Summary
Background
Long-term projections of premature mortality (defined as deaths age <75 years) help to inform decisions about public health priorities. This study aimed to project premature mortality rates in Australia to 2044, and to estimate numbers of deaths and potential years of life lost (PYLL) due to premature mortality overall and for 59 causes.
Methods
We examined the past trends in premature mortality rates using Australian mortality data by sex, 5-year age group and 5-year calendar period up to 2019. Cigarette smoking exposure data (1945–2019) were included to project lung cancer mortality. Age-period-cohort or generalised linear models were developed and validated for each cause to project premature mortality rates to 2044.
Findings
Over the 25-year period from 1990–1994 to 2015–2019, there was a 44.4% decrease in the overall age-standardised premature mortality rate. This decline is expected to continue, from 162.4 deaths/100,000 population in 2015–2019 to 141.7/100,000 in 2040–2044 (12.7% decrease). Despite declining rates, total numbers of premature deaths are projected to increase by 22.8%, rising from 272,815 deaths in 2015–2019 to 334,894 deaths in 2040–2044. This is expected to result in 1.58 million premature deaths over the 25-year period 2020–2044, accounting for 24.5 million PYLL. Of the high-level cause categories, cancer is projected to remain the most common cause of premature death in Australia by 2044, followed by cardiovascular disease, external causes (including injury, poisoning, and suicide), and respiratory diseases.
Interpretation
Despite continuously declining overall premature mortality rates, the total number of premature deaths in Australia is projected to remain substantial, and cancer will continue to be the leading cause. These projections can inform the targeting of public health efforts and can serve as benchmarks against which to measure the impact of future interventions. They emphasise the ongoing importance of accelerating the prevention, early detection, and treatment of key health conditions.
Funding
No funding was provided for this study.
Keywords: Premature mortality, Potential years of life lost, Statistical projections, Australia, Tobacco consumption, Age-period-cohort model, Generalised linear model, Cancer, Cardiovascular disease, Suicide
Research in context.
Evidence before this study
Premature mortality is a measure of unfulfilled life expectancy. As many premature deaths are potentially avoidable, preventing premature death is a key goal of many public health programs. Long-term projections of future premature mortality can help to inform decisions about which areas for action could have the greatest impact and benefits, and which should therefore be prioritised. Medline, Embase and PreMEDLINE databases were searched on 30 April 2023, for articles published in English from 1 January 2013 that used statistical methods to project national premature mortality rates for at least 20 years into the future, for all causes combined and for detailed cause of death categories. We used the search terms “forecast$ or extrapolat$ or projection$ or predict$” and “death$ or mortality” and “population”. We found two studies reporting projections for mortality from any cause for 20+ years in Korea and Nepal, and one Global Burden of Diseases (GBD) study reporting mortality projections for all ages in 195 countries and territories (including Australia). Although the GBD study provided important insights into the distribution of global health issues, their standardised modelling approach might not explicitly capture the trends in premature mortality for a specific population.
Added value of this study
We examined the trends in premature mortality rates for Australia during 1990–2019 and projected these rates from 2020 to 2044 for all causes combined and for 59 cause of death categories. For each cause category we developed and validated statistical projection models for males and females separately. The observed declines in the premature mortality rates for both males and females are expected to continue, albeit more slowly, over the projection period 2020–2044 for all age groups and across most of the major causes of death. In Australia, despite the continuous decline in the premature mortality rates for all causes, our projections suggest that the total number of premature deaths will increase and continue to be substantial. The analyses predict that there will be 1.58 million premature deaths during the 25-year period 2020–2044, accounting for a total of 24.5 million potential years of life lost.
Implications of all the available evidence
Australia is a high-income country with one of the lowest premature mortality rates in the world. However, our projections suggest that the decreases in the overall premature mortality rates during 2020–2044 will occur at a slower pace than has been observed in the previous 25 years. Our study found that cancer and cardiovascular disease will continue to be the leading causes of premature death in Australia in 2044. This suggests that the gains made from existing public health measures implemented in the past two decades will lessen over time. These projections can serve as benchmarks against which to measure the impact of future interventions, and emphasise the need for continued efforts in policy implementation and accelerating the prevention, early detection, and treatment of key health conditions.
Introduction
Australia is a high-income country that has an average life expectancy among the highest in the world, with two-thirds of deaths in Australia in 2019 occurring in people aged 75 years and older.1 However, as over one-third of all deaths in Australia in 2019 still occurred before the age of 75 years, “premature deaths” (deaths occurring before the average life expectancy in Australia) remain a significant concern. Premature mortality is a measure of unfulfilled life expectancy, especially as it has been estimated that as many as half of the premature deaths in Australia in 2010–2012 were potentially avoidable.2 Preventing premature death is a key goal of many public health programs, and long-term projections of future premature mortality can help to inform the prioritisation of areas requiring action that could have the greatest impact and benefit. However, only a limited number of studies have reported long term (20+ years) projections of premature mortality, with only one Global Burden of Diseases (GBD) study reporting projections of mortality from any cause for 20+ years for Australia and 194 other countries and territories.3
The aims of this study were to quantify and examine the trends in premature mortality rates in Australia, and to project these rates to 2044 for all causes of death combined and for 59 cause of death categories. We also estimated the numbers of premature deaths and potential years of life lost (PYLL) due to premature mortality for all causes and for 59 cause of death categories. Results from this study provide information on recent patterns and predict changes in premature deaths in Australia over the 25 years from 2020 to 2044.
Methods
Data sources
We sourced national data for the numbers of deaths from all causes combined and for the individual cause of death categories by sex, 5-year age group up to 74 years and calendar year from the Australian Institute of Health and Welfare (AIHW), which do not contain missing data.1 The cause of death categories were classified by the AIHW using the International Classification of Diseases and Related Health Problems codes.4 Categories with sufficient numbers of deaths to provide robust and valid projections are included in this study (Supplementary material Table S1), with two levels of cause of death groups being reported: 16 high-level groups (level-1 cause groups) and 43 more detailed cause of death categories (level-2 cause groups). A total of 36 cause of death categories were noncommunicable diseases (NCDs).5 An external cause is defined as the event, circumstance or condition associated with the occurrence of injury, poisoning, suicide or violence. Australian population counts for age up to 74 years by sex, 5-year age group and calendar year from 1955 to 2044 (Series B, assuming medium population growth) were obtained from the Australian Bureau of Statistics (ABS).6 These data predict an increasing population size for age up to 74 years from 23.7 million in 2019 to 31.5 million by 2044. Data on cigarette smoking exposure levels for 1945–2004 were obtained from the International Smoking Statistics Web Edition,7 and more recent cigarette smoking exposure data from the National Drug Strategy Household Survey (2007–2019) were obtained from the AIHW.8 Detailed descriptions of the data sources and data preparation for smoking exposure have been described previously.9 All aggregated measures of smoking exposure were weighted to the Australian population and data were interpolated for missing years assuming a constant annual rate of change between two adjacent known values.9 All age-standardised rates were standardised to the Segi World standard population for the main results to allow international comparisons. Age-standardised rates using the 2001 Australian population were included in Supplementary material Figure S13.
Projection models and model selection
Detailed information about the model development and validation are provided in the Supplementary material pp 6–12. We used log-linear period models with one age group (0–4 years) to project mortality rates for conditions in the perinatal period and for sudden infant death syndrome. For the projections of lung cancer mortality we used a previously validated generalised linear model (GLM) with cigarette smoking consumption as a covariate (with a 26 year lag for males and a 29 year lag for females).9 Age-stratified age-period-cohort (APC) models10 or standard APC models11 were used to project mortality rates for each of the remaining cause of death categories (Supplementary material Table S2). APC models are flexible and can implicitly incorporate changes in relevant risk factors that are reflected in past trends in the mortality rates.12 We defined the uncertainty interval (UI) as the confidence interval of the estimates based on the variances for the parameters in the model. The most appropriate statistical projection model for each cause category was selected based on the lowest Bayesian information criterion, and was validated by withholding the most recent 15 years of observed data from the model fitting and then comparing the projected mortality rates for those years with the actual observed values. This validation process showed that the 95% UIs for the projected rates generally captured the observed values, suggesting that the approach provides valid projections of premature mortality in Australia (Supplementary material Figure S3).
To project mortality rates for cause categories other than lung cancer beyond the observed period, future periods and cohorts were assumed to have the same effect as those for the most recently observed period and cohort.11 We used the default setting for the damping factor (equal to 0.92), so that the drift will be about half of that during the last observation period after 8 years, which provides similar adjustment to the damping factor used in other APC modelling approaches (NordPred, as validated previously).13 This takes into account the fact that the period and cohort effects will wane and current trends in mortality rates are not expected to continue over time.14 For lung cancer mortality, we used cohort-specific cigarette tar exposure to predict the future cohort effects (Supplementary material pp 10).9
We estimated PYLL for each age group and calendar period by multiplying the age-specific number of premature deaths by the difference between age 75 years and the estimated age at death (Supplementary material p 12). Sensitivity analyses were conducted by (1) using different damping factors and (2) by using age 70 years as the upper limit for premature death in Australia. We report the main results for four large age categories, under 5, 5–29, 30–49 and 50–74 years, based on the distribution of causes of death; detailed results by 5-year age groups are provided in Supplementary material Figures S14–S27. All statistical analyses were performed using Stata (version 17, Stata Corporation, College Station, TX).
Role of the funding source
No funding was provided for this study.
Results
Projections of premature mortality rates
The age-standardised premature mortality rate for all causes combined for Australia was 292.1 per 100,000 population in 1990–1994 and declined by 44.4% over the 25-year observed period to 162.4 per 100,000 in 2015–2019 (Supplementary material Table S3). Projections indicate that this trend will continue over the next 25-year period, with an estimated 12.7% decline in the age-standardised premature mortality rate, from 162.4 per 100,000 in 2015–2019 to 141.7 per 100,000 in 2040–2044 (Table 1).
Table 1.
Observed (2015–2019) and projected (2040–2044) age-standardised premature mortality rates per 100,000 and number of premature deaths for all causes combined and for different cause of death categories, Australia.
| Age-standardised mortality ratea |
Number of premature deaths |
||||||
|---|---|---|---|---|---|---|---|
| Observed 2015–2019 | Projected in 2040–2044 (95% UI) | Change in rates % (95% UI)b | Observed 2015–2019 | Projected in 2040–2044 (95% UI) | Change in deaths % (95% UI)c | Total projected in 2020–2044 (95% UI) | |
| Total–all causes | 162.4 | 141.7 (115.0–177.3) | −12.7 (−29.2, 9.2) | 272,815 | 334,894 (271,946–405,604) | 22.8 (−0.3, 48.7) | 1,578,500 (1,324,442–1,837,431) |
| Males–all causes | 204.2 | 178.6 (147.0–219.8) | −12.5 (−28.0, 7.6) | 168,950 | 204,447 (168,521–245,439) | 21.0 (−0.3, 45.3) | 962,753 (818,597–1,113,310) |
| Cancer | 70.7 | 57.6 (45.5–73.1) | −18.5 (−35.6, 3.4) | 63,460 | 69,914 (56,076–87,151) | 10.2 (−11.6, 37.3) | 338,568 (286,074–402,478) |
| Lung cancer | 14.4 | 8.3 (5.6–10.9) | −42.4 (−61.1, −24.3) | 13,440 | 10,414 (7271–13,556) | −22.5 (−45.9, 0.9) | 58,253 (48,263–68,243) |
| Colorectal cancer | 7.8 | 6.8 (5.4–8.8) | −12.8 (−30.8, 12.8) | 6975 | 7850 (6362–9941) | 12.5 (−8.8, 42.5) | 36,989 (31,266–44,606) |
| Pancreatic cancer | 4.7 | 4.7 (4.0–5.4) | 0.0 (−14.9, 14.9) | 4285 | 5731 (4954–6628) | 33.7 (15.6, 54.7) | 26,146 (23,090–29,615) |
| Prostate cancer | 4.3 | 3.9 (3.4–4.5) | −9.3 (−20.9, 4.7) | 4245 | 5366 (4708–6113) | 26.4 (10.9, 44.0) | 25,209 (22,484–28,281) |
| Liver cancer | 4.7 | 5.5 (4.4–6.9) | 17.0 (−6.4, 46.8) | 4215 | 6719 (5380–8394) | 59.4 (27.6, 99.1) | 31,031 (26,149–36,923) |
| Brain cancer | 4.1 | 4.1 (2.9–5.9) | 0.0 (−29.3, 43.9) | 3295 | 4426 (3190–6211) | 34.3 (−3.2, 88.5) | 20,036 (15,299–26,557) |
| Oesophageal cancer | 3.3 | 2.9 (2.5–3.5) | −12.1 (−24.2, 6.1) | 2985 | 3599 (3039–4261) | 20.6 (1.8, 42.7) | 16,732 (14,486–19,341) |
| Leukaemia | 2.7 | 2.3 (1.8–3.2) | −14.8 (−33.3, 18.5) | 2375 | 2716 (2198–3480) | 14.4 (−7.5, 46.5) | 12,876 (10,692–15,945) |
| Melanoma | 2.7 | 1.3 (1.0–1.6) | −51.9 (−63.0, −40.7) | 2345 | 1514 (1214–1886) | −35.4 (−48.2, −19.6) | 9256 (7805–11,000) |
| Oral cancer | 2.5 | 2.4 (1.9–3.1) | −4.0 (−24.0, 24.0) | 2185 | 2869 (2289–3593) | 31.3 (4.8, 64.4) | 12,946 (10,753–15,604) |
| Non-Hodgkin lymphoma | 2.2 | 1.8 (1.4–2.5) | −18.2 (−36.4, 13.6) | 1970 | 2229 (1729–2935) | 13.1 (−12.2, 49.0) | 10,580 (8513–13,332) |
| Stomach cancer | 2.1 | 1.7 (1.4–2.0) | −19.0 (−33.3, −4.8) | 1905 | 2092 (1730–2531) | 9.8 (−9.2, 32.9) | 10,016 (8518–11,783) |
| Kidney cancer | 1.9 | 1.6 (1.2–2.3) | −15.8 (−36.8, 21.1) | 1670 | 1965 (1431–2726) | 17.7 (−14.3, 63.2) | 9239 (7067–12,236) |
| Bladder cancer | 1.1 | 1.0 (0.8–1.2) | −9.1 (−27.3, 9.1) | 1040 | 1247 (983–1580) | 19.9 (−5.5, 51.9) | 5928 (4845–7270) |
| Laryngeal cancer | 0.5 | 0.3 (0.2–0.5) | −40.0 (−60.0, 0.0) | 465 | 414 (291–585) | −11.0 (−37.4, 25.8) | 2079 (1544–2810) |
| Gallbladder and bile duct cancer | 0.3 | 0.3 (0.2–0.4) | 0.0 (−33.3, 33.3) | 260 | 342 (211–548) | 31.5 (−18.8, 110.8) | 1588 (1056–2382) |
| Thyroid cancer | 0.2 | 0.2 (0.1–0.4) | 0.0 (−50.0, 100.0) | 200 | 290 (189–444) | 45.0 (−5.5, 122.0) | 1281 (866–1892) |
| Testicular cancer | 0.2 | 0.2 (0.1–0.4) | 0.0 (−50.0, 100.0) | 110 | 166 (79–357) | 50.9 (−28.2, 224.5) | 728 (369–1444) |
| Other cancers | 10.5 | 8.3 (7.3–9.7) | −21.0 (−30.5, −7.6) | 9495 | 9965 (8828–11,382) | 4.9 (−7.0, 19.9) | 47,655 (43,009–53,214) |
| Cardiovascular disease | 38.6 | 33.3 (29.8–37.6) | −13.7 (−22.8, −2.6) | 34,350 | 41,106 (36,955–46,054) | 19.7 (7.6, 34.1) | 187,907 (171,921–206,514) |
| Coronary heart disease | 21.9 | 17.7 (16.6–19.0) | −19.2 (−24.2, −13.2) | 19,535 | 21,894 (20,490–23,400) | 12.1 (4.9, 19.8) | 101,491 (95,872–107,490) |
| Cerebrovascular disease | 5.7 | 5.5 (4.7–6.5) | −3.5 (−17.5, 14.0) | 5180 | 7095 (6083–8283) | 37.0 (17.4, 59.9) | 30,609 (27,008–34,757) |
| Hypertensive disease | 1.3 | 1.9 (1.4–2.7) | 46.2 (7.7, 107.7) | 1175 | 2447 (1793–3351) | 108.3 (52.6, 185.2) | 9803 (7536–12,822) |
| Other cardiovascular disease | 9.8 | 8.1 (7.1–9.5) | −17.3 (−27.6, −3.1) | 8460 | 9670 (8589–11,020) | 14.3 (1.5, 30.3) | 46,004 (41,505–51,445) |
| Respiratory diseases | 11.4 | 10.6 (8.9–13.1) | −7.0 (−21.9, 14.9) | 10,530 | 13,433 (11,532–16,103) | 27.6 (9.5, 52.9) | 61,242 (53,848–71,121) |
| COPD | 6.4 | 6.3 (5.5–7.4) | −1.6 (−14.1, 15.6) | 6155 | 8315 (7426–9575) | 35.1 (20.6, 55.6) | 37,524 (33,973–42,251) |
| Asthma | 0.5 | 0.6 (0.3–1.1) | 20.0 (−40.0, 120.0) | 385 | 585 (316–1067) | 51.9 (−17.9, 177.1) | 2461 (1453–4134) |
| Other respiratory diseases | 4.5 | 3.7 (3.1–4.6) | −17.8 (−31.1, 2.2) | 3990 | 4533 (3790–5461) | 13.6 (−5.0, 36.9) | 21,257 (18,422–24,736) |
| Digestive diseases | 8.7 | 8.8 (7.4–10.6) | 1.1 (−14.9, 21.8) | 7425 | 10,103 (8481–12,044) | 36.1 (14.2, 62.2) | 45,729 (39,608–52,875) |
| Liver disease | 6.0 | 6.2 (5.3–7.3) | 3.3 (−11.7, 21.7) | 5020 | 6956 (5985–8082) | 38.6 (19.2, 61.0) | 31,752 (28,016–35,983) |
| Other digestive diseases | 2.7 | 2.6 (2.1–3.3) | −3.7 (−22.2, 22.2) | 2405 | 3147 (2496–3962) | 30.9 (3.8, 64.7) | 13,977 (11,592–16,892) |
| Endocrine and metabolic diseases | 8.2 | 8.2 (6.6–10.3) | 0.0 (−19.5, 25.6) | 7110 | 11,932 (8075–12,140) | 67.8 (13.6, 70.7) | 55,921 (36,998–51,757) |
| Diabetes | 5.4 | 5.3 (4.5–6.2) | −1.9 (−16.7, 14.8) | 4935 | 6650 (5677–7798) | 34.8 (15.0, 58.0) | 29,871 (26,261–34,016) |
| Other endocrine and metabolic diseases | 2.7 | 2.9 (2.1–4.0) | 7.4 (−22.2, 48.1) | 2175 | 3202 (2398–4342) | 47.2 (10.3, 99.6) | 13,686 (10,737–17,741) |
| Diseases of the nervous system | 7.7 | 7.4 (6.3–8.6) | −3.9 (−18.2, 11.7) | 6550 | 8730 (7629–10,024) | 33.3 (16.5, 53.0) | 42,235 (37,773–47,386) |
| Infectious and parasitic diseases | 3.1 | 1.9 (1.5–2.4) | −38.7 (−51.6, −22.6) | 2575 | 2278 (1811–2861) | −11.5 (−29.7, 11.1) | 14,462 (12,017–17,437) |
| Mental and behavioural disorders | 2.5 | 2.9 (2.4–3.5) | 16.0 (−4.0, 40.0) | 2360 | 3525 (2922–4273) | 49.4 (23.8, 81.1) | 16,052 (13,701–18,923) |
| Conditions in the perinatal period | 4.8 | 2.7 (2.4–3.0) | −43.8 (−50.0, −37.5) | 1580 | 1167 (1045–1302) | −26.1 (−33.9, −17.6) | 6738 (6036–7520) |
| Congenital malformations | 3.3 | 2.6 (1.8–3.7) | −21.2 (−45.5, 12.1) | 1550 | 1573 (1096–2267) | 1.5 (−29.3, 46.3) | 7910 (5824–10,782) |
| Genitourinary diseases | 1.7 | 1.8 (1.2–2.6) | 5.9 (−29.4, 52.9) | 1525 | 2267 (1552–3339) | 48.7 (1.8, 119.0) | 9542 (6973–13,175) |
| Kidney failure | 1.0 | 0.9 (0.6–1.2) | −10.0 (−40.0, 20.0) | 960 | 1168 (849–1602) | 21.7 (−11.6, 66.9) | 5056 (3864–6605) |
| Other genitourinary diseases | 0.6 | 0.9 (0.6–1.4) | 50.0 (0.0, 133.3) | 565 | 1099 (703–1737) | 94.5 (24.4, 207.4) | 4486 (3109–6570) |
| Musculoskeletal diseases | 0.9 | 0.8 (0.6–1.0) | −11.1 (−33.3, 11.1) | 765 | 955 (728–1242) | 24.8 (−4.8, 62.4) | 4381 (3499–5480) |
| Diseases of the blood | 0.6 | 0.6 (0.3–1.0) | 0.0 (−50.0, 66.7) | 475 | 620 (360–1068) | 30.5 (−24.2, 124.8) | 2888 (1836–4575) |
| Diseases of the skin | 0.3 | 0.3 (0.2–0.8) | 0.0 (−33.3, 166.7) | 295 | 420 (187–926) | 42.4 (−36.6, 213.9) | 1825 (1005–3377) |
| External causes | 38.1 | 34.7 (28.7–42.5) | −8.9 (−24.7, 11.5) | 25,765 | 32,393 (27,011–39,252) | 25.7 (4.8, 52.3) | 149,560 (127,462–176,958) |
| Suicide | 16.3 | 17.3 (14.9–20.0) | 6.1 (−8.6, 22.7) | 10,960 | 15,951 (13,841–18,389) | 45.5 (26.3, 67.8) | 70,119 (61,830–79,561) |
| Accidental poisoning | 7.1 | 6.9 (5.6–8.5) | −2.8 (−21.1, 19.7) | 4860 | 6618 (5398–8126) | 36.2 (11.1, 67.2) | 30,327 (25,389–36,302) |
| Land transport accidents | 6.9 | 4.2 (3.3–5.2) | −39.1 (−52.2, −24.6) | 4355 | 3681 (2993–4532) | −15.5 (−31.3, 4.1) | 18,790 (15,740–22,482) |
| Assault | 1.3 | 1.2 (0.7–2.0) | −7.7 (−46.2, 53.8) | 815 | 991 (611–1652) | 21.6 (−25.0, 102.7) | 4544 (2977–7099) |
| Accidental drowning | 1.1 | 0.8 (0.4–1.6) | −27.3 (−63.6, 45.5) | 640 | 677 (363–1271) | 5.8 (−43.3, 98.6) | 3278 (1945–5584) |
| Other external causes | 5.5 | 4.4 (3.7–5.2) | −20.0 (−32.7, −5.5) | 4135 | 4475 (3805–5282) | 8.2 (−8.0, 27.7) | 22,502 (19,581–25,930) |
| Other causesd | 3.8 | 4.0 (2.9–5.6) | 5.3 (−23.7, 47.4) | 2635 | 4031 (3061–5393) | 53.0 (16.2, 104.7) | 17,793 (14,022–22,952) |
| SIDS | 0.3 | 0.0 (0.0–0.1) | 85 | 12 (4–44) | −85.9 (−95.3, −48.2) | 173 (79–419) | |
| Other causes excluding SIDS | 3.6 | 4.0 (2.9–5.5) | 11.1 (−19.4, 52.8) | 2550 | 4019 (3057–5349) | 57.6 (19.9, 109.8) | 17,620 (13,943–22,533) |
|
Females - all causes |
121.7 |
106.4 (84.5–136.6) |
−12.6 (−30.6, 12.2) |
103,865 |
130,447 (103,425–160,165) |
25.6 (−0.4, 54.2) |
615,747 (505,845–724,121) |
| Cancer | 53.5 | 42.7 (34.1–53.4) | −20.2 (−36.3, −0.2) | 48,440 | 53,987 (43,659–66,549) | 11.5 (−9.9, 37.4) | 262,271 (222,444–310,000) |
| Lung cancer | 10.0 | 6.0 (3.8–8.2) | −40.0 (−62.0, −18.0) | 9565 | 8147 (5389–10,907) | −14.8 (−43.7, 14.0) | 45,658 (36,683–54,633) |
| Breast cancer | 9.9 | 7.9 (7.1–8.8) | −20.2 (−28.3, −11.1) | 8740 | 9537 (8558–10,623) | 9.1 (−2.1, 21.5) | 46,669 (42,665–51,062) |
| Colorectal cancer | 5.2 | 4.2 (3.5–5.2) | −19.2 (−32.7, 0.0) | 4715 | 5251 (4401–6367) | 11.4 (−6.7, 35.0) | 24,972 (21,495–29,361) |
| Pancreatic cancer | 3.3 | 3.2 (2.8–3.8) | −3.0 (−15.2, 15.2) | 3200 | 4365 (3733–5106) | 36.4 (16.7, 59.6) | 19,906 (17,409–22,783) |
| Ovarian cancer | 2.9 | 2.2 (1.8–2.6) | −24.1 (−37.9, −10.3) | 2710 | 2749 (2341–3228) | 1.4 (−13.6, 19.1) | 13,636 (11,964–15,560) |
| Brain cancer | 2.5 | 2.4 (1.8–3.3) | −4.0 (−28.0, 32.0) | 2035 | 2744 (2071–3649) | 34.8 (1.8, 79.3) | 12,394 (9737–15,871) |
| Liver cancer | 1.8 | 2.1 (1.7–2.7) | 16.7 (−5.6, 50.0) | 1650 | 2742 (2176–3459) | 66.2 (31.9, 109.6) | 12,080 (9923–14,728) |
| Leukaemia | 1.7 | 1.4 (1.0–2.1) | −17.6 (−41.2, 23.5) | 1455 | 1687 (1262–2364) | 15.9 (−13.3, 62.5) | 7995 (6181–10,709) |
| Uterine cancer | 1.5 | 1.7 (1.5–2.0) | 13.3 (0.0, 33.3) | 1445 | 2280 (1968–2643) | 57.8 (36.2, 82.9) | 9971 (8710–11,424) |
| Melanoma | 1.3 | 0.9 (0.7–1.2) | −30.8 (−46.2, −7.7) | 1155 | 1118 (908–1376) | −3.2 (−21.4, 19.1) | 5955 (5048–7045) |
| Non-Hodgkin lymphoma | 1.2 | 0.9 (0.7–1.4) | −25.0 (−41.7, 16.7) | 1130 | 1208 (895–1700) | 6.9 (−20.8, 50.4) | 5789 (4485–7742) |
| Stomach cancer | 1.1 | 0.9 (0.7–1.2) | −18.2 (−36.4, 9.1) | 955 | 1163 (904–1501) | 21.8 (−5.3, 57.2) | 5378 (4330–6696) |
| Oesophageal cancer | 0.7 | 0.5 (0.4–0.7) | −28.6 (−42.9, 0.0) | 710 | 735 (558–970) | 3.5 (−21.4, 36.6) | 3524 (2767–4491) |
| Oral cancer | 0.7 | 0.6 (0.5–0.8) | −14.3 (−28.6, 14.3) | 640 | 800 (597–1072) | 25.0 (−6.7, 67.5) | 3718 (2886–4800) |
| Kidney cancer | 0.7 | 0.5 (0.3–0.9) | −28.6 (−57.1, 28.6) | 620 | 671 (436–174) | 8.2 (−29.7, 73.2) | 3274 (2270–4859) |
| Bladder cancer | 0.4 | 0.3 (0.2–0.3) | −25.0 (−50.0, −25.0) | 365 | 356 (275–462) | −2.5 (−24.7, 26.6) | 1724 (1356–2200) |
| Gallbladder and bile duct cancer | 0.4 | 0.3 (0.2–0.4) | −25.0 (−50.0, 0.0) | 350 | 369 (273–502) | 5.4 (−22.0, 43.4) | 1809 (1385–2367) |
| Thyroid cancer | 0.2 | 0.2 (0.1–0.3) | 0.0 (−50.0, 50.0) | 155 | 262 (160–428) | 69.0 (3.2, 176.1) | 1171 (756–1815) |
| Laryngeal cancer | 0.1 | 0.0 (0.0–0.1) | 60 | 50 (22–107) | −16.7 (−63.3, 78.3) | 254 (123–515) | |
| Other cancers | 7.6 | 6.4 (5.4–7.6) | −15.8 (−28.9, 0.0) | 6785 | 7753 (6732–9011) | 14.3 (−0.8, 32.8) | 36,394 (32,271–41,339) |
| Cardiovascular disease | 16.1 | 12.3 (10.5–14.7) | −23.6 (−34.8, −8.7) | 14,970 | 16,682 (14,428–19,458) | 11.4 (−3.6, 30.0) | 79,341 (70,142–90,403) |
| Coronary heart disease | 5.8 | 3.6 (3.2–4.1) | −37.9 (−44.8, −29.3) | 5555 | 4981 (4443–5598) | −10.3 (−20.0, 0.8) | 25,320 (22,939–28,009) |
| Cerebrovascular disease | 4.2 | 3.9 (3.3–4.6) | −7.1 (−21.4, 9.5) | 3910 | 5412 (4598–6375) | 38.4 (17.6, 63.0) | 24,140 (21,075–27,682) |
| Hypertensive disease | 0.6 | 0.5 (0.4–0.8) | −16.7 (−33.3, 33.3) | 590 | 761 (543–1065) | 29.0 (−8.0, 80.5) | 3497 (2629–4680) |
| Other cardiovascular disease | 5.5 | 4.3 (3.6–5.2) | −21.8 (−34.5, −5.5) | 4915 | 5528 (4844–6420) | 12.5 (−1.4, 30.6) | 26,384 (23,499–30,032) |
| Respiratory diseases | 8.5 | 8.9 (7.5–11.2) | 4.7 (−11.8, 31.8) | 8165 | 12,061 (10,334–14,548) | 47.7 (26.6, 78.2) | 53,292 (46,582–62,493) |
| COPD | 5.1 | 6.2 (5.4–7.5) | 21.6 (5.9, 47.1) | 5115 | 8695 (7718–10,119) | 70.0 (50.9, 97.8) | 37,189 (33,461–42,301) |
| Asthma | 0.5 | 0.5 (0.3–0.8) | 0.0 (−40.0, 60.0) | 415 | 519 (311–879) | 25.1 (−25.1, 111.8) | 2364 (1544–3694) |
| Other respiratory diseases | 2.9 | 2.2 (1.8–2.9) | −24.1 (−37.9, 0.0) | 2635 | 2847 (2305–3550) | 8.0 (−12.5, 34.7) | 13,739 (11,577–16,498) |
| Diseases of the nervous system | 5.7 | 5.2 (4.3–6.6) | −8.8 (−24.6, 15.8) | 4945 | 6520 (5531–7773) | 31.9 (11.9, 57.2) | 31,616 (27,678–36,453) |
| Endocrine and metabolic diseases | 4.7 | 4.8 (3.7–6.4) | 2.1 (−21.3, 36.2) | 4150 | 8787 (4906–8025) | 111.7 (18.2, 93.4) | 41,151 (22,208–33,237) |
| Diabetes | 2.9 | 2.9 (2.4–3.6) | 0.0 (−17.2, 24.1) | 2680 | 3975 (3267–4832) | 48.3 (21.9, 80.3) | 17,461 (14,945–20,435) |
| Other endocrine and metabolic diseases | 1.8 | 1.9 (1.3–2.8) | 5.6 (−27.8, 55.6) | 1470 | 2267 (1639–3193) | 54.2 (11.5, 117.2) | 9535 (7263–12,802) |
| Digestive diseases | 4.6 | 4.9 (3.9–6.3) | 6.5 (−15.2, 37.0) | 4130 | 6014 (4804–7548) | 45.6 (16.3, 82.8) | 27,080 (22,504–32,666) |
| Liver disease | 2.7 | 3.2 (2.5–4.1) | 18.5 (−7.4, 51.9) | 2340 | 3776 (3001–4765) | 61.4 (28.2, 103.6) | 16,659 (13,774–20,212) |
| Other digestive diseases | 1.9 | 1.7 (1.4–2.1) | −10.5 (−26.3, 10.5) | 1790 | 2238 (1803–2783) | 25.0 (0.7, 55.5) | 10,421 (8730–12,454) |
| Infectious and parasitic diseases | 1.9 | 1.4 (1.0–1.9) | −26.3 (−47.4, 0.0) | 1555 | 1779 (1338–2369) | 14.4 (−14.0, 52.3) | 9975 (7877–12,664) |
| Mental and behavioural disorders | 1.5 | 2.2 (1.8–2.8) | 46.7 (20.0, 86.7) | 1475 | 2966 (2413–3697) | 101.1 (63.6, 150.6) | 12,605 (10,479–15,372) |
| Congenital malformations | 2.7 | 2.5 (1.7–3.6) | −7.4 (−37.0, 33.3) | 1240 | 1401 (952–2068) | 13.0 (−23.2, 66.8) | 6843 (4926–9545) |
| Conditions in the perinatal period | 3.8 | 2.1 (1.8–2.5) | −44.7 (−52.6, −34.2) | 1190 | 872 (756–1009) | −26.7 (−36.5, −15.2) | 5110 (4457–5862) |
| Genitourinary diseases | 1.2 | 1.2 (0.8–1.8) | 0.0 (−33.3, 50.0) | 1165 | 1591 (1058–2414) | 36.6 (−9.2, 107.2) | 7053 (5032–9981) |
| Kidney failure | 0.7 | 0.5 (0.4–0.8) | −28.6 (−42.9, 14.3) | 670 | 747 (523–1079) | 11.5 (−21.9, 61.0) | 3426 (2535–4666) |
| Other genitourinary diseases | 0.5 | 0.6 (0.4–1.0) | 20.0 (−20.0, 100.0) | 495 | 844 (535–1335) | 70.5 (8.1, 169.7) | 3627 (2497–5315) |
| Musculoskeletal diseases | 1.1 | 0.9 (0.6–1.2) | −18.2 (−45.5, 9.1) | 1035 | 1149 (840–1576) | 11.0 (−18.8, 52.3) | 5412 (4220–7001) |
| Diseases of the blood | 0.5 | 0.5 (0.3–0.8) | 0.0 (−40.0, 60.0) | 435 | 589 (416–858) | 35.4 (−4.4, 97.2) | 2742 (2007–3801) |
| Diseases of the skin | 0.2 | 0.2 (0.1–0.5) | 0.0 (−50.0, 150.0) | 225 | 319 (150–683) | 41.8 (−33.3, 203.6) | 1437 (815–2637) |
| External causes | 13.5 | 14.1 (10.5–19.7) | 4.4 (−22.2, 45.9) | 9260 | 13,652 (10,380–18,538) | 47.4 (12.1, 100.2) | 60,316 (47,470–78,767) |
| Suicide | 5.4 | 6.6 (5.3–8.2) | 22.2 (−1.9, 51.9) | 3585 | 6110 (4942–7552) | 70.4 (37.9, 110.7) | 25,812 (21,401–31,170) |
| Accidental poisoning | 2.9 | 2.9 (2.0–4.2) | 0.0 (−31.0, 44.8) | 2065 | 2967 (2085–4237) | 43.7 (1.0, 105.2) | 13,209 (9774–17,967) |
| Land transport accidents | 2.2 | 1.5 (1.1–1.9) | −31.8 (−50.0, −13.6) | 1370 | 1309 (1020–1671) | −4.5 (−25.5, 22.0) | 6360 (5113–7911) |
| Assault | 0.6 | 0.6 (0.3–1.3) | 0.0 (−50.0, 116.7) | 370 | 482 (240–1010) | 30.3 (−35.1, 173.0) | 2197 (1204–4192) |
| Accidental drowning | 0.4 | 0.3 (0.1–1.3) | −25.0 (−75.0, 225.0) | 195 | 243 (72–854) | 24.6 (−63.1, 337.9) | 1148 (410–3361) |
| Other external causes | 2.1 | 2.1 (1.7–2.8) | 0.0 (−19.0, 33.3) | 1675 | 2541 (2021–3214) | 51.7 (20.7, 91.9) | 11,590 (9568–14,166) |
| Other causesd | 2.3 | 2.1 (1.4–3.3) | −8.7 (−39.1, 43.5) | 1485 | 2078 (1460–3052) | 39.9 (−1.7, 105.5) | 9503 (7004–13,239) |
| SIDS | 0.3 | 0.1 (0.0–0.2) | 80 | 22 (9–63) | −72.5 (−88.8, −21.3) | 223 (108–476) | |
| Other causes excluding SIDS | 2.0 | 2.0 (1.4–3.2) | 0.0 (−30.0, 60.0) | 1405 | 2056 (1451–2989) | 46.3 (3.3, 112.7) | 9280 (6896–12,763) |
UI: uncertainty interval. COPD: chronic obstructive pulmonary disease. SIDS: sudden infant death syndrome.
All rates are age-standardised to the Segi World standard population.
Overall percentage change in the age-standardised rate projected for 2040–2044 compared to the age-standardised rate observed in 2015–2019.
Overall percentage change in the numbers of deaths projected for 2040–2044 compared to the numbers of deaths in 2015–2019.
Other causes includes diseases of the eye and ear (H00–H95), all pregnancy, childbirth and the puerperium (O00–O99), and all diseases not elsewhere classified (R00-R99).
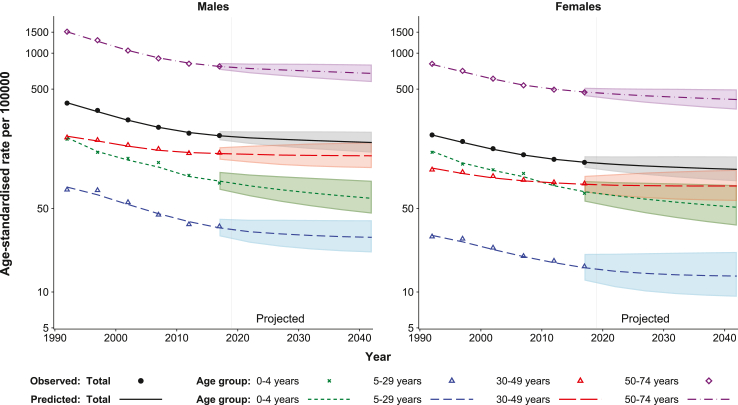
For both males and females, mortality rates are consistently lowest for those aged 5–29 years and are highest for those aged 50–74 years (Fig. 1). The mortality rates for all age groups are projected to continue to decline over the period 2020–2044, but these declines are expected to be at a slower pace than the trends in the previous 25 years from 1990–1994 to 2015–2019. In particular, the rates for those aged 5–29 and 30–49 years are projected to level off in the next 25-year period from 2015–2019 to 2040–2044 (Fig. 1).
Fig. 1.
Observed and projected age-standardised rates for premature mortality due to all causes 1990–2044, Australia. All rates are age-standardised to the Segi World standard population. The shaded area represents the 95% uncertainty interval.
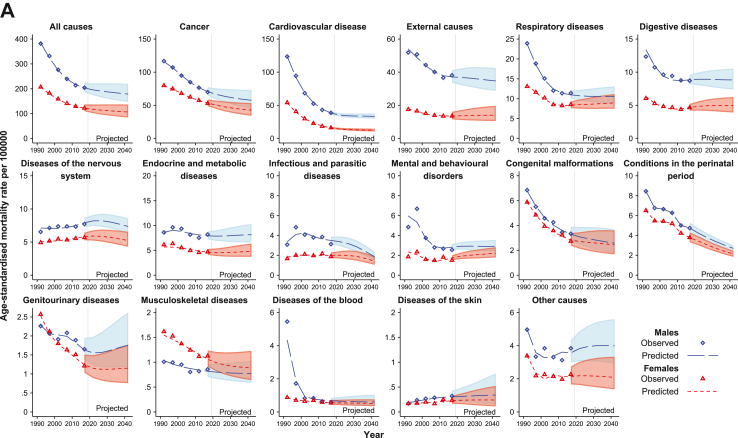
For both males and females, age-standardised premature mortality rates for most causes of death declined dramatically during 1990–2019 (Fig. 2 and Supplementary material Table S3), and from 2020 to 2044 are expected to continue to decrease at a slower pace or to remain stable (i.e. change by <0.5 per 100,000) (Fig. 2 and Table 1). The exceptions to this pattern are hypertensive disease and liver cancer for males, chronic obstructive pulmonary disease (COPD), mental and behavioural disorders for females, and suicide for both males and females, for which age-standardised rates are projected to increase by 0.5–1.2 per 100,000 over the projection period (Fig. 2 and Table 1).
Fig. 2.
Observed and projected age-standardised premature mortality rates for 1990–2044 for all causes combined and for different cause of death categories, Australia (ranked by the total numbers of deaths observed in 2015–2019) A. High-level causes of deaths B. Detailed cause of death categories. All rates are age-standardised to the Segi World standard population. The shaded area represents the 95% uncertainty interval. COPD: Chronic obstructive pulmonary disease. SIDS: sudden infant death syndrome. Other causes includes diseases of the eye and ear (H00–H95), all pregnancy, childbirth and the puerperium (O00–O99), and all diseases not elsewhere classified excluding sudden infant death syndrome (R00–R94, R96–R99).
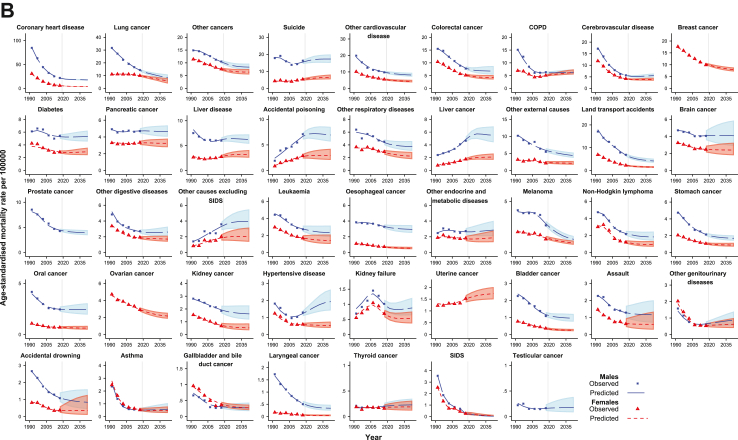
Projections of numbers of premature deaths
The total number of premature deaths is projected to increase by 22.8% (21.0% for males and 25.6% for females), from 272,815 deaths (168,950 males and 103,865 females) in 2015–2019 to 334,894 (204,447 males and 130,447 females) in 2040–2044 (Table 1). This is expected to result in a total of 1.58 million premature deaths over the period 2020–2044. Of the high-level causes of death, cancer is estimated to remain the most common cause of premature death for both males and females in 2040–2044, followed by cardiovascular disease (CVD) (Table 1 and Fig. 3A). Of the detailed NCD cause of death categories, for males coronary heart disease will remain the most common cause of premature death to 2044, followed by lung cancer and other cancers. For females, breast cancer is expected to replace lung cancer as the most common NCD cause of premature death in 2040–2044, followed by COPD and lung cancer (Fig. 3B).
Fig. 3.
Change in rank of causes of death based on the numbers of premature deaths over the period 1990–2044, Australia. A. High-level causes of death B. Detailed cause of death categories for noncommunicable diseases. COPD: Chronic obstructive pulmonary disease. SIDS: sudden infant death syndrome.
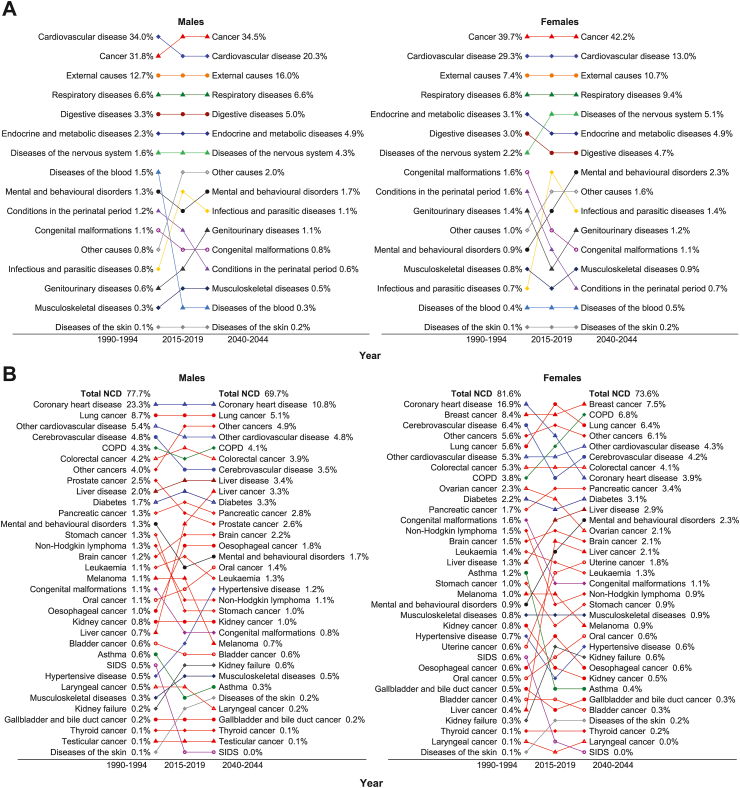
Projected PYLL due to premature deaths
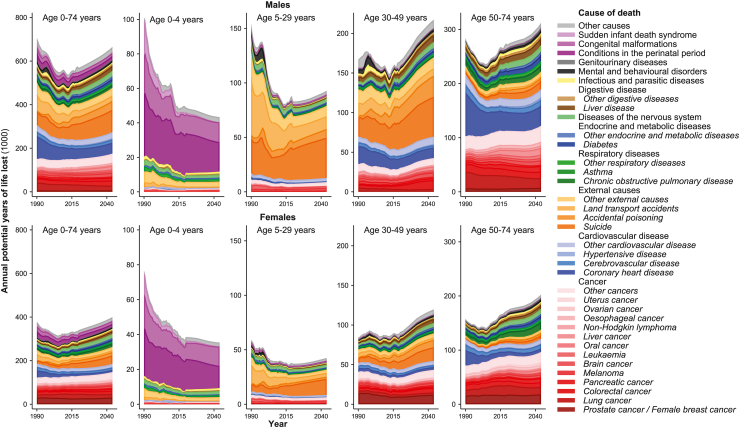
Over the 25-year period 2020–2044, annual PYLL are projected to increase for both males and females (Fig. 4), with premature mortality accounting for a total of 24.5 million PYLL (Supplementary material Table S6). For males, external causes (30.1%) and cancer (26.3%) are estimated to account for the largest proportions of PYLL due to premature mortality over the period 2020–2044. This order is reversed for females, with cancer (37.1%) expected to contribute the largest proportion of PYLL due to premature mortality, followed by external causes (18.6%) (Supplementary material Table S6). The proportional contribution of each cause of death to the PYLL due to premature mortality varied dramatically over time, as well as by sex and age group (Supplementary material Figure S7).
Fig. 4.
Estimated annual potential years of life lost due to premature death for different cause of death categories by sex and age group, 1990–2044, Australia. Other causes includes diseases of the eye and ear (H00–H95), all pregnancy, childbirth and the puerperium (O00–O99), and all diseases not elsewhere classified excluding sudden infant death syndrome (R00–R94, R96–R99).
Sensitivity analyses
For cause of death categories where APC models were used, we explored different values of the damping factor. Specifically, we applied an ‘intensive’ damping factor (0.82) which doubled the damping used in the main analyses, and a damping factor (0.99) which approximates to no damping (Supplementary material Figures S42 and S43). For cause of death categories with either increasing or decreasing trends during the last observed period, as expected, use of the ‘intensive’ damping factor resulted in projections that tended to level off. On the other hand, ‘no damping’ implies that the last observed trends will continue at the same magnitude, although this is unlikely to be the case. Nevertheless, the differences in overall results are minimal (Supplementary material Figure S42).
We also conducted a sensitivity analysis using age 70 years as the upper limit for premature death in Australia (Supplementary material Table S10). It is expected that approximately 70% of the projected number of premature deaths in 2040–2044 from the main analyses occur under the age of 70 years, although the patterns in the projected age-standardised mortality rates do not differ greatly (Supplementary material Figures S46 and S47).
Discussion
Our study provided population-level estimates and projections of the rate of premature mortality in Australia to 2044. The observed declines in the age-standardised premature mortality rates for both males and females are expected to continue over the projection period 2020–2044, although at a slower pace for all age groups and across most of the major causes of death. Of the high-level causes of death, cancer is projected to remain the most common cause of premature death in Australia to 2044, followed by CVD. In the younger age groups (5–49 years), deaths due to external causes associated with the occurrence of injury, poisoning, suicide, or violence are the largest contributors to mortality, although mortality rates for land transport accidents are expected to continue to decline to 2044. Despite the decreasing premature mortality rates, due to an ageing population and increasing population size, the overall number of premature deaths will continue to increase substantially to 2044. This is expected to result in a total of 1.58 million premature deaths over the projection period, with a total of 24.5 million PYLL.
Only a limited number of previous international studies have reported long-term (20+ years) statistical projections of cause-specific premature mortality rates, while one recent GBD study (Foreman et al., 2018) reported long-term statistical projections of all-cause mortality rates for Australia and 194 other countries and territories.3 The GBD projections for 2017–2040 reported for all causes combined and most cause of death categories for deaths under age 75 years are generally consistent with the results of our study. There are, however, some notable differences between the results from the two studies for some causes of death, including cancers of the breast, colorectum, lung, kidney, liver, and testis, and non-Hodgkin lymphoma, melanoma, and external causes (Supplementary material Figures S9 and S10). Projections from the GBD study generally overestimated the observed rate in 2015–2019 for several cancer types with decreasing trends (e.g. cancers of the breast, prostate, lung, colorectum, bladder, kidney and ovary and melanoma), and underestimated the true rate in 2015–2019 for some cause of death categories with increasing or stable trends (e.g. cancers of the liver and testis, and external causes). These differences are likely to be due to the different time periods for which observed data were available and the methods used in the two studies. In particular, projections reported by Foreman et al. for Australia were based on the observed data up to 2014 and estimates from statistical models for 2015–2016.15 The discrepancies between these estimated recent data and the observed data (e.g. in 2015–2016) likely contributed to the differences between their projected rates for 2017–2040 and the observed rates for 2017–2019, as well as differences to our projected rates for 2020 onwards (Supplementary material Figures S9 and S10). Based on the GBD estimates, the overall premature mortality rates for Australia were among the lowest in the high-income countries for both males and females in 2015. However, the GBD-projected decline over the 25-year period 2015–2040 was at a slower pace for Australia (18.2% for males and 20.5% for females) than for many other high-income countries (Supplementary material Figure S11). Bearing in mind the differences between our analysis and the GBD projections, the decline in premature mortality rates for Australia may be even slower (estimated as 14.3% for males and 15.1% for females in our study).
Our results show that age-standardised premature mortality rates for most causes of death, including cancer and CVD, are projected to decrease through to 2044, reflecting the success of past and current public health interventions, cancer control, and progress in CVD prevention.16 For cancer and CVD specifically, the declines are likely to be attributable to multiple factors including risk factor control, changes in diagnostic practices and cancer screening activities, and improvements in treatments.16,17 Cancer and CVD are known to share a number of risk factors such as tobacco smoking, obesity and overweight, diabetes, physical inactivity, and alcohol consumption.18 One of the most significant developments in the prevention of cancer and CVD in Australia was the implementation of tobacco control measures, which successfully reduced the prevalence of smoking, and subsequently reduced mortality rates for smoking-related cancers and CVD.2, 19 Decreases in the premature mortality rates for several cancer types are also likely to be driven by the implementation of organised national screening programs for cancers of the cervix, colorectum and breast,16,20 and improvements in cancer care and targeted treatment.2,19 For CVD, the decline in premature mortality is likely to be due to the implementation of a range of programs and initiatives supporting prevention and optimal detection, as well as advances in medical and surgical treatment.2
Australia is one of the 176 countries that adopted the Sustainable Development Goals (SDGs), which include a target to reduce premature mortality from NCDs by a third by 2030 (relative to 2015 levels).21 As the SDG target 3.4 is a relative measure and the baseline mortality rates in 2015 are very different across countries, it has been noted that several targets require a pace of progress that no country has achieved in recent years.22,23 Australia is one of the high-income countries with a relatively low probability of dying from NCDs, and our projections suggest that the probability of dying from NCDs will continue to decrease (Supplementary material Figure S12 and Figures S44 and S45) with coronary heart disease, lung cancer and breast cancer estimated to remain the top three causes of death for those aged 30–69 years in Australia. We acknowledge that the mortality reduction projected for NCDs is influenced by the damping factor used in the statistical models. However, in the extreme case with no damping, the numbers of premature deaths from cancer and CVD are still expected to account for 37.6% and 13.4% of the total premature deaths in Australia in 2040–2044, respectively (Supplementary material Table S9). In addition, our projections suggest increases in premature mortality rates for liver cancer and hypertensive diseases for males and COPD for females. Although cigarette smoking is the most well-studied COPD risk factor, it is not the only one, and there is consistent evidence from epidemiological studies that non-smokers may also develop chronic airflow limitation. COPD results from complex interactions between genes and the environment.24
These findings suggest that there are public health concerns which require continued or additional attention, especially as it is possible that the gains made from existing public health measures implemented in the past two decades will reduce over time. For example, there have been recent concerns regarding the adverse impact of electronic cigarettes on smoking initiation rates,25 and the promotion and availability of tobacco products on the internet.26 In addition, the influence of other disease risk factors, including obesity, alcohol use, red meat or processed meat consumption, and physical inactivity, also requires attention.17 In particular, the prevalence of obesity and overweight has increased in Australia, with over a quarter of children and adolescents overweight and obese in 2014–15.27 This trend may further increase the long-term health consequences and premature mortality from many health conditions in the future, such as CVD and some types of cancers.28 Moreover, socioeconomic inequalities in mortality remain substantial in Australia,29 so strengthening existing public health programs and implementing new programs where appropriate will be crucial to further reduce premature mortality in Australia.
Among the high-level causes of death, external causes are projected to remain the third most common cause for Australians aged under 75 years in 2044. There are opposing trends in the overall premature mortality rates for the detailed external cause of death categories, with a decrease over time for land transport accidents and assault, while an increase in mortality rates for suicide was projected and mortality rates for accidental poisoning were estimated to be relatively stable. Among Australians aged 5–49 years, external causes are projected to remain the leading cause of death, with half of these deaths being due to suicide. The pathways that lead to suicide are complex, with a wide range of social, psychological, and biological risk factors.30 The National Suicide Prevention Trial was implemented by the Australian Government in 2016 and continued monitoring of the impacts of this initiative is warranted.31 Land transport accidents were the second largest external cause of death for ages 5–29 years, followed by accidental poisoning. This order is reversed for ages 30–49 years, with accidental poisoning replacing land transport accidents as the second most common cause of death from external causes since 2015. The mortality rates due to land transport accidents for both males and females have decreased over the last three decades and are projected to continue to decline through to 2044, reflecting the positive impact of a range of interventions that have aimed to improve road safety in Australia.16 Accidental poisoning can result from unintentional contact with a substance that produces harm to a person, including accidental drug overdose.2 Although the mortality rates due to accidental poisoning for age 15–49 years are estimated to slightly decrease, mortality rates for age 50–74 years for both males and females are projected to continue to increase to 2044 (Supplementary material Figures S27 and S41), highlighting that more efficient interventions are needed to reduce poisoning events.
As with all modelled projections, this study has some limitations which should be considered when interpreting the results. The main limitation is that the projections are dependent on the assumptions made, and do not account for the possible effects of recently implemented or future interventions (e.g. new treatments), nor unforeseen events or health crises (e.g. the COVID-19 pandemic). However, these projections can serve as a projected “status quo” benchmark against which impacts of such future interventions or events could be evaluated. The projection models also assumed that the association between age and risk of death remained constant over time. For log-linear or APC models for causes of death other than lung cancer, the future cohort and future period effects are assumed to be the same as those for the most recent observed cohort and period,11 although we applied a damping factor to the drift when extrapolating into the future. This takes into account the fact that current trends are not expected to remain unchanged over time.14 Another study limitation is that the population denominators were projected by the ABS (with the population projections used here assuming medium growth),6 adding further uncertainty to our results. In addition, “premature” mortality in 2044 may more appropriately relate to an older age group because of rising life expectancy, rather than using the current average life expectancy of 75 years. This study was based on underlying cause of death coding; future work could explore data on multiple causes of death and the extent of contributions from different diseases as comorbidities. Despite these limitations this study also has many strengths. First, the long-term observed data used are known to be of high quality and have excellent population coverage.32 Second, the projection methods for lung cancer mortality take into account detailed data on cigarette tar consumption.9 Furthermore, the use of APC models to project rates for most of the cause of death categories can implicitly capture the effects of factors which contribute to mortality at a population level, including environmental and behavioural risk factors, disease prevention and treatment.12 The modelling approach used in this study might be applicable elsewhere.
It is important to acknowledge that because the projections reported in this study were based on observed data up to 2019, deaths from COVID-19 or any impact of the COVID-19 pandemic will not be captured or accounted for. During 2020–2021, Australian national and state governments introduced various rules and restrictions on public gatherings and physical distancing,33 and Australia has thus experienced lower numbers of deaths from COVID-19 than many other countries (a total of 13,718 COVID-19 deaths were registered from 1 January 2020 to 30 April 2023 in Australia, with 1643 deaths in people aged <70 years).34 Life expectancy at birth was estimated to increase by 0.7 years in the Australian population in 2020, likely due to reduced mortality from other infectious diseases during the lockdown period.35 However, excess mortality then increased in 2022, with the long-term mortality effects of COVID-19 and long COVID-19 yet unknown. Overall, there are still numerous direct and indirect consequences of the COVID-19 pandemic that may result in excess morbidity and premature death. During 2020–2021, as a result of the efforts to control the spread of the SARS-CoV-2 virus, there were a number of changes in how healthcare services were delivered during the pandemic, including the suspension of non-urgent elective surgery and a reduction in elective surgery capacity, which may contribute to rates of premature mortality in the future.10,33 Cancer screening programs in Australia were also affected, with BreastScreen Australia pausing in March and April 2020.36 It would also seem likely that population-level health service-seeking was impacted, meaning that diagnosis and treatment may have been delayed or missed.33 Nevertheless, recent data do not indicate an increase in cancer mortality at the population level.37 Moreover, there are concerns that the pandemic is likely to have had a significant impact on the mental health of the population with increased anxiety and increased rates of suicide.38 However, international data show that suicide rates did not change substantially across countries or areas-within-countries during the pandemic.39 In addition, the pandemic may have led to an increase in the prevalence of behavioural risk factors like tobacco smoking, alcohol consumption,40 physical inactivity, overweight and obesity. All these consequences may result in excess premature deaths regardless of SARS-CoV-2 infection, and estimating the impact of the pandemic on premature mortality will be the subject of future research.
While this study focused on premature mortality before age 75 years to examine the causes of death in younger age groups, it should be stressed that the disease burden experienced by the older population is substantial in Australia. For example, results from this and a previous study suggest that premature cancer deaths are projected to account for 42% of all cancer deaths over 2020–2044 and thus 58% of cancer deaths are expected to occur in people aged 75 years and above.10 It is therefore important to also consider the challenges the healthcare system faces in meeting the health care needs of older Australians.
This study provides long-term projections of premature mortality rates for all causes in Australia to 2044. This work will assist in prioritisation for public health and health services efforts, and can serve as benchmarks against which to measure the impact of future interventions. Our projections suggest that overall premature mortality rates will continue to decrease in Australia to 2044, although cancer is still expected to remain the leading cause of premature mortality in Australia in 2044. It is important that there is a focus on policy implementation that accelerates the prevention, early detection, and treatment of cancer and other key health conditions so that premature mortality can be further reduced in the future.
Contributors
KC conceived the study. QL designed the study, conducted statistical analyses, interpreted results and drafted the manuscript. JS, DO’C and KC contributed to the methods. CK, JS, MC, PBG, AP, RI, EB, DO’C and KC contributed to drafting the manuscript. QL and DO’C verified the data. All authors contributed to the interpretation of the results, critically revised the manuscript, and read and approved the final manuscript.
Data sharing statement
The tabulated mortality data that support the findings of this study are available at https://www.aihw.gov.au/. Access restrictions apply to the National Drug Strategy Household Surveys data on smoking behaviour. Approved release of these data can be obtained through an application to the Australian Institute of Health and Welfare.
Ethics approval and consent to participate
This population-based study used existing, routinely collected data for mortality and smoking intensity released by the Australian Institute of Health and Welfare. Ethics approval was not required to use these aggregated data.
Declaration of interests
KC's research is funded by the National Health and Medical Research Council (NHMRC) of Australia (Fellowship APP1194679, Centre of Research Excellence in Cervical Cancer Control 1135172). KC is co-PI and MC is an investigator of an investigator-initiated trial of cervical screening, Compass, run by the Australian Centre for Prevention of Cervical Cancer (ACPCC), which is a government-funded not-for-profit charity; the ACPCC has received equipment and a funding contribution from Roche Molecular Diagnostics, and operational support from the Australian Government. KC is also co-PI on a major investigator-initiated implementation program Elimination of Cervical Cancer in the Western Pacific (ECCWP) which will receive support from the Minderoo Foundation, the Frazer Family Foundation and equipment donations from Cepheid Inc. Neither KC and MC nor their institution on their behalf receives direct or indirect funding from industry for any project. No other conflicts of interest are declared.
The remaining authors declare that they have no conflicts of interest.
Acknowledgements
We would like to acknowledge the Australian Institute of Health and Welfare that provided the national tabulated data for all-cause mortality, the data from the National Drug Strategy Household Surveys (NDSHS), and the Australian Data Archive for providing access to the NDSHS data. However, the Institute bears no responsibility for the analyses presented within this publication or the interpretation of them.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100987.
Contributor Information
Qingwei Luo, Email: qingweiluo@sydney.edu.au.
Julia Steinberg, Email: julia.steinberg@nswcc.org.au.
Clare Kahn, Email: clarek@nswcc.org.au.
Michael Caruana, Email: michael.caruana@nswcc.org.au.
Paul B. Grogan, Email: Paul.Grogan@nswcc.org.au.
Andrew Page, Email: A.Page@westernsydney.edu.au.
Rebecca Ivers, Email: rebecca.ivers@unsw.edu.au.
Emily Banks, Email: emily.banks@anu.edu.au.
Dianne L. O'Connell, Email: dianneoconnell525@gmail.com.
Karen Canfell, Email: karen.canfell@nswcc.org.au.
Appendix A. Supplementary data
References
- 1.Australian Institute of Health and Welfare (AIHW) 2021. General record of incidence and mortality (GRIM) books.https://www.aihw.gov.au/reports/life-expectancy-death/grim-books/contents/grim-books Available from: [Google Scholar]
- 2.Australian Institute of Health and Welfare (AIHW) 2015. Premature mortality in Australia 1997–2012.https://www.aihw.gov.au/reports/life-expectancy-death/premature-mortality-in-australia-1997-2012/contents/summary Available from: [Google Scholar]
- 3.Foreman K.J., Marquez N., Dolgert A., et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet. 2018;392(10159):2052–2090. doi: 10.1016/S0140-6736(18)31694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva: 2021. ICD-10: international statistical classification of diseases and related health problems: tenth revision. [Google Scholar]
- 5.World Health Organization . World Health Organization; Geneva: 2020. WHO methods and data sources for country-level causes of death 2000-2019. [Google Scholar]
- 6.Australian Bureau of Statistics (ABS) Population projections, Australia, 2017 (base) to 2066. cat. no. 3222.0 2021. https://www.abs.gov.au/statistics/people/population/population-projections-australia/latest-release Available from:
- 7.Forey B., Hamling J., Hamling J., et al. P N Lee Statistics & Computing Ltd; 2016. International smoking statistics web edition.http://www.pnlee.co.uk/ISS.htm Available from: [Google Scholar]
- 8.Australian Institute of Health and Welfare (AIHW) 2020. Our data collections: National Drug Strategy Household Survey.https://www.aihw.gov.au/about-our-data/our-data-collections/national-drug-strategy-household-survey Available from: [Google Scholar]
- 9.Luo Q., Yu X.Q., Wade S., et al. Lung cancer mortality in Australia: projected outcomes to 2040. Lung Cancer. 2018;125:68–76. doi: 10.1016/j.lungcan.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Luo Q., O'Connell D.L., Yu X.Q., et al. Cancer incidence and mortality in Australia from 2020 to 2044 and an exploratory analysis of the potential effect of treatment delays during the COVID-19 pandemic: a statistical modelling study. Lancet Public Health. 2022;7(6):e537–e548. doi: 10.1016/S2468-2667(22)00090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sasieni P. Age-period-cohort models in Stata. Stata J. 2012;12(1):15. [Google Scholar]
- 12.Smith T.R., Wakefield J. A review and comparison of age-period-cohort models for cancer incidence. Stat Sci. 2016;31(4):591–610. [Google Scholar]
- 13.Moller B., Fekjaer H., Hakulinen T., et al. Prediction of cancer incidence in the Nordic countries: empirical comparison of different approaches. Stat Med. 2003;22(17):2751–2766. doi: 10.1002/sim.1481. [DOI] [PubMed] [Google Scholar]
- 14.Moller B., Fekjaer H., Hakulinen T., et al. Prediction of cancer incidence in the Nordic countries up to the year 2020. Eur J Cancer Prev. 2002;11(Suppl 1):S1–S96. [PubMed] [Google Scholar]
- 15.GBD Causes of Death Collaborators Global regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.PHAA Monograph Series No. 2. Public Health Association of Australia; Canberra: 2018. Top 10 public health successes over the last 20 years. [Google Scholar]
- 17.Australian Institute of Health and Welfare (AIHW) Australia’s health 2018. AIHW; Canberra: 2018. [Google Scholar]
- 18.Koene R.J., Prizment A.E., Blaes A., et al. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133(11):1104–1114. doi: 10.1161/CIRCULATIONAHA.115.020406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luo Q., Steinberg J., O’Connell D.L., et al. Changes in cancer incidence and mortality in Australia over the period 1996–2015. BMC Res Notes. 2020;13(1):561. doi: 10.1186/s13104-020-05395-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lew J.B., St John D.J.B., Xu X.M., et al. Long-term evaluation of benefits, harms, and cost-effectiveness of the National Bowel Cancer Screening Program in Australia: a modelling study. Lancet Public Health. 2017;2(7):e331–e340. doi: 10.1016/S2468-2667(17)30105-6. [DOI] [PubMed] [Google Scholar]
- 21.Bennett J.E., Kontis V., Mathers C.D., et al. NCD countdown 2030: pathways to achieving sustainable development goal target 3.4. Lancet. 2020;396(10255):918–934. doi: 10.1016/S0140-6736(20)31761-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lozano R., Fullman N., Abate D., et al. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):2091–2138. doi: 10.1016/S0140-6736(18)32281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wijnen A., Bishop K., Joshy G., et al. Observed and predicted premature mortality in Australia due to non-communicable diseases: a population-based study examining progress towards the WHO 25X25 goal. BMC Med. 2022;20(1):57. doi: 10.1186/s12916-022-02253-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Australian Institute of Health and Welfare (AIHW) AIHW; Canberra: 2023. COPD.https://www.aihw.gov.au/reports/chronic-respiratory-conditions/copd Available from: [Google Scholar]
- 25.Luo Q., Steinberg J., O'Connell D.L., et al. Lung cancer mortality in Australia in the twenty-first century: how many lives can be saved with effective tobacco control? Lung Cancer. 2019;130:208–215. doi: 10.1016/j.lungcan.2019.02.028. [DOI] [PubMed] [Google Scholar]
- 26.Soneji S., Pierce J.P., Choi K., et al. Engagement with online tobacco marketing and associations with tobacco product use among U.S. Youth. J Adolesc Health. 2017;61(1):61–69. doi: 10.1016/j.jadohealth.2017.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Australian Institute of Health and Welfare (AIHW) AIHW; Canberra: 2017. A picture of overweight and obesity in Australia. [Google Scholar]
- 28.Feletto E., Kohar A., Mizrahi D., et al. An ecological study of obesity-related cancer incidence trends in Australia from 1983 to 2017. Lancet Reg Health West Pac. 2022;29 doi: 10.1016/j.lanwpc.2022.100575. 100575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Welsh J., Joshy G., Moran L., et al. Education-related inequalities in cause-specific mortality: first estimates for Australia using individual-level linked census and mortality data. Int J Epidemiol. 2022;50(6):1981–1994. doi: 10.1093/ije/dyab080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fleischmann A., Bertolote J.M. Suicidal behavior in a global public health perspective. Int J Ment Health. 2003;32(1):67–78. [Google Scholar]
- 31.Page A., Pirkis J., Bandara P., et al. Early impacts of the ‘National Suicide Prevention Trial’ on trends in suicide and hospital admissions for self-harm in Australia. Aust N Z J Psychiatry. 2023;57(10):1384–1393. doi: 10.1177/00048674231166330. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization . 2021. WHO mortality database. [Google Scholar]
- 33.Bureau of Health Information (BHI) Healthcare quarterly, COVID-19 supplement – emergency department, ambulance, admitted patients and elective surgery, January to September 2020. BHI; Sydney (NSW): 2020. [Google Scholar]
- 34.Australian Bureau of Statistics (ABS) COVID-19 mortality in Australia: deaths registered until 30 April 2023. ABS; Canberra: 2023. https://www.abs.gov.au/articles/covid-19-mortality-australia-deaths-registered-until-30-april-2023 Available from: [Google Scholar]
- 35.Canudas-Romo V., Houle B., Adair T. Quantifying impacts of the COVID-19 pandemic on Australian life expectancy. Int J Epidemiol. 2022;51(5):1692–1695. doi: 10.1093/ije/dyab273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feletto E., Grogan P., Nickson C., et al. How has COVID-19 impacted cancer screening? Adaptation of services and the future outlook in Australia. Public Health Res Pract. 2020;30(4) doi: 10.17061/phrp3042026. [DOI] [PubMed] [Google Scholar]
- 37.Canfell K., Chiam K., Nickson C., et al. The complex impact of COVID-19 on cancer outcomes in Australia. Med J Aust. 2023;219(9):402–404. doi: 10.5694/mja2.52125. [DOI] [PubMed] [Google Scholar]
- 38.John A., Pirkis J., Gunnell D., et al. Trends in suicide during the covid-19 pandemic. BMJ. 2020;371 doi: 10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]
- 39.Pirkis J., Gunnell D., Shin S., et al. Suicide numbers during the first 9-15 months of the COVID-19 pandemic compared with pre-existing trends: an interrupted time series analysis in 33 countries. eClinicalMedicine. 2022;51 doi: 10.1016/j.eclinm.2022.101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Australian Institute of Health and Welfare (AIHW) AIHW; Canberra: 2020. Alcohol, tobacco & other drugs in Australia.https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/drug-types/alcohol Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.