Summary
The Western Pacific region is a diverse region experiencing fast economic growth and nutrition transition. We systematically examined 94 cohort studies on the associations of dietary and other lifestyle factors on non-communicable diseases (NCDs) in the region. These studies were mainly from China, Japan, the Republic of Korea, and Singapore. Patterns and changes in lifestyle risk factors for NCDs based on national surveys were examined. They showed some dietary intake improvements over the past three decades, featured as increased consumption of unsaturated oils, fruits, and vegetables, and decreased consumption of sodium and unhealthy fat. Despite a decrease in smoking rate and salt intake, the values remained higher than the global levels in 2019. The ultra-processed food intake in the region increased at a higher rate than the global estimate. National guidelines relevant to NCDs in five selected countries were highlighted. Strong future actions and policies are needed to tackle NCDs.
Keywords: Dietary intake, Lifestyle factors, Non-communicable diseases, Western Pacific region, Policy implications
Key message.
-
•
A systematic review of 94 cohort studies from the Western Pacific region indicated that dietary intakes (n = 52) and other lifestyle factors (n = 42) had a profound influence on risks of non-communicable diseases (NCDs).
-
•
In contrast to the consistent association between other lifestyle factors and NCDs, the associations between various measures of dietary intake and NCD outcomes appear to vary across countries.
-
•
Improvements in dietary intakes were observed in the Western Pacific region over the past three decades, featured as increased consumption of unsaturated oils, fruits, and vegetables and decreased consumption of sodium and unhealthy fat.
-
•
The Western Pacific region had lower intakes of sugar-sweetened beverages and processed meat than the global average, but the average annual percentage of change was higher. This increase was largely driven by some middle-income countries (e.g., China and Vietnam).
-
•
Most countries in the Western Pacific region have released national dietary guidelines, and most of their specific guidelines for food groups and nutrients are similar. However, most countries have not yet implemented cost-effective policies to improve the food environment.
-
•
Countries in the Western Pacific region need to set up strong national policies and programs to achieve the NCD global targets.
Introduction
Over a quarter of the world’s population lives in the World Health Organization (WHO) Western Pacific region, which includes 37 countries and regions with diverse geography, ethnicity, language, culture, and socioeconomic development levels. The region has been undergoing rapid shifts, such as economic development, population aging, lifestyle changes, disease burden, and technological innovation.1 Non-communicable diseases (NCDs) in this region have been rising, especially obesity, diabetes mellitus (DM), cancers, and cardiovascular diseases (CVDs). The most important and modifiable NCD risk factors are unhealthy diets, smoking, alcohol consumption, and physical inactivity. Over the past 30 years, lifestyle factors have significantly shaped health outcomes in the Western Pacific region. According to the Global Burden of Diseases (GBD) studies, lifestyle factors, including tobacco use, unhealthy diet, and alcohol consumption ranked in the top 10 risks in both 1990 and 2019. Although the ranking did not change significantly, the relative rates associated with each lifestyle factor did increase substantially.2 The burden of these factors is likely to continue to increase globally, including in the Western Pacific region.
With the fastest growing economies among countries, the dietary characteristics, food systems, and environments in the Western Pacific region are attracting international attention compared to other WHO regions. This is partly due to the region’s diverse cultures, religions, and political systems. Diets in the Western Pacific region often include high levels of salt and seafood, which are influenced by traditional cooking styles and geographical location of the countries.3 Furthermore, specific consumption patterns vary greatly across countries compared with those in other regions.4 The 2015 China Adult Chronic Disease and Nutrition Surveillance showed decreased consumption of grains in general but increased consumption of refined grains in China since 1982.5 Additionally, the nutrition-related environments in the Western Pacific region remain complex with various income levels ranging from lower middle-income countries (MICs), upper MICs, to high-income countries (HICs). Certain areas in lower MICs have less established food systems with predominantly traditional small farmer economies, farmers' markets, and wet markets, while in HICs with industrialized food systems. However, research on Western Pacific region is sparse. Few studies have examined trends in dietary intake and other lifestyle factors and their associations with NCDs in the region.
Although countries may have guidelines and policies regarding NCD prevention and control, it is unclear to what extent these guidelines and policies are consistent with international guidelines and recommendations on dietary and lifestyle factors. In addition, the implementation of the policies varies across countries, along with marked variations in their residents’ socioeconomic status, dietary patterns, and lifestyles.6
The WHO regional office issued a Regional Action Framework for the Prevention and Control of NCDs in the Western Pacific region, which presents the region’s vision, principal objectives, and recommended actions.1 Long-term progress on NCD prevention and control aims at a whole-systems change that addresses the underlying causes of NCDs and takes a lifelong approach to address social inequalities while creating a health-enhancing environment. However, the characteristics of Western Pacific region centered on nutrition and other lifestyle factors were not identified, and future strategies were not presented.
This study aimed to 1) examine the associations of dietary and other lifestyle factors on NCDs in the Western Pacific region; 2) describe patterns and trends in dietary intakes and other lifestyle factors over the past three decades in the Western Pacific region; 3) compare national guidelines for NCD prevention and control in selected countries and compare them with those issued by the WHO; and 4) provide recommendations for future actions.
Methods
Associations of dietary factors and other lifestyle factors on NCDs
We conducted a systematic review to evaluate the associations of nutrition and lifestyle factors on NCDs in adults aged 19 years or older in the Western Pacific region. PubMed/MEDLINE and Embase were searched for studies published from January 1, 2000 to October 31, 2022, using the following terms in various combinations: “NCD”, “NCDs”, “non-communicable disease”, “non-communicable diseases”, “CVD”, “CVDs”, “cardiovascular diseases”, “DM”, “diabetes”, “cancer”, “cancers”, “tumor”, “tumors”, “neoplasm”, “neoplasms”, “pulmonary disease”, “respiratory disease”, “COPD”, “chronic obstructive”, “chronic obstructive pulmonary disease”, “obesity”, “overweight”, “BMI”, “Western Pacific region”, “Western Pacific region” or 37 countries, “dietary factors”, “epidemiology”, and “cohort studies”.
The search was performed by selecting relevant terms for representative diseases and factors. We also manually searched the references of all included articles for relevant studies. The abstracts and titles, identified from the search, were screened by two review investigators to identify potentially relevant papers and their full text. Only studies with full text in English were included, and the full text was independently assessed using the inclusion criteria. These studies were included if they meet one or more of the following criteria: 1) a single food, food group, dietary pattern or nutrients that affect the incidence of diseases; 2) studies with a sample size of more than 1000; and 3) studies not conducted on patients. Any disagreements were discussed with a third reviewer until reached a consensus.
Studies on the associations of the other lifestyle factors of “smoking”, “alcohol”, “physical activity” or “insufficient activity” on NCDs were searched using a similar approach as for dietary factors (Supplementary Table S1). We used forest plots to present hazard ratios for the associations between dietary intakes in the top quartile (Q4) or quintile (Q5) and NCDs.
For quality control, one reviewer conducted data extraction, and the other reviewer independently checked for accuracy. In addition, two investigators assessed the quality of included research with the Newcastle-Ottawa Scale (NOS) to assess the quality of the studies. After evaluating its three aspects (selection, comparability, and outcome), each study could be assigned nine stars at most. The quality of studies was ranked as low quality (below 3 stars), moderate quality (4–6 stars), and high quality (7–9 stars).
Analysis of the Global Burden of Diseases (GBD) data for 1990–2019
The age-standardized leading risk ranking and its change between 1990 and 2019 based on DALYs per 100,000 population from NCDs were obtained from the GBD compare tool.
To identify secular trends of dietary intakes and other lifestyle factors in the region, the data of dietary risk factors exposure and summary exposure values (SEV) for smoking, drinking, and physical activity were used to examine the changes in age-standardized dietary and nutrition among adults from the GBD results tool 1990–2019. Then, the average annual percentage of change and 95% uncertainty interval (UI) from 1990 to 2019 were calculated by regressing a log-linear function of age-standardized DALYs per 100,000 population a year. We configured the model to detect a maximum of five join points and avoid segments comprising only two data points.
National guidelines related to NCDs in selected countries
To compare national information on dietary factors and other lifestyle factors (i.e., smoking, alcohol use, and physical activity) across countries, we searched and reviewed recent national guidelines and reports from selected countries (i.e., China, Republic of Korea, Japan, Australia, and Viet Nam).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Associations of dietary and other lifestyle factors on NCDs risks in the Western Pacific region
We conducted a systematic review of 94 cohort studies to investigate the associations of dietary intakes (n = 52) and other lifestyle factors (n = 42) on NCDs in the Western Pacific region (Table 1, Fig. 1 and Supplementary Table S2). Our main findings include: 1) dietary intakes had profound influences on NCDs, although the associations between various measures of dietary intakes and NCD outcomes across countries varied considerably; 2) a healthier lifestyle, evaluated by assessing other lifestyle factors like physical activity, smoking, and alcohol drinking, was associated with decreased risks of several NCDs; 3) there were very few studies on the associations of dietary intakes and lifestyle factors on the risks of respiratory diseases in the Western Pacific region, and future studies are warranted; and 4) most cohort studies were conducted in four countries, namely China, Japan, the Republic of Korea, and Singapore. In accordance with the NOS quality assessment scale for cohort studies, the quality scores were similar for studies on dietary intake or other lifestyle factors with NCDs (≥85% cohorts, ≥7 stars). Overall, they indicate high quality (Supplementary Tables S3 and S4).
Table 1.
Findings from 42 studies on the associations between other lifestyle factors and cardiovascular diseases (n = 5), diabetes mellitus (n = 4), cancers (n = 32) and respiratory diseases (n = 1) in the Western Pacific regiona.
| No. | Reference | Study setting | Participant characteristics Sample size; gender (men/women); age |
Factors (exposure) | HR or RR (95% CI) | Effect on risk |
|---|---|---|---|---|---|---|
| 1. Cardiovascular diseases (n = 5) | ||||||
| 1) | Jin et al., 2019 | Republic of Korea | n = 501,690; 50%/50%; 47.6 ± 14.3 years | Physical activity level (MET-minutes/week) 500–1000 MET-minutes/week (Ref. 0 MET-minutes/week) |
Atrial fibrillation HR = 0.88 (0.80–0.97) |
Decrease |
| 2) | Bennett et al., 2017 | China | n = 487,334; 51%/59%; 51 years | Physical activity (MET-h/day)b Q5 (Ref. Q1) |
HR = 0.77 (0.74–0.80) | Decrease |
| 3) | Lin et al., 2021 | China | n = 76,176; 40.7%/59.3%; 51.2 ± 11.8 years | Types of transport to get to and from work
|
HR = 0.71 (0.62–0.82) | Decrease |
| 4) | Fan et al., 2019 | China | n = 104,170; 48%/52%; 52.6 years | Types of transport to get to and from work
|
Ischemic heart disease
|
Decrease |
| 5) | Woodward et al., 2005 | Asia Australia, New Zealand | n = 562,338; 65%/35%; 46.5 years | Smoking Current smokers (Ref. Non-smokers) |
HR = 1.42 (1.36–1.48) | Increase |
| 2. Diabetes mellitus (n = 4) | ||||||
| 1) | Wakasugi et al., 2022 | Japan | n = 31,039; Not reported; Not reported | Healthy lifestyle scores (HLSs)d 5 score (Ref. 0–2 score) |
HR = 0.51 (0.32–0.81) | Decrease |
| 2) | Lv et al., 2017 | China | n = 461,211; 41%/59%; 30–79 years | Low-risk lifestyle factorsc
|
|
Decrease |
| 3) | Park et al., 2021 | Republic of Korea | n = 5,198,792; 46%/54%; ≥20 years | Smoking
|
|
Increase |
| 4) | Sairenchi et al., 2004 | Japan | n = 128,141; 31%/69%; 40–79 years | Smoking
|
|
Increase |
| 3. Cancer (n = 32) | ||||||
| 1) | Bui et al., 2022 | Republic of Korea | n = 15,175; 42.2%/57.8%; 51.5 ± 8.9 years | Physical activity (MET minutes/week) High, ≥2430 (Ref. Low, <693) |
Thyroid cancer HR = 0.65 (0.44–0.94) |
Decrease |
| 2) | Pang et al., 2021 | China | n = 460,937; Not reported; 52.0 ± 10.5 years | Physical activity (MET-h/day) ≥33.2 (Ref. <8.7) |
Liver cancer HR = 0.81 (0.71–0.93) Gallbladder cancer HR = 0.51 (0.32–0.80) Biliary tract cancer HR = 0.55 (0.38–0.78) |
Decrease |
| 3) | Ko et al., 2020 | Republic of Korea | n = 5,874,668; –/100%; 46.8 ± 14.5 years |
|
Lung cancer
|
|
| 4) | Kim et al., 2019 | Republic of Korea | n = 257,854; 50.5%/49.5%; 50.7 years | Physical activity Exercise 3–4 or 5–6 times/week (Ref. No exercise) |
Stomach cancer HR = 0.87 (0.79–0.96) Lung cancer HR = 0.80 (0.71–0.91) Liver cancer HR = 0.85 (0.75–0.98) |
Decrease |
| 5) | Eaglehouse et al., 2017 | Singapore | n = 63,257; 44.5%/55.5%; 56.4 ± 8.0 years | Physical activity Strenuous-Vigorous (Intensity ≥1/2 h/week) (Ref. None) |
Colorectal cancer HR = 0.85 (0.74–0.99) |
Decrease |
| 6) | Suzuki et al., 2008 | Japan | n = 30,157; –/100%; 40–69 years | Physical activity Walked for ≥1 h/day and exercised for ≥1 h/week (Ref. Walked for <1 h/day and exercised for <1 h/week) |
Breast cancer HR = 0.45 (0.25–0.78) |
Decrease |
| 7) | Lee et al., 2007 | Japan | n = 65,022; 46%/54%; 40–69 years | MET (hours/day) Highest (Ref. Lowest) |
Total colorectal cancer RR = 0.69 (0.49–0.97) |
Decrease |
| 8) | Lee et al., 2022 | Republic of Korea | n = 128,218; 33%/67%; 40–69 years |
|
Gastric cancer
|
Increase |
| 9) | Im et al., 2021 | China | n = 510,137; 41%/59%; 52.0 ± 10.7 years | Alcohol drinking status Current regular drinkers (Ref. Abstainers) |
Mouth and throat cancer HR = 1.73 (1.51–1.99) (Only men) Esophagus cancer HR = 1.80 (1.66–1.96) (Only men) Gallbladder and biliary tract cancer HR = 1.33 (1.09–1.62) (Only men) |
Increase |
| 10) | Im et al., 2021 | China | n = 492,643; 41%/59%; 52.0 ± 10.7 years | Alcohol drinking status Current regular drinkers per 280 g/week (Ref. Abstainers) |
Liver cancer HR = 1.44 (1.23–1.69) (Only men) |
Increase |
| 11) | Iwase et al., 2021 | Japan | n = 158,164; –/100%; 40–104 years |
|
Breast cancer
|
Increase |
| 12) | Makiuchi et al., 2019 | Japan | n = 103,143; 46.9%/53.1%; 40–69 years |
|
Intrahepatic bile duct cancer
|
Increase |
| 13) | Yang et al., 2019 | South Korea | n = 4578; Not reported; Not reported | Alcohol consumption More than 30 g/day in men and 20 g/day in women (Ref. Without significant alcohol consumption) |
Colorectal neoplasm HR = 1.86 (1.28–2.70) | Increase |
| 14) | Lu et al., 2018 | Japan | n = 95,525; 47%/53%; Not reported |
(Ref. Never/None) |
Oral cavity cancer
|
Increase |
| 15) | Wang et al., 2017 | China | n = 63,527; Not reported; Not reported |
|
Gastric adenocarcinoma
|
Increase |
| 16) | Sawada et al., 2014 | Japan | n = 48,218; 100%/–; Not reported | Alcohol consumption 150–300 g/week (Ref. Non-drinkers) |
Advanced prostate cancer HR = 1.51 (1.04–2.19) |
Increase |
| 17) | Shimazu et al., 2012 | Japan | n = 174,719; 51.4%/48.6%; 40–79 years |
|
Liver cancer
|
Increase |
| 18) | Koh et al., 2011 | Singapore | n = 61,321; Not reported; Not reported |
|
Hepatocellular carcinoma
|
Increase |
| 19) | Moy et al., 2010 | China | n = 18,244; 100%/–; 45–64 years |
|
Gastric cancer
|
Increase |
| 20) | Tsong et al., 2007 | Singapore | n = 63,257; Not reported; 45–74 years |
|
Colon cancer
|
Increase |
| 21) | Otani et al., 2003 | Japan | n = 90,004; 47%/53%; 40–69 years |
|
Colorectal cancer
|
Increase |
| 22) | Luu et al., 2022 | China | n = 61,321; 45%/55%; 45–74 years | Smoking status and BMI
|
Pancreatic cancer
|
Increase |
| 23) | Park et al., 2020 | Republic of Korea | n = 6,569,144; Not reported; 55.4 years/54.8 years | Smoking
|
Lung cancer
|
Increase |
| 24) | Saito et al., 2017 | Japan | n = 321,501; 48%/52%; ≥35 years | Smoking cessation 16–20 years (Ref. Never) |
Total cancer HR = 1.21 (1.05–1.38) (Only men) |
Increase |
| 25) | Chen et al., 2015 | China | n = 512,891; 41%/59%; 30–79 years | Smoking
|
All cancer
|
Increase |
| 26) | Wong et al., 2010 | Singapore | n = 45,900; 40.7%/59.3%; 55.5 years | Smoking Never smokers (Ref. Current smokers) |
Lung cancer HR = 0.14 (0.11–0.18) |
Increase |
| 27) | Luo et al., 2007 | Japan | n = 99,670; 47.7%/52.3%; 30–79 years | Smoking Current (Ref. Never) |
Pancreatic cancer HR = 1.8 (1.1–3.0) (Only men) |
Increase |
| 28) | Niwa et al., 2005 | Japan | n = 34,639; –/100%; 58.3 years | Smoking
|
Ovarian cancer
|
Increase |
| 29) | Inoue et al., 2004 | Japan | n = 92,792; 48%/52%; 52.9 ± 7.9 years/53.3 ± 8.0 years | Smoking
|
Total cancer
|
Increase |
| 30) | Jee et al., 2004 | Republic of Korea | n = 1,212,906; 68%/32%; 45.0 ± 10.9 years/48.6 ± 12.4 years | Smoking
|
(Only men) Esophagus cancer
|
Increase |
| 31) | Koizumi et al., 2004 | Japan | n = 29,392; 100%/–; Not reported | Smoking
|
Gastric cancer
|
Increase |
| 32) | Mizoue et al., 2000 | Japan | n = 4050; 100%/–; Not reported | Smoking
|
|
Increase |
| 4. Respiratory diseases (n = 1) | ||||||
| 1) | Leem et al., 2018 | Republic of Korea | n = 6517; 46.0%/54.0%; Not reported | Smoking history ≥20 pack-years (Ref. = Never) |
COPD RR = 2.54 (2.09–3.08) |
Increase |
MET, metabolic equivalent of task; HR, hazard ratio; HLS, healthy lifestyle scores; RR, relative risk; CI, confidence interval.
Please see the tables with references in the Supplemental Files. Exposure factors show the associations between dietary intakes in the top quartile (Q4) or quintile (Q5) and NCDs.
Total physical activity was calculated as MET hours per day (MET-h/day) by multiplying the MET of each activity (occupational tasks, commuting, household tasks, and leisure time activities) by the frequency and duration of physical activity.
Low-risk lifestyle factors included: drinking greater than zero but less than 30 g of alcohol per day; engaging in a sex-specific upper quarter of the physical activity level. Each factor was bisected and analyzed.
The HLS was calculated as the sum of the score from each component (smoking, body mass index, regular exercise, eating habits, alcohol intake) and ranged from 0 (least healthy) to 5 (healthiest).
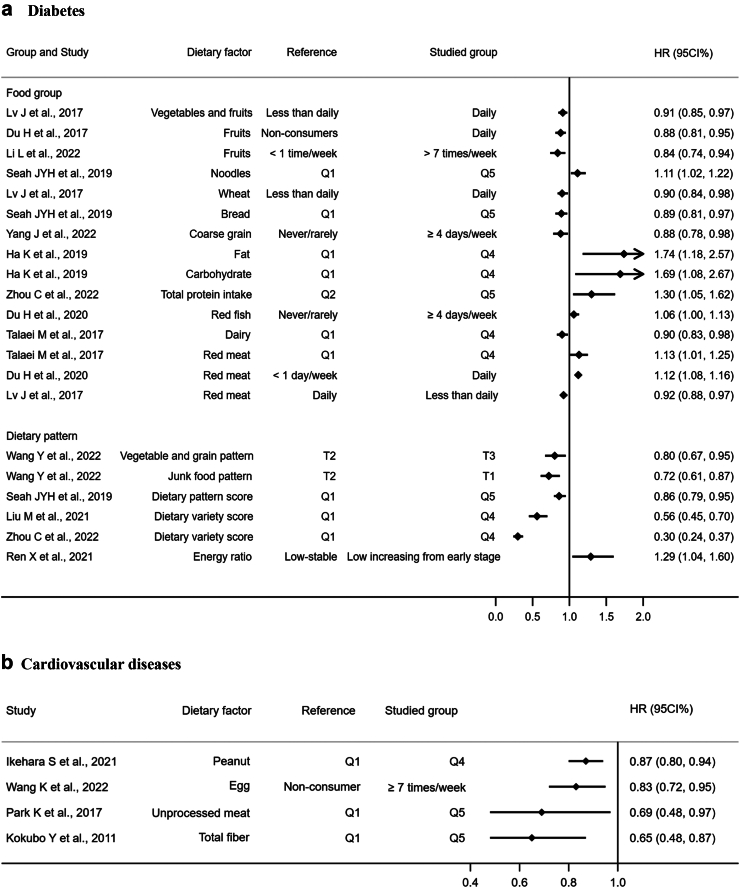
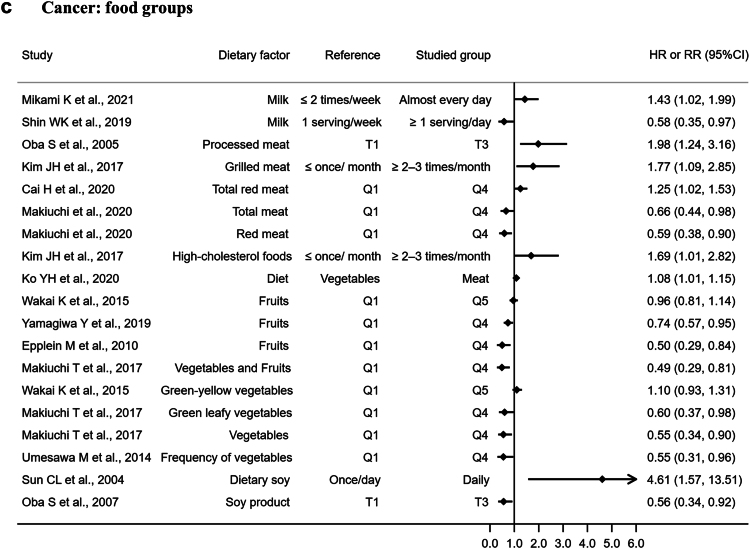
Fig. 1.
Associations (hazard ratios and 95% CI) between dietary intake and diabetes (a; n = 14), cardiovascular diseases (b; n = 4), and cancer (c and d; n = 33) based on findings from 51 cohort studies in the Western Pacific region. A forest plot showing the associations between dietary intake in the top quartile (Q4) or quintile (Q5) and NCDs. aMED, the alternate Mediterranean diet; AHEI-2010, the Alternative Health Eating Index-2010; DASH, the Dietary Approaches to Stop Hypertension; DFA, a high-dairy & high-fruit-and-vegetable & low-alcohol; HR, hazard ratio; RR, relative risk; PUFA, polyunsaturated fatty acid; CI, confidence interval; T, tertile.
Our systematic review identified 52 cohort studies examining the associations between different dietary factors and NCDs: for DM (n = 14), CVDs (n = 4), cancers (n = 33), and respiratory diseases (n = 1) in the Western Pacific region. Fig. 1 and Supplementary Table S2 summarize the key findings. Some main findings were: 1) decreased risk of DM was associated with increased dietary intakes of coarse grain,7,8 fresh fruit,9, 10, 11 wheat,11 and vegetables,8,11 while there was an increased risk with higher intakes of total fat and carbohydrates,12 fish,13 red meat,11,13,14 and junk food8; 2) CVD risks were lower with higher intakes of peanuts,15 unprocessed meats,16 and total fiber17; 3) lower cancer risks were associated with several dietary patterns (i.e., the Alternative Healthy Eating Index updated in 2010,18 an alternate Mediterranean diet score,18 Dietary Approaches to Stop Hypertension [DASH],18 a high-dairy and high-fruit-and-vegetable and low-alcohol pattern score,19 and vegetable-fruit-soy pattern20), food groups (i.e., higher intakes of milk,21,22 red meat,23, 24, 25 vegetables,26,27 and fruits,26,28 as well as lower consumption of grilled meat,29 high-cholesterol foods,29 and processed meat intake30), some nutrients (i.e., lower sodium,31,32 and saturated fat33); and 4) a higher risk of COPD was associated with lower fish intake34 and in those with a smoking history.35 Please see more results in Supplementary Table S2.
Forty-two cohort studies examined the associations between the other lifestyle factors and NCDs: DM (n = 4), CVDs (n = 5), cancers (n = 32), and respiratory diseases (n = 1) in the Western Pacific region (Table 1). Overall, a healthier lifestyle, as mainly determined by a comprehensive evaluation of physical activity, smoking, and drinking was associated with a decreased risk of several NCDs. We found that 1) increased levels of physical activity, including commuting transportation, was associated with reduced risk of DM,11 CVD,36 and cancer24; 2) smoking was associated with an increased risk of CVD,37 DM,38,39 and cancer,40,41; even former smokers who have quit still face a higher risk of these health issues than those who have never smoked; 3) alcohol consumption was associated with an increased risk of cancer,24,40 whereas light drinking was associated with a decreased DM risk.11
Overall, the main findings in the Western Pacific region were consistent with those in other regions. However, compared to studies conducted in other regions, the cohorts identified primarily consisted of participants from four upper MICs or HICs. This limitation may have constrained the generalizability of our findings. Second, there was a lack of research on several lifestyle factors (i.e., sugar-sweetened beverages [SSBs], fruit juice, and alcoholic beverages)42,43 and on those that represent the unique culture of each Western Pacific region country. For example, dietary patterns such as the Alternative Healthy Eating Index updated in 201018 and Dietary Approaches to Stop Hypertension (DASH) used in those cohorts were mainly developed from studies in other regions. Moreover, some of the above results were mainly based on some single cohort studies in the region, although the quality scores of cohorts were high. Finally, due to the limitations of the identified cohort studies (e.g., inadequate comparable results), we could not conduct a meta-analysis.
These cohort studies qualitatively showed that dietary patterns and other lifestyle factors have important associations with NCDs in the Western Pacific region.42,43 The finding were also supported by the representative but limited results from randomized controlled trials (RCTs). For example, the Japan Diabetes Prevention Program reported that a 3-year lifestyle intervention (diet or exercise) significantly reduced the cumulative incidence of type 2 DM among participants with impaired glucose tolerance.44 Supportively, the Da Qing Diabetes Preventive Study with much longer follow up (≥30-year) reported lifestyle intervention (diet, exercise, or diet plus exercise) could not only effectively delay the onset of type 2 DM, but also reduce the incidence of diabetes-related diseases compared with the control.45 Unprecedented growth in the use and availability of social media afforded new avenues for supporting lifestyle intervention against NCDs at low cost. However, mHealth lifestyle interventions targeting improve diet and exercise for NCDs in the Western Pacific region have been limited to upper MICs or HICs; additionally, these interventions primarily focused on NCD populations and relied on relatively simple interventions, such as text messages and WeChat.46,47 In comparison, other regions, such as the US, have employed more sophisticated approaches by combining websites with wearable devices for lifestyle interventions.46,47
Patterns in dietary intakes and other lifestyle behaviors in the Western Pacific region
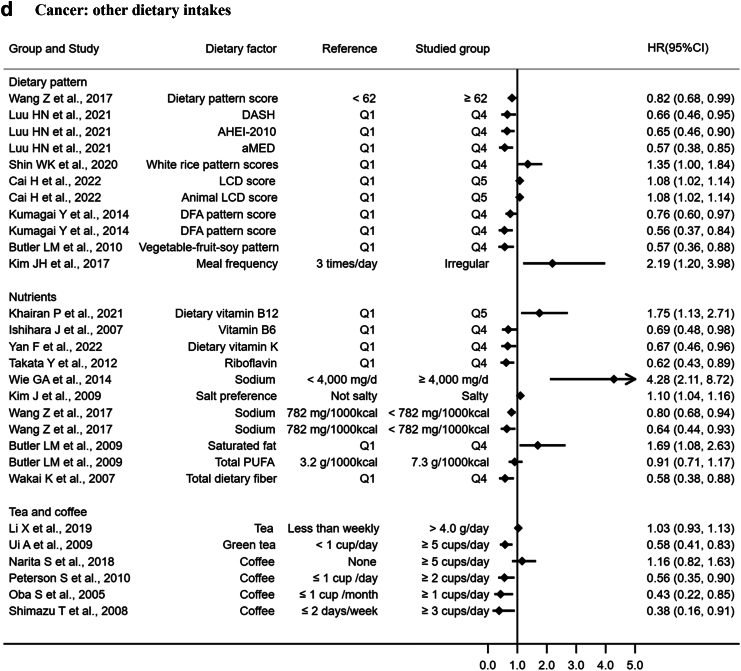
Countries in the Western Pacific region have been experiencing a nutrition transition accompanied by urbanization, economic development, and technological advancement.4 Overall, these countries have made favorable changes, featured by increased consumption of fruits and vegetables as well as decreased intakes of salt and unhealthy fat.48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61 These were also supported by the risk ranking between 1990 and 2019 based on the GBD data (Table 2, Supplementary Table S5, and Fig. 2).
Table 2.
Patterns of dietary and other lifestyle based on national data in selected countries in the Western Pacific region.
| Countries | References | Dietary intakes (A) | Other lifestyle factors (B) |
|---|---|---|---|
| China | Huang L et al., 202148 (A) 2020 Report on Nutrition and Chronic Disease Status of Chinese Residents49 (A) 2021 Scientific Research Report on Dietary Guidelines for Chinese Residents50 (B) Zhang M et al., 202251 (B) |
1) Dietary structure shifted from plant-based diets to animal-and plant-based diets from 1982 to 2015–2017
The percentage of energy intake from carbohydrates declined from 70.8% to 53.4% but the contribution of fat to total energy intake increased from 18.4% to 34.6% from 1982 to 2015–2017. 3) High consumption of cooking oil and salt Daily cooking oil intake increased from 29.5 g/day to 43.2 g/day. Although salt intake decreased from 13.9 g/day to 9.3 g/day from 1992 to 2015–2017, it remains high. |
1) Smoking The prevalence of current smoking decreased from 58.4% to 50.8% in men and remained low at around 2% in women from 2007 to 2018. 2) Alcohol
|
| Republic of Korea | Korean Health Statistics 2021: Korea National Health and Nutrition Examination Survey (KNHANES VIII-3)52 (A) Chang Y et al., 201953 (B) Kim SY et al., 202154 (B) Sung H et al., 202255 (B) |
1) About 80% of adults consume adequate energy, and the energy composition ratio has changed from 2012 to 2021
|
1) Smoking
|
| Japan | Fauzi et al., 202256 (A) National Health and Nutrition Survey62 (A and B) |
1) Decreasing trend in total energy intake from 1995 to 2019 Total energy intake among adults (≥20 years) declined from 2327 to 2141 kcal/day in men and 1855 to 1717 kcal/day in women from 1995 to 2019. 2) Decreasing trend in total protein intake from 1995 to 2019 Total protein intakes among adults (≥20 years) declined from 92.5 to 78.8 g/day in men and 75.7 to 66.4 g/day in women from 1995 to 2019. 3) Main protein sources showed opposite trends from 2001 to 2019 Meat intake increased from 87.6 to 117.4 g/day in men and 62.4 to 86.7 g/day in women, whereas fish intake declined from 116.3 to 76.3 g/day in men and 91.6 to 61.7 g/day in women. The mean vegetable intake was 280.5 g in all participants, 288.3 g in men, and 273.6 g in women with no significant change over the past 10 years (2009–2019). 4) High salt consumption from 1995 to 2019 Salt intake declined from 15.0 to 10.9 g/day in men and 13.0 to 9.3 g/day in women, but remains higher than the Health Japan 21 target of 8.0 g/day and WHO recommended level of 5.0 g/day. |
1) Smoking The prevalence of current smokers among adults (≥20 years) decreased from 52.7% to 27.1% in men, and slightly decreased from 10.6% to 7.6% in women from 1995 to 2019. 2) Alcohol The prevalence of habitual drinkers (>3 times/week) among adults (≥20 years) decreased from 54.4% to 33.9% in men, and slightly increased from 7.4% to 8.8% in women from 1995 to 2019. 3) Physical activity
|
| Australia | Australian Bureau of Statistics, 2020–202157 (A and B) Australian Institute of Health and Welfare, 201858 (A and B) |
1) About 1/3 of Australians’ energy comes from discretionary food that is high in energy and low in nutrients 2) Adherence to the recommended serving of vegetables, fruit, grains, meat and alternatives, and dairy products and alternatives is low
|
1) Smoking
|
| Viet Nam | Vietnam National Institute of Nutrition, 202159 (A and B) Vietnam Ministry of Health, 202160 (A and B) Nguyen TT et al., 201861 (A) |
1) A balanced distribution of macronutrients
From 2000 to 2020, although the intake of fruits increased from 62.4 g/day to 140.7 g/day and vegetables from 178.6 to 231.0 g/day, it only achieved 66.4%–74.4% of the recommendation. 3) Decreased rice intake and increased intakes of meat and fats from 2000 to 2020
|
1) Smoking
|
Fig. 2.
Age-standardized leading 18 risk factors (a) and 35 risk factors (b) ranking and its change between 1990 and 2019 based on DALYs per 100,000 from non-communicable diseases for both sexes and all ages in the Western Pacific region from 1990 to 2019. ∗Data were obtained from the GBD compare tool: https://vizhub.healthdata.org/gbd-compare/#0. The data were age-standardized DALYs per 100,000. Solid lines are increases and dashed lines are decreases; DALYs, disability-adjusted life-years.
Despite the decreased rates of smoking in the last 30 years, smoking remained the second leading behavioral risk factor for DALYs in the Western Pacific region (Fig. 2). The increased absolute number of smokers in MICs may explain the high attributable risk of smoking to DALYs in the Western Pacific region.2 In addition, high salt and alcohol use were among the top-ten contributors to DALYs in both 1990 and 2019. Other dietary risks and low physical activity had minor changes from 1990 to 2019, except for low vegetable consumption.
The Western Pacific region has an increased consumption of ultra-processed foods (i.e., meat and SSB) over the last 30 years. Overall, there was an increase in the consumption of processed and red meats, especially in upper MICs (i.e., China) and HICs (i.e., Australia, Japan, and the Republic of Korea),52, 53, 54, 55, 56, 57, 58 consistent with the global trends.63 The mean intakes of red meat (g/day; median IQR) in Australia (83.7 [79.2–88.6]) was higher than those in the US and selected western countries: the US, 48.5 (47.1–49.9); Canada, 46.1 (44.3–47.9); Mexico, 45.9 (40.9–51.0),64 which were comparable with those in China (49.8; 46.5–53.3) and the Republic of Korea (46.2; 43.4–49.1). Interestingly, the Western Pacific region had a lower intake of SSB than the global average, but the average annual percentage of change was higher (2.8% vs. 1.3%). This increase was largely driven by some MICs (e.g., China and Vietnam). In China, SSB intake increased substantially from 7.1 g/day in 1990 to 31.7 g/day in 2019, and 5.8 g/day to 19.4 g/day in Viet Nam. In contrast, SSB intake remained stable in some HICs (e.g., Japan and Australia). These results suggest that specialized intervention strategies are needed to support the consumption of minimally processed foods in some MICs and HICs in the Western Pacific region.
Patterns in dietary intakes varied across the Western Pacific region. For example, vegetable consumption increased in Viet Nam, but decreased in China, Australia, and Japan.48, 49, 50, 51,56, 57, 58, 59, 60, 61 Although salt intake in China and Japan slightly decreased, the intake of almost 10.0 g/day was still among the highest in the Western Pacific region and double that of the WHO’s recommended limit of below 5 g/day.65 In addition to wide variations in urbanization and economic development within the region, other factors such as geography, ethnicity, and culture might explain the shifts in dietary intakes among countries in the Western Pacific region. This diversity may be a factor in the heterogeneity of nutrition transition within the various countries. It may therefore be advantageous to establish dietary guidelines for NCD prevention based on geography and local culture, as in the case of Japan, whose dietary guidelines recommend taking advantage of the local dietary culture and local food products while incorporating new and different dishes.54, 55, 56, 57, 58,66
Over the last 30 years, the exposure risk presented by low physical activity and alcohol use consistently increased, while smoking decreased across the region. Nevertheless, smoking rates and alcohol consumption in the Western Pacific region were higher than those at the global level. Specifically, Australia and Japan, with higher incomes, also had the highest exposure risk for alcohol use but had a rapid decrease in the rate of smoking exposure risk compared to other countries. On the other hand, lower MICs (e.g., Viet Nam) had a rapid increase in rates of alcohol exposure risk.67
The discrepancy in the trend in alcohol consumption between HICs and MICs in the Western Pacific region may be due to the differences in their public health policies. HICs such as Japan already have concrete policies regulating smoking and alcohol use for NCD prevention. For example, according to the Health Japan 21 national report, the prevalence of habitual drinking in Japan between 1995 and 2019 decreased from 52.7% to 27.1%.62 Meanwhile, economic growth in MICs has made alcoholic beverages more affordable for their residents. Additionally, lower tax rates and the absence of restrictions on alcohol advertisements in the media contribute to its higher availability and use.67 Anthey and colleagues analyzed alcohol consumption data from the WHO and suggested that per-capita consumption of alcohol was expected to increase further in the Western Pacific region and might double from 2017 to 2030.68 Although the wealth of a country is associated with higher alcohol consumption, in some areas the Islamic religion plays a more dominant role in mitigating use due to its prohibition of alcohol.68 For example, in Malaysia, alcohol consumption was low despite of their relatively high gross domestic product per capita.69
National guidelines and policies on NCD prevention and control in the Western Pacific region
National dietary and other lifestyle guidelines
National dietary guidelines are important to help promote a healthy diet and for NCD prevention and control. Selected countries in the Western Pacific region have released their national dietary guidelines; some of them might have adapted the guidelines or some items on them from the WHO/Food and Agriculture Organization (FAO). Table 3 summarizes key contents of national dietary and other lifestyle guidelines from Australia, China, Japan, the Republic of Korea, and Viet Nam for NCD prevention and control in comparison with those from the WHO/FAO. We have highlighted these countries with a representation of population size, socio-economic development levels, geographic location, and ethnic groups.
Table 3.
National guidelines relevant to non-communicable diseases prevention and control in selected countries in the Western Pacific region.
| WHO/FAO70, 71, 72, 73, 74, 75, 76 | China50,77,78 | Republic of Korea79, 80, 81 | Japan82,83 | Australia84, 85, 86, 87 | Viet Nam88, 89, 90 | |
|---|---|---|---|---|---|---|
| 1) Overall guidelines for NCD prevention and control |
|
|
|
|
|
|
| 2) Macronutrients (% of total energy intake) | ||||||
| Carbohydrate | 55–75 | 50–65 | 55–65 | 50–65 | 45–65 | 55–65 |
| Protein | 10–15 | 10–15 | 7–20 | 13–20 | 15–25 | 13–20 |
| Fat | 15–30 | 20–30 | 15–30 | 20–30 | 20–35 | 20–25 |
| Free sugar | <10 | – | 10–20 | – | – | 16–20 |
| Added sugar | – | <10 | <10 | – | – | Reduced |
| Saturated fat | <10 | <10 | <7 | <7 | <10 | <10 |
| Trans fat | <1 | <1 | <1 | – | – | – |
| Linoleic acid | – | – | – | – | 4–10 | 1 |
| 3) Fibers | ||||||
| Male (g/day) | >25 | Overall 25–35 |
19–64 years: 30 ≥65 years: 25 |
18–64 years: ≥21 ≥65 years: ≥20 |
30 | 28 |
| Female (g/day) | ≥19 years: 20 | 18–64 years: ≥18 ≥65 years: ≥17 |
25 | 25 | ||
| 4) Minerals | ||||||
| Sodium (mg/day) | <2000 | <2000 | ≤2300 | Male: <3000 Female: <2600 |
≤2300 | <2000 |
| Potassium (mg/day) | >3510 | 2000 | >3500 | Male: ≥3000 Female: ≥2600 |
Male: 3800 Female: 2800 |
>3510 |
| 5) Physical activities |
|
|
≥30 min a day, ≥5 times a week, walking or exercising until sweaty |
|
|
|
| 6) Alcohol drinking | Limit alcohol consumption | Daily alcohol consumption should not exceed 15 g | Avoid even drinking one or two drinks a day | <40 g per day for men and <20 per day for women | No more than 100 g/week and no more than 40 g on any one day | Not recommended |
| 7) Smoking |
|
|
|
|
|
|
Most of the specific guidelines for food groups and nutrients are similar across countries in the Western Pacific region. These guidelines emphasize the importance of a varied and balanced diet, moderate consumption of meat and its derivatives, and limited consumption of food rich in fat, free sugars, salt, or alcohol. It is also recommended to maintain healthy body weight, engage in regular physical activity, and avoid smoking.
Regarding intakes of macro-nutrients, the suggested proportion of energy from carbohydrates, fats, and protein was 55–75%, 10–15%, and 15–30%, respectively.56,64, 65, 66 The selected national guidelines suggested a percentage of total fat contribution to total energy intake of <30%, except for Australia's suggestion of <35%.77,78,81, 82, 83, 84,91 The slight differences between Australia and the other selected four countries may be attributed to their respective traditional dietary culture. For example, the traditional Chinese diet is high in fish rather than meat and its product, while the Australian diet gains a significantly higher percentage of energy from fat, which was similar to the US (carbohydrate, 45–65%; fat, 20–35%).92 These countries recommended saturated fats intake of <10% of total energy, which is consistent with recommendations in other countries in Europe or America.93 Added sugar is <10% of total energy in China and the Republic of Korea,78,81 consistent with recommendations of the US and Sweden.93 Otherwise, the recommendation for free sugars (which could be added or naturally occurring in foods or drinks) is <10–20% for the Republic of Korea and 16–20% for Viet Nam,81,88 which exceeds the WHO guideline recommendation of 10%. Australia and Japan did not provide specific recommendations regarding free or added sugar.82,84 Fiber intake at >25 g/day was the same as recommendations by the WHO/FAO and was recommended by most studied countries78,81,85,91 except Japan (males: ≥21 g/day, females: ≥18 g/day).82
Regarding sodium intake, China and Viet Nam recommended an intake of <2000 mg/day,78,91 the same as that from the WHO/FAO recommendation.70,71 This recommendation is also adopted by most countries in America and Europe,93 while the Republic of Korea and Australia recommended ≤2300 mg/day,81 and Japan recommended <3000 mg/day for males and <2600 mg/day for females.82 One possible reason for this could be their traditional seasonings that typically added salt to the diet. For example, the Japanese diet is high in soy sauce, miso, and dried fish products,94 and the Korean diet are high in kimchi and processed food.95 The Republic of Korea and Viet Nam recommended a potassium intake of 3500 mg/day,81,91 just as the WHO recommendation,72 whereas it was lower in China (2000 mg/day), Japan (≥2600 mg/day),78,82 and Australia for females (2800 mg/day) but higher in Australia for males (3800 mg/day).84,85
The guidelines for other lifestyle factors are generally consistent, except for alcohol consumption.73,74,86,87,89,90 Japan and Australia recommended higher levels compared to those recommended by the WHO.
National policies and actions
Some Western Pacific region countries face an increased double burden of nutritional health problems (i.e., under- and over-nutrition problems, as marked by the prevalence of both underweight and obesity). Most MICs (e.g., China, Malaysia, and Viet Nam) were previously geared toward fighting widespread undernutrition and now need to curb the rapid increase in obesity prevalence.96 Since 2004, the WHO Regional Office for Western Pacific region has hosted about 30 food and nutrition-centered meetings, consultations, and workshops. Since 2012, the meeting focus has been shifting from a single nutrition risk toward solution-oriented meetings directed at NCDs.97 Countries in the Western Pacific region have responded differently to such efforts and to those by the WHO that call on actions to fight NCDs. In general, HICs have more resources and attention to give to NCD prevention and control, and thus respond better to NCDs than MICs.
Economic development creates an economic disparity in society, leaving hunger and malnutrition among the poor unresolved while increasing obesity and NCDs due to overnutrition among the wealthy, resulting in increased medical costs.96,97 In the process of national economic development, advances in food processing technology and the increase in imported foods have made energy-dense foods with high sugar and fat content available at low prices, as a consequence of which obesity is emerging as a serious public health concern among lower MICs. National nutrition action plans play an essential role in helping to improve both national and global health and reducing health disparities.
Well-established nutrition policies and programs are important tools to guide nations in handling NCD issues and providing a framework for the coordinated implementation of interventions by governments and other organizations. For example, actively responding to its challenges, the Chinese government has released a series of national plans or actions during the past five years, such as the Healthy China 2030 Blueprint, Healthy China Initiative (2019–2030), and National Nutrition Plan (2017–2030). In the context of the comprehensive implementation of the National Strategy for Healthy China98, 99, 100 in recent years, “National Nutrition Week” is held every year by the Chinese Nutrition Society and is supported by the Chinese government.101 In Australia, several strategies were also employed to improve nutrition and health, including government-led voluntary nutrient reformulation targets, interpretive front-of-pack labeling, and institutional nutrition policies.102, 103, 104 In the future, countries in the Western Pacific region may learn from the experiences of their more economically developed peers in the region, such as Japan, the Republic of Korea, and Singapore, and adapt some of the effective practices.
Key challenges
Western Pacific region countries have been undergoing rapid changes, such as demographic shifts, new approaches to disease prevention, control, and treatment, technological innovation, and economic growth, all of which affect their NCD burden as well as their related policies and actions.1 These dynamics call for setting up strong national action strategies and policies to accelerate progress toward the global NCD targets. Therefore, proposing recommendations that encompass all Western Pacific region countries is a big challenge.
We tried to make recommendations based on the previously analyzed data and references. However, the cohort studies mainly focused on only four countries, and there were very few cohort studies on added sugar and alcoholic beverages. Quantitative analysis such as meta-analysis could not be performed due to inadequate results. There were limited representative RCTs examining the effects of lifestyle factors on NCDs. This knowledge gap hampered our ability to draw definitive conclusions and provide evidence-based recommendations for preventive strategies and interventions.
In addition, there is a need for comprehensive mHealth intervention studies targeting dietary and other lifestyle factors. It is particularly important to prioritize studies conducted in lower MICs. Policies concerning restrictions on added sugars and processed products need to be strengthened, as the consumption was increasing in the Western Pacific region. Finally, it is necessary to develop effective dietary and lifestyle strategies and programs that fit the traditional cultures in the region.
Recommendations for future actions
We proposed recommendations for action strategies for NCD prevention and control regarding dietary intakes and other lifestyle factors in the Western Pacific region (Table 4).
Table 4.
Recommendations of action strategies to address dietary and other lifestyle factors for non-communicable diseases (NCDs) prevention and control in the Western Pacific region.
| Perspectives | Description |
|---|---|
| 1. Overall |
1.1 Establish comprehensive approaches with new perspectives
|
1.2 Promote cross-sector cooperation
|
|
1.3 Establish innovative policies and programs that enable tailored approaches
|
|
| 2. Promote healthy diet |
2.1 Scaling up interventions, including national investment and policy approaches to promote healthy diet
|
2.2 Enhance regulations of the food industry
|
|
2.3. Establish evidence-based recommendations that reflect national and religious characteristics for evidence-based implementation
|
|
| 3. Reduce smoking and alcohol consumption |
Reduce smoking and alcohol consumption
|
| 4. Increase physical activity |
Invest in facilities and environments that help increase physical activity
|
Regularly eating a variety of fresh and nutritious foods such as fruits, vegetables, legumes, nuts, beans, whole grains, and fish is essential for NCD prevention and control.70,75 Therefore, while most countries in the Western Pacific region recommended a balanced diet with a variety of food, some foods might be difficult to access due to production, geographical, political, and economic reasons. Appropriate national policies and investment in the food system are needed to improve local food production, policies, and exchange within and among countries in the Western Pacific region and beyond. However, increased trade in foodstuffs can increase pollution, requiring investments in green transportation, storage, and distribution infrastructure to improve access to fresh and nutritious foods.105
The DASH diet, Mediterranean dietary pattern, and vegetable and whole grain dietary pattern lower the risk of NCDs.7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18 Moreover, increased whole grain intake was associated with decreased NCDs, but the intake of such nutritious foods in the Western Pacific region is decreasing.75 While the availability and access to low-priced, ultra-processed, and energy-dense foods, including refined grains, are increasing as the result of rapid industrialization and globalization as well as national policies and standards that have prioritized safety over nutritional values and health promotion.106 National policies should promote the consumption of whole grains.
Policies regulating foods high in fat, sugar, and salt should be enforced with cross-sectorial cooperation.105 Policies such as imposing taxes, improving incentives, and industry regulations such as creating regulatory measures on food composition and labeling should be strongly considered. Therefore, future interventions need to focus on the implementation of the WHO best buys and WHO guidelines for improving the food environment.
As limiting salt intake is the most cost-effective measure to prevent and control NCDs,71 Western Pacific region countries need to encourage the reformulation of food products to contain less salt and promote front-of-pack labeling.
Although limiting the consumption of sugar-added foods and drinks is a strong recommendation from the WHO for managing NCDs, the recommendations in some countries in the Western Pacific region are insufficient.76,82, 83, 84, 85,88 SSBs need to be restricted through strong government policies such as applying taxes and banning advertising, promotion, and sponsorship on TV, radio, and in print materials. In addition, school education and media campaigns should include reducing the consumption of SSBs.
Best practices should also eliminate industrial trans fats (i.e., ban their production, distribution, and use), limit high-fat food production, reduce fried food consumption, and limit the use of fat and oil in cooking. In terms of food production, we recommend a mandatory national limit of 2 g of industrial trans fats per 100 g of total fat in all foods and a ban on the production or use of partially hydrogenated oils, which are a major source of industrially produced trans fats, as an ingredient in foods.
For evidence-based policy implementation for NCD prevention and control, appropriate national standards for nutrient intake requirements are needed. In some Western Pacific region countries, overweight and obesity coexist with underweight and micronutrient deficiencies.70 Therefore, national dietary guidelines should inform the public not only of the appropriate calorie intake levels to maintain healthy body weight but also of nutrient intake levels for maintaining health. Additionally, within the Western Pacific region, some religions require specific dietary rules to be followed (i.e., Halal for Muslim populations), so special attention to ethnic religions, and traditional culture should be given to national nutrition action/plans.
Given smoking rate and alcohol consumption in the Western Pacific region are higher than those at the global level, stronger national policies (i.e., the tobacco plain package policy in Australia) and actions are needed to regulate the marketing and consumption of tobacco and alcohol. In addition, investments related to comprehensive mHealth care using wearable devices are needed to encourage dietary habits and exercise in daily life, especially in lower MICs.46,47 Finally, accompanied by socioeconomic changes, other important factors such as sleep habits have become important factors to NCDs. Further studies are needed to incorporate them, especially representative RCTs.
Finally, comprehensively managing all areas of NCD prevention and management at the national level through a new perspective on health care, especially including dietary factors and lifestyle approaches, is required. To prevent economic inequality from being applied, it is necessary to establish policies that seek ways to provide new technologies and services such as big data, artificial intelligence, and mobile health management to underprivileged groups.
Conclusions
Western Pacific region countries have experienced different shifts in dietary intakes, other lifestyle factors, and NCD burden during the past 30 years. This region has diverse cultures, religions, political systems, socioeconomic development levels, lifestyles, and environmental factors. The Western Pacific region saw some improvement and worsening of dietary intakes such as decreased consumption of sodium and saturated and trans fats and increased consumption of processed foods and sugar-sweetened beverages. Although the smoking rate in some countries has declined, the rate remains high in some countries. The prevalence of inadequate physical activity and excessive alcohol consumption has increased in many countries. There are variations in national policies and approaches targeting NCD in the Western Pacific region. More vigorous efforts are needed to develop effective and sustainable policies and programs to fight the growing NCD epidemic in this region.
Contributors
YW, HL, and XS initiated the concepts; XS, DKY, TTN, KT, KS, and HL collected data; DKY, XS, JS, and LZ analyzed the data and produced figures; and XS, DKY, KS, HL, and YW drafted the manuscript. All authors interpreted the data, revised the manuscript critically, and approved the submission of the manuscript in its current form.
Declaration of interests
There is no conflict of interest.
Acknowledgment
We thank Profs Zumin Shi and Yue Ma for their important contribution in improving this manuscript, thank Meng Lv, Fuyuan Wen, Minji Kang, Haelim Lee, Hyeon Jin Kim, Hyunju Yon, and Hyoin Shin for their assistance in collecting some information and editing, and thank Profs Dongfeng Gu, Yaogang Wang, Liang Sun, Fengchao Liang, Xueli Yang, and Ruiyue Yang for their comments to help improve the manuscript.
Funding: The study is funded in part by research grants from the National Key R&D Program of China (2017YFC0907200, 2017YFC0907201, 2016YFC0900603), International Collaboration Project from the Chinese Ministry of Science and Technology-Prevention and Control of Chronic Diseases and Health Promotion (G2021170007L), Natural Scientific Foundation of China (82103846), Key R&D and Transformation Program of Qinghai (2023-QY-204), Key Scientific and Technologic Project in Qinghai Province (2021-NK-A3), Chinese Nutrition Society (CNS-SCP2020-40), and the National Research Foundation of Korea (NRF, NRF-2022R1A2C1003746) and Chinese Nutrition Society. The collaborating institutions have contributed additional resources. The content of the paper is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100842.
Contributor Information
Hyunjung Lim, Email: hjlim@khu.ac.kr.
Youfa Wang, Email: youfawang@xjtu.edu.cn.
Appendix A. Supplementary data
References
- 1.World Health Organization . 2022. Regional action framework for noncommunicable disease prevention and control in the Western Pacific.https://www.who.int/docs/default-source/wpro---documents/regional-committee/session-73/wpr-rc73-agenda-12-annex-ncd-prevention-and-control.pdf/ [Google Scholar]
- 2.GBD 2019 Risk Factors Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoshide S., Yamamoto K., Katsurada K., et al. Agreement regarding overcoming hypertension in the Asian Hypertension Society Network 2022. Hypertens Res. 2023;46(1):3–8. doi: 10.1038/s41440-022-00994-1. [DOI] [PubMed] [Google Scholar]
- 4.Popkin B.M. Relationship between shifts in food system dynamics and acceleration of the global nutrition transition. Nutr Rev. 2017;75(2):73–82. doi: 10.1093/nutrit/nuw064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu D., Zhao L., Zhao W. Status and trends in consumption of grains and dietary fiber among Chinese adults (1982-2015) Nutr Rev. 2020;78(Suppl 1):43–53. doi: 10.1093/nutrit/nuz075. [DOI] [PubMed] [Google Scholar]
- 6.Budreviciute A., Damiati S., Sabir D.K., et al. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.574111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang J., Du H., Guo Y., et al. Coarse grain consumption and risk of cardiometabolic diseases: a prospective cohort study of Chinese adults. J Nutr. 2022;152(6):1476–1486. doi: 10.1093/jn/nxac041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y., Wang N., Xu K., Liu T., Fu C. Associations of dietary patterns and incident type 2 diabetes in a community population cohort from Southwest China. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.773172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li L., Yang H.-Y., Ma Y., et al. Whole fresh fruit intake and risk of incident diabetes in different glycemic stages: a nationwide prospective cohort investigation. Eur J Nutr. 2022;62(2):771–782. doi: 10.1007/s00394-022-02998-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du H., Li L., Bennett D., et al. Fresh fruit consumption in relation to incident diabetes and diabetic vascular complications: findings from the China Kadoorie Biobank study. Lancet Diabetes Endocrinol. 2016;4 [Google Scholar]
- 11.Lv J., Yu C., Guo Y., et al. Adherence to a healthy lifestyle and the risk of type 2 diabetes in Chinese adults. Int J Epidemiol. 2017;46(5):1410–1420. doi: 10.1093/ije/dyx074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ha K., Joung H., Song Y. Inadequate fat or carbohydrate intake was associated with an increased incidence of type 2 diabetes mellitus in Korean adults: a 12-year community-based prospective cohort study. Diabetes Res Clin Pract. 2019;148:254–261. doi: 10.1016/j.diabres.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 13.Du H., Guo Y., Bennett D.A., et al. Red meat, poultry and fish consumption and risk of diabetes: a 9 year prospective cohort study of the China Kadoorie Biobank. Diabetologia. 2020;63(4):767–779. doi: 10.1007/s00125-020-05091-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Talaei M., Wang Y.-L., Yuan J.-M., Pan A., Koh W.-P. Meat, dietary heme iron, and risk of type 2 diabetes mellitus: the Singapore Chinese Health study. Am J Epidemiol. 2017;186(7):824–833. doi: 10.1093/aje/kwx156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ikehara S., Iso H., Kokubo Y., et al. Peanut consumption and risk of stroke and ischemic heart disease in Japanese men and women: the JPHC study. Stroke. 2021;52(11):3543–3550. doi: 10.1161/STROKEAHA.120.031212. [DOI] [PubMed] [Google Scholar]
- 16.Park K., Son J., Jang J., et al. Unprocessed meat consumption and incident cardiovascular diseases in Korean adults: the Korean Genome and Epidemiology study (KoGES) Nutrients. 2017;9(5):498. doi: 10.3390/nu9050498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kokubo Y., Iso H., Saito I., et al. Dietary fiber intake and risk of cardiovascular disease in the Japanese population: the Japan Public Health Center-based study cohort. Eur J Clin Nutr. 2011;65(11):1233–1241. doi: 10.1038/ejcn.2011.100. [DOI] [PubMed] [Google Scholar]
- 18.Luu H.N., Paragomi P., Jin A., et al. Quality diet index and risk of pancreatic cancer: findings from the Singapore Chinese Health study. Cancer Epidemiol Biomark Prev. 2021;30(11):2068–2078. doi: 10.1158/1055-9965.EPI-21-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumagai Y., Chou W.-T., Tomata Y., et al. Dietary patterns and colorectal cancer risk in Japan: the Ohsaki cohort study. Cancer Causes Control. 2014;25(6):727–736. doi: 10.1007/s10552-014-0375-5. [DOI] [PubMed] [Google Scholar]
- 20.Butler L.M., Wu A.H., Wang R., Koh W.-P., Yuan J.-M., Yu M.C. A vegetable-fruit-soy dietary pattern protects against breast cancer among postmenopausal Singapore Chinese women. Am J Clin Nutr. 2010;91(4):1013–1019. doi: 10.3945/ajcn.2009.28572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mikami K., Ozasa K., Miki T., et al. Dairy products and the risk of developing prostate cancer: a large-scale cohort study (JACC Study) in Japan. Cancer Med. 2021;10(20):7298–7307. doi: 10.1002/cam4.4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin W.-K., Lee H.-W., Shin A., Lee J.-K., Kang D. Milk consumption decreases risk for breast cancer in Korean women under 50 years of age: results from the health examinees study. Nutrients. 2019;12(1):32. doi: 10.3390/nu12010032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cai H., Sobue T., Kitamura T., et al. Association between meat and saturated fatty acid intake and lung cancer risk: the Japan Public Health Center-based prospective study. Int J Cancer. 2020;147(11):3019–3028. doi: 10.1002/ijc.33112. [DOI] [PubMed] [Google Scholar]
- 24.Ko Y.H., Kim S.J., Kim W.S., et al. Risk factors for primary lung cancer among never-smoking women in South Korea: a retrospective nationwide population-based cohort study. Korean J Intern Med. 2020;35(3):692. doi: 10.3904/kjim.2019.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Makiuchi T., Sobue T., Kitamura T., et al. Relationship between meat/fish consumption and biliary tract cancer: the Japan Public Health Center–based prospective study. Cancer Epidemiol Biomark Prev. 2020;29(1):95–102. doi: 10.1158/1055-9965.EPI-19-0514. [DOI] [PubMed] [Google Scholar]
- 26.Makiuchi T., Sobue T., Kitamura T., et al. The relationship between vegetable/fruit consumption and gallbladder/bile duct cancer: a population-based cohort study in Japan. Int J Cancer. 2017;140(5):1009–1019. doi: 10.1002/ijc.30492. [DOI] [PubMed] [Google Scholar]
- 27.Umesawa M., Iso H., Mikami K., et al. Relationship between vegetable and carotene intake and risk of prostate cancer: the JACC study. Br J Cancer. 2014;110(3):792–796. doi: 10.1038/bjc.2013.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Epplein M., Shu X.-O., Xiang Y.-B., et al. Fruit and vegetable consumption and risk of distal gastric cancer in the Shanghai Women's and Men's Health studies. Am J Epidemiol. 2010;172(4):397–406. doi: 10.1093/aje/kwq144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim J.H., Lee J., Jung S.-Y., Kim J. Dietary factors and female breast cancer risk: a prospective cohort study. Nutrients. 2017;9(12):1331. doi: 10.3390/nu9121331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oba S., Shimizu N., Nagata C., et al. The relationship between the consumption of meat, fat, and coffee and the risk of colon cancer: a prospective study in Japan. Cancer Lett. 2006;244(2):260–267. doi: 10.1016/j.canlet.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 31.Wie G.-A., Cho Y.-A., Kang H.-H., et al. Red meat consumption is associated with an increased overall cancer risk: a prospective cohort study in Korea. Br J Nutr. 2014;112(2):238–247. doi: 10.1017/S0007114514000683. [DOI] [PubMed] [Google Scholar]
- 32.Kim J., Park S., Nam B.-H. Gastric cancer and salt preference: a population-based cohort study in Korea. Am J Clin Nutr. 2010;91(5):1289–1293. doi: 10.3945/ajcn.2009.28732. [DOI] [PubMed] [Google Scholar]
- 33.Butler L.M., Wang R., Koh W.P., Stern M.C., Yuan J.M., Yu M.C. Marine n-3 and saturated fatty acids in relation to risk of colorectal cancer in Singapore Chinese: a prospective study. Int J Cancer. 2009;124(3):678–686. doi: 10.1002/ijc.23950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu W., Shi K., Cao W., et al. Association between fish consumption and risk of chronic obstructive pulmonary disease among Chinese men and women: an 11-year population-based cohort study. J Nutr. 2023;152(12):2771–2777. doi: 10.1093/jn/nxac232. [DOI] [PubMed] [Google Scholar]
- 35.Leem A.Y., Park B., Kim Y.S., Jung J.Y., Won S. Incidence and risk of chronic obstructive pulmonary disease in a Korean community-based cohort. Int J Chron Obstruct Pulmon Dis. 2018;13:509–517. doi: 10.2147/COPD.S148618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fan M., Lv J., Yu C., et al. Association between active commuting and incident cardiovascular diseases in Chinese: a prospective cohort study. J Am Heart Assoc. 2019;8(20) doi: 10.1161/JAHA.119.012556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Woodward M., Lam T.H., Barzi F., et al. Smoking, quitting, and the risk of cardiovascular disease among women and men in the Asia-Pacific region. Int J Epidemiol. 2005;34(5):1036–1045. doi: 10.1093/ije/dyi104. [DOI] [PubMed] [Google Scholar]
- 38.Park S.E., Seo M.H., Cho J.H., et al. Dose-dependent effect of smoking on risk of diabetes remains after smoking cessation: a nationwide population-based cohort study in Korea. Diabetes Metab J. 2021;45(4):539–546. doi: 10.4093/dmj.2020.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sairenchi T., Iso H., Nishimura A., et al. Cigarette smoking and risk of type 2 diabetes mellitus among middle-aged and elderly Japanese men and women. Am J Epidemiol. 2004;160(2):158–162. doi: 10.1093/aje/kwh183. [DOI] [PubMed] [Google Scholar]
- 40.Moy K.A., Fan Y., Wang R., Gao Y.T., Yu M.C., Yuan J.M. Alcohol and tobacco use in relation to gastric cancer: a prospective study of men in Shanghai, China. Cancer Epidemiol Biomark Prev. 2010;19(9):2287–2297. doi: 10.1158/1055-9965.EPI-10-0362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jee S.H., Samet J.M., Ohrr H., Kim J.H., Kim I.S. Smoking and cancer risk in Korean men and women. Cancer Causes Control. 2004;15(4):341–348. doi: 10.1023/B:CACO.0000027481.48153.97. [DOI] [PubMed] [Google Scholar]
- 42.Neuenschwander M., Ballon A., Weber K.S., et al. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ. 2019;366 doi: 10.1136/bmj.l2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Papadimitriou N., Markozannes G., Kanellopoulou A., et al. An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites. Nat Commun. 2021;12(1):4579. doi: 10.1038/s41467-021-24861-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sakane N., Sato J., Tsushita K., et al. Effect of baseline HbA1c level on the development of diabetes by lifestyle intervention in primary healthcare settings: insights from subanalysis of the Japan Diabetes Prevention Program. BMJ Open Diabetes Res Care. 2014;2(1) doi: 10.1136/bmjdrc-2013-000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gong Q., Zhang P., Wang J., et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing diabetes prevention outcome study. Lancet Diabetes Endocrinol. 2019;7(6):452–461. doi: 10.1016/S2213-8587(19)30093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McKeon G., Papadopoulos E., Firth J., et al. Social media interventions targeting exercise and diet behaviours in people with noncommunicable diseases (NCDs): a systematic review. Internet Interv. 2022;27 doi: 10.1016/j.invent.2022.100497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lu X., Yang H., Xia X., et al. Interactive mobile health intervention and blood pressure management in adults. Hypertension. 2019;74(3):697–704. doi: 10.1161/HYPERTENSIONAHA.119.13273. [DOI] [PubMed] [Google Scholar]
- 48.Huang L., Wang Z., Wang H., et al. Nutrition transition and related health challenges over decades in China. Eur J Clin Nutr. 2021;75(2):247–252. doi: 10.1038/s41430-020-0674-8. [DOI] [PubMed] [Google Scholar]
- 49.National Administration of Disease Control and Prevention of the National Health Commission . 2020. Report on nutrition and chronic disease status of Chinese residents, 2020. [Google Scholar]
- 50.The Chinese Nutrition Society . 2021. Scientific research report on dietary guidelines for Chinese residents.https://www.chinanutri.cn/yyjkzxpt/yyjkkpzx/yytsg/zgjm/202103/t20210311_224598.html [Google Scholar]
- 51.Zhang M., Yang L., Wang L., et al. Trends in smoking prevalence in urban and rural China, 2007 to 2018: findings from 5 consecutive nationally representative cross-sectional surveys. PLoS Med. 2022;19(8) doi: 10.1371/journal.pmed.1004064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Korea Disease Control and Prevention Agency . 2022. Korean Health Statistics 2021: Korea national health and nutrition examination survey (KNHANES VIII-3) [Google Scholar]
- 53.Chang Y., Kang H.Y., Lim D., Cho H.J., Khang Y.H. Long-term trends in smoking prevalence and its socioeconomic inequalities in Korea, 1992-2016. Int J Equity Health. 2019;18(1):148. doi: 10.1186/s12939-019-1051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim S.Y., Kim H.J. Trends in alcohol consumption for Korean adults from 1998 to 2018: Korea national health and nutritional examination survey. Nutrients. 2021;13(2):609. doi: 10.3390/nu13020609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sung H., Kim G., Ma X., et al. Physical activity trends in Korean adults from Korea national health and nutritional examination survey from 2014 to 2019. Int J Environ Res Public Health. 2022;19(9):5213. doi: 10.3390/ijerph19095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fauzi M., Kartiko-Sari I., Poudyal H. Trends of dietary intakes and metabolic diseases in Japanese adults: assessment of national health promotion policy and national health and nutrition survey 1995-2019. J Clin Med. 2022;11(9):2350. doi: 10.3390/jcm11092350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Australian Bureau of Statistics Health conditions and risks. 2020-2021. https://www.abs.gov.au/statistics/health/health-conditions-and-risks
- 58.Australian Institute of Health and Welfare . 2018. Nutrition across the life stages. 2018.https://www.aihw.gov.au/reports/food-nutrition/nutrition-across-the-life-stages/summary [Google Scholar]
- 59.Vietnam National Institute of Nutrition . Medical Publishing House; Hanoi: 2021. Main findings of general nutrition survey 2019-2020. [Google Scholar]
- 60.Vietnam Ministry of Health, Hanoi University of Public Health, WHO, CDC . Vietnam Ministry of Health; Hanoi: 2021. National survey on the risk factors of noncommunicable diseases in Viet Nam. [Google Scholar]
- 61.Nguyen T.T., Hoang M.V. Non-communicable diseases, food and nutrition in Vietnam from 1975 to 2015: the burden and national response. Asia Pac J Clin Nutr. 2018;27(1):19–28. doi: 10.6133/apjcn.032017.13. [DOI] [PubMed] [Google Scholar]
- 62.National Institute of Health Nutrition National health and nutrition survey. https://www.nibiohn.go.jp/eiken/kenkounippon21/en/eiyouchousa/index.html
- 63.Clonan A., Roberts K.E., Holdsworth M. Socioeconomic and demographic drivers of red and processed meat consumption: implications for health and environmental sustainability. Proc Nutr Soc. 2016;75(3):367–373. doi: 10.1017/S0029665116000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Frank S.M., Jaacks L.M., Batis C., Vanderlee L., Taillie L.S. Patterns of red and processed meat consumption across North America: a nationally representative cross-sectional comparison of dietary recalls from Canada, Mexico, and the United States. Int J Environ Res Public Health. 2021;18(1):357. doi: 10.3390/ijerph18010357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.World Health Organization Salt reduction. 2020. https://www.who.int/news-room/fact-sheets/detail/salt-reduction
- 66.The Ministry of Agriculture Forestry and Fisheries of Japan . 2016. Main points of the revision of “Dietary guidelines for Japanese”.https://www.maff.go.jp/j/syokuiku/attach/pdf/shishinn-10.pdf [Google Scholar]
- 67.Walls H., Cook S., Matzopoulos R., London L. Advancing alcohol research in low-income and middle-income countries: a global alcohol environment framework. BMJ Glob Health. 2020;5(4) doi: 10.1136/bmjgh-2019-001958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Manthey J., Shield K.D., Rylett M., Hasan O.S.M., Probst C., Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet. 2019;393(10190):2493–2502. doi: 10.1016/S0140-6736(18)32744-2. [DOI] [PubMed] [Google Scholar]
- 69.Sornpaisarn B., Shield K., Manthey J., et al. Alcohol consumption and attributable harm in middle-income South-East Asian countries: epidemiology and policy options. Int J Drug Policy. 2020;83 doi: 10.1016/j.drugpo.2020.102856. [DOI] [PubMed] [Google Scholar]
- 70.World Health Organization . 2003. Diet, nutrition, and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation.https://xueshu.studiodahu.com/books?hl=zh-CN&lr=&id=S6YsDwAAQBAJ&oi=fnd&pg=PA4&dq=World+Health+Organization.+Diet,+nutrition,+and+the+prevention+of+chronic+diseases:+report+of+a+joint+WHO/FAO+expert+consultation:+World+Health+Organization,+&ots=t9_QpsRECd&sig=MmthJYekqzu0nFF0Bwy0LewOVvw [Google Scholar]
- 71.World Health Organization . 2012. Guideline: sodium intake for adults and children.https://apps.who.int/iris/handle/10665/77985 [PubMed] [Google Scholar]
- 72.World Health Organization . 2012. Guideline: potassium intake for adults and children.https://apps.who.int/iris/handle/10665/77986 [PubMed] [Google Scholar]
- 73.World Health Organization . 2020. WHO guidelines on physical activity and sedentary behaviour.https://www.who.int/publications/i/item/9789240015128 [PubMed] [Google Scholar]
- 74.World Health Organization . 2023. No level of alcohol consumption is safe for our health.https://www.who.int/europe/news/item/04-01-2023-no-level-of-alcohol-consumption-is-safe-for-our-health [Google Scholar]
- 75.World Health Organization . 2019. Healthy diet.https://apps.who.int/iris/handle/10665/325828 [Google Scholar]
- 76.World Health Organization . 2015. Guideline: sugars intake for adults and children.https://www.who.int/publications/i/item/9789241549028 [PubMed] [Google Scholar]
- 77.The Chinese Nutrition Society . 2022. Dietary guidelines for Chinese residents 2022.http://dg.en.cnsoc.org/ [Google Scholar]
- 78.National Health Commission of the People’s Republic of China . 2018. Chinese dietary reference intakes.http://www.nhc.gov.cn/wjw/yingyang/wsbz.shtml [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ministry of Health and Welfare. The Korean Nutrition Society . 2020. Application of dietary reference intakes for Koreans 2020.https://www.kns.or.kr/fileroom/FileRoom_view.asp?mode=mod&restring=%252FFileRoom%252FFileRoom%252Easp%253Fxsearch%253D0%253D%253Dxrow%253D10%253D%253DBoardID%253DKdr%253D%253Dpage%253D1&idx=125&page=1&BoardID=Kdr&xsearch=1&cn_search= [Google Scholar]
- 80.Ministry of Health and Welfare National Cancer Center . 2020. National cancer prevention rules, Sejong.https://www.cancer.go.kr/ [Google Scholar]
- 81.Ministry of Health and Welfare. The Korean Nutrition Society . 2020. Dietary reference intakes for Koreans 2020.https://www.kns.or.kr/fileroom/FileRoom_view.asp?mode=mod&restring=%252FFileRoom%252FFileRoom%252Easp%253Fxsearch%253D0%253D%253Dxrow%253D10%253D%253DBoardID%253DKdr%253D%253Dpage%253D2&idx=108&page=2&BoardID=Kdr&xsearch=1&cn_search= [Google Scholar]
- 82.Dietary reference intakes for Japanese. 2020. https://www.mhlw.go.jp/content/10900000/000862500.pdf [Google Scholar]
- 83.Dietary guidelines for Japanese. https://www.maff.go.jp/j/syokuiku/attach/pdf/shishinn-10.pdf
- 84.Australian National Health and Medical Research Council . 2013. Australian dietary guidelines - providing the scientific evidence for healthier Australian diets.https://www.eatforhealth.gov.au/guidelines [Google Scholar]
- 85.Australian National Health and Medical Research Council . 2006. Nutrient reference values.https://www.eatforhealth.gov.au/nutrient-reference-values [Google Scholar]
- 86.Australian Government. Department of Health and Aged Care . 2021. Physical activity and exercise guidelines for all Australians: for adults (18 to 64 years)https://www.health.gov.au/topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-for-all-australians/for-adults-18-to-64-years [Google Scholar]
- 87.Australian Government. Department of Health and Aged Care . 2022. Alcohol.https://www.health.gov.au/topics/alcohol [Google Scholar]
- 88.Vietnam National Institute of Nutrition Vietnam Ministry of Health . Medical Publishing House; Hanoi: 2016. Recommended dietary allowances for Vietnamese people. [Google Scholar]
- 89.Legislation by Country Viet Nam . 2013. Law No. 09/2012/QH13, Law on prevention and control of tobacco harms.https://www.tobaccocontrollaws.org/legislation/viet-nam/laws [Google Scholar]
- 90.The Socialist Republic of Viet Nam . 2019. Law No. 44/2019/QH14 dated June 14, 2019 on prevention and control of harmful effects of alcoholic beverages.https://thuvienphapluat.vn/van-ban/EN/The-thao-Y-te/Law-44-2019-QH14-on-prevention-and-control-of-harmful-effects-of-alcoholic-beverages/419553/tieng-anh.aspx [Google Scholar]
- 91.Pham Van Hoan M. Vietnam recommended dietary allowances 2007. Asia Pac J Clin Nutr. 2008;17:409. [PubMed] [Google Scholar]
- 92.U.S. Department of Agriculture. U.S. Department of Health and Human Services . 2020. Dietary guidelines for Americans, 2020-2025.https://www.dietaryguidelines.gov/ [Google Scholar]
- 93.Cámara M., Giner R.M., González-Fandos E., et al. Food-based dietary guidelines around the world: a comparative analysis to update AESAN Scientific Committee dietary recommendations. Nutrients. 2021;13(9):3131. doi: 10.3390/nu13093131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Toda A., Ishizaka Y., Tani M., Yamakado M. Current dietary salt intake of Japanese individuals assessed during health check-up. Hypertens Res. 2015;38(2):163–168. doi: 10.1038/hr.2014.154. [DOI] [PubMed] [Google Scholar]
- 95.Park H.K., Lee Y., Kang B.W., et al. Progress on sodium reduction in South Korea. BMJ Glob Health. 2020;5(5) doi: 10.1136/bmjgh-2019-002028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Popkin B.M., Corvalan C., Grummer-Strawn L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395(10217):65–74. doi: 10.1016/S0140-6736(19)32497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Reeve E., Thow A.M., Huse O., Bell C., Peeters A., Sacks G. Policy-makers' perspectives on implementation of cross-sectoral nutrition policies, Western Pacific region. Bull World Health Organ. 2021;99(12):865–873. doi: 10.2471/BLT.20.283366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.The Communist Party of China Central Committee the State Council . 2016. Healthy China 2030 blueprint.http://www.gov.cn/xinwen/2016-10/25/content_5124174.htm [Google Scholar]
- 99.Health China Action Promotion Committee . 2019. Healthy China initiative (2019–2030)http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm [Google Scholar]
- 100.Chinese Nutrition Society National nutrition plan (2017−2030) Acta Nutr Sin. 2017;39(4):315–320. [Google Scholar]
- 101.The Chinese Nutrition Society National nutrition week. http://en.cnsoc.org/NNweek/
- 102.Australian Government. Department of Health and Aged Care . 2016. Healthy food partnership.https://www.health.gov.au/our-work/healthy-food-partnership [Google Scholar]
- 103.Australian Government. Department of Health and Aged Care . 2018. Health star rating system.http://www.healthstarrating.gov.au/internet/healthstarrating/publishing.nsf/content/home [Google Scholar]
- 104.Australian Government. Department of Health and Aged Care . 2014. National healthy school canteens – guidelines for healthy foods and drinks supplied in school canteens.https://www.health.gov.au/resources/publications/national-healthy-school-canteens-guidelines-for-healthy-foods-and-drinks-supplied-in-school-canteens?language=en [Google Scholar]
- 105.Branca F., Lartey A., Oenema S., et al. Transforming the food system to fight non-communicable diseases. BMJ. 2019;364:l296. doi: 10.1136/bmj.l296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Global Panel on Agriculture and Food Systems for Nutrition . 2016. Food systems and diets: facing the challenges of the 21st century.http://glopan.org/sites/default/files/ForesightReport.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.