Abstract
One of the most difficult procedures in interventional cardiology is the percutaneous coronary intervention (PCI) on a chronic total occlusion (CTO) lesion case. To rate the difficulty of guidewire crossing, several angiographic scoring methods have been developed such as the Japan CTO (J-CTO) score. Here we demonstrate the advantages of revascularization using PCI procedure in a CTO case with intractable heart failure. A 53-year-old man presented to the emergency room of Dr. Zainoel Abidin Hospital, Banda Aceh, Indonesia with acute decompensated heart failure. The patient had a history of past PCI with two patent drug eluting stents (DES): one in the left main (LM)-left anterior descending (LAD) artery and one in the distal left circumflex (LCX) artery. The patient had three times rehospitalizations in the last three months. According to single-photon emission computed tomography (SPECT) imaging, the right coronary artery was remained functional; however, the lesion was categorized into very difficult level (J-CTO >3). The PCI was carried out on the right coronary artery and the blood vessel was successfully revascularized after applying multiple techniques. Following the procedure, the heart failure was treated and the 6-minute walking test (6MWT) that performed 12 days after the PCI increased from 220 to 260 meters. The success of this case depended on a comprehensive history taking, adequate imaging methods, and the selection of the proper tools and PCI strategy. In conclusion, despite the challenges, PCI is still an option for patients with persistent complete occlusion. The PCI requires comprehensive preparation and the use of angiographic scoring systems, such as the J-CTO score, to determine the approach and the likelihood of success.
Keywords: CTO, PCI, heart failure, revascularization, J-CTO
Introduction
Patients with heart failure and a low ejection fraction frequently develop a chronic total occlusion (CTO) lesion [1]. A study found that percutaneous coronary intervention (PCI) reduced the morbidity and mortality more effectively than optimal medical care on heart failure cases [1,2]. About 18–52% of patients with coronary heart disease who undergo coronary angiography have CTO [3]. However, CTO PCI only makes up approximately 5% of PCI procedures in current worldwide practices [4].
The CTO PCI is one of the most challenging interventions in interventional cardiology. The PCI procedure in CTO cases requires more time, resources and radiation exposure; and has higher risk of complications compared to non-CTO PCI. Most interventional cardiologists rarely conduct CTO PCI due to its complexity, the length of time and uncertainty about the procedure’s success rate [4]. The availability of easy-to-use markers to determine the success of CTO PCI for each patient may help to lessen the uncertainty. To establish a clear clinical indication, patients should undergo a thorough pre-procedural evaluation that includes tests for symptoms, ischemia, and viability [2].
Angiographic scoring systems and CTO PCI algorithms can be used to select the best PCI strategy during preoperative planning [5]. A study combined baseline clinical data and angiographic data into a 5-point grading system (vessel entry shaped, present of calcification, present of vessel bending, occlusion length and re-try lesion) to establish the Japan CTO (J-CTO) score [5]. The goal of this score system is to assess the difficulty of the CTO crossing. The J-CTO score is used to assess the 30 min CTO crossing difficulty as well as its overall success rate [4,6]. For guidewire CTO crossing within 30 min, a cohort revealed that the J-CTO score had high discriminatory and calibrating capacity for CTO guidewire, but not for success rate [5]. The J-CTO score is a popular clinical assessment because it is simple to use and it could predict the complexity of CTO recanalization [7]. Another multicentre registry demonstrated that the J-CTO score was able in predicting the efficacy and success of CTO PCI [8]. A high J-CTO score is associated with greater chance of technical failure [8].
The aim of this case report was to highlight the challenges and the success of the PCI in a CTO patient. We present a 53-year-old male who has been submitted several times to the hospital for chest pain and had undergone previous PCI with one drug eluting stent (DES) each in left main (LM)-left anterior descending (LAD) artery and distal left circumflex (LCX) artery.
Case
In October 2022, a 53-year-old man who was experiencing usual chest pain and breathing difficulties presented to the emergency department of Dr. Zainoel Abidin Hospital, Banda Ache, Indonesia. The patient recently had PCI for coronary artery disease in LM-LAD and LCX arteries and had recently been discharged from the hospital with unstable angina pectoris and decompensated heart failure. The patient had no diabetes mellitus and hypertension. The heart rate was 97 beats per minute and blood pressure 101/69 mmHg. Gallop and congestion symptoms were detected during the physical examination
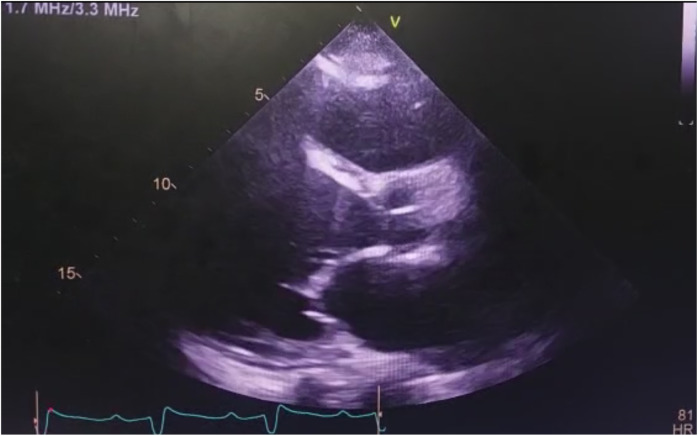
An electrocardiogram (ECG) was performed, and it revealed sinus rhythm with a complete right bundle branch block, an old inferior infarct in the inferior segment, and premature atrial contraction. Echocardiography that performed 2 days before PCI revealed left ventricular ejection fraction (LVEF) was reduced by a biplane (24–29%), with akinetic segments in the anteroseptal, anterior, apical regions, and hypokinetic in the other segments (Figure 1). The patient had a history of cardiac single-photon emission computed tomography (SPECT) imaging of which heart motions were dyskinetic at the apex and apicolateral segment; akinetic in the apico-anterior, mid-anterior, and mid-anterolateral segments; and reversible ischemia at right coronary artery (RCA) region.
Figure 1. Echocardiography revealed enlargement of left ventricle with reduced left ventricular ejection fraction (LVEF).
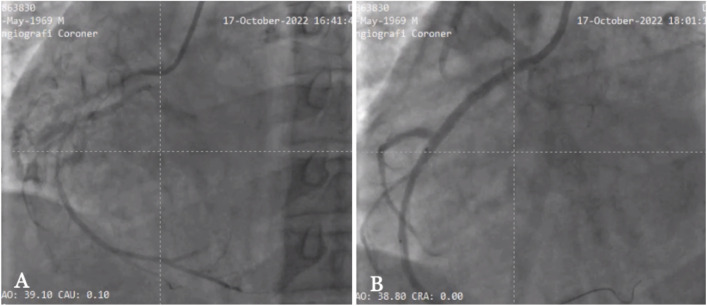
After four days admitted, coronary angiography was performed and revealed CTO in proximal RCA with J-CTO score 4 (blunt entry shaped, present of calcification, vessel bending >45 degrees and occlusion length >20 mm) (Figure 2A) that categorized the lesion to very difficult level (J-CTO >3). PCI was performed on the RCA through cannulation with Amplatzer Left (AL) 1.0/6F guiding. Wiring was conducted with an intermediate wire but the lesion was difficult to be penetrated; and the penetration the lesion was able to conducted after using a backup balloon technique (1.0/15 mm balloon). Pre-dilatation was performed several times, followed by step up to non-compliant scoring balloon 2.5/15 mm. Due to osteal lesion and target proximal landing zone to osteal RCA, catheter was changed to Judkin right (JR) 3.5/6F followed by stenting with a DES 2.75/38 mm at osteal proximal and a 2.5/24 mm stent to proximal mid area. The angiographic evaluation showed TIMI (Thrombolysis In Myocardial Infarction) 3 flow distally and the patient was hemodynamically stable (Figure 2B).
Figure 2. Coronary angiography of the patient with chronic total occlusion (CTO) before and after percutaneous coronary intervention (PCI). (A). Coronary angiography shows CTO in proximal part of right coronary artery (RCA) with collateral to mid part. (B) Restoration flow of CTO in RCA after PCI procedure.
Post PCI, the cardiac rehabilitation program was performed, and patient had significant increase of 6-minute walking test (6MWT) from 220 meters to 260 meters that performed 12 days after procedure. During follow up, no event of major adverse cardiovascular events (MACE) in first 6 months after PCI.
Discussion
CTO cases present between 15% to 30% of patients having coronary angiography [9] and complete revascularization was associated with a decrease in cardiovascular and cerebrovascular events from 9.7% to 24.2% following PCI [9]. Along with symptom assessment, the diagnosis of ischemia and the viability of the myocardium are the crucial first steps. The evaluation of ischemia in asymptomatic patients is taken into account before CTO PCI since the patients who may benefit from CTO recanalization depends on the myocardial viability. Combining viability metrics may be able to predict myocardial function more accurately than using just one viability parameter only [2]. In our case, a nuclear imaging technique SPECT scan was used to assess the myocardial function. Since the presence and extent of viable myocardium have evolved into an important clinical strategy for determining the need for revascularization and predicting the improvement in patient’s clinical outcome regarding LV function recovery, symptoms, and survival, non-invasive myocardial imaging is crucial in the evaluation of viable myocardium in patients with CAD and LV dysfunction [10].
In the LM and LCX arteries, our patient already had stent placements. If symptoms are present or there is evidence of viability or ischemia in the vicinity of the occluded artery, recanalization of the CTO should be taken into consideration. Revascularization in CTOs is intended to ameliorate symptoms and/or prognosis. In this case, we concluded that the RCA was still viable based on the results of the SPECT and echocardiogram; therefore PCI on the RCA was conducted. According to the guidelines for the care of stable coronary disease, the indications for CTO revascularization should be the same as those for a subtotal stenosis if viability, ischemia of a sufficiently large territory, and/or angina symptoms are present [2].
The type of approach and the likelihood of success must be determined during procedure planning using angiographic scores. The J-CTO score is the oldest and most well-known. Patients with higher J-CTO scores have longer procedures, use more contrast, and more frequently use the retrograde technique, all of which significantly lower the success rates [2]. With a blunt entry form, calcification, and an occlusion length of more than 20 mm, this case has a J-CTO score of 3, suggesting that it is a challenging one.
Through cannulation and AL 1.0/6F guiding from the femoral approach, PCI was carried out on the RCA. The passive-type Amplatz L (AL) catheter is appropriate for the RCA. Its large tip allows it to be inserted relatively deeply into the coronary artery [15]. Catheter size, catheter form, and the amount of backup support needed are three factors to consider when choosing a guide catheter [16].
Most operators favour the femoral technique as their primary access route for CTO reduction. Standard guide catheters are believed to give insufficient backup support, which is why trans radial intervention has not been employed commonly. Particularly in the elderly [16], it is challenging to advance along and operate the complex radial route to the desired objective. The operator may, however, prefer the radial approach in cases of severe peripheral vascular disease or for contralateral injection [17].
Wiring was done using an intermediate wire; however, it cannot pass through the lesion. The stainless-steel polymer jacket wire used as the fighter guidewire has a hydrophilic coating. Even though hydrophilic coatings need water to become slippery, once wet, they exhibit incredibly low coefficients of friction. Back up balloon technique was used to extend the support wire and was successful in penetrating the lesion distally [18, 19].
DES were used for stenting in the proximal and middle RCA base of the vessel’s narrowing area. Due to their effectiveness in treating other challenging lesion morphologies and the clinical limitations of bare metal stents in preserving restenosis-free patency in this particular lesion subset, DES appear promising for improving long-term vascular patency after CTO recanalization. DES are recommended for CTO PCI due to the lower rate of angiographic restenosis when compared to bare metal stents [2,4,9].
We encountered challenges penetrating the lesion during the PCI operation. In the end, the lesion was effectively pierced with the use of backup balloons, allowing for the RCA to receive a DES. A number of factors have been linked to the inability to cross CTO lesions, including the presence of calcification, a blunt entry point, bending at the obstruction site, the absence of bridging collaterals, the length of the lesions, the duration of the obstruction, and the presence of a side branch. For complex CTO lesions, longer durations and more frequent use of advanced crossing procedures, such as the retrograde approach and antegrade dissection and re-entry, are more likely to be required [6].
Conclusion
CTO PCI could reduce the incidence of cardiac death compared to optimal medical therapy in patients with CTO. In patients with CTO, PCI is still a possible option, despite the difficulties. Preparation and the use of angiographic scoring system, such as the J-CTO score, to estimate the probability of success and the type of approach is essential in the planning of CTO PCI.
Acknowledgments
None.
Ethics approval
Not applicable for case report. Informed consent was directly obtained from the patient for the publication of this report.
Competing interests
The authors declare that there is no conflict of interest.
Funding
This study received no external funding.
Underlying data
All data underlying the results are available as part of the article and no additional source data are required.
How to cite
Munirwan H, Kusyanto FA, Zanisa Z, et al. Chronic total occlusion percutaneous coronary intervention (CTO PCI) in an intractable heart failure patient: Is there any benefit? Narra J 2023; 3 (2): e140 - http://doi.org/10.52225/narra.v3i2.140.
References
- 1.Parikh P, Bhatt D, Bhasin V, et al. Impact of percutaneous coronary intervention on outcomes in patients with heart failure. J Am Coll Cardiol 2021. 77 (19) 2432–2447. [DOI] [PubMed] [Google Scholar]
- 2.Salinas P, Gonzalo N, Moreno VH, et al. Choice of CTO scores to predict procedural success in clinical practice. A comparison of 4 different CTO PCI scores in a comprehensive national registry including expert and learning CTO operators. PloS ONE 2021. 16(4): e0245898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ybarra LF, Cantarelli MJC, Lemke VMG, et al. Percutaneous coronary intervention in chronic total occlusion. Arq Bras Cardiol 2018;110(5):476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan C, Yang W, Song L, et al. Association of acute procedural results with long-term outcomes after CTO PCI. JACC Cardiovasc Interv 2021;14(3):278–88. [DOI] [PubMed] [Google Scholar]
- 5.Morino Y, Abe M, Morimoto T, et al. J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv 2011. Feb;4(2):213–221. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka H, Tsuchikane E, Muramatsu T, et al. A novel algorithm for treating chronic total coronary artery occlusion. J Am Coll Cardiol 2019;74(19):2392–404. [DOI] [PubMed] [Google Scholar]
- 7.Javaid SY, Ali I, Khattak TH, et al. Utility of J-CTO Score in predicting the procedural outcomes in coronary chronic total occlusion interventions: an experience at AFIC/NIHD. Pak Armed Forces Med J 2019;69:87–90. [Google Scholar]
- 8.Nombela-Franco L, Urena M, Jerez-Valero M, et al. Validation of the J-chronic total occlusion score for chronic total occlusion percutaneous coronary intervention in an independent contemporary cohort. Circ Cardiovasc Interv 2013;6(6):635–643. [DOI] [PubMed] [Google Scholar]
- 9.Christopoulos G, Wyman MR, Alaswad K, et al. Clinical utility of the Japan-chronic total occlusion score in coronary chronic total occlusion interventions results from a multicenter registry. Circ Cardiovasc Interv 2015;8(7): e002171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galassi A, Grantham A, Kandzari D, et al. Percutaneous Treatment of coronary chronic total occlusions part 1: rationale and outcomes. Interv Cardiol Rev 2014;9(3):195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elfigih IA, Henein MY. Non-invasive imaging in detecting myocardial viability: Myocardial function versus perfusion. Vol. 5, IJC Heart and Vasculature. Elsevier Ireland Ltd; 2014:51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Budoff MJ, Rasouli ML, Shavelle DM, et al. Cardiac CT angiography (CTA) and nuclear myocardial perfusion imaging (MPI)-A comparison in detecting significant coronary artery disease. Acad Radiol. 2007;14(3):252–257. [DOI] [PubMed] [Google Scholar]
- 13.Abbott BG, Case JA, Dorbala S, et al. Contemporary cardiac SPECT imaging-innovations and best practices: An information statement from the American Society of Nuclear Cardiology. Circ Cardiovasc Imaging 2018. 1;11(9):e000020. [DOI] [PubMed] [Google Scholar]
- 14.Rallidis LS, Makavos G, Nihoyannopoulos P.. Right ventricular involvement in coronary artery disease: Role of echocardiography for diagnosis and prognosis. Am Soc Echocardiogr 2014;27(3):223–239. [DOI] [PubMed] [Google Scholar]
- 15.Shalbaf A, Behnam H, Alizade-Sani Z, et al. Automatic classification of left ventricular regional wall motion abnormalities in echocardiography images using nonrigid image registration. J Digit Imaging 2013;26(5):909–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watson TJ, Ong PJL, Tcheng JE, editors. Primary angioplasty: A practical guide. Singapore: Springer; 2018. [PubMed] [Google Scholar]
- 17.Prashant PU. Current and emerging catheter technologies for percutaneous transluminal coronary angioplasty. Res Rep Clin Cardiol 2014;5:213–226 [Google Scholar]
- 18.Galassi A, Grantham A, Kandzari D, et al. Percutaneous treatment of coronary chronic total occlusion part 2: Technical approach. Interv Cardiol Rev 2014;9(3):201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buller CE. Coronary guidewires for chronic total occlusion procedures: Function and design. Interv Cardiol (London). 2013;5(5):533–540. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required.