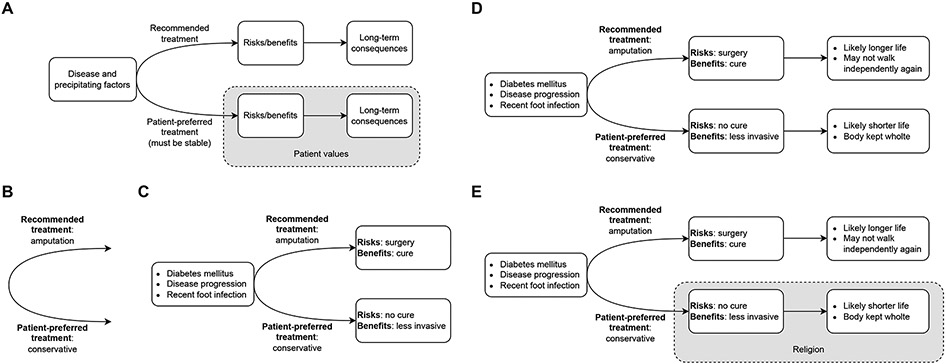
Paul Appelbaum outlines four criteria that patients must meet to be deemed to have capacity [1, 2, 3]. These four criteria are 1) communicating a choice, 2) understanding the relevant information, 3) appreciating the situation and its consequences, and 4) reasoning about treatment options. While Appelbaum’s framework is routinely used to determine whether patients have capacity, we recognize that the criteria may be difficult for primary teams to recall during an evaluation, necessitating psychiatry consultations. Here, we have developed a visual aide for determining capacity (Figure 1A). In short, if one is able to fill out a similar diagram following a capacity evaluation, then a patient likely has capacity. We argue this aide empowers primary teams to conduct their own capacity assessments.
Figure 1: Diagrammatic approach to determining capacity.
A) General framework. B-E) Specific example for determining capacity, built after a patient communicates a choice (B), understands the relevant information (C), appreciates the situation and its consequences (D), and reasons about treatment options (E)
Communicate a choice
Let us work through an example of a capacity evaluation and build the diagram as we go. Imagine a patient with advanced diabetes has developed gangrene of the foot. Her physicians have stated she requires a foot amputation, but she refuses, stating it is against her wishes. This is a common type of scenario in which psychiatry consultation is requested for capacity assessment. With this tool in hand, the primary team defers psychiatry consultation. They present the patient with various treatment options and she states a strong preference for conservative measures. Figure 1B captures the patient communicating a choice. If we start at the left, we can see a split between the team’s recommendation and what the patient wants.
Creating this diagram requires consistency of choice - the diagram’s static nature implies static choice. If the patient’s choice keeps changing, we will not be able to faithfully draw this diagram, and the patient can be deemed to likely lack capacity.
Understand the relevant information
Next, the patient should understand her medical illness, the treatments available, and risks and benefits. She states she knows she has diabetes mellitus, that it has been worsening, and that it places her at increased risk for certain types of infections, including what she has now. Based on her prior conversation, she knows she has at least two options in front of her: amputation, as recommended by the team, or conservative measures, which would mean continued antibiotics and wound care. She states the risks of amputation are the general risks of surgery, and the benefit is that it will likely lead to a cure. The risk of conservative measures is it is much less likely to lead to a cure, but the benefit is that it is less invasive. This conversation allows the team to fill out the diagram as shown in Figure 1C.
Appreciate the situation and its consequences
Appreciating the situation means the patient should understand the implication of her decision on her medical condition as well as her personal future. This requires the patient to take the consequences of her decisions one step further. If she goes through with surgery, she knows she will likely live longer, but that she may never walk independently again. If she gets conservative treatment, she understands she may not live as long, but that her body will be kept whole.
The team can now fill the diagram out further, including the longer-term consequences (Figure 1D). An implicit feature of this diagram is that the consequences should logically follow from the stated risks and benefits. If a patient is able to state the risks and benefits appropriately, and yet the perceived consequences do not logically follow (e.g., by negating the risks entirely), then it raises concern for lack of capacity.
Reason about treatment options
Finally, the patient must be able to reason about her options. In other words, the patient should be able to describe how she made her decision. From the perspective of the diagrammatic approach, this means the patient’s decision should be in line with her values. By focusing on her values, we allow the patient to make an “unreasonable” choice that the treatment team may disagree with. In our example, the patient states she is a deeply religious person and that her beliefs forbid her from accepting an amputation, because it is important that her body be kept whole. We can now introduce patient-specific values onto the diagram (Figure 1E).
Limitations
This approach does not factor in the sliding scale, in which different “levels” of capacity are needed depending on the risk/benefit ratio of particular decisions. This is a nuanced skill that is difficult to communicate diagrammatically, and is likely best learned through direct experience with capacity evaluations.
Conclusion
Determining capacity is an important skill for all patient-facing physicians. While Appelbaum’s framework has largely become the de facto framework for determining capacity, there is a need to efficiently and intuitively convey these principles. Our diagrammatic approach bridges this gap, and provides a valuable tool to empower primary teams to evaluate capacity.
Acknowledgements:
This work was supported by grant R25MH094612 from the National Institute of Mental Health, Bethesda, MD (B.A.B.).
Footnotes
Conflict of Interest Statement: The authors declare no conflicts of interest.
References
- [1].Grisso T, Appelbaum PS. Assessing competence to consent to treatment: A guide for physicians and other health professionals. Oxford University Press, USA; 1998. [Google Scholar]
- [2].Berg JW, Appelbaum PS, Grisso T. Constructing competence: formulating standards of legal competence to make medical decisions. Rutgers Law Review. 1996;48:345. [PubMed] [Google Scholar]
- [3].Appelbaum PS. Assessment of patients’ competence to consent to treatment. New England Journal of Medicine. 2007;357(18):1834–40. [DOI] [PubMed] [Google Scholar]