The promise of finding a cure for HIV involving analytical treatment interruptions (ATIs) has over-shadowed potential psychosocial considerations needed to adequately support participants and communities.1 ATIs are crucial to HIV research, providing insights into virus behaviour by suspending medications to assess the effect of interventions on maintaining HIV suppression without antiretroviral treatment (ART).2 However, the prominence of ATIs in HIV trials has been mostly powered to detect time to viral rebound.3 The recent shift towards more permissive ATIs allows for longer periods of viraemia (eg, weeks to months) to occur, particularly for interventions involving the immune system.2 Extended ATIs require a more robust consideration of risks and benefits; extending beyond clinical-related aspects of research participation to include potential mental, emotional, social, and relational effects of trials requiring the interruption of ART.4
Interrupting a proven HIV treatment for a potentially extended period can cause harms.5 The ethical question is whether the potential harms are proportional and justified. For people with HIV, ATIs can yield increased side-effects and adverse events for HIV care.5 There are also psychosocial and emotional risks of interrupting effective therapy, such as anxiety, stigma around becoming viraemic, or emotional distress in not being cured.6 ATI trials might lead to sudden rebounds in viraemia (from weeks to months), breaking the well established undetectable equals untransmittable (U=U) principle (ie, people with HIV who have suppressed and undetectable viral load from proper medication adherence cannot sexually transmit HIV). This consequence of ATI raises ethical concerns about informed consent and necessitates increased support for partners, including regular HIV testing and access to preventive measures such as pre-exposure prophylaxis (PrEP).
The potential for harms during ATIs differs across populations and geographical settings given restricted resources, variable political will, continued HIV-related stigma and discrimination, and growing social and economic inequality. Resource-restricted settings still face shortages of PrEP—whether oral, on-demand, or long-acting PrEP—for partners without HIV. These settings are often highly constrained health-care system infrastructures, restricting the ability to diffuse novel HIV treatment regimens required to allow ATIs to progress in case of developing ART resistance. Urgent attention is needed to understand how to adequately support trial participants to mitigate the risk of HIV transmission to sexual partners during ATIs.7 Groups facing heightened vulnerabilities during ATIs might include people in HIV serodifferent relationships8 and both cisgender and transgender women with HIV who are at risk of gender-based violence.9
Research informing the implementation of ATI trials among marginalised populations and in resource-restricted settings is scarce. To mitigate potential harms, ATI trials should proactively centre community and patient perspectives with the integration of sociobehavioural sciences and bioethics research. Understanding local realities will be crucial to designing acceptable HIV cure research strategies and risk mitigation plans, including ATI-specific consent processes, to help people with HIV make decisions about engaging in ATI trials and avoiding the risks of therapeutic or curative misconception.
The scientific promise of HIV research should be accompanied by justice-informed frameworks, drawing from community-informed knowledge, to mitigate potential harms related to ATIs (figure). As a baseline, studies should include free open access to condoms, PrEP, and post-exposure prophylaxis for all partners of participants available from the trial and access to rapid HIV viral load and CD4 monitoring. For ATI trials to be designed and implemented through an equity lens, additional enhancements require meaningful community engagement and multidisciplinary researchers to understand contextually relevant needs. Furthermore, commitments to non-maleficence, an ethical principle underscoring obligations to prevent harm and promote wellbeing of participants, requires an intersectional perspective for understanding the complexities of gender, sexuality, race, age, and ability.10 Funders are also accountable and should invest in sociobehavioural, psychosocial, and community-based strategies embedded within ATI trials, including holistic approaches for trial implementation, execution, and beyond to ensure that people with HIV and affected communities remain engaged in HIV cure-related research.
Figure:
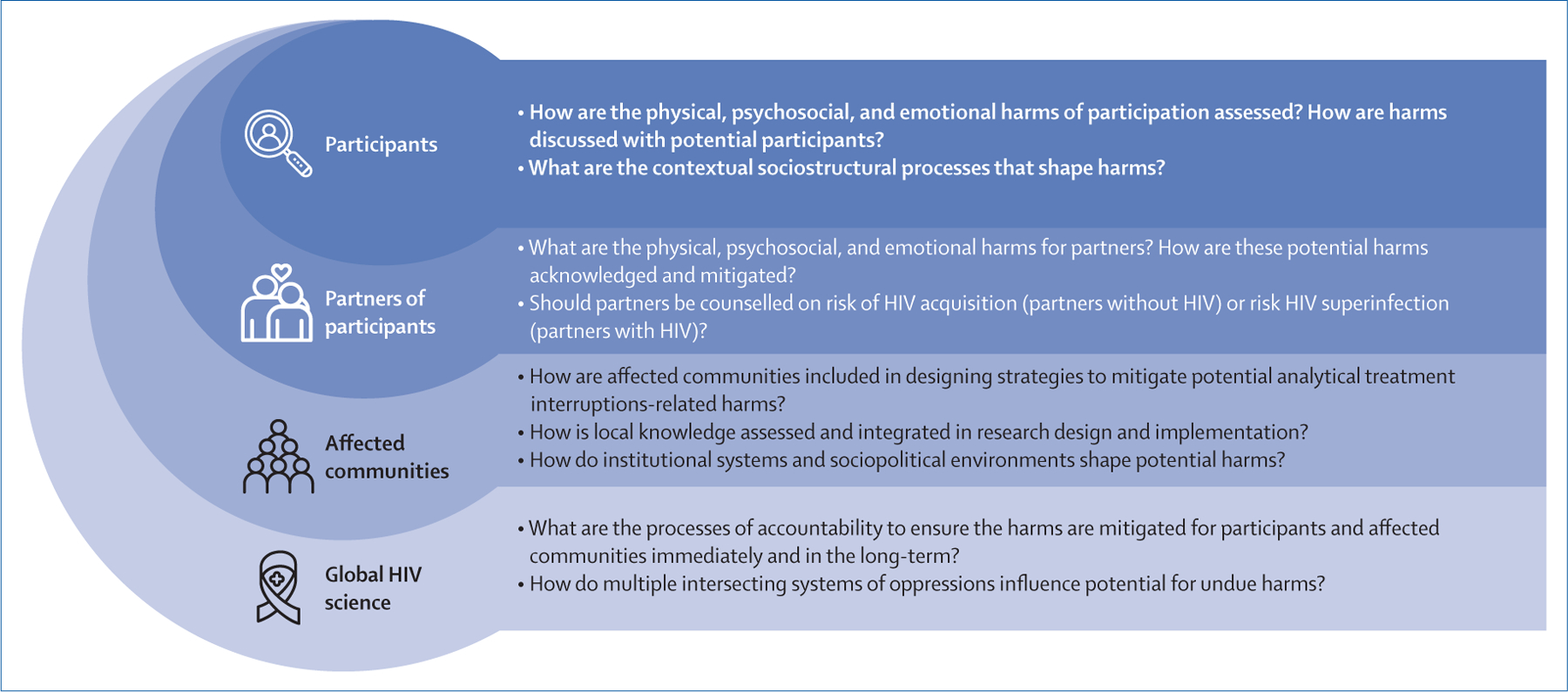
Key questions to mitigate potential harms related to HIV cure-related research with analytical treatment interruptions
A call for justice-informed HIV trials with ATIs demands acknowledgment of the geographical locations and communities that make this research possible. For example, in resource-restricted settings, how are risks minimised, benefits maximised, and accountability processes integrated? As ATI trials are scaled up, a clear roadmap for prioritising few but high quality and well-supported trials is essential. Given the promise of HIV cure, integrating community input into trial design and implementation, alongside comprehensive and evidence-based psychosocial support (eg, robust partner protections),7 is crucial for enhancing innovative and equitable research that centres participant and community wellbeing.
References
- 1.Villa TJ. An individual community member’s perspective on HIV cure-related research. HIV Res Clin Pract 2023; 24: 2249690. [PubMed] [Google Scholar]
- 2.Julg B, Dee L, Ananworanich J, et al. Recommendations for analytical antiretroviral treatment interruptions in HIV research trials-report of a consensus meeting. Lancet HIV 2019; 6: e259–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li JZ, Aga E, Bosch RJ, et al. Time to viral rebound after interruption of modern antiretroviral therapies. Clin Infect Dis 2021; 74: 865–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bilger A, Plenn E, Barg FK, et al. Participant experiences in HIV cure-directed trial with an extended analytical treatment interruption in Philadelphia, United States. HIV Res Clin Pract 2023; 24: 2267825. [PMC free article] [PubMed] [Google Scholar]
- 5.Richart V, Fernández I, de Lazzari E, et al. High rate of long-term clinical events after antiretroviral therapy resumption in HIV-positive patients exposed to antiretroviral therapy interruption. AIDS 2021; 35: 2463–68. [DOI] [PubMed] [Google Scholar]
- 6.De Scheerder MA, van Bilsen WPH, Dullaers M, Martinez-Picado J, Davidovich U, Vandekerckhove L. Motivations, barriers and experiences of participants in an HIV reservoir trial. J Virus Erad 2021; 7: 100029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dubé K, Morton T, Fox L, et al. A partner protection package for HIV cure-related trials involving analytical treatment interruptions. Lancet Infect Dis 2023; 23: e418–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubé K, Agarwal H, Stockman JK, et al. “I would absolutely need to know that my partner is still going to be protected”: perceptions of HIV cure-related research among diverse HIV serodifferent couples in the United States. AIDS Res Hum Retroviruses 2023; 39: 400–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dubé K, Barr E, Philbin M, et al. Increasing the meaningful involvement of women in HIV cure-related research: a qualitative interview study in the United States. HIV Res Clin Pract 2023; 24: 2246717. [PMC free article] [PubMed] [Google Scholar]
- 10.Dubé K, Kanazawa J, Campbell C, et al. Considerations for increasing racial, ethnic, gender, and sexual diversity in HIV cure-related research with analytical treatment interruptions: a qualitative inquiry. AIDS Res Hum Retroviruses 2022; 38: 50–63. [DOI] [PMC free article] [PubMed] [Google Scholar]


