition, if the tumor involves the optic canal, the optic canal should be opened, since early optic canal unroofing could improve visual symptoms.13)
Conclusions
Tuberculum sellae meningiomas commonly present as bitemporal hemianopia and loss of visual acuity due to the compression of the optic nerve; however, they can cause small scotomas at the lower visual field center. Even if the visual field defect is not sufficiently large, daily activities, including walking or reading can be hindered. When patients exhibit visual deficits, especially in the lower center fields, surgical removal should be considered even if the tumors are small and visual deficits are limited, since improvement of both vision and daily activities can be achieved.
Informed Consent
Informed consent for publication was obtained from the patients.
Conflicts of Interest Disclosure
The authors declare no conflicts of interest directly related to the content of this article.
References
- 1). Margalit N, Shahar T, Barkay G, et al. : Tuberculum sellae meningiomas: surgical technique, visual outcome, and prognostic factors in 51 cases. J Neurol Surg B Skull Base 74: 247-258, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Kitano M, Taneda M, Nakao Y: Postoperative improvement in visual function in patients with tuberculum sellae meningiomas: results of the extended transsphenoidal and transcranial approaches. J Neurosurg 107: 337-346, 2007 [DOI] [PubMed] [Google Scholar]
- 3). Sade B, Lee JH: High incidence of optic canal involvement in tuberculum sellae meningiomas: rationale for aggressive skull base approach. Surg Neurol 72: 118-123, 2009 [DOI] [PubMed] [Google Scholar]
- 4). Lee SJ, Hong SH, Cho YH, Kim JH, Kim CJ: Anatomical origin of tuberculum sellae meningioma: off-midline location and its clinical implications. World Neurosurg 89: 552-561, 2016 [DOI] [PubMed] [Google Scholar]
- 5). Fahlbusch R, Schott W: Pterional surgery of meningiomas of the tuberculum sellae and planum sphenoidale: surgical results with special consideration of ophthalmological and endocrinological outcomes. J Neurosurg 96: 235-243, 2002 [DOI] [PubMed] [Google Scholar]
- 6). Iwai Y, Yamanaka K, Nakajima H, Yasui T, Mochizuki K: Surgical treatment of tuberculum sellae meningiomas: the importance of opening the entrance of the optic canal. Jpn J Neurosurg (Tokyo) 9: 610-614, 2000. (Japanese) [Google Scholar]
- 7). Schick U, Hassler W: Surgical management of tuberculum sellae meningiomas: involvement of the optic canal and visual outcome. J Neurol Neurosurg Psychiatry 76: 977-983, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).In: The Visual Fields, a Textbook and Atlas of Clinical Perimetry. ed 5. Harrington DO, Ed. CV Mosby, St. Louis, 1981 [Google Scholar]
- 9). Schiefer U, Isbert M, Mikolaschek E, et al. : Distribution of scotoma pattern related to chiasmal lesions with special reference to anterior junction syndrome. Graefes Arch Clin Exp Ophthalmol 242: 468-477, 2004 [DOI] [PubMed] [Google Scholar]
- 10). Donaldson LC, Eshtiaghi A, Sacco S, Micieli JA, Margolin EA: Junctional scotoma and patterns of visual field defects produced by lesions involving the optic chiasm. J Neuroophthalmol 42: e203-e208, 2022 [DOI] [PubMed] [Google Scholar]
- 11). Marigold DS, Patla AE: Visual information from the lower visual field is important for walking across multi-surface terrain. Exp Brain Res 188: 23-31, 2008 [DOI] [PubMed] [Google Scholar]
- 12). Black AA, Wood JM, Lovie-Kitchin JE: Inferior visual field reductions are associated with poorer functional status among older adults with glaucoma. Ophthalmic Physiol Opt 31: 283-291, 2011 [DOI] [PubMed] [Google Scholar]
- 13). Nozaki K, Kikuta K, Takagi Y, Mineharu Y, Takahashi JA, Hashimoto N: Effect of early optic canal unroofing on the outcome of visual functions in surgery for meningiomas of the tuberculum sellae and planum sphenoidale. Neurosurgery 62: 839-846, 2008 [DOI] [PubMed] [Google Scholar]
- 14). Kachhara R, Nigam P, Nair S: Tuberculum sella meningioma: surgical management and results with emphasis on visual outcome. J Neurosci Rural Pract 13: 431-440, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Pamir MN, Ozduman K, Belirgen M, Kilic T, Ozek MM: Outcome determinants of pterional surgery for tuberculum sellae meningiomas. Acta Neurochir (Wien) 147: 1121-1130, 2005 [DOI] [PubMed] [Google Scholar]
- 16). Carlson AP, Stippler M, Myers O: Predictive factors for vision recovery after optic nerve decompression for chronic compressive neuropathy: systematic review and meta-analysis. Neurol Surg B Skull Base 74: 20-38, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Seol HJ, Park HY, Nam DH, et al. : Clinical outcomes of tuberculum sellae meningiomas focusing on reversibility of postoperative visual function. Acta Neurochir (Wien) 155: 25-31, 2013 [DOI] [PubMed] [Google Scholar]
- 18). Zevgaridis D, Medele RJ, Müller A, Hischa AC, Steiger HJ: Meningiomas of the sellar region presenting with visual impairment: impact of various prognostic factors on surgical outcome in 62 patients. Acta Neurochir (Wien) 143: 471-476, 2001 [DOI] [PubMed] [Google Scholar]


