Abstract
Purpose
To describe the mechanism of progressive hyperopia and its management in the long-term course of traumatic cataract with a posterior capsule tear (PCT) following blunt ocular trauma.
Observation
A 37-year-old woman presented with blurry vision and photophobia after being hit in the right eye by a slipper. She was found to have PCT with the formation of a traumatic cataract with emmetropia (0 diopters [D]). Three years after the injury, a broader hyperopic change of +8.0 D was found in the patient at her first visit to our clinic. Optical coherence tomography (OCT) analysis of the anterior segment of the eye revealed damage to the posterior capsule and cataracts due to disorganization of the lens fibers and liquefaction of the lens. Femtosecond laser-associated cataract surgery was performed for anterior capsulotomy and segmentation of the nucleus without further enlargement of the PCT, facilitating the placement of a capsular tension ring segment and a multifocal intra ocular lens (IOL) in the capsular bag. At 1-month post-operation, her uncorrected visual acuity was 20/20 in the right eye, with a well-centered IOL.
Conclusions and Importance
Isolated PCT due to blunt trauma is rare, and there have been no reports of progressive hyperopia after three years of follow-up. In such cases, the lens may liquefy, resulting in decreased refraction and significant hyperopia.
Keywords: Blunt ocular trauma, Hyperopia, Posterior capsule tear, Traumatic cataract
1. Introduction
Blunt ocular trauma can cause various symptoms, including corneal endothelial damage, iris root avulsion, traumatic cataracts, and lens dislocation.1 Isolated posterior capsule tear (PCT) following blunt eye injury or lens dislocation, is a rare condition.2 Traumatic cataracts can often result in sudden vision loss, and surgery is often performed immediately after the injury. Here, we report a rare case of a patient with gradual and marked hyperopia due to PCT caused by blunt ocular trauma. We also describe the mechanism of hyperopic changes in blunt traumatic cataracts and the surgical management for the implantation of multifocal intraocular lenses (IOL).
2. Case report
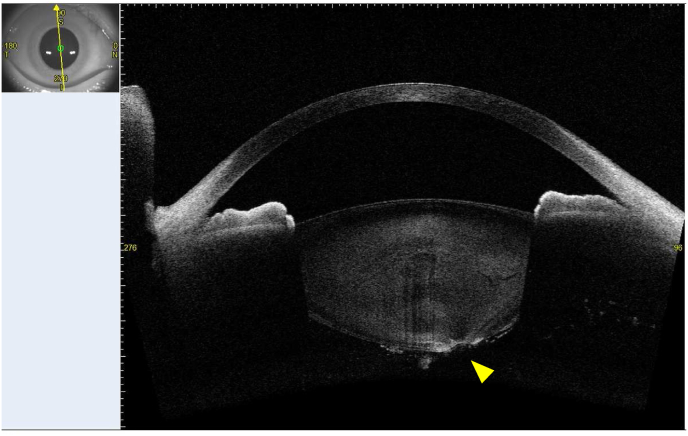
A 37-year-old woman visited her primary care eye clinic after a slipper had hit her right eye. Anterior segment biomicroscopy showed traumatic PCT surrounding the opacity of the lens material and vitreous opacity, with herniation of the lens material (Fig. 1A). Her uncorrected visual acuity (UCVA) was 20/32 in her right eye and 20/16 in her left eye, with emmetropia (+0 diopters [D]). The patient did not require any surgical treatment. Three years after the trauma, refraction of the right eye became +8.0D hyperopic. She complained of progressively blurry vision. The best-corrected visual acuity (BCVA) of her right eye was 20/50 and that of her left eye was 20/16, with a refraction of +8.0D −0.74D × 20° on the right and −0.32D −0.29D × 90° on the left. Intra ocular pressure (IOP) was 19.0 mmHg in both, the right and the left eye, respectively, and her right and left pupil diameters were 3.4 mm and 3.2 mm, respectively. The mean corneal refractive power of the right eye was 44.27D and that of the left eye was 44.43D as measured by swept-source anterior segment optical coherence tomography (SS-AS OCT). The right eye had an axial length of 22.20 mm, which was similar to the left eye (22.20 mm) by A-scan ultrasonography. Slit-lamp microscopy revealed no corneal or iris abnormalities. Lens opacity with fibrotic tissues and vitreous cell reflux from the capsule tear had decreased in the right eye compared with that at the first visit to the previous clinic (Fig. 1B). Fundus findings were normal in both right and left eyes. SS-AS OCT showed distorted lens fibers and round hole at the posterior capsule in the right eye (Fig. 2). The anterior chamber depths were 3.28 mm and 3.37 mm on the right and left, respectively. Lens inclinations and eccentricities were 6.0° and 0.41 mm on the right and 2.4° and 0.16 mm on the left. The central lens thickness was 4.46 mm in the right and 4.09 mm in the left eye, indicating a thicker lens in the injured right eye. A transverse lens fiber crack was observed in the lens nucleus (Fig. 2). The patient expressed a strong desire for cataract surgery with a multifocal IOL. Femtosecond laser-assisted capsulotomy surgery (FLACS) was performed using a LenSx femtosecond laser (Alcon Inc., Geneva, Switzerland). The capsulorrhexis was 5.0 mm in diameter and was centered on the capsular bag. Quartered segmentation of the lens nucleus was performed once laser energy was applied. The patient was then placed under the operating microscope, and paracentesis and main incisions were performed using a 2.2 mm slit knife. Careful delineation using a viscoelastic material and standard lens aspiration were carefully performed to avoid tear enlargement in PCT. A capsular tension ring was not used at this time. A 25.0D multifocal IOL (CNAET0; Alcon Laboratories, TX, USA) was implanted into the capsular bag (Fig. 3). At one-month post-operative visit, her UCVA was 20/20 with a refraction of 0.00D −0.70D × 163° in the right eye. SS-AS-OCT revealed a fixed IOL position with an eccentricity of 0.29 mm and an inclination of 5.3° in the right eye.
Fig. 1.
Slit lamp biomicroscopy of the right eye showing a round shaped PCT (with arrows demarcating the tear). A: A slit lamp image at the first visit after trauma. B. A slit lamp image three years after trauma. PCT, posterior capsule tear.
Fig. 2.
SS-AS OCT showing distortion of lens fibers and PCT of the right eye (with arrows demarcating the tear). There is a large fissure from the central portion of the lens nucleus to the equator showing the dark area. SS-AS OCT, swept-source anterior segment optical coherence tomography; PCT, posterior capsule tear.
Fig. 3.
Post-operative retroillumination image of the IOL centered in the bag with an outline of the PCT (with arrows demarcating the tear), no eccentricity, or tilt. PCT, posterior capsule tear; IOL, intraocular lens.
3. Discussion
Blunt traumatic cataracts are relatively common in males pediatric patients; however, there is little literature on isolated PCT associated with this condition.3, 4, 5 Blunt trauma causes compression along the anterior-posterior axis and simultaneous expansion of the equatorial plane.3,5 The anteroposterior vector forces to the posterior capsule from blunt ocular trauma preferentially tear the elastic posterior capsule in young patients, probably due to strong adhesions to the Wieger's ligament.4,5 As indicated in a previous study,4 we hypothesize the mechanism of blunt trauma-induced blowout PCT in this case to be due to combination of the following forces 1) equatorial elongation of the globe following blunt trauma leads to stretching of zonules and posterior capsule; 2) anteroposterior vector force to the posterior capsule from direct trauma; 3) preferential rupture of elastic posterior capsule because the zonules are strong in this patient. This case is rare, because it involved a traumatic cataract with isolated PCT that did not immediately require cataract surgery. In this patient, the indication for surgery was not only visual loss but also progressive hyperopia. Previous studies have indicated that changes in the lens composition may induce hyperopia.6, 7, 8 Furthermore, intensive glycemic control has often been reported to induce acute hyperopia caused by changes in the lens composition in patients with diabetes.6, 7, 8 Hyperglycemia in patients with diabetes occur when excess glucose in the lens is converted to sorbitol, a sugar alcohol, by the action of aldose reductase.9 However, strict glycemic control in patients with diabetes leads to a sudden hypoglycemic state, and excess sugar in the lens leaks into the aqueous humor; however, the accumulated sorbitol persists, resulting in difference in osmotic pressure between the lens and aqueous humor.8 It is widely hypothesized that hyperopia is caused by an osmotic pressure difference between the lens and aqueous humor, which causes an influx of water from the aqueous humor into the lens causing lenticular swelling and a decrease in the overall refractive index of the lens.7,8 In addition, we reported that water clefts, which are a type of lens opacity, also cause hyperopia.10 Water clefts are formed when the cortex separates from the Y-shaped suture on the surface of the lens, and the interior of the opacity is thought to be filled with fluid, similar to aqueous humor.11,12 In this patient, the large crack in the center of the lens nucleus with low signal intensity (Fig. 2) suggested that hyperopic changes occurred, owing to refractive changes at the border in the low- and high-luminance planes. Additionally, in this patient, the lens fibers near the injured capsule were swollen and liquefied, which increased lens thickness. Protein structure, water content, and capsule property of the lens are important for maintaining the lens biometry and gradient refractive index (GRIN) of the lens.13,14 The GRIN of the lens is thought to result in minimal refractive power at the lens periphery and a maximum refractive index at the center of the lens. Furthermore, lens fiber cracks and PCT after blunt trauma may induce the oxidative stress and damage the internal circulation of salt and water in the lens as well as intracellular homeostasis. We presume that hyperopic shift was induced by the change of protein conformation, which would result in a release of their bound water and an increase in the content of free water, specifically in the injured region, subsequently affecting the GRIN of the lens.13 We speculate that PCT induced water inflow and oxidative stress by blunt trauma reduced the water outflow in lens cortex and nucleus, thereby diluting the protein concentration, and specifically decreasing the refractive index in the lens nucleus. Thus, changes to the lens geometry and water content by traumatic cataracts and capsule tears can result in modification of the GRIN, inducing a progressive hyperopic shift.13,14
In this case, a patient with a blunt traumatic cataract was treated with FLACS following implantation of a multifocal IOL in the capsular bag. For surgical management, it is important to minimize the stretching of the PCT, prevent posterior dislocation of the lens material, and retain an almost complete capsule to support the multifocal IOL in the capsular bag. We safely performed femtosecond laser-assisted capsulotomy and nuclear segmentation without PCT enlargement and conducted viscodissection and careful aspiration of the lens material. These steps facilitated the retention of most of the capsular bag and the placement of multifocal IOL placement in the capsular bag. In addition, the formation of fibrosis around the PCT may have prevented the PCT enlargement during cataract surgery.
4. Conclusion
This patient represents an unusual case of traumatic cataract with isolated PCT that presented with hyperopic changes over a three-year period. This case suggests that trauma-induced changes in lens biometry and GRIN can cause progressive hyperopia depending on the site of injury and with passage of time. Furthermore, our report suggests the advantages of using FLACS and multifocal IOL for the management of traumatic PCT.
Patient consent statement
Written consent to publish potentially identifying information, such as details or the case and photographs, was obtained from the patient.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Kanzawa Medical University (Approved No. C034).
Funding
None.
CRediT authorship contribution statement
Teppei Shibata: Writing – original draft, Methodology, Investigation, Conceptualization. Yusuke Seki: Methodology. Yukiya Seida: Methodology. Tsuyoshi Yoshita: Investigation. Shunsuke Tsuchiya: Resources. Hiroshi Sasaki: Writing – review & editing, Supervision, Conceptualization. Eri Kubo: Writing – review & editing, Project administration, Investigation, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Contributor Information
Teppei Shibata, Email: prefse74@yahoo.co.jp.
Yusuke Seki, Email: yusuke-s@kanazawa-med.ac.jp.
Yukiya Seida, Email: seida-y@kanazawa-med.ac.jp.
Tsuyoshi Yoshita, Email: info-yec@yoshita-eye.com.
Shunsuke Tsuchiya, Email: s.tsuchiya@med.kanazawa-u.ac.jp.
Hiroshi Sasaki, Email: sasaki-h@k5.dion.ne.jp.
Eri Kubo, Email: kuboe@kanazawa-med.ac.jp.
References
- 1.Canavan Y.M., Archer D.B. Anterior segment consequences of blunt ocular injury. Br J Ophthalmol. 1982;66(9):549–555. doi: 10.1136/bjo.66.9.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saika S., Kin K., Ohmi S., Ohnishi Y. Posterior capsule rupture by blunt ocular trauma. J Cataract Refract Surg. 1997;23(1):139–140. doi: 10.1016/s0886-3350(97)80167-8. [DOI] [PubMed] [Google Scholar]
- 3.Choudhary N., Verma S.R., Sagar S., Fatima E. Posterior capsule rupture with herniation of lens fragment following blunt ocular trauma. Int Med Case Rep J. 2016;9:305–307. doi: 10.2147/IMCRJ.S117911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mansour A.M., Jaroudi M.O., Hamam R.N., Maalouf F.C. Isolated posterior capsular rupture following blunt head trauma. Clin Ophthalmol. 2014;8:2403–2407. doi: 10.2147/OPTH.S73990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wolter J.R. Coup-contrecoup mechanism of ocular injuries. Am J Ophthalmol. 1963;56:785–796. doi: 10.1016/0002-9394(63)92943-x. [DOI] [PubMed] [Google Scholar]
- 6.Lin S.F., Lin P.K., Chang F.L., Tsai R.K. Transient hyperopia after intensive treatment of hyperglycemia in newly diagnosed diabetes. Ophthalmologica. 2009;223(1):68–71. doi: 10.1159/000173714. [DOI] [PubMed] [Google Scholar]
- 7.Okamoto F., Sone H., Nonoyama T., Hommura S. Refractive changes in diabetic patients during intensive glycaemic control. Br J Ophthalmol. 2000;84(10):1097–1102. doi: 10.1136/bjo.84.10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saito Y., Ohmi G., Kinoshita S., et al. Transient hyperopia with lens swelling at initial therapy in diabetes. Br J Ophthalmol. 1993;77(3):145–148. doi: 10.1136/bjo.77.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kador P.F., Akagi Y., Kinoshita J.H. Diabetic cataracts in animal models: prevention and reversibility with aldose reductase inhibitors. Diabet Med. 1985;2(3):194–196. doi: 10.1111/j.1464-5491.1985.tb00634.x. [DOI] [PubMed] [Google Scholar]
- 10.Tanimura N., Hatsusaka N., Miyashita H., et al. Visual function and functional decline in patients with waterclefts. Invest Ophthalmol Vis Sci. 2019;60(10):3652–3658. doi: 10.1167/iovs.19-26793. [DOI] [PubMed] [Google Scholar]
- 11.Brown N.P., Harris M.L., Shun-Shin G.A., Vrensen G.F., Willekens B., Bron A.J. Is cortical spoke cataract due to lens fibre breaks? The relationship between fibre folds, fibre breaks, waterclefts and spoke cataract. Eye. 1993;7(Pt 5):672–679. doi: 10.1038/eye.1993.154. [DOI] [PubMed] [Google Scholar]
- 12.Michael R., Barraquer R.I., Willekens B., van Marle J., Vrensen G.F. Morphology of age-related cuneiform cortical cataracts: the case for mechanical stress. Vis Res. 2008;48(4):626–634. doi: 10.1016/j.visres.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Donaldson P.J., Grey A.C., Maceo Heilman B., Lim J.C., Vaghefi E. The physiological optics of the lens. Prog Retin Eye Res. 2017;56:e1–e24. doi: 10.1016/j.preteyeres.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Rich W., Reilly M.A. A review of lens biomechanical contributions to presbyopia. Curr Eye Res. 2023;48(2):182–194. doi: 10.1080/02713683.2022.2088797. [DOI] [PubMed] [Google Scholar]