Abstract
Accurately defining gross tumour volume (GTV) and organs at risk (OAR) is key to successful radiation therapy (RT) treatment outcomes for patients with gynaecological cancers. With improved access to magnetic resonance imaging (MRI) for RT simulation and planning, the optimisation and tailoring of proven diagnostic MRI techniques towards RT specific planning goals is fast evolving. Modifying MRI techniques for radiation oncology (RO) with the priority of anatomy visualisation and spatial location over diagnosis and disease characterisation relies heavily on successful collaboration between radiology and radiation oncology staff. This ‘How I Do It’ paper describes a qualitative analysis of the adaptation of a diagnostic MRI vaginal opacification technique into an RT specific MRI simulation procedure using aqueous ultrasound gel for improving natural anatomical visualisation of the vaginal canal. This technique is explained and could be introduced in other RO departments for dedicated RT planning scans in MR‐Sim sessions with minimal difficulty. We found 10‐15 cc of aqueous gel delivered vaginally produced optimal MRI planning images for most patients. With this small amount of gel and careful application technique, the full extent of the vaginal vault and cervix can be well visualised on T2 Weighted (T2W) imaging, while tending not to unfold the natural fornices of the collapsed vagina, representing a significant improvement in image quality from the outdated tampon procedure.
Keywords: Gynaecological, MRI, radiation therapy, simulation, vagina
This ‘How I Do It’ paper describes the adaptation of a proven diagnostic magnetic resonance imaging (MRI) technique into a radiation therapy (RT) specific MRI simulation procedure. This well‐tolerated technique could be easily introduced in other radiation oncology departments for dedicated RT planning scans with minimal difficulty and is an example of the successful collaborations between radiographers and radiation therapists showcasing effective knowledge sharing and skill pooling.
Introduction
Accurate anatomical identification is crucial for achieving positive treatment outcomes in gynaecological radiation therapy; however, many challenges exist in terms of accurate anatomical delineation and reducing inter‐observer contouring variability. 1 , 2 , 3
In the radiation oncology (RO) setting, tampons have historically been used at simulation appointments to assist with vaginal wall delineation for patients with gynaecological cancers. Early studies showed that sufficient gas remained trapped in the tampon fibres after insertion to distend the anatomy and provide good negative contrast on computed tomography (CT) imaging. 4 This decades old method is still widely used in RO departments for CT simulation scanning; however, a tampon often does not reveal the true shape and extent of the natural vaginal anatomy. 5
Our current departmental procedure for gynaecological planning involves two CT scans: One CT scan acquired with a full bladder, followed by an empty bladder CT scan with tampon in‐situ. Both of these CT scans are used in the radiation therapy (RT) planning process to aid target volume delineation. The full and empty bladder scans allow the RO to assess the impact of varying bladder size on the patient's target volume.
Magnetic resonance imaging (MRI) has been identified as playing an increasing role in the diagnosis, staging and planning of RT treatment for gynaecological malignancies. MRI‐only planning for pelvic tumour sites has been shown to be technically feasible and a likely future radiotherapy pathway. 6 For the female pelvis, the vagina and gross tumour volume (GTV) have been identified as key areas of inter‐observer variability, with enhanced soft tissue contrast from a planning MRI a potential solution. 1 , 2 , 3 , 7 , 8 Studies have also suggested that MRI of gynaecological cancers can be complicated by the natural collapse of the vagina – making it difficult to visualise the walls and fornices. It has been also reported that the presence of a vaginal tampon in MRI examinations may artificially deform the adjacent anatomical structures, and not define the natural recesses of the vagina. 2 , 5
Diagnostic MRI examinations have historically deployed vaginal opacification methods using bacteriostatic ultrasound gel due to its viscosity and yielding high signal intensity on T2 weighted imaging. The aim of the procedure being to achieve vaginal distention using a significant volume of aqueous gel. This has been shown to improve the diagnostic usefulness of gynaecological MRI, as the gel unfolds the vaginal fornices and can reveal signs of tumour invasion and/or exophytic growth. Studies report a volume of 50–100 cc of aqueous gel provides adequate distention to improve the diagnostic usefulness of the scans. The opacification facilitates more accurate evaluation of tumour size and staging, particularly when vaginal wall involvement is present. 9 , 10 , 11 , 12
This diagnostic procedure has proven to be safe, cost effective, well‐tolerated and an effective method of delineating vaginal anatomy on MRI, with very low risk of complications. 5 , 11 , 13 However, the gross distension introduced by the diagnostic vaginal opacification method is not recommended for gynaecological RT planning scans as the overall irradiated volume would be increased by the distention process. Furthermore, this gross distension is neither reproducible nor practical in a daily treatment setting.
Given these points, along with the commissioning of a dedicated MRI simulator (MR‐Sim), our RO department has adapted the proven diagnostic opacification method in a novel way; by using a significantly reduced volume of gel to delineate, but not distend, the vaginal anatomy for RT simulation scanning. Coined ‘Viscous Aqueous Gel Illustrating Natural Anatomy’ (VAGINA), the objectives of introducing this method were to assess if vaginal anatomy can be accurately delineated without distension, using aqueous gel, and if it is feasible to replace the empty bladder + tampon CT scan with an empty bladder + VAGINA MRI scan. This methods paper details the protocol we have implemented, as well as providing qualitative examples of examination results.
Materials and Methods
In order to qualitatively assess the usefulness of this technique for RT planning, 10 gynaecological patients who attended the department for radiotherapy planning were identified. All images were acquired in accordance with existing departmental ethics approval via the Hunter New England Human Research Ethics Committee for low‐risk MRI research (2020/ETH02542: Radiation Oncology Imaging Metaproject). The diagnostic method for vaginal opacification was modified for MR‐Sim with the goal of delineating and visualising the vaginal vault, without distension. The 60 cc of gel used in the diagnostic setting 11 was incrementally reduced across all 10 patients.
For the 10 patients, two 120 kV 2 mm axial CT scans (SOMATOM CONFIDENCE, Siemens Healthcare, Erlangen, Germany) were acquired for treatment planning in accordance with current departmental procedure. Following the CT session, the patient was escorted directly to the MR‐Sim (MAGNETOM, Skyra 3 T, Siemens Healthcare, Erlangen, Germany). Using a sterile 50 mL catheter tip syringe, Aquasonic 100® ultrasound transmission gel was drawn and warmed to 36°C (Fig. 1). The syringe is then inserted into the vagina by the radiation oncologist until the tip reaches the cervix, where they will gently withdraw the syringe while administering the gel evenly. This is performed all while the patient is on the MR‐Sim couch, lying flat so as to not expel the gel through moving prior to the scan.
Figure 1.

Aquasonic 100® ultrasound transmission gel drawing into 50 mL catheter tip syringe.
Patients were then positioned and aligned to their treatment tattoos using a DORADOnova MR 3 T external laser bridge (LAP; Luneburg, Germany), on a QFix Insight™ flat couch overlay with a Siemens 18ch Body flex coil placed over the pelvis. Both sagittal and axial T2W scans were acquired (Table 1). The images were then imported into an Eclipse™ treatment planning system (Varian Medical Systems, Palo Alto, CA, USA), and fused to the empty bladder + tampon CT scan using a rigid registration method.
Table 1.
MRI acquisition parameters.
| Axial T2 | Sagittal T2 | |
|---|---|---|
| Pulse sequence | TSE | TSE |
| TE (ms) | 91 | 79 |
| TR (ms) | 5710 | 6650 |
| FOV (mm) | 240 | 210 |
| Bandwidth (Hz/Px) | 399 | 399 |
| Slice thickness (mm) | 2.5 | 2 |
| 3D distortion correction | Yes | Yes |
| No. of slices | 45 | 90 |
FOV, field of view; TE, echo time; TR, repetition time; TSE, turbo spin echo.
As one of the objectives of the study was to assess the feasibility of replacing the empty bladder CT + tampon scan with an empty bladder + VAGINA MRI scan, the data sets were then used for contouring and qualitative image comparisons performed to assess the delineation of the vaginal anatomy.
Results
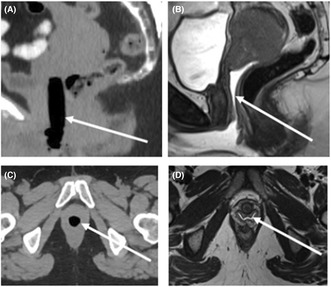
Over the course of the 10 patients, the volume of aqueous gel delivered was reduced incrementally from 30 mL (Fig. 2A). The 30 mL was qualitatively assessed as distending the vault beyond its natural form. Ultimately 10‐15 cc was found to be an optimal volume for most patients (Fig. 2B).
Figure 2.
Sagittal T2‐weighted MRI comparing different individuals with various gel volumes. (A) Shows 30 cc of gel, note vaginal distension, and (B) shows 10 cc of gel delineating vaginal vault without distension.
With the smaller volume of gel, the full extent of the vaginal vault and cervix can be well visualised on T2W imaging, while tending not to unfold the natural fornices of the collapsed vagina (Figs. 3 and 4).
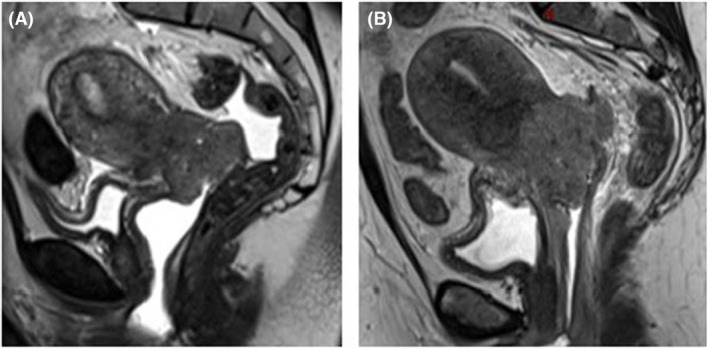
Figure 3.
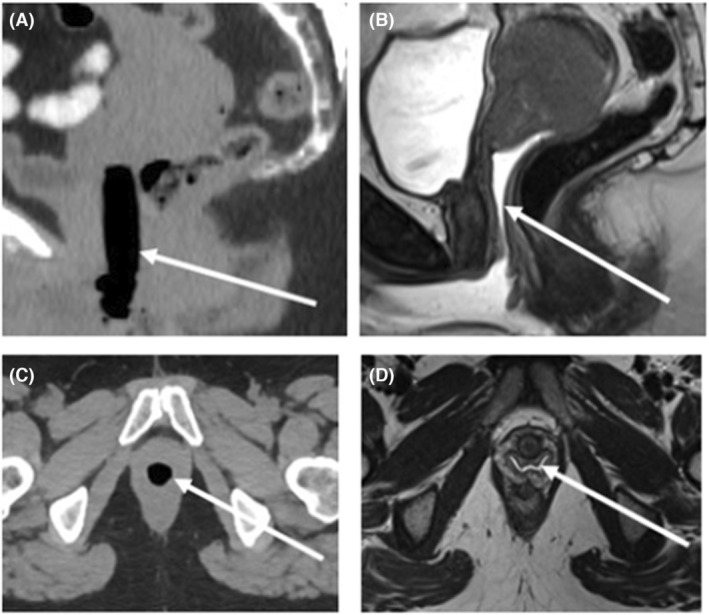
A 38‐year‐old female with cervical squamous cell carcinoma. (A) Sagittal CT reconstruction with tampon in‐situ. (B) Sagittal T2‐weighted image with vaginal gel in‐situ. (C) Axial CT with tampon in‐situ. (D) Axial T2‐weighted image with vaginal gel in‐situ.
Figure 4.

Blended sagittal CT/MR from Figure 3 highlighting the differences between tampon position and true extent of vaginal vault and cervix position.
Furthermore, we found that along with visualising the natural vaginal anatomy, the aqueous gel revealed a great deal of disease detail that would not have been visible on the planning CT (Figs. 5 and 6).
Figure 5.
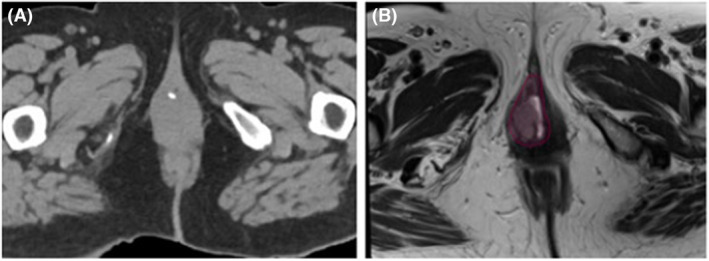
74‐year‐old female with recurrent endometrial carcinoma with vaginal metastases. GTV shown around the vaginal nodule on MRI (B), otherwise not seen on CT (A).
Figure 6.
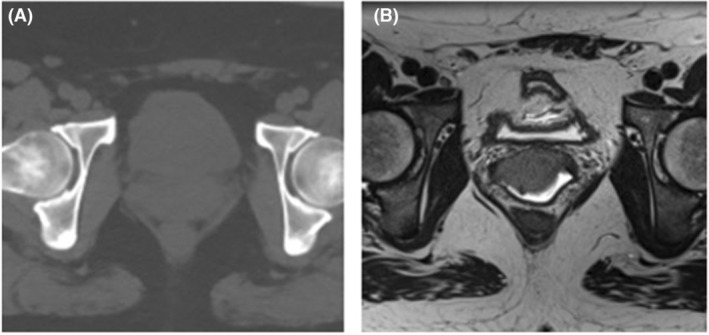
33‐year‐old female with squamous cell carcinoma of cervix, stage 2B. The full extent of this disease extension into the lower third of the vagina would not have been fully appreciated in CT (A) without T2W MRI + gel (B).
As a result of our qualitative image analysis, the second ionising CT scan (empty bladder + tampon in‐situ) has now been removed from our departmental clinical protocol, and replaced with a T2W sagittal and axial VAGINA MR‐Sim scan.
Discussion
The adaptation of this diagnostic technique has facilitated more accurate delineation of natural vaginal anatomy for gynaecological RT planning. The VAGINA MRI technique is useful for visualising disease extension into the vaginal canal, which may have otherwise been obscured by the tampon. We believe this is a reasonable step to help improve contouring accuracy, and represents a significant improvement in image quality from the outdated tampon procedure. It is important to note that the volume of aqueous gel delivered is not a one‐size‐fits‐all approach. In an ideal setting, a series of scans with varying amounts of gel would have been acquired on one patient to compare the effect on the anatomy. However beneficial it would be to have multiple scans on one patient, this was not proposed given the delicate clinical setting. It is therefore advised when trying to reproduce these results, centres may need to find their individually optimal volume considering several individual anatomical factors. These may include but not be limited to vaginal vault length, number of vaginal births, vaginal stenosis; this could be advised by the RO through internal examinations previously performed on the patient. We do, nonetheless, recommend aiming to deploy the smallest amount of gel possible to achieve visualisation without distension. There was a learning curve associated with optimal gel deployment technique, with the superior vaginal vault often the most difficult area to accurately define. Visual qualitative assessment is performed by the MRI radiographer/MRI RT at the time of image acquisition. Recommendations for tailoring MRI techniques with radiotherapy priorities in mind is becoming more prominent in literature across multiple anatomical sites. 14 , 15 This technique is an example of the direct clinical benefits of increased integration of MR‐Sim into routine RT clinical practice. Simple adaptations such as this procedure are an important part of addressing the clinical practicalities of implementing future MRI‐only planning workflows. This technique could be introduced in other RO departments for dedicated RT planning scans in MR‐Sim sessions with minimal difficulty. The development of this technique is reflective of successful collaborations between the radiology and radiation oncology professions. 16 For the continued development of MRI in RT practice, the close inter‐disciplinary relationships, effective knowledge sharing and skill pooling is key. This will improve the use of resources, minimising the duplication of effort and can lead to more efficient pathways and improved outcomes for patients. 17
Funding information
The authors do not have any financial grants, industrial links or affiliations to declare.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
All images used in the study were acquired in accordance with existing departmental ethics approval via the Hunter New England Human Research Ethics Committee for low‐risk MRI research (2020/ETH02542: Radiation Oncology Imaging Metaproject).
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. Eminowicz G, McCormack M. Variability of clinical target volume delineation for definitive radiotherapy in cervix cancer. Radiother Oncol 2015; 117: 542–547. [DOI] [PubMed] [Google Scholar]
- 2. Wu DH, Mayr NA, Karatas Y, et al. Interobserver variation in cervical cancer tumor delineation for image‐based radiotherapy planning among and within different specialties. J Appl Clin Med Phys 2005; 6: 106–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lim K, Small W Jr, Portelance L, et al. Consensus guidelines for delineation of clinical target volume for intensity‐modulated pelvic radiotherapy for the definitive treatment of cervix cancer. Int J Radiat Oncol Biol Phys 2011; 79: 348–355. [DOI] [PubMed] [Google Scholar]
- 4. Cohen WN, Seidelmann FE, Bryan PJ. Use of a tampon to enhance vaginal localization in computed tomography. Am J Roentgenol 1977; 128: 1064–1065. [DOI] [PubMed] [Google Scholar]
- 5. Young P, Daniel B, Sommer G, Kim B, Herfkens R. Intravaginal gel for staging of female pelvic cancers—preliminary report of safety, distention, and gel‐mucosal contrast during magnetic resonance examination. J Comput Assist Tomogr 2012; 36: 253–256. [DOI] [PubMed] [Google Scholar]
- 6. O'Connor LM, Skehan K, Choi JH, et al. Optimisation and validation of an integrated magnetic resonance imaging‐only radiotherapy planning solution. Phys Imaging Radiat Oncol 2021; 20: 34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gardner CS, Sunil J, Klopp AH, et al. Primary vaginal cancer: role of MRI in diagnosis, staging and treatment. Br J Radiol 2015; 88: 20150033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eminowicz G, Hall‐Craggs M, Diez P, McCormack M. Improving target volume delineation in intact cervical carcinoma: literature review and step‐by‐step pictorial atlas to aid contouring. Pract Radiat Oncol 2016; 6: e203–e213. [DOI] [PubMed] [Google Scholar]
- 9. Dimopoulos JCA, Schard G, Berger D, et al. Systematic evaluation of MRI findings in different stages of treatment of cervical cancer: potential of MRI on delineation of target, pathoanatomic structures, and organs at risk. Int J Radiat Oncol Biol Phys 2006; 64: 1380–1388. [DOI] [PubMed] [Google Scholar]
- 10. Engelaere C, Poncelet E, Durot C, Dohan A, Rousset P, Hoeffel C. Pelvic MRI: is endovaginal or rectal filling needed? Korean J Radiol 2018; 19: 397–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brown MA, Mattrey RF, Stamato S, Sirlin CB. MRI of the female pelvis using vaginal gel. Am J Roentgenol 2005; 185: 1221–1227. [DOI] [PubMed] [Google Scholar]
- 12. Balleyguier C, Sala E, da Cunha T, et al. Staging of uterine cervical cancer with MRI: guidelines of the European Society of Urogenital Radiology. Eur Radiol 2011; 21: 1102–1110. [DOI] [PubMed] [Google Scholar]
- 13. Atcı N, Özgür T, Öztürk F, Dolapçıoğlu KS. Utility of intravaginal ultrasound gel for local staging of cervical carcinoma on MRI. Clin Imaging 2016; 40: 1104–1107. [DOI] [PubMed] [Google Scholar]
- 14. Richardson M, Skehan K, Wilton L, et al. Visualising the urethra for prostate radiotherapy planning. J Med Radiat Sci 2021; 68: 282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Speight R, Schmidt MA, Liney GP, et al. IPEM topical report: A 2018 IPEM survey of MRI use for external beam radiotherapy treatment planning in the UK. Phys Med Biol 2019; 64: 175021. [DOI] [PubMed] [Google Scholar]
- 16. Rai R, Kumar S, Batumalai V, et al. The integration of MRI in radiation therapy: collaboration of radiographers and radiation therapists. J Med Radiat Sci 2017; 64: 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McGee KP, Hu Y, Tryggestad E, et al. MRI in radiation oncology: Underserved needs. Magn Reson Med 2016; 75: 11–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


