Abstract
Background
Clavicle fractures are among the most common upper limb fractures in adults, with the midshaft region being the most frequently affected site. Minimally invasive plate osteosynthesis (MIPO) has emerged as an alternative to the traditional open reduction and internal fixation (ORIF) technique, offering potential advantages. The purpose of this study was to conduct a systematic review to explore the results of this technique in the existing literature, with emphasis on the occurrence of surgical complications and functional outcomes and also to provide a comprehensive comparison of MIPO and ORIF in the management of midshaft clavicle fractures.
Methods
We conducted a systematic review to evaluate the complication incidence and clinical outcomes of MIPO for midshaft clavicle fractures. We searched PubMed/Medical Literature Analysis and Retrieval System Online (MEDLINE), Scopus, the Cochrane Database of Controlled Trials, and the Cochrane Database of Systematic Reviews databases without language or date restrictions. Studies focusing on midshaft clavicle fractures treated with MIPO were included, while other clavicle fractures and nonclinical studies were excluded. The risk of bias was assessed using the Methodological Index for Nonrandomized Studies criteria and the Risk of Bias Tool 2 Cochrane tool. Data synthesis included qualitative analysis, and if applicable, quantitative analysis and meta-analysis. Adherence to Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines ensured reporting quality.
Results
A total of 107 studies were initially identified, after applying inclusion and exclusion criteria, 22 studies were included for data extraction. These studies involved the evaluation of 714 clavicles treated with the MIPO technique. Of the 714 MIPO cases, 11 cases of implant failure, 5 nonunions, 2 infections, and 28 cases with neurological impairment were observed. Quantitative analysis comparing MIPO with ORIF revealed that MIPO had significantly shorter surgery time (mean difference −12.95, 95% confidence interval [−25.27 to −0.63], P = .04) and lower occurrence of numbness (odds ratio 0.29, 95% CI [0.15-0.56], P = .0002) compared to ORIF. Time to bone union, functional outcomes, and other complications were similar between MIPO and ORIF at the final follow-up. An overall moderate risk of bias was found across the studies.
Conclusion
The MIPO technique yields good and comparable results to ORIF for midshaft clavicle fractures. Additionally, the MIPO technique may offer advantages such as reduced surgical time and lower chances of neurological impairment.
Keywords: Minimally invasive plate osteosynthesis, MIPO, Midshaft clavicle fractures, Surgical treatment, Clinical outcomes, Comparative analysis, Systematic review
Fractures of the midshaft of the clavicle are among the most commonly encountered injuries on the upper extremity, accounting for 75% of all clavicle fractures.12 The management of midshaft clavicle fractures has historically been nonoperative;31 however, a significant shift in the treatment approach has occurred, with a growing emphasis on surgical interventions, especially open reduction and internal fixation (ORIF).7 This approach yields more predictable results in cases of highly displaced fractures,2 albeit with potential complications related to surgical morbidity, implant failure, and wound-related complications.18,25,37
The recognition of complications in the conventional plate ORIF technique has led to the development of alternative surgical techniques, including various nailing methods.
Another surgical technique that has gained attention in recent years is the minimally invasive plate osteosynthesis (MIPO) technique. The MIPO technique involves the use of smaller incisions and the insertion of a low-profile plate along the length of the clavicle, spanning the fracture site and providing stable fixation. This approach offers the potential benefits of reduced soft tissue disruption, lower rates of skin numbness, minimized damage to the periosteal blood supply, and a lower risk of infection or implant-related complications.25,37
Despite the growing adoption and study of the MIPO technique for midshaft clavicle fractures, only one other systematic review to our knowledge specifically evaluated its outcomes and compared it with the ORIF technique,37 and none other was published in the past four years, while a considerable number of related articles have been reported since. With this study, we aim to fill this gap in updating the knowledge by evaluating the surgical procedure time, effectiveness, and complication incidence of the MIPO technique for midshaft clavicle fractures across the existing studies. We hypothesized that the MIPO technique would demonstrate equivalent clinical outcomes (assessed by functional scores), equivalent time to bone union, lower surgical procedure time, and lower complication rates (infection, implant failure, nonunion, and paresthesia) when compared to the ORIF surgical technique.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.20
Eligibility criteria
Studies reporting original data on the use of the MIPO technique for the treatment of patients with midshaft clavicle fractures were targeted for this study. The surgical fixation of clavicle fractures through multiple (>1) smaller incisions, employing the bridge plating technique, was classified as MIPO. No other restrictions to MIPO technique variation were applied. Studies reporting on clavicle fractures of other anatomical sections than midshaft and treated exclusively with other surgical techniques were excluded. No restrictions were applied in terms of the type of functional outcome assessed or the type of complications reported. We excluded scoping and systematic reviews, technical notes, letters to the editor, and nonclinical studies such as anatomical and biomechanical studies. There were no other restrictions to study designs. Only studies in English were included. The inclusion and exclusion criteria for this study are summarized in Table I.
Table I.
Inclusion and exclusion criteria of the targeted studies.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Clinical trials, cross-sectional studies, and case series reporting original data. | Biomechanical, cadaveric studies, systematic reviews, technical notes, and review articles. |
| Reporting of MIPO techniques. | Reporting solely other treatment techniques (e.g. conservative, ORIF) |
| Included patients with midshaft clavicle fractures | Included patients with fractures on different sites of the clavicle (lateral or medial third). |
Information source and search strategy
Before the initial search, registration of the systematic review with the International Prospective Register of Systematic Reviews was completed (CRD42021262433). A comprehensive literature search was developed by the authors and was run by an experienced medical librarian on 18th January 2023 in the following databases: PubMed/MEDLINE, Scopus, Cochrane Database of Controlled Trials and the Cochrane Database of Systematic Reviews. Both controlled vocabularies (e.g. MeSH terms) and keywords were searched. There were no restrictions on geography, age of participants, or language of publication. Additionally, a hand search was conducted of the reference lists of selected articles.
All identified studies were exported to reference management software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia) to remove duplicates and organize the studies for screening. Two reviewers (V.L.B. and A.P.V.) independently screened the studies for eligibility based on the title and abstract, and full-text articles were retrieved for studies that met the eligibility criteria. Disagreements between reviewers were resolved by a third independent reviewer (G.V.L.), as suggested by the reporting guidelines for meta-analysis PRISMA.20
Data extraction
Specific information on study design, methods, patient demographics, interventions, and outcomes was collected, accordingly to the Cochrane Handbook for Systematic Reviews of Interventions5 recommendations. Two authors (V.L.B. and A.P.V.) independently extracted data from the included studies using a standardized data extraction form. A third author (H.L.S.) reviewed the extracted data and decided on conflicts when present. We extracted outcomes if they were present in two or more of the studies included. Outcomes that were not consistently reported in at least two studies were not evaluated. The following outcomes data were extracted from each study: (1) Surgical time in minutes; (2) Time to radiographic bone union in weeks; (3) Implant failure or loosening; (4) nonunion; (5) superficial or deep infection; (6) paresthesia or sensitivity impairment; (7) Constant Murley score4; (8) Disabilities of the Arm, Shoulder and Hand (DASH) score11; (9) Quick-DASH (q-DASH) score22; and (10) surgical technique used as a comparison when present. All of the functional scores (Constant, DASH, Q-DASH) were collected at the final follow-up, as we predicted that intermediate time point evaluations would vary across the studies.
Additionally, patient's age, positioning of the patient (beach chair or supine), number of incisions, reduction method, type of implant used, and time of follow-up were extracted when available.
Study risk of bias
The Methodological Index for Nonrandomized Studies (MINORS)23 criteria was utilized to objectively score the quality of each study. According to these criteria, comparative studies had a maximum possible score of 24, whereas noncomparative studies had a maximum score of 16. Higher scores indicated a lower risk of bias. The Cochrane Risk of Bias Tool 229 was employed for the assessment of the risk of bias in the included clinical trials, and the overall risk of bias was graded as high, somewhat concerning, or low. Risk Of Bias In Nonrandomized Studies—of Interventions28 tool for nonrandomized experimental studies. Two authors independently evaluated the included articles for risk of bias (A.P.V. and F.L.G.) and conflicts were decided by a third independent author (V.L.B.)
Effect measures
Continuous data such as time to bone union (in weeks) and surgical time (in minutes) were evaluated by the mean difference between the MIPO technique and alternative surgical treatments. Risk ratios (RRs) were calculated to determine the relative risk of complications such as implant failure or loosening, nonunion, superficial or deep infection, and numbness associated with the MIPO technique compared to other evaluated treatments. Finally, functional scores, including the Constant Murley score, the DASH score, and the q-DASH score were assessed by calculating the mean difference between treatments at the final follow-up.
Synthesis methods
All selected studies were included in the descriptive analysis regarding patient demographics and surgical technique employed (positioning, number of incisions, reduction methods and types of implants) for the MIPO technique. The incidence of complications associated with the MIPO technique was also analyzed descriptively. For the outcomes of “Time to bone union” and “Follow-up” time was converted into weeks and months, respectively, to ensure consistency across the studies. When in a study with a comparison group, an outcome of interest wasn’t available, this study was not included in the analysis.
The assessment of heterogeneity was made accordingly to the recommendations outlined in the Cochrane Handbook for Systematic Reviews of Interventions.8 Heterogeneity among the included studies was evaluated using the Chi-square and I2 statistic tests. According to the Cochrane guidelines, heterogeneity levels below 40% may be considered unimportant, while levels between 30% and 60% suggest moderate heterogeneity, 50%-90% indicate substantial heterogeneity and above 75% considerable heterogeneity. Funnel plots were employed for assessing publication bias, detecting potential asymmetry in the plot, publication bias and other sources of small-study effects. Statistical analysis was performed with Review Manager software, version 5.4 (RevMan 5.4; The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark)
Results
Study selection
We identified 107 records on database searching (Pubmed/MEDLINE, Scopus, and Cochrane Database of Controlled Trials and the Cochrane Database of Systematic Reviews). After the removal of duplicates, 64 articles were screened through their titles and/or abstracts.
Considering the eligibility criteria, 32 studies were excluded and 32 were retrieved for full-text screening in more detail and assessed for eligibility. Of those, 10 studies were excluded due to: 6 were not available in English language, 3 were only study protocols without reporting data, and 1 was a systematic review. Twenty-two studies1,3,6,9,10,13, 14, 15, 16, 17,19,21,24,26,27,30,32,33, 34, 35, 36 were included for analysis. A PRISMA flow diagram was used to document the study selection process (Fig. 1).
Figure 1.
PRISMA flow diagram with study selection. PRISMA, preferred reporting items for systematic reviews and meta-analyses.
Study characteristics
Patients
A total of 22 studies1,3,6,9,10,13, 14, 15, 16, 17,19,21,24,26,27,30,32, 33, 34, 35, 36 were included in the analysis, comprising 714 patients who underwent the MIPO technique for midshaft clavicle fractures. Among these studies, 113,9,13, 14, 15,17,25,27,32, 33, 34 compared the MIPO group with other surgical techniques, while the remaining studies did not involve a comparator group. In the comparator studies, a total of 294 patients were operated using alternative surgical methods. The mean patient age across both groups was 40.75 (±8.4) years.
Surgical technique MIPO
Regarding the MIPO surgical technique, among the included studies, 10 reported utilizing the beach chair position,1,3,9,10,14,24,26,33, 34, 35 while 7 studies opted for the supine position for patient positioning during the procedure.6,15, 16, 17,19,30,35 A 2-incision technique was described in 15 articles as the standard approach for plate osteosynthesis,1,3,6,10,13,15, 16, 17,21,26,33, 34, 35 while an additional incision over the fracture site to aid in reduction with a clamp was employed in 4 articles,9,19,30,36 resulting in a 3-incision technique. In terms of reduction methods, traction alone was used in 8 reports,3,14,16,17,21,30,35,36 whereas a joystick maneuver with the assistance of k-wires or pins was employed in 5 reports.6,10,19,24,25 For the fixation of the fracture, a clavicle-specific locking plate was utilized in 15 reports1,3,6,9,10,13, 14, 15, 16,32, 33, 34, 35, 36 while 5 reports mentioned the use of reconstruction plates.19,21,24,26,30
Comparison technique
Eleven studies included a comparison group3,9,13, 14, 15,17,25,27,32, 33, 34 that underwent a different surgical technique for clavicle fracture treatment. Specifically, one study compared the MIPO technique with titanium elastic nail osteosynthesis,3 another study compared it with intramedullary nail fixation,34 while the remaining 9 studies compared the MIPO technique with ORIF using a plate.
Study characteristics can be found in Table II.
Table II.
Individual studies characteristics: MIPO (Minimally Invasive Plate Osteosynthesis); n = Number of clavicles.
| Study | Intervention/ Comparison | Study design | n = | Mean age (y) | Number of incisions in MIPO | Patient positioning | Reduction method | Implant type in MIPO technique | Mean follow-up (mo) |
|---|---|---|---|---|---|---|---|---|---|
| Al Sadek et al 20161 | MIPO | Case Series | 12 | 47.5 | 2 | Beach Chair | n/a | Clavicle Locking Plate | n/a |
| Chen et al 20183 | MIPO | Randomized Clinical trial | 27 | 37.8 | 2 | Beach Chair | Traction | Clavicle Locking Plate | n/a |
| Titanium Elastic Nail | 27 | 39.1 | n/a | ||||||
| Delvaque et al 20196 | MIPO | Retrospective Cohort | 19 | 37 | 2 | Supine | Joystick | Clavicle Locking Plate | 3 |
| - | n/a | ||||||||
| Jiang et al 20129 | MIPO | Randomized Clinical trial | 32 | 40 | 3 | Beach Chair | Incision over fracture | Clavicle Locking Plate | n/a |
| ORIF | 32 | 45 | |||||||
| Jirangkul et al 202210 | MIPO | Case Series | 30 | 42.4 | 2 | Beach Chair | Joystick | Clavicle Locking Plate | 15.86 |
| Kim et al 202013 | MIPO | Retrospective Cohort | 16 | 14.6 | 2 | n/a | n/a | Clavicle Locking Plate | n/a |
| ORIF | 33 | 15.1 | |||||||
| Kim et al 201814 | MIPO | Randomized Clinical trial | 15 | 38.1 | n/a | Beach Chair | Traction | Clavicle Locking Plate | 13.3 |
| ORIF | 15 | 38.1 | 13.7 | ||||||
| Ko et al 202215 | MIPO | Case Control Study | 29 | 48.8 | 2 | Supine | n/a | Clavicle Locking Plate | 12.5 |
| ORIF | 30 | 48.5 | 12.6 | ||||||
| Kundangar et al 201917 | MIPO | Nonrandomized experimental study | 21 | 2 | Supine | Traction | Clavicle Locking Plate | 24 | |
| ORIF | 16 | 24 | |||||||
| Kundangar et al 201816 | MIPO | Case Series | 22 | 36.1 | 2 | Supine | Traction | Clavicle Locking Plate | n/a |
| Lee et al 201318 | MIPO | Case Series | 14 | 42.9 | 2 | Supine | Joystick | Reconstruction Plate | 17.6 |
| Mendes Junior et al 202121 | MIPO | Retrospective Cohort | 32 | 41 | 2 | n/a | Traction | Reconstruction Plate | 12 |
| Sohn et al 201224 | MIPO | Case Series | 19 | 42.3 | n/a | Beach Chair | Joystick | Reconstruction Plate | 13.8 |
| Sohn et al 201525 | MIPO | Retrospective Cohort | 19 | 46.7 | 2 | n/a | Joystick | n/a | n/a |
| ORIF | 14 | 44.1 | n/a | ||||||
| Sohn et al 201226 | MIPO | Case Series | 15 | 42.6 | 2 | Beach Chair | n/a | Reconstruction Plate | 13.9 |
| Sohn et al 201527 | MIPO | Randomized Clinical Trial | 19 | n/a | n/a | n/a | n/a | n/a | |
| ORIF | 18 | n/a | |||||||
| Tieyi et al 201430 | MIPO | Retrospective Cohort | 269 | 40.2 | 2 | Supine | Traction | Reconstruction Plate | 40.6 |
| - | 12 | ||||||||
| You et al 201832 | MIPO | Nonrandomized experimental study | 38 | 38.3 | 3 | n/a | Incision over fracture | Clavicle Locking Plate | 12 |
| ORIF | 35 | 36.9 | 12 | ||||||
| Zehir et al 201833 | MIPO | Retrospective Cohort | 22 | 32.3 | 3 | Beach Chair | Incision over fracture | Clavicle Locking Plate | 14.57 |
| ORIF | 30 | 34.7 | 16.50 | ||||||
| Zehir et al 201534 | MIPO | Randomized Clinical Trial | 21 | 32.4 | 3 | Beach Chair | Incision over fracture | Clavicle Locking Plate | 14.4 |
| MIPO w.Nail | 24 | 33.7 | 11.8 | ||||||
| Zhang et al 201735 | MIPO | Case Series | 27 | 32.6 | 2 | Supine | Traction | Clavicle Locking Plate | 15.8 |
| Zhang et al 201636 | MIPO | Case Series | 15 | 48.3 | 2 | Beach Chair | Traction | Clavicle Locking Plate | 16.5 |
Risk of bias in individual studies
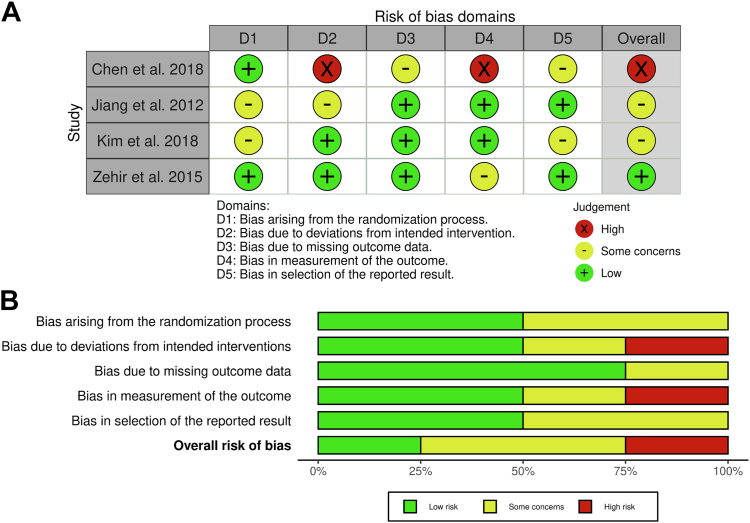
The risk of bias in the included studies was evaluated using the Methodological Index for Nonrandomized Studies) criteria. Among the studies without a comparator group, the mean score was 7.72 out of 16, the studies with a comparator group had a higher mean score of 16.2 out of 24 (Table III). Risk of bias in the randomized controlled trials was evaluated using the Risk of Bias Tool 2 tool (Fig. 2, A and B) and ROBINS-I tool (Fig. 3, A and B) for nonrandomized experimental studies. The assessment of the evaluated studies indicated an overall high to moderate risk of bias, with only 1 study demonstrating an overall low risk of bias.
Table III.
MINORS criteria for assessment of risk of bias. Scores graded as (0) not reported, (1) reported, but inadequately (2) reported and adequate.
| Al Sadek et al1 2016 | Delvaque et al6 2019 | Jirangkul et al10 2022 | Kim et al13 2020 | Ko et al15 2022 | Kundangar et al16 2018 | Lee et al19 2013 | Mendes Junior et al21 2021 | Sohn et al26 2012 | Sohn et al27 2015 | Sohn et al24 2013 | Sohn et al25 2015 | Tieyi et al30 2014 | Zehir et al33 2018 | Zhang et al35 2017 | Zhang et al36 2016 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A clearly stated aim | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 2 |
| Inclusion of consecutive samples | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 2 | 1 | 0 | 0 | 0 | 2 |
| Prospective collection | 0 | 0 | 2 | 1 | 0 | 2 | 2 | 1 | 0 | 2 | 2 | 2 | 0 | 0 | 2 | 2 |
| Endpoint appropriated to the study aim | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 |
| Unbiased evaluation of endpoints | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 |
| Follow-up appropriate to the endpoint | 0 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 1 |
| Loss to follow-up less than 50% | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 |
| Prospective Calculation of Sample Size | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| Additional criteria in case of comparative study | ||||||||||||||||
| An adequate control group | 2 | 2 | 2 | 2 | 2 | |||||||||||
| Contemporary groups | 0 | 2 | 0 | 2 | 0 | |||||||||||
| Baseline equivalence groups | 1 | 2 | 2 | 1 | 2 | |||||||||||
| Adequate statistical analysis | 2 | 2 | 2 | 1 | 2 | |||||||||||
| Total | 4 | 9 | 10 | 13 | 16 | 10 | 8 | 6 | 7 | 17 | 10 | 20 | 5 | 15 | 6 | 10 |
MINORS, methodological index for non randomized studies.
Figure 2.
(A and B): Risk of bias assessment by the RoB2 tool. RoB2, risk of bias 2.
Figure 3.
(A and B): Risk of bias assessment by the ROBINS-I tool. ROBINS-I, risk of bias in nonrandomized studies of interventions.
Synthesis of results
One study25 was excluded from the synthesis as it was published by the same author,27 in the same year and with a very similar cohort (similar demographic value) to another study included, leading us to believe that they represent the same group of patients. Studies that compared MIPO with different procedures were excluded from the meta-analysis3,33 as we aimed to compare with the ORIF procedure.
Surgical time
In the analysis of surgical time, data from 6 studies9,13,15,16 were included. The results indicated that the MIPO group had significantly shorter surgery times compared to the ORIF group (Mean diff −12.95, 95% CI: −25.27 to −0.63; P = .04) (Fig. 4) .
Figure 4.
Surgical time compared between MIPO and ORIF groups.
Time to bone union
Seven studies9,13, 14, 15, 16,27,33 reported on the time to union as an outcome measure of comparison. The analysis comparing the MIPO group with the comparison group revealed no significant difference in the time to union between the 2 groups. (Mean diff −1.47, 95% CI: −3.15 to 0.22; P = .09) (Fig. 5)
Figure 5.
Time to union compared between MIPO and ORIF groups. MIPO, minimally invasive plate osteosynthesis; ORIF, open reduction and internal fixation; CI, confidence interval.
Complications
Complications were reported by 8 studies.9,13, 14, 15, 16, 17,27,33 The results indicated a significantly lower risk of numbness in the MIPO technique group when compared to the comparison procedures (OR 0.29; CI 95% 0.15-0.56; P = .0002) (Fig. 6, A). The analysis did not reveal any significantly increased risk between the techniques in terms of infection, implant failure, and nonunion rates. (Fig. 6, B-D)
Figure 6.
(A): Paresthesia compared between MIPO and ORIF groups. (B): Infection compared between MIPO and ORIF groups. (C): Nonunion compared between MIPO and ORIF groups. (D): Implant failure compared between MIPO and ORIF groups. MIPO, minimally invasive plate osteosynthesis; ORIF, open reduction and internal fixation; CI, confidence interval.
Functional scores
Regarding the functional scores, 2 studies17,33 utilized the q-DASH assessment. The mean differences in q-DASH scores between the MIPO group and the comparison group were found to be nonsignificant (Fig. 7, A). Similarly, among the 2 studies that used the DASH score13,32 no significant mean differences were observed (Fig. 7, B). The Constant scores, assessed by 6 studies,13,14,17,25,27,32 also did not show any significant differences (Mean diff: 0.15; CI 95%: −1.71 to 2.00; P = .88) between the MIPO technique and the comparison procedures (Fig. 7, C).
Figure 7.
(A): q-DASH compared between MIPO and ORIF group. (B): DASH compared between MIPO and ORIF groups. (C): Constant compared between MIPO and ORIF groups. q-DASH, quick disabilities of the arm shoulder and hand score; DASH, disabilities of the arm shoulder and hand score; MIPO, minimally invasive plate osteosynthesis; ORIF, open reduction and internal fixation; CI, confidence interval.
Risk of bias across studies
There was no clear evidence of reporting bias; the studies included in the quantitative analysis had similar sample sizes and standard deviations. There was no clear evidence of different proportions of larger studies showing either positive or negative differences.
However, this analysis is limited because of the inclusion of only up to eight studies in the meta-analysis.
Additional analysis
One study25 was excluded from the synthesis of surgical time, time to bone union and complications as it was published by the same author,27 in the same year and with a very similar cohort (similar demographic value) to another study included, leading us to believe that they represent the same group of patients. To verify if the inclusion of the study would affect the results we implemented a sensitivity analysis for the outcomes of paresthesia, infection, bone nonunion, and implant failure (Fig. 8, A-D).
Figure 8.
(A): Sensitivity analysis including the study by Sohn et al6 in the comparison of paresthesia between MIPO and ORIF groups. (B): Sensitivity analysis including the study by Sohn et al6 in the comparison of infection between MIPO and ORIF groups. (C): Sensitivity analysis including the study by Sohn et al6 in the comparison of bone nonunion between MIPO and ORIF groups. (D): Sensitivity analysis including the study by Sohn et al6 in the comparison of implant failure between MIPO and ORIF groups. MIPO, minimally invasive plate osteosynthesis; ORIF, open reduction and internal fixation; CI, confidence interval.
It was observed that adding the mentioned study did not affect the direction of the difference between groups. Other analyses such as subgroup or meta-regression were not performed.
Discussion
In this review, we were able to observe some relevant characteristics of the MIPO technique for midshaft clavicle fracture treatment. In our review, most of the studies reportedly used a beach chair positioning, with 2 incisions technique. Most commonly, traction was used for reduction, and a clavicle-contoured locked plate was used.
In the broader context of existing evidence, our study provides valuable insights into the comparison between the MIPO technique and ORIF for midshaft clavicle fractures. A previous systematic review37 focused on MIPO vs. ORIF studies for midshaft clavicle fractures reported a significant reduction in overall complications in the MIPO group, similar to our findings. However, it analyzed all complications without separately evaluating each complication risk. Our findings align with the previous review in demonstrating a significant reduction in numbness incidence with the MIPO technique compared to ORIF; however, we did not observe significant differences in other complications such as implant loosening, infection, and nonunion suggesting that while MIPO may offer advantages in terms of reduced numbness, these benefits may not extend uniformly across all complications. Notably, our study revealed a significant reduction in surgical time with the MIPO technique, which contrasts with the previous review's findings which did not observe differences in surgical time.37 We attribute this discrepancy to variations in study inclusion criteria or differences in the specific populations and surgical techniques evaluated. Furthermore, our analysis showed no significant differences in functional scores between the MIPO and ORIF groups suggesting that the long-term functional outcomes are equivalent between the different surgical approaches.
It is important to acknowledge limitations within the evidence included. One notable limitation is the overall moderate risk of bias observed across the observational, experimental, and clinical trials studies, as revealed by our risk of bias assessment. A significant limitation observed is the lack of detailed descriptions regarding the measurement of clinical endpoints (e.g. What was considered as infection?) and radiological outcomes (e.g. which parameters were considered to confirm bone union) in the majority of the studies. More rigorous and reproducible reporting on measurement methods as well as more detailed patient recruitment and allocation description could contribute to more robust and confident data.
In this study, we opted for broader inclusion criteria, encompassing all reports of MIPO for midshaft clavicle fractures, regardless of study design and comparison group. While this approach aimed to provide a comprehensive view of MIPO outcomes, it resulted in a limited number of studies directly comparing MIPO with surgical techniques other than ORIF with plate, such as titanium elastic nail and Intramedullary nails, which were then not subject to meta-analysis. Therefore, the comparative results between MIPO and these alternative techniques should be interpreted with caution.
Despite not being considered as an outcome of interest for this review, esthetic satisfaction with the surgical scar was not evaluated in the majority of the studies. As we believe that this may be also an advantage of the MIPO technique,13 future research in this topic may consider including this outcome in their analysis. Finally, as the topic of MIPO for midshaft clavicle fractures is of growing interest, it is possible that relevant articles may have been published since our research began. While we made efforts to conduct a thorough search, it is important to acknowledge the possibility of missing recent studies that could have influenced the overall findings. Furthermore, the lack of standardized and comparable reporting of fracture classifications across all included studies prevented us from conducting subgroup analyses based on fracture types.
Our results contribute to the growing body of evidence supporting the use of the MIPO technique for clavicle fractures, as it demonstrates a low risk of complications and good clinical outcomes in the short and mid-term. Moreover, the MIPO technique offers the advantage of shorter surgical time and potentially reduced risk of local area numbness. It is important to note that further high-quality clinical trials, with a greater emphasis on standardized reporting of methods, are needed to enhance our understanding of the outcomes and optimize the use of MIPO in this context. While this study’s findings may suggest that MIPO is comparable to ORIF, the existing data's limitations and lack of consistency across studies prevent us from definitively establishing the equivalence or superiority of both techniques at this point. Continued research efforts will provide more robust evidence to guide clinical decision-making and further refine the management of clavicle fractures.
Conclusion
This systematic review indicates that the MIPO technique for midshaft clavicle fractures demonstrates similar clinical outcomes to ORIF, while providing the added benefits of shorter surgical time and potentially lower risk of local area paresthesia. Future research with improved methodological rigor and standardized reporting is necessary to further enhance our understanding of MIPO's effectiveness and refine its application in clinical practice.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this systematic review and meta-analysis.
References
- 1.Al-Sadek T.A., Niklev D., Al-Sadek A. Midshaft clavicular fractures - osteosynthesis with minimally invasive technique. Open Access Maced J Med Sci. 2016;4:647–649. doi: 10.3889/oamjms.2016.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baertl S., Alt V., Rupp M. Surgical enhancement of fracture healing - operative vs. nonoperative treatment. Injury. 2021;52:S12–S17. doi: 10.1016/j.injury.2020.11.049. [DOI] [PubMed] [Google Scholar]
- 3.Chen L., Chen H., Nisar M., Chen H., Pan J., Peng L., et al. A retrospective comparison of minimally invasive percutaneous plate osteosynthesis (MIPPO) and minimally invasive percutaneous titanium elastic nail osteosynthesis (MIPTENO) for midshaft clavicle fracture. Int J Clin Exp Med. 2018;11:870–876. [Google Scholar]
- 4.Conboy V.B., Morris R.W., Kiss J., Carr A.J. An evaluation of the constant-murley shoulder assessment. J Bone Joint Surg Br. 1996;78:229–232. [PubMed] [Google Scholar]
- 5.Cumpston M., Li T., Page M.J., Chandler J., Welch V.A., Higgins J.P., et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10 doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delvaque J.G., Bégué T., Villain B., Mebtouche N., Aurégan J.C. Surgical treatment of mid-shaft clavicle fractures by minimally invasive internal fixation facilitated by intra-operative external fixation: a preliminary study. Orthop Traumatol Surg Res. 2019;105:847–852. doi: 10.1016/j.otsr.2019.01.022. [DOI] [PubMed] [Google Scholar]
- 7.Frima H., van Heijl M., Michelitsch C., van der Meijden O., Beeres F.J.P., Houwert R.M., et al. Clavicle fractures in adults; current concepts. Eur J Trauma Emerg Surg. 2020;46:519–529. doi: 10.1007/s00068-019-01122-4. [DOI] [PubMed] [Google Scholar]
- 8.Higgins J.P.T., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., et al., editors. Cochrane Handbook for systematic reviews of interventions version 6.3 (updated February 2022) Cochrane; 2022. www.training.cochrane.org/handbook : Hoboken, NJ 2022. [Google Scholar]
- 9.Jiang H., Qu W. Operative treatment of clavicle midshaft fractures using a locking compression plate: comparison between mini-invasive plate osteosynthesis (MIPPO) technique and conventional open reduction. Orthop Traumatol Surg Res. 2012;98:666–671. doi: 10.1016/j.otsr.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Jirangkul P., Kosiyatrakul A., Lorsuwannarat N. Minimally invasive plate osteosynthesis for displaced midshaft clavicle fractures: an indirect reduction using joystick technique. J Orthop Sci. 2022;28:1365–1372. doi: 10.1016/j.jos.2022.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy C.A., Beaton D.E., Smith P., Van Eerd D., Tang K., Inrig T., et al. Measurement properties of the QuickDASH (disabilities of the arm, shoulder and hand) outcome measure and cross-cultural adaptations of the QuickDASH: a systematic review. Qual Life Res. 2013;22:2509–2547. doi: 10.1007/s11136-013-0362-4. [DOI] [PubMed] [Google Scholar]
- 12.Khan L.A., Bradnock T.J., Scott C., Robinson C.M. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91:447–460. doi: 10.2106/JBJS.H.00034. [DOI] [PubMed] [Google Scholar]
- 13.Kim H.Y., Yang D.S., Bae J.H., Cha Y.H., Lee K.W., Choy W.S. Clinical and radiological outcomes after various treatments of midshaft clavicle fractures in adolescents. Clin Orthop Surg. 2020;12:396–403. doi: 10.4055/cios20026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim J.Y., Yoo B.C., Yoon J.P., Kang S.J., Chung S.W. A comparison of clinical and radiological outcomes of minimally invasive and conventional plate osteosynthesis for midshaft clavicle fractures. Orthopedics. 2018;41:e649–e654. doi: 10.3928/01477447-20180711-05. [DOI] [PubMed] [Google Scholar]
- 15.Ko S.H., Kim M.S. Comparison of supraclavicular nerve injuries after clavicle mid-shaft surgery via minimally invasive plate osteosynthesis versus open reduction and internal fixation. Arch Orthop Trauma Surg. 2022;142:1895–1902. doi: 10.1007/s00402-021-03941-w. [DOI] [PubMed] [Google Scholar]
- 16.Kundangar R.S., Mohanty S.P., Bhat N.S. Minimally invasive plate osteosynthesis (MIPO) in AO/OTA type B displaced clavicle fractures. Musculoskelet Surg. 2019;103:191–197. doi: 10.1007/s12306-018-0577-1. [DOI] [PubMed] [Google Scholar]
- 17.Kundangar R., Singh K.A., Mohanty S.P., Eshwari K. Clinical outcome of internal fixation of middle third clavicle fractures using locking compression plate: comparison between open plating and MIPO. J Orthop. 2019;16:414–418. doi: 10.1016/j.jor.2019.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee G.B., Kim H., Jeon I.H., Koh K.H. Long-term outcomes of initially conservatively treated midshaft clavicle fractures. Clin Shoulder Elb. 2021;24:9–14. doi: 10.5397/cise.2020.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee H.J., Oh C.W., Oh J.K., Yoon J.P., Kim J.W., Na S.B., et al. Percutaneous plating for comminuted midshaft fractures of the clavicle: a surgical technique to aid the reduction with nail assistance. Injury. 2013;44:465–470. doi: 10.1016/j.injury.2012.09.030. [DOI] [PubMed] [Google Scholar]
- 20.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339 doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mendes Junior A.F., Mota Neto J.D., Oppe I.G., de Simoni L.F., Giordano V., Labronici P.J. Surgical treatment of comminuted midshaft clavicle fracture by minimally invasive technique: description and preliminary results. Rev Bras Ortop (Sao Paulo) 2021;56:490–496. doi: 10.1055/s-0040-1714226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moradi A., Menendez M.E., Kachooei A.R., Isakov A., Ring D. Update of the Quick DASH questionnaire to account for modern technology. Hand (N Y) 2016;11:403–409. doi: 10.1177/1558944715628006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 24.Sohn H.S., Kim B.Y., Shin S.J. A surgical technique for minimally invasive plate osteosynthesis of clavicular midshaft fractures. J Orthop Trauma. 2013;27:e92–e96. doi: 10.1097/BOT.0b013e31826579c7. [DOI] [PubMed] [Google Scholar]
- 25.Sohn H.S., Kim W.J., Shon M.S. Comparison between open plating versus minimally invasive plate osteosynthesis for acute displaced clavicular shaft fractures. Injury. 2015;46:1577–1584. doi: 10.1016/j.injury.2015.05.038. [DOI] [PubMed] [Google Scholar]
- 26.Sohn H.S., Shin S.J., Kim B.Y. Minimally invasive plate osteosynthesis using anterior-inferior plating of clavicular midshaft fractures. Arch Orthop Trauma Surg. 2012;132:239–244. doi: 10.1007/s00402-011-1410-6. [DOI] [PubMed] [Google Scholar]
- 27.Sohn H.S., Shon M.S., Lee K.H., Song S.J. Clinical comparison of two different plating methods in minimally invasive plate osteosynthesis for clavicular midshaft fractures: a randomized controlled trial. Injury. 2015;46:2230–2238. doi: 10.1016/j.injury.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 28.Sterne J.A., Hernán M.A., Reeves B.C., Savović J., Berkman N.D., Viswanathan M., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355 doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sterne J.A.C., Savovic J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 30.Tieyi Y., Shuyi L., Yan Z., Guohua H., Jin S., Rui J. Minimally invasive plating for fresh displaced midshaft fractures of the clavicle. Orthopedics. 2014;37:679–683. doi: 10.3928/01477447-20140924-05. [DOI] [PubMed] [Google Scholar]
- 31.Wiesel B., Nagda S., Mehta S., Churchill R. Management of midshaft clavicle fractures in adults. J Am Acad Orthop Surg. 2018;26:e468–e476. doi: 10.5435/JAAOS-D-17-00442. [DOI] [PubMed] [Google Scholar]
- 32.You J.M., Wu Y.S., Wang Y. Comparison of post-operative numbness and patient satisfaction using minimally invasive plate osteosynthesis or open plating for acute displaced clavicular shaft fractures. Int J Surg. 2018;56:21–25. doi: 10.1016/j.ijsu.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Zehir S., Sahin E., Songür M., Altunkiliç T., ÖZdemir G. Minimal invasive percutaneous Plate Osteosynthesis (MIPPO) vs. open plating in superior plating of midshaft clavicle fractures. Acta Orthop Belg. 2018;84:491–496. [PubMed] [Google Scholar]
- 34.Zehir S., Zehir R., Şahin E., Çalbıyık M. Comparison of novel intramedullary nailing with mini-invasive plating in surgical fixation of displaced midshaft clavicle fractures. Arch Orthop Trauma Surg. 2015;135:339–344. doi: 10.1007/s00402-014-2142-1. [DOI] [PubMed] [Google Scholar]
- 35.Zhang T., Chen W., Sun J., Zhang Q., Zhang Y. Minimally invasive plate osteosynthesis technique for displaced midshaft clavicular fracture using the clavicle reductor. Int Orthop. 2017;41:1679–1683. doi: 10.1007/s00264-016-3392-z. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y., Xu J., Zhang C., Sun Y. Minimally invasive plate osteosynthesis for midshaft clavicular fractures using superior anatomic plating. J Shoulder Elbow Surg. 2016;25:e7–e12. doi: 10.1016/j.jse.2015.06.024. [DOI] [PubMed] [Google Scholar]
- 37.Zhao E., Zhang R., Wu D., Guo Y., Liu Q. Comparison between minimally invasive plate osteosynthesis and conventional open plating for midshaft clavicle fractures: a systematic review and meta-analysis. Biomed Res Int. 2019;2019 doi: 10.1155/2019/7081032. [DOI] [PMC free article] [PubMed] [Google Scholar]