Abstract
Background and study aims In cases of inaccessible papilla, EUS-guided biliary drainage (EUS-BD) has been described as an alternative to calibrate benign biliary stenosis. However, few studies are available.
Patients and methods This tw-center, retrospective study was designed to evaluate technical success and clinical success at 1 year. All patients who underswent EUS-BD without the rendezvous technique used for calibration of benign biliary stenosis were included from 2016 to 2022. Patients underwent EUS-hepaticogastrostomy (EUS-HGS) during the first session. Then, HGS was used to access the bile duct, allowing calibration of the stenosis: Dilation of the biliary stenosis and placement of double pigtail stents through the stenosis for 1 year.
Results Thirty-six patients were included. Technical success was 89% (32/36), with four failures to cross the stenosis but EUS-HGS was performed in 100% of the cases. Nine patients were excluded during calibration because of oncological relapse in six and complex stenosis in three. Three patients had not yet reached 1 year of follow-up. Twenty patients had a calibration for at least 1 year. Clinical success after stent placement was considered in all cases after 1 year of follow-up. Thirteen patients underwent stent removal and no relapse occurred after 435 days of follow-up (SD=568). Global morbidity was 41.7% (15/36) with only one serious complication (needing intensive care), including seven cases of cholangitis due to intrabiliary duct obstruction and five stent migrations. No deaths were reported.
Conclusions EUS-BD for calibration in case of benign biliary stenosis is an option. Dedicated materials are needed to decrease morbidity.
Keywords: Pancreatobiliary (ERCP/PTCD), Strictures, Biliary tract, Endoscopic ultrasonography, Intervention EUS
Introduction
For benign biliary stenosis, endoscopic retrograde cholangiopancreatography (ERCP) plus placement of multiple plastic and covered metal stents is considered the standard treatment 1 . This calibration over 1 year excludes patients with inaccessible papilla.
Since the first hepaticogastrostomy (HGS) in 2001 2 , the procedure has gradually replaced percutaneous drainage for malignant lesions due to the lower risk of morbidities reported in randomized studies 3 . The safety of endoscopic ultrasound (EUS) has also improved due to the increasing number of EUS-HGS procedures being performed 4 .
EUS-guided biliary drainage (EUS-BD) has become a valuable option for gaining access to the bile duct in patients with benign disease of the bile duct and inaccessible papilla 5 . EUS-HGS or EUS-hepaticojejunostomy (EUS-HJS) is being increasingly performed to gain access to the bile duct 6 .
EUS-BD has been described as a feasible method for gaining access to the bile duct to manage bile duct lithiasis 7 8 9 10 11 12 13 14 .
Some scholars, including members of our team, have published promising studies about the possibility of calibrating biliary stenosis using EUS-BD 15 16 17 18 . Most of these publications are pilot studies with very few patients and a short follow-up period. In this context, we designed our study to evaluate the technical and long-term clinical success of benign bile duct calibration with EUS-BD.
Patients and methods
Eligibility criteria
In accordance with our inclusion criteria, we selected patients who underwent EUS-BD for benign biliary stenosis calibration from May 2016 to May 2022 in two tertiary expert centers (Institut Paoli Calmettes, Marseille, France; CHUV-Centre Hospitalier Universitaire Vaudois-, Lausanne, Switzerland) ( Fig. 1 ). The exclusion criteria were neoplastic bile duct stenosis, complex stenosis, and follow-up <1 year. Patients who underwent rendezvous techniques were excluded because calibration was performed via ERCP after the rendezvous procedure.
Fig. 1.
Patient selection flowchart.
Patients were identified by searching their medical records for key words such as “hepatico gastrostomy” or “hepaticojejunostomy”. All patients from Paoli Calmettes Institute were identified using the full text with ConSoRe software. ConSoRe is a new generation of big data health software developed by Unicancer, one of Europe’s largest cancer research organizations. ConSoRe employs artificial intelligence based on machine learning and natural language processing. Data were analyzed and collected using Endobase and Soarian software in CHUV. After identifying patients who underwent EUS-BD procedures, only those with benign stenosis of the bile duct were selected using data in computerized patient files.
All patient data were collected retrospectively using the hospital’s prospectively established computerized patient file and, in the absence of recent data, by contacting the patients’ physicians or referring gastroenterologists or the patients themselves.
Study objectives
The main goals were technical success and clinical success at 1 year postoperatively. The secondary objectives were technical and clinical success of the first procedure, including the creation of transhepatic access (HGS), duration of calibration, number of patients who underwent stent removal, number of pigtail plastic stents used, morbidity rate, mortality rate, number of general anesthesia procedures, total duration of hospitalization, number of endoscopies scheduled and unscheduled, and rate of recurrence after stent removal.
EUS-BD technique
The technique was described in a previous paper ( Fig. 2 , Fig. 3 , Fig. 4 , Fig. 5 ). 15 . The procedure was implemented in two steps. The first stage was placement of a fully-covered self-expandable metal stent (SEMS) using the HGS/HJS technique under EUS and x-ray guidance. An antimigration double-pigtail stent was added. This antimigration stent could be placed at the site of stenosis if the wire easily crossed the stenosis. The second stage was ideally performed 1 month later (at the discretion of the endoscopists) and involved the placement of double-pigtail plastic stents from the stomach/jejunum to the duodenum/jejunum through biliary stenosis/hepaticojejunal anastomotic stenosis. Endoscopic reevaluation was performed every 3 months to remove the stent, dilate the balloon, and place new double-pigtail stents. The goal of the calibration was stent removal after 1 year. In stent exchange, previous stents (metal stents or plastic stent) need to be removed, the fistula should be cannulated with a wire because of the orientation of the fistula created with the echoendoscope, and then the anastomosis and fistula should be dilated to compensate for movement of the scope in the stomach. Because the fistula has already been created, there is no bile leakage and the time of the procedure is standardized so the hospital stay is only 1 day.
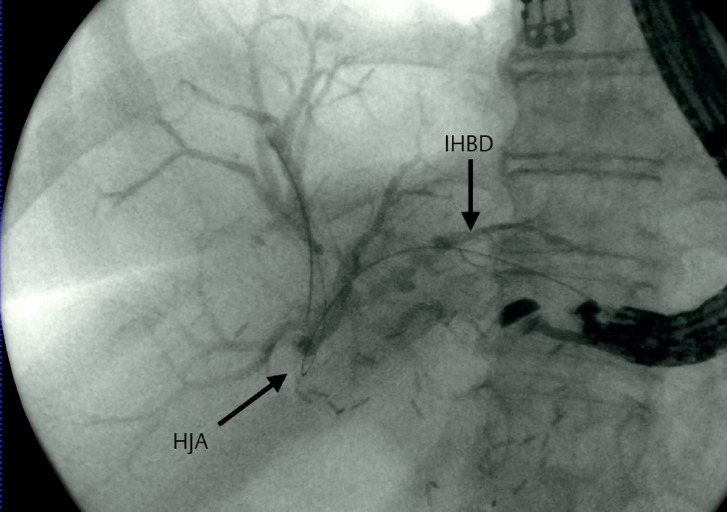
Fig. 2.
Opacified IHBD after puncture. Wire not crossing HJA. IHBD=Intra Heptaic Biliary Duct; HJA=Hepatic Jejunal Anastomosis.
Fig. 3.
Metal stent after 1st HGS.
Fig. 4.
Metal stent with double flare to prevent migration.
Fig. 5.
Placement of 3 pigtail plastic stents to calibrate HJA.
Definitions
Follow-up ended in May 2022 or at the death of the patients. Morbidity was defined as the rate of complications in the first month following the first stage of the procedure, and complications were graded according to the Clavien-Dindo classification 19 . Mortality was defined as the number of deaths in the first month following the first stage of the procedure. Technical success was defined as successful placement of a covered metal stent during the first stage of either HGS or HJS and successful crossing of the stenosis during the 1st or following procedure. Clinical success was defined as disappearance of symptoms and/or normalization of the patient’s condition at 2 months after the procedure.
Iatrogenic cholangitis was defined as cholangitis caused by intrabiliary duct obstruction due to the covered stents causing visible dilation of the intrabiliary duct on the computed tomograph scan. ( Fig. 6 , Fig. 7 ). Complex stenosis was defined as multiple stenoses, including stenosis of the biliary branch ducts.
Fig. 6.
Iatrogenic cholangitis with dilation of IHBD due to obstruction of IHBD.
Fig. 7.
Iatrogenic cholangitis due to dilation of IHBD obstructed by metal stent.
Statistical analysis
The data were collected using Microsoft Excel software. Descriptive statistics were expressed as means with extremes. For quantitative data, medians and means were calculated, and percentages and frequencies were calculated for qualitative data.
Statistical tests were carried out with SAS Enterprise Guide v8.3 software. Pearson’s chi-squared test, or Fisher’s test when necessary, was used to compare the nominal qualitative data.
The Wilcoxon test was used for the comparison of ordinal qualitative data. A Student’s t test was conducted to compare quantitative data. A significance level of P <0.05 was used to compare similarities between the two groups as well as differences in intervention outcomes.
The primary outcome was extraction of stents and associated materials during the first year after the procedure. Patients with unknown status were excluded. Missing primary or secondary data were not imputed.
Ethical considerations
Approval was obtained from the Institutional Review Board and the local medical ethics committee. The Institutional Review Board number was obtained (HEPATICOBENINO2-IPC 2021–086).
Outcomes
Patient and procedure characteristics
Thirty-six patients who underwent EUS-BD for benign biliary stenosis were enrolled.
Patient characteristics
Altered anatomy was the cause for EUS-BD in 34 patients, but for two patients, the cause was duodenal stenosis due to chronic pancreatitis.
Altered anatomy was a consequence of surgery for malignancy in 19 patients and for benign disease in 15 patients (2 patients with benign disease had duodenal stenosis).
The indications for biliary drainage were cholangitis for 29 patients (80.6%) (including 1 patient with liver abscess), cholestasis for three (8.3%), and jaundice for one patient (2.8%), and one patient asked for EUS-BD because of the discomfort of percutaneous drainage.
Twenty-four patients had a Karnofsky index ≥80% and four had a Karnofsky index ≤40%. The American Society of Anesthesiologists score was 1 to 2 for 16 patients (44.4%). Two patients (5.6%) had an ASA score of 4.
Detailed characteristics are shown in Table 1 .
Table 1 Patient characteristics.
| Characteristic | Variable | Subvariable | Number n=36 |
| Sex | Male | 20 (55.6%) | |
| Female | 16 (44.4%) | ||
| Age | Mean (SD) | 68.9 (13.8) | |
| IMC | Mean (SD) | 22 (4.5) | |
| Stenosis localization | HJA | 32 (88.9.7%) | |
| MBD | 4 (11.1%) | ||
| Altered anatomy | No | 2 (5.6%) | |
| Yes | 34 (94.4%) | ||
| Type of surgery (n=34) | Whipple surgery | 18 (52.9%) | |
| Total pancreatectomy | 2 (5.9%) | ||
| Right hepatectotmy with hepatico-jejunal anastomosis | 2 (5.9%) | ||
| Partial gastrectomy (Bilroth 2) | 1 (2.9%) | ||
| Gastrectomy | 1 (2.9%) | ||
| Another cause of hepatico-jejunal anastomosis | 9 (26.5%) | ||
| Surgical pathology | Malignant pathology | 19 (52.8) | |
| Pancreatic adenocarcinoma | 8 (42%) | ||
| Cholangicarcinoma | 3 (15.8%) | ||
| Gastric adenocarcnima | 2 (10.5%) | ||
| Pancreatic neuroendocrine tumors | 2 (10.5% | ||
| Duodenal adenocarcinoma | 1 (5.2%) | ||
| Ampulloma carcinoma | 1 (5.2%) | ||
| Gallbladder carcinoma | 1 (5.2%) | ||
| Colonic liver metastases | 1 (5.2%) | ||
| Benign pathology | 17 (47.2%) | ||
| Post biliary surgery (8 post cholecystectomy and 1 post repair surgery of abdominal trauma) | 9 (47.1%) | ||
| IPMN | 4 (23.5%) | ||
| Inflammatory stenosis | 4 (23.5%) | ||
First hepaticogastrostomy characteristics
Thirty-five patients underwent HGS and one patient underwent HJS. The covered metal stent was 8 cm in length for 21 patients (61.8%) and 10 cm in length for 10 patients (29.4%) (3 missing data points). An antimigration double-pigtail stent was placed in 29 of 34 patients (85.3%). The mean hospital stay was 7.7 days (SD 8.0). The SEMS was removed after a mean of 12.3 days (SD 17.7). Early stent removal was performed five times on Days 4, 5, 7, 12 and 15 due to iatrogenic cholangitis.
Results
Thirteen patients were excluded during calibration, five because of oncological relapse during calibration, four because of failure to cross the stenosis, two because of complex stenosis (stenosis of the right biliary duct needing percutaneous drainage associated), and two because of changes in performance status for another cause (radiotherapy complication for one and potential oncological relapse without evidence for the other) ( Fig. 8 ).
Fig. 8.
Results of included patients.
Three patients were followed for <1 year after calibration, which is ongoing. As a result, 20 patients underwent calibration for 1 year. The clinical success rate at 1 year after HGS was 100%. The technical success rate was 89% (32/36). The stenosis was crossed in 17 patients (47.2%) during the first HGS/HJS. Stenosis was never crossed in four patients. HGS/HJS was successfully performed after two attempts in two patients and after three attempts in one patient. Among these patients, two underwent percutaneous drainage with external drainage to help HGS.
The success rate for HGS was 100%. Clinical success was defined as the disappearance of symptoms and was achieved in 100% of patients who underwent HGS. Definitive stents ablation was obtained in 13 of 20 patients (65%). No relapse occurred in the 13 patients with stent removal after 435 days of follow-up (SD 68). The mean number of pigtail stents placed was 2.7 (SD 0.8). The maximum number of stents placed was four. The mean duration of calibration (patients with stent removal) was 330 days (SD 105).
Morbidity
First HGS morbidity
Mainly only moderate complications were reported. No deaths were reported ( Table 2 ). The global morbidity rate was 67% (24/36). Only one patient (3%) had a serious complication (grade IV), nine patients (37.5%) patients developed grade II Clavien-Dindo complications, and 15 patients (41.7%) developed grade IIIB or higher complications ( Table 3 ). A large proportion of these complications were iatrogenic cholangitis—46% of the IIIB complications. In other words, iatrogenic cholangitis requiring new endoscopy occurred in 20% of patients who underwent the HGS procedure.
Table 2 Calibration morbidity.
| Morbidity of the first procedure (HGS) | 65% |
| mean of total hospitalization (SD)/patient | 25.5 days (4.0) |
| Mean scheduled calibration/patient | 3.5 (2.6) |
| Mean emergency endoscopic stent change/patient | 2.1 (2.1) |
| Mean anesthesia/patient | 5.9 (4.0) |
Table 3 Types of complications post HGS.
| IIIb | IVa | Date | Treatment | |
| HGS, hepaticogastrostomy; D, day. | ||||
| Stent migration | 5 | D1, D5, D7, 2 at D21 | Placement of an additional covered stent | |
| Experimental cholangitis | 7 | D4, D5, D7, D7, D12, D15, D25 | Ablation of the covered stent and placement of plastic stent (double pig tail) | |
| Bleeding | 2 | D7, D15 | Endoscopic hemostasis | |
| Cholecystitis | 1 | D7 | Percutaneous drainage | |
| Intensive care | 1 | D0 | Antibiotic therapy | |
Minor complications (Clavien-Dindo grade 2) included fever (8 patients), bacteremia (4 patients; all of them managed with antibiotics), and bladder infection (1 patient). All complications were managed with conservative treatment or repeat endoscopy.
Significantly more patients who did not undergo stent removal after 1 year developed grade IIIB complications (P=0.02)
Calibration
The mean hospital time per patient, including all management, was 25.5 days (SD 20.9), and there were 2.1 (SD 2.1) unscheduled calibrations per patient because of cholangitis. The total number of procedures performed under anesthesia per patient was 5.6 (SD4).
Discussion
To our knowledge, this project is the largest study of the management of benign biliary stenosis using EUS-BD. As we previously noted, standard management involves calibration with ERCP 1 . In cases of papilla inaccessibility with ERCP, other techniques have been described.
Percutaneous placement of an external internal drain (percutaneous transhepatic cholangiography [PTCD]) is the typical alternative to ERCP. The rate of complications is up to 25%, with a 3-year recurrence rate of 34%, and patients experience serious discomfort due to permanent access to the bile duct 20 21 .
Redo surgery is described as an alternative in cases of ERCP failure. The rate of long-term resolution is up to 84%, but the recurrence rate is also described as being as high as 45%. The morbidity rate is reported to range from 9% to 67% and the mortality rate is reported to be 3% 22 23 .
Another alternative is e-ERCP (enteroscopy-assisted ERCP). This technique is time-consuming and must be repeated for each stent exchange. In addition, the risk of perforation is estimated to range from 3.5% to 11% for each procedure 24 25 .
EUS-BD calibration has a substantial risk of morbidity in the first stage and the risk of morbidity after subsequent stent exchange is lower than that of e-ERCP. In contrast to PTCD, internal drainage with EUS-BD without an external drain offers a very relevant advantage for the patient, and because of the very high morbidity rate and risk of mortality associated with surgery, calibration with EUS-BD appears to be a very interesting approach for managing benign biliary lesions in patients with inaccessible papilla.
The technical success rate was high and the clinical success rate was 100%, so its use in the treatment of all cases of cholangitis related to biliary stenosis is suitable. Stent exchange can be performed during a 1-day hospital stay (outpatient), so the advantages for the patient are very relevant.
A key point of the study is that stenting allows selection of patients without increasing risk of mortality. Benign biliary stenosis can be managed in patients with complex stenosis not seen on imaging or stenoses considered benign that are found to be recurrences (malignant) of malignant disease previously operated on. Sixteen of 36 patients did not complete the 1-year follow-up, including four because of technical failure and none because of complications regarding endoscopic treatment. Seven patients had oncological relapse or complications due to previous oncological treatment. Two had complex stenosis that needed complex management (EUS-BD, percutaneous, and surgery). Three patients were being managed in the long term. These patients, however, were excluded from the analysis and could have benefited from drainage. These patients were included despite not being followed for at least 1 year, and thus, an overall morbidity rate for the first HGS could not be calculated. These inclusions could be debated.
Another key point of our study is the efficiency of the technique. There was no recurrence after the removal of the stent after 1 year.
A key point is the high rate of morbidity. Ogura et al. has already described the increased risk of complications due to shearing wire in cases of a thin intrahepatic bile duct (IHBD), and it is known that this is the case for benign biliary stenosis 26 . Our main complications were stent migrations and iatrogenic cholangitis. Stent migration occurred in 80% of the first 10 patients enrolled in the study. All migrations occurred before the implantation of 10- cm metal stents with an antimigration effect (Taewong Medical). The choice of the type of covered stent is probably crucial. In our study, the main complication was iatrogenic cholangitis. This cholangitis may be explained by the use of covered stents. However, many studies conducted in the east showed that the incidence of complications with covered stents was not higher than that with EUS-guided biliary stents 27 . Covered stents are commonly used for EUS-BD in Asia. However, in cases of benign biliary stenosis with altered anatomy, digestive contamination preexists because of the lack of papilla. Mukai et al. described an earlier rate of recurrent biliary obstruction in cases of preexisting cholangitis before EUS-BD, even when using plastic stents 28 .
In our study, we used covered metal stents with potential occlusion of small IHBD, explaining our rate of iatrogenic cholangitis because of preexisting digestive bacteremic contamination. The use of plastic stents is not widespread in Europe, probably because HGS/HJS is performed using a cystotome and large fistula creation, and mechanical tract dilation is performed to place plastic stents in the east. In our experience, insertion of a plastic stent after use of a cystotome has a higher incidence of bile leakage than insertion of a covered metal stent. In a recent comparison of plastic stents and metal-covered stents, metal stents have a lower rate of complications 29 . However, Matsumani et al. described the use of plastic stents to avoid experimental cholangitis 30 .
Decreasing the rate of iatrogenic cholangitis is probably a key point because, as shown in our results, the rate of complications is a risk factor for failure of stent removal. It is likely that, because of these complications, physicians and patients choose to forego stent removal to avoid the need for redo HGS/HJS to treat recurrence. Because this pathology is rare, defining the material needs for manufacturers is challenging. Perhaps covered metal stents with smaller diameters could be an option because of the smaller diameter of the IHBD in patients with benign biliary stenosis.
In our study, removal of the metal stent was sometimes performed very early because of iatrogenic cholangitis. The mean time to removal was 12.3 days. No complications occurred during metal stent removal. As a result, we suggest not scheduling changes beyond 2 weeks. The fistula was created very quickly, and no leakage was noticed during the metal/pigtail change.
Removing SEMS as soon as possible (before 2 weeks) and antibiotic therapy for several days is a valuable option.
An important point is that all complications have been described. Early change from a metal stent to a plastic stent could be debated as a complication because this change is the goal of treatment. An early change could be misclassified as a complication. The choice to include this kind of complication is based on an important message. These patients and the endoscopist must be aware that the patients may need an unscheduled and early change of metal stent to pigtail stent.
As previously mentioned, there is no risk of metal stent migration with an antimigration (flare) metal stent. Early scheduled replacement of the metal stent with a plastic stent may decrease the rate of unscheduled changes by half because half of unscheduled changes occurred before 12 days. Therefore, the morbidity rate should decrease to 22% (7/36). Furthermore, because early endoscopic stent change is not considered a supplementary endoscopic session, the rate of complications (2 bleeding, 1 cholecystis, and 1 patient needing intensive care) should be reconsidered and estimated as 11% (4/36).
Limitations of this study include the multicenter retrospective design as asserted in endoscopy and gastrointestinal endoscopy journals; however, such studies are widespread 31 . It has been emphasized that both units work very similarly, so the risk of potential bias due to the retrospective multicenter design tends to decrease. Due to the retrospective design, we do not have data about calibration by duodenoscopy in cases of altered anatomy. Indeed, in Billroth 2 or Whipple surgeries, the anastomosis site can sometimes be reached with a duodenoscope or colonoscope. Because of this lack of data, we cannot propose an algorithm for calibrating stenosis with EUS-BD in patients with altered anatomy.
Another limitation is the insufficient follow-up. To our knowledge, our follow-up is the longest described, but a longer follow-up period is needed to determine the rate of recurrence.
Conclusions
In conclusion, EUS-BD is an option for calibration of benign stenosis in cases of ERCP failure. Clinical success, no recurrence after stent removal, and the longest follow-up period described in the literature underscore that EUS-BD is a suitable option. The key point is to decrease the rate of complications and not hesitate to remove the stents, even in cases of complications during calibration and anxiety regarding stent removal.
More patients and longer follow-up are still needed to confirm the efficiency of this technique.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Dumonceau J.-M., Tringali A, Papanikolaou IS et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline – Updated October 2017. Endoscopy. 2018;50:910–930. doi: 10.1055/a-0659-9864. [DOI] [PubMed] [Google Scholar]
- 2.Giovannini M, Moutardier V, Pesenti C et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: A new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 3.Marx M, Caillol F, Autret A et al. EUS-guided hepaticogastrostomy in patients with obstructive jaundice after failed or impossible endoscopic retrograde drainage: A multicenter, randomized phase II Study. Endosc Ultrasound. 2022;11:495–502. doi: 10.4103/EUS-D-21-00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marx M, Caillol F, Sfumato P et al. EUS-guided hepaticogastrostomy in the management of malignant biliary obstruction: Experience and learning curve in a tertiary referral center. Dig Liver Dis. 2022;54:1236–1242. doi: 10.1016/j.dld.2022.05.008. [DOI] [PubMed] [Google Scholar]
- 5.Iwashita T, Uemera S, Tezuka R et al. Current status of endoscopic-guided anterograde intervention for biliary diseases in patients with surgically altered anatomy. Dig Endosc. 2023;35:264–274. doi: 10.1111/den.14393. [DOI] [PubMed] [Google Scholar]
- 6.Nakai Y, Kogure H, Isayama H et al. Endoscopic ultrasound-guided biliary drainage for benign biliary disease. Clin Endosc. 2019;52:212–219. doi: 10.5946/ce.2018.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Itoi T, Sofuni A, Tsuchiya T et al. Endoscopic ultrasonography‑guided transhepatic antegrade stone removal in patients with surgically altered anatomy: Case series and technical review (with videos) J Hepatobiliary Pancreat Sci. 2014;21:E86–E93. doi: 10.1002/jhbp.165. [DOI] [PubMed] [Google Scholar]
- 8.Hosmer A, Abdelfatah MM, Law R et al. Endoscopic ultrasound‑guided hepaticogastrostomy and antegrade clearance of biliary lithiasis in patients with surgically‑altered anatomy. Endosc Int Open. 2018;6:E127–E130. doi: 10.1055/s-0043-123188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iwashita T, Nakai Y, Hara K et al. Endoscopic ultrasound‑guided antegrade treatment of bile duct stone in patients with surgically altered anatomy: A multicenter retrospective cohort study. J Hepatobiliary Pancreat Sci. 2016;23:227–233. doi: 10.1002/jhbp.329. [DOI] [PubMed] [Google Scholar]
- 10.Iwashita T, Uemura S, Shimuzu M. Endsocpic ultrasonography-guided antegrade treatment for bile duct stone with multi-step approach in a patient with surgically altered anatomy. Dig Endosc. 2018;30:77–78. doi: 10.1111/den.13021. [DOI] [PubMed] [Google Scholar]
- 11.Ogura T, Kawai J, Nishiguchi K et al. Transluminal intrahepaticbile duct stone removal using a novel spiral basket catheter via the endoscopic ultrasound-guided hepaticogastrostomy route (with video) Dig Endosc. 2022;34:234–237. doi: 10.1111/den.14121. [DOI] [PubMed] [Google Scholar]
- 12.Mukai S, Itoi T, Sofuni A et al. EUS‑guided antegrade intervention for benign biliary diseases in patients with surgically altered anatomy (with videos) Gastrointest Endosc. 2019;89:399–407. doi: 10.1016/j.gie.2018.07.030. [DOI] [PubMed] [Google Scholar]
- 13.Weilert F, Binmoeller KF, Marson F et al. Endoscopic ultrasound-guided anterograde treatment of biliary stones following gastric bypass. Endoscopy. 2011;43:1105–1108. doi: 10.1055/s-0030-1256961. [DOI] [PubMed] [Google Scholar]
- 14.Nakai Y, Isayama H, Koike K. Two-step endoscopic ultrasonography-guided antegrade treatment of a difficult bile duct stone in a surgically altered anatomy patient. Dig Endosc. 2018;30:125–127. doi: 10.1111/den.12965. [DOI] [PubMed] [Google Scholar]
- 15.Pizzicanella M, Caillol F, Pesenti C et al. EUS‑guided biliary drainage for the management of benign biliary strictures in patients with altered anatomy: A single‑center experience. Endosc Ultrasound. 2020;9:45–52. doi: 10.4103/eus.eus_55_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miranda-García P, Gonzalez JM, Tellechea JI et al. EUS hepaticogastrostomy for bilioenteric anastomotic strictures: A permanent access for repeated ambulatory dilations? Results from a pilot study. Endosc Int Open. 2016;4:E461–E465. doi: 10.1055/s-0042-103241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogura T, Takenaka M, Shiomi H et al. Long‑term outcomes of EUS‑guided transluminal stent deployment for benign biliary disease: Multicenter clinical experience (with videos) Endosc Ultrasound. 2019;8:398–403. doi: 10.4103/eus.eus_45_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park DH, Jang JW, Lee SS et al. EUS‑guided transhepatic antegrade balloon dilation for benign bilioenteric anastomotic strictures in a patient with hepaticojejunostomy. Gastrointest Endosc. 2012;75:692–693. doi: 10.1016/j.gie.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 19.Dindo D, Demartines N, Clavien P-A. Classification of Surgical Complications: A New Proposal With Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kühn JP, Busemann A, Lerch MM et al. Percutaneous biliary drainage in patients with non dilated intrahepatic bile ducts compared with patients with dilated Intrahepatic bile ducts. Am. J. Roentgenol. 2010;195:851–857. doi: 10.2214/AJR.09.3461. [DOI] [PubMed] [Google Scholar]
- 21.Kucukay F, Okten RS, Yurdakul M et al. long-term results of percutaneous biliary balloon dilation treatment for benign hepaticojejunostomy strictures: Are repeated balloon dilations necessary? J Vasc Interv Radiol. 2012;23:1347–1355. doi: 10.1016/j.jvir.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Luu C, Lee B, Stabile BE. Choledochoduodenostomy as the biliary–enteric bypass of choice for benign and malignant distal common bile duct strictures. Am Surg. 2013;79:1054–1057. [PubMed] [Google Scholar]
- 23.Khajanchee YS, Cassera MA, Hammill CW et al. Outcomes following laparoscopic choledochoduodenostomy in the management of benign biliary obstruction. J.Gastrointest. Surg. 2012;16:801–805. doi: 10.1007/s11605-011-1768-3. [DOI] [PubMed] [Google Scholar]
- 24.Monkemüllern K, Fry LC, Bellutti M et al. ERCP with the double-balloon enteroscope in patients with Roux-en-Y anastomosis. Surg Endosc. 2009;23:1961–1967. doi: 10.1007/s00464-008-0239-8. [DOI] [PubMed] [Google Scholar]
- 25.ItokawaFItoi T, Ishii K et al. Single- and double-balloon enteroscopyassisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y plus hepaticojejunostomy anastomosis and Whipple resection: Enteroscopy in hepaticojejunostomy. Dig. Endosc. 2014;26:136–143. doi: 10.1111/den.12254. [DOI] [PubMed] [Google Scholar]
- 26.Ogura T, Masuda D, Takeuchi T et al. Liver impaction technique to prevent shearing of the guidewire during endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2015;47:E583–E584. doi: 10.1055/s-0034-1393381. [DOI] [PubMed] [Google Scholar]
- 27.Ogura T, Higuchi K. Technical tips for endoscopic ultrasound-guided hepaticogastrostomy. World J Gastroenterol. 2016;22:3945–395. doi: 10.5009/gnl20096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mukai S, Itoi T, Sofuni A et al. Urgent and early EUS-guided biliary drainage in patients with acute cholangitis. Endosc Ultrasound. 2021;10:191–199. doi: 10.4103/eus.eus_70_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kawakubo K, Isayama H, Kato H et al. Multicenter retrospective study of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction in Japan. J Hepatobiliary Pancreat Sci. 2014;21:328–334. doi: 10.1002/jhbp.27. [DOI] [PubMed] [Google Scholar]
- 30.Matsunami Y, Itoi T, Soufi A et al. EUS-guided hepaticoenterostomy with using a dedicated plastic stent for the benign pancreatobiliary disease: A single-center study of a large case series. Endosc Ultrasound. 2021;10:294–304. doi: 10.4103/EUS-D-20-00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wallace MB, Bowman D, Hamilton-Gibbs H et al. Ethics in publication, part 2: duplicate publishing, salami slicing, and large retrospective multi center case series. Gastrointest Endosc. 2018;87:1335–1337. doi: 10.1016/j.gie.2018.01.002. [DOI] [PubMed] [Google Scholar]