Abstract
Cutaneous mucormycosis is a rare, opportunistic fungal infection that typically affects immunocompromised hosts. Current treatment consists of systemic antifungal therapy, surgical debridement, and when applicable, restoration of immune function. Despite intervention, the morbidity and mortality of invasive fungal disease remains high. There are few reports of primary or secondary cutaneous mucormycosis involving the ocular adnexa. The authors describe the course of two children with cutaneous mucormycosis of the eyelid treated with subcutaneous liposomal amphotericin B (LAmB) injections (3.5 mg/mL) in an off-label application as an adjunct to debridement and systemic anti-fungal therapy. To the authors’ knowledge, these are the first two cases of invasive fungal disease involving the eyelid treated with subcutaneous LAmB injections, and the first reported case of disseminated fungal infection with secondary cutaneous involvement of the eyelid.
Precis:
The authors describe two cases of cutaneous mucormycosis of the eyelid treated with subcutaneous liposomal amphotericin B injections.
Introduction:
Cutaneous mucormycosis is the third most common presentation of invasive fungal infection following rhino-orbital-cerebral and pulmonary disease.1,2 Unique to cutaneous mucormycosis, immunocompromised and immunocompetent patients are equally affected, although an immunocompromised state portends a worse prognosis.3–5 Infection occurs either primarily, via direct traumatic fungal inoculation, or secondarily, through contiguous spread from a nearby location, or rarely, from disseminated disease.4 Regardless of the route of inoculation, the signs and symptoms of cutaneous fungal infection can vary widely and mimic many other skin conditions. Like other forms of invasive fungal disease, timely diagnosis and intervention are critical to avoid progressive angioinvasion and life-threatening infection.5 Currently, the treatment of cutaneous mucormycosis includes systemic antifungal therapy, surgical debridement, and if applicable, reversal of immunosuppression.6 Despite this being a cutaneous disease, there is limited discussion in the literature regarding the potential utility of local interventions.
The authors report two cases of cutaneous mucormycosis involving the eyelids that were treated with subcutaneous liposomal amphotericin B (LAmB) injections in an off-label application as an adjunct to surgical debridement and systemic antifungal therapy. The collection and evaluation of protected health information and photographic consent was performed in compliance with the provisions of the United States of America Health Insurance Portability and Accountability Act of 1996 and adhered to the World Medical Association’s ethical principles for medical research involving human subjects outlined in the Declaration of Helsinki as amended in 2013.
Case Presentations:
Case 1.
A 4-year-old male with Stage IV metastatic neuroblastoma and a complicated hospital course requiring prolonged mechanical ventilation was found to have a progressively enlarging soft tissue lesion of the left maxilla at the site of endotracheal (ET) tube taping (Figure 1A). Magnetic resonance imaging (MRI) demonstrated fat-stranding in the subcutaneous tissue of the left face (Figure 1B). There was no evidence of orbital involvement. Biopsy of the left cheek revealed ribbon-like, non-septate fungal hyphae. KOH smear demonstrated non-septate hyphae consistent with Mucorales. Fungal culture utilizing Potato Flake Agar (PFA) confirmed Rhizopus spp. (Order: Mucorales) sensitive to amphotericin B. The patient was started on systemic LAmB 5 mg/kg/dose and immunosuppressive medications were weaned off within one week of diagnosis of fungal infection. He underwent facial debridement, and pathology demonstrated fungal elements extending into the left lower eyelid. On examination, the eyelid appeared well perfused without evidence of necrosis (Figure 1C). To avoid further debridement that could compromise the eyelid and ocular surface, the patient was treated with subcutaneous LAmB injections in an off-label application. The left lower eyelid was injected serially over the course of three days with 1 mL of LAmB (3.5 mg/mL) each day. Approximately 0.25 mL of LAmB was injected at two points pre-orbicularis and two points sub-orbicularis in the left lower eyelid to evenly distribute the medication along the affected tissues. The debrided left cheek was also treated with gauze soaked in LAmB that was changed daily. Following the series of LAmB injections, the patient had transient worsening of eyelid erythema, edema and conjunctival chemosis, all of which resolved within a few days. Control of the cutaneous infection was eventually achieved, and the left lower eyelid recovered without debridement. The primary cutaneous fungal infection was attributed to direct inoculation from a breakdown in the skin barrier secondary to the adhesive tape securing the ET tube. Seven weeks later, following control of the cutaneous infection, the patient underwent reconstruction of his left facial defect with a split-thickness skin graft. No further intervention of the left lower eyelid was required. At fourteen months, he demonstrates recovery from the infection and surgery (Figure 1D).
Figure 1.
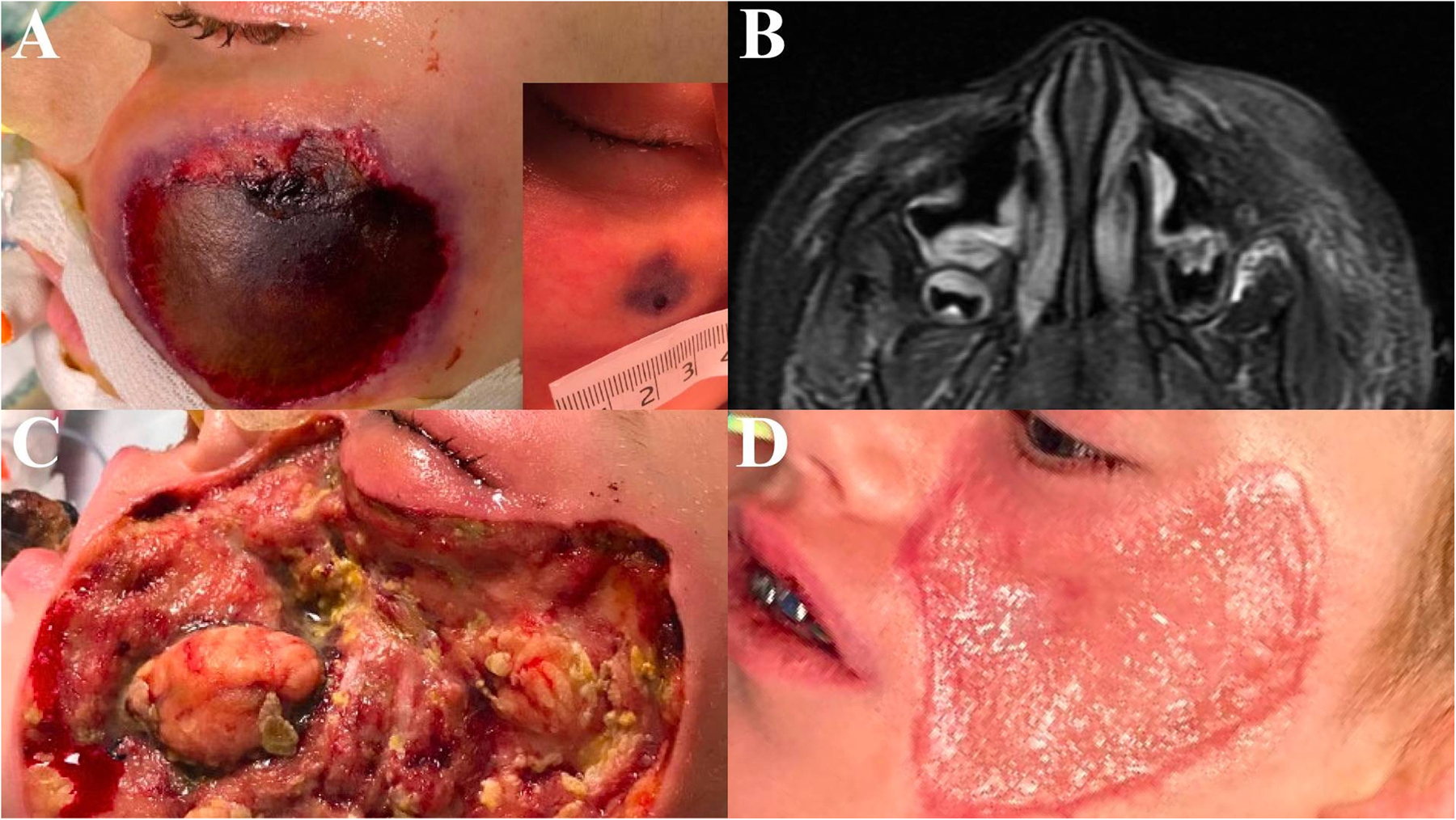
Case 1. A 4-year-old male with Stage IV metastatic neuroblastoma presenting with cutaneous mucormycosis of the left maxilla from primary inoculation. A – Progressive enlarging soft tissue lesion of the left maxilla at the site of endotracheal tube (ET) taping. The appearance of the initial lesion is demonstrated (inset). B – Magnetic resonance imaging (MRI) demonstrating subcutaneous fat stranding in the left mid-face. C – Left maxilla following surgical debridement with persistent fungal elements seen on histopathology at the left lower eyelid tissue margin. Note, there is no evidence of gross necrosis of the eyelid. D – Fourteen months later following reconstruction with split thickness skin graft.
Case 2.
A 4-year-old female with acute lymphoblastic leukemia (ALL) was transferred from an outside hospital for evaluation of right periorbital edema and pulmonary infiltrates. Examination was notable for right lower eyelid edema, erythema, duskiness of the eyelid margin, and necrosis of the inferior palpebral conjunctiva (Figure 2A). The vision, intraocular pressure, extraocular motility, and dilated fundus exam were normal. MRI demonstrated enhancement of the right preseptal tissue (Figure 2B). Biopsy of the right lower eyelid palpebral conjunctiva and pretarsal orbicularis revealed broad, ribbon-like, non-septate fungal hyphae (Figure 2C). KOH smear demonstrated non-septate hyphae consistent with Mucorales, however, fungal culture utilizing PFA did not isolate fungus. A portion of the right lower eyelid palpebral conjunctiva and pretarsal orbicularis biopsies were sent for Universal PCR (University of Washington, Department of Laboratory Medicine, Seattle, WA). Zygomycete PCR revealed Rhizomucor spp. (Rhizomucor pusillus). The patient was started on intravenous LAmB 5 mg/kg/dose and additional chemotherapy was held during the period of active fungal infection. Conservative debridement of the necrotic conjunctiva was performed, and the patient was treated with two, serial subcutaneous 1 mL injections of LAmB (3.5 mg/mL) in an off-label application. The injection was performed in the subcutaneous, pre-orbicularis plane at two points in the right lower eyelid to evenly distribute the medication along the affected tissue. The initial injection was at the time of eyelid biopsy. The patient’s eyelid continued to have a mildly dusky appearance, thus following discussion with the multi-disciplinary team and parents, a second injection was performed twelve days later while the patient was sedated for an unrelated procedure. The clinical appearance of the eyelid improved. During the interim period between injections, the patient also underwent a broncheoalveolar lavage (BAL) with biopsy which revealed fungal infection. Serum PCR also demonstrated Rhizomucor spp., establishing the diagnosis of disseminated disease with a presumed pulmonary source. Despite fungal invasion of the inferior marginal arcade and subsequent necrosis of the right lower eyelid margin, the patient did not require further debridement or subcutaneous LAmB injections. Twenty months following treatment, the right lower eyelid maintained adequate protection of the ocular surface, thus reconstruction was deferred (Figure 2D).
Figure 2.
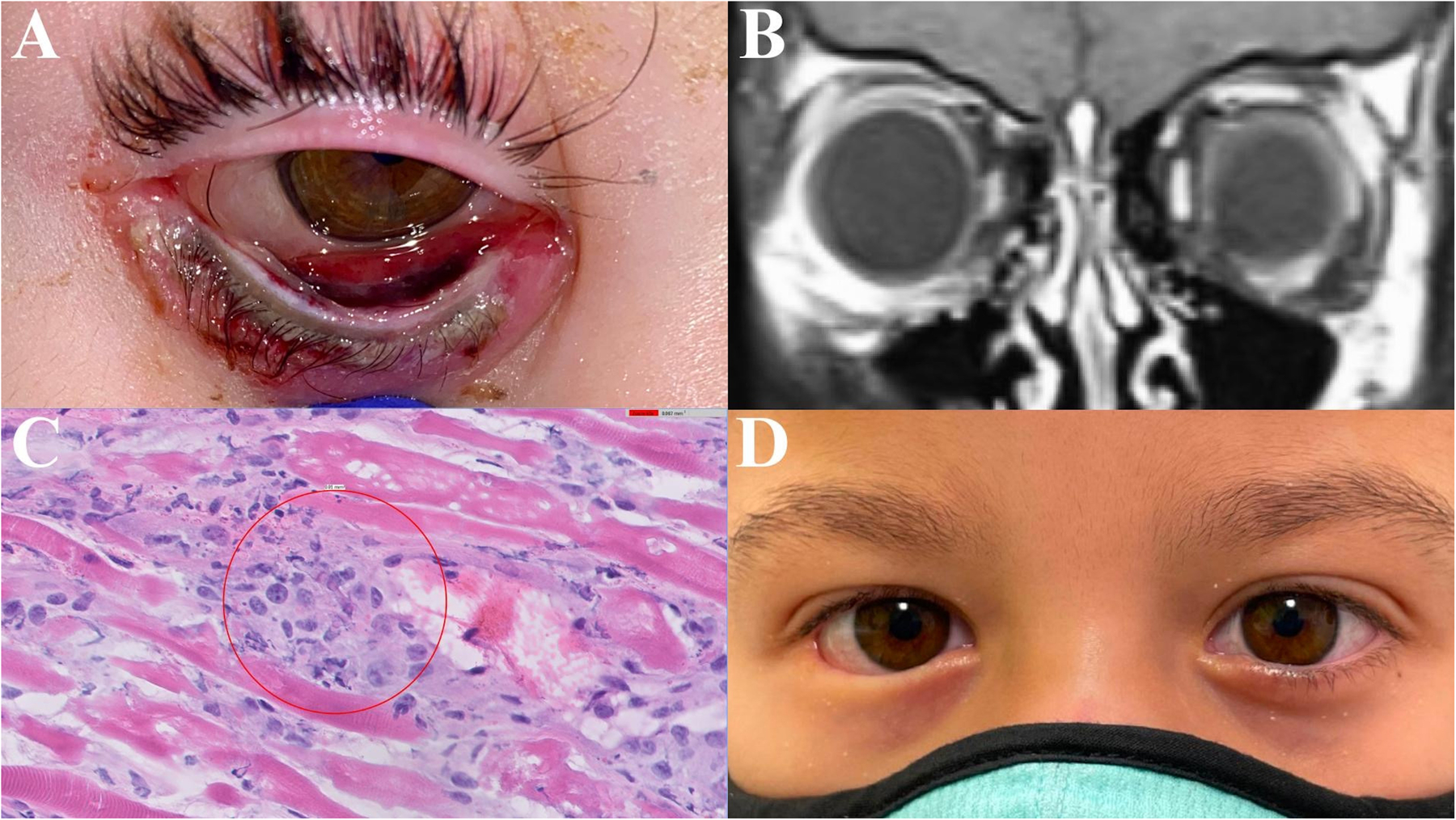
Case 2. A 4-year-old female with acute lymphoblastic leukemia (ALL) presenting with cutaneous mucormycosis of the right lower eyelid from disseminated pulmonary disease. A – Right lower eyelid edema, erythema, duskiness of the eyelid margin, and necrosis of the inferior palpebral conjunctiva. B – Magnetic resonance imaging (MRI) demonstrating enhancement of the right preseptal tissue. C – Right lower eyelid palpebral conjunctiva and pretarsal orbicularis histopathology demonstrating broad, ribbon-like, non-septate fungal hyphae (hematoxylin-eosin stain, original magnification 60x). D – Twenty months following treatment, the right lower eyelid maintains adequate protection of the ocular surface without further intervention.
Discussion:
Acute invasive fungal infections are rapidly progressive and potentially lethal. Cutaneous mucormycosis infections occur primarily from direct inoculation at a site of trauma (Case 1) but can also occur secondarily due to contiguous spread or disseminated fungal disease (Case 2). Reverse dissemination, or hematogenous dissemination to the skin, is extremely rare and is typically the result of hematogenous spread from a localized pulmonary source.1,3 Although cutaneous infection has a better prognosis than other clinical forms of mucormycosis, the mortality rate is not negligible, and ranges between 4–50%.3–4,6 In disseminated disease, mortality is consistently reported to be greater than 90%.3,4 It is important to note that in contrast to other forms of acute invasive fungal infections, cutaneous infection regularly affects both immunocompetent and immunocompromised patients.3,4 Those with underlying immune impairment, especially hematologic malignancy, tend to have more extensive disease, and thus a worse prognosis.2
Due to the variable presentation, a high level of suspicion for any progressive skin lesion, especially in the setting of trauma, burns, and applied topical adhesives is necessary. As demonstrated in the authors’ first case, primary cutaneous mucormycosis secondary to an adhesive bandage is a well-recognized occurrence.6 Suspicious lesions warrant biopsy with frozen section pathology to assess for broad, non-septate hyphae that is diagnostic of Mucorales. In addition, vascular invasion and thrombosis of small vessels may be seen. PCR and DNA sequencing of clinical samples can supplement conventional histopathology in confirming the diagnosis. Systemic antifungals should be started based on suspicion, and once confirmed with biopsy, surgical debridement should be performed to decrease the risk of further invasion and dissemination.1,5,7
In anatomical regions where the preservation of tissue is critical, such as the eyelids, the use of local-acting anti-fungal therapy may be beneficial. Several cases in the literature describe the use of topical amphotericin B (wound irrigation and/or impregnated gauze) in an off-label application as an adjuvant following wide-surgical debridement.7–9 In cases of invasive fungal orbital disease, retrobulbar amphotericin B injections have been effective in an off-label application in decreasing morbidity with minimal adverse events.10 Similarly, intralesional and subcutaneous injection of amphotericin B in an off-label application have been successfully used in the treatment of cutaneous leishmaniasis and chromoblastomycosis infections with minimal to no injection-site complications.11–14
In this series, the patients were injected with 1 mL of LAmB (3.5 mg/mL) per injection. This formulation was chosen due to institutional availability. The concentration was based on known efficacy and safety in the retrobulbar tissues.10 Both patients tolerated the injections well. Each developed a mild, local injection site reaction of erythema, edema and chemosis that resolved within days. Serum concentrations of LAmB were monitored in both patients and neither required alteration of their systemic anti-fungal dose during or after cutaneous LAmB injections. To the authors’ knowledge, the local injection of amphotericin B for other cutaneous disorders has not led to notable systemic accumulation or adverse events.11–14 This is in contrast to the intravenous administration of the drug which can have nephrotoxic as well as other side effects. It is likely that systemic absorption of cutaneously injected drug is low because of the low volume and concentration of each local injection.
Although both deoxycholate and liposomal formulations have been successfully utilized in the local treatment of cutaneous leishmaniasis, the liposomal formulation may have advantages.14 Liposomes are better able to penetrate the epidermis and dermis, possibly allowing for better infiltration of antifungal medication to the diseased tissue.14 LAmB also has a lower overall side effect profile in case of systemic absorption.13,14 In general though, care should be taken while simultaneously treating a patient with systemic and local amphotericin B, regardless of the formulation. A larger sample size and more in-depth assessment of antifungal minimal inhibitory concentration, dose, and extent of safety of subcutaneous injections would be beneficial in determining the appropriate treatment regimen.
There are few reports of primary or secondary cutaneous mucormycosis involving the eyelids.15–20 To the authors’ knowledge, these are the first two cases of invasive fungal disease involving the eyelid successfully treated with subcutaneous LAmB injections in an off-label application as an adjunct to surgical debridement and systemic anti-fungal therapy. The authors also report the first case of disseminated fungal infection with secondary cutaneous involvement of the eyelid. Neither of the patients required further debridement of the periocular tissue and maintained adequate globe protection. In conclusion, the use of localized antifungal injections could prove a useful addition in the treatment of cutaneous fungal infections in an effort to preserve critical structures such as the ocular adnexa.
Financial Interests:
Supported by the National Eye Institute, National Institutes of Health, Bethesda, Maryland (grant no.: EY002162); and Research to Prevent Blindness, New York, New York (unrestricted grant). The authors have no conflicts of interest to disclose.
Footnotes
Meeting Presentation: Presented at the American Society of Ophthalmic Plastic and Reconstructive Surgery Fall Scientific Symposium, October 29, 2022, Chicago, Illinois.
References:
- 1.Jeong W, Keighley C, Wolfe R, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect 2019;25:26–34. [DOI] [PubMed] [Google Scholar]
- 2.Kato H, Foster CM, Karri K. Incidence, predisposing conditions and outcomes of cutaneous mucormycosis: a national database study. Mycoses 2021;64:569–572. [DOI] [PubMed] [Google Scholar]
- 3.Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis 2005;41:634–653. [DOI] [PubMed] [Google Scholar]
- 4.Skiada A, Rigopoulos D, Larios D, et al. Global epidemiology of cutaneous zygomycosis. Clin Dermatol 2012;30:628–632. [DOI] [PubMed] [Google Scholar]
- 5.Ziaka M, Papakonstantinou E, Vasileiou E, et al. Pediatric cutaneous mucormycosis: a case report and review of the literature. Mycoses 2022;65:674–682. [DOI] [PubMed] [Google Scholar]
- 6.Wirth F, Perry R, Eskenazi A, et al. Cutaneous mucormycosis with subsequent visceral dissemination in a child with neutropenia: a case report and review of the pediatric literature. J Am Acad Dermatol 1997;36:336–41. [DOI] [PubMed] [Google Scholar]
- 7.Konigsberg MW, Wu CH, Strauch RJ. Topical treatment for cutaneous mucormycosis of the upper extremity. J Hand Surg Am 2020;45:1189.e1–1189.e5. [DOI] [PubMed] [Google Scholar]
- 8.Di Pentima MC, Chan S, Powell J, et al. Topical amphotericin B in combination with standard therapy for severe necrotizing skin and soft-tissue mucormycosis in an infant with bilineal leukemia: case report and review. J Pediatr Hematol Oncol 2014;36:e468–70. [DOI] [PubMed] [Google Scholar]
- 9.Dawood AA, Al-Ahmad NS, Hussainy AM. Gangrenous cutaneous mucormycosis of anterior chest wall: a case report. Kuwait Med J 2003;35:137–139. [Google Scholar]
- 10.Ashraf DC, Idowu OO, Hirabayashi KE, et al. Outcomes of a modified treatment ladder algorithm using retrobulbar amphotericin B for invasive fungal rhino-orbital sinusitis. Am J Ophthalmol 2022;237:299–309. [DOI] [PubMed] [Google Scholar]
- 11.Ranawaka RR. Treatment of chromoblastomycosis with a combination of debulking surgery, intralesional amphotericin B, and oral terbinafine. Int J Dermatol 2021;60:1040–1041. [DOI] [PubMed] [Google Scholar]
- 12.Goyonlo VM, Vosoughi E, Kiafar B, et al. Efficacy of intralesional amphotericin B for the treatment of cutaneous leishmaniasis. Indian J Dermatol 2014;59:631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goswami P, Ghiya BC, Kumar V, et al. Comparison of efficacy of two different concentrations of intralesional amphotericin B in the treatment of cutaneous leishmaniasis; a randomized controlled trial. Indian Dermatol Online J 2019;10:627–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yardley V, Croft SL. Activity of liposomal amphotericin B against experimental cutaneous leishmaniasis. Antimicrob Agents Chemother 1997;41:752–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaman K, Kaur H, Rudramurthy SM, et al. Cutaneous mucormycosis of scalp and eyelids in a child with type 1 diabetes mellitus. Indian J Dermatol Venereol Leprol 2015;81:275–8. [DOI] [PubMed] [Google Scholar]
- 16.Chahal HS, Abgaryan N, Lakshminarayanan R, et al. Orbital mucormycosis following periorbital cutaneous infection. Ophthal Plast Reconstr Surg 2015;33:S146–S148. [DOI] [PubMed] [Google Scholar]
- 17.Chakravarti A, Bhargava R, Bhattacharya S. Cutaneous mucormycosis of nose and facial region in children: a case series. Int J Pediatr Otorhinolaryngol 2013;77:869–72. [DOI] [PubMed] [Google Scholar]
- 18.Bhansali A, Sharma A, Kashyap A, et al. Mucor endophthalmitis. Acta Ophthalmol Scand. 2001;79:88–90. [DOI] [PubMed] [Google Scholar]
- 19.Gupta R, Hari P, Anandula V. Eyelid fungal infections are rare, and often associated with predisposing factors. We present the case of a child with an ulcerated lesion of fungal etiology on the eyelid. Can J Ophthalmol 2017;52:e28–e29. [DOI] [PubMed] [Google Scholar]
- 20.Mukherjee B, Chatterjee R, Biswas J. Reverse masquerade syndrome: fungal adnexal infection mimicking carcinoma in a HIV-positive patient. Indian J Ophthalmol 2013;61:521–523. [DOI] [PMC free article] [PubMed] [Google Scholar]


