Abstract
BACKGROUND:
During pregnancy, the body requires more complex nutritional intake. Therefore, problems with fulfilling nutrition during pregnancy occur often. One of the most common nutritional problems in pregnancy is iron deficiency anemia, the most widespread micronutrient problem and the most difficult to overcome worldwide. This study aimed to determine awareness and prevention behavior associated with the incidence of iron deficiency in pregnant women living in urban slum areas.
MATERIALS AND METHODS:
This was a cross-sectional study. The data collection used KoboToolbox, an Android-based tool. Iron status was examined by serum ferritin level assay using ELISA at the Microbiology Laboratory Unit of Hasanuddin University Hospital.
RESULTS:
The prevalence of pregnant women who experienced iron deficiency was 78%. The logistic regression analysis showed that poor awareness (AOR = 3.03, CI 95% 1.26-7.29, P = 0.013) and practices in taking iron enhancers (AOR = 2.85, CI 95% 1.18–6.92, P = 0.020) became the main factors associated with iron deficiency among pregnant women.
CONCLUSIONS:
Poor awareness and practices regarding consuming iron enhancers increased the risk of iron deficiency among pregnant women living in urban slum areas. Iron deficiency is a major health concern for pregnant women, especially those living in slum settlements, which must be addressed. A more optimal healthcare system for pregnant women may reduce the incidence of iron anemia in pregnancy by improving health promotion and optimizing healthcare services.
Keywords: Awareness and prevention, maternal iron deficiency, serum ferritin level, Urban slum areas
Introduction
Increasingly complex nutrition is required by the body during pregnancy. Therefore, difficulties in fulfilling these nutrition requirements are common. One of the most common nutritional problems in pregnant women is iron deficiency anemia, the most widespread micronutrient problem and the most difficult to overcome worldwide.[1]
The incidence of anemia is still high, affecting a fairly large proportion of people worldwide. According to World Health Organization (WHO) data, approximately 29.9% of women globally in the 15–49 age group have anemia. This is equivalent to more than half a billion people. The prevalence is 29.6% in non-pregnant women and 36.5% in pregnant women.[2] The incidence of anemia in pregnant women is very high in lower-middle-income countries (LMICs), especially in Southeast Asia and Africa. Based on the World Bank income category, the prevalence of anemia in pregnant women in LMICs is 45%. Meanwhile, in high-income countries, the prevalence of anemia in pregnant women is only around 17%.[3]
Anemia in pregnancy is potentially harmful to the mother and child. Therefore, it requires serious attention from all parties involved in health services. Anemia in pregnant women can cause complications such as bleeding, increased risk of birthweight, abortion, and increased risk of mortality for both mother and baby.[4] Low hemoglobin levels in pregnant women can impact fetal growth and development. Hence, pregnant women with a history of anemia are more likely to have infants with low birthweight.[5]
Considering the impact of iron deficiency anemia on pregnant women and the potential future health conditions, preventing anemia during pregnancy is crucial. Poor awareness and prevention restrict efforts to reduce the prevalence of iron deficiency anemia.[6] According to Rogers' theory (1962), commonly known as the AIETA theory, the body undergoes a series of sequential stages while adopting new behaviors: awareness, interest, evaluation, trial, and adoption. If the behavior adoption through this process is built on awareness, the behavior will persist.
Knowledge and awareness can powerfully influence behavior and better habits, such as fulfilling the nutritional needs that the body requires during pregnancy;[7] approximately 95% of iron deficiency anemia is caused by diet.[8] A lack of maternal awareness of iron deficiency anemia causes the condition in most pregnancies.[9] The underlying cause of this high incidence is low education, which affects the level of knowledge and awareness regarding the causes of anemia, its impact, and its prevention. Awareness of iron deficiency anemia greatly determines the mother's behavior during pregnancy. Therefore, awareness of the causes of anemia and preventive behavior toward its risk factors play a significant role in preventing it in pregnancy.
Materials and Methods
Study design and setting
This sub-study of the Indonesian Birth Cohort Study was based in the Tallo subdistrict, one of the heavy informal settlements in Makassar City, Indonesia. We performed a cross-sectional study that aimed to describe the iron deficiency awareness and precautions of pregnant women.
Study participant and sampling
The sample in this study was all pregnant women in the second and third trimesters who were residents in the study site. The data on these women were obtained from three public health center work areas in the Tallo subdistrict.
A total of 205 pregnant women were assessed for their eligibility to participate in the study. Of these, 32 were excluded because they were <16 or >45 years old, had an infectious disease, were carrying two fetuses, or were unwilling to give blood samples. As shown in Figure 1, 173 pregnant women were eligible to participate.
Figure 1.
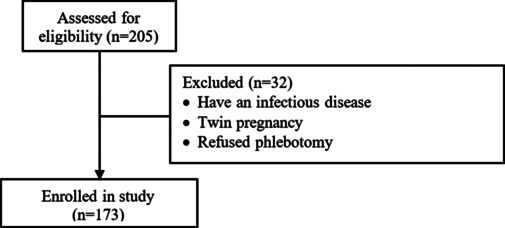
Flow diagram of participants
Data collection and tool
Interview procedures and blood sample collections were conducted during pregnancy care visits at the primary health center or the participant's residence during a home visit. The researchers took around 15–30 minutes to conduct the interviews and collect blood specimens for each participant. All interviews were recorded using the Android-based KoboToolbox platform.
Ethical consideration
This study was approved by the Hasanuddin University Health Research Ethics Committee, with ethical approval recommendation number 13974/UN4.14.1/TP.01.02/2022 before the commencement. Written informed consent was obtained from all the study participants, and confidentiality was maintained. Patient identifiers were removed, and privacy was ensured.
Variable measurements
Consumption of iron enhancers and inhibitors
Each question to measure pregnant women's awareness of iron deficiency originated from previous studies.[10,11,12,13] Ten items were used to measure the awareness of pregnant women about iron deficiency anemia. These were found valid and reliable, with a Cronbach's alpha value of >0.7. A score of 1 was given for each correct answer, and an incorrect answer was given a 0. The maximum score that could be obtained was 10. Participants who scored 0–4 were categorized as low awareness, and those scoring 5–10 were categorized as high awareness. This cutoff point was obtained from the mean value of the answers.
The variable of adherence to the consumption of iron tablets was categorized as adherent if pregnant women consumed ≥90 tablets during the pregnancy and as non-adherent if they consumed <90 tablets during the pregnancy, following Indonesian Ministry of Health recommendations.
The variables of the eating habits of pregnant women included consumption habits of iron enhancer and inhibitor food sources. Consumption habits were measured using a modified food frequency questionnaire with iron enhancer food ingredients and items, including oranges, tomatoes, mangoes, papayas, guavas, chilies, lemons and limes, and spinach. Food sources of iron inhibitors include tea, coffee, milk, cheese, yogurt, and ice cream. The frequency of consumption was given a score of 50 if consumed once a day, 25 if consumed 4–6 times a week, 15 if consumed three times a week, 10 if consumed 1–2 times a week, 1 if consumed less than once per week, and 0 if never consumed. Each participant's score was totaled and divided by the number of food ingredients. The average score obtained was then categorized as “frequent” if the average score was 15–50, “sometimes” if the average score was 10–14.9, and “never” if the average score was 0–9.9.
Laboratory assay
A trained phlebotomist carried out the blood specimen collection for iron status assays. Blood was collected using a 0.9-mm needle and a 3-cc vacutainer. Serum samples were obtained by centrifugation at 3,500 × g for 30 minutes at 4°C, then transferred to a polypropylene tube. Serial ferritin levels were examined at the Microbiology Laboratory unit at Hasanuddin University Hospital using the ELISA method (Ferritin ELISA Kit, DBC-Diagnostics Biochem Canada Inc). Compared with the RIA kit, the standard kit was used as a control, with an R2 value of 0.97. Pregnant women were classified as having adequate iron reserves in the body if the serum ferritin level was 25–283 ng/mL. They were classified as experiencing iron deficiency if the serum ferritin was <25 ng/mL, based on the ELISA kit procedure. The ELISA reader used a Thermo Scientific-Multiskan FC with a 96-well plate type. The examination results were read using a standard curve in SkanIt 3.1 software.
Statistical data analysis
Data were analyzed using Stata version 14 software. The relationships between all variables were analyzed using Chi-square test analysis. Univariate and multivariate analyses were performed using logistic regression analysis to determine the risk factors for maternal iron deficiency in pregnant women, tested with predictor variables with a confidence level of 95% (α =0.05).
Results
Of the participants, 131 (75.7%) were 20–35 years old, and 119 (68.8%) had completed secondary education. The majority (148; 85.6%) were housewives. At the beginning of the pregnancy, the participants were measured for mid-upper arm circumference (MUAC) and body mass index (BMI). As shown in Table 1, 133 (76.9%) had a MUAC of ≥23.5 cm, and 170 (98.3%) had a BMI of ≥18.5 kg/m2.
Table 1.
Descriptive characteristics of participants
| Characteristic | Mean±SD or n (%) | |
|---|---|---|
| Age, years | ||
| <20 | 23 | 13.3 |
| 20–35 | 131 | 75.7 |
| >35 | 19 | 11.0 |
| Education | ||
| Completed primary | 36 | 20.8 |
| Completed secondary | 119 | 68.8 |
| Completed tertiary | 18 | 10.4 |
| Occupation | ||
| Housewife | 148 | 85.6 |
| Employee | 5 | 2.9 |
| Business | 17 | 9.8 |
| Laborer | 3 | 1.7 |
| MUAC | ||
| <23.5 cm | 40 | 23.1 |
| ≥23.5 cm | 133 | 76.9 |
| BMI | ||
| <18.5 kg/m2 | 3 | 1.7 |
| ≥18.5 kg/m2 | 170 | 98.3 |
| Gestational age | ||
| Second trimester | 77 | 44.5 |
| Third trimester | 96 | 55.5 |
| Gravida | ||
| Primigravida | 48 | 27.7 |
| Multigravida | 125 | 72.3 |
| Parity | ||
| Nulliparous | 110 | 63.6 |
| Multiparous | 63 | 36.4 |
| Abortus | ||
| Yes | 31 | 17.9 |
| No | 142 | 82.1 |
| Pregnancy spacing, years | ||
| <2 | 91 | 52.6 |
| ≥2 | 82 | 47.4 |
| Age at first marriage | 20.4 | 0.3 |
Table 2 shows that 67.0% of participants had heard of anemia in pregnancy, and 56.6% could define anemia correctly. However, under half (49.1%) could identify the symptoms of anemia. Nearly half (42.2%) correctly identified the cause of anemia. Only a small proportion of participants believed that anemia in pregnancy was dangerous (41.0%) and agreed that anemia was a health problem (40.5%) and could cause serious problems for both mother and fetus (16.8%). More than half of the participants thought that they might have anemia (56.6%), knew how to prevent and treat anemia (55.5%), and were willing to take iron tablets if prescribed to prevent and treat anemia (59.1%).
Table 2.
Awareness of iron deficiency anemia in pregnancy
| Item | n | % |
|---|---|---|
| Ever heard about anemia in pregnancy | 116 | 67.0 |
| Know what anemia is | 98 | 56.6 |
| Know the signs/symptoms of anemia | 85 | 49.1 |
| Know the causes of anemia in pregnancy | 73 | 42.2 |
| Knowing whether anemia is dangerous | 71 | 41.0 |
| Believe that anemia is a health problem in pregnant women | 70 | 40.5 |
| Thinking that they could be anemic | 98 | 56.6 |
| Thinking that anemia can cause serious health problems for the mother and baby | 29 | 16.8 |
| Know the prevention and treatment of iron deficiency anemia | 96 | 55.5 |
| Willing to take iron tablets if prescribed to prevent and treat anemia | 101 | 59.1 |
Table 3 shows that more than half of the participants (57.2%) attended less than four antenatal care (ANC) visits; pregnant women are recommended to attend at least four during pregnancy. Most of the participants (74.4%) were not compliant with consuming iron tablets. Over half (55.5%) never took iron inhibitors. This figure contrasts with the number of participants who consumed iron enhancers (69.4%). For three of these four variables, the majority of participants reported no behavior to prevent iron deficiency in pregnancy.
Table 3.
Practices for preventing iron deficiency in pregnancy
| Variables | n | % |
|---|---|---|
| Antenatal care visits | ||
| <4 | 99 | 57.2 |
| ≥4 | 74 | 42.8 |
| Compliance with consumption of iron tablets | ||
| No | 128 | 74.4 |
| Yes | 44 | 25.6 |
| Taking iron enhancers | ||
| Never | 53 | 30.6 |
| Sometimes | 67 | 38.8 |
| Often | 53 | 30.6 |
| Taking iron inhibitors | ||
| Never | 96 | 55.5 |
| Sometimes | 61 | 35.3 |
| Often | 16 | 9.2 |
Table 4 shows the relationship between awareness and some variables that may be related to the incidence of iron deficiency in pregnancy. Most participants who did not experience iron deficiency had good awareness (78.9%, P = 0.017). Most participants who experienced iron deficiency were not compliant in consuming iron tablets (78.5%, P = 0.024). Most participants who did not experience iron deficiency regularly consumed food sources rich in ascorbic acid (vitamin C; 47.4%, P = 0.040). Among those who experienced iron deficiency, the interval between previous pregnancies was under two years (57.0%, P = 0.028).
Table 4.
Factors related to iron deficiency in pregnancy
| Variable | Iron deficiency n=135 (78%) | Normal n=38 (22%) | Total | Unadjusted OR (95% CI) | P a |
|---|---|---|---|---|---|
| Awareness | |||||
| Poor | 42.2 | 21.1 | 37.6 | 2.74 (1.16–6.42) | 0.017 |
| Good | 57.8 | 78.9 | 62.4 | 1 | |
| ANC visits | |||||
| <4 | 57.1 | 57.9 | 57.2 | 0.96 (0.46–2.00) | 0.925 |
| ≥4 | 42.9 | 42.1 | 42.8 | 1 | |
| Compliance with consumption of iron tablets | |||||
| No | 78.5 | 60.5 | 74.6 | 2.38 (1.10–5.14) | 0.024 |
| Yes | 21.5 | 39.5 | 25.4 | 1 | |
| Taking iron enhancers | |||||
| Never | 32.6 | 23.7 | 30.6 | 2.51 (1.00–6.27) | 0.040 |
| Sometimes | 41.5 | 28.9 | 38.8 | 2.61 (1.10–6.19) | |
| Often | 25.9 | 47.4 | 30.6 | 1 | |
| Taking iron inhibitors | |||||
| Never | 52.6 | 65.8 | 55.5 | 1 | 0.238 |
| Sometimes | 38.5 | 23.7 | 35.3 | 2.03 (0.87–4.72) | |
| Often | 8.9 | 10.5 | 9.2 | 1.05 (0.31–3.57) | |
| Age, years | |||||
| <20 | 14.8 | 7.9 | 13.3 | 1 | 0.058 |
| 20–35 | 77.0 | 71.1 | 75.7 | 0.57 (0.15–2.08) | |
| >35 | 8.2 | 21.0 | 11.0 | 0.20 (0.04–0.94) | |
| Education | |||||
| Completed primary | 20.0 | 23.7 | 20.8 | 0.37 (0.09–1.96) | 0.480 |
| Completed secondary | 68.1 | 71.0 | 68.8 | 0.42 (0.07–1.95) | |
| Completed tertiary | 11.9 | 5.3 | 10.4 | 1 | |
| Pregnancy spacing, years | |||||
| <2 | 57.0 | 36.8 | 52.6 | 2.27 (1.08–4.77) | 0.028 |
| ≥2 | 43.0 | 63.2 | 47.4 | 1 | |
| Parity | |||||
| Nulliparous | 65.2 | 57.9 | 63.6 | 1 | 0.409 |
| Multiparous | 34.8 | 42.1 | 36.4 | 0.73 (0.35–1.53) |
aP: the value of the difference between groups obtained from the Chi-square test
Table 5 shows the results of the univariate and multivariate logistic regression analysis. In the multivariate model, the significant relationship variable was that pregnant women with poor awareness were 3.03 times more at risk of experiencing iron deficiency than those with good awareness. Pregnant women who did not often consume iron enhancers were 2.8 times more at risk of iron deficiency than those who often consumed iron enhancers. These findings are associated with a significantly increased likelihood of depletion of iron stores in the body. Other factors analyzed but unrelated to iron deficiency in pregnancy include age, education, ANC visits, gestation interval, and parity.
Table 5.
Logistic regression analysis of factors associated with the incidence of iron deficiency in pregnancy
| Variable | Model 1 |
Model 2 |
||||
|---|---|---|---|---|---|---|
| Adjusted OR | 95% CI | P | Adjusted OR | 95% CI | P | |
| Awareness | ||||||
| Poor | 2.71 | 1.03–7.18 | 0.043* | 3.03 | 1.26–7.29 | 0.013** |
| Good | 1 | 1 | ||||
| ANC visits | ||||||
| <4 | 0.73 | 0.31–1.70 | 0.469 | |||
| ≥4 | 1 | |||||
| Compliance with iron supplementation | ||||||
| No | 2.76 | 1.10–6.86 | 0.029* | |||
| Yes | 1 | |||||
| Taking iron enhancers | ||||||
| Never | 4.31 | 1.48–12.56 | 0.005* | 2.83 | 1.10–7.26 | 0.030** |
| Sometimes | 4.41 | 1.57–12.39 | 0.007* | 2.85 | 1.18–6.92 | 0.020** |
| Often | 1 | 1 | ||||
| Taking iron inhibitors | ||||||
| Never | 1 | |||||
| Sometimes | 2.84 | 1.07–7.53 | 0.036* | |||
| Often | 1.21 | 0.30–4.84 | 0.780 | |||
| Age, years | ||||||
| <20 | 1 | |||||
| 20–35 | 0.99 | 0.22–4.50 | 0.998 | |||
| >35 | 0.29 | 0.04–2.15 | 0.230 | |||
| Education | ||||||
| Completed primary | 0.17 | 0.02–1.33 | 0.093 | |||
| Completed secondary | 0.27 | 0.04–1.57 | 0.147 | |||
| Completed tertiary | 1 | |||||
| Pregnancy spacing, years | ||||||
| <2 | 1.85 | 0.75–4.55 | 0.176 | |||
| ≥2 | 1 | |||||
| Parity | ||||||
| Nulliparous | 1 | |||||
| Multiparous | 1.78 | 0.64–4.99 | 0.268 | |||
Discussion
This study found that the prevalence of iron deficiency during pregnancy in the slums of Makassar City was 78.0%. This figure is large compared to a community-based study in East Ethiopia that found only around 52.9%.[14] Another study conducted in Austria reported that around 65% of pregnant women experienced iron deficiency.[15] This finding shows that the incidence of iron deficiency in slums in Makassar City is very high compared to other regions studied.
This study found a significant relationship between awareness and the incidence of iron deficiency in pregnant women. According to prior research, a correlation exists between awareness and the incidence of anemia in pregnant women.[16] Other studies have also reported a significant relationship between knowledge and the occurrence of anemia in pregnant women.[17,18] According to multiple studies, pregnant women's awareness influences their behavior during pregnancy. A lack of understanding among pregnant women has an adverse effect on their behavior to prevent anemia.[11,19] Pregnant women with good knowledge are more adherent to iron deficiency prevention practices than pregnant women with poor knowledge.[20] This association is an indication that the level of knowledge significantly contributed to the level of adherence. What it means is that non-adherence occurs as a result of ignorance and inadequate knowledge a pregnant woman has about anemia.[21] Poor awareness and knowledge have also been evident in Ethiopian pregnant women, resulting in improper food consumption behavior.[22] Pregnant women with a high level of knowledge and awareness can choose foods that will increase the quality of their pregnancy, specifically if they regularly adhere to consuming iron supplements.[23] However, unlike these results, a study conducted in India found no correlation between knowledge and the occurrence of anemia.[24]
Based on our survey, only a small proportion of participants believed that anemia during pregnancy was a harmful health problem that might result in severe complications for the mother and fetus. This certainly has an impact on the actions of the mother during her pregnancy. Awareness is strongly related to health behavior in preventing and maintaining oneself to avoid disease.[17] Also, pregnant women with good awareness are more attentive to the symptoms they experience and can act to reduce the severity of iron deficiency anemia.[25] An understanding and awareness of anemia during pregnancy contribute to the practice of iron consumption during this time.[26]
In general, pregnant women in slums are less concerned with education. They are typically more attentive to dietary needs. Their lack of interest in education leads to low health status awareness. Formal education also affects health knowledge and awareness.[27] Several studies have stated that when a woman's education level increases, awareness of anemia also increases.[28]
This study also found a significant relationship between the preventive measure of consuming iron enhancers and the incidence of iron deficiency in pregnant women. Behavior in consuming daily food is an external factor related to the ongoing absorption of iron in the body. This study is in line with others finding a relationship between vitamin C intake and the incidence of anemia.[29] In contrast, another study found no correlation between the use of iron enhancers and the incidence of anemia in the third trimester of pregnancy, thus contradicting our study's findings.[30]
Several interaction factors between the foods consumed influence iron absorption in the body. The increase in iron absorption is dominated by the effect of ascorbic acid (vitamin C) and has an impact on preventing iron deficiency.[31] Ascorbic acid performs as a good regulator of iron absorption from food and can contribute to the defense against phytic acid and tannins, which interrupt iron absorption.[32] Ascorbic acid is required for iron absorption since iron is more effectively and efficiently absorbed in an acidic environment.[33]
These study findings suggest focused awareness and education strategies designed to improve nutritional habits by encouraging the consumption of iron enhancers and rich sources of iron to make positive health contributions to avert iron deficiency.
Financial support and sponsorship
This sub-study was supported by the Center for Epidemiology and Population Health Studies (CEPHS) at the Faculty of Public Health, Hasanuddin University.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the contribution of the phlebotomist who collected blood samples, all participants in this study, and their families. The biological samples analyzed in the study are the same samples that were collected with the support of the PMDSU program.
References
- 1.Ekwere TA, Ekanem AM. Maternal knowledge, food restriction and prevention strategies related to anaemia in pregnancy: A cross-sectional study. Int J Community Med Public Health. 2015;2:331–8. [Google Scholar]
- 2.WHO Prevalence of anaemia in pregnant women (aged 15-49) (%) 2021 [Google Scholar]
- 3.The World Bank Prevalence of anemia among pregnant women (%)-Least developed countries: UN classification | Data. 2019 [Google Scholar]
- 4.Shah T, Khaskheli MS, Ansari S, Lakhan H, Shaikh F, Zardari AA, et al. Gestational Anemia and its effects on neonatal outcome, in the population of Hyderabad, Sindh, Pakistan. Saudi J Biol Sci. 2022;29:83–7. doi: 10.1016/j.sjbs.2021.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sari YAP, Wahiduddin W, Ansariadi A, Bustan N, Russeng SS, Sirajuddin S, et al. Determinants of low birth weight occurrence in Bahteramas regional general hospital, Southeast Sulawesi Province, Indonesia. Open Access Maced J Med Sci. 2022;10:1107–13. [Google Scholar]
- 6.Hermayanti D, Setiawan M, Nurdiana H. Improvement of knowledge on iron deficiency anemia and its prevention among Bustanul Athfal teachers in Malang. Health Sci Int Conf. 2019 [Google Scholar]
- 7.Al Shammari E, Ashraf SA, Al Shammari R, Al Rashidi A, Awadelkareem AM, Elkhalifa AEO. Nutritional knowledge and awareness of primary health care physicians working in hail region, Saudi Arabia: A cross-sectional study. Curr Res Nutr Food Sci. 2021;9:402–8. [Google Scholar]
- 8.Shahzad S, Islam K, Azhar S, Fiza S, Ahmed W, Murtaza Z. Impact of knowledge, attitude and practice on iron deficiency anaemia status among females of reproductive age group (20- 21-year-old) studying in government home economics college Lahore, Pakistan. Int Arch Biomed Clin Res. 2017;3:31–6. [Google Scholar]
- 9.Bansal R, Bedi M, Kaur J, Kaur K, Shergill HK, Khaira HK, et al. Prevalence and factors associated with anemia among pregnant women attending antenatal clinic. Adesh Univ J Med Sci Res. 2020;2:42–8. [Google Scholar]
- 10.Ademuyiwa IY, Ayamolowo SJ, Oginni MO, Akinbode MO. Awareness and prevention of anemia among pregnant women attending antenatal clinic at a university teaching hospital in Nigeria. Calabar J Health Sci. 2020;4:20–6. [Google Scholar]
- 11.Duko B, Tadesse B, Gebre M, Teshome T. Awareness of anemia and associated factors among pregnant women attending antenatal care, South Ethiopia. J Womens Health Care. 2017;6:1–5. [Google Scholar]
- 12.George M, George N, Ramesh N. Awareness regarding anemia, gestational diabetes and pregnancy induced hypertension among antenatal women attending outpatient department in a rural hospital. Natl J Community Med. 2016;7:362–7. [Google Scholar]
- 13.Vibhute NA, Shah U, Belgaumi U, Kadashetti V, Bommanavar S, Kamate W. Prevalence and awareness of nutritional anemia among female medical students in Karad, Maharashtra, India: A cross-sectional study. J Family Med Prim Care. 2019;8:2369–72. doi: 10.4103/jfmpc.jfmpc_353_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fite MB, Bikila D, Habtu W, Tura AK, Yadeta TA, Oljira L, et al. Beyond hemoglobin: Uncovering iron deficiency and iron deficiency anemia using serum ferritin concentration among pregnant women in eastern Ethiopia: A community-based study. BMC Nutr. 2022;8:82.. doi: 10.1186/s40795-022-00579-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeisler H, Dietrich W, Heinzl F, Klaritsch P, Humpel V, Moertl M, et al. Prevalence of iron deficiency in pregnant women: A prospective cross-sectional Austrian study. Food Sci Nutr. 2021;9:6559–65. doi: 10.1002/fsn3.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeyaprabha K. Awareness of anemia and its association with the severity of the disease in pregnant women. Int J Sci Study. 2021;8:157–60. [Google Scholar]
- 17.Ekasari T, Natalia MS, Zakiyyah M. Knowledge and parity prevention of anemia in pregnancy. Bali Med J. 2022;11:1095–8. [Google Scholar]
- 18.Asghari S, Mohammadzadegan-Tabrizi R, Rafraf M, Sarbakhsh P, Babaie J. Prevalence and predictors of iron-deficiency anemia: Women's health perspective at reproductive age in the suburb of dried Urmia Lake, Northwest of Iran. J Educ Health Promot. 2020;9:332.. doi: 10.4103/jehp.jehp_166_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Animut K, Berhanu G. Determinants of anemia status among pregnant women in Ethiopia: Using 2016 Ethiopian demographic and health survey data; application of ordinal logistic regression models. BMC Pregnancy Childbirth. 2022;22:663.. doi: 10.1186/s12884-022-04990-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Appiah PK, Nkuah D, Bonchel DA. Knowledge of and adherence to anaemia prevention strategies among pregnant women attending antenatal care facilities in Juaboso district in Western-North Region, Ghana. J Pregnancy. 2020;2020:2139892.. doi: 10.1155/2020/2139892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shehata SF, Alahmari FS, Alahmari SA, Aljamaan AM, Alamrah HM, Alsharif NM, et al. General population awareness regarding iron deficiency anaemia and its relation with nutrition and dietary habits. Int J Community Med Public Health. 2020;7:3803–9. [Google Scholar]
- 22.Mohammed SH, Taye H, Larijani B, Esmaillzadeh A. Food taboo among pregnant Ethiopian women: Magnitude, drivers, and association with anemia. Nutr J. 2019;18:19.. doi: 10.1186/s12937-019-0444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muthuraj LP, Kandasamy S, Subbiah P, Sibqathulla MJ, Velappan LK, Gopal M, et al. Sociocultural and drug-related factors associated with adherence to iron–folic acid supplementation among pregnant women-A mixed-methods study. J Educ Health Promot. 2023;12:121.. doi: 10.4103/jehp.jehp_1008_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nivedita K, Shanthini FN. Knowledge, attitude and practices of pregnant women regarding anemia, iron rich diet and iron supplement. Int J Reprod Contracept Obstet Gynecol. 2016;5:425–31. [Google Scholar]
- 25.Aboud SAE, El Sayed HAE, Ibrahim HAF. Knowledge, attitude and practice regarding prevention of iron deficiency anemia among pregnant women in Tabuk region. Available online www.ijpras. com Int J Pharm Res Allied Sci. 2019;8:87–97. [Google Scholar]
- 26.Nasir BB, Fentie AM, Adisu MK. Adherence to iron and folic acid supplementation and prevalence of anemia among pregnant women attending antenatal care clinic at Tikur Anbessa Specialized Hospital, Ethiopia. PLoS One. 2020;15:e0232625.. doi: 10.1371/journal.pone.0232625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raghupathi V, Raghupathi W. The influence of education on health: An empirical assessment of OECD countries for the period 1995-2015. Arch Public Health. 2020;78:20.. doi: 10.1186/s13690-020-00402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Sattam Z, Hassan S, Majeed B, Al-Attar Z. Knowledge about anemia in pregnancy among females attending primary health care centers in Baghdad. Open Access Maced J Med Sci. 2022;10:785–92. [Google Scholar]
- 29.Kusudaryati DP, Prananingrum R. Hubungan usia, asupan vitamin C dan besi dengan kadar hemoglobin pada remaja putri anemia. Pros Univ Res Colloq. 2019:250–5. [Google Scholar]
- 30.Pratiwi R, Widari D. Hubungan konsumsi sumber pangan enhancer dan inhibitor zat besi dengan kejadian anemia pada ibu hamil. Relation of iron enhancer and inhibitor food consumption with anemia in pregnant women. Amerta Nutr. 2018;2:283–91. [Google Scholar]
- 31.He H, Qiao Y, Zhang Z, Wu Z, Liu D, Liao Z, et al. Dual action of vitamin C in iron supplement therapeutics for iron deficiency anemia: Prevention of liver damage induced by iron overload. Food Funct. 2018;9:5390–401. doi: 10.1039/c7fo02057k. [DOI] [PubMed] [Google Scholar]
- 32.Krisnanda R. Vitamin C helps in the absorption of iron in iron deficiency anemia. J Penelit Perawat Prof. 2020;2:279–86. [Google Scholar]
- 33.Piskin E, Cianciosi D, Gulec S, Tomas M, Capanoglu E. Iron absorption: Factors, limitations, and improvement methods. ACS Omega. 2022;7:20441–56. doi: 10.1021/acsomega.2c01833. [DOI] [PMC free article] [PubMed] [Google Scholar]


