Abstract
Introduction
Research indicates that the immobilisation mask required for radiation therapy (RT) for head and neck cancers can provoke intense anxiety. However, little is known about the rates of this anxiety, whether it changes over a course of treatment and how it is managed in clinical practice. This study aimed to describe the rates and patterns of situational anxiety in patients undergoing RT for head and neck cancer and the use of anxiety management interventions in current clinical practice in a major regional cancer setting in New South Wales, Australia.
Methods
Situational anxiety rates and patterns were assessed at five time points using the State‐Trait Anxiety Inventory prior to treatment planning (SIM), the first three treatment sessions (Tx 1, Tx 2 and Tx 3) and treatment 20 (Tx 20). Sessions were observed to record the use of general supportive interventions (music and support person) and anxiety‐specific interventions (break from the mask, relaxation techniques and anxiolytic medication). Sociodemographic and clinical information was extracted from the medical record.
Results
One hundred and one patients were recruited. One‐third had clinically significant anxiety at any of the first three time points (33.3–40%), and a quarter at Tx 3 (26.4%) and Tx 20 (23.4%). Of the sample, 55.4% had available data for categorisation into one of four pattern groups: ‘No Anxiety’ (46.4%); ‘Decreasing Anxiety’ (35.7%); ‘Increasing Anxiety’ (7.1%); and ‘Stable High Anxiety’ (10.7%). Most participants had social support present at SIM (53.5%) and listened to music during treatment (86.7–92.9%). Few participants received relaxation techniques alone (1.2–2.3%). Anxiolytic medication was provided for 10% of patients at some stage during the treatment journey and 5% required a break from the mask at SIM, with frequency decreasing throughout the treatment course.
Conclusions
In this regional cancer setting, situational anxiety was common, but generally decreased throughout treatment. Some patients experience persistent or increasing anxiety, with up to 10% of patients receiving specific anxiety management interventions.
Keywords: Claustrophobia, head and neck, psychology
Patients wearing an immobilisation mask during RT for head and neck cancer often experience situational anxiety. This anxiety generally decreases throughout treatment. However, some patients experience persistent or increasing anxiety, with up to 10% of patients receiving anxiety management interventions.
Introduction
Over 5000 people in Australia were diagnosed with head and neck cancer (HNC) in 2022. 1 Many people with HNC receive radiation therapy (RT), either as a primary treatment, or combined with chemotherapy and/or surgery. 2 Patients undergoing RT for cancer may experience significant symptoms of depression and anxiety, 3 and those with HNC are at particular risk of mental health difficulties, due to the intensive nature of treatment (and side effects) and the overlap of risk factors (smoking and alcohol use) for some forms of HNC. 4 , 5
Additionally, a unique aspect of RT for HNC is the use of a tight‐fitting immobilisation mask. While mask‐making procedures can vary worldwide, commonly the mask is moulded over the patient's head (sometimes encompassing the neck and shoulders) and secured to the treatment couch. By limiting patient movement, the mask ensures the safe and accurate delivery of radiation. 6 Qualitative research has demonstrated that the procedure can provoke significant distress. 7 , 8 , 9 , 10 This has been variously labelled ‘mask anxiety’ 7 , 8 , 9 , 10 , 11 and ‘situational anxiety’. 12
There is limited research into the rates of situational anxiety. The largest study (n = 100), 7 used a modified version of the one‐item Distress Thermometer (DT) at one (variable) time point between treatment planning (SIM) and completion of RT and found 20% reported moderate distress (DT score = 4–7) and 6% reported severe distress (DT score = 8–10) about the mask.
Situational anxiety has been thought to be most acute at the commencement of RT and to naturally decline thereafter. 7 However, emerging literature suggests that a subset of patients experience different patterns of anxiety. 11 , 12 A recent small (n = 57), longitudinal study 12 examined patterns of situational anxiety. Using the six‐item short form of the State‐Trait Anxiety Inventory (STAI‐6) 13 to measure state anxiety (baseline, weekly from Weeks 1–5 and the end of treatment), they found that while situational anxiety generally peaked at the beginning of treatment and decreased over time, there was a subset of patients that remained highly anxious throughout treatment and another that became increasingly anxious. 12 The authors categorised participants into five different patterns of anxiety, namely ‘No Anxiety’ (19%), ‘Decreasing Anxiety’ (27%), ‘Fluctuating Anxiety’ (19%), ‘Increasing Anxiety’ (19%) and ‘Stable High Anxiety’ (16%). These results echoed a previous, smaller (n = 35) longitudinal study involving patients who reported situational anxiety. They used a modified DT at baseline (SIM or week 1 of treatment), mid‐treatment (2 or 4 weeks into treatment, depending on the length of prescribed treatment) and the end of treatment (Week 4 or Weeks 6–7). 14 The study found that 22% of participants reported sustained anxiety, and 6% reported increasing anxiety over the course of treatment. However, these existing studies have been conducted exclusively in cancer centres in major cities. There are a number of important health disparities that exist between those who reside in major cities and those who live in regional or rural towns (e.g., smoking rates, alcohol use and prevalence of chronic health conditions). Factors such as these may affect a person's ability to cope with the treatment journey, including the experience of procedural anxiety. 15 Despite this, there is little to no research on the rates and patterns of situational anxiety in regional settings.
The significant impact of situational anxiety on some patients' experience of RT warrants effective interventions. Additionally, if situational anxiety does not naturally decrease over the course of treatment, but persists or increases, it becomes increasingly important to provide management interventions. One recommendation for managing severe procedural anxiety in medical settings is to administer anxiolytic medication, often benzodiazepines. 16 , 17 However, these pose a host of risks for certain patients, including confusion, ataxia and increased falls risk. 18 Although effective, many patients report a strong preference to avoid medication where possible. 7 Additionally, benzodiazepine dependence can occur within a month of use. 18 Given the frequency (5 days per week 19 ) and the length of most courses of RT (up to 7 weeks 19 ), this approach to the management of (sustained) anxiety in RT is problematic. Non‐pharmacological anxiety management interventions previously mentioned in the literature and suggested by informal online sources, include playing music in the treatment room, allowing patients to take a break from the mask and modifying the mask to reduce the sense of confinement (including removing the mouth and eyepieces of the mask). 10 , 20 , 21
While there is some discussion of anxiety management interventions, there is very limited published literature on current clinical practice in terms of the types or rates of anxiety management interventions. A recent small‐scale (n = 35) study found many participants perceived benefit from discussion with staff (72–86%), self‐taught strategies such as breath regulation and meditation (94%), and music (72%) during treatment. 11 Of those prescribed medication, 60% perceived benefit although 40% chose to discontinue because the risks outweighed the benefit.
It appears that situational anxiety is a significant problem for a subset of patients and there is emerging evidence that this anxiety may persist or increase over the course of RT for a subset of patients. These findings warrant replication. If confirmed, there is a need to provide clinical interventions to manage situational anxiety. However, in order to suggest additional, innovative interventions it is important to establish how anxiety is currently being managed in clinical practice.
This study aimed to describe the rates and patterns of situational anxiety in patients undergoing RT for HNC in a major regional cancer setting in NSW, Australia. We also aimed to document the use of anxiety management interventions in current clinical practice in the same major regional cancer RT department.
Methods
The study protocol was approved by the Hunter New England Health Human Research Ethics Committee (16/02/17/4.07).
Design
Prospective, observational study.
Setting
A Department of Radiation Oncology, at a public cancer centre in regional New South Wales (NSW), Australia.
Eligibility criteria
New patients with HNC who required a mask for RT were eligible. Patients were excluded from participating if they were: unable to comprehend written or spoken English; aged less than 18 years; receiving fewer than 20 fractions; or too ill/impaired to undertake the study, in the opinion of the treating radiation oncologist (RO).
Procedure
Recruitment
All eligible patients were flagged by clinical trial coordinators. Flagged patients were then introduced to the study and provided with the participant information and consent form by the RO during the new patient clinic. The RO informed potentially interested patients that they would be contacted by phone to further discuss the study and answer any questions. All potential participants were contacted by phone, by an experienced research assistant (RA), prior to their initial radiation planning (SIM) appointment to confirm interest in the study. A signed written consent form was returned prior to the SIM appointment.
Data collection
The RA met participants in the waiting room prior to SIM and treatment sessions 1, 2, 3 and 20 (Tx 1, Tx 2, Tx 3 and Tx 20) to complete a pre‐session survey. The RA then observed the patient in the treatment planning room during SIM (from the control room). During treatment sessions, the RA observed from inside the treatment bunker during treatment set‐up, and the control room during treatment delivery.
Measures
Sociodemographic and clinical information
Sociodemographic (age, sex and marital status) and clinical information (cancer site, histopathology, treatment intent, stage, surgery prior to RT, concurrent chemotherapy, RT dose and fractions), and mental health history (depression, anxiety or claustrophobia noted in clinical records) were extracted from the patient medical record with patient consent.
Situational anxiety
Situational anxiety was assessed using the STAI‐6 13 immediately prior to SIM, Tx 1, Tx 2, Tx 3 and Tx 20. The STAI‐6 is a six‐item scale derived from the original 20‐item State Anxiety subscale of the STAI. 22 , 23 The six items (three describing anxiety states and three describing feelings of calm) are rated on a four‐point Likert scale (1 – not at all, 2 – somewhat, 3 – moderately and 4 – very much). Items are summed (calm items are reverse scored), with higher scores indicating greater anxiety (range 6–24). The STAI‐6 is valid and reliable 24 and suitable for time‐pressured (clinic) situations where using the full measure is not feasible. 24 The established threshold for clinically significant anxiety on the full State Anxiety subscale is 40 or more. 25 Thus, the STAI‐6 scores were prorated (multiplied by 20 and divided by 6) to be comparable to the full subscale, consistent with previous research. 12 , 24
Anxiety management interventions
The research team (including an RO and radiation therapists on the team) devised a list of the clinical anxiety management interventions currently employed in the department as standard care. The list included general supportive interventions, namely music (recorded music playing over speakers in the treatment room) and allowing the presence of a support person (y/n)). Specific interventions for anxious patients were also listed: mask removal (y/n); delivery of relaxation techniques (such as breathing regulation) by staff (y/n); and administration of anxiolytic medication (y/n). These interventions were similar to clinical care strategies described previously. 11
‘Relaxing techniques’ was considered a discreet episode of instruction by the RT or a nurse on breathing techniques and visual imagery, and excluded simple general reassurance, such as single phrases like ‘it's OK’ or ‘we'll look after you’; a break from the mask was recorded if the patient indicated anxiety or emotional distress to the RT and the mask was removed to manage this (rather than being removed for physical discomfort); anxiolytic medication was recorded if identified anxiolyic medication was prescribed. Prior to the trial, a RO provided a summary of commonly used anxiolytics in the RT department.
The identification of the need for an anxiety intervention and the choice of intervention is at the clinical discretion of the attending RTs. RTs informally reported trialling less intensive interventions, such as relaxing techniques, prior to mask removal or medication. In some clinical cases, a high apparent level of anxiety may warrant direct escalation to medication. Use of anxiety management interventions was observed and recorded by the RA (B. Psych) at SIM, Tx 1, Tx 2, Tx 3 and Tx 20.
Statistical analysis
Statistical analyses were performed using SPSS Version 22. Demographic and clinical characteristics are reported descriptively (counts and percentages for categorical variables and means, standard deviations (SD) and ranges for continuous variables). STAI‐6 results were reported descriptively (mean, SD) and a paired‐sample t‐test was conducted to compare differences in the mean STAI‐6 scores (SIM vs. Tx 20 and Tx 1 vs. Tx 20) for each anxiety category. Participants were also categorised into under threshold (<40) and over threshold (≥40) for clinically significant state anxiety at each time point and reported by count and percentage.
To allow for comparison, we classified participants into patterns of anxiety similar to those of Burns et al, 12 previously described above. Classifications were not identical, as the data collection time points varied between studies. In our study, the data collection time points were primarily clustered at the beginning of the treatment journey (SIM, Tx 1, Tx 2 and Tx 3), with one data collection timepoint at the end of treatment (Tx 20), whereas Burns et al 12 collected data over several weeks, then the end of treatment (baseline, weekly from Weeks 1 to 5 and the end of treatment). For the purpose of this analysis, we were interested in the change in anxiety from the start of treatment to the end of treatment. All participants who had data available for at least one time point at the start of treatment (Tx 1 or Tx 2 or Tx 3) and at the end of treatment (Tx 20), were categorised. For those with data available at more than one start of treatment timepoint, the earliest timepoint was used. We chose to use Tx 1, Tx 2 or Tx 3 for the start of treatment rather than SIM as we believe this was the best reflection of their anxiety relating to the mask. It is possible that some (possibly many) participants were unaware of the nature of the mask‐making procedure at the time of data collection prior to SIM. While patients do receive education about the procedure, many patients report not feeling adequately prepared for what it entails. 26 Additionally, as the pre‐session surveys were completed in the waiting room prior to the SIM appointment, participants were yet to receive the standard RT education (explanation of the procedure and images of the mask or other equipment) that is provided immediately before the SIM session. Thus, their anxiety rating may have been lower prior to the appointment. Given that participants were categorised based on the change from the start of treatment to the end of treatment, our approach excludes the ‘Fluctuating Anxiety’ group reported by Burns et al. 12 Criteria for inclusion in each of the categories were:
No Anxiety
Below threshold (<40) at the start and the end of treatment.
Decreasing anxiety
Above threshold (≥40) at the start of treatment and below threshold (<40) at the end of treatment; or above threshold (≥40) at the start of treatment and a clinically meaningful reduction (½ SD 27 ) at the end of treatment.
Increasing anxiety
Below threshold (<40) at the start of treatment and above threshold (≥40) at the end of treatment; or above threshold start of treatment and a clinically meaningful increase (½ SD 27 ) at the end of treatment.
Stable high anxiety
Above threshold (≥40) at the start of treatment and the end of treatment.
Anxiety management interventions (including music; social support; mask removal/taking a break from the mask; use of relaxation techniques; and anxiolytics) are reported descriptively at each time point (count and percentage).
Results
Sample
Between September 2016 and November 2018, 131 patients were approached to participate. Of those, 101 patients agreed to participate and were enrolled in the study, 12 patients declined, seven patients were unable to be contacted to confirm interest in the study, eight patients were missed (approached by RO but not recruited prior to SIM appointment), and three patients were found to be ineligible (no longer requiring a mask/ having fewer than 20 fractions/ having treatment elsewhere).
Sociodemographic and clinical characteristics
The sample was predominantly male (76.2%) with mean (SD) age of 70 years. 10 More than half (57.4%) had cutaneous malignancies. Most participants were being treated with curative intent (93.1%) and over half (59.4%) had early‐stage (I‐II) cancers. Further information is presented in Table 1.
Table 1.
Sociodemographic and clinical characteristics (N = 101).
| Sociodemographics | Mean (SD) | Range |
|---|---|---|
| Age (years) | 69.6 (10.1) | 34–88 |
| Prescribed radiation therapy dose (Gy) | 57.4 (8.01) | 48–70 Gy |
| Prescribed number of treatment fractions | 25.9 (6.44) | 13–35 a |
| n* | %* | |
|---|---|---|
| Sex | ||
| Male | 77 | 76.2 |
| Female | 24 | 23.8 |
| Marital status | ||
| Single | 16 | 15.8 |
| Married/de‐facto | 67 | 66.4 |
| Divorced/separated | 8 | 7.9 |
| Widowed | 10 | 9.9 |
| History of mental health diagnoses | 19 | 18.8 |
| Clinical characteristics | n* | %* |
|---|---|---|
| Site | ||
| Cutaneous | 58 | 57.4 |
| Oropharynx | 16 | 15.8 |
| Oral cavity or lip | 14 | 13.9 |
| Hypopharynx or larynx | 7 | 6.9 |
| Nasal cavity paranasal sinus | 5 | 5 |
| Other | 1 | 1 |
| Histopathology | ||
| SCC | 78 | 77.2 |
| BCC | 14 | 13.9 |
| Sarcoma/AFX | 6 | 5.9 |
| Other | 3 | 3 |
| Treatment intent | ||
| Curative | 94 | 93.1 |
| Palliative | 7 | 6.9 |
| Stage | ||
| 1 | 19 | 18.8 |
| 2 | 41 | 40.6 |
| 3 | 32 | 31.7 |
| 4 | 9 | 8.9 |
| Surgery prior to RT | 70 | 69.3 |
| Concurrent chemotherapy | 16 | 15.8 |
Categorical data are presented as the number and percentage of participants. Continuous data are presented as means (standard deviations) and range. Table key: Gy = Grey, total amount of radiation, SCC = squamous cell carcinoma, BCC = basal cell carcinoma, AFX = atypical fibroxanthoma.
Inclusion criteria specified that participants must be receiving at least 20 fractions to be considered eligible. The number of prescribed fractions was amended for one participant following enrolment in the trial. Thus, given they are missing data for fraction 20, they are included only in the rates and intervention data, and excluded from the categories of anxiety patterns.
Rates of situational anxiety
Approximately a third of participants scored over threshold for clinically significant anxiety at any of the first three time points (33.3–40%) and approximately a quarter scored over threshold at Tx 3 (26.4%) and Tx 20 (23.4%). Overall, there was a gradual decline in the mean (SD) STAI‐6 scores at each time point from 35.1 (14.8) to 30.6 (10.9).
Patterns of situational anxiety
Due to missing data, only 56 participants could be categorised into one of the four groups. Almost half (46.4%) of the reduced sample were categorised in the ‘No Anxiety’ group and more than a third (35.7%) in the ‘Decreasing Anxiety’ group. Seven per cent were considered to have ‘Increasing Anxiety’, and 10% were categorised as ‘Stable High Anxiety’. Mean anxiety scores for the ‘No Anxiety’ group were highest at SIM (28.1, SD = 8.8) and lowest at Tx 3 (23.2, SD = 5.1). There was a significant decrease (P = 0.035) in the mean anxiety score from SIM (28.1) to Tx 20 (24.9); however, the difference between Tx 1 and Tx 20 was not significant. Mean anxiety scores for the ‘Decreasing Anxiety’ group were highest at Tx 1 (46.0, SD = 9.6) and lowest at Tx 20 (27.8, SD = 6.4). There was a significant decrease (P < 0.001) in the mean anxiety score between both SIM (43.3) and Tx 1 (46.0) when compared to Tx 20 (27.8). For the ‘Increasing Anxiety’ group, mean anxiety scores were highest at Tx 20 (41.7, SD = 1.9) and lowest at Tx 2 (27.8, SD = 5.1). There was a significant increase (P = 0.018) in the mean anxiety score from both SIM (35.8) and Tx 1 (32.2) when compared to Tx 20 (41.7). The mean anxiety scores for the ‘Stable High Anxiety’ group were highest at Tx 1 (52.7, SD = 15.7) and lowest at SIM (38.8, SD = 15.3). There was no significant difference between SIM or Tx 1 scores compared with Tx 20 in this group. Anxiety scores for each group are detailed in Table 2 and depicted in Figure 1.
Table 2.
Rates and patterns of situational anxiety by timepoint (N = 101).
| Total sample | SIM | Tx 1 | Tx 2 | Tx 3 | Tx 20 | ||
|---|---|---|---|---|---|---|---|
| (n) | 98 a | 75 a | 57 a | 53 a | 64 a | ||
| Mean | 35.1 | 34.9 | 33.0 | 31.0 | 30.6 | ||
| Std. deviation | 14.8 | 14.7 | 13.2 | 12.3 | 10.9 | ||
| Under threshold (<40) | 62 (63.3%) | 45 (60.0%) | 38 (66.7%) | 39 (73.6%) | 49 (76.6%) | ||
| Over threshold (≥40) | 36 (36.7%) | 30 (40.0%) | 19 (33.3%) | 14 (26.4%) | 15 (23.4%) | ||
| Pattern categories (n = 56) | P (SIM and Tx 20) | P (T × 1 and Tx 20) | |||||
|---|---|---|---|---|---|---|---|
| No anxiety (n = 26) | 26 | 20 | 18 | 19 | 26 | ||
| Mean | 28.1 | 23.5 | 24.3 | 23.2 | 24.9 | 0.035 | 0.280 |
| Std. deviation | 8.8 | 5.2 | 7.2 | 5.1 | 4.9 | ||
| Range | 20.0–46.7 | 20.0–36.67 | 20.0–46.7 | 20.0–36.7 | 20.0–36.7 | ||
| Decreasing anxiety (n = 20) | 20 | 18 | 16 | 14 | 20 | ||
| Mean | 43.3 | 46.0 | 42.5 | 38.6 | 27.8 | <0.001 | <0.001 |
| Std. deviation | 12.3 | 9.6 | 13.9 | 12.7 | 6.4 | ||
| Range | 23.3–66.7 | 36.7–80.0 | 20.0–66.7 | 20.0–63.3 | 20.0–40.0 | ||
| Increasing anxiety (n = 4) | 4 | 3 | 3 | 2 | 4 | ||
| Mean | 35.8 | 32.2 | 27.8 | 31.7 | 41.7 | 0.018 | 0.047 |
| Std. deviation | 1.7 | 5.1 | 5.1 | 7.1 | 1.9 | ||
| Range | 33.3–36.7 | 26.7–36.7 | 23.3–33.3 | 26.7–36.7 | 40.0–43.3 | ||
| Stable high anxiety (n = 6) | 6 | 6 | 3 | 4 | 6 | ||
| Mean | 38.8 | 52.7 | 47.8 | 51.7 | 51.7 | 0.141 | 0.319 |
| Std. deviation | 15.3 | 15.7 | 11.7 | 12.3 | 14.6 | ||
| Range | 20.0–53.3 | 40.0–80.0 | 36.7–60.0 | 43.3–70.0 | 40.0–80.0 |
Observations within each variable may not add to the total sample size due to missing values.
Figure 1.
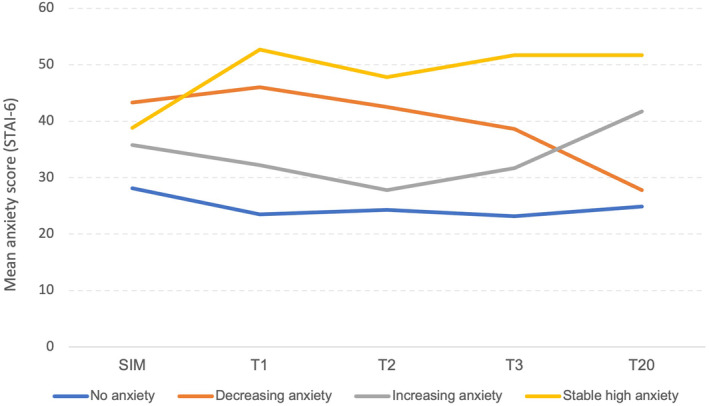
Mean STAI‐6 scores by anxiety pattern group at the start of treatment to the end of treatment.
Clinical Interventions for anxiety management
Interventions provided are shown in Table 3.
Table 3.
Rates of anxiety management interventions at each treatment time point.
| SIM (N = 101) | Tx 1 (N = 93 b ) | Tx 2 (N = 77 b ) | Tx 3 (79 b ) | Tx 20 (N = 77 b ) | |
|---|---|---|---|---|---|
| General supportive interventions | |||||
| Music | 7 (6.9%) a | 85 (90.4%) | 72 (86.7%) | 78 (86.7%) | 78 (92.9%) |
| Social support | 54 (53.5%) | 32 (34.4%) | 24 (31.2%) | 25 (31.6%) | 26 (33.8%) |
| Specific anxiety management interventions | |||||
| Break from the mask (mask removed) | 5 (5.0%) | 3 (3.2%) | 2 (2.4%) | 2 (2.2%) | 1 (1.2%) |
| Relaxing techniques only | 2 (2.0%) | 2 (2.1%) | 2 (2.3%) | 0 (0%) | 1 (1.2%) |
| Anxiolytic medication only | 2 (2.0%) | 4 (4.2%) | 4 (4.6%) | 2 (2.3%) | 3 (3.7%) |
| Relaxing techniques + anxiolytic | 5 (5.0%) | 4 (4.2%) | 5 (5.7%) | 4 (4.6%) | 2 (2.4%) |
The iPod used to play music in the SIM room was broken for most of the period of the study recruitment.
Observations within each variable may not add to the total sample size due to missing values.
General supportive interventions
As playing music is standard procedure at our cancer centre, most participants received music during treatment (86.7–92.9%). However, very few (6.9%) participants received music during SIM due to technical difficulties with the music in the SIM room. At SIM, about half (53.5%) the participants had social support present, decreasing to approximately a third (31.2–34.4%) of participants at each of the treatment time points.
Specific anxiety management interventions
Five participants (5.0%) required a break from the mask (mask removed) at SIM. Anxiolytic medication was provided for 10% of patients at some stage during the treatment journey, either combined with relaxation techniques (2.4–5.7%) or alone (2.0–4.6%). Very few participants received relaxation techniques alone (1.2–2.3%).
Discussion
The findings of this study replicated and extended those of Burns et al. 12 in an urban setting. Similar to Burns et al, 12 in our regional setting, we found that most participants had manageable levels of anxiety (below threshold), which tended to decrease over the course of RT treatment. Also similar to Burns et al., 12 we found a subset of people experienced anxiety at clinically important levels and anxiety did not naturally decrease over time for all. The finding that subsets of participants experienced sustained or increasing anxiety is consistent with the findings of Burns 12 and Nixon. 11 In comparison with Burns, 12 our cohort overall reported somewhat less anxiety. Many more of our sample were categorised into the ‘No Anxiety’ (46%, vs. 19%) and ‘Decreasing Anxiety’ groups (35% vs. 26%), and fewer in the ‘Increasing Anxiety’ (7% vs. 19%) and ‘Stable High Anxiety’ groups (11% vs. 16%). It should be noted we used a higher STAI‐6 cut‐off score (40 or more, the established threshold for STAI‐S) to classify Anxiety compared with the cut‐point of 35 used by Burns. 12 These results are also somewhat comparable to Nixon 11 who reported 6% of participants experienced anxiety that increased over time. However, in contrast to the current study, Nixon 11 reported 22% experienced anxiety that remained constant (compared with 11% in the current study). It is worth noting however that drawing direct comparisons between the two studies is difficult, due to alternate approaches in analyses. Despite this, our findings represent a sizable portion of patients experiencing clinically significant situational anxiety at the end of treatment (23%). This not only suggests a need for improved management of anxiety during RT procedures but also the use of standard measurements of anxiety during RT. [Correction added on 30 November 2023, after first online publication: The percentage of Situational Anxiety in the “Discussion” section has been changed from 16% to 23% in this version].
This study also aimed to document the clinical use of specific anxiety management interventions to support patients with situational anxiety in a major regional cancer RT department. General supportive interventions were commonly used, with approximately 5% of patients requiring a break from the mask and 10% of participants requiring specific anxiety management interventions (relaxation techniques and/or anxiolytic medication). Overall, the frequency of specific anxiety management interventions reduced over time, by approximately half.
Patient receipt of specific anxiety management interventions relies on patients expressing their concern, or staff detecting their anxiety. Radiation therapists are not always able to accurately detect patient anxiety. 28 This is evident at treatment commencement 12 , 28 and continues through treatment with the greatest disparity at the end of treatment. 12 Thus, patients' need for intervention may go undetected, especially among those whose anxiety increases over time.
Given the portion of patients identified in this study, consistent with the literature, it is clear that a number of patients are likely to go through treatment without receiving an anxiety management intervention. This suggests that more work is needed to identify a suitable screening tool to identify patients who meet criteria for clinically significant anxiety prior to and during treatment, to appropriately support these patients through the treatment journey. While there are established screening tools available for patients undergoing HNC treatment, these tools primarily focus on assessing general distress. They take into account factors such as fatigue, difficulties with eating and drinking, mouth sores, sleep disturbances, pain, constipation and loss of interest in usual activities. 29 However, none of these existing tools specifically include situational anxiety as a significant contributor to the overall distress and anxiety experienced by HNC patients.
In the absence of a suitable method of identification, a previous qualitative study (a subset of participants from the same sample) 26 by our team revealed several simple strategies may be used to reduce anxiety. Patients expressed a desire for more information, reporting feeling generally unprepared for the procedure. Additionally, increased control of the music and soundtracks during their treatment sessions was considered important to ensure that the selection of music was calming for the individual. Furthermore, increased communication from clinicians is considered important, especially during particularly anxiety‐provoking times such as when the mask is being clamped down, and a warning from clinicians that patients may become anxious, and what to do (e.g., notify clinicians) if that occurs.
Limitations and future directions
A limitation of this analysis is that close to half of the sample were unable to be included in the patterns analysis due to missing data. At the time of data collection, one RA was responsible for attending participant treatment sessions to complete the pre‐session surveys and collect observational data. The study was conducted in a cancer centre with six treatment bunkers so participant appointments often overlapped, preventing the RA from collecting data from all participants. Furthermore, patient appointment times were often shifted last minute (either at the discretion of the patient or the department) without the knowledge of the RA. Additionally, patients who arrived in the department early were often treated at the time of their arrival, without the RA being present.
Due to incomplete data, it was not possible to map the anxiety management interventions delivered to the groups. This would be useful to explore in future research, to identify the pattern of anxiety for those who received intervention. Another limitation is the lack of an established measure for anxiety during RT procedures. In the absence of a well‐validated measure, we used the STAI‐6, which was not developed for this purpose, but has been used previously. 12 Validation studies of the STAI‐6 for this purpose are warranted. Another limitation of this study is that we did not collect prior experience with RT in this study. Participants who were familiar with the procedure may have demonstrated a different pattern of anxiety to those who were experiencing it for the first time. Additionally, it is important to acknowledge that non‐English speaking patients were excluded from this study. This group of participants might display unique anxiety patterns, potentially stemming from communication challenges with the healthcare team. Consequently, investigating these population subsets could offer valuable insights and represent an important avenue for future research.
We note that the music was unavailable for most (90/101) participants at SIM. Given music can be an effective intervention for anxiety, 30 , 31 it is possible that the observed rates of anxiety and anxiety management may have been reduced had music been available. However, this study is a naturalistic observational study in a ‘real’ RT department and as such reflects the clinical practice reality at the time. We did not assess participants beyond treatment 20 in this study, which may be considered a limitation. Due to the large number of patients being treated with a course of only 20 fractions, it was not feasible in this sample to assess beyond treatment 20; however, this may be an interesting avenue for further research to assess the end of treatment timepoints for those receiving a longer course of RT. Lastly, the recruitment period for this study occurred between 2016 and 2018, and thus, some treatment procedures may have changed since that time.
Conclusions
In a regional cancer setting, anxiety was common and general and specific anxiety management interventions were employed. Most of those with clinically significant anxiety decreased while some experienced persistent anxiety. Standardised measures of anxiety in this group, administered regularly, would assist in evaluating anxiety levels and needs for and effectiveness of treatments. Further research is warranted to examine the interplay between patient‐reported situational anxiety patterns and the anxiety management interventions received.
Author Contributions
KC and SO conceived the initial study idea with valuable input from MK, MT and CW into design and radiation oncology speciality knowledge. Additionally, MK, MT and CW introduced the study to eligible patients. SO facilitated data collection within the radiation oncology department, which was collected by EF and another research assistant (JS). EF analysed the data with input from KC and BB and drafted the manuscript. KC, SO, MK, MT, CW, AB, BB and KM provided extensive feedback on the manuscript.
Funding Statement
This research was funded by the Calvary Mater Newcastle James Lawrie Grant.
Conflict of Interest
The authors have no competing interests to declare.
Patient Consent Statement
Written informed consent was obtained from all participants.
Ethics Approval
The study protocol has received approval from the Hunter New England Health Human Research Ethics Committee (16/02/17/4.07).
Acknowledgements
The research team would like to acknowledge Jessica Searston for significant contributions to the recruitment and data collection in this study. Open access publishing facilitated by The University of Newcastle, as part of the Wiley ‐ The University of Newcastle agreement via the Council of Australian University Librarians.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.
References
- 1. Australian Institute of Health and Welfare . Cancer in Australia 2021. Supplementary tables for Chapter 5: Number of new cancer cases. 2021.
- 2. Australian Institute of Health and Welfare . Cancer data in Australia 2022. Available from: https://www.aihw.gov.au/reports/cancer/cancer‐data‐in‐australia/data?page=2.
- 3. Holmes N, Williamson K. A survey of cancer patients undergoing a radical course of radiotherapy, to establish levels of anxiety and depression. J Radiother Pract 2008; 7: 89–98. [Google Scholar]
- 4. Buchmann L, Conlee J, Hunt J, Agarwal J, White S. Psychosocial distress is prevalent in head and neck cancer patients. Laryngoscope 2013; 123: 1424–1429. [DOI] [PubMed] [Google Scholar]
- 5. Haman KL. Psychologic distress and head and neck cancer: part 1‐‐review of the literature. J Support Oncol 2008; 6: 155–163. [PubMed] [Google Scholar]
- 6. Thornton AF Jr, Ten Haken RK, Gerhardsson A, Correll M. Three‐dimensional motion analysis of an improved head immobilization system for simulation, CT, MRI, and PET imaging. Radiother Oncol 1991; 20: 224–228. [DOI] [PubMed] [Google Scholar]
- 7. Nixon JL, Cartmill B, Turner J, et al. Exploring the prevalence and experience of mask anxiety for the person with head and neck cancer undergoing radiotherapy. J Med Radiat Sci 2018; 65: 282–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Effeney LC, Nixon JL, Pigott AE. Occupational therapy for people with mask anxiety undergoing radiotherapy. Aust Occup Ther J 2021; 68: 374–383. [DOI] [PubMed] [Google Scholar]
- 9. Keast R, Sundaresan P, Burns M, Butow PN, Dhillon HM. Exploring head and neck cancer patients' experiences with radiation therapy immobilisation masks: A qualitative study. Eur J Cancer Care (Engl) 2020; 29: e13215. [DOI] [PubMed] [Google Scholar]
- 10. Klug N, Butow PN, Burns M, Dhillon HM, Sundaresan P. Unmasking anxiety: a qualitative investigation of health professionals; perspectives of mask anxiety in head and neck cancer. J Med Radiat Sci 2020; 51: 12–21. [DOI] [PubMed] [Google Scholar]
- 11. Nixon JL, Brown B, Pigott AE, et al. A prospective examination of mask anxiety during radiotherapy for head and neck cancer and patient perceptions of management strategies. J Med Radiat Sci 2019; 66: 184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burns M, Campbell R, French S, et al. Trajectory of anxiety related to radiation therapy mask immobilization and treatment delivery in Hhead and neck cancer and radiation therapists' Ability to detect this anxiety. Adv Radiat Oncol 2022; 7: 100967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Marteau TM, Bekker H. The development of a six‐item short‐form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br J Clin Psychol 1992; 31: 301–306. [DOI] [PubMed] [Google Scholar]
- 14. National Comprehensive Cancer Network . NCCN Clinical Practice Guidelines in Oncoloy (NCCN Guidelines®): Distress Management, Version 2. 2021. Available from: https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf.
- 15. National Rural Health Alliance . Mental Health in Rural and Remote Australia. 2017.
- 16. Traeger L, Greer JA, Fernandez‐Robles C, Temel JS, Pirl WF. Evidence‐based treatment of anxiety in patients with cancer. J Clin Oncol 2012; 30: 1197–1205. [DOI] [PubMed] [Google Scholar]
- 17. Choy Y. Treatment of acute procedural anxiety in adults: UpToDate. 2019. [updated Mar 05 2019] Available from: https://www.uptodate.com/contents/treatment‐of‐acute‐procedural‐anxiety‐in‐adults.
- 18. Psycho‐Oncology Co‐operative Research Group . Clinical Pathway for the Screening, Assessment and Management of Anxiety and Depression in Adult Cancer Patients. Sydney: Psycho‐oncology Co‐operative Research Group, 2017. [Google Scholar]
- 19. Cancer Council Australia . Understanding Radiation Therapy: A Guide for People with Cancer, their Families and Friends. Cancer Council Australia, Sydney, 2021. [Google Scholar]
- 20. Oncolink Team . Claustrophobia and anxiety with mask use for radiation therapy 2020. Available from: https://www.oncolink.org/cancer‐treatment/radiation/support/claustrophobia‐and‐anxiety‐with‐mask‐use‐for‐radiation‐therapy.
- 21. Icon Cancer Centre . Tips for getting through treatment with a radiation therapy mask. Available from: https://iconcancercentre.com.au/brochure/tips‐for‐getting‐through‐treatment‐with‐a‐radiation‐therapy‐mask/.
- 22. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State‐Trait Anxiety Inventory. Consulting Psychologists Press, Palo Alto, CA, 1983. [Google Scholar]
- 23. Spielberger CD, Gonzalez‐Reigosa F, Martinez‐Urrutia A, Natalicio LFS, Natalicio DS. The state‐trait anxiety inventory. Interamerican Soc Psychol 1971; 5(3 & 4): 145–158. [Google Scholar]
- 24. Tluczek A, Henriques JB, Brown RL. Support for the reliability and validity of a six‐item state anxiety scale derived from the State‐Trait Anxiety Inventory. J Nurs Meas 2009; 17: 19–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Julian LJ. Measures of anxiety: State‐Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale‐Anxiety (HADS‐A). Arthritis Care Res 2011; 63(S11): S467–S472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Forbes E, Clover K, Baker AL, Britton B, Carlson M, McCarter K. ‘Having the mask on didn't worry me until … they clamped my head down so I wouldn't move’: A qualitative study exploring anxiety in patients with head and neck cancer during radiation therapy. J Med Radiat Sci 2023; 70: 283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health‐related quality of life: the remarkable universality of half a standard deviation. Med Care 2003; 41: 582–592. [DOI] [PubMed] [Google Scholar]
- 28. Oultram S, Findlay N, Clover K, Cross L, Ponman L, Adams C. A comparison between patient self‐report and radiation therapists' ability to identify anxiety and distress in head and neck cancer patients requiring immobilization for radiation therapy. J Radiother Pract 2012; 11: 74–82. [Google Scholar]
- 29. Wall LR, Cartmill B, Ward EC, et al. “ScreenIT”: Computerized screening of swallowing, nutrition and distress in head and neck cancer patients during (chemo)radiotherapy. Oral Oncol 2016; 54: 47–53. [DOI] [PubMed] [Google Scholar]
- 30. Chen L‐C, Wang T‐F, Shih Y‐N, Wu L‐J. Fifteen‐minute music intervention reduces pre‐radiotherapy anxiety in oncology patients. Eur J Oncol Nurs 2013; 17: 436–441. [DOI] [PubMed] [Google Scholar]
- 31. Karadag E, Uğur Ö, Çetinayak O. The effect of music listening intervention applied during radiation therapy on the anxiety and comfort level in women with early‐stage breast cancer: A randomized controlled trial. Eur J Integr Med 2019; 27: 39–44. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.


