Abstract
Aims: Inflammation is associated with vascular events. We aimed to investigate the relationship between high-sensitivity C-reactive protein (hsCRP) levels with and without intracranial arterial stenosis (ICAS) and the prognosis of patients with minor stroke or transient ischemic attack.
Methods: We used data from the Clopidogrel in High-Risk Patients with Acute Nondisabling Cerebrovascular Events trial (derivation cohort) and the Third China National Stroke Registry (validation cohort). Patients were divided into four groups according to the dichotomy of hsCRP level and ICAS status. The primary outcome was new ischemic stroke within 90 days, and the secondary outcome was dependence or death (Modified Rankin Scale score of 3–6) at 90 days. The associations between hsCRP level with and without ICAS and risk of outcomes were analyzed using multivariate Cox regression and logistic regression models.
Results: In the derivation cohort, compared with patients with nonelevated hsCRP levels and no ICAS, those with both elevated hsCRP levels and ICAS had increased risk of recurrent stroke (adjusted hazard ratio [HR], 2.62; 95% confidence interval [CI], 1.28–5.34;p=0.008) and dependence or death (adjusted odds ratio [OR], 7.58; 95% CI, 1.30–44.13;p=0.02). Consistent relationships of elevated hsCRP levels and presence of ICAS with recurrent stroke (adjusted HR, 1.67; 95% CI, 1.13–2.45;p=0.009) and dependence or death (adjusted OR, 1.87; 95% CI, 1.23–2.84;p=0.003) were observed in the validation cohort.
Conclusion: Concomitant presence of increased hsCRP levels and ICAS was associated with increased risk of stroke recurrence and dependence or death in patients with minor ischemic stroke or transient ischemic attack.
Keywords: Ischemic stroke, C-reactive protein, Intracranial arterial stenosis, Recurrence, Neurologic function, Prognosis
Approximately 10%–20% of patients with minor ischemic stroke or transient ischemic attack (TIA) developed recurrence within 3 months after symptom onset 1 , 2) , most of which even occurred within the first 2 days 3) . Early identification of high-risk patients helps in the application of intensive secondary prevention or screening of candidate for potential additional treatment 4) .
Patients with residual inflammation risk had a higher rate of subsequent stroke 5) , suggesting that inflammation contributed to the residual risk of recurrent stroke 5 , 6) . The role of inflammation in stroke pathogenesis through various mechanisms has been well addressed previously 7) . The association between greater inflammation burden evaluated using various circulating inflammation markers and increased recurrence risk has been previously suggested 8) . Intracranial arterial stenosis (ICAS) has been perceived as an inflammatory process and an accessible image marker of recurrence 9) . Contrarily, high-sensitivity C-reactive protein (hsCRP) is a well acknowledged inflammatory biomarker associated with recurrent stroke 10) and reflects intracranial atherosclerotic burden 11) . The addition of ICAS to hsCRP might improve the resolution capability of the degree of vascular inflammation 4) . However, how the degree of vascular inflammation burden determined by the combination of ICAS and hsCRP affects recurrent stroke is still undetermined. On the contrary, inflammation has been correlated with poor functional outcome in patients with minor stroke or TIA 10) . Nevertheless, the role of the combination of hsCRP and ICAS in predicting dependence or death is less established.
Using data from the Clopidogrel in High-Risk Patients with Acute Nondisabling Cerebrovascular Events (CHANCE) trial 12) , we aimed to explore the outcomes of minor stroke and TIA according to hsCRP levels and ICAS. We further verified the results by using a prospective cohort of the Third China National Stroke Registry (CNSR-III).
Methods
Study Design
Details on the design and methods of the CHANCE trial and CNSR-III have been previously described 13 , 14) .
In brief, the CHANCE trial was a randomized, double-blind, placebo-controlled clinical trial that included patients with acute minor stroke (National Institutes of Health Stroke Scale (NIHSS) ≤ 3) or moderate-to-high risk of TIA (ABCD2 score ≥ 4) within 24 h of symptom onset to assess the efficacy and safety of clopidogrel added to aspirin.
The CNSR-III was a nationwide, multicenter, prospective, observational registry that included consecutive patients who presented to hospitals within 7 days after acute ischemic stroke or TIA between August 2015 and March 2018 from 201 study sites in China. For the present study, we extracted patients with minor stroke (NIHSS ≤ 3) or moderate-to-high risk of TIA (ABCD2 score ≥ 4) and admitted within 24 hours after the index event from CNSR-III.
Standard Protocol Approvals and Patient Consents
The CHANCE trial and CNSR-III protocols were approved by the ethics committee at each study center. All the included patients or their legal proxies provided written informed consent.
Image Analysis
In the image substudy of the CHANCE trial, patients provided a three-dimensional (3D) time-of-flight magnetic resonance angiography (MRA) of MR image sequence 9) . In the CNSR-III, either image of MRA, computerized tomography angiography, or digital subtraction angiography was collected during hospitalization 14) . A centralized interpretation by two readers blinded to patients’ information was performed in the center laboratory of Beijing Tiantan Hospital in both the CHANCE trial and CNSR-III. ICAS was determined by the presence of 50%–99% stenosis according to the Warfarin–Aspirin Symptomatic Intracranial Disease trial criteria or occlusion of at least one of the following arterial segments: intracranial portion of internal carotid arteries, middle cerebral arteries (M1/M2), intracranial portion of vertebral arteries, and basilar artery 15) .
Measurement of hsCRP
All fasting blood specimens were collected within 24±12 hours after enrollment and transported through cold chain to the core laboratory in Beijing Tiantan Hospital. All samples were stored at −80℃. The hsCRP concentration was determined centrally and blindly using a Roche Modular analyzer via turbidimetric immunoassay.
Follow-up and Outcomes
In the CHANCE trial, participants were followed up by face-to-face interview at 90 days by trained research personnel 13) , whereas participants in the CNSR-III were followed up by face-to-face or telephone interview at 3 months and 1 year 14) .
The primary outcome was a new ischemic stroke within 90 days. The secondary outcome was dependence or death defined as a Modified Rankin Scale score of 3–6 at 90 days and new ischemic stroke or dependence or death within 1 year in the CNSR-III cohort.
Statistical Analysis
A hsCRP cutoff level of ≥ 2 mg/L has been applied to defined high-risk patients in the previous randomized clinical trial 16 , 17) . We therefore used this cutoff level and the presence of ICAS to classify patients. Furthermore, a cutoff hsCRP level >3 mg/L has been recommended by the Centers for Disease Control and American Heart Association for risk stratification of cardiovascular disease 18) . We have proved its usefulness in recurrent stroke 10) . We further conducted sensitivity analyses using this cutoff level.
Proportions were used for categorical variables. Mean with SD or medians with interquartile ranges were used for continuous variables. Categorical variables were compared using chi-squared statistics or Fisher’s exact test as appropriate. Continuous variables were compared via one-way analysis of variance or Kruskal–Wallis test.
We first assessed the associations between hsCRP levels and ICAS and outcomes using the cohort of the CHANCE trial (derivation cohort) and then verified the relationships in the cohort of CNSR-III (validation cohort). Multivariate Cox proportional-hazards regression and logistic regression models were used. The potential confounders were demographic factors, previously published traditional or clinical risk factors, baseline leukocyte count, and study intervention or secondary prevention medications used during the follow-up period. Adjusted hazard ratios (HRs) and their 95% confidence intervals (CIs) were reported.
The receiver operating characteristic (ROC) curve with area under the curve was used. The Essen Stroke Risk Score was developed to identify patients at the highest risk of subsequent vascular event 19 , 20) . We therefore calculated the c-statistics and net reclassification index to evaluate improvement in risk classification by hsCRP and presence of ICAS over the Essen Stroke Risk Score.
A two-sided p<0.05 was considered to indicate statistical significance. All statistical analyses were conducted using the SAS software version 9.3 (SAS Institute, Inc., Cary, NC).
Results
Patient Characteristics
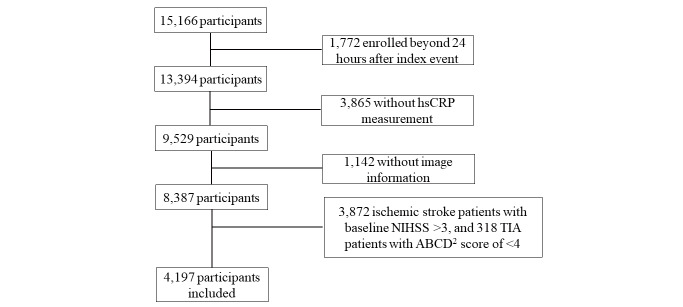
A total of 807 patients were included in the derivation cohort and 4,197 in the validation cohort ( Supplemental Fig.1 ) . In the derivation cohort, 322 (39.9%), 127 (15.7%), 216 (26.8%), and 142 (17.6%) patients had nonelevated hsCRP levels without ICAS, elevated hsCRP levels without ICAS, nonelevated hsCRP levels with ICAS, and elevated hsCRP levels with ICAS, respectively. Age, history of ischemic stroke, TIA, hypertension and diabetes, baseline NIHSS score, and baseline leukocyte count differed among the four groups ( Table 1 ) . Furthermore, the body mass index and history of myocardial infarction, congestive heart failure, known atrial fibrillation, or flutter and hypercholesterolemia differed in the validation cohort ( Supplemental Table 1 ) .
Supplemental Fig.1. Flow Chart Showing the Participant Selection.
Abbreviation: hsCRP= high-sensitive C-reactive protein, NIHSS=National Institutes of Health Stroke Scale, TIA=transient ischemic attack.
Table 1. Baseline Characteristics According to hsCRP Levels and Presence of ICAS in the Derivation Cohort.
| Characteristics |
hsCRP <2mg/L and absence of ICAS, n = 259 |
hsCRP ≥ 2mg/L and absence of ICAS, n = 190 |
hsCRP <2mg/L and with ICAS, n = 176 |
hsCRP ≥ 2 mg/L and with ICAS, n = 182 |
P value |
|---|---|---|---|---|---|
| Age, median (IQR) | 60 (53-68) | 62 (54-72) | 66 (57-74) | 67 (59-73) | <0.001 |
| BMI, median (IQR) | 24.2 (22.1-25.7) | 24.5 (22.5-26.8) | 24.5 (22.4-26.4) | 24.5 (22.4-27.0) | 0.17 |
| Female, No. (%) | 86 (33.2) | 60 (31.6) | 72 (40.9) | 64 (35.2) | 0.26 |
| Current or previous smoking, No. (%) | 111 (42.9) | 85 (44.7) | 68 (38.6) | 79 (43.4) | 0.67 |
| Medical history, No. (%) | |||||
| Ischemic stroke | 35 (13.5) | 26 (13.7) | 35 (19.9) | 44 (24.2) | 0.01 |
| TIA | 6 (2.3) | 3 (1.6) | 5 (2.8) | 12 (6.6) | 0.03 |
| Myocardial infarction | 1 (0.4) | 3 (1.6) | 6 (3.4) | 4 (2.2) | 0.09 |
| Congestive heart failure | 4 (1.5) | 3 (1.6) | 6 (3.4) | 3 (1.6) | 0.56 |
| Known atrial fibrillation or flutter | 4 (1.5) | 6 (3.2) | 6 (3.4) | 2 (1.1) | 0.31 |
| Hypercholesterolemia | 32 (12.4) | 26 (13.7) | 19 (10.8) | 28 (15.4) | 0.61 |
| Hypertension | 154 (59.5) | 129 (67.9) | 104 (59.1) | 140 (76.9) | <0.0001 |
| Diabetes mellitus | 38 (14.7) | 30 (15.8) | 42 (23.9) | 45 (24.7) | 0.01 |
| Baseline NIHSS score, median (IQR) | 1 (0-2) | 2 (0-2) | 2 (0-3) | 2 (1-3) | 0.001 |
| Baseline leukocyte count (*109/L), median (IQR) | 6.3 (5.1-7.3) | 7.0 (5.9-8.4) | 6.8 (5.7-8.2) | 7.5 (6.3-9.1) | <0.0001 |
| Index event | 0.22 | ||||
| TIA, No.(%) | 73 (28.2) | 46 (24.2) | 47 (26.7) | 36 (19.8) | |
| Minor stroke, No.(%) | 186 (71.8) | 144 (75.8) | 129 (73.3) | 146 (80.2) | |
| Treatment allocation | 0.83 | ||||
| Aspirin alone, No.(%) | 124 (47.9) | 97 (51.1) | 88 (50.0) | 95 (52.2) | |
| Clopidogrel plus aspirin, No.(%) | 135 (52.1) | 93 (48.9) | 88 (50.0) | 87 (47.8) |
Abbreviation: hsCRP = high-sensitive C-reactive protein; ICAS= Intracranial arterial stenosis; BMI=body mass index; IQR= interquartile range; NIHSS= National Institutes of Health Stroke Scale; TIA= transient ischemic attack.
Supplemental Table1. Baseline characteristics according to the status of hsCRP levels and ICAS in the validation cohort.
| Characteristics |
hsCRP <2mg/L and absence of ICAS n = 1472 |
hsCRP ≥ 2mg/L and absence of ICAS n = 866 |
hsCRP <2mg/L and with ICAS n = 1029 |
hsCRP ≥ 2mg/L and with ICAS n = 830 |
P value |
|---|---|---|---|---|---|
| Age, median (IQR) | 60 (52-67) | 63 (54-71) | 63 (55-70) | 64 (57-73) | <0.0001 |
| BMI, median (IQR) | 24.3 (22.5-26.2) | 24.7 (22.6-27.1) | 24.6 (22.7-26.5) | 25.0 (23.0-27.3) | <0.0001 |
| Female, No. (%) | 433 (29.4) | 257 (29.7) | 284 (27.6) | 275 (33.1) | 0.08 |
| Current or previous smoking, No. (%) | 503 (34.2) | 306 (35.3) | 336 (32.7) | 259 (31.2) | 0.28 |
| Medical history, No. (%) | |||||
| Ischemic stroke | 234 (15.9) | 142 (16.4) | 210 (20.4) | 193 (23.3) | <0.0001 |
| TIA | 37 (2.5) | 28 (3.2) | 39 (3.8) | 31 (3.7) | 0.25 |
| Myocardial infarction | 20 (1.4) | 18 (2.1) | 13 (1.3) | 23 (2.8) | 0.04 |
| Congestive heart failure | 1 (0.1) | 1 (0.1) | 2 (0.2) | 6 (0.7) | 0.04 |
| Known atrial fibrillation or flutter | 31 (2.1) | 24 (2.8) | 40 (3.9) | 38 (4.6) | 0.005 |
| Hypercholesterolemia | 113 (7.7) | 103 (11.9) | 97 (9.4) | 82 (9.9) | 0.009 |
| Hypertension | 844 (57.3) | 539 (62.2) | 685 (66.6) | 570 (68.7) | <0.0001 |
| Diabetes mellitus | 290 (19.7) | 183 (21.1) | 251 (24.4) | 257 (31.0) | <0.0001 |
| Baseline NIHSS, median (IQR) | 1.5 (1-2) | 2.0 (1-2) | 2.0 (1-2) | 2.0 (1.0-3.0) | 0.01 |
| Index event | 0.24 | ||||
| TIA, No.(%) | 99 (6.7) | 59 (6.8) | 70 (6.8) | 40 (4.8) | |
| Minor stroke, No.(%) | 1373 (93.3) | 807 (93.2) | 959 (93.2) | 790 (95.2) |
hsCRP and Recurrent Ischemic Stroke
The univariate analyses are presented in Supplement Table 2 . The derivation cohort included 73 (9.0%) patients with ischemic stroke within 90 days. Compared with the patients with nonelevated hsCRP levels and no ICAS, those with both elevated hsCRP levels and ICAS had increased risk of recurrent ischemic stroke after adjustment (adjusted HR, 2.62; 95% CI, 1.28–5.34; p=0.008) ( Table 2 ) , and a nominally significant association with recurrent ischemic stroke was observed among patients with nonelevated hsCRP levels and with ICAS (adjusted HR, 2.03; 95% CI, 0.98–4.20; p=0.058) ( Table 2 ) . In the validation cohort, we observed a consistent association of elevated hsCRP levels and ICAS with recurrent ischemic stroke within 90 days (adjusted HR, 1.67; 95% CI, 1.13–2.45; p=0.009) ( Table 2 ) . Similar results were observed in the sensitivity analysis with an hsCRP cutoff level of 3 mg/L ( Supplemental Table 3 ) .
Supplemental Table2. Univariable Analyses of Risks for Recurrent Ischemic Stroke and Dependence or Death within 90 days in the Derivation Cohort.
| Characteristics | No IS recurrence | IS Recurrence | HR (95% CI) | P value | mRS: 0-3 | mRS: 3-6 | OR (95% CI) | P value |
|---|---|---|---|---|---|---|---|---|
| Age, median (IQR) | 62.9 (55.0-71.7) | 65.8 (54.7-73.1) | 1.01 (0.99-1.03) | 0.37 | 62.8 (54.8-71.7) | 67.4 (58.3-74.0) | 1.03 (1.00-1.05) | <0.0001 |
| BMI, median (IQR) | 24.3 (22.5-26.4) | 25.3 (22.0-27.5) | 1.03 (0.96-1.10) | 0.43 | 24.3 (22.4-26.4) | 25.4 (22.8-27.5) | 1.05 (0.97-1.14) | 0.26 |
| Female, No. (%) | 248 (33.8) | 34 (46.6) | 1.66 (1.05-2.62) | 0.03 | 256 (34.1) | 25 (46.3) | 1.66 (0.95-2.90) | 0.07 |
| Current or previous smoking, No. (%) | 315 (42.9) | 28 (38.4) | 0.83 (0.52-1.34) | 0.45 | 322 (42.9) | 19 (35.2) | 0.72 (0.41-1.29) | 0.27 |
| Medical history, No. (%) | ||||||||
| Ischemic stroke | 121 (16.5) | 19 (26.0) | 1.74 (1.03-2.94) | 0.04 | 126 (16.8) | 13 (24.1) | 1.57 (0.82-3.02) | 0.18 |
| Transient ischemic attack | 21 (2.9) | 5 (6.8) | 2.35 (0.95-5.84) | 0.07 | 24 (3.2) | 2 (3.7) | 1.16 (0.27-5.06) | 0.84 |
| Myocardial infarction | 14 (1.9) | 0 (0) | 0.05 (0-109.6) | 0.44 | 13 (1.7) | 0 (0) | / | 1.00 |
| Angina | 22 (3.0) | 1 (1.4) | 0.47 (0.07-3.39) | 0.46 | 22 (2.9) | 1 (1.9) | 0.62 (0.08- 4.72) | 0.65 |
| Congestive heart failure | 13 (1.8) | 3 (4.1) | 2.29 (0.72-7.28) | 0.16 | 12 (1.6) | 3 (5.6) | 3.62 (0.99-13.23) | 0.052 |
| Known atrial fibrillation or flutter | 14 (1.9) | 4 (5.5) | 2.70 (0.98-7.39) | 0.054 | 14 (1.9) | 4 (7.4) | 4.21 (1.34-13.25) | 0.01 |
| Hypercholesterolemia | 96 (13.1) | 9 (12.3) | 0.93 (0.46-1.87) | 0.84 | 95 (12.7) | 8 (14.8) | 1.20 (0.55-2.62) | 0.65 |
| Hypertension | 475 (64.7) | 52 (71.2) | 1.33 (0.80-2.21) | 0.27 | 484 (64.5) | 40 (74.1) | 1.57 (0.84-2.94) | 0.16 |
| Diabetes mellitus | 138 (18.8) | 17 (23.3) | 1.29 (0.75-2.23) | 0.35 | 141 (18.8) | 14 (25.9) | 1.51 (0.80-2.85) | 0.20 |
| Baseline NIHSS, median (IQR) | 2 (0-2) | 2 (1-3) | 1.31 (1.05-1.62) | 0.01 | 2 (0-2) | 2 (2-3) | 1.68 (1.28-2.22) | <0.0001 |
| Baseline leukocyte count (*109/L), median (IQR) | 6.7 (5.6-8.2) | 7.2 (6.2-8.2) | 1.01 (0.98-1.05) | 0.48 | 6.7 (5.6-8.2) | 7.4 (6.2-8.7) | 1.02 (0.97-1.07) | 0.45 |
| Minor stroke as index event, No.(%) | 542 (73.8) | 63 (86.3) | 2.17 (1.11-4.22) | 0.02 | 550 (73.3) | 53 (98.1) | 19.3 (2.7-140.3) | 0.003 |
| Treatment allocation of clopidogrel plus aspirin | 371 (50.5) | 32 (43.8) | 0.78 (0.49-1.24) | 0.29 | 373 (49.7) | 27 (50.0) | 1.01 (0.58-1.76) | 0.97 |
Abbreviation: HR = hazard ratio; CI=confidence intervals; OR=odds ratio; mRS=Modified Rankin Scale score; IQR= interquartile range;
Table 2. Risk of Recurrent Ischemic Stroke and Dependence or Death According to hsCRP Levels and Presence of ICAS.
| Cohort | Outcomes | Group* | Events, n (%) | Model 1 † | Model 2 ‡ | Model 3 § | |||
|---|---|---|---|---|---|---|---|---|---|
| Adjusted HR/OR (95% CI) | P value | Adjusted HR/OR (95% CI) | P value | Adjusted HR/OR (95% CI) | P value | ||||
| Derivation Cohort | Recurrent ischemic stroke within 90-days | 1 | 13 (5.0) | Reference | / | Reference | / | Reference | / |
| 2 | 15 (7.9) | 1.60 (0.76-3.38) | 0.22 | 1.60 (0.75-3.39) | 0.23 | 1.60 (0.75-3.41) | 0.22 | ||
| 3 | 19 (10.8) | 2.14 (1.05-4.36) | 0.04 | 2.02 (0.98-4.18) | 0.06 | 2.03 (0.98-4.20) | 0.058 | ||
| 4 | 26 (14.3) | 2.99 (1.52-5.89) | 0.002 | 2.61 (1.29-5.27) | 0.008 | 2.62 (1.28-5.34) | 0.008 | ||
| Dependence or death within 90-days | 1 | 6 (2.3) | Reference | / | Reference | / | Reference | / | |
| 2 | 9 (4.8) | 2.05 (0.71-5.89) | 0.18 | 1.14 (0.20-6.57) | 0.89 | 1.11 (0.19-6.48) | 0.91 | ||
| 3 | 15 (8.5) | 3.58 (1.35-9.50) | 0.01 | 3.44 (0.59-20.18) | 0.17 | 3.32 (0.56-19.73) | 0.19 | ||
| 4 | 24 (13.2) | 5.95 (2.35-15.07) | <0.0001 | 7.85 (1.37-45.04) | 0.02 | 7.58 (1.30-44.13) | 0.02 | ||
| Validation Cohort | Recurrent ischemic stroke within 90-days | 1 | 53 (3.6) | Reference | / | Reference | / | Reference | / |
| 2 | 47 (5.4) | 1.47 (0.99-2.18) | 0.06 | 1.39 (0.93-2.06) | 0.11 | 1.38 (0.93-2.05) | 0.11 | ||
| 3 | 55 (5.3) | 1.45 (1.00-2.12) | 0.05 | 1.42 (0.97-2.07) | 0.07 | 1.41 (0.96-2.06) | 0.08 | ||
| 4 | 59 (7.1) | 1.88 (1.29-2.74) | 0.001 | 1.69 (1.15-2.48) | 0.007 | 1.67 (1.13-2.45) | 0.009 | ||
| Recurrent ischemic stroke within 1-year | 1 | 88 (6.0) | Reference | / | Reference | / | Reference | / | |
| 2 | 60 (6.9) | 1.14 (0.82-1.59) | 0.42 | 1.11 (0.80-1.55) | 0.54 | 1.12 (0.80-1.56) | 0.52 | ||
| 3 | 96 (9.3) | 1.55 (1.16-2.07) | 0.003 | 1.53 (1.14-2.05) | 0.005 | 1.54 (1.15-2.06) | 0.004 | ||
| 4 | 97 (11.7) | 1.93 (1.44-2.58) | <0.0001 | 1.77 (1.32-2.39) | 0.0002 | 1.76 (1.30-2.38) | 0.0002 | ||
| Dependence or death at 90-days | 1 | 47 (3.2) | Reference | / | Reference | / | Reference | / | |
| 2 | 41 (4.8) | 1.31 (0.85-2.01) | 0.23 | 1.14 (0.72-1.82) | 0.57 | 1.13 (0.71-1.80) | 0.60 | ||
| 3 | 51 (5.0) | 1.40 (0.93-2.11) | 0.10 | 1.18 (0.76-1.82) | 0.46 | 1.16 (0.75-1.79) | 0.50 | ||
| 4 | 74 (9.1) | 2.36 (1.61-3.47) | <0.0001 | 1.85 (1.22-2.81) | 0.004 | 1.87 (1.23-2.84) | 0.003 | ||
| Dependence or death at 1- year | 1 | 57 (3.9) | Reference | / | Reference | / | Reference | / | |
| 2 | 50 (5.9) | 1.29 (0.87-1.91) | 0.21 | 1.16 (0.76-1.78) | 0.49 | 1.1 8(0.77-1.80) | 0.46 | ||
| 3 | 66 (6.5) | 1.47 (1.02-2.13) | 0.04 | 1.31 (0.88-1.94) | 0.18 | 1.32 (0.89-1.95) | 0.17 | ||
| 4 | 73 (9.0) | 1.85 (1.28-2.67) | 0.001 | 1.49 (1.00-2.21) | 0.05 | 1.53 (1.02-2.28) | 0.04 | ||
Abbreviation: hsCRP = high-sensitive C-reactive protein; ICAS= Intracranial arterial stenosis; HR = hazard ratio; OR=odds ratio; CI=confidence intervals;
* Group 1: hsCRP <2mg/L and absence of ICAS; Group 2: hsCRP ≥ 2mg/L and absence of ICAS; Group 3: hsCRP <2mg/L and with ICAS;
Group 4: hsCRP ≥ 2mg/L and with ICAS;
† Model 1, adjusted for age and sex;
‡ Model 2: In the derivation cohort, for the outcome of ischemic stroke, the models were adjusted for age, sex, body mass index, current or previous smoking, medical history of hypertension, diabetes mellitus, hypercholesterolemia, ischemic stroke, transient ischemic attack, myocardial infarction, angina and known atrial fibrillation or flutter, National Institutes of Health Stroke Scale (NIHSS) score at 1 day after randomization, qualifying event, randomized treatment of aspirin monotherapy or dual antiplatelet therapy, and the use of lipid-lowering agents, hypoglycemic agents or antihypertension agents during 90-day follow-up period; for the outcome of dependence or death, the models were adjusted for age, sex, body mass index, current or previous smoking, medical history of hypertension, diabetes mellitus, hypercholesterolemia, ischemic stroke, transient ischemic attack, myocardial infarction, angina, and known atrial fibrillation or flutter, NIHSS score at 1 day after randomization, pre-stroke modified Rankin Scale (mRS) score, qualifying event, randomized treatment of aspirin monotherapy or dual antiplatelet therapy, the use of lipid-lowering, hypoglycemic or antihypertension agents and recurrence of stroke during 90-day follow-up. In the validation cohort, for the outcome of ischemic stroke, the models were adjusted for age, sex, body mass index, current or previous smoking, medical history of hypertension, diabetes mellitus, hypercholesterolemia, ischemic stroke, transient ischemic attack, myocardial infarction, angina, known atrial fibrillation or flutter, baseline NIHSS score, qualifying event, recombinant tissue plasminogen activator (rtPA) treatment, endovascular therapy, and the use of antiplatelet agents, lipid- lowering agents, hypoglycemic agents, antihypertension agents or anticoagulation agents during follow-up period; for the outcome of dependence or death, the models were adjusted for age, sex, body mass index, current or previous smoking, medical history of hypertension, diabetes mellitus, hypercholesterolemia, ischemic stroke, transient ischemic attack, myocardial infarction, and known atrial fibrillation or flutter, baseline NIHSS score, pre-stroke mRS score, qualifying event, rtPA treatment, endovascular therapy, the use of antiplatelet agents, lipid-lowering agents, hypoglycemic agents, antihypertension agents or anticoagulation agents and recurrence of stroke during follow-up period;
§ Model 3:adjusted for all factors in Model 2 and baseline leukocyte counts.
Supplemental Table 3. Risk of Recurrent Ischemic Stroke and Dependence or Death at 90 Days According to hsCRP Level of ≥ 3mg/L and Presence of ICAS.
| Cohort | Outcomes | Group | Events, n (%) | Model 1 * | Model 2 † | ||
|---|---|---|---|---|---|---|---|
| Adjusted HR (95% CI) | P value | Adjusted HR (95% CI) | P value | ||||
| Derivation Cohort | Ischemic Stroke | hsCRP <3mg/L and absence of ICAS | 16 (5.0) | Reference | / | Reference | / |
| hsCRP ≥ 3mg/L and absence of ICAS | 12 (9.4) | 1.92 (0.91-4.07) | 0.09 | 1.80 (0.85-3.85) | 0.13 | ||
| hsCRP <3mg/L and with ICAS | 26 (12.0) | 2.42 (1.29-4.55) | 0.006 | 2.26 (1.19-4.29) | 0.01 | ||
| hsCRP ≥ 3mg/L and with ICAS | 19 (13.4) | 2.81 (1.43-5.53) | 0.003 | 2.33 (1.15-4.71) | 0.02 | ||
| Dependence or death | hsCRP <3mg/L and absence of ICAS | 8 (2.5) | Reference | / | Reference | / | |
| hsCRP ≥ 3mg/L and absence of ICAS | 7 (5.6) | 2.22 (0.79-6.28) | 0.13 | 0.88 (0.15-5.10) | 0.89 | ||
| hsCRP <3mg/L and with ICAS | 20 (9.3) | 3.69 (1.58-8.60) | 0.003 | 3.06 (0.63-14.88) | 0.17 | ||
| hsCRP ≥ 3mg/L and with ICAS | 19 (13.4) | 5.60 (2.36-13.3) | <0.0001 | 9.48 (1.65-54.46) | 0.01 | ||
| Validation Cohort | Ischemic Stroke | hsCRP <3mg/L and absence of ICAS | 70 (4.0) | Reference | / | Reference | / |
| hsCRP ≥ 3mg/L and absence of ICAS | 30 (5.0) | 1.20 (0.78-1.84) | 0.41 | 1.16 (0.75-1.78) | 0.50 | ||
| hsCRP <3mg/L and with ICAS | 71 (5.7) | 1.38 (0.99-1.93) | 0.06 | 1.33 (0.95-1.86) | 0.10 | ||
| hsCRP ≥ 3mg/L and with ICAS | 43 (7.0) | 1.64 (1.12-2.41) | 0.01 | 1.54 (1.04-2.28) | 0.03 | ||
| Dependence or death | hsCRP <3mg/L and absence of ICAS | 58 (3.4) | Reference | / | Reference | / | |
| hsCRP ≥ 3mg/L and absence of ICAS | 30 (5.0) | 1.33 (0.84-2.10) | 0.22 | 1.26 (0.77-2.06) | 0.35 | ||
| hsCRP <3mg/L and with ICAS | 61 (5.0) | 1.34 (0.93-1.94) | 0.12 | 1.13 (0.76-1.68) | 0.55 | ||
| hsCRP ≥3mg/L and with ICAS | 64 (10.6) | 2.67 (1.83-3.90) | <0.0001 | 2.29 (1.52-3.45) | <0.0001 | ||
* Model 1, adjusted for age and sex;
† Model 2: For the outcome of ischemic stroke, the models were adjusted for age, sex, body mass index, current or previous smoking, medical history of hypertension, diabetes mellitus, hypercholesterolemia, ischemic stroke, transient ischemic attack, myocardial infarction, known atrial fibrillation or flutter, National Institutes of Health Stroke Scale score at 1 day after randomization, qualifying event, randomized treatment of aspirin monotherapy or dual antiplatelet therapy, and the use of lipid-lowering agents, hypoglycemic agents or antihypertension agents during 90-day follow-up period; for the outcome of dependence or death, the models were adjusted for age, sex, body mass index, current or previous smoking, medical history of hypertension, diabetes mellitus, hypercholesterolemia, ischemic stroke, transient ischemic attack, myocardial infarction, and known atrial fibrillation or flutter, baseline NIHSS score, baseline mRS score, index event, and the use of antiplatelet therapy , lipid-lowering, hypoglycemic or antihypertension agents and recurrence of stroke during follow-up.
With respect to recurrent ischemic stroke within 1 year, similar results were observed, in addition to a more apparent relationship between nonelevated hsCRP levels and ICAS and recurrence ( Table 2 ) . We therefore conducted further analyses to determine whether the addition of hsCRP and ICAS improved the prediction value. The area under the ROC curves for the prediction model of the Essen Stroke Risk Score (0.58, p=0.002) increased after including hsCRP and ICAS in the model, resulting in the improvement of continuous net reclassification index (28.1%, p<0.0001) ( Table 3 ) .
Table 3. Reclassification and Discrimination Statistics for Recurrent Stroke within 1-year by Adding hsCRP and ICAS to ESSEN Score in the Validation Cohort.
| Outcomes | Model | AUC | NRI,% | ||
|---|---|---|---|---|---|
| Estimate (95% CI) | P value | Estimate (95% CI) | P value | ||
| Ischemic Stroke Recurrence | ESRS | 0.54 (0.50-0.57) | / | Reference | / |
| ESRS+hsCRP | 0.54 (0.51-0.58) | 0.40 | 10.9 (-0.2-21.9) | 0.05 | |
| ESRS+ICAS | 0.57 (0.55-0.61) | 0.002 | 26.8 (15.8-37.8) | <0.0001 | |
| ESRS+hsCRP+ICAS | 0.58 (0.55-0.62) | 0.002 | 28.1 (17.2-39.1) | <0.0001 | |
C-statistics, net reclassification index (NRI) and their 95% confidence interval were calculated respectively to evaluate improvement in risk classification by hsCRP and presence of ICAS over Essen Stroke Risk Score.
Abbreviations: hsCRP = high-sensitive C-reactive protein; ICAS= Intracranial arterial stenosis; AUC=Area under the curve; CI=Confidence Interval; NRI= Net Reclassification Index; ESRS=Essen Stroke Risk Score.
hsCRP and Dependence or Death
In the derivation cohort, a total of 54 (6.7%) patients had dependence or death at 90 days. Compared with the patients with nonelevated hsCRP levels and no ICAS, those with both elevated hsCRP levels and ICAS had increased risk of dependence or death (adjusted OR, 7.58; 95% CI, 1.30–44.13; p=0.02, Table 2 ).
In the validation cohort, a consistent significant relationship was observed at 90 days (adjusted OR, 1.87; 95% CI, 1.23–2.84; p=0.003, Table 2 ) and 1 year (adjusted OR, 1.53; 95% CI, 1.02–2.28; p=0.04, Table 2 ). Similar results were found in the sensitivity analyses ( Supplemental Table 3 ) .
Discussion
The present study showed that a greater inflammation burden assessed by the combination of hsCRP levels and the presence of ICAS predicted higher risk of recurrent ischemic stroke and dependence or death in patients with minor ischemic stroke or TIA.
Patients were at a high risk of developing new vascular events early after acute minor stroke or TIA, which frequently worsened the prognosis. However, traditional statistical prediction models based on clinical risk factors did not account for the entire risk 2 , 21) . There has been a substantial interest to find simple and readily available markers to predict recurrence. Furthermore, a gradient relationship between the numbers of elevated biomarkers and risk of vascular events has been previously reported 22 , 23) . In line with that, we previously showed that the combination of inflammation biomarkers of hsCRP and soluble CD40 ligand or image marker of multiple infarctions better predicted recurrent stroke than any one alone in patients with minor stroke or TIA, indicating the addictive effect of inflammation burden on vascular event 4 , 8 , 24) . Furthermore, in view of the pathological role of inflammation in ICAS 25) , our previous study illustrating the summation effect of ICAS and higher neutrophil counts on recurrence further supported this hypothesis 26) . In contrary with neutrophil counts, hsCRP is an inflammation biomarker commonly used in the clinical setting; its application in the prediction of vascular events has been investigated through mechanisms such as promotion of endothelial cell dysfunction, atherosclerosis, progression and destabilization of atherosclerotic plaques, and arterial thrombosis 27 - 29) . In the present study, we found that the combination of hsCRP and ICAS gradually increased the hazard of recurrence or poor prognosis compared with hsCRP or ICAS alone, indicating the synergistic effect of hsCRP and ICAS on stroke recurrence and grim prognosis, consistent with the gradual increased areas under the ROC curves for the prediction models of the Essen Stroke Risk Score when including hsCRP or ICAS alone, and both. ICAS was adjudicated when 50%–99% stenosis or arterial occlusion was present in the present study. The ability of the dichotomous variable of ICAS and the continuous variable of hsCRP level to reflect vascular inflammatory burden might not be comparable. This may explain why the area of the model with the Essen Stroke Risk Score and ICAS only slightly changed when hsCRP was added. Further research is warranted to confirm our findings.
For patients with ICAS, stroke could be due to hypoperfusion resulting in stenosis and unstable plaque-related thromboembolism. In view of hsCRP, the mechanisms leading to the occurrence of stroke might also include arterial stenosis 11) as well as unstable plaque and thrombosis 30) , in addition to more risk factors, such as older age and comorbidity, as our results indicated. A previous study showed that intraplaque inflammation was associated with early stroke recurrence, independent of the degree of stenosis 31) . hsCRP might accelerate the progression of arterial stenosis in patients with ICAS as a systemic inflammatory marker or indicate an active inflammation in the initial ICAS part as a local inflammatory marker. However, due to the lack of image information of recurrence in the present study, the exact reason for the increased risk of recurrent stroke in the patients with elevated hsCRP levels and ICAS was not identified.
Measurements of the hsCRP level and determination of ICAS were centralized in the present study to ensure consistency of the assessments. Furthermore, we evaluated and validated the predictive value of the combination of hsCRP and ICAS in two independent cohorts to provide stronger evidence. hsCRP should increase under various patient conditions represented by infection. We previously demonstrated that the measurement time of hsCRP affected its association with stroke recurrence: hsCRP measured in the first 72 hours after ischemic stroke or TIA but not beyond 72 hours was associated with an increased risk of 1‐year stroke recurrence 32) . We controlled the sampling time within that window and further adjusted the baseline leukocyte counts to exclude their influence on the results. It is noteworthy that the predictive accuracy of the Essen Stroke Risk Score was lower than that in the previous study 20) , which might be mainly due to the dramatic reduction of recurrence rate caused by the improvement of secondary prevention management of ischemic cerebrovascular disease.
Conversely, though we included patients with minor stroke or TIA in the present study, we found that elevated levels of hsCRP and presence of ICAS predicted disability or death. Because recurrence might worsen prognosis, we added recurrence as a confounding factor in the multivariate analyses, and identical results were obtained. It has been shown that CRP activates the complement pathway, which exerts cytotoxic effect and exacerbates cerebral tissue damage, enhancing neuronal cell apoptosis and infarct size, all of which might explain neurologic functional impairment 33 - 35) .
Taken together, we found that the combination of image marker of ICAS and biomarker of hsCRP is useful for the risk stratification of recurrent stroke, exceeding the predictability of using any of the markers alone. Given the protection of anti-inflammatory therapy in subsequent vascular events after coronary heart disease, our results might have potential importance for the selection of high-risk patients for anti-inflammatory treatment.
Although this post hoc analysis was based on the data from two well-designed large cohorts, there were still several limitations. First, the measurement of hsCRP level was only once at baseline. The dynamic fluctuation might be more meaningful. Second, leukocyte count is a common marker for infection. Though we adjusted it as a confounder in the multivariate regression models, baseline data regarding stroke-associated infections would be more informative. Third, a considerable percentage of patients had TIA as the index event in the present study, precluding us from defining responsible arterial stenosis or occlusion. Fourth, the prevalence of ICAS in Asian descent has been reported to be higher than that of Western descent. Therefore, the generalizability of our findings needs further validation 36 , 37) .
Conclusion
Elevated hsCRP levels and the presence of ICAS were strongly associated with the incidence of recurrent stroke and dependence or death in patients with acute minor stroke or high-risk TIA.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81870905, U20A20358), the Capital’s Funds for Health Improvement and Research (2020-1-2041) and Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2019-I2M-5-029).
Role of the Funding Source
The sponsors had no role in study design, collection, analysis and interpretation of data, writing of the report and the decision to submit the article for publication.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1).Ois A, Gomis M, Rodriguez-Campello A, Cuadrado-Godia E, Jimenez-Conde J, Pont-Sunyer C, Cuccurella G, Roquer J. Factors associated with a high risk of recurrence in patients with transient ischemic attack or minor stroke. Stroke, 2008; 39: 1717-1721 [DOI] [PubMed] [Google Scholar]
- 2).Chandratheva A, Geraghty OC, Rothwell PM. Poor performance of current prognostic scores for early risk of recurrence after minor stroke. Stroke, 2011; 42: 632-637 [DOI] [PubMed] [Google Scholar]
- 3).Pan Y, Jing J, Chen W, Meng X, Li H, Zhao X, Liu L, Wang D, Johnston SC, Wang Y, Wang Y, investigators C. Risks and benefits of clopidogrel-aspirin in minor stroke or tia: Time course analysis of chance. Neurology, 2017; 88: 1906-1911 [DOI] [PubMed] [Google Scholar]
- 4).Li J, Wang A, Zhao X, Liu L, Meng X, Lin J, Jing J, Zou X, Wang Y, Wang Y, Investigators C. High-sensitive c-reactive protein and dual antiplatelet in intracranial arterial stenosis. Neurology, 2018; 90: e447-e454 [DOI] [PubMed] [Google Scholar]
- 5).Li J, Pan Y, Xu J, Li S, Wang M, Quan K, Meng X, Li H, Lin J, Wang Y, Zhao X, Liu L, Wang Y, Investigators C-I. Residual inflammatory risk predicts poor prognosis in acute ischemic stroke or transient ischemic attack patients. Stroke, 2021; 52: 2827-2836 [DOI] [PubMed] [Google Scholar]
- 6).Wang Y. Residual recurrence risk of ischaemic cerebrovascular events: Concept, classification and implications. Stroke Vasc Neurol, 2021; 6: 155-157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Coveney S, McCabe JJ, Murphy S, O’Donnell M, Kelly PJ. Anti-inflammatory therapy for preventing stroke and other vascular events after ischaemic stroke or transient ischaemic attack. Cochrane Database Syst Rev, 2020; 5: CD012825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Li J, Wang Y, Lin J, Wang D, Wang A, Zhao X, Liu L, Wang C, Wang Y, Investigators C. Soluble cd40l is a useful marker to predict future strokes in patients with minor stroke and transient ischemic attack. Stroke, 2015; 46: 1990-1992 [DOI] [PubMed] [Google Scholar]
- 9).Liu L, Wong KS, Leng X, Pu Y, Wang Y, Jing J, Zou X, Pan Y, Wang A, Meng X, Wang C, Zhao X, Soo Y, Johnston SC, Wang Y, Investigators C. Dual antiplatelet therapy in stroke and icas: Subgroup analysis of chance. Neurology, 2015; 85: 1154-1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Li J, Zhao X, Meng X, Lin J, Liu L, Wang C, Wang A, Wang Y, Wang Y, Investigators C. High-sensitive c-reactive protein predicts recurrent stroke and poor functional outcome: Subanalysis of the clopidogrel in high-risk patients with acute nondisabling cerebrovascular events trial. Stroke, 2016; 47: 2025-2030 [DOI] [PubMed] [Google Scholar]
- 11).Wang J, Liu Y, Zhang L, Li N, Wang C, Gao X, Zhou Y, Wang A, Wu S, Zhao X. Associations of high sensitivity c-reactive protein levels with the prevalence of asymptomatic intracranial arterial stenosis. Eur J Neurol, 2014; 21: 512-518 [DOI] [PubMed] [Google Scholar]
- 12).Wang Y, Wang Y, Zhao X, Liu L, Wang D, Wang C, Wang C, Li H, Meng X, Cui L, Jia J, Dong Q, Xu A, Zeng J, Li Y, Wang Z, Xia H, Johnston SC, Investigators C. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med, 2013; 369: 11-19 [DOI] [PubMed] [Google Scholar]
- 13).Wang Y, Johnston SC, Wang Y. Clopidogrel with aspirin in minor stroke or transient ischemic attack. N Engl J Med, 2013; 369: 1376-1377 [DOI] [PubMed] [Google Scholar]
- 14).Wang Y, Jing J, Meng X, Pan Y, Wang Y, Zhao X, Lin J, Li W, Jiang Y, Li Z, Zhang X, Yang X, Ji R, Wang C, Wang Z, Han X, Wu S, Jia Z, Chen Y, Li H. The third china national stroke registry (cnsr-iii) for patients with acute ischaemic stroke or transient ischaemic attack: Design, rationale and baseline patient characteristics. Stroke Vasc Neurol, 2019; 4: 158-164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR. American journal of neuroradiology, 2000; 21: 643-646 [PMC free article] [PubMed] [Google Scholar]
- 16).Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr., Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ, Group JS. Rosuvastatin to prevent vascular events in men and women with elevated c-reactive protein. N Engl J Med, 2008; 359: 2195-2207 [DOI] [PubMed] [Google Scholar]
- 17).Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ, Group CT. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med, 2017; 377: 1119-1131 [DOI] [PubMed] [Google Scholar]
- 18).Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, 3rd, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Rifai N, Smith SC, Jr., Taubert K, Tracy RP, Vinicor F, Centers for Disease C, Prevention, American Heart A. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the centers for disease control and prevention and the american heart association. Circulation, 2003; 107: 499-511 [DOI] [PubMed] [Google Scholar]
- 19).Weimar C, Diener HC, Alberts MJ, Steg PG, Bhatt DL, Wilson PW, Mas JL, Rother J, Investigators REoAfCHR. The essen stroke risk score predicts recurrent cardiovascular events: A validation within the reduction of atherothrombosis for continued health (reach) registry. Stroke, 2009; 40: 350-354 [DOI] [PubMed] [Google Scholar]
- 20).Meng X, Wang Y, Zhao X, Wang C, Li H, Liu L, Zhou Y, Xu J, Wang Y. Validation of the essen stroke risk score and the stroke prognosis instrument ii in chinese patients. Stroke, 2011; 42: 3619-3620 [DOI] [PubMed] [Google Scholar]
- 21).Whiteley W, Tian Y, Jickling GC. Blood biomarkers in stroke: Research and clinical practice. Int J Stroke, 2012; 7: 435-439 [DOI] [PubMed] [Google Scholar]
- 22).Zhong C, Zhu Z, Wang A, Xu T, Bu X, Peng H, Yang J, Han L, Chen J, Xu T, Peng Y, Wang J, Li Q, Ju Z, Geng D, He J, Zhang Y. Multiple biomarkers covering distinct pathways for predicting outcomes after ischemic stroke. Neurology, 2019; 92: e295-e304 [DOI] [PubMed] [Google Scholar]
- 23).Looker HC, Colombo M, Agakov F, Zeller T, Groop L, Thorand B, Palmer CN, Hamsten A, de Faire U, Nogoceke E, Livingstone SJ, Salomaa V, Leander K, Barbarini N, Bellazzi R, van Zuydam N, McKeigue PM, Colhoun HM, Investigators S. Protein biomarkers for the prediction of cardiovascular disease in type 2 diabetes. Diabetologia, 2015; 58: 1363-1371 [DOI] [PubMed] [Google Scholar]
- 24).Wang G, Jing J, Li J, Pan Y, Yan H, Meng X, Zhao X, Liu L, Li H, Wang DZ, Wang Y, Wang Y. Association of elevated hs-crp and multiple infarctions with outcomes of minor stroke or tia: Subgroup analysis of chance randomised clinical trial. Stroke Vasc Neurol, 2021; 6: 80-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol, 2012; 32: 2045-2051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26).Zhu B, Liu H, Pan Y, Jing J, Li H, Zhao X, Liu L, Wang D, Johnston SC, Wang Z, Wang Y, Wang Y, Investigators C. Elevated neutrophil and presence of intracranial artery stenosis increase the risk of recurrent stroke. Stroke, 2018; 49: 2294-2300 [DOI] [PubMed] [Google Scholar]
- 27).Tanaka A, Shimada K, Sano T, Namba M, Sakamoto T, Nishida Y, Kawarabayashi T, Fukuda D, Yoshikawa J. Multiple plaque rupture and c-reactive protein in acute myocardial infarction. J Am Coll Cardiol, 2005; 45: 1594-1599 [DOI] [PubMed] [Google Scholar]
- 28).Kashiwagi M, Tanaka A, Kitabata H, Tsujioka H, Matsumoto H, Arita Y, Ookochi K, Kuroi A, Kataiwa H, Tanimoto T, Ikejima H, Takarada S, Kubo T, Hirata K, Nakamura N, Mizukoshi M, Imanishi T, Akasaka T. Relationship between coronary arterial remodeling, fibrous cap thickness and high-sensitivity c-reactive protein levels in patients with acute coronary syndrome. Circ J, 2009; 73: 1291-1295 [DOI] [PubMed] [Google Scholar]
- 29).Kazantsev AN, Karkayeva MR, Tritenko AP, Korotkikh AV, Zharova AS, Chernykh KP, Bagdavadze GS, Lider RY, Kazantseva YG, Zakharova KL, Shmatov DV, Kravchuk VN, Peshekhonov KS, Zarkua NE, Lutsenko VA, Sultanov RV, Artyukhov SV, Kharchilava EU, Solotenkova KN, Zakeryayev AB. Carotid enadrterectomy for thrombosis of the internal carotid artery in patients with covid-19. Curr Probl Cardiol, 2022: 101252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Esmon CT. Inflammation and thrombosis. J Thromb Haemost, 2003; 1: 1343-1348 [DOI] [PubMed] [Google Scholar]
- 31).Marnane M, Merwick A, Sheehan OC, Hannon N, Foran P, Grant T, Dolan E, Moroney J, Murphy S, O’Rourke K, O’Malley K, O’Donohoe M, McDonnell C, Noone I, Barry M, Crowe M, Kavanagh E, O’Connell M, Kelly PJ. Carotid plaque inflammation on 18f-fluorodeoxyglucose positron emission tomography predicts early stroke recurrence. Ann Neurol, 2012; 71: 709-718 [DOI] [PubMed] [Google Scholar]
- 32).Wang Y, Li J, Pan Y, Wang M, Meng X, Wang Y. Association between high-sensitivity c-reactive protein and prognosis in different periods after ischemic stroke or transient ischemic attack. J Am Heart Assoc, 2022; 11: e025464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33).Gill R, Kemp JA, Sabin C, Pepys MB. Human c-reactive protein increases cerebral infarct size after middle cerebral artery occlusion in adult rats. J Cereb Blood Flow Metab, 2004; 24: 1214-1218 [DOI] [PubMed] [Google Scholar]
- 34).Pepys MB, Hirschfield GM. C-reactive protein: A critical update. J Clin Invest, 2003; 111: 1805-1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35).Jia H, Qu M, Fan G, Wu H, Wang L. Mir-499-5p suppresses c-reactive protein and provides neuroprotection in hypoxic-ischemic encephalopathy in neonatal rat. Neurosci Res, 2020; 161: 44-50 [DOI] [PubMed] [Google Scholar]
- 36).Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, Wang Y, Zou X, Leung TW, Cai Y, Bai Q, Wu Y, Wang C, Pan X, Luo B, Wong KS, Group CS. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in china: The chinese intracranial atherosclerosis (cicas) study. Stroke, 2014; 45: 663-669 [DOI] [PubMed] [Google Scholar]
- 37).Suri MF, Qiao Y, Ma X, Guallar E, Zhou J, Zhang Y, Liu L, Chu H, Qureshi AI, Alonso A, Folsom AR, Wasserman BA. Prevalence of intracranial atherosclerotic stenosis using high-resolution magnetic resonance angiography in the general population: The atherosclerosis risk in communities study. Stroke, 2016; 47: 1187-1193 [DOI] [PMC free article] [PubMed] [Google Scholar]