Abstract
Background:
Osteochondral allograft transplantation (OCAT) allows the restoration of femoral condyle osteochondritis dissecans (OCD) lesions using an osteochondral unit. When OCD lesions are irreparable, or treatments have failed, OCAT is an appropriate approach for revision or salvage surgery. Based on its relative availability, cost-effectiveness, lack of donor site morbidity, and advances in preservation methods, OCAT is also an attractive option for primary surgical treatment for femoral condyle OCD.
Hypothesis:
OCAT for large femoral condyle OCD lesions would be highly successful (>90%) based on significant improvements in knee pain and function, with no significant differences between primary and salvage procedure outcomes.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients were enrolled into a registry for assessing outcomes after OCAT. Those patients who underwent OCAT for femoral condyle OCD and had a minimum of 2-year follow-up were included. Reoperations, treatment failures, and patient-reported outcomes were compared between primary and salvage OCAT cohorts.
Results:
A total of 22 consecutive patients were included for analysis, with none lost to the 2-year follow-up (mean, 40.3 months; range, 24-82 months). OCD lesions of the medial femoral condyle (n = 17), lateral femoral condyle (n = 4), or both condyles (n = 1) were analyzed. The mean patient age was 25.3 years (range, 12-50 years), and the mean body mass index was 25.2 kg/m2 (range, 17-42 kg/m2). No statistically significant differences were observed between the primary (n = 11) and salvage (n = 11) OCAT cohorts in patient and surgical characteristics. Also, 91% of patients had successful outcomes at a mean of >3 years after OCAT with 1 revision in the primary OCAT cohort and 1 conversion to total knee arthroplasty in the salvage OCAT cohort. For both primary and salvage OCATs, patient-reported measures of pain and function significantly improved at the 1-year and final follow-up, and >90% of patients reported that they were satisfied and would choose OCAT again for treatment.
Conclusion:
Based on the low treatment failure rates in conjunction with statistically significant and clinically meaningful improvements in patient-reported outcomes, OCAT can be considered an appropriate option for both primary and salvage surgical treatment in patients with irreparable OCD lesions of the femoral condyles.
Keywords: cartilage, knee, osteochondral allograft transplantation, osteochondritis dissecans
Osteochondritis dissecans (OCD) is an osteochondral disorder most commonly diagnosed in patients between 12 and 19 years of age.3,14 The incidence is highest in men, with the femoral condyles being most affected, such that patients typically present due to knee pain, effusion, and/or mechanical symptoms. Depending on the extent and severity of symptoms, in conjunction with diagnostic imaging findings, management for femoral condylar OCD may be nonsurgical or surgical. Nonsurgical management consisting of activity restrictions, orthotics, and physical therapy may be initially indicated but can be associated with high rates of failure to relieve symptoms as well as early onset osteoarthritis, particularly in patients with unstable lesions. 25 Surgical management can include a wide array of procedures, including retroarticular drilling, bone grafting, marrow-stimulation procedures, osteochondral fixation, offloading osteotomy, autologous chondrocyte implantation, osteochondral autograft transfer, or osteochondral allograft (OCA) transplantation (OCAT).8,21,30
While fixation to stabilize and repair viable OCD lesions is preferable, when possible, OCD cartilage is often pathologic, and subchondral bone is often necrotic and insubstantial. 3 Other surgical treatment options can be considered, but each has significant limitations. Osteochondral autograft transfer is often not indicated based on lesion size, location, extent, and/or severity.10,16,21 Marrow-stimulation procedures, retroarticular drilling, and autologous chondrocyte implantation have reported failure rates as high as 33%.19,20,34 For these techniques, failure mechanisms are typically related to poor articular cartilage repair tissue quality and/or poor quality subchondral bone. 17 OCAT addresses these limitations by allowing anatomic restoration of femoral condyle OCD lesions using an osteochondral unit consisting of viable hyaline cartilage with an intact cartilage-bone interface and structurally intact subchondral bone. When OCD lesions are irreparable or primary treatments have failed, OCAT has been reported to be an appropriate approach for revision surgery, even when performed as a salvage procedure.5,7,9,15,24,31 In conjunction with its relative availability, cost-effectiveness, and lack of donor site morbidity, recent advances in tissue-preservation methods, surgical techniques, and patient management strategies make OCAT an attractive option for primary surgical treatment for femoral condyle OCD.6,22,23,26–29 In general, previous studies have reported higher success rates for primary versus salvage OCAT for the treatment of femoral OCD.7,9,24 However, to date, the authors are not aware of any prospective studies directly comparing salvage versus primary OCAT for the treatment of femoral condylar OCD.
The present study aimed to prospectively assess outcomes for patients undergoing OCAT for femoral condylar OCD based on patient-reported outcome measures for pain and function, as well as reoperation and treatment failure rates, and compare primary versus salvage OCAT treatment. Based on recent advances in allograft tissue preservation, transplantation techniques, and patient management strategies associated with reduced treatment failure rates,22,23,27-29 this study was designed to test the hypothesis that OCAT for large femoral condyle OCD lesions would be highly successful (>90%) based on significant improvements in knee pain and function, with no significant differences between primary and salvage procedure outcomes.
Methods
The study protocol received institutional review board approval and included participants who provided written informed consent. Patients were prospectively enrolled into a dedicated registry established to follow OCAT outcomes. All OCAs transplanted for this study were obtained from an American Association of Tissue Banks–accredited source (MTF Biologics), preserved for up to 56 days after recovery using a commercially available preservation method (Missouri Osteochondral Preservation System), and used in conformance with the United States Food and Drug Administration classification of a human cell and tissue product under section 361 of the Public Health Services Act. 29
Study Patients
Patients were identified from those enrolled in the registry between January 1, 2016, and December 31, 2021, who underwent OCAT for ≥1 large (>2 cm2) OCD lesions involving 1 or both femoral condyles. Additional inclusion criteria were as follows:
Failed nonsurgical and/or surgical treatments for the primary problem
Absence of global knee osteoarthritis or degenerative knee osteoarthritis in any compartment
Absence of infectious, inflammatory, or immune-mediated arthritides
Intact knee ligament stability or stability/ligament reconstruction achieved concurrently with OCAT
Neutral limb alignment or neutral limb alignment achieved concurrently with OCAT by realignment osteotomy
Willingness and ability to comply with postoperative weightbearing restrictions and rehabilitation
Patients were categorized into 2 study cohorts based on previous OCD treatments, as follows:
Primary OCAT: OCAT performed for femoral condyle OCD as the first definitive surgical treatment attempt (ie, only nonsurgical management with or without diagnostic arthroscopy or minor arthroscopic procedure (ie, chondroplasty performed previously)
Salvage OCAT: OCAT performed for femoral condyle OCD and at least 1 previous major surgical treatment attempt (ie, retroarticular drilling, bone grafting, marrow-stimulation procedure, osteochondral fixation, offloading osteotomy, autologous chondrocyte implantation procedure, osteochondral autograft transfer, and/or OCAT)
Surgical Procedures
All OCATs were performed using press-fit cylindrical (plug) or custom-cut patient-specific shell OCAs to resurface the entire portion of the femoral condyle affected by the OCD, as previously described26,27 (Figures 1 and 2). Once the OCA was configured to match the recipient bed, 2.0-mm diameter subchondral drill holes were created in the base of the recipient socket for marrow stimulation and in the OCA bone to provide channels for cellular repopulation and revascularization of the allograft bone. The donor bone was then thoroughly irrigated with 1 to 1.5 L of isotonic saline to remove residual donor marrow elements and saturated with autogenous bone marrow aspirate concentrate (BMAC; Angel System; Arthrex) immediately before implantation. In cases requiring resection of recipient bone to a depth greater than the desired 7 to 9 mm to reach viable, bleeding bone, a Reamer Irrigator Aspirator (RIA; DePuy Synthes) bone graft obtained from the ipsilateral femur was placed into the defect before OCA implantation. 32 Cylindrical OCAs were press-fit into the recipient socket. Shell OCAs were stabilized with bioabsorbable nails (ConMed).
Figure 1.
Intraoperative images demonstrating (A) a large OCD lesion on the lateral femoral condyle, (B) cylindrical plug OCA created from donor lateral femoral condyle with inset showing a deep portion of the allograft with subchondral drill holes after thorough irrigation with isotonic saline and saturation with autogenous BMAC, and (C) OCA positioned over prepared recipient socket immediately before transplantation. BMAC, bone marrow aspirate concentrate; OCA, osteochondral allograft; OCD, osteochondritis dissecans.
Figure 2.
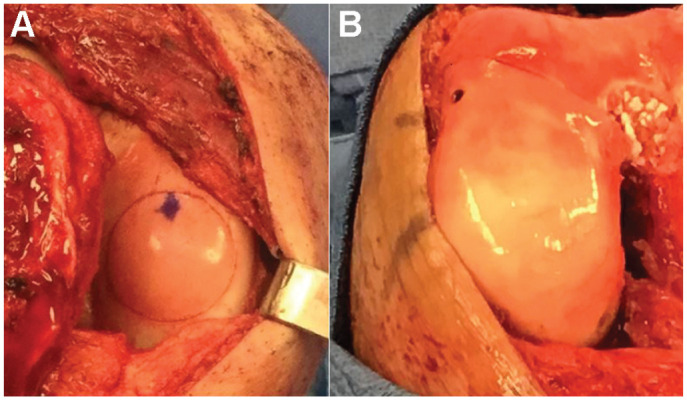
Intraoperative images demonstrating (A) a 30 mm-diameter press-fit cylindrical (plug) OCA transplanted into the medial femoral condyle of a patient with OCD in the right knee. (B) a large custom-cut shell OCA transplanted and stabilized with bioabsorbable nails into the lateral femoral condyle of a patient with OCD in the right knee. OCA, osteochondral allograft; OCD, osteochondritis dissecans.
If relevant comorbidities were noted in the affected knee, such as lower extremity malalignment or ligament-related instability, these were addressed accordingly at the time of OCAT (eg, autograft or allograft ligament reconstruction, distal femoral osteotomy, high tibial osteotomy). Osteotomy planning was performed using commercially available software (mediCAD) to determine the optimal location and the degree of correction required to achieve the desired limb alignment.
The viable chondrocyte density (VCD) of OCAs at the time of OCAT was determined when possible, based on the patient’s informed consent and nonimplanted donor tissue availability, as previously described. 28 Briefly, the number of viable chondrocytes based on Calcein-AM staining was counted for 6 tissue sections and divided by the tissue area (in mm2) to determine the VCD for each OCA assessed; then, the %VCD was calculated using the following formula: (VCD of donor OCA/VCD at mean time of recovery) ×100.28,29
Rehabilitation Protocol
Each patient received procedure-specific postoperative rehabilitation instructions based on the location and size of the grafts transplanted.6,22,23 In general, patients underwent 6 to 8 weeks of nonweightbearing postoperatively. Range of motion exercises and formal physical therapy were initiated within the first 2 weeks to prevent the risk of arthrofibrosis. Physical therapists at our institution attended pre- and postoperative clinic visits, provided inpatient therapy, and coordinated outpatient therapy. Follow-up appointments were scheduled for 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and then annually, with standardized radiographic imaging ordered for each appointment after the 2-week postoperative visit.
Outcome Measures
Patient electronic medical records were used to determine descriptive data, operative data, postoperative complications, and reoperations. Patient-reported outcomes included the Patient-Reported Outcomes Measurement Information System (PROMIS) Physical Function and Mobility domains, the International Knee Documentation Committee (IKDC) form, the Single Assessment Numeric Evaluation, and the visual analog scale (VAS) for pain, which were collected preoperatively at 3 months, 6 months, and yearly after surgery.1,2,4,12 Patient satisfaction was measured through 2 questions taken from the Surgical Satisfaction Questionnaire–8: “How satisfied are you with the results of your surgery?” and “Looking back, if you ‘had to do it all over again’ would you have the surgery again?” 11 Treatment failure was defined as reoperation to revise any of the previously implanted osteochondral allografts (revision) or conversion to arthroplasty at any time during the follow-up. Treatment was categorized as successful when patients returned to functional activities without the need for revision or arthroplasty surgery. The initial success rate was calculated using the following formula: 100%– (% revision+% arthroplasty).
Statistical Analysis
Data were included for statistical analyses when applicable registry data were available for patients undergoing OCAT for femoral condyle OCD with >2-year follow-up data, including patient characteristics, operative data, complications, reoperations, revisions, failures, and patient-reported outcomes. Descriptive statistics were calculated to report means, medians, ranges, and percentages. Normality tests were performed. One-way analyses of variance with Tukey post hoc analyses were used to assess for significant differences in patient-reported outcome measures over time. Differences in patient-reported outcome measures were also evaluated for minimum clinically important differences.13,18,33 Primary and salvage cohorts were compared for statistically significant differences using t tests or Fisher exact tests. Statistical significance was set at P < .05.
Results
All eligible patients with femoral condyle OCD who were prospectively enrolled in the registry and met the inclusion criteria (n = 22 consecutive cases) were included for analysis, with none lost to the 2-year follow-up (mean, 40.3 months; range, 24-82 months). OCD lesions of the medial femoral condyle (n = 17), lateral femoral condyle (n = 4), or both medial and lateral condyles (n = 1) were included. The mean patient age was 25.3 years (range, 12-50 years), and the mean body mass index was 25.2 kg/m2 (range, 17-42 kg/m2). On average, patients had undergone 2.5 previous knee surgeries (range, 0-6) before their OCAT. The mean lesion size at the time of OCAT was 5.6 cm2 (range, 2-9.6 cm2), with 17 classified as osteochondral and 6 as chondral. Also, shell allografts and plug allografts were used to treat 15 and 7 patients, respectively. The Reamer-Irrigator-Aspirator system was used in 2 patients. The mean VCD of the assessed OCAs (n = 12) was 99.1% (range, 79%-117%) at the time of transplantation. Four patients underwent surgical procedures to address comorbidities, with 1 patient undergoing concurrent anterior cruciate ligament reconstruction (ACLR) with meniscal allograft transplantation (MAT), 1 patient undergoing concurrent MAT with trochlear OCAT, 1 patient undergoing subsequent distal femoral osteotomy, and 1 patient undergoing concurrent high tibial osteotomy.
Eleven primary and 11 salvage OCAT patients were included. Data for patient and surgical characteristics as well as %VCD are provided in Table 1. No statistically significant differences between primary OCAT and salvage OCAT cohorts were noted.
Table 1.
Patient and Surgical Characteristics and %VCD by Study Cohort a
| Variable | Primary OCAT (n = 11) | Salvage OCAT (n = 11) | P |
|---|---|---|---|
| Age, y | 23.9 | 26.6 | .54 |
| BMI, kg/m2 | 26.4 | 24.1 | .41 |
| MFC/LFC/both, n | 7/4/0 | 10/0/1 | .31 |
| Lesion size, cm2 | 5.5 | 5.7 | .96 |
| Chondral/osteochondral, n | 3/8 | 3/9 | >.99 |
| Plug/shell, n | 5/6 | 2/9 | .36 |
| VCD, % | 93 | 101 | .19 |
Data are reported as mean unless otherwise indicated BMI, body mass index; both, medial and lateral femoral condyles transplanted; chondral, chondral only with no bony involvement; LFC, lateral femoral condyle; MFC, medial femoral condyle; OCAT, osteochondral allograft transplant; osteochondral: bone and cartilage involvement; VCD, viable chondrocyte density.
Treatment Outcomes
The overall success rate for the entire study population was 90.9% (20/22) at a mean follow-up of 40.3 months (range, 24-82 months). One patient in the primary OCAT cohort required revision OCAT, and 1 patient in the salvage OCAT cohort required conversion to total knee arthroplasty (TKA). The revision OCAT was performed in a 20-year-old male patient 22 months after primary OCAT of the medial femoral condyle. This patient’s primary OCAT was performed using a custom-cut shell allograft, which required resection of recipient bone to a depth of 15 mm to reach viable, bleeding bone and a corresponding donor tissue thickness. This patient experienced a fall 15 months postoperatively, and subsequent magnetic resonance imaging revealed evidence for incomplete OCA osteointegration and concern for impending failure (Figure 3).
Figure 3.
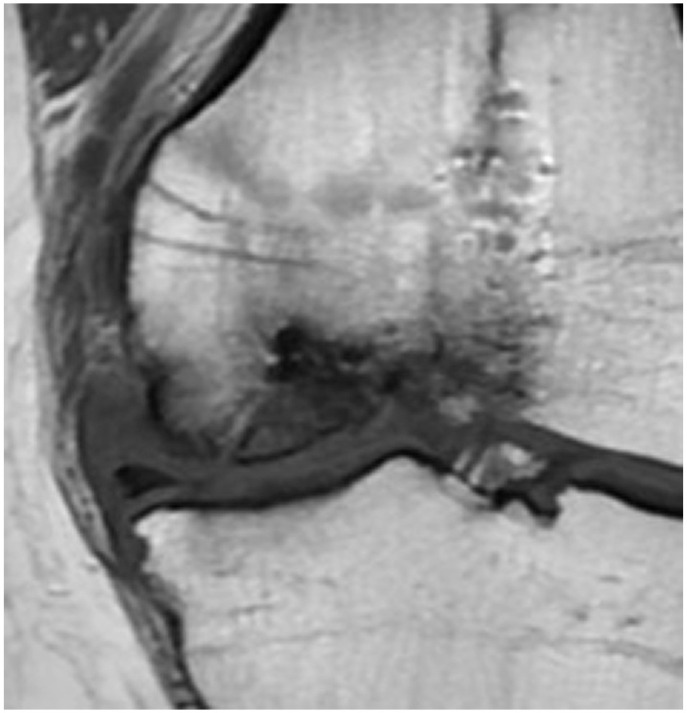
Coronal plane T1-weighted MRI of the left knee of a 20-year-old male patient 22 months after primary OCAT of the medial femoral condyle, showing evidence for incomplete OCA osteointegration and concern for impending failure. MRI, magnetic resonance imaging; OCA, osteochondral allograft.
Revision OCAT was performed using another custom-cut shell allograft; the patient had radiographic evidence for osteointegration and returned to functional activities without further surgery 24 months after revision. As such, the overall success rate for the entire study population at >2 years was 95.5% when including this successful revision OCAT. The TKA was performed in a 55-year-old female patient 53 months after salvage OCAT of the medial femoral condyle. This patient opted for TKA based on the progression of knee pain and dysfunction with radiographic evidence for degenerative knee OA after 4.5 years of return to functional activities.
In addition, 4 other reoperations (18.1%) were performed, including 1 distal femoral osteotomy, 1 lysis of adhesions, and 2 implant (hardware) removals. One implant removal was performed in a 30-year-old female patient 39 months after primary OCAT of the medial femoral condyle with concurrent ACLR and MAT, allowing for arthroscopic assessment of the transplants (Figure 4).
Figure 4.

Arthroscopic image from an anterolateral portal in the right knee of a 30-year-old female patient 39 months after primary plug OCAT for the treatment of medial femoral condyle OCD with concurrent ACLR and MAT, showing the integrity of the osteochondral and meniscus allografts. ACLR, anterior cruciate ligament reconstruction; MAT, meniscal allograft transplantation; OCAT, osteochondral allograft transplantation; OCD, osteochondritis dissecans.
Patient-Reported Outcomes and Satisfaction
VAS pain, IKDC, Single Assessment Numeric Evaluation, PROMIS-Physical Function, and PROMIS-Mobility scores showed statistically significant (P < .05) and clinically meaningful13,18,33 improvements in both study cohorts at the 1-year and final follow-up (Table 2). There were no significant differences in patients undergoing primary or salvage OCAT. At the final follow-up, 20 patients (90.9%) reported that they were satisfied or very satisfied, and 21 patients (95.5%) reported that they would choose OCAT again for treatment.
Table 2.
Patient-Reported Outcomes Overall and by Study Cohort a
| VAS Pain | IKDC | SANE | PROMIS-PF | PROMIS-Mobility | |
|---|---|---|---|---|---|
| All (n = 22) | |||||
| Preop | 5.0 (2-8) | 44.8 (26-62) | 54.5 (20-85) | 39.7 (21-49) | 40.5 (27-60) |
| 1-y follow-up | 1.5 (0-8.5) | 60.1 (38-91) | 68.4 (42-100) | 45.6 (33-59) | 44.8 (30-60) |
| Final follow-up | 1.3 (0-6) | 69.9 (51-98) | 80.4 (48-100) | 49.8 (36-61) | 50.0 (36-60) |
| Primary OCAT | |||||
| Preop | 5.2 (2-8) | 47.3 (36-62) | 50.9 (20-82) | 37.2 (21-44) | 37.7 (27-43) |
| 1-year follow-up | 1.2 (0-5) | 62.6 (38-91) | 72.0 (42-100) | 46.5 (39-58) | 46.3 (40-60) |
| Final follow-up | 1.2 (0-6) | 72.6 (52-98) | 87.3 (70-100) | 51.5 (40-61) | 50.8 (42-60) |
| Salvage OCAT | |||||
| Preop | 4.8 (3-7.5) | 42.8 (26-54) | 58.1 (25-85) | 41.5 (34-49) | 42.7 (33-60) |
| 1-y follow-up | 1.7 (0-8.5) | 57.5 (45-85) | 64.7 (45-85) | 44.7 (33-59) | 42.7 (30-60) |
| Final follow-up | 1.3 (0-4) | 67.4 (51-91) | 75.3 (48-90) | 48.0 (36-60) | 49.4 (36-60) |
Data are reported as mean (range). IKDC, International Knee Documentation Committee; OCAT, osteochondral allograft transplant; PF, physical function; preop, preoperative; PROMIS, Patient-Reported Outcomes Measurement Information System; SANE, Single Assessment Numeric Evaluation.
Discussion
The results of this study provide evidence to support the acceptance of the hypothesis in that osteochondral allograft transplantation as surgical treatment for large femoral condyle OCD lesions was highly successful in significantly improving knee pain and function with no significant differences between primary and salvage procedure outcomes. In the present study, 91% of patients had successful outcomes at a mean of >3 years after OCAT, with 1 revision in the primary OCAT cohort and 1 conversion to TKA in the salvage OCAT cohort. The revision OCAT was associated with radiographic healing and restored knee function 2 years after the revision transplant, bringing the overall success rate to 96%. The TKA conversion was performed 4.5 years after salvage OCAT when the patient’s age (55 years) was considered more appropriate for arthroplasty. For both primary and salvage OCATs, patient-reported measures of pain and function significantly improved at the 1-year and final follow-up, and >90% of patients reported that they were satisfied and would choose OCAT again to treat their femoral condyle OCD. Taken together, the data suggest that OCAT is an appropriate option for primary surgical treatment and as a salvage procedure for patients who experience treatment failure after another primary surgical intervention for femoral condyle OCD when high-chondrocyte-viability OCAs, optimized transplantation techniques, and robust patient management strategies can be implemented.22,23,27-29
Previous studies assessing outcomes after OCAT for the treatment of OCD lesions in the knee have reported similarly high success rates, ranging from 80% to 100%; nonetheless, they have not directly compared primary versus salvage cohorts.7,9,15,24 In the largest study to date, Sadr et al 24 reported outcomes for 135 patients treated with OCAT for OCD lesions of the femoral condyles (n = 123), trochlea, or patella, 81% of which were considered salvage surgeries. The authors reported a reoperation rate of 23% and a treatment failure rate of 8% at a mean follow-up of 6.3 years. They did not find age, sex, previous surgery, graft size, anatomic location, or preoperative function scores significantly associated with failures. Our results demonstrated similar reoperation (18%) and treatment failure (9%) rates. In addition, the 1 revision OCAT performed to address a primary OCAT treatment failure was associated with a successful outcome; most reoperations (eg, lysis of adhesions, “hardware” removal) were not directly related to the OCA, and TKA conversion was performed after 4.5 years of functional graft survival such that it could be considered an effective bridging procedure for this patient.
While cohort sizes in the present study prevented valid determination of risk factors for reoperations or treatment failures, primary and salvage cohorts were similar for all variables assessed, and treatment success rates were identical between cohorts. In conjunction with previous data suggesting that salvage OCAT is superior to other methods for revision of failed OCD surgical treatments,5,31 current evidence indicates that OCAT may provide the most consistent results for surgical treatment of femoral condyle OCD across the spectrum of patients affected, both as a primary and a salvage surgical treatment option. Based on the documented advantages over other surgical treatment options, consideration should be given to the use of OCAT as a primary treatment option for patients with irreparable femoral condyle OCDs who have failed nonsurgical management.
Limitations
This study was limited by its relatively small sample size and the fact that it was performed at a single institution specializing in joint preservation surgery. As such, these outcomes may not be generalizable. In addition, the results reported represent only short- to mid-term outcomes, such that conclusions regarding long-term outcomes after primary and salvage OCAT cannot be determined. Further, direct comparisons to other surgical treatment options for femoral condyle OCD were not included in the experimental design, making outcomes only applicable to OCAT. Given the relative infrequency of surgically indicated OCD lesions at a single institution, however, this study provides valuable data to the body of literature assessing outcomes of OCAT for this pathology, particularly in comparing primary versus salvage surgical treatment options.
Conclusion
Based on the low treatment failure rates in conjunction with statistically significant and clinically meaningful improvements in patient-reported outcomes, osteochondral allograft transplantation can be considered an appropriate option for primary and salvage surgical treatment for patients with irreparable OCD lesions of the femoral condyles.
Footnotes
Final revision submitted July 28, 2023; accepted September 6, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.N. has received financial or material support from AO Foundation and Arthroscopy; education payments from Arthrex and Elite Orthopedics; consulting fees from Arthrex and Guidepoint Consulting; nonconsulting fees from Vericel, Arthrex, and Stryker; royalties from Arthroscopy; and hospitality payments from Synthes GmbH. J.P.S. has received research support from Arthrex; financial or material support from Thieme; education payments from Elite Orthopedics; consulting fees from Medical Device Business Services, DePuy, Orthopedic Designs North America, Smith & Nephew, and Arthrex; nonconsulting fees from Synthes GmbH and Medical Device Business Services; and royalties from Thieme. R.M. has received research support from Cartiheal, Moximed, and Novocart. M.K. has received education payments from Elite Orthopedics and Arthrex; nonconsulting fees from Synthes GmbH; and honoraria from Synthes GmbH. J.L.C. has received research support from AO Trauma, Arthrex, Collagen Matrix, DePuy, Orthopaedic Trauma Association, Purina, Regenosine, and SITES Medical; financial or material support from Thieme; consulting fees from Arthrex and Trupanion; royalties from Arthrex, MTF Biologics, and Thieme; and is a board or committee member for MTF Biologics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Missouri (ref No. 2003053).
References
- 1. Askew RL, Cook KF, Revicki DA, Cella D, Amtmann D. Evidence from diverse clinical populations supported clinical validity of PROMIS pain interference and pain behavior. J Clin Epidemiol. 2016;73:103-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res.2008;31(2):165-169. [DOI] [PubMed] [Google Scholar]
- 3. Bruns J, Werner M, Habermann C. Osteochondritis dissecans: etiology, pathology, and imaging with a special focus on the knee joint. Cartilage. 2018;9(4):346-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Christensen J, Peters C, Gililland J, Stoddard G, Pelt C. Physical activity, pain interference and comorbidities relate to PROMIS physical function in younger adults following total knee arthroplasty. Disabil Rehabil. 2021;43(26):3741-3747. [DOI] [PubMed] [Google Scholar]
- 5. Chui K, Jeys L, Snow M. Knee salvage procedures: the indications, techniques and outcomes of large osteochondral allografts. World J Orthop. 2015;6(3):340-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Crecelius CR, Van Landuyt KJ, Schaal R. Postoperative Management for articular cartilage surgery in the knee. J Knee Surg. 2021;34(1):20-29. [DOI] [PubMed] [Google Scholar]
- 7. Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35(6):907-914. [DOI] [PubMed] [Google Scholar]
- 8. Erickson BJ, Chalmers PN, Yanke AB, Cole BJ. Surgical management of osteochondritis dissecans of the knee. Curr Rev Musculoskelet Med. 2013;6(2):102-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Garrett JC. Osteochondritis dissecans. Clin Sports Med. 1991;10(3):569-593. [PubMed] [Google Scholar]
- 10. Grimm N, Danilkowicz R, Shea K. OCD lesions of the knee: an updated review on a poorly understood entity: current concept review. J Pediatr Orthop. 2019;1(1). [Google Scholar]
- 11. Haff RE, Stoltzfus J, Lucente VR, Murphy M. The surgical satisfaction questionnaire (SSQ-8): a validated tool for assessment of patient satisfaction following surgery to correct prolapse and/or incontinence. J Minim Invasive Gynecol. 2011;18(6):S49-S50. [Google Scholar]
- 12. Higgins LD, Taylor MK, Park D, et al. Reliability and validity of the International Knee Documentation Committee (IKDC) subjective knee form. Joint Bone Spine. 2007;74(6):594-599. [DOI] [PubMed] [Google Scholar]
- 13. Hung M, Bounsanga J, Voss MW, Saltzman CL. Establishing minimum clinically important difference values for the Patient-Reported Outcomes Measurement Information System Physical Function, hip disability and osteoarthritis outcome score for joint reconstruction, and knee injury and osteoarthritis outcome score for joint reconstruction in orthopaedics. World J Orthop. 2018;9(3):41-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kessler JI, Nikizad H, Shea KG, Jacobs JC, Bebchuk JD, Weiss JM. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am J Sports Med. 2014;42(2):320-326. [DOI] [PubMed] [Google Scholar]
- 15. Lyon R, Nissen C, Liu XC, Curtin B. Can fresh osteochondral allografts restore function in juveniles with osteochondritis dissecans of the knee? Clin Orthop Relat Res. 2013;471(4):1166-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Masquijo J, Kothari A. Juvenile osteochondritis dissecans (JOCD) of the knee: current concepts review. EFORT Open Rev. 2019;4(5):201-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miura K, Ishibashi Y, Tsuda E, Sato H, Toh S. Results of arthroscopic fixation of osteochondritis dissecans lesion of the knee with cylindrical autogenous osteochondral plugs. Am J Sports Med. 2007;35(2):216-222. [DOI] [PubMed] [Google Scholar]
- 18. Ogura T, Ackermann J, Mestriner AB, Merkely G, Gomoll AH. The minimal clinically important difference and substantial clinical benefit in the patient-reported outcome measures of patients undergoing osteochondral allograft transplantation in the knee. Cartilage. 2021;12(1):42-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paatela T, Vasara A, Sormaala M, Nurmi H, Kautiainen H, Kiviranta I. Chondral and osteochondritis dissecans lesions treated by autologous chondrocytes implantation: a mid- to long-term nonrandomized comparison. Cartilage. 2021;13(suppl 1):S1105-S1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pascual-Garrido C, Friel NA, Kirk SS, et al. Midterm results of surgical treatment for adult osteochondritis dissecans of the knee. Am J Sports Med. 2009;37(suppl 1):S125-S130. [DOI] [PubMed] [Google Scholar]
- 21. Pascual-Garrido C, McNickle AG, Cole BJ. Surgical treatment options for osteochondritis dissecans of the knee. Sports Health. 2009;1(4):326-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rucinski K, Cook JL, Crecelius CR, Stucky R, Stannard JP. Effects of compliance with procedure-specific postoperative rehabilitation protocols on initial outcomes after osteochondral and meniscal allograft transplantation in the knee. Orthop J Sports Med. 2019;7(11):2325967119884291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rucinski K, Stucky R, Crecelius CR, Stannard JP, Cook JL. Effects of patient assessment and education by an integrated care team on postoperative adherence and failure rates after osteochondral allograft and meniscal allograft transplantation in the knee. Orthop J Sports Med. 2023;11(5):23259671231160780. doi: 10.1177/23259671231160780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sadr KN, Pulido PA, McCauley JC, Bugbee WD. Osteochondral allograft transplantation in patients with osteochondritis dissecans of the knee. Am J Sports Med. 2016;44(11):2870-2875. [DOI] [PubMed] [Google Scholar]
- 25. Sanders TL, Pareek A, Johnson NR, et al. Nonoperative management of osteochondritis dissecans of the knee: progression to osteoarthritis and arthroplasty at mean 13-year follow-up. Orthop J Sports Med. 2017;5(7):2325967117704644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schreiner AJ, Stannard JP, Cook CR, et al. Initial clinical outcomes comparing frozen versus fresh meniscus allograft transplants. Knee. 2020;27(6):1811-1820. [DOI] [PubMed] [Google Scholar]
- 27. Stannard JP, Cook JL. Prospective assessment of outcomes after primary unipolar, multisurface, and bipolar osteochondral allograft transplantations in the knee: a comparison of 2 preservation methods. Am J Sports Med. 2020;48(6):1356-1364. [DOI] [PubMed] [Google Scholar]
- 28. Stoker AM, Stannard JP, Cook JL. Chondrocyte viability at time of transplantation for osteochondral allografts preserved by the Missouri Osteochondral Preservation System versus Standard Tissue Bank Protocol. J Knee Surg. 2018;31(8):772-780. [DOI] [PubMed] [Google Scholar]
- 29. Stoker AM, Stannard JP, Kuroki K, Bozynski CC, Pfeiffer FM, Cook JL. Validation of the Missouri Osteochondral Allograft Preservation System for the maintenance of osteochondral allograft quality during prolonged storage. Am J Sports Med. 2018;46(1):58-65. [DOI] [PubMed] [Google Scholar]
- 30. Tabaddor RR, Banffy MB, Andersen JS, et al. Fixation of juvenile osteochondritis dissecans lesions of the knee using poly 96L/4D-lactide copolymer bioabsorbable implants. J Pediatr Orthop. 2010;30(1):14-20. [DOI] [PubMed] [Google Scholar]
- 31. Tisano B, Ellis HB, Wyatt C, Wilson PL. Osteochondral allograft for unsalvageable osteochondritis dissecans in the skeletally immature knee. Orthop J Sports Med. 2022;10(2):23259671211072516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Uppal HS, Peterson BE, Misfeldt ML, et al. The viability of cells obtained using the Reamer-Irrigator-Aspirator system and in bone graft from the iliac crest. Bone Jt J. 2013;95(9):1269-1274. [DOI] [PubMed] [Google Scholar]
- 33. Winterstein AP, McGuine TA, Carr KE, Hetzel SJ. Comparison of IKDC and SANE outcome measures following knee injury in active female patients. Sports Health. 2013;5(6):523-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wu IT, Custers RJH, Desai VS, et al. Internal fixation of unstable osteochondritis dissecans: do open growth plates improve healing rate? Am J Sports Med. 2018;46(10):2394-2401. [DOI] [PubMed] [Google Scholar]



