Abstract
Rationale
Psychological resilience (the ability to thrive in adversity) may protect against mental-health symptoms in healthcare professionals during coronavirus disease (COVID-19) waves.
Objectives
To identify determinants of resilience in ICU staff members.
Methods
In this cross-sectional survey in 21 French ICUs, staff members completed the 10-item Connor-Davidson Resilience Scale, Hospital Anxiety and Depression Scale, and Impact of Event Scale–Revised (for post-traumatic stress disorder [PTSD]). Factors independently associated with resilience were identified.
Measurements and Main Results
The response rate was 73.1% (950 of 1,300). The median 10-item Connor-Davidson Resilience Scale score was 29 (interquartile range, 25–32). Symptoms of anxiety, depression, and PTSD were present in 61%, 39%, and 36% of staff members, respectively. Distress associated with the COVID-19 infodemic was correlated with symptoms of depression and PTSD. More resilient respondents less often had symptoms of anxiety, depression, and PTSD. Greater resilience was independently associated with male sex, having provided intensive care during the early waves, having managed more than 50 patients with COVID-19, and, compared with earlier waves, working longer hours, having greater motivation, and more often involving families in end-of-life decisions. Independent risk factors for lower resilience were having managed more than 10 patients who died of COVID-19, having felt frightened or isolated, and greater distress from the COVID-19 infodemic.
Conclusions
This study identifies modifiable determinants of resilience among ICU staff members. Longitudinal studies are needed to determine whether prior resilience decreases the risk of mental ill health during subsequent challenges. Hospital and ICU managers, for whom preserving mental well-being among staff members is a key duty, should pay careful attention to resilience.
Keywords: coronavirus, acute respiratory distress syndrome, post-traumatic growth, post-traumatic stress disorder, vulnerability
At a Glance Commentary
Scientific Knowledge on the Subject
Symptoms of mental ill health were extremely common in ICU healthcare professionals during the first coronavirus disease (COVID-19) waves. Whether psychological resilience relates to mental-health symptoms in this setting has not been investigated.
What This Study Adds to the Field
During the COVID-19 wave seen between October and December 2021 in France, symptoms of anxiety, depression, and post-traumatic stress disorder were more prevalent than during previous waves (61%, 39%, and 36%, respectively). Greater psychological resilience was independently associated with a lower prevalence of all three categories of mental-health symptoms. Factors independently associated with greater resilience were male sex, having provided intensive care during the early waves, having managed more than 50 patients with COVID-19, working longer hours, having greater motivation, and making end-of-life decisions jointly with family members. Independent risk factors for lower resilience were having managed more than 10 patients who died of COVID-19, having felt frightened or isolated, and reporting greater distress from the COVID-19 infodemic. Greater resilience was associated with lower prevalences of anxiety, depression, and post-traumatic stress disorder symptoms. Only 8% of respondents felt supported by their institutions.
With more than 760 million cases worldwide and more than 6.8 million deaths, the coronavirus disease (COVID-19) pandemic has placed unprecedented demands on healthcare systems and has required healthcare professionals (HCPs) to work under high-stress conditions for unusually long periods. The COVID-19 pandemic was thus a traumatic event that adversely affected physical and mental health. The huge efforts made by HCPs to provide high-quality care under new, fast changing, high-risk circumstances often came at the cost of mental ill health. Studies documented high prevalences of insomnia, acute stress, anxiety, and depression among ICU staff members during COVID-19 waves (1–3). HCPs reported feeling unsafe and even fearing for their lives while caring for patients with COVID-19 (4, 5). A fear of infecting others, inadequate time for rest, and limitations in the ability to care for one’s own family were associated with an increased prevalence of mental-health symptoms (1, 6). Nurses reported feeling isolated because partners, family members, neighbors, and the public avoided physical proximity (7). Additional physical and emotional stressors were the shortage of personal protective equipment, restrictions placed on patient visitation by families, and the increased number of patients with severe illness or death (2, 8). Burnout syndrome, a state of physical and emotional exhaustion due to prolonged commitment to emotionally demanding work situations, was documented in 45% of frontline HCPs (8–10). According to a survey done early in the pandemic, more than a quarter of HCPs exposed to patients with COVID-19 experienced symptoms associated with post-traumatic stress disorder (PTSD) (10).
In 2014, the American Psychological Association defined psychological resilience (hereafter “resilience”) as the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress (11). Resilience is thus the ability to thrive in the face of adversity (12). Resilience shapes an individual’s response to trauma (13) and correlates positively with overall health, psychological well-being, efficient coping strategies (14), and better quality of life among HCPs (15). Resilience may protect against the development of mental-health symptoms such as anxiety, depression, and PTSD in traumatic settings (16). Thus, among hospital physicians in France, resilience was lower among individuals who had histories of anxiety, stress, or depression (17). If the protective effect of resilience is confirmed, then providing staff members with resilience-building tools, on a regular basis and particularly during challenging events, would be crucial (18).
Resilience can be assessed quantitatively using a standardized and validated tool developed by Connor and Davidson (12). Among revised versions, the 10-item Connor-Davidson Resilience Scale (CD-RISC-10) developed by Campbell-Sills and Stein has demonstrated excellent performance characteristics, including good internal consistency and strong test–retest reliability (19).
The primary objective of this cross-sectional study was to identify determinants of psychological resilience among HCPs working in French ICUs during the COVID-19 wave in late 2021, that is, after several previous COVID-19 waves.
Methods
The Comité de Protection des Personnes Sud-Méditerranée ethics committee approved this study on March 31, 2020 (2020-A00809-30; Commission Nationale des Recherches Impliquant la Personne Humaine: 20.03.27.73019). An online questionnaire was sent between October 30 and December 1, 2021, to each of the 1,300 HCPs who worked in any of 21 ICUs belonging to the FAMIREA study group.
Survey Instrument
The survey items are reported in the tables and figures. Some items had been used for previous studies done during the first and second COVID-19 waves in France (1, 10), and others were identified through a literature review and semistructured interviews with HCPs working in the participating ICUs. The survey collected data on exposure to COVID-19 (number of patients managed, infection in family and/or friends), visitation policies for family members, professional and personal impact of the pandemic (fear of being infected or of infecting family and friends, ability to rest, family balance, ability to care for family, tiredness, working conditions, intention to leave the ICU), and personal characteristics (demographics and consumption of alcohol, tobacco, and psychotropic drugs).
The survey also included three validated self-reported questionnaires assessing resilience, anxiety and depression, and PTSD, respectively. Resilience was evaluated using the unidimensional CD-RISC-10. In keeping with the definition of resilience as the ability to thrive in the face of adversity by making positive adjustments to challenging demands, this tool assesses favorable responses to change, stress management, and goal achievement despite obstacles and pressure. The 10 items are adaptability (ability to adapt and adjust to changing circumstances and new situations), personal competence (sense of self-confidence and belief own ability to handle challenges effectively), social support (availability of social support systems and perceived degree of support from family, friends, or other sources), tolerance for negative affect (ability to cope with and manage negative emotions and stress without becoming overwhelmed), stress control (ability to control stress in response to various stressors), spiritual influence (feeling supported by spiritual or existential beliefs and practices), positive acceptance (ability to accept and make peace with past experiences, including adverse ones), determination and tenacity (persistence and determination in the face of challenges or setbacks), trust in one’s instincts and decision-making abilities, and meaning and purpose (perceived meaning and purpose in one’s life). Each of these 10 items is rated on a Likert-type scale ranging from 0 to 4, and the total score can thus range from 0 to 40, with higher scores indicating greater resilience. Symptoms of anxiety and depression were assessed using the Hospital Anxiety and Depression Scale (HADS) (1, 10, 20) and were defined as scores >7 of 21 on the relevant subscale. To detect symptoms of PTSD, we relied on the Impact of Events Scale–Revised (IES-R) (21), whose 22 items assess subjective distress caused by traumatic events. The items include 14 of the 17 Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, symptoms of PTSD. Respondents are asked to indicate their degree of distress during the past week caused by difficulties related to a specific stressful life event. The total score can range from 0 to 88, and subscores can be calculated for the intrusion, avoidance, and hyperarousal subscales. We defined the presence of PTSD-related symptoms as an IES-R score ⩾22.
The study took place in France from October to December 2021, at the beginning of the Omicron wave. Every day, 50,000 new cases were diagnosed, with an incidence rate of 550 per 100,000, and more than 17,000 hospital beds were occupied by patients with COVID-19, including more than 3,200 in ICUs. Since the beginning of the pandemic in France, more than 8 million people had caught the disease and almost 120,000 had died. An invitation to take part in this cross-sectional study was sent to all HCPs working in the participating ICUs, using mailing lists, WhatsApp groups, a poster with quick-response codes in each ICU, and local invitations by study investigators. HCPs were defined as nursing staff members (nurses and nursing assistants), medical staff members (residents, interns, clinical fellows, and senior intensivists), and other professionals providing patient care in the ICUs. For variables depicting the COVID-19 experience, the responses were either binary (yes or no) or made on visual analog scales (VASs) ranging from 0 to 10 assessing frustration, fear, isolation, commitment, motivation, support, and working conditions. VASs are easy and rapid to complete and have been proved reliable for measuring characteristics, subjective phenomena, and attitudes that are expected to range across a continuum of values and for which direct measurements cannot be readily obtained. The COVID-19 infodemic was scored on a VAS ranging from 0 to 10. The infodemic was defined as the rapid and extensive spread of a mixture of both accurate and inaccurate information in which facts merge with rumors and fears, making it difficult to obtain trustworthy information (22). The COVID-19 infodemic has been reported to result in confusion, risk-taking behaviors, and mistrust in health authorities, thereby undermining the public health response (22).
Study Outcomes
Resilience measured using the CD-RISC-10 score was the primary outcome. We did not use a cutoff value for this score.
The secondary outcomes were symptoms of anxiety and depression, defined as scores >7 on the relevant HADS subscales, and symptoms consistent with PTSD, defined as an IES-R score ⩾22.
Statistical Analysis
The data are described as median (interquartile range) or number and percentage. Categorical variables were compared using the Fisher exact test and continuous variables using the nonparametric Wilcoxon test or Kruskal-Wallis test. Spearman’s coefficient was computed to assess correlations.
Factors independently associated with CD-RISC-10 score were identified by building a linear regression model. Logistic regression was also performed to assess independent predictors of symptoms of anxiety, depression, and PTSD. For all models, we first performed univariate analyses including all the variables shown in Tables 1–3. Variables associated with P values <0.20 were used to build multivariate models. The final models were obtained by stepwise variable selection using an automatic procedure based on the Akaike information criterion. Interactions and correlations between the explanatory variables were carefully checked. For logistic models, continuous variables were checked for log-linearity assumptions and dichotomized if needed. For linear models, the linearity assumption was carefully checked. We assessed calibration and discrimination of multivariate logistic regression models and the percentage of variation (r2) explained by the model for multivariate linear regression models. Surface plots were created to depict relationships between important variables. We did not adjust for multiple comparisons. No imputation methods were used.
Table 1.
Characteristics of the 950 Respondents
| n (%) or Median (IQR) | |
|---|---|
| Men | 332 (35) |
| Age, yr | 37 (30–45) |
| University-affiliated hospital | 446 (47) |
| Role in the ICU | |
| Nurse/nursing assistant | 416 (44)/135 (14) |
| Senior physician/resident | 280 (29)/100 (11) |
| Other healthcare professional | 19 (2) |
| Total ICU experience, yr | 7 (3–14) |
| ICU work during previous COVID-19 wave(s) | 833 (89) |
| Managed >50 patients with COVID-19 in current wave | 497 (52) |
| Managed >10 patients with COVID-19 who died in current wave | 467 (49) |
| Has had COVID-19 | 217 (23) |
| Family members have had severe COVID-19 | 327 (34) |
| Started/increased treatment for anxiety, depression, or PTSD | 78/19 (10) |
| Needed new psychological support | 182 (19) |
| Excessive alcohol intake/cannabis/other recreational drugs | 25/18/3 (5) |
| Visitation policies for family members | |
| Unchanged from before the pandemic/restricted | 595 (63)/239 (25) |
| Unlimited family visits | 75 (8) |
| No family visits allowed | 41 (4) |
| New communication media used for the current wave* | 335 (35) |
| Satisfaction with visitation policies (VAS scores) | 7 (5–8) |
| Compared with previous waves (VAS scores) | |
| I experience more fear/more exhaustion | 5 (3–7)/8 (6–9) |
| I experience more frustration/more isolation | 7 (5–8)/4 (2–6) |
| I can rest more regularly/can spend more time with family | 4 (3–6)/5 (3–7) |
| I experience more distress from the infodemic/from social frustration | 5 (3–7)/5 (2–8) |
| I can take more days off | 10 (9–10) |
| I believe that end-of-life decisions followed a more consensual process† | 8 (5–9) |
| During this wave | |
| I believe that my work time has increased | 7 (5–8) |
| I believe that my professional commitment/motivation has increased | 6 (5–8)/6 (4–8) |
| I am proud of the work I have been doing | 7 (6–9) |
| I believe that I intend to leave the ICU | 7 (5–9)/7 (4–8) |
| I have been supported by | |
| My colleagues | 735 (77) |
| My family/my friends | 832 (88)/642 (68) |
| My superiors/my institution | 256 (27)/76 (8) |
| The lay public/the government | 45 (5)/39 (4) |
| VAS score for overall perceived support | 5 (5–7) |
| Television/social media >1 h/d | 268 (29)/236 (24) |
| Reading books/newspapers >1 h/d | 140 (15) |
Definition of abbreviations: COVID-19 = coronavirus disease; IQR = interquartile range; PTSD = post-traumatic stress disorder; VAS = visual analog scale with two anchors (0 indicating no symptoms/lowest possible rating and 10 the worst symptoms/highest possible rating).
Including videoconferences, routine calls from healthcare professionals to family members, and WhatsApp groups.
Consensual was defined as sharing of end-of-life decisions between the family and healthcare professionals.
Table 3.
Multivariable Analysis of the Determinants of Symptoms of Anxiety, Depression, and Post-Traumatic Stress Disorder
| Anxiety Symptoms, Odds Ratio (95%CI) | Depression Symptoms, Odds Ratio (95%CI) | PTSD-related Symptoms, Odds Ratio (95%CI) | |
|---|---|---|---|
| Male sex | — | — | 0.49 (0.35–0.71) |
| ICU work during previous wave(s) | — | 2.20 (1.30–3.73) | — |
| Severe COVID-19 in one or more family members | 1.57 (1.02–2.41) | 1.52 (1.01–2.30) | 2.14 (1.42–3.23) |
| VASs* | |||
| Compared with previous COVID-19 waves | |||
| This wave is more frightening | 1.22/point (1.13–1.31) | 1.13/point (1.04–1.22) | — |
| This wave is more frustrating | — | 1.10/point (1.02–1.20) | — |
| I was able to spend more time with family | 0.83/point (0.77–0.90) | 0.84/point (0.75–0.94) | — |
| I was able to rest more regularly | — | 0.84/point (0.75–0.94) | 0.82/point (0.74–0.92) |
| I was not able to go on vacation | 1.29/point (1.12–1.49) | 1.17/point (1.00–1.37) | — |
| I worked longer hours | — | — | 1.08/point (1.01–1.16) |
| I had greater pride in my work | 0.59/point (0.43–0.81) | 0.66/point (0.48–0.91) | — |
| End-of-life decisions were more often consensual† | — | — | 0.88/point (0.82–0.94) |
| I experienced greater social frustration | — | 1.10/point (1.02–1.20) | — |
| I thought the infodemic was more distressing | — | — | 1.09/point (1.03–1.15) |
| Time spent reading books/newspapers >1 h/d | 0.69 (0.49–0.97) | 0.46/point (0.32–0.67) | — |
| CD-RISC-10 score | 0.93/point (0.91–0.96) | 0.93/point (0.90–0.9)5 | 0.95/point (0.92–0.97) |
| Area under the curve | 0.76 (0.73–0.79) | 0.79 (0.76–0.82) | 0.75 (0.78–0.84) |
| Hosmer-Lemeshow chi-square test | 0.5396 | 0.8703 | 0.7985 |
Definition of abbreviations: CD-RISC-10 = 10-item Connor-Davidson Resilience Scale; CI = confidence interval; COVID-19 = coronavirus disease; PTSD = post-traumatic stress disorder; VAS = 10-point visual analog scale.
All VASs had two anchors: 0, indicating the absence of symptoms or lowest possible rating, and 10, indicating the worst possible symptoms or highest possible rating.
Consensual was defined as sharing of end-of-life decisions between the family and healthcare professionals.
All tests were two sided, and P values less than 0.05 were considered to indicate statistical significance. Analyses were done using R version 3.6.2 (https://www.r-project.org).
Results
Respondents
Among the 1,300 HCPs working in the 21 participating ICUs, 950 completed the survey. Table 1 details their main characteristics. Among the respondents, 380 (40%) were physicians, 551 (58%) were nursing staff members, and 19 (2%) were other HCPs. Response rates were 73.1% overall, 79.2% among physicians, and 69.5% among nursing staff members. Overall, median ICU experience was 7 (3–14) years. Only 7% of respondents had not worked in ICUs during at least one previous COVID-19 wave. Importantly, only 8% of respondents felt supported by their healthcare institutions.
Mental-Health Symptoms, Experience of the Pandemic, and Resilience
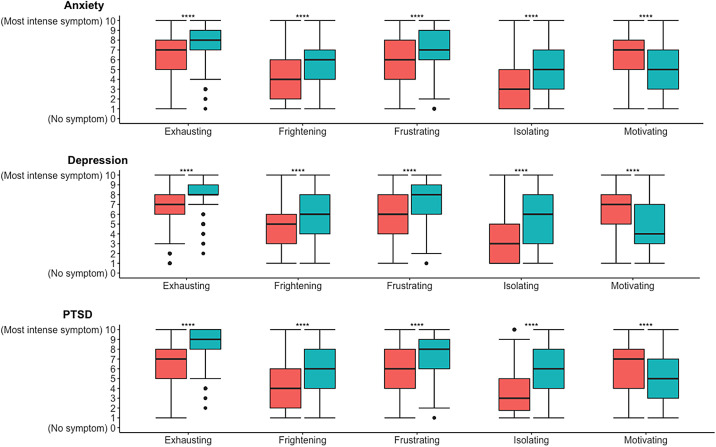
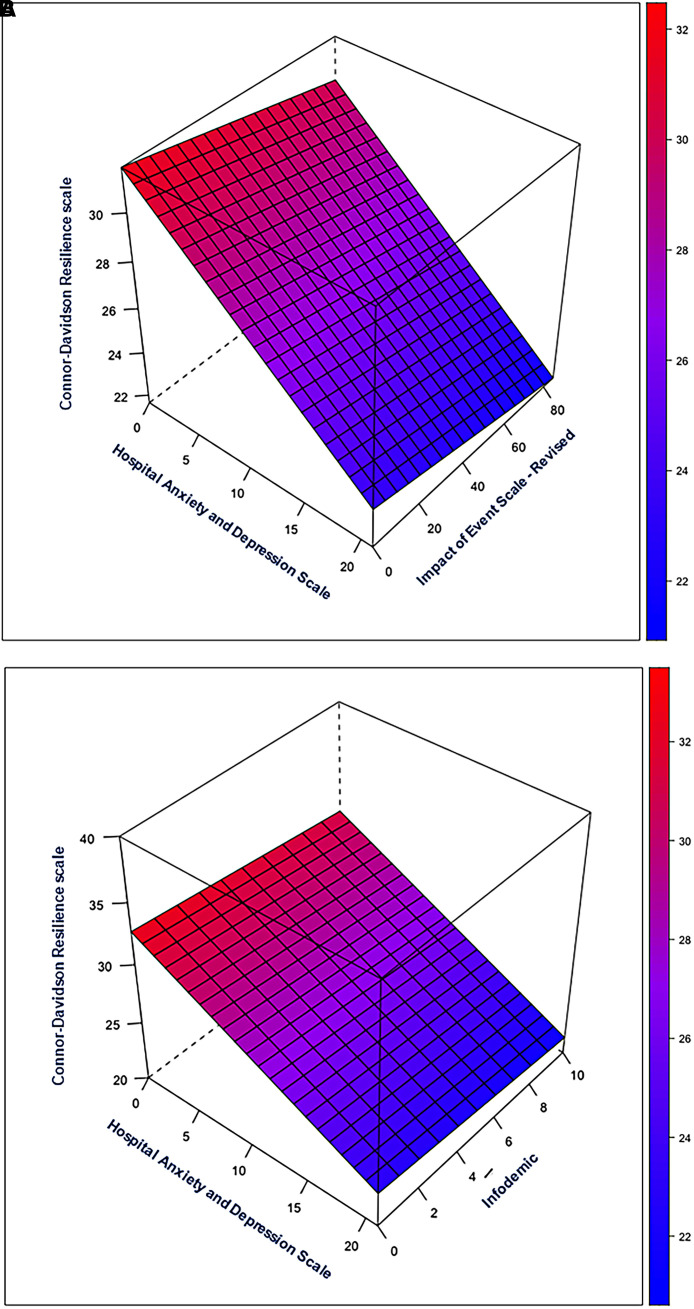
Table 2 reports CD-RISC-10, HADS, and IES-R scores. Anxiety symptoms were significantly more common among residents than for the other job categories (see Figure E1 in the online supplement). Exhaustion, frustration, lack of motivation, fear, and isolation related to the current COVID-19 wave were all significantly associated with symptoms of anxiety, depression, and PTSD (Figure 1). Greater perceived distress related to the COVID-19 infodemic was significantly associated with higher prevalences of depression and PTSD symptoms (see Figure E2). Spending at least an hour a day reading books showed a significant association with lower prevalences of symptoms of anxiety and depression (see Figure E3). A higher CD-RISC-10 score, indicating greater resilience, was independently associated with lower prevalences of symptoms of anxiety, depression, and PTSD (Table 3). The only other variable independently associated with all three categories of symptoms, although in the opposite direction, was severe COVID-19 in at least one family member. Figure 2A depicts the association linking greater resilience to lower prevalences of anxiety, depression, and PTSD symptoms, and Figure 2B indicates a persistent association of greater resilience with lower prevalences of anxiety and depression symptoms at all degrees of infodemic-related distress. Figure E4 depicts the negative correlation linking resilience to symptoms of anxiety, depression, and PTSD.
Table 2.
Mental-Health Symptoms and Resilience Among the 950 Respondents
| Median (Interquartile Range) or n (%) | |
|---|---|
| CD-RISC-10 score* | 29 (25–32) |
| HADS† | |
| Anxiety subscale score | 8 (5–11) |
| HCPs with symptoms of anxiety | 578 (61) |
| Depression subscale score | 5 (3–8) |
| HCPs with symptoms of depression | 366 (39) |
| IES-R‡ | |
| Total score | 14 (5–30) |
| Intrusion subscore | 6 (2–12) |
| Avoidance subscore | 5 (1–10) |
| Hyperarousal subscore | 3 (1–8) |
| HCPs with PTSD-related symptoms | 339 (36) |
Definition of abbreviations: CD-RISC-10 = 10-item Connor-Davidson Resilience Scale; HADS = Hospital Anxiety and Depression Scale; HCP = healthcare professional; IES-R = Impact of Events Scale–Revised; PTSD = post-traumatic stress disorder.
The score on the CD-RISC-10 can range from 0 to 40. No cutoff was used for this study.
The anxiety and depression subscales can each range from 0 to 21.
The total IES-R score can range from 0 to 88. A total score of 22 or more defined symptoms consistent with PTSD. The intrusion and avoidance subscores can each range from 0 to 32 and the hyperarousal score from 0 to 24.
Figure 1.
Intensity of unidimensional variables (this wave is exhausting, frightening, frustrating, isolating, or motivating) assessed using visual analog scales with two anchors: 0 (no symptom/lowest rating) and 10 (most intense symptom/highest rating) among healthcare professionals with (green) and without (red) symptoms of anxiety, depression, and PTSD. PTSD = post-traumatic stress disorder. **** indicates P < 0.001.
Figure 2.
Regression surface plots. (A). Regression surface plot describing the relationships of anxiety, depression, and post-traumatic stress disorder with resilience assessed using the 10-item Connor-Davidson Resilience Scale as the response variable. (B) Regression surface plot describing the relationships of anxiety, depression, and resilience with distress ascribed to the coronavirus disease (COVID-19) infodemic as the response variable. The height of the surface represents the value of the response variable (resilience in A and infodemic-related distress in B).
Determinants of Resilience
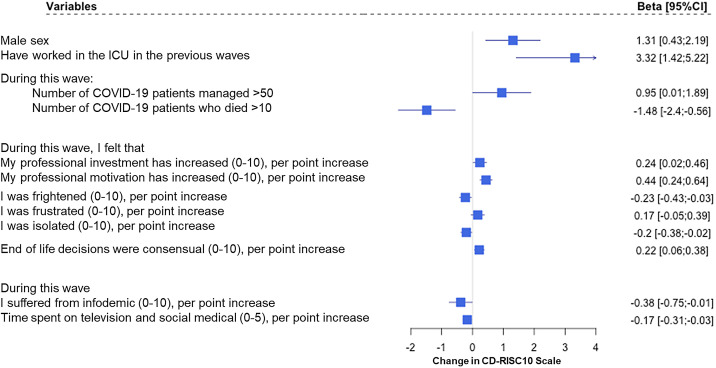
Factors associated with resilience by univariate analysis are shown in Figure E5. By multivariate analysis (Figure 3), factors independently associated with greater resilience were male sex, having worked in the ICU during previous waves, and managing a greater number of patients with COVID-19. Other factors, assessed in comparison with previous waves, were working longer hours, feeling greater motivation, and more often sharing end-of-life decisions with families. Conversely, factors independently associated with lower resilience were having managed more than 10 patients who had died during the current wave, a higher degree of fear or isolation, and greater infodemic-related distress.
Figure 3.
Forest plot showing the results of the multivariate linear regression analysis with CD-RISC 10 score as the dependent variable. Consensual end-of-life decisions were defined as shared between healthcare professionals and the family. CD-RISC 10 = 10-item Connor-Davidson Resilience Scale; CI = confidence interval; COVID-19 = coronavirus disease.
Discussion
In this cross-sectional survey, we assessed resilience in a large sample of HCPs working in 21 French ICUs during repeated COVID-19 waves. The associations linking resilience to the number of patients with COVID-19 managed, personal experience of the pandemic, the end-of-life decision-making process, and response to the infodemic suggest strategies for strengthening the ability of HCPs to cope with adverse working conditions. Greater resilience was associated with fewer symptoms of anxiety, depression, and PTSD. Strengths of our study include the large sample size; the use of validated instruments to assess resilience and symptoms of anxiety, depression, and PTSD; rating of personal experience compared with previous COVID-19 waves; and the identification of factors independently associated with greater resilience.
Two previous studies were conducted in similar samples of French ICUs, in April and May 2020 and in November 2020 (1, 10). From the earliest study to the present study (October to December 2021), the prevalences of anxiety and depression symptoms increased from 50.4% to 61.0% and from 30.4% to 39.0%, respectively. PTSD symptoms were not assessed in the first study; their prevalence increased between the second and third studies from 28.4% to 36.0%. These findings are of great concern, as they indicate that measures to improve the mental well-being of HCPs are either ineffective or not offered. A noteworthy finding is that only 8% of respondents felt supported by their institutions. Of note, the worsening staff shortages in French hospitals in recent years may, independently from COVID-19, have contributed to this increasing ill ease among HCPs.
Compared with a 2020 meta-analysis of psychological symptoms among HCPs during the COVID-19 pandemic, the proportion of respondents with depression was only slightly higher in our study (39% vs. 31.8%), but the prevalences were far higher for anxiety (61% vs. 34.4%) and PTSD-related symptoms (36% vs. 11.4%) (23). A study of 442 HCPs working in Turkey during the first COVID-19 wave demonstrated a prevalence of anxiety closer to ours, of 51.6%, and a higher prevalence of depression, of 64.7% (6). Of 10 ICU nurses in Alabama, 7 met diagnostic criteria for PTSD according to the results of in-depth in-person interviews (4). Interviews may be more sensitive than the IES-R for detecting PTSD.
Few previous studies assessed resilience among HCPs using the CD-RISC-10. Several versions of the Connor-Davidson Resilience Scale have been used, as well as other resilience scales, hindering comparisons. Among 848 hospital HCPs in Japan during the first wave, the median CD-RISC-10 score was 22 (18–27), lower than in our study done during a later wave (29 [25–32]) (24). The score was significantly lower in the group with versus without depression (18 [13–22] vs. 23 [19–29]). Among emergency nurses in the United States, the median CD-RISC-10 score was 29 (20–30) in October and November 2021, in keeping with our results (25). A survey of nurses working in COVID-19 ICUs in India in September 2020 demonstrated a high degree of resilience, with a mean CD-RISC-10 score of 31.23 ± 4.68 (26). Perhaps more important than the degree of resilience is the identification of factors associated with resilience, knowledge of which could inform resilience-building interventions. Hospital directors, administrators, policy makers, and professional societies have a duty to promote the well-being of HCPs at all times, particularly during challenges such as a pandemic (27, 28). Younger and less experienced HCPs being more at risk of burnout, they should be given specific attention.
We suggest five types of intervention. First, all HCPs should have access to multidisciplinary individualized care should they experience work-related distress. Educational sessions designed to encourage awareness among HCPs of fear, frustration, feelings of isolation, decreased motivation, and other signs of mental ill health would be valuable. HCPs should feel free to discuss these signs with their superiors and to seek specific care, including time off work.
Second, ICU directors and head nurses should regularly evaluate their ICU team members for factors associated with mental ill health. Special support could then be provided, for instance, to HCPs who are handling their first COVID-19 wave or who have provided care to more than 10 patients who died of COVID-19. Alternating between COVID-19 ICU sectors and other ICU sectors might provide benefits, although in our study, managing a larger number of patients with COVID-19 was associated with greater resilience. ICU directors and head nurses should also be generous in expressing their gratitude to their staff members.
Third, to decrease infodemic-related distress, ICUs should provide their HCPs with true and up-to-date information on COVID-19 that frees staff members from the need to consult the general media and social media (29). Medical journals and health journalists should commit to providing readily accessible, fact-based information designed for a broad audience. A model for characterizing the many reported infodemic management strategies has been reported (30).
Fourth, hospitals should provide resilience-building training sessions and resilience care centers (14). Several methods may deserve consideration, including role playing, simulation, mindfulness, and formal training (31–33).
Fifth, offering frontline HCPs paid time off to be used for resilience-building activities during pandemic waves would be useful. Unfortunately, the current severe staff shortages are a major obstacle to such an intervention. A recent consensus report suggested to include both general and specific occupational interventions to support healthcare workers’ basic physical needs, lower psychological distress, reduce moral distress and burnout, and foster mental health and resilience (34).
The optimal means of developing resilience remain unclear, however, and further work on this point is urgently awaited. The interventions evaluated so far have varied widely, focusing on the individual (e.g., emotional regulation techniques, stress management, healthy lifestyle, psychological support from a therapist or using online tools), the workplace (e.g., shorter hours, breaks, mentoring, information, partnering less experienced with more experienced HCPs), or both. In a Cochrane mixed-methods systematic review including 16 studies, the level of evidence of effectiveness was deemed low (35). Another review included 44 randomized controlled trials of psychological interventions and again showed that evidence of efficacy was of only very low certainty (25). There is some evidence, chiefly from before-and-after studies among nurses, that combining several interventions into a resilience bundle may improve effectiveness (36–38). On the other hand, a simple 3-hour in-person interactive class on regulating autonomic responses to stress was followed by significant increases in CD-RISC-10 scores in a sample of 104 frontline community and hospital HCPs (39). Other similarly brief and simple interventions have been reported to increase resilience (40, 41, 42). We are not aware of any studies comparing different interventions. Randomized controlled trials are needed to evaluate and compare both simple interventions and more complex bundles designed to improve resilience among HCPs. Resilience-building strategies must strike a fair balance between the personal efforts asked of HCPs (e.g., incorporating mindfulness, relaxation, and exercise practices into their routine) and efforts provided by healthcare institutions (e.g., scheduling changes, paid time off, well-being training sessions provided on paid time).
Post-traumatic growth (PTG) is the occurrence of positive psychological changes produced through adaptation to a traumatic event (42). Although PTG and resilience are different, they correlate positively with each other (43). Thus, when HCPs completed surveys at three time points during the first COVID-19 wave, greater resilience at the first time point predicted greater PTG at the second time point, which in turn predicted greater resilience at the third time point (44). Although this finding is not proof of causality, attention to PTG may be warranted. Little information is available on factors associated with PTG. Some evidence suggests a positive role for social support (45, 46), deliberate reconstructive rumination (47, 48), and psychosocial interventions (47). Work is needed to elucidate the relationships between resilience and PTG and to identify means of enhancing PTG in HCPs.
This study has limitations. First, respondents were solely from France, possibly compromising generalizability, yet the extensive participation of ICUs in a long-standing network yielded a robust 73.1% response rate.
Second, although we did not explore the link between greater resilience and outcomes such as health-related quality of life, job retention, and moral distress, we did evaluate anxiety, depression, and PTSD symptoms, established indicators of mental well-being. Future studies will need to assess health-related quality of life and career-change intentions.
Third, this study demonstrates increased resilience among HCPs with experience in previous COVID-19 waves, those managing higher patient volumes, and those working longer hours. This suggests that less experienced HCPs may have left after prior waves, potentially introducing selection bias. However, this bias may be minimal, as only 7% had not worked in ICUs during previous COVID-19 waves, with a median ICU experience of 7 years.
Fourth, we did not compare respondents who were and were not receiving mental-health care. No center effect possibly related to differences regarding institution-provided support to HCPs was noted. Although respondents cited colleagues, family, and friends as primary social support, this should not be equated with mental-health care.
Fifth, we observed lower resilience scores among women compared with men. One potential explanation is that women may respond to CD-RISC-10 items with less self-affirmation or self-regard, potentially biasing results. This could lead to lower scores among women with similar resilience as men. Although no studies have explored this possibility, existing research consistently demonstrates lower self-esteem among women compared with men (49).
Sixth, HCPs handle challenges uniquely, and there are diverse valid responses to any situation, which resilience may not fully capture. Last, potential endogeneity in the main findings should be considered, as resilience, anxiety, and depression were assessed simultaneously. Notably, the CD-RISC-10 considers the preceding month, while the HADS and IES-R focus on the preceding week. Given substantial intraindividual variability, values from the same time point are crucial for assessing associations. Although resilience is significantly linked to mental-health symptoms, not all respondents with low resilience reported such symptoms, as would be expected in the event of endogeneity. Variables such as sex, COVID-19 exposure, fear, and isolation were also associated with resilience. Similarly, in a 2023 systematic review of 35 studies that assessed resilience and anxiety/depression simultaneously, 8 studies demonstrated no significant associations linking resilience to anxiety and depression (50, 51). We acknowledge that the significant statistical associations reported in our study raise hypotheses but do not constitute evidence of causal links between resilience and mental-health symptoms. Moreover, there is also a potential for reverse causality between the observed associations seen in this work given the cross-sectional nature of the study. Longitudinal studies would help determine how resilience relates to anxiety, depression, and PTSD.
Conclusions
This study among critical-care HCPs identified determinants of resilience that are amenable to change. The results suggest a need for interventions to decrease feelings of fear and isolation, as well as to teach infodemic-coping strategies. The ICU places a heavy burden on HCPs at all times because of the high patient acuity, patient and family suffering, complex care, limited control, ethical dilemmas, and long working hours. The added stress generated by a pandemic is therefore particularly challenging, notably when institutional support and recognition are limited That only 8% of respondents felt supported by their institutions is evidence that hospital managers, ICU heads, and policy makers are not doing enough to develop a workplace culture and interventions aimed at relieving the mental-health burden placed on HCPs. The responsibility falls squarely on them.
Footnotes
Sponsored by French Ministry of Health grant covid-2020-67.
Author Contributions: E.A. and N.K.-B. designed the study and obtained the funding and authorizations. G.D. and F.P. were part of the steering committee and helped design the project and select the metrics and mental health outcomes. L.A., A.C., R.C.-J., O.G., V.L., F.T., F.B., M.J., D.R., K.K., A.K., V.S., A.L., J.B., A.V.B., J.D., L.P., J.R., and F.B. took part in designing the survey instrument, validated the pilot, and guided survey completion in their departments. All authors took part in analyzing the data, raising hypotheses, and guiding the analysis. All authors revised the text for important intellectual content and approved submission of the final version.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202305-0806OC on January 1, 2024
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Azoulay E, Cariou A, Bruneel F, Demoule A, Kouatchet A, Reuter D, et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19: a cross-sectional study. Am J Respir Crit Care Med . 2020;202:1388–1398. doi: 10.1164/rccm.202006-2568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mehta S, Machado F, Kwizera A, Papazian L, Moss M, Azoulay É, et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med . 2021;9:226–228. doi: 10.1016/S2213-2600(21)00068-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open . 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Levi P, Moss J. Intensive care unit nurses’ lived experiences of psychological stress and trauma caring for COVID-19 patients. Workplace Health Saf . 2022;70:358–367. doi: 10.1177/21650799211064262. [DOI] [PubMed] [Google Scholar]
- 5. Moore DJ, Dawkins D, Hampton MD, McNiesh S. Experiences of critical care nurses during the early months of the COVID-19 pandemic. Nurs Ethics . 2022;29:540–551. doi: 10.1177/09697330211043273. [DOI] [PubMed] [Google Scholar]
- 6. Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res . 2020;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Benbenishty J, Ashkenazy S, Levdov Avital I, Jakobson L, Kolpak O, DeKeyser Ganz F. Nurses’ perceptions of social rejection, resilience and well-being during COVID-19: a national comparative study. J Clin Nurs . 2022;31:2189–2197. doi: 10.1111/jocn.16034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Azoulay E, De Waele J, Ferrer R, Staudinger T, Borkowska M, Povoa P, et al. ESICM Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care . 2020;10:110. doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res . 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Azoulay E, Pochard F, Reignier J, Argaud L, Bruneel F, Courbon P, et al. FAMIREA Study Group Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross-sectional study. Chest . 2021;160:944–955. doi: 10.1016/j.chest.2021.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol . 2014;5 doi: 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety . 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 13. Dzau VJ, Kirch DG, Nasca TJ. To care is human—collectively confronting the clinician-burnout crisis. N Engl J Med . 2018;378:312–314. doi: 10.1056/NEJMp1715127. [DOI] [PubMed] [Google Scholar]
- 14. Shaffer KM, Riklin E, Jacobs JM, Rosand J, Vranceanu AM. Psychosocial resiliency is associated with lower emotional distress among dyads of patients and their informal caregivers in the neuroscience intensive care unit. J Crit Care . 2016;36:154–159. doi: 10.1016/j.jcrc.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. DePierro J, Katz CL, Marin D, Feder A, Bevilacqua L, Sharma V, et al. Mount Sinai’s Center for Stress, Resilience and Personal Growth as a model for responding to the impact of COVID-19 on health care workers. Psychiatry Res . 2020;293:113426. doi: 10.1016/j.psychres.2020.113426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rakesh G, Morey RA, Zannas AS, Malik Z, Marx CE, Clausen AN, et al. Resilience as a translational endpoint in the treatment of PTSD. Mol Psychiatry . 2019;24:1268–1283. doi: 10.1038/s41380-019-0383-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Douillet D, Caillaud A, Riou J, Miroux P, Thibaud E, Noizet M, et al. Assessment of physicians’ resilience level during the COVID-19 pandemic. Transl Psychiatry . 2021;11:283. doi: 10.1038/s41398-021-01395-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Roberts NJ, Kelly CA, Lippiett KA, Ray E, Welch L. Experiences of nurses caring for respiratory patients during the first wave of the COVID-19 pandemic: an online survey study. BMJ Open Respir Res . 2021;8:e000987. doi: 10.1136/bmjresp-2021-000987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress . 2007;20:1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 20. Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, et al. French FAMIREA Group Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med . 2001;29:1893–1897. doi: 10.1097/00003246-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 21. Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, et al. FAMIREA Study Group Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med . 2005;171:987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 22. Scales D, Gorman J, Jamieson KH. The COVID-19 infodemic—applying the epidemiologic model to counter misinformation. N Engl J Med . 2021;385:678–681. doi: 10.1056/NEJMp2103798. [DOI] [PubMed] [Google Scholar]
- 23. Batra K, Singh TP, Sharma M, Batra R, Schvaneveldt N. Investigating the psychological impact of COVID-19 among healthcare workers: a meta-analysis. Int J Environ Res Public Health . 2020;17:9096. doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Awano N, Oyama N, Akiyama K, Inomata M, Kuse N, Tone M, et al. Anxiety, depression, and resilience of healthcare workers in Japan during the coronavirus disease 2019 outbreak. Intern Med . 2020;59:2693–2699. doi: 10.2169/internalmedicine.5694-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst Rev . 2020;7:CD012527. doi: 10.1002/14651858.CD012527.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jose S, Cyriac MC, Dhandapani M, Mehra A, Sharma N. Mental health outcomes of perceived stress, anxiety, fear and insomnia, and the resilience among frontline nurses caring for critical COVID-19 patients in intensive care units. Indian J Crit Care Med . 2022;26:174–178. doi: 10.5005/jp-journals-10071-24119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. Taking action against clinician burnout: a systems approach to professional well-being. Washington, DC: National Academies Press; 2019. [PubMed] [Google Scholar]
- 28. Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc . 2017;92:129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 29. Welp A, Manser T. Integrating teamwork, clinician occupational well-being and patient safety—development of a conceptual framework based on a systematic review. BMC Health Serv Res . 2016;16:281. doi: 10.1186/s12913-016-1535-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sundelson AE, Jamison AM, Huhn N, Pasquino SL, Sell TK. Fighting the infodemic: the 4 i framework for advancing communication and trust. BMC Public Health . 2023;23:1662. doi: 10.1186/s12889-023-16612-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rushton CH. In: Moral resilience: transforming moral suffering in healthcare. Rushton CH, editor. Oxford, UK: Oxford University Press; 2018. Conceptualizing moral resilience; pp. 125–149. [Google Scholar]
- 32. Lang KR. The professional ills of moral distress and nurse retention: is ethics education an antidote? Am J Bioeth . 2008;8:19–21. doi: 10.1080/15265160802147181. [DOI] [PubMed] [Google Scholar]
- 33. Rushton CH, Broome ME. Safeguarding the public’s health: ethical nursing. Hastings Cent Rep . 2015;45 doi: 10.1002/hast.410. [DOI] [PubMed] [Google Scholar]
- 34. Sprung CL, Devereaux AV, Ghazipura M, Burry LD, Hossain T, Hamele MT, et al. Task Force for Mass Critical Care Writing Group Critical care staffing in pandemics and disasters: a consensus report from a subcommittee of the Task Force for Mass Critical Care—systems strategies to sustain the health care workforce. Chest . 2023;164:124–136. doi: 10.1016/j.chest.2023.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev . 2020;11:CD013779. doi: 10.1002/14651858.CD013779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Davis M, Batcheller J. Managing moral distress in the workplace: creating a resiliency bundle. Nurse Lead . 2020;18:604–608. doi: 10.1016/j.mnl.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mintz-Binder R, Andersen S, Sweatt L, Song H. Exploring strategies to build resiliency in nurses during work hours. J Nurs Adm . 2021;51:185–191. doi: 10.1097/NNA.0000000000000996. [DOI] [PubMed] [Google Scholar]
- 38. Andersen S, Mintz-Binder R, Sweatt L, Song H. Building nurse resilience in the workplace. Appl Nurs Res . 2021;59:151433. doi: 10.1016/j.apnr.2021.151433. [DOI] [PubMed] [Google Scholar]
- 39. Grabbe L, Higgins MK, Baird M, Pfeiffer KM. Impact of a resiliency training to support the mental well-being of front-line workers: brief report of a quasi-experimental study of the community resiliency model. Med Care . 2021;59:616–621. doi: 10.1097/MLR.0000000000001535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. DeTore NR, Sylvia L, Park ER, Burke A, Levison JH, Shannon A, et al. Promoting resilience in healthcare workers during the COVID-19 pandemic with a brief online intervention. J Psychiatr Res . 2022;146:228–233. doi: 10.1016/j.jpsychires.2021.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kelly LA, Schaeffer R, Roe S, Buchda VL. Using text messages to support nurse well-being. Nurs Adm Q . 2021;45:338–345. doi: 10.1097/NAQ.0000000000000490. [DOI] [PubMed] [Google Scholar]
- 42. Meyerson DA, Grant KE, Carter JS, Kilmer RP. Posttraumatic growth among children and adolescents: a systematic review. Clin Psychol Rev . 2011;31:949–964. doi: 10.1016/j.cpr.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 43.Atay N, Sahin-Bayindir G, Buzlu S, Koç K, Kuyuldar Y. The relationship between posttraumatic growth and psychological resilience of nurses working at the pandemic clinics. Int J Nurs Knowl. 2023;34:226–235. doi: 10.1111/2047-3095.12397. [DOI] [PubMed] [Google Scholar]
- 44. Lyu Y, Yu Y, Chen S, Lu S, Ni S. Positive functioning at work during COVID-19: posttraumatic growth, resilience, and emotional exhaustion in Chinese frontline healthcare workers. Appl Psychol Health Well-Being . 2021;13:871–886. doi: 10.1111/aphw.12276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ning J, Tang X, Shi H, Yao D, Zhao Z, Li J. Social support and posttraumatic growth: a meta-analysis. J Affect Disord . 2023;320:117–132. doi: 10.1016/j.jad.2022.09.114. [DOI] [PubMed] [Google Scholar]
- 46. Dou J, Liu C, Xiong R, Zhou H, Lu G, Jia L. Empathy and post-traumatic growth among Chinese community workers during the COVID-19 pandemic: roles of self-disclosure and social support. Int J Environ Res Public Health . 2022;19:15739. doi: 10.3390/ijerph192315739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Roepke AM. Psychosocial interventions and posttraumatic growth: a meta-analysis. J Consult Clin Psychol . 2015;83:129–142. doi: 10.1037/a0036872. [DOI] [PubMed] [Google Scholar]
- 48. Ryu J-H, Suh K-H. Self-disclosure and post-traumatic growth in Korean adults: a multiple mediating model of deliberate rumination, positive social responses, and meaning of life. Front Psychol . 2022;13:878531. doi: 10.3389/fpsyg.2022.878531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bleidorn W, Arslan RC, Denissen JJA, Rentfrow PJ, Gebauer JE, Potter J, et al. Age and gender differences in self-esteem-a cross-cultural window. J Pers Soc Psychol . 2016;111:396–410. doi: 10.1037/pspp0000078. [DOI] [PubMed] [Google Scholar]
- 50. Yap YY, Sathar J, Law KB, Zulkurnain PAB, Edmund SC, Chang KM, et al. Clinical characteristics and outcomes of thrombotic microangiopathy in Malaysia. Blood Res . 2018;53:130–137. doi: 10.5045/br.2018.53.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yap MC, Wu F, Huang X, Tang L, Su K, Tong X, et al. Association between individual resilience and depression or anxiety among general adult population during COVID-19: a systematic review. J Public Health (Oxf) . 2023;45:e639–e655. doi: 10.1093/pubmed/fdad144. [DOI] [PubMed] [Google Scholar]