Abstract
Background
Biceps tenodesis is a common treatment for pathologies involving the long head of the biceps brachii. Given variations in surgical approach, focus has been placed on the location of the tenodesis to maintain appropriate length-tension relationship. The purpose of this study is to assess for variations in the tunnel placement in subpectoral biceps tenodesis procedures and correlation of tunnel position with patient-reported outcomes.
Methods
This is a retrospective case series of outcomes as a function of tunnel location with open subpectoralis biceps tenodesis. The location of the biceps tenodesis tunnel was measured on postoperative Grashey radiographs. Correlation between the tenodesis tunnel and postoperative American Shoulder and Elbow Surgeons (ASES) score and Visual Analog Scale (VAS) was assessed.
Results
31 patients were included in the study with an average follow-up of 17 months. The overall tunnel position from the superior edge of the greater tuberosity ranged from 4.20 cm to 12.61 cm, with an average of 7.46 cm. Final ASES score and VAS were 84.5 and 1.2, respectively. There was only weak correlation between both ASES score and tunnel position (r = −0.12) and VAS and tunnel position (r = −0.23).
Discussion
Subpectoralis biceps tenodesis continues to be a viable treatment option for biceps and superior labral pathology. There remains no consensus on tenodesis location, and this study found no significant difference between tunnel location and patient-reported outcomes. Therefore, it is likely that a range of tenodesis locations exists in which favorable clinical results are achieved, explaining the numerous recommendations on tunnel placement.
Keywords: Biceps tenodesis, Subpectoral biceps tenodesis, Tenodesis tunnel, Patient-reported outcomes, Shoulder, Long head of biceps
Biceps tenodesis is a common surgical treatment of pathologies of the long head of the biceps.16 Variations in the surgical approach exist, particularly with respect to the location of the tenodesis.15,16 Attention is given to the tenodesis location as it affects tendon length which has potential implications on the tendon length-tension relationship and subsequently pain and function.4 An abundance of literature exists on suprapectoral and subpectoral biceps tenodesis locations and fixation techniques, supporting the use of either approach in achieving reliable outcomes.7,8,13 A 2020 meta-analysis comparing both approaches showed that both locations had favorable and comparable results.4
Despite recognizing the importance of the biceps tenodesis location, to the best of our knowledge, there are no studies assessing the tunnel location within each group. With respect to subpectoral biceps tenodesis, there are multiple conflicting recommendations on the ideal location for placement of the tenodesis tunnel. Most commonly, the tenodesis is recommended to be placed immediately (or approximately 1 cm) proximal to the inferior border of the pectoralis major tendon. Other recommendations include placing the tunnel as far proximal as the pectoralis major tendon will allow while others place the tunnel in a location that attempts to return the musculotendinous junction to its native location.3,9,10,12,14,17 Nonetheless, it is not apparent if the location of the tenodesis tunnel in the subpectoral approach affects outcomes. Therefore, this study was conducted to assess for variations in the tunnel placement in subpectoral biceps tenodesis procedures and correlation of tunnel position with patient-reported outcomes.
Materials and methods
This is a retrospective case series of patients who underwent open subpectoralis biceps tenodesis over a 3-year period. Surgical indications included failure of conservative treatment for biceps labral complex injuries including biceps tenosynotivitis, biceps tendon tears, and unstable superior labral tears. Exclusion criteria were follow-up less than 6 months and concurrent procedures such as rotator cuff repair, lysis of adhesions, labral repair, or capsulorrhaphy. Institutional review board approval was granted.
For this approach, the patient’s arm is placed at approximately 30 degrees of abduction and external rotation. The inferior portion of the pectoralis major tendon in palpated and a 2-3 cm incision is made on the anteromedial aspect of the proximal humerus. Blunt dissection is used to again identify the inferior portion of the pectoralis major tendon and the biceps running deep to it. The long head of the biceps tendon will consistently be located traversing superiorly into the bicipital groove and can be delivered into the operative field by use of surgeon’s finger or a right angle clamp. Tenodesis site is then identified and is ideally in line with the bicipital groove and approximately 1 cm proximal to the distal insertion of the pectoralis major tendon.19 Techniques for securing the tendon is surgeon specific. In the present study, we included patients from three surgeons. For surgeons A and B, the tunnel is typically drilled to 6 mm and the tendon is secured with an Arthrex biceps button (Arthrex, Naples, FL, USA). For surgeon C, the tunnel is drilled to 8 mm and the tendon is secured with an Arthrex biotenodesis screw (Arthrex, FL, USA).
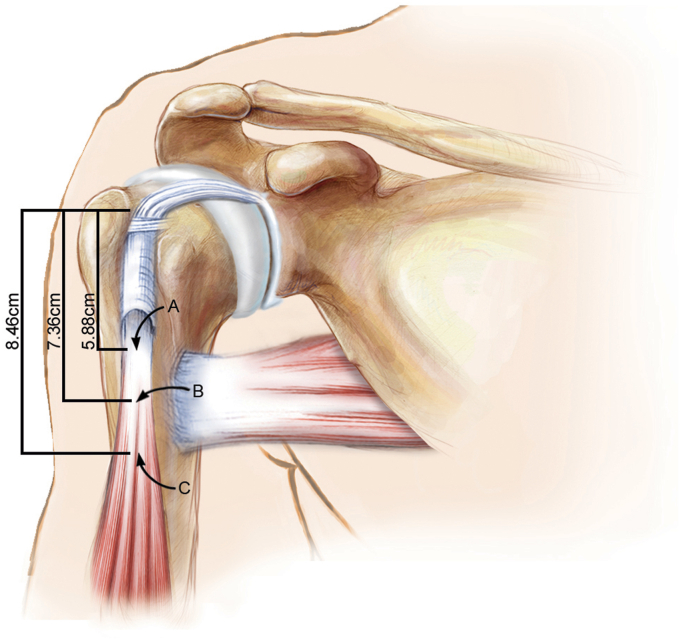
The location of the biceps tenodesis tunnel was measured on postoperative Grashey radiographs (Fig. 1) taken in a standard fashion to allow for comparisons of measurements. Measurements were conducted via our digital picture archiving and communication system as previously described.10 The distance from the superior aspect of the tenodesis tunnel to the superolateral portion of the greater tuberosity was determined in parallel to the longitudinal axis of the humerus. Patient outcomes were assessed by the American Shoulder and Elbow Surgeons (ASES) score and the Visual Analog Scale (VAS), determined preoperatively and postoperatively at the final follow-up.
Figure 1.
Variations in the tunnel position by each surgeon.
Patients were stratified by one of three surgeons that performed the procedure. The average tunnel position of each surgeon was calculated, and an analysis of variance was calculated to assess for a difference in positions among the surgeons. In addition, a Pearson’s correlation test was performed to evaluate whether the tenodesis tunnel locations was correlated with the ASES score or VAS. Statistical analyses were conducted via SPSS (IBM Corp., Armonk, NY, USA), and P values ≤ .05 were deemed statistically significant.
Results
The study included 31 patients (9 females and 22 males) with an average age of 45.8 years ± 11.1 years. Average follow-up was 17 months, with a minimum follow-up of 10 months. No complications such as humeral fracture, neurovascular injury, or infections occurred. The mean ASES improved by 39 points, from 45.5 to 85.5 (P < .0001), and average VAS improved from 4.7 to 1.2 (P < .0001).
The surgeries were performed by three surgeons, with 9 shoulders from surgeon A, 7 from surgeon B, and 15 from surgeon C. The overall tunnel position from the top edge of the tuberosity ranged from 4.20 cm to 12.61 cm, with an average of 7.46 cm. The tunnel position varied among the 3 surgeons, with average placement of 5.88 cm, 7.36 cm, and 8.46 cm from the superolateral portion of the greater tuberosity (P = .0036) (Fig. 2). Even within each surgeon’s cohort, variations in tunnel placement existed. The ranges of each surgeon were 4 cm, 5.1 cm, and 6.9 cm (Fig. 4).
Figure 2.
Average locations of biceps tenodesis tunnel by surgeon.
Figure 4.
American Shoulder and Elbow Surgeons Shoulder score as a function of tunnel position. Each blue circle is a patient's American Shoulder and Elbow Surgeons Shoulder score and tunnel position.
Fig. 3 demonstrates ASES as a function of tunnel position. There was weak correlation between final ASES and tunnel position (r = −0.12), with a P value of 0.54. To achieve statistical significance for such a correlation, 542 subjects are needed. Furthermore, even if statistical significance was reached, then the tunnel position would explain 1.44% of the variance in ASES, which is not clinically significant. Similarly, correlation between final VAS and tunnel position was weak (r = −0.23, P = .25).
Figure 3.
Variations in the tunnel position by each surgeon. The blue circle is the average tunnel position for each surgeon.
Discussion
Subpectoralis biceps tenodesis a viable option to treat pathology of the biceps and superior labrum.16 However, the exact location of the tunnel can be difficult to obtain depending on the goal location, with no consensus on the target location and whether it impacts surgical outcomes. Mazzocca et al and Provencher et al recommended placing the tunnel 1 cm proximal to the inferior border of the pectoralis major tendon.14,17 Denard et al3 recommended placing the tendon just proximal to most inferior aspect of the inferior border of the pectoralis major tendon. Johannsen et al10 have recommended placing the tunnel as far proximal as allowed by the pectoralis major tendon. Others have recommended that the tendon be positioned on the basis of placing the musculotendinous junction at its native location.9,12 Two techniques have been described to achieve this goal.9,12 The first is to place the tendon so that the musculotendinous junction is 3 cm distal to the inferior border to the pectoralis major tendon.12 The other is to place the tendon so that the musculotendinous junction is 2 cm distal from the proximal pectoralis insertion.9 In the present study, a large range in tunnel locations was found. While the 3 surgeons strived to obtain the same location for the tenodesis tunnel, there was a considerable variation, including locations from 4.20 cm to 12.61 cm from the superolateral portion of the greater tuberosity. The range of location represented in this study incorporates the majority of the recommended locations in the literature.3,9,10,12,14,17 One of the surgeons had an average tunnel placement of 5.88 cm, similar to a previous study on open subpectoral biceps tenodesis reporting tunnel placement of 5.43 cm.10 Nonetheless, this is different than the 7.36 cm and 8.46 cm by the other surgeons in this study.
As all the surgeons strived to place the tendon superior to the inferior border of the pectorialis major or as far superior into the bicipital grove as possible, there could be several reasons for this large range of locations. One possibility was the size of the patient’s pectoralis and the amount of abduction the arm was placed in to obtain exposure could make the pectoralis tendon more difficult to retract. Additionally, while the average distance to the inferior boarder is 7.5 cm from the top of the humeral head, there is some variability.6,11 These would lead to the position of the tunnel being variable in regards to radiographic landmarks but not in respects to the pectoralis. Further, a systematic review of 201 articles found that both the insertion as well as the number of layers of the sternal portion of the pectoralis major have been reported inconsistently and that these inconsistencies have made their way into numerous articles and clinical diagnoses.4
This study found no clinical difference between the location of the bicep tenodesis tunnel and clinical outcomes. The final ASES scores achieved in this case series are comparable to previously reported results of subpectoral biceps tenodesis which range from 82.3 to 92.3 for subpectoral biceps tenodesis, and there was no association between tunnel location and final ASES scores.4 Therefore, it is likely that there exists a range of tenodesis locations that yield equal clinical results, explaining the numerous recommendations on tunnel placement.
Several studies also have reported equal results of the subpectoralis biceps tenodesis compared to suprapectoralis biceps tenodesis.4,7,8,13 In his editorial commentary, Dr. Paul Brady elaborates on the notion that while controversy exists regarding the ideal tenodesis location regarding suprapectoral vs. subpectroal tenodesis, “biceps tenodesis location may not matter.1 The current study allows greater generalizability of the comparisons of subpectoral and suprapectoral biceps tenodesis by lessening the importance of the performed location in the subpectoral group. Future studies can analyze whether the same is true within the suprapectoral group.
The finding of this study should be taken with some precaution. There have been case reports of humeral fractures after biceps tenodesis placement in the metaphysis.2,18 Additionally, one should be cautious of the radial nerve when using a bicortical device.5 Dickens et al described the radial nerve as being 16.6 mm deep and 14.5 mm medial from the tenodesis site when the tenodesis tunnel was located 1 cm proximal to the inferior border of the pectoralis major and centered in the inferior aspect of the bicipital groove.13 As the tenodesis tunnel is moved more distally, the radial nerve becomes closer to the tunnel posteriorly. While neither fractures nor radial nerve injuries were seen in our study, they remain important considerations.
This study has several limitations. While this is a novel study comparing clinical outcome measurements with subpectoral biceps tenodesis tunnel location, it is retrospective study with short term follow-up. Furthermore, radiographic evaluation was used to determine the tenodesis tunnel placement. While this has been shown to be correlated with anatomical landmarks, patient factors might affect the anatomy, and the exact relationship of the tunnel location relative to the pectoralis major tendon were not determined.10 A computed tomography scan would have aided in reducing possible measurement error and will be utilized in future studies. Finally, patients with concurrent procedures were excluded from the study. Although the rationale behind this was to minimize confounders, many patients require additional procedures, and there could be a more complex interplay with additional procedures. Additional prospective, long term studies are needed to verify the results of the current study and increase its generalizability. Any follow-up studies examining this topic should include a larger cohort of patients with a variety of pathologies other than those involving the biceps tendon to ensure it is adequately powered. Including patient-reported outcomes such as pain and esthetics including the pop-eye deformity would further strengthen the effect of this study, and these factors will be recorded and analyzed in any follow-up studies on this subject.
Conclusion
There are multiple recommendations in the literature as to the ideal location of the biceps tenodesis tunnel. However, this is likely a result of the large range of acceptable locations. Our results showed that variations existed not only among surgeons but within each surgeon and that these variations did not affect patient outcomes.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: Brent A. Ponce receives royalties from Stryker/Wright/Tornier, is a consultant at Stryker/Wright/Tornier, is a consultant at Smith & Nephew, and is a consultant at ODi (Orthopedic Designs North America Incorporated). All the other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
This study was approved by Hughston Sports Medicine Center Institutional Review Board: HIRB2016-12.
References
- 1.Brady P. Editorial commentary: biceps tenodesis location may not matter: go high…go low…go wherever you want to go! Arthroscopy. 2020;36(12):2982–2983. doi: 10.1016/j.arthro.2020.09.026. [DOI] [PubMed] [Google Scholar]
- 2.Dein E.J., Huri G., Gordon J.C., McFarland E.G. A humerus fracture in a Baseball Pitcher after biceps tenodesis. Am J Sports Med. 2014;42:877–879. doi: 10.1177/0363546513519218. [DOI] [PubMed] [Google Scholar]
- 3.Denard P.J., Dai X., Hanypsiak B.T., Burkhart S.S. Anatomy of the biceps tendon: implications for restoring physiological length-tension relation during biceps tenodesis with Interference screw fixation. Arthrosc J Arthrosc Relat Surg. 2012;28:1352–1358. doi: 10.1016/j.arthro.2012.04.143. [DOI] [PubMed] [Google Scholar]
- 4.van Deurzen D.F.P., Gurnani N., Alta T.D.W., Willems J.H., Onstenk R., van den Bekerom M.P.J. Suprapectoral versus subpectoral tenodesis for long head biceps brachii tendinopathy: a systematic review and meta-analysis. Orthop Traumatol Surg Res. 2020;106:693–700. doi: 10.1016/j.otsr.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Dickens J.F., Kilcoyne K.G., Tintle S.M., Giuliani J., Schaefer R.A., Rue J.-P. Subpectoral biceps tenodesis an anatomic study and evaluation of at-risk structures. Am J Sports Med. 2012;40:2337–2341. doi: 10.1177/0363546512457654. [DOI] [PubMed] [Google Scholar]
- 6.de Figueiredo E.A., Terra B.B., Cohen C., Monteiro G.C., de Castro Pochini A., Andreoli C.V., et al. The pectoralis major footprint: an anatomical study. Rev Bras Ortop Engl Ed. 2013;48:519–523. doi: 10.1016/j.rboe.2013.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gombera M.M., Kahlenberg C.A., Nair R., Saltzman M.D., Terry M.A. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43:1077–1083. doi: 10.1177/0363546515570024. [DOI] [PubMed] [Google Scholar]
- 8.Green J.M., Getelman M.H., Snyder S.J., Burns J.P. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii without the use of interference screws. Arthroscopy. 2017;33:19–25. doi: 10.1016/j.arthro.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Jarrett C.D., McClelland W.B., Xerogeanes J.W. Minimally invasive proximal biceps tenodesis: an anatomical study for optimal placement and safe surgical technique. J Shoulder Elbow Surg. 2011;20:477–480. doi: 10.1016/j.jse.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Johannsen A.M., Macalena J.A., Carson E.W., Tompkins M. Anatomic and radiographic comparison of arthroscopic suprapectoral and open subpectoral biceps tenodesis sites. Am J Sports Med. 2013;41:2919–2924. doi: 10.1177/0363546513503812. [DOI] [PubMed] [Google Scholar]
- 11.Klepps S., Auerbach J., Calhon O., Lin J., Cleeman E., Flatow E. A cadaveric study on the anatomy of the deltoid insertion and its relationship to the deltopectoral approach to the proximal humerus. J Shoulder Elbow Surg. 2004;13:322–327. doi: 10.1016/j.jse.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 12.LaFrance R., Madsen W., Yaseen Z., Giordano B., Maloney M., Voloshin I. Relevant anatomic landmarks and measurements for biceps tenodesis. Am J Sports Med. 2013;41:1395–1399. doi: 10.1177/0363546513482297. [DOI] [PubMed] [Google Scholar]
- 13.Mardani-Kivi M., Keyhani S., Ebrahim-Zadeh M.H., Hashemi-Motlagh K., Saheb-Ekhtiari K. Rotator cuff tear with concomitant long head of biceps tendon (LHBT) degeneration: what is the preferred choice? Open subpectoral versus arthroscopic intraarticular tenodesis. J Orthop Traumatol. 2019;20:26. doi: 10.1186/s10195-019-0531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazzocca A.D., Cote M.P., Arciero C.L., Romeo A.A., Arciero R.A. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36:1922–1929. doi: 10.1177/0363546508318192. [DOI] [PubMed] [Google Scholar]
- 15.McCrum C.L., Alluri R.K., Batech M., Mirzayan R. Complications of biceps tenodesis based on location, fixation, and indication: a review of 1526 shoulders. J Shoulder Elbow Surg. 2019;28:461–469. doi: 10.1016/j.jse.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Nho S.J., Strauss E.J., Lenart B.A., Provencher M.T., Mazzocca A.D., Verma N.N., et al. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18:645–656. doi: 10.5435/00124635-201011000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Provencher M.T., LeClere L.E., Romeo A.A. Subpectoral biceps tenodesis. Sports Med Arthrosc Rev. 2008;16:170–176. doi: 10.1097/JSA.0b013e3181824edf. [DOI] [PubMed] [Google Scholar]
- 18.Reiff S.N., Nho S.J., Romeo A.A. Proximal humerus fracture after keyhole biceps tenodesis. Am J Orthop (Belle Mead NJ) 2010;39:E61–E63. [PubMed] [Google Scholar]
- 19.Scully W.F., Wilson D.J., Grassbaugh J.A., Branstetter J.G., Marchant B.G., Arrington E.D. A simple surgical technique for subpectoral biceps tenodesis using a double-loaded suture anchor. Arthrosc Tech. 2013;2:e191–e196. doi: 10.1016/j.eats.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]