Abstract
Background
Proximal ulna fracture-dislocations are challenging injuries with a myriad of existing classification systems. The Coronoid, proximal Ulna, Radius, and Ligaments classification (CURL) is a simple framework designed to focus attention on the key components affecting outcome and guide surgical management. This study evaluates interobserver and intraobserver reliability of this new classification.
Methods
Four observers independently reviewed plain radiographs and computed tomography (CT) scans of patients with proximal ulna fracture-dislocations. Each observer scored the Coronoid (C), proximal Ulna (U), and Radius (R) components for each fracture on 2 occasions. The osseous components were subclassified as ‘intact’, ‘simple’, or ‘complex’. The Ligament component (L) was not rated as this requires intraoperative classification. Interobserver and intraobserver reliability was calculated using Cohen’s weighted kappa coefficients. X-ray and CT were compared for patients with both imaging modalities. The Landis and Koch criteria were used to interpret the strength of the kappa statistics.
Results
One hundred seventy seven patients had plain X-rays; 58 patients had both X-ray and CT scans. Overall, in the X-ray only cohort, there was ‘almost perfect’ interobserver reliability for the radial head (k = 0.94) and coronoid (k = 0.83), and ‘substantial’ reliability (k = 0.68) for the proximal ulna. For the X-ray and CT cohort, interobserver reliability was ‘almost perfect’ across both modalities for the radial head (k = 0.88 and k = 0.93, respectively) and ‘moderate’ for the proximal ulna (k = 0.48 and k = 0.52, respectively). For the coronoid, interobserver reliability for X-ray interpretation was ‘substantial’ (k = 0.74) and for CT was ‘almost perfect’ (k = 0.89). Intraobserver reliability was ‘almost perfect’ for all components, other than CT assessment of the proximal ulna which demonstrated ‘substantial’ reliability (k = 0.74).
Conclusion
The Coronoid, proximal Ulna, Radius, and Ligaments classification demonstrates strong interobserver and intraobserver reliability, supporting use of the classification for proximal ulna fracture-dislocations. CT is recommended for improved characterization of any fracture with a coronoid component.
Keywords: Fracture, Dislocation, Fracture-dislocation, Proximal ulna, Classification, Reliability
Fracture-dislocations of the elbow account for 2%-5% of elbow fractures.13 There are a variety of classification systems used to describe the array of injury patterns seen, each with a different emphasis.9,13,20,34,39,41,44,46 The subset of fracture-dislocations that includes a proximal ulna fracture alongside instability of the ulnohumeral joint (UHJ) and/or the proximal radio-ulnar joint (PRUJ) can be particularly difficult to evaluate, classify, and treat. Several terms are used to categorize these injuries including Monteggia variants, atypical Monteggia lesions, type D olecranon fractures, transolecranon fracture-dislocations, and unstable olecranon fracture-dislocations, to name a few.28,29,38,47
The Monteggia pattern of injury was originally described as a proximal ulna fracture with associated radio-humeral dislocation,13,14 with further classification by Bado in 1967.4 Although the posterior Monteggia lesion (Bado Type II) has been subclassified by Jupiter into 4 groups to better describe the ulna fracture,19,32 the classification does not describe the proximal ulna fracture in detail or account for important concomitant osseo-ligamentous injuries.13,33
Trans-olecranon fracture-dislocations can range from an isolated olecranon fracture with ulnohumeral instability, to a highly comminuted proximal ulna fracture with associated radial head and coronoid fractures.7,26,29,35,48 Although the proximal radioulnar articulation is characteristically preserved in these injuries,26 they may be confused with the anterior Monteggia pattern. While classically described as an isolated osseous injury,8,10,26,29 conflicting studies demonstrate damage to the collateral ligaments.5,26,37 In addition, Doornberg and Wong both describe a pattern of injury: the posterior transolecranon fracture-dislocation—an injury associated with radial head fracture, radioulnar disruption, and potential collateral ligament injury.10,48
The overlap between these complex injury patterns inevitably leads to confusion and difficulty in applying the classifications in practice. This is reflected by studies demonstrating their poor therapeutic and prognostic value.11,13,21 Furthermore, attempting to ‘name’ the fracture type may distract from understanding the full pathoanatomy of the injury, especially in the presence of concomitant radial head and coronoid fractures, which when present, are known to adversely affect prognosis.12,25,31,36,44 It is therefore preferable to have a simple, reliable framework that allows a comprehensive description of the whole spectrum of proximal ulna fracture-dislocations with focus on the components that directly influence surgical management and outcome.6,30
The primary aim of this study was to assess interobserver and intraobserver reliability of a new classification when applied as a preoperative tool to assess proximal ulna fracture-dislocations of the elbow.
The secondary aim was to compare the reliability of X-ray and computed tomography (CT) assessment where both modalities were used for the same fracture.
Materials and methods
This is a diagnostic study using a clinical cohort of patients and multiple observers to evaluate the reliability of a novel classification system for fractures of the proximal ulna with associated instability of the ulnohumeral or proximal radioulnar joints.
CURL classification system
Rationale
The Coronoid, proximal Ulna, Radius, and Ligament system (CURL) was developed as a simple, reliable framework to encompass the whole spectrum of proximal ulna fracture-dislocations with focus on the components that directly influence surgical management and outcome. It is based on the understanding that proximal ulna fracture-dislocations comprise a spectrum that includes relatively benign injuries with an isolated proximal ulna fracture to highly complex injuries affecting all the osseo-ligamentous constraints (Fig. 1). The purpose of simplifying the classification of these injuries is to aid in identification of all injured components, quantify severity of these components, and assist in formulating a surgical plan, with the hope that this will lead to more consistent outcomes.
Figure 1.
Plain radiographs demonstrating the wide spectrum of injury seen in proximal ulna fracture dislocations.
Components
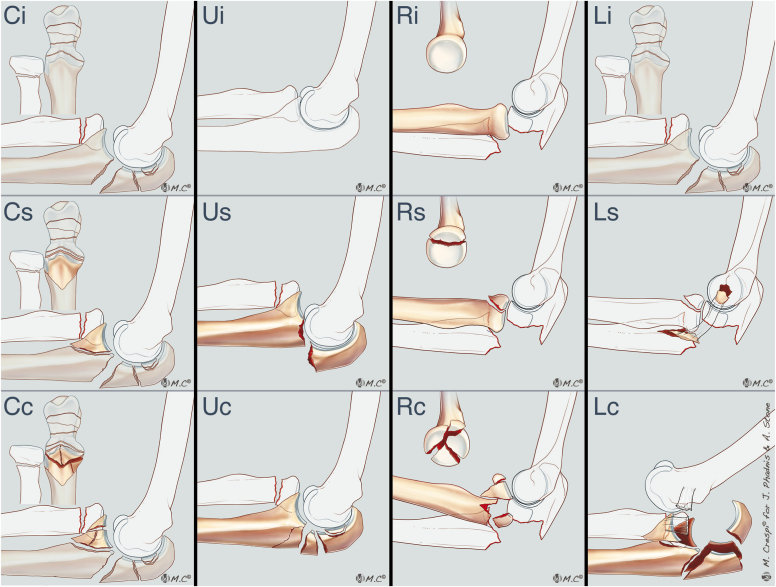
The classification (Fig. 2) comprises 3 osseous components (Coronoid, proximal Ulna, and Radius) that can be assessed from preoperative imaging and form the basis of this study. The Ligament component completes the classification as ligament injuries can be inferred from preoperative imaging but require intraoperative verification.
Figure 2.
Illustrations depicting the different components and grading of the Coronoid (C), proximal Ulna (U), Radial Head (R), and Ligaments (L) (CURL) classification of proximal ulna fracture-dislocations. For each component, “i” indicates intact, “s” indicates simple, and “c” indicates complex.
The purpose of this study was to assess the reliability of the preoperative bony components, which form the core of the classification system. Each of the bony components is subcategorized as intact (no fracture), simple, or complex. Simple and complex fractures were defined as follows:
Coronoid (C)
An intact coronoid was defined as the coronoid in continuity with the proximal ulna. A simple fracture was defined as a fractured coronoid in a single fragment, and a complex fracture was defined as coronoid fracture with multiple fracture lines creating > 1 fragment (Fig. 2).
Proximal ulna (U)
By definition, all included injuries have a proximal ulna fracture; hence, there were no intact ulnas. A simple fracture was defined as a proximal ulna fracture (intra-articular or extra-articular) with a single fracture line exiting the dorsal cortex of the ulna. Undisplaced secondary fracture lines were considered simple. A complex fracture was defined as a proximal ulna fracture with multiple displaced intra-articular or extra-articular lines (Fig. 2).
Radius (R)
A simple fracture was defined as an undisplaced radial neck fracture or a partial articular fracture comprising < 3 articular fragments (Fig. 2). A complex fracture was defined as any displaced complete articular fracture, partial articular fractures with 3 or more articular fragments, or a displaced radial neck fracture.
Ligaments (L)
This component is categorized as intact (no collateral ligament injury), simple (isolated lateral or medial collateral ligament injury), or complex (both ligaments injured). Although the ligament component may be inferred from preoperative imaging of avulsion fragments (Fig. 2), it requires intraoperative assessment for confirmation. It was therefore not included in the present preoperative reliability study.
Patients
Inclusion/exclusion criteria
Patients were identified using the institution’s trauma database over an 11-year period (April 2009-September 2020). The initial search identified 1223 patients including duplicates and pediatric patients (aged < 18 years at time of injury) who were subsequently excluded, leaving 930 patients. Preliminary screening for traumatic elbow fracture-dislocations was undertaken by 2 of the authors (H.G. and R.B.). The criteria for inclusion were the presence of a proximal ulna fracture with evidence of UHJ and/or PRUJ instability. UHJ instability was defined as coronal or sagittal plane incongruity of the ulnohumeral articulation manifesting as either asymmetric alignment of the UHJ and/or subluxation or dislocation of the radial head relative to the capitellum. PRUJ instability was defined as loss of congruence between lesser sigmoid notch and radial head. Classic Monteggia injuries involving the ulna diaphysis with a stable UHJ were excluded, as were olecranon fractures without radiographic evidence of joint instability. Rotatory fracture dislocations with the presence of a coronoid fracture but no proximal ulna fracture were also excluded. Final screening of cases for inclusion was performed by all authors leaving a sample population of 177 patients for analysis.
Radiological evaluation
All 177 patients had initial plain radiographs at presentation. Fifty-eight (32.8%) patients also had CT scans. This was at the discretion of the surgical team who determined the need for advanced imaging based on the X-rays. For patients who had a CT scan, X-ray was used to perform classification first, without viewing the CT images, followed by a repeat classification 1 week later with CT imaging only.
Complete assessment was independently performed by 4 observers (H.G., R.B., R.M., and J.P.) on 2 separate occasions with a 4-week interval. One of the assessors was a medical student, 1 was a research fellow, and 2 were fellowship-trained shoulder and elbow specialists. Consensus on how to perform the classification was agreed prior to data collection. Observers completed the study using the same institutional imaging software.
Statistical analysis
For the purpose of the study, each of the 3 bony components were assigned a score to allow calculation of interobserver and intraobserver reliability. In the absence of a component being fractured (eg, intact radial head), a score of 0 was assigned. A simple fracture of the component was assigned a score of 1 and a complex fracture was assigned a score of 2. Hence, the maximum possible score was 6 and minimum 1 as all injuries by nature had a proximal ulna fracture.
Interobserver reliability was calculated using Light’s derivation of Cohen’s Kappa (k).23 The 4 observers were compared using a pairwise approach, resulting in 6 different statistical comparisons of interobserver agreement. The arithmetic mean of the 6 pair agreements was calculated to find the overall Kappa statistic for each component of the CURL score. Our data were weighted to account for its ordinal nature and determine whether or not there was a gradient between scores, that is, whether the relative agreement between adjacent scores 1 and 2 is different to the relative agreement between the scores 0 and 2.
Interobserver statistical analysis was carried out on 2 separate cohorts defined as follows: All patients who had X-rays and all patients who had both an X-ray and a CT. The intraobserver reliability was calculated for each observer using the Cohen’s weighted Kappa. Interpretation of the Kappa statistics was accomplished in accordance with the criteria presented by Landis and Koch in 197722: K values of 0.81-1 are considered almost perfect, 0.61-0.8 substantial, 0.41-0.6 moderate, 0.21-0.4 fair, 0-0.2 slight, and < 0 poor. A score of −1 represents total disagreement between the observers and +1 represents perfect agreement. P values of < .05 were considered statistically significant and were calculated to account for averaging of the data.45 Statistical analysis was conducted using SPSS (version 27; IBM Corp., Armonk, NY, USA).
Results
Patient demographics
There were 82 male (46.3%) and 95 female (53.7 %) patients. Mean age was 60.1 years (range: 18-96 years, standard deviation 20.0). The left elbow was affected in 93 of 177 (52.5%) patients.
There were 55 (31%) patients with a proximal radius fracture and 46 (25.9%) patients with a coronoid fracture.
Interobserver reliability: X-rays
Using plain radiographs alone, the CURL score across all 4 observers demonstrated substantial to almost perfect agreement as a total score and for the individual components in both the first and second set of observations. This is detailed in Table 1.
Table I.
Overall interobserver reliability for the CURL classification of patients who had only an X-ray on admission.
| Score component | Weighted kappa | Agreement | SE (95% CI) | Significance |
|---|---|---|---|---|
| First set | ||||
| Coronoid | 0.86 | Almost Perfect | 0.03 (0.80 to 0.93) | <0.0001 |
| Proximal ulna | 0.72 | Substantial | 0.06 (0.61 to 0.83) | <0.0001 |
| Radial head | 0.94 | Almost Perfect | 0.03 (0.90 to 0.98) | <0.0001 |
| Total | 0.85 | Almost Perfect | 0.03 (0.80 to 0.90) | <0.0001 |
| Second set | ||||
| Coronoid | 0.80 | Substantial | 0.04 (0.72 to 0.88) | <0.0001 |
| Proximal ulna | 0.64 | Substantial | 0.06 (0.52 to 0.76) | <0.0003 |
| Radial head | 0.93 | Almost Perfect | 0.02 (0.88 to 0.97) | <0.0001 |
| Total | 0.80 | Substantial | 0.03 (0.75 to 0.85) | <0.0001 |
| Overall (mean of both sets) | ||||
| Coronoid | 0.83 | Almost Perfect | ||
| Proximal ulna | 0.68 | Substantial | ||
| Radial head | 0.94 | Almost Perfect | ||
| Total | 0.83 | Almost Perfect | ||
CI, confidence interval; SE, standard error; CURL, Coronoid, proximal Ulna, Radius, and Ligament system.
Interobserver reliability: X-ray vs. CT
For the 58 patients who had both preoperative X-ray and CT, interobserver reliability across the 4 observers demonstrated higher values for CT compared with X-ray for total CURL score and all individual components, with the greatest improvement in agreement for CT over X-ray seen for the coronoid component of the classification. The results are detailed in Table II.
Table II.
Overall interobserver reliability for the CURL classification of patients who had both an X-ray on admission and a preoperative CT scan.
| Score component | Weighted kappa | Agreement | SE (95% CI) | Significance |
|---|---|---|---|---|
| First set | ||||
| X-ray | ||||
| Coronoid | 0.77 | Substantial | 0.06 (0.66 to 0.89) | <0.0003 |
| Proximal ulna | 0.46 | Moderate | 0.13 (0.28 to 0.72) | <0.0027 |
| Radial head | 0.87 | Almost Perfect | 0.04 (0.79 to 0.96) | <0.0003 |
| Total | 0.74 | Substantial | 0.05 (0.63 to 0.84) | <0.0003 |
| CT | ||||
| Coronoid | 0.90 | Almost Perfect | 0.04 (0.82 to 0.98) | <0.0001 |
| Proximal ulna | 0.51 | Moderate | 0.14 (0.24 to 0.76) | <0.001 |
| Radial head | 0.93 | Almost Perfect | 0.04 (0.86 to 1.01) | <0.0001 |
| Total | 0.82 | Almost Perfect | 0.04 (0.74 to 0.90) | <0.0003 |
| Second set | ||||
| X-ray | ||||
| Coronoid | 0.71 | Substantial | 0.07 (0.58 to 0.84) | <0.0001 |
| Proximal ulna | 0.50 | Moderate | 0.13 (0.26 to 0.75) | <0.0028 |
| Radial head | 0.88 | Almost Perfect | 0.05 (0.79 to 0.97) | <0.0004 |
| Total | 0.69 | Substantial | 0.05 (0.59 to 0.79) | <0.0002 |
| CT | ||||
| Coronoid | 0.87 | Almost Perfect | 0.05 (0.78 to 0.96) | <0.0004 |
| Proximal ulna | 0.53 | Moderate | 0.13 (0.27 to 0.79) | <0.001 |
| Radial head | 0.93 | Almost Perfect | 0.03 (0.87 to 0.99) | <0.0002 |
| Total | 0.81 | Almost Perfect | 0.04 (0.74 to 0.89) | <0.0001 |
| Overall (mean of both sets) | ||||
| X-ray | ||||
| Coronoid | 0.74 | Substantial | ||
| Proximal ulna | 0.48 | Moderate | ||
| Radial head | 0.88 | Almost Perfect | ||
| Total | 0.72 | Substantial | ||
| CT | ||||
| Coronoid | 0.89 | Almost Perfect | ||
| Proximal ulna | 0.52 | Moderate | ||
| Radial head | 0.93 | Almost Perfect | ||
| Total | 0.82 | Almost Perfect | ||
CI, confidence interval; SE, standard error; CT, computed tomography; CURL, Coronoid, proximal Ulna, Radius, and Ligament system.
Intraobserver reliability
Intraobserver agreement for each of the 4 observers was significant to perfect for all components and total CURL scores. Most parameters showed a kappa value of more than 0.9 with almost perfect agreement. The results are detailed in Table III.
Table III.
Intraobserver reliability of the 4 observers for the CURL classification across the modality of X-ray and CT.
| Coronoid |
Proximal ulna |
Radial head |
Total |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kappa | SE | Significance | Kappa | SE | Significance | Kappa | SE | Significance | Kappa | SE | Significance | |
| X-ray | ||||||||||||
| Observer 1 | 0.91 | 0.03 | <0.001 | 0.71 | 0.06 | <0.001 | 0.96 | 0.01 | <0.001 | 0.90 | 0.02 | <0.001 |
| Observer 2 | 0.90 | 0.03 | <0.001 | 0.93 | 0.03 | <0.001 | 0.96 | 0.01 | <0.001 | 0.92 | 0.02 | <0.001 |
| Observer 3 | 0.98 | 0.01 | <0.001 | 0.91 | 0.04 | <0.001 | 1.00 | 0.00 | <0.001 | 0.96 | 0.01 | <0.001 |
| Observer 4 | 0.77 | 0.05 | <0.001 | 0.72 | 0.06 | <0.001 | 0.91 | 0.03 | <0.001 | 0.78 | 0.03 | <0.001 |
| Mean | 0.89 | 0.82 | 0.96 | 0.89 | ||||||||
| CT | ||||||||||||
| Observer 1 | 0.95 | 0.03 | <0.001 | 0.68 | 0.15 | <0.001 | 0.95 | 0.03 | <0.001 | 0.92 | 0.03 | <0.001 |
| Observer 2 | 0.95 | 0.03 | <0.001 | 1.00 | 0.00 | <0.001 | 1.00 | 0.00 | <0.001 | 0.97 | 0.02 | <0.001 |
| Observer 3 | 0.96 | 0.03 | <0.001 | 0.69 | 0.11 | <0.001 | 0.98 | 0.02 | <0.001 | 0.91 | 0.03 | <0.001 |
| Observer 4 | 0.89 | 0.04 | <0.001 | 0.60 | 0.11 | <0.001 | 0.84 | 0.06 | <0.001 | 0.81 | 0.05 | <0.001 |
| Mean | 0.94 | 0.74 | 0.94 | 0.90 | ||||||||
SE, standard error; CT, computed tomography; CURL, Coronoid, proximal Ulna, Radius, and Ligament system.
Discussion
The primary aim of this study was to assess interobserver and intraobserver reliability of the CURL classification system when applied as a preoperative tool to assess proximal ulna fracture-dislocations of the elbow. The secondary aim was to compare the reliability of X-ray and CT assessment where both modalities were used for the same fracture.
A strong interobserver and intraobserver reliability was demonstrated for all osseous components of the classification. Higher reliability values for CT compared with X-ray were found for total CURL score and all individual components, with the greatest improvement in agreement seen for the coronoid component.
There are only a few existing studies that investigate the reliability of the other classification systems used to describe fracture-dislocations that involve the proximal ulna.6,13,17,42,43 Indeed, to our knowledge, there exist no data reporting the observer reliability of Monteggia and Monteggia-type injuries described by Bado, Jupiter, and Ring.17
Previous authors have assessed the interobserver reliability of coronoid fracture classification independent of other fractures that comprise the patient’s overall injury and have demonstrated that observer agreement for coronoid fractures increases with use of advanced imaging compared to X-ray.1,16,24 This was verified in the present study, where agreement from radiographs was substantial in both sets of data (k = 0.77 and k = 0.71), but was almost perfect across both sets of CT scores (k = 0.90 and k = 0.87).
For the proximal radius, the most common classification used is that of Mason and its derivations; however, its ability to direct treatment and predict short-term prognosis limits its value.17,48 Our results show strong interobserver reliability with regard to radiographic assessment of radial head fractures in both sets of data, with almost perfect agreement in our X-ray only cohort (k = 0.80-0.86) and substantial agreement in our CT and X-ray cohort (k = 0.71-0.77) which is superior to the reliability of the mason classification assessed by other authors.3,18,27 This is likely to be because we have simplified the classification based upon clearly defined parameters that affect decision-making and treatment, which is the overall premise of CURL.
The CURL system was developed by the senior author to make analysis, planning, and surgical execution of these complex injuries more simple and user friendly. Additionally, it allows teaching regarding these injuries to be focused on the most critical structures involved with strong emphasis on the coronoid as a key influencer of outcome. This is why the coronoid comes first in the CURL system.
The proposed CURL classification system has some evident strength. It offers a more simplistic approach to each component of the fracture-dislocation in parallel to providing an overall understanding of the total severity of the injury pattern. Furthermore, it provides a shift away from the multiple different classifications and eponyms currently required to describe these injuries.
It is important to understand that the intention of CURL is not to generate a numerical score; however, assigning numerical values to the fracture subtypes was required in the present study for assessment of reliability and will be useful for future prognostic studies. In clinical practice, the purpose of CURL is to move away from naming fractures and focus attention on recognition and management of the most important injury components affecting outcome. By understanding that these injuries are part of the same spectrum, and providing a simple framework for preoperative interpretation, with emphasis on the coronoid, the aim is to improve surgical planning with regard to variables like patient positioning, surgical approach, implant requirements, and need for expert help. The result would be to expect improved outcomes for an injury with frequent complications.
We acknowledge that there are some inherent limitations to the retrospective methodology regarding selection bias; however, the large sample is a strength which increases the reliability of the results.2 Most similar studies use far smaller sample sizes with infrequent assessment of intraobserver reliability.6,11,13,15,17,25,40,43 Furthermore, it is acknowledged that interobserver and intraobserver reliability does not equate to accuracy of the classification.
Finally, ligament injury was not assessed as part of this study, although it is an important component of the CURL classification. We did not feel the preoperative inference of a ligament injury seen on imaging could be reliably corroborated from the operative notes as the surgical treatment was performed by a range of surgeons, many of whom did not document or treat sometimes obvious ligament injuries in the definitive surgery. The ligament component would better be verified in a prospective study with surgery performed by clinicians using the CURL system.
Future research direction regarding the CURL classification includes correlation of preoperative imaging with intraoperative ligament injuries and a study to assess the prognostic value of the CURL system with regard to patient outcome.
Conclusion
The CURL classification system demonstrates high interobserver and intraobserver reliability across each osseous component of the classification. The coronoid component of these injuries is critical, and CT is recommended for any injury with a possible coronoid component to optimize characterization. We propose that the CURL classification system is a reliable preoperative framework for assessment of the full spectrum of ‘proximal ulna fracture-dislocations’.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this study.
References
- 1.Adams J.E., Sanchez-Sotelo J., Kallina C.F.T., Morrey B.F., Steinmann S.P. Fractures of the coronoid: morphology based upon computer tomography scanning. J Shoulder Elbow Surg. 2012;21:782–788. doi: 10.1016/j.jse.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Audige L., Bhandari M., Kellam J. How reliable are reliability studies of fracture classifications? A systematic review of their methodologies. Acta Orthop Scand. 2004;75:184–194. doi: 10.1080/00016470412331294445. [DOI] [PubMed] [Google Scholar]
- 3.Ayyaswamy B., Howell L., Anand A., Charalambous C.P. Interobserver and intraobserver variations in radial head fracture classification-assessment of two classification systems. J Orthop. 2019;16:463–467. doi: 10.1016/j.jor.2019.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bado J.L. The Monteggia lesion. Clin Orthop Relat Res. 1967;50:71–86. [PubMed] [Google Scholar]
- 5.Bailey C.S., MacDermid J., Patterson S.D., King G.J. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. 2001;15:542–548. doi: 10.1097/00005131-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Benetton C.A., Cesa G., El-Kouba Junior G., Ferreira A.P., Vissoci J.R., Pietrobon R. Agreement of olecranon fractures before and after the exposure to four classification systems. J Shoulder Elbow Surg. 2015;24:358–363. doi: 10.1016/j.jse.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 7.Biga N., Thomine J. La luxation trans-olecranienne du coude. Rev Chir Orthop Traumatol. 1974;60:557–567. [PubMed] [Google Scholar]
- 8.Cho C.H., Kim D.H., Na S.S., Choi B.C., Kim B.S. Trans-olecranon fracture-dislocations of the elbow: a systematic review. Diagnostics. 2020;10:1058. doi: 10.3390/diagnostics10121058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colton C.L. Fractures of the olecranon in adults: classification and management. Injury. 1973;5:121–129. doi: 10.1016/s0020-1383(73)80088-9. [DOI] [PubMed] [Google Scholar]
- 10.Doornberg J., Ring D., Jupiter J.B. Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin Orthop Relat Res. 2004;429:292–300. doi: 10.1097/01.blo.0000142627.28396.cb. [DOI] [PubMed] [Google Scholar]
- 11.Doornberg J.N., Guitton T.G., Ring D., Science of Variation G. Diagnosis of elbow fracture patterns on radiographs: interobserver reliability and diagnostic accuracy. Clin Orthop Relat Res. 2013;471:1373–1378. doi: 10.1007/s11999-012-2742-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Englert C., Zellner J., Koller M., Nerlich M., Lenich A. Elbow dislocations: a review ranging from soft tissue injuries to complex elbow fracture dislocations. Adv Orthop. 2013;2013 doi: 10.1155/2013/951397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giannicola G., Greco A., Sacchetti F.M., Cinotti G., Nofroni I., Postacchini F. Complex fracture-dislocations of the proximal ulna and radius in adults: a comprehensive classification. J Shoulder Elbow Surg. 2011;20:1289–1299. doi: 10.1016/j.jse.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Givon U., Pritsch M., Levy O., Yosepovich A., Amit Y., Horoszowski H. Monteggia and equivalent lesions. A study of 41 cases. Clin Orthop Relat Res. 1997;337:208–215. doi: 10.1097/00003086-199704000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Guitton T.G., Kinaci A., Ring D. Diagnostic accuracy of 2- and 3-dimensional computed tomography and solid modeling of coronoid fractures. J Shoulder Elbow Surg. 2013;22:782–786. doi: 10.1016/j.jse.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Haapamaki V., Kiuru M., Koshinen S. Multidetector computer tomography diagnosis of adult elbow fractures. Acta Radiol. 2004;45:65–70. doi: 10.1080/02841850410003310. [DOI] [PubMed] [Google Scholar]
- 17.Hamoodi Z., Singh J., Elvey M.H., Watts A.C. Reliability and validity of the Wrightington classification of elbow fracture-dislocation. Bone Joint Lett J. 2020;102-B:1041–1047. doi: 10.1302/0301-620X.102B8.BJJ-2020-0013.R1. [DOI] [PubMed] [Google Scholar]
- 18.Iannuzzi N.P., Leopold S.S. In brief: the Mason classification of radial head fractures. Clin Orthop Relat Res. 2012;470:1799–1802. doi: 10.1007/s11999-012-2319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jupiter J.B., Leibovic S.J., Ribbans W., Wilk R.M. The posterior Monteggia lesion. J Orthop Trauma. 1991;5:395–402. doi: 10.1097/00005131-199112000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Kani K.K., Chew F.S. Terrible triad injuries of the elbow. Emerg Radiol. 2019;26:341–347. doi: 10.1007/s10140-019-01676-1. [DOI] [PubMed] [Google Scholar]
- 21.Konrad G.G., Kundel K., Kreuz P.C., Oberst M., Sudkamp N.P. Monteggia fractures in adults: long-term results and prognostic factors. J Bone Joint Surg Br. 2007;89:354–360. doi: 10.1302/0301-620X.89B3.18199. [DOI] [PubMed] [Google Scholar]
- 22.Landis J.R., Gary G.K. The Measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 23.Light R. Measures of response agreement for qualitative data: some generalizations and alternatives. Psychol Bull. 1971;76:365. [Google Scholar]
- 24.Lindenhovius A., Karanicolas P.J., Bhandari M., van Dijk N., Ring D., Collaboration for Outcome Assessment in Surgical T Interobserver reliability of coronoid fracture classification: two-dimensional versus three-dimensional computed tomography. J Hand Surg Am. 2009;34:1640–1646. doi: 10.1016/j.jhsa.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 25.Matsunaga F.T., Tamaoki M.J., Cordeiro E.F., Uehara A., Ikawa M.H., Matsumoto M.H., et al. Are classifications of proximal radius fractures reproducible? BMC Musculoskelet Disord. 2009;10:120. doi: 10.1186/1471-2474-10-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Midtgaard K.S., Nolte P.C., Miles J.W., Tanghe K.K., Peebles L.A., Provencher M.T., et al. Biomechanical significance of the collateral ligaments in transolecranon fracture-dislocations. J Shoulder Elbow Surg. 2021;30:1245–1250. doi: 10.1016/j.jse.2020.09.010. [DOI] [PubMed] [Google Scholar]
- 27.Morgan S.J., Groshen S.L., Itamura J.M., Shankwiler J., Brien W.W., Kuschner S.H. Reliability evaluation of classifying radial head fractures by the system of Mason. Bull Hosp Jt Dis. 1997;56:95–98. [PubMed] [Google Scholar]
- 28.Morrey B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect. 1995;44:175–185. [PubMed] [Google Scholar]
- 29.Mouhsine E., Akiki A., Castagna A., Cikes A., Wettstein M., Borens O., et al. Transolecranon anterior fracture dislocation. J Shoulder Elbow Surg. 2007;16:352–357. doi: 10.1016/j.jse.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 30.Müller M., Perren S.M., Allgöwer M., Schneider R. 3rd ed. Springer-Verlag; Berlin: 1991. Manual of Internal Fixation: Techniques recommended by the AO-ASIF group; pp. 130–133. Willenegger H. 978-3-642-08091-3. [Google Scholar]
- 31.Regan W., Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg. 2008;71:1348–1354. doi: 10.1055/s-2008-1038166. [DOI] [PubMed] [Google Scholar]
- 32.Rehim S.A., Maynard M.A., Sebastin S.J., Chung K.C. Monteggia fracture dislocations: a historical review. J Hand Surg Am. 2014;39:1384–1394. doi: 10.1016/j.jhsa.2014.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reynders P., De Groote W., Rondia J., Govaerts K., Stoffelen D., Broos P.L. Monteggia lesions in adults. A multicenter Bota study. Acta Orthop Belg. 1996;62:78–83. [PubMed] [Google Scholar]
- 34.Ring D., Jupiter J.B. Fracture-dislocation of the elbow. Hand Clin. 2002;18:55–63. doi: 10.1016/s0749-0712(02)00004-5. [DOI] [PubMed] [Google Scholar]
- 35.Ring D., Jupiter J.B., Sanders R.W., Mast J., Simpson N.S. Transolecranon fracture-dislocation of the elbow. J Orthop Trauma. 1997;11:545–550. doi: 10.1097/00005131-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Ring D., Jupiter J.B., Simpson N. Monteggia fractures in adults. J Bone Joint Surg. 1998;80:1733–1744. doi: 10.2106/00004623-199812000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Sanchez-Sotelo J., Morrey M. Complex elbow instability: surgical management of elbow fracture dislocations. EFORT Open Rev. 2016;1:183–190. doi: 10.1302/2058-5241.1.000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scharplatz D., Allgower M. Fracture-dislocations of the elbow. Injury. 1975;7:143–159. doi: 10.1016/0020-1383(75)90012-1. [DOI] [PubMed] [Google Scholar]
- 39.Schatzker J., Tile M., Axelrod T.S. Springer; Berlin: 2005. The rationale of operative fracture care; pp. 123–129. 978-3-642-06164-6. [Google Scholar]
- 40.Sheps D., Hildebrand K., Keifer K. The inter-observer reliability of classification systems for radial head fractures. Orthop Proc. 2008;90:140. [Google Scholar]
- 41.Sotereanos D.G., Darlis N.A., Wright T.W., Goitz R.J., King G.J. Unstable fracture-dislocations of the elbow. Instr Course Lect. 2007;56:369–376. [PubMed] [Google Scholar]
- 42.Sullivan C.W., Desai K. Classifications in brief: Mayo classification of olecranon fractures. Clin Orthop Relat Res. 2019;477:908–910. doi: 10.1097/CORR.0000000000000614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tamaoki M.J., Matsunaga F.T., Silveira J.D., Balbachevsky D., Matsumoto M.H., Belloti J.C. Reproducibility of classifications for olecranon fractures. Injury. 2014;45:S18–S20. doi: 10.1016/S0020-1383(14)70015-4. [DOI] [PubMed] [Google Scholar]
- 44.Thayer M.K., Swenson A.K., Hackett D.J., Hsu J.E. Classifications in brief: Regan-Morrey classification of coronoid fractures. Clin Orthop Relat Res. 2018;476:1540–1543. doi: 10.1007/s11999.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vovk V., Wang R. Combining p-values via averaging. Biometrika. 2020;107:791–808. doi: 10.1093/biomet/asaa027. [DOI] [Google Scholar]
- 46.Watts A.C., Singh J., Elvey M., Hamoodi Z. Current concepts in elbow fracture dislocation. Shoulder Elbow. 2021;13:451–458. doi: 10.1177/1758573219884010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wolfgang G., Burke F., Bush D., Parenti J., Perry J., LaFollette B., et al. Surgical treatment of displaced olecranon fractures by tension band wiring technique. Clin Orthop Relat Res. 1987:192–204. [PubMed] [Google Scholar]
- 48.Wong J.C., Getz C.L., Abboud J.A. Adult Monteggia and olecranon fracture dislocations of the elbow. Hand Clin. 2015;31:565–580. doi: 10.1016/j.hcl.2015.06.006. [DOI] [PubMed] [Google Scholar]