Abstract
Background
Lateral ankle sprain (LAS) is the most common sports injury, leading to a high rate of recurrence and the development of chronic ankle instability. One possible explanation is the lack of objective, evidence-based criteria to inform return to sport decisions following LAS. The aim of this study was therefore to assess the efficacy of a new functional score to distinguish patients at risk of recurrent LAS within two years after the initial injury.
Methods
The Ankle-GO score was used in 64 active patients two months after LAS. This composite score includes 2 self-reported questionnaires and 4 functional tests, for a maximum score of 25 points. The rate of reinjury was prospectively recorded 2 years after inclusion. Potential predictive variables for reinjury were tested using the Chi-square and independent t-tests. The area under the receiver operating characteristics curve (AUC) with the optimal cut-off score was determined to assess the predictive value of the Ankle-GO score for the risk of reinjury. Multivariate logistic regression was then used to determine the influence of risk factors of reinjury.
Results
Fifty-four (85%) patients were included (23 men and 31 women, 34.7 ± 13 years old) including 18 (33.3%) with a reinjury. The two-month Ankle-GO score was lower in patients with a recurrent LAS (5.4 ± 2.8 points vs. 9.1 ± 4.5, p = 0.002) and predicted the risk of reinjury (AUC = 0.75). Patients with < 8 points were found to have a significantly higher risk of reinjury (OR = 8.6; 95%CI: 2-37.2, p = 0.001). Women also tend to have a higher risk of recurrence (OR = 3.8; 95%CI: 0.9–15.5, p = 0.065).
Conclusion
The Ankle-GO score is a new objective criterion for RTS after LAS. Patients with a low score at two months have a 9-fold greater risk of recurrence within two years.
Keywords: Lateral ankle sprain, Return-to-sport, Reinjury, Risk factors, Ankle-GO
Key points
• The two-year risk of ankle sprain recurrence is nine times higher in patients with a low Ankle-GO score.
• Women tend to have a fourfold higher risk of re-injury within two years, despite an initial Ankle-GO score comparable to men.
• This innovative score could significantly influence the clinical management of LAS by providing an objective assessment of the readiness to RTS after LAS.
Background
Lateral ankle sprain (LAS) is the most common sports injury. It is associated with a significant risk of recurrence, in particular a two-fold increased risk in the year following the initial injury [1, 2]. Moreover, about 40% of individuals develop chronic ankle instability (CAI) after their first LAS [3, 4]. One potential contributing factor to this high rate of recurrence and the consequences of LAS is a premature return to sport (RTS) [5]. Studies show that nearly 50% of patients RTS within three days after LAS, and 80% within a week [6, 7], despite lingering impairment and residual functional deficiencies [8].
There is no consensus on objective criteria for the RTS following LAS to date [2, 9] and this decision is usually time-based. A recent multidisciplinary consensus of international experts identified 5 domains as objective criteria for the evaluation of the RTS [5]. In addition to Pain severity and Ankle impairment, this consensus emphasized the importance of monitoring the Athlete’s perception, Sensorimotor control, and Sport/functional performance. The Ankle-GO is a recently developed objective score [10] based on this “PAASS” framework and including various functional tests and patient self-reported questionnaires. These tests were chosen for their ability to differentiate CAI patients from copers and healthy individuals [11].
Although the Ankle-GO has been shown to reliably discriminate and predict RTS at the same level of play after LAS [10], its ability to identify patients at risk of recurrence has not yet been established. This study assessed whether the Ankle-GO score could predict the risk of reinjury following LAS. We hypothesized that the scores in patients with recurrent LAS within two years after injury would be lower at two-months post-LAS and predictive of the risk of re-injury. We also hypothesized that other established risk factors (age, sex and type or level of sports) [12] could influence the risk of reinjury.
Methods
Population
A priori power analysis showed that a minimum sample size of 54 participants (G*Power, Version 3.1, University of Dusseldorf, Germany) was needed to detect a moderate effect size for logistic regression (OR = 3.5), with a power of 0.80 and type 1 error of 0.05 [13, 14]. Considering a potential risk of 20% lost to follow-up patients [3], sixty-four patients (36 women and 28 men, 33.7 ± 13.2 years old) with recent LAS were included in the study (Table 1). The patients were all recruited in the same clinic, from January to August 2021. LAS was defined according to the International Ankle Consortium criteria as “an acute traumatic injury to the lateral ligament complex of the ankle joint from an excessive and sudden inversion mechanism of the rear foot or combined plantar flexion and adduction of the foot that prevents (the patient) from participating in sports” [15]. Only patients who practiced a sport at least once a week and who wished to RTS were included. The injury had occurred less than one month before inclusion, and patients were all initially examined by the same experienced orthopaedic surgeon. Exclusion criteria were the presence of a fracture and suspected syndesmosis injury (i.e. mechanism of injury involving dorsiflexion and external rotation of the foot, pain during palpation of the anteroinferior tibio-fibular ligament or the dorsiflexion lunge, a positive squeeze test) [16]. A prescription for personalized rehabilitation was given to the patients on the day of the consultation.
Table 1.
Demographic characteristics
| Participants | |
|---|---|
| Sex (men/women) | 64 (36/28) |
| Age (years ± SD) | 34.8 ± 13.2 |
| Type of sport, n (%) | |
| Pivot contact | 19 (29.7%) |
| Pivot | 22 (34.4%) |
| In line | 23 (35.9%) |
| Level of practice, n (%) | |
| Professional | 2 (3.2%) |
| Intensive (> 6 h per week) | 21 (32.8%) |
| Regular (2–6 h per week) | 34 (53%) |
| Leisure (< 2 h per week) | 7 (10.9%) |
Patient Follow-up
Two months after injury, all patients completed the Ankle-GO score supervised by the same experienced physical therapist who was not managing rehabilitation. The Ankle-GO is a valid, reliable, objective score [10] including 6 items selected on the basis of the PAASS framework from the International Ankle Consortium [5] and considered to be relevant for the monitoring of LAS patients [2, 9]. The total score is 25 points and the method of calculation is summarized in Table 2. Four tests in the Ankle-GO evaluate functional performance: the Single Leg Stance on a firm surface [17], the modified Star Excursion Balance Test [18, 19], the Side Hop Test [20], and the Figure-of-8 Test [21]. The two subscales of the Foot and Ankle Ability Measure to evaluate activities in daily life (FAAMadl) and sports (FAAMsport) [22], as well as the Ankle Ligament Reconstruction-Return to Sport after Injury (ALR-RSI) [23] were also used to assess the patient’s perception.
Table 2.
Ankle-GO score calculation
| TESTS | RAW VALUES | POINTS | MAXIMUM SCORE | ||
|---|---|---|---|---|---|
| FUNCTIONAL PERFORMANCE TESTING | Single leg stance test (SLS) | > 3 errors | 0 | 3 | |
| 1–3 errors | 1 | ||||
| 0 error | 2 | ||||
| No apprehension | + 1 | ||||
| Star excursion balance test (SEBT) | < 90% | 0 | 7 | ||
| 90–95% | 2 | ||||
| > 95% | 4 | ||||
| Anterior (ANT) > 60% | + 1 | ||||
| Posteromedial (PM) > 90% | + 1 | ||||
| No apprehension | + 1 | ||||
| Side hop Test (SHT) | > 13 s | 0 | 5 | ||
| 10–13 s | 2 | ||||
| < 10 s | 4 | ||||
| No apprehension | + 1 | ||||
| Figure-of-8 hop Test (F8T) | > 18 s | 0 | 3 | ||
| 13–18 s | 1 | ||||
| < 13 s | 2 | ||||
| No apprehension | + 1 | ||||
| PATIENT REPORTED OUTCOME MEASURE | Foot and Ankle Ability Measure (FAAM) | Activities of Daily Living | < 90% | 0 | 2 |
| 90–95% | 1 | ||||
| > 95% | 2 | ||||
| Sport | < 80% | 0 | 2 | ||
| 80–95% | 1 | ||||
| > 95% | 2 | ||||
| Ankle ligament reconstruction-return to sport after injury (ALR-RSI) | < 55% | 0 | 3 | ||
| 55–63% | 1 | ||||
| 63–76% | 2 | ||||
| > 76% | 3 | ||||
| Ankle-GO | 25 | ||||
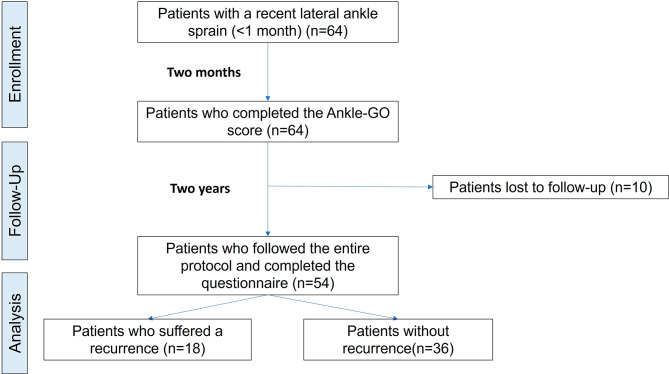
Patients were contacted by a blind assessor two years after the initial LAS and asked if they suffered a recurrent LAS. Recurrent LAS was defined as a new ipsilateral LAS in the same location and of the same type [24]. The mechanism of injury was also reported (“contact” or “non-contact”). The study cohort is summarized in a flow chart. (Fig. 1). Patients provided informed consent, and this study received Institutional Ethics Approval (IRB00010835).
Fig. 1.
Flowchart of inclusion and analysis
Data Analysis
The analysis and presentation of data were consistent with the CHecklist for statistical Assessment of Medical Papers (CHAMP) [25]. There were two groups according to the recurrence or not of LAS (primary outcome). Data were checked for normality and homogeneity of variance. The relationship between potential predictive variables and recurrent LAS was tested using the Chi-square test for categorical measurements and the Mann-Whitney or independent t-tests. Variables with a P value < 0.20 were considered for further analysis in logistic regression. The discriminant validity of all items and the total Ankle-GO score was assessed using independent t-tests and Cohen’s d effect sizes with 95% confidence intervals (CIs) between patients with recurrent LAS at two years and those without. Effect sizes were interpreted as small: d = 0.20–0.49, moderate: d = 0.50–0.79, and large: d ≥ 0.80 [26].
The predictive validity of the two-month Ankle-GO score to identify patients who would have a recurrent LAS was also evaluated with the receiver operating characteristic curve. The area under the curve (AUC) was determined with a precision score considered to be null (AUC = 0.5), low (0.5 < AUC < 0.7), fair to good (0.7 ≤ AUC < 0.9), high (0.9 ≤ AUC < 1), or perfect (AUC = 1). The optimal cut-off score was calculated using the Youden index (J = sensitivity + specificity − 1). Variables were then recoded into dichotomous variables that were either above or below the cut-off point to simplify interpretation of risk factors and the related odds ratios [27, 28]. Because other factors could influence the risk of reinjury [12], multivariate logistic regression (stepwise method) was performed to determine whether the chosen variables (i.e. only those with a predictive p value < 0.20) were associated with reinjury [28, 29]. Odds ratios (OR) and 95% CI) were reported for the variables associated with an increased risk of reinjury. The statistical analysis was performed using JASP (Amsterdam 0.12.2.0). The level of significance was set at 0.05.
Results
Two years after the initial LAS, fifty-four patients (85%) responded to the survey. Eighteen (33.3%) of these suffered a recurrent LAS (Table 3). All of these were non-contact injuries. To determine the potential ability of the parameters to LAS recurrence, we first identified the variables that showed differences between the two groups (injured vs. non-injured). In total, 9 variables met the criterion of p < 0.20: the two FAAM subscales, all of the SEBT components (ANT, PM, PL and COMP), the SHT, sex and the Ankle-GO score (Tables 3 and 4).
Table 3.
Comparison between injured and non-injured patients at the end of the follow up period
| Lost to follow-up | 10/64 (15%) | ||
| Reinjury (n = 54) | YES, n = 18 (33.3%) | NO, n = 36 (66.6%) | p value |
| Sex (women/men) | 18 (4/14) | 36 (19/17) | 0.032 |
| Age (years ± SD) | 36.8 ± 9.7 | 34.3 ± 14.7 | 0.51 |
| Ankle-GO (points ± SD) | 5.4 ± 2.8 | 9.1 ± 4.5 | 0.002 |
| Type of reinjury | 18 ankle sprains (100% non-contact) | ||
| Type of sport, n (%) | |||
| Pivot contact | 7 (38.9%) | 8 (22.2%) | 0.259 |
| Pivot | 2 (11.1%) | 10 (27.8%) | |
| In line | 9 (50%) | 18 (50%) | |
| Level of sport, n (%) | |||
| Professional | 1 (5.6%) | 1 (2.8%) | 0.794 |
| Intensive (> 6 h per week) | 7 (38.9) | 11 (30.5%) | |
| Regular (2–6 h per week) | 8 (44.4%) | 21 (58.6%) | |
| Leisure (< 2 h per week) | 2 (11.1%) | 3 (8.3%) | |
Table 4.
Mean (± SD) Ankle-GO scores at two months in patients with a recurrent LAS two years after the initial LAS and in those without
| Injured | Uninjured | p-value | Cohen’s d | 95% CI Lower limit | 95% CI Upper limit | |
|---|---|---|---|---|---|---|
| FAAMadl (%) | 78.6 ± 14.4 | 87.2 ± 14.8 | 0.046 | 0.3 | 0.01 | 1.17 |
| FAAMsport (%) | 51.4 ± 17.2 | 61.3 ± 23.9 | 0.124 | 0.29 | -0.12 | 1.02 |
| ALR-RSI (%) | 40.6 ± 21 | 46.1 ± 22.3 | 0.386 | 0.29 | -0.32 | 0.82 |
| SLS (errors) | 3.7 ± 3.2 | 3.1 ± 2.7 | 0.447 | 0.29 | -0.79 | 0.35 |
| SEBT Comp (%) | 76.6 ± 8.2 | 81.2 ± 6.8 | 0.035 | 0.3 | 0.05 | 1.20 |
| SEBT Ant (%) | 57.7 ± 7.2 | 61.7 ± 6.2 | 0.039 | 0.3 | 0.03 | 1.19 |
| SEBT PM (%) | 88.9 ± 9.6 | 93.7 ± 7.9 | 0.053 | 0.3 | -0.01 | 1.12 |
| SEBT PL (%) | 83 ± 11.8 | 88.8 ± 9.9 | 0.065 | 0.3 | -0.03 | 1.12 |
| SHT (s) | 25 ± 8.2 | 20.1 ± 12.5 | 0.138 | 0.29 | -1.01 | 0.14 |
| F8T (s) | 23.3 ± 9.6 | 19.9 ± 9.7 | 0.234 | 0.29 | -0.92 | 0.22 |
FAAMadl−sport= Foot and Ankle Ability Measures-Activities of daily living & sport subscales; ALR-RSI = Ankle Ligament Reconstruction Return to Sport after Injury; SLS = Single Leg Stance; SEBT = Star Excursion Balance Test; Comp = Composite score, Ant = Anterior, PM = posteromedial, PL = posterolateral; SHT = Side Hop Test; F8T = Figure of eight test
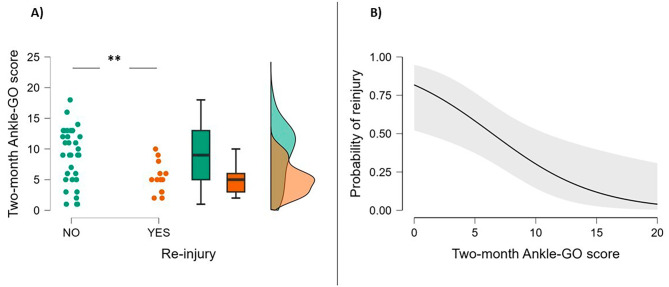
The Ankle-GO score at two months was significantly lower in patients with recurrent LAS (p < 0.002) (Fig. 2; Table 3). Of all the items of the Ankle-GO score, only the FAAMadl, anterior direction and the SEBT composite score were found to be significantly lower in patients with recurrent LAS (Table 4).
Fig. 2.
(a) Ankle-GO scores at two months in patients with a recurrent LAS within two years and those without (b) Estimate plot of the probability of recurrence. **p < 0.01
The predictive capacity of the 2-month Ankle-GO score to identify patients who would have a recurrent LAS within 2 years after the initial injury was good (AUC = 0.75; 95% CI: 0.62–0.88; p = 0.003). A Youden index of 0.47 was observed for a cut-off score of 8 points, corresponding to a sensitivity of 83% and a specificity of 64%. Thus, Ankle-GO scores were re-coded as being either above or below this cut-off point. The full model containing all predictors (Ankle-GO score and sex) was statistically significant (p < 0.001), indicating that the model identified participants at a higher risk of having a recurrent LAS during follow-up. The model explained between 25% (Cox and Snell R²) and 34% (Nagelkerke R²) of the variance in recurrent LAS’s and correctly classified 78% of cases.
The Ankle-GO score was the only statistically significant contribution to the model on multivariate logistic regression, with an OR of 8.6 (95% CI: 2 to 37.2, p = 0.004). That is, patients who scored below 8 points on the Ankle-GO score two months after an initial LAS had a nearly 9 times greater risk of reinjury within the next two years. There was also a trend (OR = 3.8; 95% CI: 0.9 to 15.5, p = 0.065) showing that woman had a risk of reinjury that was almost 4 times greater than men, controlling for other factors in the model.
Discussion
The main objective of this study was to evaluate the capacity of the Ankle-GO score to predict the risk of recurrent LAS two years after the initial injury. First, our results confirmed a high rate of recurrence, with up to 30% of patients reporting a new LAS [15, 30, 31]. The cause of this high rate of reinjury is often explained by poor management of RTS [5] as no evidence-based criteria have been published to date to help make this decision [2, 9]. The goal of the Ankle-GO score is to address this need, and assist clinicians in the decision-making process [10].
The present study showed that the two-month Ankle-GO score effectively predicts the two-year post-LAS risk of recurrence. Scores were significantly lower in patients with reinjury than in those without (Table 3), with a difference between the two groups that was greater than the established minimum detectable change (1.2 points) [10]. In particular, patients with a score < 8 points on the Ankle-Go scale had a nearly 9 times greater risk of recurrence during the first two years after LAS.
To the best of our knowledge, this is the first objective RTS criterion to identify individuals with an increased risk of reinjury following LAS. Interestingly, the same cut-off score (8-points) was reported to identify patients who will return to their preinjury level of sports 4 months after LAS, with a sensitivity of 67% and a specificity of 92% [10]. This ability to predict both the level of play after the RTS and the risk of reinjury is due to the multidimensional design of the Ankle-GO. Because the causes of reinjury and the development of CAI are multifactorial [12], this score was designed to provide a comprehensive assessment, including various components to evaluate all potential deficits associated with LAS and CAI [4, 5, 32]. The selection of items and the rating system for the Ankle-GO score (Table 2) was described in a previous study [10]. In summary, the score includes several items (questionnaires and functional tests) that were chosen according to the PAASS framework [5], clinical guidelines [33, 34] and systematic reviews with expert opinions on RTS [2, 9]. All items were selected based on their relevance, reliability and ability to differentiate CAI patients from copers and healthy individuals [11]. The Ankle-GO is a valid and reliable score [10] including 2 patient-reported outcome measures (FAAM and ALR-RSI), assessing perceived ankle confidence and psychological readiness to RTS [23, 35]. Low scores on these questionnaires are strongly associated with a poor prognosis and greater disability in those with CAI [36, 37]. Functional assessments are highly recommended for the management of LAS patients [4, 33]. Thus, the Ankle-GO score also includes 4 functional tests to evaluate postural control, hopping, jumping and agility, which are frequently impaired following LAS and CAI [2, 5, 9, 38]. Furthermore, and as recommended by Caffrey et al., [21] the feeling of instability reported during the tests was also considered when calculating the Ankle-GO.
When comparing the two-month scores, only the FAAMadl and SEBT scores were significantly lower in patients with a recurrent LAS (Table 4). Because no single component of the Ankle-GO score independently predicted the risk of reinjury, the use of combined scores rather than single evaluations are advisable in patients with LAS. It is important to note that the two-month values of all of the Ankle-GO items were below the criteria used to define CAI (FAAMadl scale, ˂90% and FAAMsport scale, ˂80%) [15] in both groups. Similarly, the mean functional test values identified poor balance control during the SLS (> 3 errors) [39] and SEBT (composite score < 89.6%) [40], as well as slow agility test performances (> 12.8s on the SHT and > 17.36s on the F8T) [11, 39] in all patients, whatever their reinjury status. Only posteromedial performance on the SEBT exceeded the cut-off score of (> 91%) [39] in patients with no recurrent LAS, although the difference with the injured group was not significant (93.7 ± 7.9 vs. 88.9 ± 9.6 respectively, p = 0.053). This confirms the study by Mcann et al., [8] which showed that the resolution of structural and functional impairment was incomplete, and revealed LAS-related activity limitations at the time of RTS (after an average of 12 days). Although the RTS occurred within a week following LAS in 80% of patients [6, 7], this decision should be based on objective criteria rather than time-related considerations.
Very few prospective studies have evaluated the role of sex in the risk of recurrence in patients with an initial LAS [41]. Results show the risk of reinjury is almost 4 times higher in women than in men, with no baseline differences in the two-month Ankle-GO score (7.7 vs. 8 points, p = 0.8, respectively). Despite conflicting evidence on the influence of sex on LAS [12], women seem to be at a higher risk of LAS [33, 42, 43] and of developing CAI [44] than men. A recent study has also shown that there was a higher risk of recurrence in women following ankle surgery [45]. Because of these differences, clinicians should use the Ankle-GO score for both sexes but be more cautious about low scores in women. Unlike previous results, age was not identified as a risk factor for reinjury in our study [12, 46]. Several studies have shown that patients under the age of 24 were at a higher risk of LAS [28, 47]. In the current study, 13 patients (20%) were under 25, and only one had recurrent LAS. Further larger studies targeting adolescents should be performed using the Ankle-GO score to reduce the risk of reinjury.
The socioeconomic costs of poor management of initial LAS can be high because of the high rates of recurrence and CAI [30]. The economic burden of suboptimal care and follow-up after initial LAS has numerous causes including the costs of direct and indirect healthcare and long-term rehabilitation as well as the loss of productivity and quality of life from CAI which diminishes the individual’s ability to perform physical activities and potentially leads to a sedentary lifestyles with associated health problems [48, 49]. A long-term analysis of costs after LAS is essential to assess treatment efficacy, and to determine if it is cost-effective and associated with a favourable clinical outcome [30].
The use of the free application Ankle-GO (https://anklego.com/) during the late phase of rehabilitation allows to quickly identify, in a clinician-friendly and reliable way, patients who are at risk of a new injury.
Strength and Limitations
To our knowledge, this is the first prospective study to evaluate the value of objective RTS criteria to predict the risk of reinjury within two years. However, this study has certain limitations. First, it is well known that the risk of reinjury after LAS is multifactorial [12]. Although age, sport and level of play were included in the predictive model and did not influence recurrence, we did not consider all known risk factors of LAS reinjury. For instance, although the severity of the injury was systematically assessed by the surgeon (pain, swelling, ligament laxity) this was not considered in the analysis. Indeed, very recently Netterstrom et al. 2022 in their meta-analysis reported limited and contradictory evidence that clinical tests can provide an accurate assessment of injury severity [50]. Previously, Pourkazemi et al. in their systematic review raised concerns about the validity of grading systems based solely on symptoms [51]. Furthermore, they revealed that the severity of the initial ankle sprain does not necessarily predict re-injury.
The exact number and content of rehabilitation sessions for each patient was not controlled and may have influenced the results. As the International Ankle Consortium guidelines recommend physical therapy on a case-by-case basis according to each patient’s specific individual deficits [32], a detailed analysis of the type of rehabilitation was beyond the scope of this study. It would therefore seem appropriate to assess the influence of rehabilitation content on the Ankle-Go score at the time of RTS.
In addition, reinjury during follow-up was based on a single survey at two years. Thus, the number, severity and exact timing of recurrence were not examined. This study is an important step in establishing objective RTS criteria after LAS for secondary prevention. However, it is important to note that the Ankle-GO does not include all the items of the PAASS framework [5]. It could be important to combine this score with other measures such as strength, range of motion or neurocognitive assessments [52] in order to obtain a broader overview of patients’ deficits. Further studies using the Ankle-GO score are needed to assess its ability to identify potential copers (secondary prevention), predict the development of CAI (tertiary prevention), as well as the occurrence of a first ankle sprain in a healthy population (primary prevention) [53, 54].
Clinical Implications
The decision to RTS should not be primarily based on time but on objective criteria. The Ankle-GO score is a cost-effective, rapid (takes less than 20 min), and user-friendly tool for clinicians.
The Ankle-GO score includes various components that target critical outcomes associated with LAS to allow clinicians to identify remaining impairment and reduce the risk of reinjury. During the later stages of rehabilitation and on the RTS continuum, it can provide a goal-oriented assessment similar to the clinical assessment of acute lateral ankle sprain injuries [32]. For example, dynamic postural control exercises should be prescribed in patients with a low Ankle-GO score and reduced SEBT values to manage remaining deficits.
Conclusions
A low Ankle-GO score is associated with an increased risk of reinjury within 2 years after LAS. Patients with a score < 8 points two months after the initial LAS had a 9 times greater risk of reinjury. In addition, there was a trend towards a higher risk of re-injury in women. The Ankle-GO score is the first objective tool to help clinicians objectively evaluate patients for the RTS. Further studies are needed to assess the predictive value of the Ankle-GO score for the development of CAI.
Abbreviations
- LAS
Lateral Ankle Sprain
- RTS
Return to Sport
- CAI
Chronic Ankle Instabily
- ALR-RSI
Ankle Ligament Reconstruction-Return to Sport after Injury
- PAASS
Pain, Ankle impairments, Athlete perception, Sensorimotor control, Sport performance
- CHAMP
CHecklist for statistical Assessment of Medical Papers
- OR
Odds ratios
- 95% CI
95% confidence intervals
- AUC
Area Under the Curve
- FAAMadl−sport
Foot and Ankle Ability Measures-Activities of daily living & sport subscales
- SLS
Single Leg Stance
- SEBT
Star Excursion Balance Test
- Comp
Composite score
- Ant
Anterior
- PM
Posteromedial
- PL
Posterolateral
- SHT
Side Hop Test
- F8T
Figure of eight test
Author Contributions
According to the definition given by the International Committee of Medical Journal Editors (ICMJE), the authors listed qualify for authorship based on making one or more of the substantial contributions to the intellectual content of the manuscript. Dr Brice PICOT, François FOURCHET, Ronny LOPES and Alexandre HARDY collaborated in designing the Ankle-GO score, were responsible for the original conception of the study and obtained ethical approval and co-authored the manuscript. Gauthier RAULINE and Kinan FREIHA helped recruit participants analysed the initial data and co-authored the manuscript. Dr Eugénie VALENTIN helped with data analysis and interpretation of the results and co-authored the manuscript. Dr Pieter D’HOOGHE provided technical advice on the clinic testing protocol, helped with interpretation of the results and co-authored the manuscript.
Funding
None.
Data Availability
Data are available upon reasonable request. Please contact: alexandre.hardy@me.com.
Declarations
Ethics Approval and Consent to Participate
This study received Institutional Ethics Approval (IRB00010835) from the scientific board of Ramsay Santé, France. Participants gave informed consent to participate in the study before taking part. Patients provided informed written consent to participate in this study. The study was performed in accordance with the standards of ethics outlined in the Declaration of Helsinki.
Consent for Publication
Not applicable.
Competing Interests
Brice PICOT, François FOURCHET, Ronny LOPES, Gauthier RAULINE, Kinan FREIHA, Pieter D’HOOGHE, Eugénie VALENTIN and Alexandre HARDY declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Verhagen Ea, Tulder LM, van Beek M, van der Bouter AJ, van Mechelen LM. An economic evaluation of a proprioceptive balance board training programme for the prevention of ankle sprains in volleyball. Br J Sports Med. 2005;39:111–5. doi: 10.1136/bjsm.2003.011031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tassignon B, Verschueren J, Delahunt E, Smith M, Vicenzino B, Verhagen E, et al. Criteria-based return to Sport decision-making following lateral ankle Sprain Injury: a systematic review and narrative synthesis. Sports Med. 2019;49:601–19. doi: 10.1007/s40279-019-01071-3. [DOI] [PubMed] [Google Scholar]
- 3.Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016;44:995–1003. doi: 10.1177/0363546516628870. [DOI] [PubMed] [Google Scholar]
- 4.Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54:572–88. doi: 10.4085/1062-6050-344-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith MD, Vicenzino B, Bahr R, Bandholm T, Cooke R, Mendonça LDM et al. Return to sport decisions after an acute lateral ankle sprain injury: introducing the PAASS framework-an international multidisciplinary consensus. Br J Sports Med. 2021;bjsports-2021-104087. [DOI] [PubMed]
- 6.Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA. The Epidemiology of Lateral Ligament Complex Ankle Sprains in National Collegiate Athletic Association Sports. Am J Sports Med. 2017;45:201–9. doi: 10.1177/0363546516660980. [DOI] [PubMed] [Google Scholar]
- 7.McKeon JMM, Bush HM, Reed A, Whittington A, Uhl TL, McKeon PO. Return-to-play probabilities following new versus recurrent ankle sprains in high school athletes. J Sci Med Sport. 2014;17:23–8. doi: 10.1016/j.jsams.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 8.McCann R, Kosik K, Terada M, Gribble P. Residual impairments and Activity limitations at Return to play from a lateral ankle sprain. Int J Athletic Therapy Train. 2018;23:83–8. doi: 10.1123/ijatt.2017-0058. [DOI] [Google Scholar]
- 9.Wikstrom EA, Mueller C, Cain MS. Lack of Consensus on Return-to-Sport Criteria following lateral ankle sprain: a systematic review of Expert opinions. J Sport Rehabilitation. 2020;29:231–7. doi: 10.1123/jsr.2019-0038. [DOI] [PubMed] [Google Scholar]
- 10.Picot B, Lopes R, Rauline G, Fourchet F, Hardy A. Development and validation of the Ankle-GO score for Discriminating and Predicting Return-to-Sport outcomes after lateral ankle sprain. Sports Health. 2023;19417381231183647. [DOI] [PMC free article] [PubMed]
- 11.Picot B, Hardy A, Terrier R, Tassignon B, Lopes R, Fourchet F. Which Functional Tests and Self-Reported Questionnaires Can Help Clinicians Make Valid Return to Sport Decisions in Patients With Chronic Ankle Instability? A Narrative Review and Expert Opinion. Frontiers in Sports and Active Living [Internet]. 2022 [cited 2022 Jun 8];4. Available from: https://www.frontiersin.org/article/10.3389/fspor.2022.902886. [DOI] [PMC free article] [PubMed]
- 12.Delahunt E, Remus A. Risk factors for lateral ankle sprains and chronic ankle instability. J Athl Train. 2019;54:611–6. doi: 10.4085/1062-6050-44-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 14.Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in Epidemiological studies. Commun Stat - Simul Comput. 2010;39:860–4. doi: 10.1080/03610911003650383. [DOI] [Google Scholar]
- 15.Gribble PA, Delahunt E, Bleakley CM, Caulfield B, Docherty CL, Fong DT-P, et al. Selection criteria for patients with chronic ankle instability in Controlled Research: A position Statement of the International Ankle Consortium. J Athl Train. 2014;49:121–7. doi: 10.4085/1062-6050-49.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Netterström-Wedin F, Bleakley C. Diagnostic accuracy of clinical tests assessing ligamentous injury of the ankle syndesmosis: a systematic review with meta-analysis. Phys Ther Sport. 2021;49:214–26. doi: 10.1016/j.ptsp.2021.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Riemann B, Caggiano A, Lephart NM. Examination of a clinical method of assessing Postural Control during a functional performance Task. J Sport Rehabilitation. 1999;8:171–83. doi: 10.1123/jsr.8.3.171. [DOI] [Google Scholar]
- 18.Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47:339–57. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Picot B, Terrier R, Forestier N, Fourchet F, McKeon PO. The Star Excursion Balance Test: an Update Review and practical guidelines. Int J Athl Ther Train. 2021;1:1–9. [Google Scholar]
- 20.Docherty CL, Arnold BL, Gansneder BM, Hurwitz S, Gieck J. Functional-performance deficits in volunteers with functional ankle instability. J Athl Train. 2005;40:30–4. [PMC free article] [PubMed] [Google Scholar]
- 21.Caffrey E, Docherty CL, Schrader J, Klossnner J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J Orthop Sports Phys Ther. 2009;39:799–806. doi: 10.2519/jospt.2009.3042. [DOI] [PubMed] [Google Scholar]
- 22.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the foot and ankle ability measure (FAAM) Foot Ankle Int. 2005;26:968–83. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 23.Sigonney F, Lopes R, Bouché P-A, Kierszbaum E, Moslemi A, Anract P, et al. The ankle ligament reconstruction-return to sport after injury (ALR-RSI) is a valid and reproducible scale to quantify psychological readiness before returning to sport after ankle ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28:4003–10. doi: 10.1007/s00167-020-06020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, Finch CF, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)) Br J Sports Med. 2020;54:372–89. doi: 10.1136/bjsports-2019-101969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mansournia MA, Collins GS, Nielsen RO, Nazemipour M, Jewell NP, Altman DG, et al. A CHecklist for statistical Assessment of Medical Papers (the CHAMP statement): explanation and elaboration. Br J Sports Med. 2021;55:1009–17. doi: 10.1136/bjsports-2020-103652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen J. Statistical Power Analysis for the behavioral sciences. 2. New York: Routledge; 1988. [Google Scholar]
- 27.Peat J, Barton B. Medical statistics: a guide to data analysis and critical appraisal. Wiley; 2008.
- 28.Pourkazemi F, Hiller CE, Raymond J, Black D, Nightingale EJ, Refshauge KM. Predictors of recurrent sprains after an index lateral ankle sprain: a longitudinal study. Physiotherapy. 2018;104:430–7. doi: 10.1016/j.physio.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 29.Hosmer D, Lemeshow S, Sturdivant R. Model-Building Strategies and Methods for Logistic Regression. Applied Logistic Regression [Internet]. John Wiley & Sons, Ltd; 2013 [cited 2024 Jan 27]. p. 89–151. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/9781118548387.ch4.
- 30.Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT-P, et al. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50:1493–5. doi: 10.1136/bjsports-2016-096188. [DOI] [PubMed] [Google Scholar]
- 31.Malliaropoulos N, Ntessalen M, Papacostas E, Longo UG, Maffulli N. Reinjury after Acute lateral ankle sprains in Elite Track and Field athletes. Am J Sports Med. 2009;37:1755–61. doi: 10.1177/0363546509338107. [DOI] [PubMed] [Google Scholar]
- 32.Delahunt E, Bleakley CM, Bossard DS, Caulfield BM, Docherty CL, Doherty C, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br J Sports Med. 2018;52:1304–10. doi: 10.1136/bjsports-2017-098885. [DOI] [PubMed] [Google Scholar]
- 33.Martin RL, Davenport TE, Fraser JJ, Sawdon-Bea J, Carcia CR, Carroll LA, et al. Ankle Stability and Movement Coordination Impairments: lateral ankle ligament sprains revision 2021: clinical practice guidelines linked to the International classification of Functioning, Disability and Health from the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2021;51:CPG1–80. doi: 10.2519/jospt.2021.0302. [DOI] [PubMed] [Google Scholar]
- 34.Martin RL, Davenport TE, Paulseth S, Wukich DK, Godges JJ. Ankle Stability and Movement Coordination Impairments: ankle ligament sprains: clinical practice guidelines linked to the International classification of Functioning, disability and Health from the Orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Therapy. 2013;43:A1–40. doi: 10.2519/jospt.2013.0305. [DOI] [PubMed] [Google Scholar]
- 35.Carcia CR, Martin RL, Drouin JM. Validity of the foot and ankle ability measure in athletes with chronic ankle instability. J Athl Train. 2008;43:179–83. doi: 10.4085/1062-6050-43.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suttmiller AMB, Cavallario JM, Baez SE, Martinez JC, McCann RS. Perceived Instability, Pain, and psychological factors for prediction of function and disability in individuals with chronic ankle instability. J Athl Train. 2022;57:1048–54. doi: 10.4085/1062-6050-0605.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suttmiller AMB, McCann RS. Injury-related fear in individuals with and without chronic ankle instability: a systematic review. J Sport Rehabil. 2021;30:1203–12. doi: 10.1123/jsr.2021-0015. [DOI] [PubMed] [Google Scholar]
- 38.Schurz AP, Wagemans J, Bleakley C, Kuppens K, Vissers D, Taeymans J. Impairment-based assessments for patients with lateral ankle sprain: a systematic review of measurement properties. PLoS ONE. 2023;18:e0280388. doi: 10.1371/journal.pone.0280388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Linens SW, Ross SE, Arnold BL, Gayle R, Pidcoe P. Postural-stability tests that identify individuals with chronic ankle instability. J Athl Train. 2014;49:15–23. doi: 10.4085/1062-6050-48.6.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Butler RJ, Lehr ME, Fink ML, Kiesel KB, Plisky PJ. Dynamic balance performance and Noncontact Lower Extremity Injury in College Football players: an initial study. Sports Health. 2013;5:417–22. doi: 10.1177/1941738113498703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wikstrom EA, Cain MS, Chandran A, Song K, Regan T, Migel K, et al. Lateral ankle sprain and subsequent ankle sprain risk: a systematic review. J Athl Train. 2021;56:578–85. doi: 10.4085/1062-6050-168-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of Ankle Sprain Injury: a systematic review and Meta-analysis of prospective epidemiological studies. Sports Med. 2014;44:123–40. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 43.Mason J, Kniewasser C, Hollander K, Zech A. Intrinsic risk factors for Ankle Sprain Differ between male and female athletes: a systematic review and Meta-analysis. Sports Med Open. 2022;8:139. doi: 10.1186/s40798-022-00530-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tanen L, Docherty CL, Van Der Pol B, Simon J, Schrader J. Prevalence of chronic ankle instability in High School and Division I athletes. Foot Ankle Spec. 2014;7:37–44. doi: 10.1177/1938640013509670. [DOI] [PubMed] [Google Scholar]
- 45.Thès A, Andrieu M, Cordier G, Molinier F, Benoist J, Colin F, et al. Five-year clinical follow-up of arthroscopically treated chronic ankle instability. Orthopaedics & Traumatology: Surgery & Research; 2023. [DOI] [PubMed] [Google Scholar]
- 46.Hiller CE, Refshauge KM, Herbert RD, Kilbreath SL. Intrinsic predictors of lateral ankle sprain in adolescent dancers: a prospective cohort study. Clin J Sport Med. 2008;18:44. doi: 10.1097/JSM.0b013e31815f2b35. [DOI] [PubMed] [Google Scholar]
- 47.Fousekis K, Tsepis E, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012;40:1842–50. doi: 10.1177/0363546512449602. [DOI] [PubMed] [Google Scholar]
- 48.Janssen KW, Hendriks MRC, van Mechelen W, Verhagen E. The cost-effectiveness of measures to prevent recurrent ankle sprains: results of a 3-Arm randomized controlled trial. Am J Sports Med. 2014;42:1534–41. doi: 10.1177/0363546514529642. [DOI] [PubMed] [Google Scholar]
- 49.Lin C-WC, Uegaki K, Coupé VMH, Kerkhoffs GM, van Tulder MW. Economic evaluations of diagnostic tests, treatment and prevention for lateral ankle sprains: a systematic review. Br J Sports Med. 2013;47:1144–9. doi: 10.1136/bjsports-2012-090319. [DOI] [PubMed] [Google Scholar]
- 50.Netterström-Wedin F, Matthews M, Bleakley C. Diagnostic accuracy of clinical tests assessing Ligamentous Injury of the talocrural and subtalar joints: a systematic review with Meta-analysis. Sports Health. 2022;14:336–47. doi: 10.1177/19417381211029953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pourkazemi F, Hiller CE, Raymond J, Nightingale EJ, Refshauge KM. Predictors of chronic ankle instability after an index lateral ankle sprain: a systematic review. J Sci Med Sport. 2014;17:568–73. doi: 10.1016/j.jsams.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 52.Maricot A, Corlùy H, De Pauw K, Lathouwers E, Meeusen R, Roelands B, et al. Deficits in neurocognitive performance in patients with chronic ankle instability during a neurocognitive balance task – A retrospective case-control study. Phys Ther Sport. 2024;66:1–8. doi: 10.1016/j.ptsp.2023.12.009. [DOI] [PubMed] [Google Scholar]
- 53.Wikstrom EA, Hubbard-Turner T, McKeon PO. Understanding and treating lateral ankle sprains and their consequences: a constraints-based approach. Sports Med. 2013;43:385–93. doi: 10.1007/s40279-013-0043-z. [DOI] [PubMed] [Google Scholar]
- 54.Wikstrom EA, Brown CN. Minimum reporting standards for copers in chronic ankle instability research. Sports Med. 2014;44:251–68. doi: 10.1007/s40279-013-0111-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. Please contact: alexandre.hardy@me.com.