Summary
Countries and areas in the Western Pacific region (WPR) experienced the COVID-19 pandemic and took various preventive measures, which affected non-communicable diseases (NCDs) risks and mortality. Due to differences in COVID-19 prevention measures and other characteristics such as culture, religions, political systems, socioeconomic development, lifestyles, and health care systems, the effects of COVID-19 on NCDs varied greatly among WPR countries. Most countries had an increased all-cause and NCDs mortality during the pandemic, but some developed countries, including New Zealand, Singapore and Australia reported decreased mortality. The pandemic and the preventive measures increased NCD risk factors including unhealthy diet, lack of physical activity and sleep disorders. The effects varied by socioeconomic status and health conditions. COVID-19 related stress, food shortages, and confined lifestyle had immediate detrimental effects on NCDs, and also affected pregnancy outcomes with long-term effects on NCDs risks in coming years.
Keywords: COVID-19, NCDs, Mortality, Western Pacific region
Introduction
The COVID-19 pandemic was announced following the discovery of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) at end of 2019 in Wuhan, China.1 As of 31 December 2022, more than 639 million confirmed cases and 6.6 million deaths have been reported worldwide, with more than 98 million confirmed cases and 283,164 deaths in the WHO Western Pacific region (WPR).2
In the WPR, Non-Communicable Diseases (NCDs) account for 80% of all deaths, with 50% of premature deaths occurring in low-and-middle-income countries.3,4 The urgent need to reduce the burden of NCDs has been recognised by the United Nations, with Sustainable Development Goal 3.4 focused on reducing premature mortality from NCDs through effective prevention and treatment by a third by 2030. However, many countries are unlikely to achieve this goal, in particular, with the interruption of NCD services by the COVID-19 pandemic.5,6
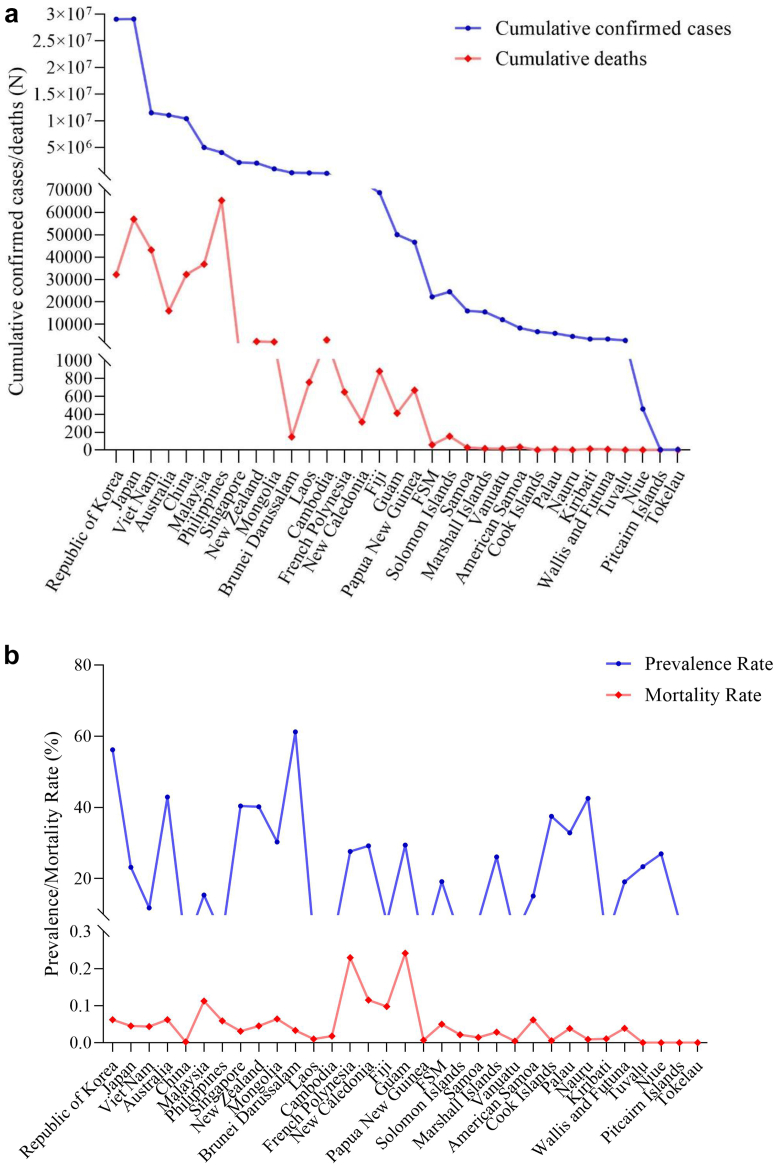
The total confirmed cases, deaths, prevalence of COVID-19 and related mortality across WPR countries were shown in Fig. 1. Overall, the COVID-19 pandemic varies dramatically across WPR countries. By 31 December in 2022, the Republic of Korea had the highest cumulative confirmed cases (29,059,273), followed by Japan (29,105,070), Viet Nam (11,524,647), Australia (11,047,174) and China (10,388,942). Niue (458), Tokelau (5), and Pitcairn Islands (4) had relatively lower cases.
Fig. 1.
Total confirmed cases, deaths, the prevalence and mortality of COVID-19 across counties in the WesternPacific region. a. Cumulative confirmed cases and deaths; b. prevalence and mortality rate of COVID-19.
Data source: World Health Organization—COVID-19 data dashboard in the Western Pacific Region (https://covid19.who.int/table) (data on 31 December 2022).
Aligned with cumulative cases, Brunei Darussalam had the highest prevalence of COVID-19 (61.2%), followed by the Republic of Korea (56.2%). Except Tokelau had no COVID-19 cases, Cambodia, China, Papua New Guinea, and Tokelau were countries had lower prevalence, which were 0.8%, 0.7% and 0.5%, respectively (Fig. 1).
Deaths due to COVID-19 were proportionately associated with confirmed cases of infection. Philippines had the highest prevalence of cumulative deaths (65,309), followed by Japan (56,974) and Viet Nam (43,184). No COVID-19 related death has been reported for Tuvalu, Niue, Pitcairn Islands, and Tokelau countries. Guam had the highest COVID-19 mortality (0.24%), followed by French Polynesia (0.23%). Nauru (0.009%), Papua New Guinea (0.007%), Cook Islands (0.006%), Vanuatu (0.005%) and China (0.002%) had relatively lower mortality across countries in the WPR (Fig. 1).
As COVID-19 affects individuals and populations differently depending on factors such as health conditions, lifestyle, and prevention measures, its effects on NCDs as well as mortality varied greatly by countries. WPR countries have a diverse population structure with substantial differences in socioeconomic status, burdens of NCDs, health services as well as COVID-19 prevention measures. To the best of our knowledge, no study has comprehensively examined the influence of COVID-19 on NCDs in WPR countries.
This study aimed to fill in this knowledge gap and aimed to comprehensively examine the impact of the COVID-19 pandemic on NCDs risks and deaths, and compare the differences across studies among WPR countries. It comprehensively assessed the existing literature to understand the impact of the COVID-19 pandemic on NCDs in hospital and population mortality, and on NCDs risk factors.
Impact of COVID-19 on NCDs and excess mortality of all causes in the WPR
COVID-19 has both direct and indirect impact on NCDs. In terms of direct effects, COVID-19 has a high susceptibility among people with NCDs, and vice versa. That is, pre-existing NCDs as a risk factor for becoming infected by a severe form of COVID-19, leading to death in most causes; whereas COVID-19 effects on NCD outcomes and complications. In China, a meta-analysis suggested that comorbid diabetes increased the severity or mortality of COVID-19 with a pooled relative risk of 2.96 (95% CI 2.31–3.79).7 The interaction between COVID-19 and NCDs may further increase the global burden of disease.8
Indirect effects of COVID-19 on NCDs are varying, with one of the important aspects is that COVID-19 has substantially disrupted the provision of essential health services for NCD.9 According to WHO PULSE survey, 77% of all countries have experienced partially or completely health service disruptions during the COVID-19 pandemic: 49% of diabetes treatment, 43% of cancer treatment, and 31% of cardiovascular emergency responses were disrupted.10 No doubt that these health service disruptions may lead to delayed NCDs diagnosis, faster disease progression, and ultimately, higher rates of mortality.
Excess mortality, defined as the increase of the all-cause mortality above the expected mortality based on historical trends, has been widely used to estimate the death toll of COVID-19 pandemic. A total of 18.2 million people died because of the COVID-19 pandemic during the period of January 2020–December 2021, with excess mortality rate exceeded 300 deaths per 100,000 of population in 21 countries worldwide.6 In Singapore for instance, based on the data from the Ministry of Health, a higher than usual number of deaths during COVID-19 pandemic was reported with the excess mortality linked to COVID-19 infection between January 2020 and January 202211 In other words, COVID-19 aggravated existing illnesses, resulting in further mortalities.
COVID-19 Excess Mortality Collaborators6 evaluated the excess mortality during COVID-19 pandemic worldwide. In WPR, of a total of 18 countries’ data were available, 15 countries had excess mortality due to COVID-19 pandemic, with Guam had the highest excess mortality (107 per 100,000), while China has the lowest excess mortality (1 per 100,000). Interestingly, three countries in the WPR: New Zealand, Singapore, and Australia reported decreased mortality during COVID-19 pandemic (between January 1, 2020 and December 31, 2021), which were 9.3, 15.8 and 37.6 per 100,000, respectively.6 However, it is worth noting that excess mortality often represented all-cause mortality during the COVID-19 pandemic.6 That is, excess mortality may be resulted from either COVID-19 infection or NCD, or a combination of the two.
COVID-19 effects on NCDs mortality
COVID-19 affected NCDs mortality differently by countries and regions. All-cause excess mortality during COVID-19 pandemic has been reported around the world, with NCDs being listed as the major underlying cause of death.1 Data on the effect of COVID-19 on NCD mortality are limited in the WPR, thus we performed a narrative review to assess associations across WPR countries. Details of key words (Panel 1) and searching strategies in Web of Science (Supplementary Table S1) and PubMed (Supplementary Table S2) were presented in Supplementary files.
Panel 1. Search strategies and analyses of the association between COVID-19 excess mortality and NCDs.
The Web of Science and PubMed database was searched for studies published between 1 January 2019 and 25 Oct 2022. The searching strategies included in the search are shown in Supplementary Table S1–S5. The following search terms and their combinations were used: “coronavirus”, “COVID-19”, “NCD”, “non-communicable diseases”, “CVD”, “cardiovascular diseases”, “diabetes”, “respiratory diseases”, “COPD”, “chronic obstructive pulmonary disease”, “cancer”, “neoplasms”, “mental health”, “psychiatry”, “prevalence”, “incidence”, “death”, “mortality”, “morbidity”, “detection”, “health service”, “dietary pattern”, “dietary behaviour change”, “Western Pacific region”, and names of all 37 countries and areas in the WPR.
Regarding the impact of the COVID-19 pandemic on NCDs in-hospital mortality and NCDs mortality at the population level, there were 2007 studies from Web of Science and 2058 studies from PubMed that resulted initially, of which 46 were identified, 13 studies were included as relevant based on a review of the title and abstract and then a full-text review. Studies that reported mortality before and during COVID-19 pandemic period in WPR countries were included. A total of 10 studies on NCDs in-hospital or after-hospital mortality and 3 studies on NCDs mortality at the population level were extracted for details.
Studies reported in-hospital mortality were found across four countries in the WPR, including China, Philippines, Japan and Singapore (Table 1). Of a total of 10 included studies, eight studies reported on cardiovascular mortality,12, 13, 14, 15, 16, 17, 18, 19, 20, 21 one on cancer mortality20 and one on mental health mortality.21 Six studies reported increased mortality,12,13,16,19, 20, 21 whereas four studies reported decreased in-hospital or after-hospital mortality.14,15,17,18
Table 1.
Summary of studies on the impact of the COVID-19 pandemic on NCDs in-hospital mortality in the Western Pacific region.
| Study settings | Comparisons | Outcome measures | Effects |
|---|---|---|---|
| 1.CVD | |||
| China12 | Pre-COVID (2019) vs post-COVID (2020) period | In-hospital mortality | Increased by 18.0% in patients with cerebrovascular disease |
| Philippines13 | Pre-COVID (Feb 2019–Jan 2020) vs COVID period (Feb 2020–Jan 2021) | Proportion of death | Increased from 7% pre-pandemic to 13% during the pandemic in stroke patients |
| Singapore14 | Pre-COVID (Dec 2019–Feb 2020) vs COVID period (Feb–Mar 2020) | In-hospital mortality | Decreased by 1.6% but no significant difference in cardiac-related mortality |
| Japan15 | Pre-COVID (before Apr 2020) vs COVID period (after Apr 2020) | In-hospital mortality | 7% lower risk but no significant difference in patients with acute coronary syndrome |
| China16 | Pre-COVID (2019) vs COVID period (2020) | In-hospital mortality | Increased by 6.6% in patients with stroke |
| China17 | Pre-COVID (Jan–Apr 2019) vs COVID period (Jan–Apr 2020) | In-hospital mortality | Decreased by 11.9% in cardiac intensive care units |
| China18 | Pre-COVID (2010–2019) vs COVID period (2020) | In-hospital mortality | Mortality from first-ever stroke in 2020 was not significantly different from that in 2019, but it was noticeably lower than that for the previous 5 and 10 years |
| China19 | Pre-COVID (2019) vs COVID period (2020) | In-hospital mortality | Increased from 1.1 pre-COVID to 4.2% during the pandemic |
| Cancer | |||
| Japan20 | Pre-COVID (Apr 2019–Mar 2020) vs COVID period (Apr 2020–Mar 2021) | In-hospital mortality | Increased from 9.0% pre-COVID period to 32.0% during COVID period |
| 2.Mental health | |||
| Hong Kong, China21 | Pre-COVID (Jan–Nov 2019) vs during COVID (Jan–Nov 2020) | In-hospital mortality | Increased by 26.0% in patients with mental disorders |
Among six studies that reported increased NCDs mortality, four were conducted in China, with the range of increase between 6.6 and 26% 12,16,19,21; one study reported in Philippines that increased by 6% compared to pre-COVID period13; one study reported in Japan that increased by 27% compared to pre-COVID period.20 Among four studies that reported decreased mortality, with the range of decrease between 1.6% and 11.9%14,15,17,18; two studies reported in China,17,18 one study reported in Japan15 and one was in Singapore.14
Five population-mortality studies compared the mortality during the pandemic to either pre-COVID period or predicted post-COVID period (Table 2). Among these studies,22, 23, 24 two reported cardiovascular mortality,22,23 two reported cancer mortality23,24 and one reported respiratory disease mortality.23 Of these studies, four were conducted in Japan22,23 and one in Australia.24 Four of five studies reported increased mortality,22,23 and one predicted the increased mortality by gender with 36.4% (95% Uncertainty Interval [UI] 15.3–63.9) increase for males, 36.6% (95% UI 15.8–64.1) increase for females between 2020 and 2044.24
Table 2.
Summary of studies on the impact of the COVID-19 pandemic on NCDs mortality at population level in the Western Pacific region.
| Study settings | Comparisons | Outcome measures | Effects |
|---|---|---|---|
| 1.CVD | |||
| Japan22 | Pre-pandemic (2010–19) vs pandemic period (Mar–Dec 2020) | Death on temperature-sensitive disease (including cardiovascular disease and respiratory diseases) | Decreased by 8%–56% |
| Japan23 | Pre-pandemic (2012–2019) vs pandemic period (Jan 2020–May 2021) | Largest excess death percentage | Increased by 5.0–14.4% |
| 2.Cancer | |||
| Japan23 | Pre-pandemic (2012–2019) vs pandemic period (Jan 2020–May 2021) | Largest excess death percentage | Increased by 3.7–6.5% |
| Australia24 | 2017–2019 vs predicted (2020–2044) | Cancer death | Increased by 36.4% (95% uncertainty interval [UI] 15.3–63.9) for males, 36.6% (95% UI 15.8–64.1) for females |
| 3.Respiratory disease | |||
| Japan23 | Pre-pandemic (2012–2019) vs pandemic period (Jan 2020–May 2021) | Largest excess death percentage | Increased by 6.2–19.4% |
Four studies conducted in Japan reported increases in all-cause mortality between 3.7 and 19.4%.23,24 Interestingly, one study in Japan reported decreased mortality on temperature-sensitive disease, which mainly included cardiovascular disease and respiratory diseases.22
In summary, regarding in-hospital mortality, six of ten studies reported an increase, while four studies reported a decrease in mortality in WPR countries. In terms of mortality at population level, four of five studies reported increased all-cause mortality and cancer mortality, whereas one study reported decreased mortality in cardiovascular and respiratory diseases. Although the effects of COVID-19 pandemic on NCD mortality across WPR countries were different, the majority of studies found an increased NCD mortality in-hospital and at population level.
It is noteworthy that from the existing studies, the actual cause of death seems unclear. It is hard to distinguish if NCDs increased susceptibility to contracting COVID-19, or worsened its course, versus if COVID-19 precipitated a NCD event that was part of the pre-existing NCD (e.g., diabetes).
COVID-19 effects on risk for NCDs and risk factors
Some studies have assessed the effects of COVID-19 on the burden of NCDs. Evidence from 11 cohort studies (mainly in the USA and Europe) suggests that COVID-19 infection increases the risk of incident diabetes by 64% (type 2 diabetes increased by 78%, and type 1 diabetes increased by 42%).25
Most types of NCDs often share common modifiable risk factors, with main focus on unhealthy lifestyles, such as unhealthy diets and lack of physical activity.26 COVID-19 mitigation strategies in many countries, such as lockdown, physical distancing and self-isolation, further increase the behavioural risk of NCDs.
To further understand the impact of the COVID-19 pandemic on NCDs burden (e.g., increased or decreased prevalence of NCDs) and its risk factors (e.g., poor diet and low physical activity) in WPR, we performed a review of all systematic reviews conducted in the region. The searching terms included in this search are shown in Panel 1 and Supplementary Table S3. There were 2853 studies that resulted initially, of which 27 were identified, 10 studies were further included based on a review of the title and abstract and then a full-text review (Table 3).
Table 3.
Summary of systematic reviews on how COVID-19 pandemic affected the risk for NCDs and NCDs risk factors in the Western Pacific region.
| Study settings | Comparisons or summary | Outcomes | Effects |
|---|---|---|---|
| 1. COVID-19 affects the risk for NCDs | |||
| Cancer | |||
| China (10 out of a total of 31 included studies)27 | Cancer patients vs non-cancer patients during COVID-19 pandemic | Cancer mortality | Pooled Odds Ratio (OR) = 6.62, 95% CI 2.68–16.34 |
| China (82 out of a total of 110 included studies)28 | Reported on cancer prevalence during COVID-19 pandemic | Cancer prevalence in hospitalised patients with COVID-19 | Pooled prevalence = 1.7%, 95% CI 1.3%–2.3% |
| China (8 out of a total of 15 included studies)29 | Reported on cancer prevalence during COVID-19 pandemic | Cancer prevalence in hospitalised patients with COVID-19 | Pooled prevalence = 20.0%, 95% CI 14.5%–26.2% |
| Mental disorders | |||
| China (a total of 66 included studies)30 | Reported prevalence of psychological status during COVID-19 pandemic | Prevalence of different psychological symptoms | Anxiety: 28.6%, depression: 30.6%, sleep disorder: 26.3%, acute stress: 36.5%, somatic symptoms: 17.0%, fear: 36.8%, obsessive-compulsive symptoms: 37.1%, comprehensive psychological symptoms 26.7% |
| China (8 out of a total of 15 included studies)31 | Reported on anxiety prevalence of in pregnant women during COVID-19 pandemic | Anxiety prevalence in hospitalised patients with COVID-19 | Pooled prevalence = 34%, 95% CI 26%–43% |
| China (11 out of a total of 15 included studies)31 | Reported on depression prevalence of in pregnant women during COVID-19 pandemic | Depression prevalence in hospitalised patients with COVID-19 | Pooled prevalence = 30%, 95% CI 23%–37% |
| Vietnam (a total of 13 included studies)32 | Reported on depression prevalence of during COVID-19 pandemic | Depression prevalence in hospitalised patients with COVID-19 | Pooled prevalence = 14.6%, 95% CI 11.5%–18.1% |
| 2. COVID-19 affects NCD risk factors | |||
| Sleep | |||
| China (a total of 98 included studies)33 | Reported insomnia symptom during the early and late stages of COVID-19 in China | Prevalence of insomnia | The range of the pooled prevalence of insomnia symptoms were 37.0% (95% CI 34.1–39.9%) and 41.8% (95% CI 33.6–50.0%) |
| China (a total of 17 included studies)34 | Reported sleep disturbances and sleep quality during COVID-19 pandemic | Prevalence of sleep disturbances | Pooled prevalence = 45.1%, 95% CI 37.2%–53.1% |
| Environment | |||
| Republic of Korea35 | PM2.5 levelsa during the period of COVID-19-induced lockdown compared to 2019 | Reduction percentage of PM2.5 levels | Decreased by 54% |
| China35 | PM2.5 levelsa during the period of COVID-19-induced lockdown compared to 2019 | Reduction percentage of PM2.5 levels | Decreased by 44% |
PM2.5 levels means particulate matter less than 2.5 μm in diameter.
Of 10 studies, seven reviews reported NCDs prevalence during the COVID-19 pandemic, three reported on cancer prevalence27, 28, 29 and four reported on mental disorders.30, 31, 32 Within countries in WPR, China was included in six of seven reviews, with the range of pooled prevalence for cancer being between 1.7 and 20.0%, for mental disorders being between 26.3 and 37.1%. One study highlighted significant high mortality among cancer patients during the COVID-19 pandemic.27 Apart from China, Vietnam is the only county in the WPR included in one review that reported the prevalence of depression (14.6%) during the COVID-19 pandemic.32
In terms of NCD risk factors, sleep and environment were discussed in the three reviews.33, 34, 35 China33, 34, 35 and South Korea35 were countries in WPR that were included in the reviews. The range of sleep disorder prevalence during the COVID-19 pandemic was between 37 and 45.1%. The COVID-19 pandemic affects the environment factor is interesting that PM2.5 (i.e., particulate matter less than 2.5 μm in diameter) during the period of COVID-19-induced lockdown decreased by 44% in China35 and 54% in Republic of Korea.35
COVID-19 effects on the changes of dietary behaviour
Although sleep and environment are the only factors included in the systemic reviews in the WPR, diet is one of the most important risk factors for NCDs, with dietary changes during the COVID-19 pandemic have been widely discussed in the literature.36 Therefore, we further performed a review to understand dietary behaviour changes in the WPR during the COVID-19 pandemic. The searching strategies are shown in Panel 1, Supplementary Tables S4 and S5.
Of a total of 258 studies that resulted initially, 148 studies were included as relevant based on a review of the title and abstract and then a full-text review. A total of 13 studies that included national data were extracted for details (Table 4). Of a total of 13 studies, 6 studies were performed in China,37, 38, 39, 40, 41, 42 2 in Vietnam,43,44 2 in Japan,45,46 1 in South Korea,47 1 in Malaysia48 and 1 in New Zealand.49
Table 4.
Summary of studies on dietary behaviour change pre-post the COVID-19 pandemic in the Western Pacific region.
| Study settings | Region | Sample size | Tools of dietary assessment | Survey method | Comparisons | Effects |
|---|---|---|---|---|---|---|
| China37 | Nationwide | NA | Summary data from China Statistical Yearbook | Aggregated data on dietary consumption | Pre-COVID (2015–2019) vs post-COVID (2020) | Increased consumption of grain, poultry, eggs, and dairy. Decreased red meat consumption. Changes varied by region, age and illiteracy rate. |
| China38 | Nationwide (67.9% in Guangdong province) | 2723 | FFQa | Online survey | During the lockdown (after Jan 2020) vs pre-COVID-19 period (Oct 2019) | Prevalence of increased or decreased intake: Fruit: 23.3%, 17.9%. Vegetable: 25.3%, 11.7%. Snacks: 38.2%, 13.6% |
| China39 | Nationwide | 2289 | FFQ | Online survey | Under vs before home isolation (Survey period: 23 Mar to 26 Apr 2020) | 23% of adults reported changed their diets to be healthier and 30% reported consuming more vegetables, fruits, and milk products under home isolation |
| China40 | Nationwide | 10,082 | FFQ | Online questionnaire | Pre-COVID vs COVID period (May 2020) | Decreases in the frequency of intake of rice, meat, poultry, fresh vegetables, fresh fruit, soybean products, and dairy products; increase in the consumption of wheat products, other staple foods, and preserved vegetables |
| China41 | Nationwide | 441 | The Corona Cooking Survey (CCS) questionnaire | Online questionnaire | Pre-COVID vs during COVID period (April–June 2020) | No changes in healthy food consumption. Salty snack decreased 3.3%. Alcohol decreased 2.8% |
| China42 | Nationwide | 652 | The Corona Cooking Survey (CCS) questionnaire | Online questionnaire | Pre-COVID vs during COVID period (April–June 2020) | Decreased intake of salty snacks and alcoholic beverages during the lockdown; increase in the frequency of family members recommending diets. |
| Vietnam43 | Nationwide (eleven hospitals across Vietnam) | 4348 | One question on perceived dietary change | The online and printed versions of the questionnaire assisted by researchers | During lockdown (Apr 2022) vs after lockdown (Apr–May 2020) | Patients under lockdown were less likely to have “unchanged or healthier” eating behaviour (OR 0.38, 0.29–0.51) |
| Vietnam44 | Nationwide (10 universities) | 7616 nursing and medical students | One question on perceived dietary change | Online survey | Pre-COVID vs during COVID period (April–May 2020) | Towards to a healthier eating behaviour: 42.8%. Unchanged or less healthy: 57.2% |
| Japan45 | Nationwide (users of the CALO mama health app) | 5929 | Users record items of every meal in the app | Online survey | Pre-COVID (Jan–May 2020) and during COVID period (Apr–May 2020) | Increase in the frequency of intake of vegetables, beans, seaweeds, fish, meats, dairy products, and snacks; decrease in alcohol intake during COVID. |
| Japan46 | Nationwide (registered in a research company, MyVoice) | 6000 | One question on perceived dietary change | Online survey | Pre-COVID (Nov 2019) vs during COVID (Nov 2020) | Towards to a healthier (20.3%), unhealthier (8.2%) and unchanged (71.6%) diet during COVID. |
| South Korea47 | Nationwide | 229,269 | Question on changes in diet behaviours | Computer-assisted personal interviews | Pre-COVID vs during COVID | 17% increased unhealthy diet. 8.4% decreased unhealthy diet. Having NCDs were more likely to decrease unhealthy diet. |
| Malaysia48 | Nationwide | 1045 young adults (≤30 years) | Dietary diversity questionnaire | Online survey | During COVID (June 2021) vs pre-pandemic | 45.3% consumed more fruits and 60.2% had higher plain water intake during the pandemic. 41.0%–66.8% of the young adults changed their dietary intake patterns during the pandemic. |
| New Zealand49 | Nationwide | 3028 | 7-point frequency response scale | Online questionnaire | Pre-COVID vs during COVID lockdown (April–May 2020) | Towards unhealthy dietary pattern: an increased consumption of sweet snacks (41%), salty snacks (33%), alcohol (33%), and sugary drinks (20%). |
FFQ: Food frequency questionnaire.
All studies reported changes in dietary behaviours due to the COVID-19 pandemic. Either positive or negative changes in dietary behaviour during the COVID-19 pandemic were reported across studies. Although it is hard to observe the consistent changes in healthy or unhealthy food items during or after COVID-19 across studies in the WPR, five studies in the WPR clearly indicated an overall change towards a healthy diet (healthier change > unhealthier change based on fruit and vegetable consumption or perceived change) during or after COVID-19. Specifically, a national study conducted in China (N = 2289) reported that 23% of adults reported changing their diets to be healthier.39 In a study in Vietnam that included 7616 nursing and medical students, 42.8% reported a change towards a healthier eating behaviour during the COVID-19 pandemic.44 Two national studies in Japan found healthier dietary behaviour, with increased consumption of vegetables, beans, meats and dairy products during the COVID-19 pandemic.45,46 A national study in Malaysia found 45.3% of 1045 young adults (aged ≤30 years) consumed more fruits and 60.2% had higher plain water intake during the COVID-19 pandemic.48 Interestingly, some positive effect of dietary consumption, such as alcohol and unhealthy snacks, due to COVID-19 has also been observed. Results from two national studies in China indicated a decrease in salty snacks and alcoholic beverages during the COVID-19 lockdown.41,42 A national study in Japan including 5929 participants found a decrease in alcohol consumption during the COVID-19 pandemic.45
Four studies indicated the changes in dietary behaviour towards being ‘unhealthy’. Results from a national study in China that include 10,082 participants who completed Food Frequency Questionnaire found that COVID-19 led to decreases in healthy food consumption (e.g., fresh fruit, vegetable, soybean and dairy products).50 A national study in South Korea that include 229,269 participants found more individuals reported an increase in the unhealthy diet than a decrease in unhealthy diet (17% vs 8.4%) during the pandemic.47 A national study in New Zealand including 3028 participants conclude dietary behaviour towards an unhealthy dietary pattern, with increased consumption of sweet and salty snacks, alcohol and sugary drinks.49 In a study of 4348 patients in Vietnam, participants under lockdown were found to be less likely to have “unchanged or healthier” eating behaviour (OR 0.38 95% CI 0.29–0.51).43
The changes in dietary behaviour were affected by various factors such as age, region and socioeconomic status. In China, Zheng X et al. analysed provincial level food consumption data between 2015 and 2020 and found that rural residents and those living in the eastern region were more likely to adopt a healthier diet due to the COVID-19 pandemic.37 In Japan, perceived threat of COVID-19 has been found to be positively associated with both healthier and unhealthier dietary changes with odds ratios (OR) of 1.06 (95% CI 1.04–1.07) and 1.02 (1.00–1.04), respectively.46 Surprisingly, decrease in household income also affected dietary change in both directions with ORs of 1.42 (1.18–1.70) and 1.53 (1.20–1.95) for healthier change and unhealthy change.
There are some limitations in the studies described above. Firstly, almost all the studies were conducted via online survey due to various reasons including lockdown. Secondly, the participants were generally young adults or with high socioeconomic status. It is unlikely that they are representative of the general population. It is unknown whether individuals with NCDs experienced a different dietary change during the pandemic. Only one study in Korea reported that individuals with NCDs were more likely to decrease the consumption of unhealthy diets during the pandemic with an OR of 1.15 (1.04–1.27) for those with diabetes.47 Thirdly, food consumption data are often self-reported which may have measurement bias. Lastly, as different definitions were used to describe dietary pattern across WPR regions, we were not able to reliably synthesize the evidence of changes on dietary pattern in the included studies.
In summary, the changes in dietary behaviour during the COVID-19 pandemic across WPR countries are inconsistent. The bidirectional influence of the COVID-19 pandemic on dietary behaviour is observed in the WPR, with studies indicating either positive or negative changes in dietary behaviour that may have a significant impact on future NCD burden in the WPR.
Lessons learned from the COVID-19 pandemic and future policy direction
Countries with low mortality during COVID-19 pandemic: stringent prevention measures work
Some countries, such as China, had relatively higher total number of COVID-19 cases, while had a lower number of deaths or mortality rate. This may be due to its strict COVID control policies over an extended period, relative to other countries, during the pandemic. China maintained its “Dynamic zero-COVID” strategy since pandemic began till December 7, 2022, which means to reduce virus transmission and implement effective control strategies. China has done this by stamping out outbreaks with mass testing and issuing lockdowns to achieve zero cases since the COVID-19 pandemic begins at late 2019.51 However, with the relaxing of its “dynamic zero-COVID” strategy, China saw another surge of the cases since early December 2022. By early February 2023, the surge of COVID-19 cases was under control. Its consequences are yet to be studied in-depth.
Countries with decreased mortality during the COVID-19 pandemic: telemedicine saves life
In WPR, most countries had increased excess mortality, while three countries including New Zealand, Singapore, and Australia had decreased mortality during the COVID-19 pandemic. The main reason may be due to the high-level of health service in these high-income countries. In Australia for instance, the overall health system ranks among the best in the world, with one of the highest life expectancies (82.5 years) globally.52 The COVID-19 pandemic brings extreme challenge to healthcare service, from prevention to rehabilitation. In addition, the COVID-19 pandemic also has significant impact on special health service such as pre-hospital emergency care. Pre-hospital emergency care is the community-oriented system that responds to the medical needs of patents with emergency illness outside of health care facilities until they are transferred to a medical facility,53 thereby plays a vital role in sustaining people's life during COVID-19 pandemic.
To ensure the continuity care for patients during the COVID-19 pandemic, telemedicine has been proposed and implemented across the globe, in particular in high-income countries, including New Zealand, Singapore, and Australia. The importance of implementing telemedicine for health care delivery in developing counties may have more profound impact than developed countries. However, some challenges remain in applying this technology in developing countries, mainly including affordability, accessibility and availability.54 This digital technology has also been recognised in playing a critical role across all aspects of health within the WPR that including both developing and developed countries, which has the potential to promote health and well-being in achieving sustainable development goals.55 Continuous efforts are needed by working together with policy makers, administrators, and researcher to best place telemedicine in achieving high quality of care globally.
COVID-19 pandemic on NCDs mortality: health care system makes difference beyond the economic development level
The impact of the COVID-19 pandemic on NCDs mortality is substantial, with increased NCD mortality during the COVID-19 pandemic being common worldwide. An excess acute cardiovascular mortality of 8% was observed in England and Wales,56 17%–164% of cardiovascular events and deaths were markable increased in the United States during the COVID-19 pandemic.57 The main reason may be due to healthcare system factors given the resources have been pushed to be adapted and reallocated in coping with the burden of COVID-19. Patients with NCDs are often delayed in accessing medications prescriptions or semi-elective procedures (e.g., transcatheter aortic valve replacement for cardiovascular procedure) that lead to a higher risk of deaths. In China, a population-based survey found that 30.1% of the participants reported drug shortage during the COVID-19 pandemic.58 In the WPR, most studies have also reported increased NCDs mortality, whereas a study conducted in Japan estimated substantial decreases in the burden of cardiovascular and respiratory disease.22 This is explained by the behavioural modifications during COVID-19, that is, COVID-19 related policies inhibit people's behaviour and outdoor mobility causing decreased mortality. An efficient surveillance and health care service in Japan is likely to be an important contributor to the prevention of excess mortality during the COVID-19 pandemic.59
Long-term effects of COVID-19 related psychological and behaviour changes deserve attention
Individual risk factor of NCDs, such as dietary risk and physical inactivity, that impacted by COVID-19 in the WPR are often studied.60 Due to grocery shopping restriction, stockpiling food are common during COVID-19 pandemic. This resulted in reduced fresh food (e.g., fruits and vegetables) and increased highly processed or unhealthy food consumption (e.g., snacks and junk foods). Food shortage is a great concern during COVID-19 pandemic, especially among people with NCDs. An online survey conducted in China found that 26.9% reported food shortage during the COVID-19 pandemic, with a substantial difference was highlighted among people with or without diabetes (59.5% vs 25.0%).58 The issue of food insecurity and insufficient accessibility due to disruptions on market supply chain has also been proposed,61 which brings new challenge in food inequality across the world. As a result of the COVID-19 pandemic, early healthy food intervention for NCDs prevention may become difficult. Based on Barker's foetal origin hypothesis, nutrition in early stage of life can affect the risk of NCDs in adulthood.62 Lessons learned from natural disasters including famine tell us that early life development issues have an important role in the contemporary high burden of NCDs. In addition, dietary behaviour changes may be related to prevention policies during different time period of the epidemic across WPR countries. Such information needs to be further explored in order to better place appropriate prevention policies in promoting healthy eating across WPR countries in the future.
Stress, fear, food shortages, and confined lifestyle during the COVID-19 pandemic may have detrimental effects on pregnancy outcomes. The effect on COVID-19 infection on the pregnancy outcome has been reported in various countries.63 In China, a study from Wuhan City (where COVID-19 outbreak was reported) suggested that COVID-19 during later pregnancy was associated with an over 3 times increased risks of preterm birth (OR 3.34, 95% CI 1.60–7.00) and caesarean section delivery (OR 3.63, 95% CI 1.95–6.76).64 In the Republic of Korea, the prevalence of preterm birth was 38.5% among pregnant women infected with COVID-19.65 The long-term inter-generational effects of the COVID-19 pandemic on NCDs are of concerns and need to be monitored in the future.
Although the factors discussed above are common that impacted by COVID-19, sleep and environment are only factors that included in the systemic reviews in the WPR (Table 3). COVID-19 has significantly increased the risk for sleep disorder, but its effect on environment is beneficial due to decreases in mobility.35 Accumulating studies reported COVID-19 itself is the risk factor for NCDs, but existing data have often failed to incorporate this risk factor in exploring its link to NCDs, indicating further research is needed.
Long COVID-19 and NCDs as future research direction
Different variants of COVID-19 affect mortality and NCD burdens differently. Delta wave increases progressively in-hospital mortality, followed by Omicron BA.1/BA.2 and Omicron BA.4/BA.5 wave in South Africa.66 Post-COVID symptom, including fatigue, cough, heart palpitations, shortness of breath and anxiety/depression were similar between Omicron (B.1.1.529) and Delta (B.1.617.2), while Omicron had less musculoskeletal pain than Delta.67
Long-term effects of COVID-19 (long COVID) or a post-COVID-19 syndrome, is known to impact negatively multiple organ systems.68 The adverse health effects range from ‘invisible symptoms’ (e.g., fatigue and difficulty concentrating) to various cardiopulmonary, neuromuscular, haematological, and gastrointestinal sequelae.68, 69, 70 Evidence from severe COVID-19 survivors in Wuhan China suggested about half of the individuals had symptoms of depression 18 months after discharge.71 As a result, long COVID substantially increases the needs for NCD care, further direct-medical costs and the healthcare services utilization.72 Reposition health system, including planning, budgeting and resource allocation, for long COVID and its implications are recommended by NCD Alliance.73
Conclusions
The impact of the COVID-19 pandemic on NCDs burden in the WPR was substantial. COVID-19 led to both health and economic consequences not only at individual level, also at country and global level. Given the diverse populations in the WPR, policies and guidelines should be developed to mitigate the consequence of COVID-19 pandemic in health system and address specific needs in WPR countries through international collaboration.
Contributors
XX, ZS, YFW, and YGW initiated the concepts; LHZ, JL, and XX screened the publications and extracted data; LHZ, JL, and XX and ZS analyzed the data and produced figures; and XX and ZS drafted the manuscript. All authors interpreted the data, revised the manuscript critically, and approved the submission of the manuscript.
Declaration of interests
The authors declared no conflict of interest.
Acknowledgement
We thank Dr. Yue Ma for her assistance in logistic support and editing, and thank Profs Dongfeng Gu, Wen Peng, Lin Zhang, Liang Sun, Xiaomin Sun, Fengchao Liang, Xueli Yang, and Ruiyue Yang for their comments to help improve the manuscript.
Funding: The study is supported in part by National Natural Science Foundation of China (No. 71910107004, 91746205), Major Science and Technology Project of Public Health in Tianjin (No. 21ZXGWSY00090), and National Heart Foundation of Australia Post-doctoral Fellowship (No. 102597).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100795.
Contributor Information
Youfa Wang, Email: youfawang@xjtu.edu.cn.
Yaogang Wang, Email: YaogangWang@tmu.edu.cn.
Appendix A. Supplementary data
References
- 1.Gobiņa I., Avotiņš A., Kojalo U., et al. Excess mortality associated with the COVID-19 pandemic in Latvia: a population-level analysis of all-cause and noncommunicable disease deaths in 2020. BMC Public Health. 2022;22(1):1–12. doi: 10.1186/s12889-022-13491-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2022. WHO coronavirus (COVID-19) dashboard.https://covid19.who.int/ [Google Scholar]
- 3.Shin H.R., Varghese C.J.E. WHO Western Pacific regional action plan for the prevention and control of NCDs (2014-2020) Epidemiol Health. 2014;36 doi: 10.4178/epih/e2014007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2022. Noncommunicable diseases. [Google Scholar]
- 5.Bennett J.E., Stevens G.A., Mathers C.D., et al. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392(10152):1072–1088. doi: 10.1016/S0140-6736(18)31992-5. [DOI] [PubMed] [Google Scholar]
- 6.Wang H., Paulson K.R., Pease S.A., et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022;399(10334):1513–1536. doi: 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guo L., Shi Z., Zhang Y., et al. Comorbid diabetes and the risk of disease severity or death among 8807 COVID-19 patients in China: a meta-analysis. Diabetes Res Clin Pract. 2020;166 doi: 10.1016/j.diabres.2020.108346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang A.Y., Cullen M.R., Harrington R.A., Barry M. The impact of novel coronavirus COVID-19 on noncommunicable disease patients and health systems: a review. J Intern Med. 2021;289(4):450–462. doi: 10.1111/joim.13184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gadsden T., Downey L.E., Vilas V.D.R., Peiris D., Jan S. The impact of COVID-19 on essential health service provision for noncommunicable diseases in the South-East Asia region: a systematic review. Lancet Reg Health Southeast Asia. 2022;1 doi: 10.1016/j.lansea.2022.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Organization WH . World Health Organization; 2020. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. [Google Scholar]
- 11.Ministry of Health Singapore . 2022. Report on excess mortality during the COVID-19 pandemicup to June 2022. [Google Scholar]
- 12.Tu W.J., Xu Y., Chen H., Li J., Du J. Impact of the COVID-19 pandemic lockdown on hospitalizations for cerebrovascular disease and related in-hospital mortality in China: a nationwide observational study. Arch Gerontol Geriatr. 2022;104 doi: 10.1016/j.archger.2022.104832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quiles L.E.P., Diamante P.A.B., Pascual J.L.V. Impact of the COVID-19 pandemic in the acute stroke admissions and outcomes in a philippine tertiary hospital. Cerebrovasc Dis Extra. 2022;12(2):76–84. doi: 10.1159/000525057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phua K., Chew N.W.S., Sim V., et al. One-year outcomes of patients with ST-segment elevation myocardial infarction during the COVID-19 pandemic. J Thromb Thrombolysis. 2022;53(2):335–345. doi: 10.1007/s11239-021-02557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morishita T., Takada D., Shin J.H., Higuchi T., Kunisawa S., Imanaka Y. Trends, treatment approaches, and in-hospital mortality for acute coronary syndrome in Japan during the coronavirus disease 2019 pandemic. J Atheroscler Thromb. 2022;29(5):597–607. doi: 10.5551/jat.62746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhong M., Xiong H., Zhang K., Fu S. The impact of COVID-19 on the acute stroke care pathway: looking beyond the short term. Int J Gen Med. 2022;15:3069–3075. doi: 10.2147/IJGM.S349356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Z., Chen M., Hu Q., Chen Y., Tang J. Reduction of inhospital mortality of patient admissions to cardiac intensive care units during the COVID-19 pandemic in Hunan, China. Int Heart J. 2021;62(3):540–545. doi: 10.1536/ihj.20-522. [DOI] [PubMed] [Google Scholar]
- 18.Liu J., Yang Q., Zhang X., et al. A sharp decline in burden of stroke in rural China during COVID-19 pandemic. Front Neurol. 2020;11 doi: 10.3389/fneur.2020.596871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu Q., Lin B., Zhu C., Hu J. Emergency hospitalization caused by non-COVID-19 respiratory diseases before and during the COVID-19 pandemic: a retrospective observational cohort study. Front Med (Lausanne) 2022;9 doi: 10.3389/fmed.2022.929353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kasuga A., Nojima M., Okamoto T., et al. Impact of the COVID-19 pandemic on the management and end-of-life care of unresectable pancreatic cancer. Intern Med. 2022;61:3641. doi: 10.2169/internalmedicine.0492-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiong X., Wai A.K.C., Wong J.Y.H., et al. Impact of varying wave periods of COVID-19 on in-hospital mortality and length of stay for admission through emergency department: a territory-wide observational cohort study. Influenza Other Respir Viruses. 2022;16(2):193–203. doi: 10.1111/irv.12919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ohashi Y., Takane Y., Nakajima K. Impact of the COVID-19 pandemic on changes in temperature-sensitive cardiovascular and respiratory disease mortality in Japan. PLoS One. 2022;17(10) doi: 10.1371/journal.pone.0275935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nomura S., Eguchi A., Ghaznavi C., et al. Excess deaths from non-COVID-19-related causes in Japan and 47 prefectures from January 2020 through May 2021 by place of death. SSM Popul Health. 2022;19 doi: 10.1016/j.ssmph.2022.101196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luo Q., O'Connell D.L., Yu X.Q., et al. Cancer incidence and mortality in Australia from 2020 to 2044 and an exploratory analysis of the potential effect of treatment delays during the COVID-19 pandemic: a statistical modelling study. Lancet Public Health. 2022;7(6):e537–e548. doi: 10.1016/S2468-2667(22)00090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lai H., Yang M., Sun M., et al. Risk of incident diabetes after COVID-19 infection: a systematic review and meta-analysis. Metabolism. 2022;137 doi: 10.1016/j.metabol.2022.155330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gbadamosi M.A., Tlou B. Modifiable risk factors associated with non-communicable diseases among adult outpatients in Manzini, Swaziland: a cross-sectional study. BMC Public Health. 2020;20(1):665. doi: 10.1186/s12889-020-08816-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Venkatesulu B.P., Chandrasekar V.T., Girdhar P., et al. A systematic review and meta-analysis of cancer patients affected by a novel coronavirus. medRxiv. 2021;5:kaa102. doi: 10.1093/jncics/pkaa102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zarifkar P., Kamath A., Robinson C., et al. Clinical characteristics and outcomes in patients with COVID-19 and cancer: a systematic review and meta-analysis. Clin Oncol. 2021;33(3):E180–E191. doi: 10.1016/j.clon.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang H., Han H., He T., et al. Clinical characteristics and outcomes of COVID-19-infected cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst. 2021;113(4):371–380. doi: 10.1093/jnci/djaa168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li W., Zhang H., Zhang C., et al. The prevalence of psychological status during the COVID-19 epidemic in China: a systemic review and meta-analysis. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.614964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sun F., Zhu J., Tao H., Ma Y., Jin W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J Psychosom Obstet Gynaecol. 2021;42(2):91–99. doi: 10.1080/0167482X.2020.1857360. [DOI] [PubMed] [Google Scholar]
- 32.Tran Q.D., Vu T.Q.C., Phan N.Q. Depression prevalence in Vietnam during the Covid-19 pandemic: a systematic review and meta-analysis. Ethics Med Public Health. 2022;23 doi: 10.1016/j.jemep.2022.100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Y., Chen B., Hong Z., et al. Insomnia symptoms during the early and late stages of the COVID-19 pandemic in China: a systematic review and meta-analysis. Sleep Med. 2022;91:262–272. doi: 10.1016/j.sleep.2021.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xia L., Chen C.H., Liu Z.Q., et al. Prevalence of sleep disturbances and sleep quality in Chinese healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.646342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khan I., Shah D., Shah S.S. COVID-19 pandemic and its positive impacts on environment: an updated review. Int J Environ Sci Technol. 2021;18(2):521–530. doi: 10.1007/s13762-020-03021-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mekanna A.N., Panchal S.K., Li L. Beyond lockdowns: a systematic review of the impacts of COVID-19 lockdowns on dietary pattern, physical activity, body weight, and food security. Nutr Rev. 2022:nuac088. doi: 10.1093/nutrit/nuac088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zheng X., Wang Y., Zhang Y., Deng T., Yang Y. Impacts of COVID-19 pandemic on dietary consumption among Chinese residents: evidence from provincial-level panel data. Int J Environ Res Public Health. 2022;19(13) doi: 10.3390/ijerph19137612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang G.Y., Lin X.L., Fang A.P., Zhu H.L. Eating habits and lifestyles during the initial stage of the COVID-19 lockdown in China: a cross-sectional study. Nutrients. 2021;13(3):970. doi: 10.3390/nu13030970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang X., Lei S.M., Le S., et al. Bidirectional influence of the COVID-19 pandemic lockdowns on health behaviors and quality of life among Chinese adults. Int J Environ Res Public Health. 2020;17(15) doi: 10.3390/ijerph17155575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jia P., Liu L., Xie X., et al. Changes in dietary patterns among youths in China during COVID-19 epidemic: the COVID-19 impact on lifestyle change survey (COINLICS) Appetite. 2021;158 doi: 10.1016/j.appet.2020.105015. [DOI] [PubMed] [Google Scholar]
- 41.Jiao W., Liu M.T., Schulz P.J., Chang A. Impacts of self-efficacy on food and dietary choices during the first COVID-19 lockdown in China. Foods. 2022;11(17) doi: 10.3390/foods11172668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiao W., Xiang Y.T., Chang A. Are foods from the COVID-19 pandemic lockdown low in nutrients? An analysis of Chinese psychological distress effects. Nutrients. 2022;14(21):4702. doi: 10.3390/nu14214702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nguyen T.T., Nguyen M.H., Pham T.T.M., et al. Negative impacts of COVID-19 induced lockdown on changes in eating behavior, physical activity, and mental health as modified by digital healthy diet literacy and eHealth literacy. Front Nutr. 2021;8 doi: 10.3389/fnut.2021.774328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Duong T.V., Pham K.M., Do B.N., et al. Digital healthy diet literacy and self-perceived eating behavior change during COVID-19 pandemic among undergraduate nursing and medical students: a rapid online survey. Int J Environ Res Public Health. 2020;17(19):7185. doi: 10.3390/ijerph17197185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sato K., Kobayashi S., Yamaguchi M., et al. Working from home and dietary changes during the COVID-19 pandemic: a longitudinal study of health app (CALO mama) users. Appetite. 2021;165 doi: 10.1016/j.appet.2021.105323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shimpo M., Akamatsu R., Kojima Y., Yokoyama T., Okuhara T., Chiba T. Factors associated with dietary change since the outbreak of COVID-19 in Japan. Nutrients. 2021;13(6):2039. doi: 10.3390/nu13062039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mun H., So E.S. Changes in physical activity, healthy diet, and sleeping time during the COVID-19 pandemic in South Korea. Nutrients. 2022;14(5):960. doi: 10.3390/nu14050960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tan S.T., Tan C.X., Tan S.S. Changes in dietary intake patterns and weight status during the COVID-19 lockdown: a cross-sectional study focusing on young adults in Malaysia. Nutrients. 2022;14(2):280. doi: 10.3390/nu14020280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gerritsen S., Egli V., Roy R., et al. Seven weeks of home-cooked meals: changes to New Zealanders' grocery shopping, cooking and eating during the COVID-19 lockdown. J R Soc N Z. 2021;51:S4–S22. [Google Scholar]
- 50.Yu B., Zhang D., Yu W., Luo M., Yang S., Jia P. Impacts of lockdown on dietary patterns among youths in China: the COVID-19 Impact on Lifestyle Change Survey. Publ Health Nutr. 2021;24(11):3221–3232. doi: 10.1017/S1368980020005170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Di Renzo L., Gualtieri P., Pivari F., et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):1–15. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fullman N., Yearwood J., Abay S.M., et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391(10136):2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yoosefi Lebni J., Ziapour A., Mehedi N., Irandoost S.F. The role of clerics in confronting the COVID-19 crisis in Iran. J Relig Health. 2021;60(4):2387–2394. doi: 10.1007/s10943-021-01295-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Combi C., Pozzani G., Pozzi G. Telemedicine for developing countries. A survey and some design issues. Appl Clin Inform. 2016;7(4):1025–1050. doi: 10.4338/ACI-2016-06-R-0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.World Health Organization . 2021. Digital technology and COVID-19 in the Western Pacific region. [Google Scholar]
- 56.Wu J., Mamas M.A., Mohamed M.O., et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107(2):113–119. doi: 10.1136/heartjnl-2020-317912. [DOI] [PubMed] [Google Scholar]
- 57.Wadhera R.K., Shen C., Gondi S., Chen S., Kazi D.S., Yeh R.W. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77(2):159–169. doi: 10.1016/j.jacc.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yan A.F., Sun X., Zheng J., et al. Perceived risk, behavior changes and Health-related outcomes during COVID-19 pandemic: findingsamong adults with and without diabetesin China. Diabetes Res Clin Pract. 2020;167 doi: 10.1016/j.diabres.2020.108350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yoneoka D., Tanoue Y., Kawashima T., et al. Large-scale epidemiological monitoring of the COVID-19 epidemic in Tokyo. Lancet Reg Health West Pac. 2020;3 doi: 10.1016/j.lanwpc.2020.100016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu X., Yan A.F., Wang Y., Shi Z. Dietary patterns and changes in weight status among Chinese men and women during the COVID-19 pandemic. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.709535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hawkes C., Ambikapathi R., Anastasiou K., et al. From food price crisis to an equitable food system. Lancet. 2022;400(10350):413–416. doi: 10.1016/S0140-6736(22)01348-4. [DOI] [PubMed] [Google Scholar]
- 62.Godfrey K.M., Barker D.J. Fetal nutrition and adult disease. Am J Clin Nutr. 2000;71(5 Suppl) doi: 10.1093/ajcn/71.5.1344s. [DOI] [PubMed] [Google Scholar]
- 63.Wei S.Q., Bilodeau-Bertrand M., Liu S., Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021;193(16):E540–E548. doi: 10.1503/cmaj.202604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang R., Mei H., Zheng T., et al. Pregnant women with COVID-19 and risk of adverse birth outcomes and maternal-fetal vertical transmission: a population-based cohort study in Wuhan, China. BMC Med. 2020;18(1):330. doi: 10.1186/s12916-020-01798-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chung Y., Kim E.J., Kim H.S., et al. Maternal and neonatal outcomes in pregnant women with coronavirus disease 2019 in Korea. J Korean Med Sci. 2022;37(41):e297. doi: 10.3346/jkms.2022.37.e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jassat W., Abdool Karim S.S., Ozougwu L., et al. Trends in cases, hospitalization and mortality related to the Omicron BA.4/BA.5 sub-variants in South Africa. Clin Infect Dis. 2022;76:1468. doi: 10.1093/cid/ciac921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Magnusson K., Kristoffersen D.T., Dell'Isola A., et al. Post-covid medical complaints following infection with SARS-CoV-2 Omicron vs Delta variants. Nat Commun. 2022;13(1):7363. doi: 10.1038/s41467-022-35240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Davis H.E., McCorkell L., Vogel J.M., Topol E.J. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21:133. doi: 10.1038/s41579-022-00846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nalbandian A., Sehgal K., Gupta A., et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xie Y., Xu E., Bowe B., Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583–590. doi: 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhou J., Yang Y., Jiang L., Liu X.F., Liu X.Y., Wang L.R. 18-month mental health outcomes among survivors of severe COVID-19 in Wuhan, China. Asian J Psychiatr. 2023;81 doi: 10.1016/j.ajp.2023.103453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tene L., Bergroth T., Eisenberg A., David S.S.B., Chodick G. Risk factors, health outcomes, healthcare services utilization, and direct medical costs of patients with long COVID. Int J Infect Dis. 2022;128:3–10. doi: 10.1016/j.ijid.2022.12.002. [DOI] [PubMed] [Google Scholar]
- 73.NCD Alliance . 2020. Briefing note: impacts of COVID-19 on people living with NCDs.https://ncdalliance.org/resources/briefing-note-impacts-of-covid-19-on-people-living-with-ncds [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.