Abstract
Background
Prediabetes is a high-risk state for diabetes, and numerous studies have shown that the body mass index (BMI) and triglyceride-glucose (TyG) index play significant roles in risk prediction for blood glucose metabolism. This study aims to evaluate the relative importance of BMI combination with TyG index (TyG-BMI) in predicting the recovery from prediabetic status to normal blood glucose levels.
Methods
A total of 25,397 prediabetic subjects recruited from 32 regions across China. Normal fasting glucose (NFG), prediabetes, and diabetes were defined referring to the American Diabetes Association (ADA) criteria. After normalizing the independent variables, the impact of TyG-BMI on the recovery or progression of prediabetes was analyzed through the Cox regression models. Receiver Operating Characteristic (ROC) curve analysis was utilized to visualize and compare the predictive value of TyG-BMI and its constituent components in prediabetes recovery/progression.
Results
During the average observation period of 2.96 years, 10,305 individuals (40.58%) remained in the prediabetic state, 11,278 individuals (44.41%) recovered to NFG, and 3,814 individuals (15.02%) progressed to diabetes. The results of multivariate Cox regression analysis demonstrated that TyG-BMI was negatively associated with recovery from prediabetes to NFG and positively associated with progression from prediabetes to diabetes. Further ROC analysis revealed that TyG-BMI had higher impact and predictive value in predicting prediabetes recovering to NFG or progressing to diabetes in comparison to the TyG index and BMI. Specifically, the TyG-BMI threshold for predicting prediabetes recovery was 214.68, while the threshold for predicting prediabetes progression was 220.27. Additionally, there were significant differences in the relationship of TyG-BMI with prediabetes recovering to NFG or progressing to diabetes within age subgroups. In summary, TyG-BMI is more suitable for assessing prediabetes recovery or progression in younger populations (< 45 years old).
Conclusions
This study, for the first time, has revealed the significant impact and predictive value of the TyG index in combination with BMI on the recovery from prediabetic status to normal blood glucose levels. From the perspective of prediabetes intervention, maintaining TyG-BMI within the threshold of 214.68 holds crucial significance.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12944-024-02060-w.
Keywords: Triglyceride-Glucose index, Body mass index, Prediabetes regression, Prediabetes recovering, Recovery from prediabetes
Background
Prediabetes, defined by blood glucose levels higher than normal but below the threshold for diabetes, is also referred to as non-diabetic hyperglycemia or moderate hyperglycemia [1–3]. The term prediabetes was initially used to designate individuals with a high likelihood of developing diabetes in the future [4]. However, with advancements in research, prediabetes is now recognized as a marker indicating heightened risk for future kidney disease, microvascular complications, small fiber neuropathy, tumors, vascular diseases [1–3]. It is also closely linked to accelerated bone loss [5], rapid cognitive aging [6], and even an increased risk of mortality [5]. Fortunately, most cases of hyperglycemia in prediabetes are recoverable. Several randomized controlled trials investigating drug interventions or lifestyle modifications have reported research outcomes demonstrating the recovery of prediabetes to normal blood glucose levels [7–17]. In summary, recovery from prediabetes is beneficial, as the significant return to normal blood glucose levels reduces the risk of diabetes and various long-term complications in study participants. Given that there are over 400 million people worldwide in a prediabetic state [18], it will be of great benefit to reverse the situation and the consequent benefits if the changeable factors that affect the return to normal blood glucose in pre-diabetes can be identified early.
Over the past few decades, disease progression-related research, including prediabetes, has received widespread attention worldwide [1–3]. Relatively less research, however, has focused on the process of recovery from prediabetes to normal blood glucose [19]. From the perspective of disease development, insulin resistance (IR) and β-cell dysfunction are key factors in the progression from normal blood glucose to prediabetes [1, 20, 21]. From a treatment standpoint, improving IR and β-cell function are key elements in facilitating the transition from prediabetes to normal blood glucose [22]. This bidirectional evidence further underscores the importance of effectively assessing IR status for the prevention and management of prediabetes. Currently, the hyperinsulinemic-euglycemic clamp technique is upheld as the gold standard for measuring IR in the field [23]. However, due to its technical complexity and invasiveness, this technique is greatly limited in clinical practice and disease screening [24]. TyG-BMI is an alternative for assessing IR, developed in recent years. It builds upon the IR surrogate index TyG index and further considers the potential impact of obesity [25]. According to the report of Ko et al., TyG-BMI has significantly higher value in assessing IR compared to traditional lipid measurement parameters, lipid ratios, adipokine, and the TyG index. Subsequently, in multiple longitudinal studies, researchers have found that TyG-BMI also has good predictive value in assessing prediabetes and diabetes progression [26–30]. However, it remains unclear whether TyG-BMI plays a significant role and to what extent it influences the process of recovery from prediabetes to normal blood glucose.
Methods
Data source and study population
This retrospective analysis of a longitudinal study employed health examination data from the Rich Healthcare Group in China on a national scale. The dataset, collected and compiled by Chen et al., includes adult health examination participants recruited by the Rich Healthcare Group (2010–2016) in 32 regions across 11 cities in China, and these subjects underwent health examinations at least twice during this period (n = 685,277). In the initial data analysis, Chen et al. investigated the association between BMI and the risk of future diabetes [31]. They excluded participants who had the following conditions: (i) participants with missing data at baseline, including sex, fasting plasma glucose (FPG), weight and height (n = 135,317); (ii) participants who had a confirmed diabetes diagnosis at the time of the first evaluation (n = 7,112); (iii) subjects with extreme BMI values (n = 152); (iv) participants with an interval of less than 2 years between two consecutive visits (n = 324,233); and (v) participants with unknown diabetes status during longitudinal observation (n = 6,630). In the end, Chen et al. evaluated 211,833 participants in their data analysis related to the association between BMI and diabetes. The dataset used for their research analysis has also been publicly shared on the DRYAD database by them [32]. According to the DRYAD database usage terms, the researchers can engage in secondary analysis based on the original data provided by Chen et al. after properly acknowledging the data source [32].
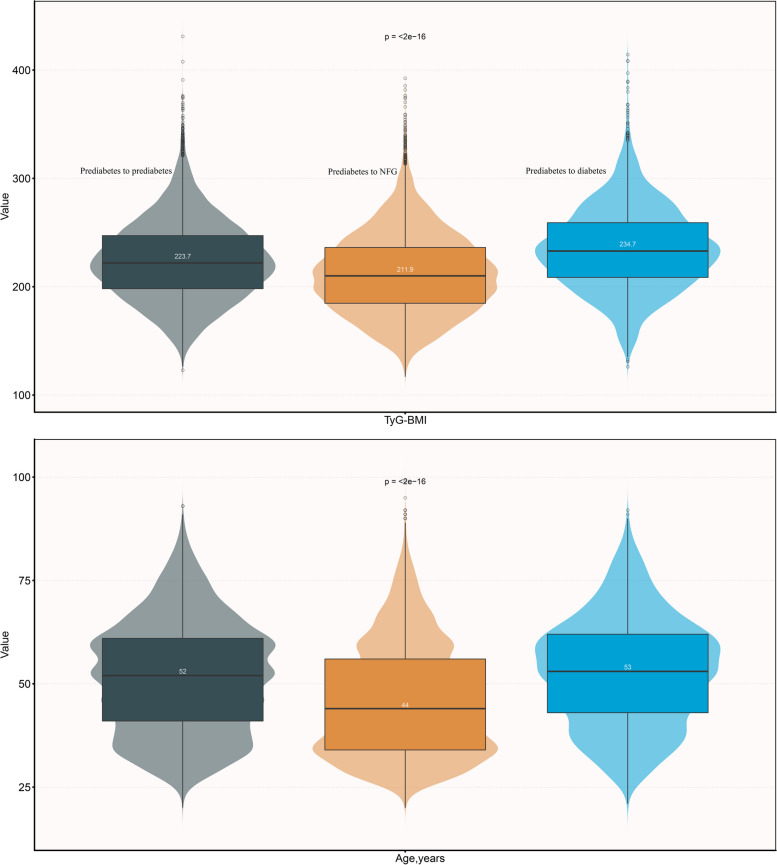
The research hypothesis of the current study: Does TyG-BMI play a role in the recovery of prediabetic status to normal blood glucose, and if so, to what extent? Based on the dataset analyzed by Chen et al. [32], this study further conducted the inclusion of the study population following the criteria outlined in Fig. 1, as detailed below: (i) Non-prediabetic subjects were excluded according to ADA's pre-diabetic diagnostic criteria [33] (ii) Participants with missing values for independent variables. (iii) Participants who lacked follow-up FPG data or had an unclear diabetes status. This research is a secondary analysis, a new research protocol has been submitted and approved by the Jiangxi Provincial People's Hospital Ethics Committee (No. 2021–067). Additionally, considering that the dataset has been anonymized, the ethics Committee of the author's institution waived the signing of the informed consent form of the participants. The entire secondary analysis process strictly adhered to the STROBE reporting guidelines, as detailed in Supplementary Table 1.
Fig. 1.
Flow chart of study participants
Baseline data measurement and collection
As previously described in the earlier study [31], participants were required to complete a standardized questionnaire survey during each health screening, documenting their living habits (drinking/smoking status), the presence of chronic diseases (such as diabetes), and family history (family history of diabetes). Anthropometric measurements, including height, weight, and blood pressure (BP), were conducted by trained healthcare professionals in a standard environment. Among them, BP measurements were taken using a mercury sphygmomanometer, a trusted device for accurately measuring blood pressure. Participants were instructed to wear light clothing and take off their shoes for precise height and weight measurements, which were recorded to 1 decimal place. Biochemical measurements required participants to collect venous blood samples after at least 10 h on an empty stomach, which were subsequently analyzed in a standard laboratory using automated analytical instruments. The current dataset includes the following biochemical parameters: aspartate aminotransferase (AST), high-density lipoprotein cholesterol (HDL-C), alanine aminotransferase (ALT), triglycerides (TG), creatinine (Cr), total cholesterol (TC), blood urea nitrogen (BUN), low-density lipoprotein cholesterol (LDL-C) and FPG, in which FPG was measured by oxidase method.
Calculation [25]
Follow-up and outcomes
The study population included individuals who were initially diagnosed with prediabetes at baseline. Any changes in blood glucose status that occurred during the follow-up period constituted the outcomes of interest, including the progressing to diabetes or recovery of prediabetes to NFG. The determination of NFG, prediabetes, and diabetes in the current analysis was based on the ADA’s diagnostic criteria, which relies on FPG levels [33]. Specific as follows: (i) NFG: During the observation period, FPG returned to below 5.6 mmol/L. (ii) Prediabetes: FPG levels ranging from 5.6 to 6.9 mmol/L. (iii) Diabetes: FPG levels exceeding 7.0 mmol/L during the observation period or self-reported diabetes diagnosis by other healthcare professionals.
Statistical analysis
The study's analyses utilized R version 3.4.1 and Empower(R) version 2.0 software. A two-tailed P-value < 0.05 indicated statistical significance. For the description of baseline variables were grouped and summarized according to study outcomes. The type of baseline variable and type of distribution (Judging by histogram) were first assessed, and then in subsequent tables were reported as mean [standard deviation (SD)]/median (interquartile spacing)/frequency (%).
For the multi-classified study endpoints in the current study, the researchers used one-versus-rest to split the data to a binary dataset for each class [34, 35], and investigated the effect of TyG-BMI on the recovery/progression of prediabetes separately. As the main analytical method, stepwise-adjusted multivariate Cox regression models were used for the assessment of associations in the current study [36], and the hazard ratio (HR) per SD increase and its confidence interval (CI) were recorded. Furthermore, before establishing the models, the variance inflation factor was calculated for covariates to assess collinearity among covariates [37]. Three progressively adjusted multivariate regression models were constructed for the association analysis in the current study. Model I adjusted height, age and sex; Model II further considered the potential influence of lifestyle factors and BP; Model III made additional adjustments to FPG, TG, Cr, BUN and ALT based on model II. Based on Model III, the researchers also employed restricted cubic splines (RCS) in four knots nested within Cox regression to fit and visualize the relationship of TyG-BMI with the progression or recovery of prediabetes.
To validate the stability of the impact of TyG-BMI on the recovery/progression of prediabetes, the researchers conducted a series of sensitivity analyses: (i) TyG-BMI was categorized into quartiles and examined the trend of association between TyG-BMI and prediabetes recovery/progression based on the median of the categorical variable. (ii) According to the prediabetes and diabetes diagnostic criteria published by the WHO [38], the study subjects were re-included and excluded, and performed the same steps of association analysis. (iii) The occurrence of diabetes events as the study outcome precludes us from observing the potential recovering to NFG in this subset of the population. Therefore, the competing risk model was applied with diabetes events as the competing endpoint to assess the association of TyG-BMI and its components with prediabetes recovery or reversal. (iv) Considering the direct and indirect potential impact of a family history of diabetes on blood glucose [39, 40], the researchers conducted the same analysis in people without a family history of diabetes. (v) To account for potential unmeasured confounding, the researchers calculated the E-value [41]. (vi) 3 and 5 knots of RCS were used to test the linearity of the relationship of TyG-BMI with prediabetes recovery.
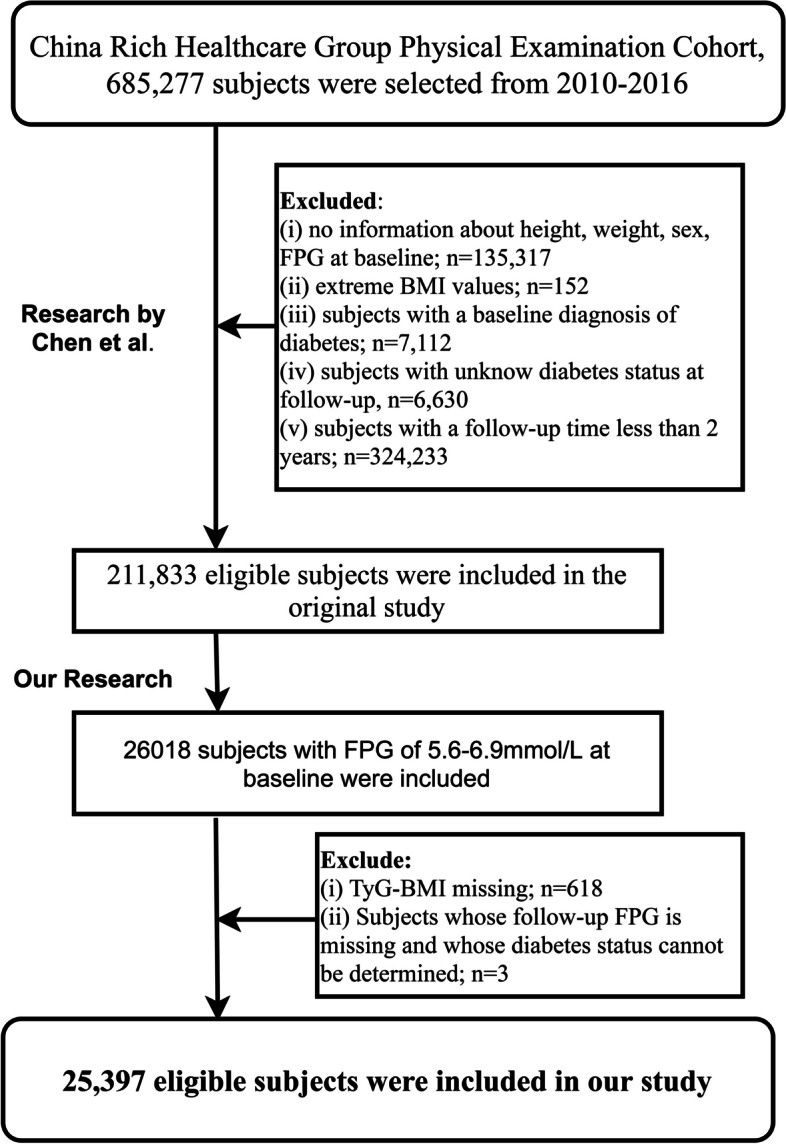
After determining the relationship of TyG-BMI with prediabetes recovery/progression, the researchers aimed to further assess the predictive power of TyG-BMI in prediabetes recovery/progression. To address this issue, the researchers conducted ROC analysis, calculating metrics such as the area under the curve (AUC), optimal threshold, sensitivity, and specificity, and compared the predictive value of TyG-BMI and its component parts for prediabetes recovery/progression using the DeLong test [42].
The researchers also conducted several subgroup analyses within several common phenotypic subgroups known to have a significant impact on blood glucose levels, including sex, age, and BMI. Age stratification followed WHO classification standards [43], while BMI stratification followed the guidelines suggested by the Chinese Obesity Working Group [44]. Likelihood ratio tests were used to assess interactions between TyG-BMI and the stratification variables.
Results
Follow-up results and study population characteristics
This study included a total of 25,397 participants initially diagnosed with prediabetes, with an average age of 49 years and males comprising 66.28% of the cohort. Over an average observation period of 2.96 years, among the 25,397 participants, 10,305 individuals (40.58%) remained in the prediabetic state, 11,278 individuals (44.41%) experienced a return to normal blood glucose levels, and 3,814 individuals (15.02%) progressed to diabetes.
Under the condition where prediabetes progressing to diabetes or recovering to NFG were considered as competing risks, the researchers computed the cumulative incidence rates of prediabetes recovering to NFG or progressing to diabetes using cumulative incidence functions and visualized these competing risks with cumulative incidence curves (Fig. 2). According to the calculations, in the third, fourth, fifth, and sixth years of follow-up, the cumulative incidence rates of prediabetes recovering to NFG were 31.72%, 50.45%, 64.89%, and 72.88%, respectively, and that of prediabetes progressing to diabetes were 9.4%, 16.57%, 23.36%, and 26.93%, respectively. It can be observed that prediabetic participants had a higher likelihood of recovering to NFG compared to progressing to diabetes.
Fig. 2.
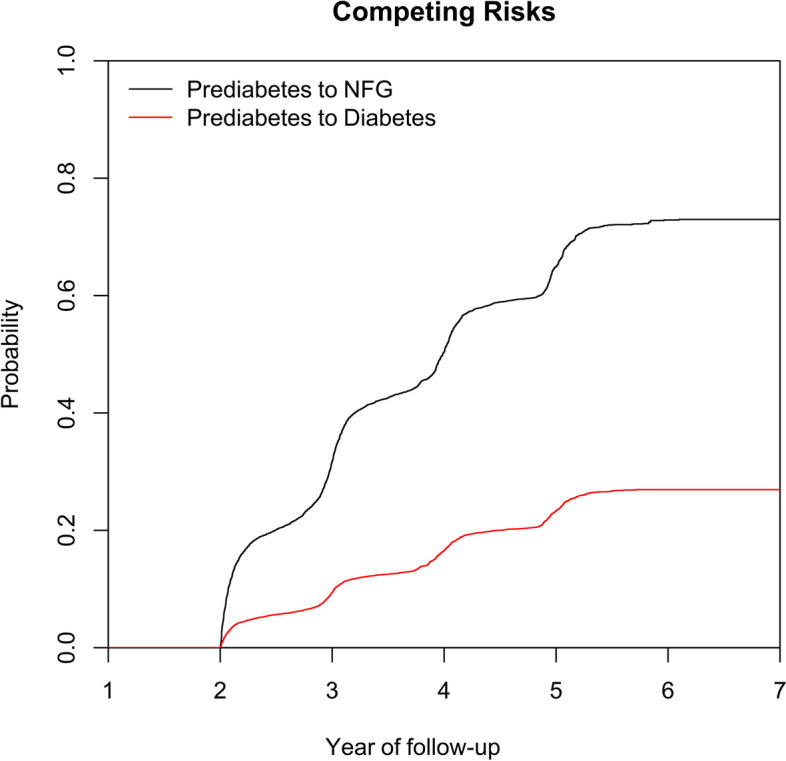
Cumulative incidence curve of prediabetes recovering to NFG or progressing to diabetes
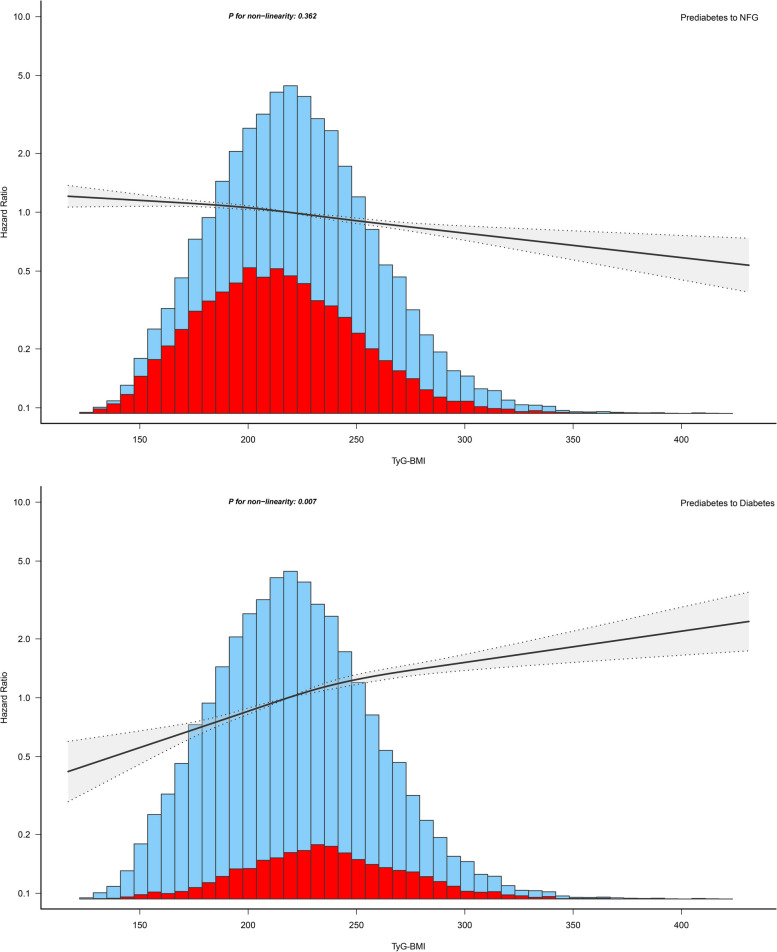
The baseline characteristics of the study population were summarized at the initial point of inclusion, based on their glycemic status observed during the follow-up period (Table 1). It is noteworthy that, in comparison to participants who remained prediabetic or progressed to diabetes in the future, the researchers observed distinct baseline characteristics among those who later recovered to NFG, as summarized below: (i) Individuals who eventually recovered to NFG had relatively lower baseline values for Cr, LDL-C, BMI, weight, age, TG, BUN, BP measurements, FPG, ALT, TyG index, TyG-BMI, AST, TC, with age and TyG-BMI showing particularly notable differences (Fig. 3). (ii) Among this subgroup, there was a higher proportion of females, a greater prevalence of a family history of diabetes, and fewer individuals with smoking and drinking habits.
Table 1.
Baseline characteristics summarized according to subjects' glycemic status during follow-up
| Glucose status during follow-up | |||
|---|---|---|---|
| Prediabetes | NFG | Diabetes | |
| No. of subjects | 10,305 | 11,278 | 3814 |
| Sex | |||
| Male | 7031 (68.23%) | 7087 (62.84%) | 2716 (71.21%) |
| Female | 3274 (31.77%) | 4191 (37.16%) | 1098 (28.79%) |
| Age, years | 52.00 (41.00–61.00) | 44.00 (34.00–56.00) | 53.00 (43.00–62.00) |
| Height, cm | 166.56 (8.32) | 166.75 (8.40) | 166.92 (8.28) |
| Weight, kg | 69.40 (61.00–77.50) | 67.00 (58.80–75.38) | 72.00 (64.00–80.00) |
| BMI, kg/m2 | 25.08 (3.25) | 24.19 (3.31) | 25.92 (3.43) |
| SBP, mmHg | 129.12 (17.83) | 124.18 (16.77) | 131.11 (17.98) |
| DBP, mmHg | 79.46 (11.24) | 76.74 (10.77) | 80.51 (11.31) |
| FPG, mmol/L | 5.99 (0.32) | 5.83 (0.24) | 6.15 (0.37) |
| TC, mmol/L | 5.03 (0.95) | 4.90 (0.95) | 5.07 (0.99) |
| TG, mmol/L | 1.50 (1.02–2.21) | 1.28 (0.87–1.92) | 1.68 (1.14–2.49) |
| HDL-C, mmol/L | 1.31 (1.13–1.51) | 1.34 (1.15–1.54) | 1.29 (1.09–1.50) |
| LDL-C, mmol/L | 2.91 (2.47–3.37) | 2.84 (2.41–3.33) | 2.89 (2.43–3.40) |
| TyG index | 8.89 (0.61) | 8.73 (0.62) | 9.03 (0.61) |
| TyG-BMI | 223.73 (36.74) | 211.89 (37.27) | 234.69 (38.41) |
| ALT, U/L | 22.90 (16.00–33.40) | 20.30 (14.20–31.00) | 25.00 (18.00–38.60) |
| AST, U/L | 24.00 (20.00–29.00) | 23.60 (19.60–29.00) | 25.00 (21.00–31.70) |
| BUN, mmol/L | 4.91 (4.18–5.80) | 4.80 (4.03–5.68) | 4.90 (4.13–5.78) |
| Cr, umol/L | 73.10 (62.00–83.72) | 72.00 (60.00–82.60) | 72.70 (62.00–82.70) |
| Family history of diabetes | 236 (2.29%) | 244 (2.16%) | 140 (3.67%) |
| Smoking status | |||
| Current | 926 (8.99%) | 877 (7.78%) | 377 (9.88%) |
| Past | 136 (1.32%) | 193 (1.71%) | 69 (1.81%) |
| Never | 2362 (22.92%) | 2903 (25.74%) | 724 (18.98%) |
| Not recorded | 6881 (66.77%) | 7305 (64.77%) | 2644 (69.32%) |
| Drinking status | |||
| Current | 148 (1.44%) | 135 (1.20%) | 55 (1.44%) |
| Past | 568 (5.51%) | 732 (6.49%) | 199 (5.22%) |
| Never | 2708 (26.28%) | 3106 (27.54%) | 916 (24.02%) |
| Not recorded | 6881 (66.77%) | 7305 (64.77%) | 2644 (69.32%) |
Values were expressed as mean (standard deviation) or medians (quartile interval) or n (%)
Abbreviations: NFG normal fasting glucose, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, FPG fasting plasma glucose, TG triglyceride, TC total cholesterol, HDL-C, high-density lipoprotein cholesterol, LDL-C, low-density lipoprotein cholesterol, TyG index triglyceride-glucose index, TyG-BMI triglyceride glucose-body mass index, ALT alanine aminotransferase, AST aspartate aminotransferase BUN blood urea nitrogen Cr creatinine
Fig. 3.
Violin chart showing baseline characteristics of TyG-BMI and age according to glucose status during follow-up
Evaluating the impact of TyG-BMI on the recovering to NFG or progressing to diabetes in prediabetes
The researchers assessed whether there was multicollinearity between TyG-BMI and other covariates when taking the recovery or progression of prediabetes as the dependent variable. The results were presented in Supplementary Tables 2 and 3. Weight and TC were excluded from subsequent models due to variance inflation factor exceeding 5. Additionally, the researchers generated Schoenfeld residual plots to examine the time-varying effects of TyG-BMI (Supplementary Figs. 1 and 2), and P-values for all correlations were higher than 0.05, indicating no violation of the proportional hazards assumption.
Three stepwise adjusted multivariate Cox regression models were used to explore the impact of TyG-BMI on prediabetes recovery/progression (Table 2), it can be observed that in all models, TyG-BMI showed a significant negative association with prediabetes recovering to NFG and a positive association with prediabetes progressing to diabetes [Model III: Prediabetes to NFG (HR): 0.90 (0.88–0.93); Prediabetes to diabetes (HR): 1.26 (1.21–1.31)].
Table 2.
Multivariate Cox regression analysis of the role of BMI, TyG index, TyG-BMI in assessing changes in glycemic status in patients with prediabetes
| HR (95%CI) | E-value | ||||
|---|---|---|---|---|---|
| Non-adjusted Model | Model I | Model II | Model III | ||
| Prediabetes to NFG | |||||
| TyG-BMI (per SD increase) | 0.80 (0.79, 0.82) | 0.84 (0.83, 0.86) | 0.86 (0.84, 0.88) | 0.90 (0.88, 0.93) | 1.46 |
| TyG-BMI (quartiles) | |||||
| Q1 | Ref | Ref | Ref | Ref | |
| Q2 | 0.81 (0.77, 0.85) | 0.90 (0.86, 0.95) | 0.92 (0.88, 0.97) | 0.97 (0.92, 1.02) | |
| Q3 | 0.67 (0.64, 0.71) | 0.78 (0.74, 0.82) | 0.80 (0.76, 0.85) | 0.87 (0.82, 0.93) | |
| Q4 | 0.59 (0.56, 0.62) | 0.66 (0.63, 0.70) | 0.70 (0.66, 0.74) | 0.82 (0.77, 0.89) | |
| P-trend | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 | |
| Prediabetes to Diabetes | |||||
| TyG-BMI (per SD increase) | 1.43 (1.39, 1.47) | 1.40 (1.36, 1.45) | 1.38 (1.34, 1.42) | 1.26 (1.21, 1.31) | 1.83 |
| TyG-BMI (quartiles) | |||||
| Q1 | Ref | Ref | Ref | Ref | |
| Q2 | 1.56 (1.40, 1.74) | 1.41 (1.26, 1.57) | 1.38 (1.23, 1.54) | 1.27 (1.12, 1.43) | |
| Q3 | 2.17 (1.95, 2.41) | 1.90 (1.71, 2.11) | 1.83 (1.64, 2.04) | 1.57 (1.39, 1.76) | |
| Q4 | 2.81 (2.54, 3.11) | 2.52 (2.27, 2.80) | 2.39 (2.15, 2.66) | 1.82 (1.61, 2.06) | |
| P-trend | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 | |
Model I adjusted for age, sex and height
Model II adjusted for age, sex, height, family history of diabetes, smoking status, drinking status, SBP, DBP
Model III adjusted for age, sex, height, family history of diabetes, smoking status, drinking status, SBP, DBP, FPG, TG ALT, BUN and Cr
Abbreviations: HR hazard ratios, CI confidence interval, other abbreviations as in Table 1
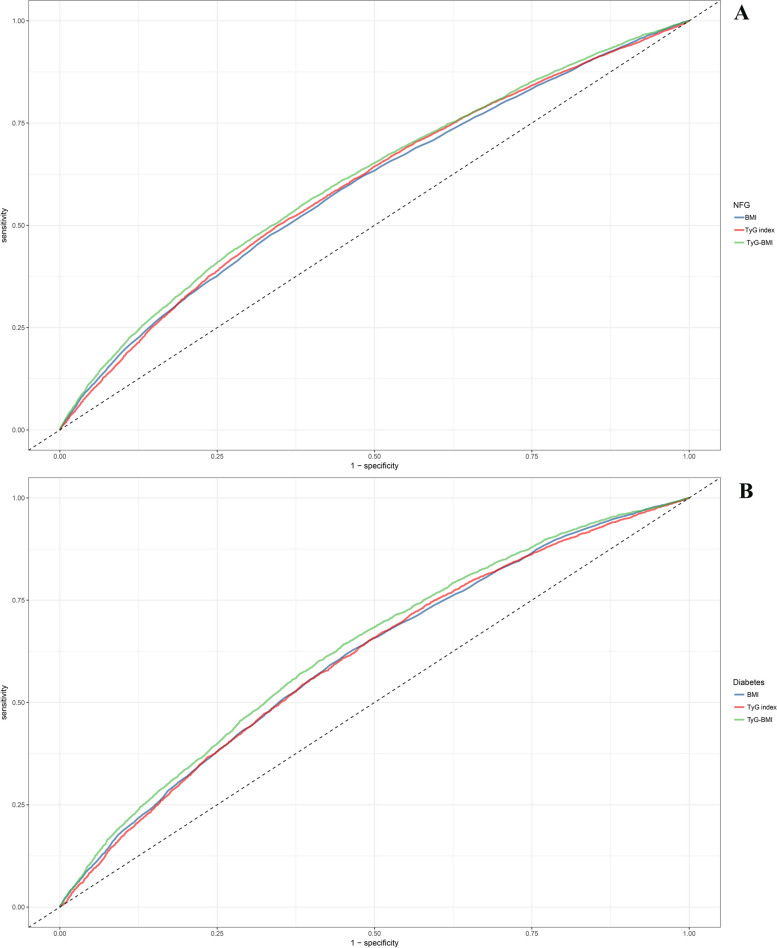
The researchers further visualized the dose–response relationship curve of TyG-BMI with prediabetes recovering to NFG/progressing to diabetes based on RCS. As shown in Fig. 4, after adjusting for covariates in Model III, TyG-BMI exhibited a linear negative correlation with prediabetes recovering to NFG (P-non-linearity = 0.362) and a nonlinear positive correlation with prediabetes progressing to diabetes (P-non-linearity = 0.007).
Fig. 4.
Apply the 4-knots RCS model to fit the dose–response relationship between TyG-BMI and recovery from prediabetes to NFG/progressing to diabetes
Sensitivity analysis
After transforming TyG-BMI as a categorical variable, the new analysis results showed that the negative association of TyG-BMI with prediabetes recovering to NFG gradually strengthened between quartiles (Q1 1 vs Q2 0.97 vs Q3 0.87 vs Q4 0.82), maintaining a negative trend (P-trend < 0.0001). In the association between TyG-BMI quartiles and prediabetes progressing to diabetes, the positive association between them gradually increased between quartiles (Q1 1 vs Q2 1.27 vs Q3 1.57 vs Q4 1.82), maintaining a positive trend (P-trend < 0.0001) (Table 2). When assessing the study population according to the prediabetes and diabetes diagnostic criteria published by the WHO, it can be observed similar results to the analysis conducted using the ADA criteria (Supplementary Table 4: Sensitivity-1). In the context of considering competing risks, the association of TyG-BMI with the recovery of prediabetes to NFG or progressing to diabetes remained consistent with the main analysis results (Supplementary Table 4: Sensitivity-2). When analyzing people without a family history of diabetes separately, the results were still similar to the ones reported above (Supplementary Table 4: Sensitivity-3). Furthermore, the researchers generated E-values to assess the sensitivity to unmeasured confounding (Table 2), and the results can be considered relatively robust for each SD increment. Finally, 3-knot and 5-knot RCS models were constructed, and the results were consistent with the findings from the 4-knot RCS, indicating a linear negative relationship of TyG-BMI with the recovery of prediabetes to NFG (Supplementary Figs. 3 and 4).
Subgroup analysis based on common population phenotypes
Regarding different sexes, ages, and BMIs, the researchers conducted subgroup analyses to explore whether there is specificity in the relationship of TyG-BMI with the recovery or progression of prediabetes within these common population phenotypes (Table 3). In these subgroups, it can be observed that BMI and sex did not produce significant interactions with TyG-BMI in relation to prediabetes progression/recovery. However, age showed significant interactions with TyG-BMI in both prediabetes progression and recovery. It's worth noting that in relatively younger populations (< 45 years old), the negative correlation of TyG-BMI with the recovery of prediabetes to NFG weakened, while the positive correlation with the progression of prediabetes to diabetes strengthened. In relatively older populations (≥ 45 years old), the negative correlation of TyG-BMI with the recovery of prediabetes to NFG strengthened, while the positive correlation with the progression of prediabetes to diabetes weakened. In summary, TyG-BMI appeared to be more suitable for evaluating the progression or recovery of prediabetes in younger populations.
Table 3.
Exploratory subgroup analysis of the role and differences of TyG-BMI in assessing changes in glycemic status in prediabetes patients
| HR per SD de/increase (95%CI) | ||
|---|---|---|
| Prediabetes to NFG | Prediabetes to Diabetes | |
| Sex | ||
| Male | 0.92 (0.89, 0.94) | 1.22 (1.17, 1.27) |
| Female | 0.91 (0.87, 0.95) | 1.27 (1.19, 1.35) |
| P-interaction | 0.7710 | 0.2870 |
| Age, years | ||
| < 45 | 0.94 (0.91, 0.97) | 1.36 (1.28, 1.43) |
| 45–59 | 0.87 (0.84, 0.91) | 1.17 (1.10, 1.24) |
| ≥ 60 | 0.87 (0.82, 0.92) | 1.16 (1.09, 1.23) |
| P-interaction | 0.0013 | < 0.0001 |
| BMI, kg/m2 | ||
| < 24 | 0.95 (0.90, 1.00) | 1.40 (1.24, 1.58) |
| 24–27.9 | 0.91 (0.86, 0.98) | 1.21 (1.10, 1.34) |
| ≥ 28 | 0.88 (0.81, 0.96) | 1.19 (1.08, 1.30) |
| P-interaction | 0.2858 | 0.0813 |
Comparing the predictive value of TyG-BMI and its individual components for the recovering to NFG or progressing to diabetes in prediabetes
After establishing the impact of TyG-BMI on the recovering to NFG or progressing to diabetes in prediabetes, the researchers conducted further assessments using ROC analysis to assess the predictive value of TyG-BMI and its constituent components. Detailed results from the ROC analysis were presented in Table 4, and they were visualized in Fig. 5. It is evident that TyG-BMI demonstrated a significantly higher predictive value for the recovering to NFG or progressing to diabetes in prediabetes compared to BMI and the TyG index [Prediabetes to NFG (AUC): TyG-BMI 0.61 vs TyG index 0.60 vs BMI 0.59; Prediabetes to diabetes (AUC): TyG-BMI 0.63 vs BMI 0.60 vs TyG index 0.60; all Delong P < 0.001]. Additionally, it is worth noting that, in terms of predictive threshold analysis, the thresholds for TyG-BMI and its constituent components for predicting the recovery of prediabetes to NFG (BMI 23.81, TyG index 8.68, TyG-BMI 214.68) were slightly lower than those for predicting progressing to diabetes (BMI 24.82, TyG index 8.79, TyG-BMI 220.27).
Table 4.
ROC analysis of the predictive value of BMI, TyG index, TyG-BMI on changes in glucose status during follow-up of prediabetes subjects
| AUC | 95%CI low | 95%CI upp | Best threshold | Specificity | Sensitivity | |
|---|---|---|---|---|---|---|
| Prediabetes to NFG | ||||||
| BMI* | 0.59 | 0.59 | 0.60 | 23.81 | 0.66 | 0.48 |
| TyG index* | 0.60 | 0.59 | 0.61 | 8.68 | 0.66 | 0.50 |
| TyG-BMI | 0.61 | 0.61 | 0.62 | 214.68 | 0.61 | 0.55 |
| Prediabetes to Diabetes | ||||||
| BMI* | 0.60 | 0.60 | 0.62 | 24.82 | 0.55 | 0.62 |
| TyG index* | 0.60 | 0.60 | 0.62 | 8.79 | 0.51 | 0.65 |
| TyG-BMI | 0.63 | 0.62 | 0.64 | 220.27 | 0.55 | 0.64 |
AUC area under the curve, other abbreviations as in Table 1
*P < 0.001, compare with TyG-BMI
Fig. 5.
ROC analysis shows the predictive value of TyG-BMI and its components for recovery from prediabetes to NFG/progressing to diabetes
Discussion
This second analysis of a Chinese healthcare cohort indicated that TyG-BMI was negatively correlated with the recovery of prediabetes to NFG and positively correlated with the progression of prediabetes to diabetes. Furthermore, in predicting the recovering to NFG or progressing to diabetes in prediabetes, TyG-BMI exhibited higher impact and predictive value compared to the TyG index and BMI.
Prediabetes, a high-risk state for diabetes, can lead to a range of long-term complications and seriously jeopardize the body's health [1–6, 45, 46]. In previous epidemiological investigations, many researchers have evaluated the role of TyG-BMI in the development of prediabetes, diabetes, and various chronic diseases or adverse outcomes [26–30, 47–54]. In summary, TyG-BMI is a reliable surrogate marker for IR [25], and an elevated TyG-BMI indicates decreased insulin sensitivity, thereby increasing the risk of diabetes and various other chronic diseases or adverse outcomes. In the current study, the researchers further validated the role of TyG-BMI in the development of diabetes, and the results showed that for every one SD increase in TyG-BMI, the diabetes risk increased by 23%. It is important to note that although previous research has made some progress in understanding the role of TyG-BMI in prediabetes and diabetes progression [26–30], it is still unclear how TyG-BMI affects the process of prediabetes recovering to NFG. To address this issue, the current study further analyzed the impact of TyG-BMI on the recovery of prediabetes, and the study results indicated a significant linear negative association between TyG-BMI and prediabetes recovery (P-non-linearity = 0.362). Subsequent sensitivity analyses further confirmed the stability of this finding. Additionally, in the current study, the researchers observed a significant interaction with age in the relationship between TyG-BMI and prediabetes recovery/progression. Specifically, this can be explained by a relatively higher risk of TyG-BMI-related prediabetes progressing to diabetes in younger individuals (< 45 years old), and conversely, a younger age is more favorable for prediabetes recovering to NFG in relation to TyG-BMI. The elevated risk of TyG-BMI-related diabetes in younger populations has also been documented in previous studies [26–29]. The underlying reasons for this 'peculiar' outcome may be linked to China's family planning policy, rapid societal development, and accelerated aging. Amidst these burgeoning societal factors, there is a conspicuous decline in the labor force in contemporary Chinese society [55, 56]. Young individuals, who are the primary contributors to the workforce, face substantial societal and psychological pressures compared to the past, which exacerbate their susceptibility to IR [57, 58]. Consequently, this contributes to an increased incidence risk of TyG-BMI-related diabetes. Conversely, the more pronounced advantage observed among young individuals in terms of the recovery of TyG-BMI-related prediabetes to NFG levels is likely primarily attributable to their higher β-cell recovery capacity [59, 60].
Several studies have previously reported on the use of TyG-BMI for predicting prediabetes and diabetes, and, interestingly, the outcomes of these published studies have shown remarkable consistency, indicating that TyG-BMI outperformed both the standalone TyG index and BMI in the prediction of prediabetes and diabetes [26–29]. These congruent findings have been reaffirmed in the current investigation [Prediabetes to diabetes (AUC): TyG-BMI 0.63 vs BMI 0.60 vs TyG index 0.60; All Delong P < 0.001]. Furthermore, the researchers conducted an additional assessment to evaluate the predictive value of TyG-BMI and its constituent components for prediabetes recovery; as anticipated, TyG-BMI demonstrated substantial predictive utility in the context of prediabetes recovery, surpassing the predictive performance of the individual TyG index and BMI. These findings further underscored the significant role of TyG-BMI in the prediction of glycemic metabolic disorders. In addition, within the current study, the researchers also assessed the predictive thresholds of TyG-BMI for prediabetes recovery and progression. The results showed that the threshold for predicting recovery of prediabetes was 214.68, while the threshold for predicting progression of prediabetes was 220.27. In contrast, the TyG-BMI prediction threshold for predicting recovery of prediabetes was lower, suggesting that stricter intervention strategies and preventive criteria may be required for prediabetes patients to recover to NFG. To the best of our knowledge, the predictive value of TyG-BMI and its constituent components for the disease trajectory of prediabetes has not been previously reported. In light of the findings from the current study, the researchers believe that TyG-BMI may warrant greater attention in the risk assessment and prediction of glycemic-related disorders.
While research on the recovery of prediabetes is relatively scarce, the findings from the current study, based on cumulative incidence functions, along with the analysis of incidence rates in other ethnic populations [61, 62], suggested that the prediabetic state represents a valuable opportunity, because this phase holds immense potential for recovering to NFG. Moreover, the recovery of prediabetes is expected to significantly reduce the risk of diabetes and various chronic complications [7–17]. Therefore, the benefits of prediabetes recovering to NFG cannot be overstated, and any preventive or intervention strategies that facilitate this unique process may hold substantial clinical significance. The findings from the current study are anticipated to provide clinical practitioners and fellow researchers with valuable insights and assistance in several key areas: (i) In the domain of diabetes prevention, the early evaluation of TyG-BMI among individuals with prediabetes may offer a robust means of identifying the risk of diabetes onset. (ii) For early intervention in prediabetes, monitoring TyG-BMI and maintaining it below 216.68 could potentially expedite the recovery of prediabetes to NFG or increase the probability of recovering to NFG. (iii) In the construction of predictive models for prediabetes recovery, the inclusion of TyG-BMI may substantially enhance the predictive efficiency of these models. (iv) Given that the current study concurrently assessed both the recovery and progression of prediabetes, the results consistently highlighted TyG-BMI as a superior predictive marker compared to the standalone TyG index and BMI. These findings suggested that TyG-BMI could serve as an excellent novel indicator for assessing and screening glycemic-related disorders, and if this can be validated in more studies then it could provide a great boost to reducing the risk of glucose metabolism-related diseases. (v) Although the current study did not explore the mechanisms by which TyG-BMI mediates prediabetes recovery, it is plausible that the resolution of IR plays a pivotal role in this process, which is supported by the fact that TyG-BMI is utilized as a surrogate marker for IR [25], and intervention studies have provided evidence that the improvement of β-cell function is a key factor in prediabetes recovery [22]. Building upon these results and analyses, further assessing the dynamic changes in TyG-BMI in future research will hold significant value in understanding its role in the recovery of prediabetes to NFG, providing robust evidence for clinical validation of mechanisms, and facilitating the development of subsequent preventive strategies.
Study strengths and limitations
The foremost strength of this study lies in its first revelation of the role and predictive value of TyG-BMI in the recovery of prediabetes to NFG, and the core findings of this research remain robust even under rigorous sensitivity analyses. Furthermore, the large sample size further enhances the reliability of these results.
Several limitations should be duly acknowledged in summarizing as follows: (i) The most prominent limitation may stem from the diagnostic criteria used for study outcomes. As the study population consisted of individuals undergoing routine health screenings at Rich Healthcare Group, only a few participants underwent oral glucose tolerance tests. The present study, under existing circumstances, adopted a method frequently employed in prior research, defining study endpoints solely based on follow-up data of FPG and self-reported diabetes diagnosis [18], potentially leading to an underestimation of the incidence rates of prediabetes and diabetes. Nevertheless, it is noteworthy that the present study consistently yielded concordant results in the main analysis and sensitivity analyses, even at lower incidence rates. Thus, one might argue that the results of the current study are relatively reliable from a reverse perspective. (ii) Given that most participants in the study were of Chinese heritage, caution is advised when extrapolating these results to different ethnic populations. (iii) Following collinearity screening, although AST, HDL-C, and LDL-C all met the model adjustment requirements, their substantial missing values (exceeding 39%) limited the value of imputation and potentially impacted data accuracy [63]. Consequently, to avoid the inability to reflect the authenticity of real-world research due to data missingness, the current research did not include these covariates for adjustment in the multivariable models. As supplementary analysis, this study regards the above-reported variables as unmeasured confounders in the multivariable regression, and further E-value analysis indicated that even in the presence of unmeasured confounding, the results of the current study remained relatively robust. (iv) The current study lacked repeated measurements of TyG-BMI, preventing further exploration of the critical role of IR in the recovery of prediabetes. (v) The follow-up duration in the current study was relatively short, necessitating further research to validate the impact of TyG-BMI on medium- to long-term recovery of prediabetes.
Conclusion
This large-scale cohort study revealed that the combination of the BMI and TyG index significantly influences the recovery of prediabetic states to normal blood glucose levels, demonstrating substantial predictive value. From the perspective of prediabetes intervention, maintaining TyG-BMI within the range of 214.68 is of paramount significance.
Supplementary Information
Acknowledgements
We would like to thank Dr. Chen Ying and his team members for their great efforts in data collection and organization.
Abbreviations
- TyG
Triglyceride-glucose
- BMI
Body mass index
- NFG
Normal fasting glucose
- ADA
American diabetes association
- ROC
Receiver operating characteristic
- Cr
Creatinine
- BUN
Blood urea nitrogen
- SD
Standard deviation
- VIF
Variance inflation factor
- RCS
Restricted cubic splines
- AUC
Area under the curve
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- HDL-C
High-density lipoprotein cholesterol
- TC
Total cholesterol
- TG
Triglyceride
- LDL-C
Low-density lipoprotein cholesterol
- FPG
Fasting plasma glucose
- BP
Blood pressure
- HR
Hazard ratio
- CI
Confidence interval
- IR
Insulin resistance
Authors’ contributions
YZ and GT-S: conceptualization; Supervision; and Project administration. YZ and GT-S: Methodology. HY-Y, MB-K and JJ-Q: writing-original draft preparation. YZ, GT-S, SM-H and CH-Y: writing-reviewing and editing. HY-Y, JJ-Q and MB-K: Software. HY-Y, JJ-Q, CH-Y, SM-H and MB-K: formal analysis. HY-Y, JJ-Q, CH-Y, SM-H and MB-K: data curation and validation. All authors read and approved the final manuscript.
Funding
This work was supported by Natural Science Foundation of Jiangxi Province [No. 20232BAB216004 to YZ]. Natural Science Foundation of Jiangxi Province,20232BAB216004
Availability of data and materials
The data set supporting the results of this study has been uploaded to Dryad database (https://doi.org/10.5061/dryad.ft8750v).
Declarations
Ethics approval and consent to participate
As the current study is a post-hoc analysis, a new research protocol has been submitted and approved by the Ethics Committee of Jiangxi Provincial People's Hospital (Approval No. 2021–067). Additionally, considering that the dataset has been anonymized, the institutional ethics committee waived the requirement for informed consent from the participants. The entire post-hoc analysis process strictly adhered to the STROBE reporting guidelines, in accordance with the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hongyi Yang, Maobin Kuang, and Jiajun Qiu have contributed equally to this work.
Contributor Information
Guotai Sheng, Email: tgs200509@163.com.
Yang Zou, Email: jxyxyzy@163.com.
References
- 1.Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–2290. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beulens J, Rutters F, Rydén L, Schnell O, Mellbin L, Hart HE, et al. Risk and management of pre-diabetes. Eur J Prev Cardiol. 2019;26:47–54. doi: 10.1177/2047487319880041. [DOI] [PubMed] [Google Scholar]
- 3.Cai X, Zhang Y, Li M, Wu JH, Mai L, Li J, et al. Association between prediabetes and risk of all cause mortality and cardiovascular disease: updated meta-analysis. BMJ. 2020;370:m2297. doi: 10.1136/bmj.m2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Echouffo-Tcheugui JB, Selvin E. Prediabetes and what it means: the epidemiological evidence. Annu Rev Public Health. 2021;42:59–77. doi: 10.1146/annurev-publhealth-090419-102644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindsay C, Shieh A. Prediabetes and skeletal health. Curr Opin Endocrinol Diabetes Obes. 2023;30:200–205. doi: 10.1097/MED.0000000000000812. [DOI] [PubMed] [Google Scholar]
- 6.Roriz-Filho JS, Sá-Roriz TM, Rosset I, Camozzato AL, Santos AC , Chaves ML, et al. (Pre)diabetes, brain aging, and cognition. Biochim Biophys Acta. 2009;1792:432–43. doi: 10.1016/j.bbadis.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Chen Y, Zhang P, Wang J, Gong Q, An Y, Qian X, et al. Associations of progression to diabetes and regression to normal glucose tolerance with development of cardiovascular and microvascular disease among people with impaired glucose tolerance: a secondary analysis of the 30 year Da Qing Diabetes Prevention Outcome Study. Diabetologia. 2021;64:1279–1287. doi: 10.1007/s00125-021-05401-x. [DOI] [PubMed] [Google Scholar]
- 8.Vistisen D, Kivimäki M, Perreault L, Hulman A, Witte DR, Brunner EJ, et al. Reversion from prediabetes to normoglycaemia and risk of cardiovascular disease and mortality: the Whitehall II cohort study. Diabetologia. 2019;62:1385–1390. doi: 10.1007/s00125-019-4895-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pratte KA, Johnson A, Beals J, Bullock A, Manson SM, Jiang L, et al. Regression to normal glucose regulation in american indians and alaska natives of a diabetes prevention program. Diabetes Care. 2019;42:1209–1216. doi: 10.2337/dc18-1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perreault L, Pan Q, Schroeder EB, Kalyani RR, Bray GA, Dagogo-Jack S, et al. Regression From Prediabetes to Normal Glucose Regulation and Prevalence of Microvascular Disease in the Diabetes Prevention Program Outcomes Study (DPPOS) Diabetes Care. 2019;42:1809–1815. doi: 10.2337/dc19-0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE, et al. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the diabetes prevention program outcomes study. Lancet. 2012;379:2243–2251. doi: 10.1016/S0140-6736(12)60525-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perreault L, Temprosa M, Mather KJ, Horton E, Kitabchi A, Larkin M, et al. Regression from prediabetes to normal glucose regulation is associated with reduction in cardiovascular risk: results from the diabetes prevention program outcomes study. Diabetes Care. 2014;37:2622–2631. doi: 10.2337/dc14-0656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amer OE, Sabico S, Alfawaz HA, Aljohani N, Hussain SD, Alnaami AM, et al. Reversal of prediabetes in saudi adults: results from an 18 month lifestyle intervention. Nutrients. 2020;12:804. doi: 10.3390/nu12030804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramachandran A, Snehalatha C, Mary S, Selvam S, Kumar CK, Seeli AC, et al. Pioglitazone does not enhance the effectiveness of lifestyle modification in preventing conversion of impaired glucose tolerance to diabetes in Asian Indians: results of the Indian diabetes prevention programme-2 (IDPP-2) Diabetologia. 2009;52:1019–1026. doi: 10.1007/s00125-009-1315-x. [DOI] [PubMed] [Google Scholar]
- 15.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, et al. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet. 2002;359:2072–2077. doi: 10.1016/S0140-6736(02)08905-5. [DOI] [PubMed] [Google Scholar]
- 17.Eriksson KF, Lindgärde F. Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise. The 6-year Malmö feasibility study. Diabetologia. 1991;34:8918. doi: 10.1007/BF00400196. [DOI] [PubMed] [Google Scholar]
- 18.Rooney MR, Fang M, Ogurtsova K, Ozkan B, Echouffo-Tcheugui JB, Boyko EJ, et al. Global prevalence of prediabetes. Diabetes Care. 2023;46:1388–1394. doi: 10.2337/dc22-2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sallar A, Dagogo-Jack S. Regression from prediabetes to normal glucose regulation: State of the science. Exp Biol Med (Maywood) 2020;245:889–896. doi: 10.1177/1535370220915644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bi Y, Zhu D, Jing Y, Hu Y, Feng W, Shen S, et al. Decreased beta cell function and insulin sensitivity contributed to increasing fasting glucose in Chinese. Acta Diabetol. 2012;49(Suppl 1):S51–S58. doi: 10.1007/s00592-010-0194-4. [DOI] [PubMed] [Google Scholar]
- 21.Magkos F, Lee MH, Lim M, Cook AR, Chhay V, Loh TP, et al. Dynamic assessment of insulin secretion and insulin resistance in Asians with prediabetes. Metabolism. 2022;128:154957. doi: 10.1016/j.metabol.2021.154957. [DOI] [PubMed] [Google Scholar]
- 22.Snehalatha C, Mary S, Selvam S, Sathish Kumar CK, Shetty SB, Nanditha A, et al. Changes in insulin secretion and insulin sensitivity in relation to the glycemic outcomes in subjects with impaired glucose tolerance in the Indian diabetes prevention programme-1 (IDPP-1) Diabetes Care. 2009;32:1796–1801. doi: 10.2337/dc09-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237:E214–E223. doi: 10.1152/ajpendo.1979.237.3.E214. [DOI] [PubMed] [Google Scholar]
- 24.Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294:E15–26. doi: 10.1152/ajpendo.00645.2007. [DOI] [PubMed] [Google Scholar]
- 25.Er LK, Wu S, Chou HH, Hsu LA, Teng MS, Sun YC, et al. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS ONE. 2016;11:e0149731. doi: 10.1371/journal.pone.0149731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiang C, Yang R, Kuang M, Yu M, Zhong M, Zou Y. Triglyceride glucose-body mass index in identifying high-risk groups of pre-diabetes. Lipids Health Dis. 2021;20:161. doi: 10.1186/s12944-021-01594-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Han Y, Hu H, Li Q, Deng Z, Liu D. Triglyceride glucose-body mass index and the risk of progression to diabetes from prediabetes: A 5-year cohort study in Chinese adults. Front Public Health. 2023;11:1028461. doi: 10.3389/fpubh.2023.1028461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang X, Liu J, Cheng Z, Zhong Y, Chen X, Song W. Triglyceride glucose-body mass index and the risk of diabetes: a general population-based cohort study. Lipids Health Dis. 2021;20:99. doi: 10.1186/s12944-021-01532-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Song B, Zhao X, Yao T, Lu W, Zhang H, Liu T, et al. Triglyceride Glucose-Body Mass Index and Risk of Incident Type 2 Diabetes Mellitus in Japanese People With Normal Glycemic Level: A Population-Based Longitudinal Cohort Study. Front Endocrinol (Lausanne) 2022;13:907973. doi: 10.3389/fendo.2022.907973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuang M, Yang R, Huang X, Wang C, Sheng G, Xie G, et al. Assessing temporal differences in the predictive power of baseline TyG-related parameters for future diabetes: an analysis using time-dependent receiver operating characteristics. J Transl Med. 2023;21:299. doi: 10.1186/s12967-023-04159-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen Y, Zhang XP, Yuan J, Cai B, Wang XL, Wu XL, et al. Association of body mass index and age with incident diabetes in Chinese adults: a population-based cohort study. BMJ Open. 2018;8:e021768. doi: 10.1136/bmjopen-2018-021768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen Y, et al. Data from: Association of body mass index and age withincident diabetes in Chinese adults: a population-based cohort study Dryad. Dataset. 2018 doi: 10.5061/dryad.ft8750v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American Diabetes Association 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018;41:S13–S27. doi: 10.2337/dc18-S002. [DOI] [PubMed] [Google Scholar]
- 34.Gharavi E, Gu A, Zheng G, Smith JP, Cho HJ, Zhang A, et al. Embeddings of genomic region sets capture rich biological associations in lower dimensions. Bioinformatics. 2021;37:4299–4306. doi: 10.1093/bioinformatics/btab439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mugler EM, Tate MC, Livescu K, Templer JW, Goldrick MA, Slutzky MW. Differential representation of articulatory gestures and phonemes in precentral and inferior frontal gyri. J Neurosci. 2018;38:9803–9813. doi: 10.1523/JNEUROSCI.1206-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fitchett EJA, Seale AC, Vergnano S, Sharland M, Heath PT, Saha SK, et al. Strengthening the Reporting of Observational Studies in Epidemiology for Newborn Infection (STROBE-NI): an extension of the STROBE statement for neonatal infection research. Lancet Infect Dis. 2016;16:e202–e213. doi: 10.1016/S1473-3099(16)30082-2. [DOI] [PubMed] [Google Scholar]
- 37.Wax Y. Collinearity diagnosis for a relative risk regression analysis: an application to assessment of diet-cancer relationship in epidemiological studies. Stat Med. 1992;11:1273–1287. doi: 10.1002/sim.4780111003. [DOI] [PubMed] [Google Scholar]
- 38.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 39.Ramezankhani A, Habibi-Moeini AS, Zadeh SST, Azizi F, Hadaegh F. Effect of family history of diabetes and obesity status on lifetime risk of type 2 diabetes in the Iranian population. J Glob Health. 2022;12:04068. doi: 10.7189/jogh.12.04068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hu X, Yu W, Yang L, Pan W, Xu K, Chen X, et al. First-degree family history of diabetes is associated with nonalcoholic fatty liver disease independent of glucose metabolic status. J Diabetes Complications. 2022;36:108083. doi: 10.1016/j.jdiacomp.2021.108083. [DOI] [PubMed] [Google Scholar]
- 41.VanderWeele TJ, Ding P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann Intern Med. 2017;167:268–274. doi: 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- 42.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. doi: 10.2307/2531595. [DOI] [PubMed] [Google Scholar]
- 43.World Health Day 2012 focuses on ageing and health. East Mediterr Health J. 2012;18:303. Arabic, English. [PubMed]
- 44.Zhou BF. Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. [PubMed] [Google Scholar]
- 45.Schmidt AM. Highlighting Diabetes Mellitus: The Epidemic Continues. Arterioscler Thromb Vasc Biol. 2018;38:e1–e8. doi: 10.1161/ATVBAHA.117.310221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5:423–430. doi: 10.1016/S2213-8587(17)30097-9. [DOI] [PubMed] [Google Scholar]
- 47.Nikbakht HR, Najafi F, Shakiba E, Darbandi M, Navabi J, Pasdar Y. Triglyceride glucose-body mass index and hypertension risk in iranian adults: a population-based study. BMC Endocr Disord. 2023;23:156. 10.1186/s12902-023-01411-5. [DOI] [PMC free article] [PubMed]
- 48.Wen Z, Li Y, Xu L, Yue C, Wang Q, Chen R, et al. Triglyceride Glucose-Body Mass Index Is a Reliable Indicator of Bone Mineral Density and Risk of Osteoporotic Fracture in Middle-Aged and Elderly Nondiabetic Chinese Individuals. J Clin Med. 2022;11:5694. doi: 10.3390/jcm11195694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang R, Dai L, Zhong Y, Xie G. Usefulness of the triglyceride glucose-body mass index in evaluating nonalcoholic fatty liver disease: insights from a general population. Lipids Health Dis. 2021;20:77. doi: 10.1186/s12944-021-01506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huo RR, Zhai L, Liao Q, You XM. Changes in the triglyceride glucose-body mass index estimate the risk of stroke in middle-aged and older Chinese adults: a nationwide prospective cohort study. Cardiovasc Diabetol. 2023;22:254. doi: 10.1186/s12933-023-01983-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cheng Y, Fang Z, Zhang X, Wen Y, Lu J, He S, et al. Association between triglyceride glucose-body mass index and cardiovascular outcomes in patients undergoing percutaneous coronary intervention: a retrospective study. Cardiovasc Diabetol. 2023;22:75. doi: 10.1186/s12933-023-01794-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khamseh ME, Malek M, Abbasi R, Taheri H, Lahouti M, Alaei-Shahmiri F. Triglyceride Glucose Index and Related Parameters (Triglyceride Glucose-Body Mass Index and Triglyceride Glucose-Waist Circumference) Identify Nonalcoholic Fatty Liver and Liver Fibrosis in Individuals with Overweight/Obesity. Metab Syndr Relat Disord. 2021;19:167–173. doi: 10.1089/met.2020.0109. [DOI] [PubMed] [Google Scholar]
- 53.Park PG, Pyo JY, Ahn SS, Song JJ, Park YB, Huh JH, et al. New index using triglyceride glucose-body mass index for predicting mortality in patients with antineutrophil cytoplasmic antibody-associated vasculitis. Front Med (Lausanne) 2023;10:1168016. doi: 10.3389/fmed.2023.1168016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Du Z, Xing L, Lin M, Sun Y. Estimate of prevalent ischemic stroke from triglyceride glucose-body mass index in the general population. BMC Cardiovasc Disord. 2020;20:483. doi: 10.1186/s12872-020-01768-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang F. Can China afford to continue its one-child policy?.Asia Pacific Issues, 2005, 17. http://hdl.handle.net/10125/3796. Accessed 10 Nov 2023.
- 56.Eriksson M, Ng N. Changes in access to structural social capital and its influence on self-rated health over time for middle-aged men and women: a longitudinal study from northern Sweden. Soc Sci Med. 2015;130:250–258. doi: 10.1016/j.socscimed.2015.02.029. [DOI] [PubMed] [Google Scholar]
- 57.Sanghez V, Razzoli M, Carobbio S, Campbell M, McCallum J, Cero C, et al. Psychosocial stress induces hyperphagia and exacerbates diet-induced insulin resistance and the manifestations of the Metabolic Syndrome. Psychoneuroendocrinology. 2013;38:2933–2942. doi: 10.1016/j.psyneuen.2013.07.022. [DOI] [PubMed] [Google Scholar]
- 58.Motoyama S, Yamada H, Yamamoto K, Wakana N, Terada K, Kikai M, et al. Social Stress Increases Vulnerability to High-Fat Diet-Induced Insulin Resistance by Enhancing Neutrophil Elastase Activity in Adipose Tissue. Cells. 2020;9:996. doi: 10.3390/cells9040996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Helman A, Avrahami D, Klochendler A, Glaser B, Kaestner KH, Ben-Porath I, et al. Effects of ageing and senescence on pancreatic β-cell function. Diabetes Obes Metab. 2016;18(Suppl 1):58–62. doi: 10.1111/dom.12719. [DOI] [PubMed] [Google Scholar]
- 60.Suleiman M, Marselli L, Cnop M, Eizirik DL, De Luca C, Femia FR, et al. The Role of Beta Cell Recovery in Type 2 Diabetes Remission. Int J Mol Sci. 2022;23:7435. doi: 10.3390/ijms23137435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alizadeh Z, Baradaran HR, Kohansal K, Hadaegh F, Azizi F, Khalili D. Are the determinants of the progression to type 2 diabetes and regression to normoglycemia in the populations with pre-diabetes the same? Front Endocrinol (Lausanne) 2022;13:1041808. doi: 10.3389/fendo.2022.1041808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mehreen TS, Kamalesh R, Pandiyan D, Kumar DS, Anjana RM, Mohan V, et al. Incidence and Predictors of Dysglycemia and Regression to Normoglycemia in Indian Adolescents and Young Adults: 10-Year Follow-Up of the ORANGE Study. Diabetes Technol Ther. 2020;22:875–882. doi: 10.1089/dia.2020.0109. [DOI] [PubMed] [Google Scholar]
- 63.Samad MD, Abrar S, Diawara N. Missing Value Estimation using Clustering and Deep Learning within Multiple Imputation Framework. Knowl Based Syst. 2022;249:108968. doi: 10.1016/j.knosys.2022.108968. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data set supporting the results of this study has been uploaded to Dryad database (https://doi.org/10.5061/dryad.ft8750v).