Abstract
Background:
Nicotine and tobacco product (NTP) and cannabis use are common in adolescence/young adulthood and increase risk for negative psychosocial outcomes. This study investigated associations among adolescent/young adults’ initial experiences with NTPs, lifetime frequency of substance use, substance-related problems, and mental health symptoms.
Method:
Adolescents/young adults enrolled in a study on NTP and cannabis use were asked at what age they initated use of NTPs and were assigned to groups based on which product/substance(s) they reported using at the earliest age. Participants who reported use of NTPs (in isolation, without cannabis) first (N=78, “NTP-only”), simultaneous use of NTPs and cannabis first (e.g., blunt or bowl; N=25, “Simult-only”), use of both NTPs in isolation and simultaneous use at the same age (N=48, “NTP+Simult”), and no NTP use (N=53, “NTP-naïve”) were compared on substance use, substance-related problems, and mental health symptoms.
Results:
Groups differed on lifetime frequency of NTP, simultaneous, and cannabis use, with NTP users reporting more substance use episodes and substance-related problems than the NTP-naïve group. Lifetime frequency of cannabis use did not differ across NTP use groups. NTP use was associated with increased anxiety and depression, with no significant differences between groups.
Conclusions:
Adolescents/young adults who use nicotine may be at increased risk for greater nicotine use and mental health consequences, but initiating NTP use simultaneously with cannabis may not increase risk of negative outcomes above and beyond nicotine initation. Prospective longitudinal research is needed to establish temporal associations between first used NTP/cannabis products and relevant outcomes.
Keywords: nicotine, cannabis, adolescence, young adulthood, co-use
Introduction
Nicotine and tobacco product (NTP) use is alarmingly prevalent among U.S. adolescents and young adults, with over 2 million high school students reporting current use of NTPs (Gentzke et al., 2022). The landscape of youth NTP and substance use has changed rapidly over the past decade with the increased popularity of vaping devices and legalization of cannabis for recreational use by those over age 21 in nearly half of U.S. states (Johnston et al., 2022). NTPs and cannabis are now among the most commonly used substances in adolescence and early adulthood, aside from alcohol (Johnston et al., 2022). The 2021 Monitoring the Future study found that youth cannabis use has reached historic highs, with 43% of high school seniors reporting use within the past year and 29% use within the past 30 days. Although NTP use decreased slightly from its peak in 2019, in 2021 nearly 20% of high school seniors reported current use of e-cigarettes, with a quarter of those using daily, and approximately 4% reported current cigarette use (Johnston et al., 2022).
Although many prior studies have focused on single substance use, co-use of NTPs and cannabis, defined as use of both substances within a given time period (e.g., 30 days; Tucker et al., 2019), and sometimes also referred to as concurrent use, is alarmingly prevalent, with about 1-in-5 young adults in the U.S. reporting past month use of both substances (Cohn et al., 2019). Prior research shows that use of one substance confers greater risk for using the other. Young adults who use NTPs are more likely to initiate or increase use of cannabis (Agrawal et al., 2008, 2012; Berg et al., 2015; Lai et al., 2000; Saddleson et al., 2015) and those who initiate cannabis use are more likely to subsequently report increased use of NTPs (Agrawal et al., 2008, 2012; Behrendt et al., 2012; Cohn et al., 2019; Tucker et al., 2019; Tullis et al., 2003). Further, co-use is associated with greater addiction severity characteristics among adolescents and young adults, with co-users reporting heavier use of and greater dependence on both substances, along with worse treatment outcomes and unsuccessful cessation attempts (Abrantes et al., 2009; Ford et al., 2002; Ramo et al., 2013; Tullis et al., 2003; Vogel et al., 2018).
Adolescents and young adults who co-use NTPs and cannabis are at elevated risk of poorer psychosocial and health outcomes. Prior research has identified a number of problems related to NTP and cannabis co-use, including worse mental health (e.g., symptoms of anxiety and depression), increased use of alcohol and illicit drugs, exposure to smoke-related toxins, legal problems, and poor academic achievement (Georgiades & Boyle, 2007; Hernández-Serrano et al., 2018; Meier & Hatsukami, 2016; Moore & Budney, 2001; Peters et al., 2014; Ramo et al., 2013; Smith et al., 2021). In accordance with well-established detrimental effects of isolated cannabis (e.g., Squeglia et al., 2009) and nicotine (e.g., Yuan et al., 2015) use on the developing brain, emerging evidence suggests that co-use may have harmful effects on adolescent brain development, which may impact cognitive functioning into adulthood (e.g., Hernandez Mejia et al., 2021). Further, although most research on cannabis and NTPs has focused on substance co-use, evidence suggests that sequential (i.e., back-to-back use of both substances within a single occasion, episode, or session of substance use) and simultaneous (i.e., consuming both substances at the same time by mixing them togther, such as in a blunt or a bowl) use are indicative of increased harms, including worse mental and physical health and behavioral delinquency, relative to use of products on separate occasions (Tucker et al., 2019).
Despite the troubling prevalence of NTP and cannabis use, relatively little is known about the topography and development of co-use, specifically regarding how patterns of early NTP use impact later substance use and psychosocial outcomes. Regarding outcomes of use, extant research suggests that early use of NTPs may constitute a “gateway” (e.g., Kandel & Kandel, 2015; Patton et al., 2005) to cannabis use, as well as heavier use or riskier routes of cannabis and other substance administration. A longitudinal study of 16–21-year-olds found that adolescents who progressed to persistent NTP and cannabis co-use earlier were at increased risk for eventual problematic substance use than those who only used one substance or who initiated co-use later (Dunbar et al., 2020). In addition to reporting heavier use of cannabis, combustible products, and products containing both nicotine and cannabis (e.g., blunts, spliffs), early concurrent users were more likely to report use of multiple types of cannabis and NTP products (e.g., both vaping and consuming cannabis edibles), sequential use, and simultaneous use in early adulthood (Dunbar et al., 2020).
In sum, prior research demonstrates that early experiences with NTPs and cannabis during adolescence/young adulthood predicts increased substance use and riskier patterns of use (e.g., simultaneous use; use of combustible products). We aimed to extend previous research by investigating whether adolescent/young adults’ first used NTP was associated with patterns of NTP and cannabis use and psychosocial correlates of substance use. Participants were asked to report at what age they first used NTPs, both solely (i.e., in isolation, without cannabis) and simultaneously with cannabis (i.e., within the same discrete episode or session of use), and were assigned to groups based on the substance(s) that they reported using at the youngest age. Specifically, participants were differentiated into those who used NTPs at the earliest age, those who used NTPs and cannabis simultaneously in the same session (e.g., blunts, bowls) at the earliest age, those who used both NTPs and simultaneous products at the same age (i.e., within the same year), and those who have never used NTPs.
We hypothesized that participants who used NTPs and cannabis simultaneously first would report greater lifetime use of each product compared to those who used NTPs in isolation first or those who have not used NTPs. In addition, we expected that participants who reported NTP use, in isolation or simultaneously with cannabis, would report more symptoms of anxiety, depression, and stress than those who had not used NTPs.
Methods
Study Design
Data for this report were taken from an ongoing project investigating the effects of cannabis and nicotine use on adolescent/young adult brain development. As previously reported (e.g., Anonymous, 2020, 2022) participants (N=204; ages 16–22) were recruited from San Diego County via electronic and physical flyers posted on social media sites, and at high schools, four-year universities, and community colleges. Because the parent study focuses on co-use of nicotine and cannabis, participants recruited for the study were individuals who reported frequent (≥ 1 ×/week on average) use of NTPs and/or cannabis, as well as a group of individuals who reported minimal (≤15 episodes of cannabis and of NTP use in the past 6 months) use (see Anonymous et al., 2020 for group inclusion details).
To be eligible to enroll in the parent study, participants had to be between the ages of 16 and 22 and meet the criteria for one of the substance use categories described above. Exclusion criteria included current or past DSM-5 psychiatric disorder other than tobacco and/or cannabis use disorder; lifetime illicit substance use >10 times (excluding cannabis, which is legal in the state where the study was conducted); acute influence of alcohol or cannabis at testing (confirmed with breathalyzer, urine, and oral fluid toxicology); current use of psychoactive medications (including prescription antidepressants and anxiolytics), major medical issues, or history of developmental disability or prenatal substance exposure.
Individuals aged 18 years or older provided verbal informed consent prior to the screening. For those younger than 18, permission was obtained from their parent or legal guardian before receiving verbal assent to participate from the youth.After providing written informed consent in accordance with the University of California, San Diego Human Research Protections Program, participants underwent a single laboratory visit which included a thorough demographic, psychological, and substance use interview, neurocognitive assessment, and magnetic resonance imaging scan session. Participants were asked to refrain from alcohol use for 24 hours and cannabis use for 12 hours prior to the appointment, which was verified by oral fluid, urine, and breathalyzer (for alcohol). To avoid withdrawal effect contamination during assessment, NTP use was not restricted prior to testing. No participants screened positive for alcohol or any illicit substances.
Measures
Sociodemographics
As described by Anonymous (2020, 2022), a demographic and psychosocial interview was conducted to assess background information on socioeconomic status (with maternal education as a proxy), education, race/ethnicity, and medical history.
Substance Use History and Problems
A modified version of the Customary Drinking and Drug Use Record structured interview (CDDR; Brown et al., 1998; Jacobus et al., 2018; Karoly, Schacht, Jacobus, et al., 2019; Karoly, Schacht, Meredith, et al., 2019) was used to assess detailed NTP, simultaneous NTP and cannabis use, and cannabis use in isolation. Participants were asked to provide age of initiation of use for each substance, as well as an estimate of the number of times that they have used each substance thus far in their lifetime (henceforth referred to as “Lifetime Use”). Participants who used combustible products (e.g., cigarettes) were instructed to report the number of full or partial cigarettes smoked, while those who used electronic nicotine delivery systems (ENDS; e.g., e-cigarettes or vaporizers) were instructed to report “use occasions” or “episodes,” separated by engaging in some other activity after puffing on an ENDS/times the ENDS products were put down and picked up. Substance related problems were assessed via the Marijuana Adolescent Problems Inventory (MAPI; Johnson & White, 1989) and Hooked on Nicotine Checklist (HONC; DiFranza et al., 2002).
Substance initiation groups were defined by earliest age of initiation of each substance use category reported on the CDDR, which could include one or multiple products and/or methods of use (Brown et al., 1988). Participants were each assigned to one of the following groups: NTP-only (used NTPs in isolation first), Simult-only (used NTPs and cannabis simultaneously in the same session, e.g., blunts, bowls, spliffs first), NTP+Simult (used NTPs in isolaton and NTPs and cannabis simultaneously at the same age), and NTP-naïve (never used NTPs). Participants who reported using cannabis, but never NTPs, were included in the NTP-naïve group.
Mental Health
Participants completed a series of self-report measures to assess mental health and emotional states. The 21 item version of the Depression, Anxiety and Stress Scale (DASS-21) was administered to assess depression, anxiety, and stress symptomology (Lovibond & Lovibond, 1995). The Beck Depression Inventory (BDI-II; Beck et al., 1996) was administered to measure depression symptoms. The State-Trait Anxiety Inventory (STAI; Spielberger et al., 1970) was administered to measure participants’ state of anxiety on the day of the assessment.
Statistical Analysis
SPSS Version 26.0 software was used for all analyses. Substance use quantities were log transformed to reduce skewness of the distributions. Group differences were investigated via ANOVA, ANCOVA, multinomial logistic regression, or independent χ² with a p < .05 statistical significance threshold. Pairwise Z-Tests with Bonferroni correction were conducted on significant χ² results to identify specific group differences. For ANCOVA models, pairwise comparisons were conducted on the estimated marginal means (EMMs) with Bonferroni correction. Age and self-reported biological sex were included as covariates in all analyses. Figures were made using the ggplot2 package in R (Wickham, 2011).
Results
Participant Characteristics
Demographic information is presented in Table 1. Across groups, the sample was 52.9% male, 50.0% White, 38.7% Hispanic, and average age was 19.44 years (SD = 1.58). Substance use groups were found to differ on age, sex, years of education, and age of substance use initiation (see Table 1 for group differences). All substance use groups were older and had completed more years of education than the NTP-naïve group. Among substance use groups, the NTP+Simult group was the oldest and reported the latest age of NTP initiation, with the NTP-only group initiating NTP use at a younger age than the other groups. Regarding gender, the NTP+Simult group included a larger percentage of male participants than the NTP-naïve group, with no other differences between groups.
Table 1.
Sample demographics and group differences
| Variable | Group (mean (SD) or %) | p value | |||
|---|---|---|---|---|---|
| NTP-only (N=78) | Simult-only (N=25) | NTP+Simult (N=48) | NTP-naïve (N=53) | ||
| Age | 19.74 (1.42)c | 19.12 (1.33)d | 19.88 (1.57)d,f | 18.75 (1.71)c,f | <.001 |
|
| |||||
| % Male | 55.1 | 56.0 | 66.7f | 35.8f | .02 |
|
| |||||
| Race | <.001 | ||||
| Asian | 20.5 | 4.0e | 18.8 | 34.0e | |
| White | 59.0a | 28.0a | 50.0 | 47.2 | |
| More than one race | 20.5 | 44.0e | 27.1 | 15.1e | |
| Other | 0.0a | 24.0a,d | 4.2d | 3.8 | |
|
| |||||
| % Non-Hispanic | 59.0 | 28.0 | 50.0 | 47.2 | .06 |
|
| |||||
| % Hispanic | 33.3 | 52.0 | 39.6 | 39.6 | .42 |
|
| |||||
| Education Years Completed | 13.28 (1.34)c | 12.76 (1.30) | 13.21 (1.32)f | 12.49 (1.71)c,f | .01 |
|
| |||||
| Age of NTP Initiation | 16.09 (1.98)b | 16.64 (2.20) | 17.48 (1.47)b | - | <.001 |
|
| |||||
| Mother’s Education (% Bachelors or above) | 40.9 | 56.0 | 57.8 | 71.6 | .51 |
|
| |||||
| Past Month NTP Use | 108.14 248.04) | 79.92 (171.46) | 153.19 (347.50) | - | .595 |
|
| |||||
| Past Month Cannabis Use | 30.03 (36.35) | 22.60 (21.10) | 49.19 (116.41) | 8.29 (16.05) | .163 |
|
| |||||
| Past Month Simult Use | 9.28 (21.66) | 9.24 (14.39) | 12.10 (21.03) | 0.0 (0.0) | .251 |
|
| |||||
| Lifetime NTP use | 4170.6 (11,577.3)c | 731.2 (2,544.2) | 2,982.7 (5,310.5) | 0.0 (0.0)c | .015 |
|
| |||||
| Lifetime Cannabis use | 795.0 (1,451.0)c | 589.8 (672.1) | 1,130.4 (2,246.7)f | 26.7 (129.9)c,f | <.001 |
|
| |||||
| Lifetime Simult use | 206.0 (547.8)c | 214.9 (411.7)e | 248.2 (522.3)f | 0.0 (0.0)c,e,f | .022 |
Note: NTP = “Nicotine and tobacco product”); bolded subscripts a-f indicate statistically significant results for the following between group comparisons:
NTP-only vs. Simult-only,
NTP-only vs. NTP+Simult,
NTP-only vs. NTP-naïve,
Simult-only vs. NTP+Simult,
Simult-only vs. NTP-naïve,
NTP+Simult vs. NTP-naïve
Substance Use History and Problems
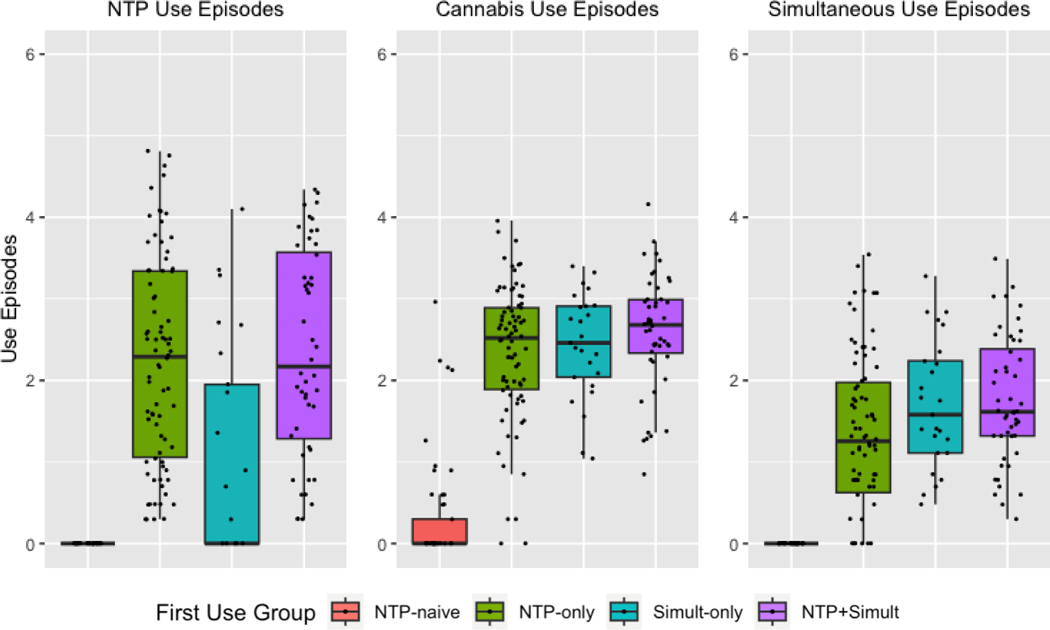
Group differences were observed on lifetime NTP use [F (3,198) = 41.84, p <.001, η2 = .39], simultaneous use [F (3,198) = 45.12, p <.001, η2 = .41], and cannabis use [F (3,198) = 58.78, p <.001, η2 = .47]. See Table 2 and Figure 1 for estimated marginal means from the ANCOVA models. Groups differed on the MAPI [F (3,198) = 13.19, p <.001; η2 = .17], with the use groups reporting significantly more problems related to cannabis use (NTP-only EMM = 35.64, SE = 1.12; Simult-only EMM = 37.96, SE = 2.08; NTP+Simlult EMM= 35.92, SE = 1.57) as compared to the NTP-naïve group (EMM = 25.22, SE = 1.50; all ps <.001). Groups also differed on the HONC [F (3,198) = 7.61, p <.001; η2 = .17], where the NTP-only (EMM = 2.80, SE = .33) and NTP+Simult (EMM = 2.74, SE = .58) groups reported more nicotine related problems than the NTP-naïve group (EMM = .38, SE = .42), while the Simult-only group reported marginally less problems than the other use groups (ps <.10). No other group differences were observed for lifetime substance use or substance use problems.
Table 2.
Lifetime substance use estimated marginal means derived from ANCOVA models controlling for age and sex
| Variable | Group (Estimated marginal means (SE)) | p value | |||
|---|---|---|---|---|---|
| NTP-only (N=78) | Simult-only (N=25) | NTP+Simult (N=48) | NTP-naïve (N=53) | ||
| Lifetime NTP Use | 2.19 (.12)a,c | 1.06 (.22)a,d,e | 2.26 (.16)d,f | .14 (.16)c,e,f | <.001 |
|
| |||||
| Lifetime Simult Use | 1.29 (.09)b,c | 1.73 (.15)e | 1.71 (.11)b,f | .07 (.11)c,e,f | <.001 |
|
| |||||
| Lifetime Cannabis Use | 2.10 (.09)c | 2.25 (.16)e | 2.31 (.12)f | .38 (.12)c,e,f | <.001 |
Note: NTP = “Nicotine and tobacco product”; bolded subscripts a-f indicate statistically significant results for the following between group comparisons:
NTP-only vs. Simult-only,
NTP-only vs. NTP+Simult,
NTP-only vs. NTP-naïve,
Simult-only vs. NTP+Simult,
Simult-only vs. NTP-naïve,
NTP+Simult vs. NTP-naïve (Bonferroni corrected p < .05).
Fig 1. Differences in lifetime NTP, cannabis, and simultaneous product use episodes between first used product groups.
Note: ***p < .001; ** p <.05, NS = not significant. The NTP-naïve group differed from all subtstance use groups at the p <.001 level for all types of substance use. Bars represent 95% confidence intervals. Dots represent individual data points. NTP = “Nicotine and Tobacco Product”
Mental Health
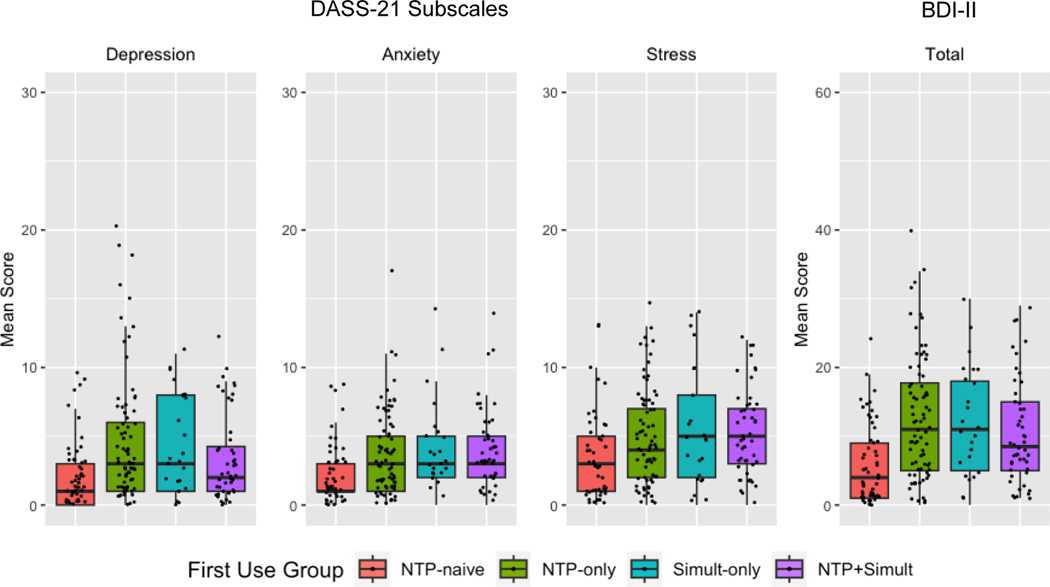
Group differences were observed on the DASS-21 Depression subscale [F (3,198) = 4.25, p < .01, η2 = .06], Anxiety subscale [F (3,198) = 3.54, p = .02, η2 = .05], and Stress subscale [F (3,198) = 3.56, p = .02, η2 = .05]. However, inspection of the pairwise differences revealed differences between the NTP-naïve and use groups only: Depression – NTP-only (EMM = 4.50, SE = .43) vs. NTP-naïve (EMM = 2.18; SE = .53; p <.01), Anxiety – NTP+Simult (EMM = 3.93, SE = .43) vs. NTP-naïve (EMM = 2.23; SE = .42; p =.04), and Stress – NTP+Simult (EMM = 5.30, SE = .51) vs. NTP-naïve (EMM = 3.23; SE = .50; p =.03). Other comparisons between the NTP-naïve and use groups had similar mean difference magnitudes but did not meet the significance threshold after Bonferroni correction (ps < .12). Group differences were also observed on the BDI-II total score [F (3,198) = 7.90, p < .001, η2 = .11], where the NTP-naïve group (EMM = 5.87, SE = 1.09) was found to differ from all use groups (NTP-only EMM = 12.48, SE = .87, p < .001; Simult-only EMM = 12.12, SE = 1.53, p < .01; NTP+Simult EMM= 10.86, SE = 1.12, p = .01). See Figure 2 for group differences. No group differences were observed on the STAI [F (3,198) = 0.93, p = .43].
Fig 2. Differences in self-reported mental health symptomatology on the DASS-21 and BDI-II between first used product group.
Note: ***p < .001; ** p <.05, NS = not significant. There were no significant differences between substance use groups on any scales. Bars represent 95% confidence intervals. Dots represent individual data points. NTP = “Nicotine and Tobacco Product”
Discussion
Given widespread use of NTPs and cannabis, constantly evolving product availability, and changes in regulatory policy, it is critical to understand how adolescent/young adults’ early exposure to substances impacts patterns of use and outcomes into adulthood. In this preliminary report, we sought to investigate associations among adolescent/young adult nicotine users’ first used substance, lifetime substance use, and mental health symptoms. Results demonstrated that participants’ first used nicotine substances were related to lifetime use of that substance, which has potential implications for both future research and prevention efforts.
First used product was significantly associated with lifetime substance use. As expected, the NTP-only and NTP+Simult groups reported more independent lifetime NTP uses, which suggests that initial NTP use may continue to influence product choice through adolescence/young adulthood. Interestingly, all NTP use groups endorsed similar levels of lifetime cannabis use. Although this study was not designed to explicitly test the gateway hypothesis, this pattern of results is consistent with prior research demonstrating that NTP use may be associated with cannabis initiation (Agrawal et al., 2012; Lai et al., 2000). Because we did not distinguish between individuals who initially used cannabis products in isolation, we cannot make inferences about the “reverse gateway hypothesis,” which suggests that cannabis use may lead to initiation of NTPs and nicotine dependence (Agrawal et al., 2008; Patton et al., 2005). Prospective longitudinal studies are necessary to clarify the association between first used substance and patterns of substance use into early adulthood.
Overall, the NTP-only, Simult-only, and NTP+Simult groups did not significantly differ from one another with respect to cannabis or nicotine related problems, except that the Simult-only group reported fewer nicotine related problems than the NTP-only and NTP+Simult groups. This is somewhat expected since these participants did not initially engage in NTP use in isolation and also endorsed less overall lifetime NTP use than the NTP-only and NTP+Simult groups. Although anxiety, depression, and stress were not differentially associated with first used product, the NTP-only, Simult-only, and NTP+Simult groups all scored higher on measures of mental health symptomatology than NTP-naïve group, consistent with prior literature linking nicotine use to mental health (Cohn et al., 2018; Hindocha et al., 2021; Tucker et al., 2019).
To our knowledge, this study is the first to explore how first NTP/cannabis use is associated with lifetime substance use and mental health symptoms in adolescent/young adult nicotine users. Prior studies on this topic have focused exclusively on first used NTPs, comparing modes of delivery such as combustible products (e.g., cigarettes), ENDS, and smokeless tobacco. As cigarettes continue to fall out of favor among youth in the United States (Johnston et al., 2022), the majority of young adults report initially consuming nicotine via other products (Ross et al., 2018; Simon et al., 2023; Sutfin et al., 2015), yet combustible products remain the most common form of simultaneous cannabis and NTP use (Schauer et al., 2017; Tucker et al., 2019). The present study did not differentiate between different routes of NTP/cannabis administration. Although the inclusion of participants using a range of products may make results generalizable to more nicotine users (e.g., versus just cigarette smokers), use of combustible products is associated with increased nicotine dependence and poorer behavioral outcomes (Azagba et al., 2019; Martinez et al., 2009; Staff et al., 2020). Thus, future work on outcomes of first used NTP/cannabis products may benefit from differentiation between product types, specifically combustible products versus ENDS. Additionally, the present study focused on initial NTP and simultaneous NTP/cannabis use, without identifying initial sole use of cannabis. Future studies differentiating first use of sole cannabis products are necessary to understand the influence of first sole cannabis use on psychosocial outcomes.
The association between first used NTP product and lifetime use is consistent with extant literature testing nicotine and cannabis use trajectories within adolescent/young adult populations. Although these studies have not explicitly tested adolescent/young adults’ first used products, results have indicated that high risk patterns of cannabis and NTP use (i.e., sequential or simultaneous use) are often initiated by early adulthood and are associated with addiction severity and poorer psychosocial outcomes (Dunbar et al., 2020; Lanza et al., 2021; Tucker et al., 2019). The results of the present study suggest that adolescents’ first used NTP and/or cannabis product may impact ongoing product use; however, we did not find predicted differences in mental health symptoms based on first used product. One possible explanation for this finding is a lack of variability in substance use patterns at the time of testing. Because the larger study targeted adolescents/young adults who co-use subtances, the majority of the sample, regardless of first used product, reported using both NTPs and cannabis upon enrollment. It is possible that inclusion of participants who continued to use only NTPs or cannabis in isolation would have resulted in more variability in mental health symptoms. Another potential explanation is the exclusion of youth taking psychotropic medications, which likely limited mental health symptomatology in the sample. Given well-documented associations between substance use and psychopathology in adolescents and young adults (Saban & Flisher, 2010), future research should assess use trajectories in populations with a broader range of mental health functioning to increase generalizability.
The finding that first used NTP/cannabis product is associated with lifetime substance use has potential implications for both research and prevention efforts. Although few existing studies have explicitly reported on participants’ first used substances, our results suggest that adolescent/young adult’s earliest NTP use experiences may influence future use. Researchers using longitudinal methods to study trajectories of substance use should consider asking participants to report on their first used substances to aid in determining whether these early experiences have more distal consequences on use and psychosocial outcomes. If this is the case, researchers might also consider whether other factors (e.g., family history of substance use, genetics) might predispose adolescents/young adults to initiate different substances or combinations thereof. Our findings also have potential implications for prevention and harm reduction efforts. There are established links between certain types of substance use and increased negative outcomes (e.g., for simultaneous NTP and cannabis use; (Tucker et al., 2019). If the association between initial and ongoing simultaneous use can be prospectively established, then targeted efforts to prevent or delay simultaneous product use in adolescence/early adulthood could be especially beneficial. Science-based psychoeducational prevention programs for youth (e.g., Just Say Know; Squeglia et al., 2021) could incorporate findings related to first used substances and consequences into their curriculum. The results of the present study represent a crucial first step towards understanding how first used NTP/cannabis products influence outcomes in ways that can benefit future research and preventations efforts.
This study should be considered in the context of its limitations. The cross-sectional nature of the data makes it impossible to test directional hypotheses relating first used cannabis/NTP product to later substance use and psychosocial outcomes, although the inherent temporality of the first use question is suggestive of directional outcomes. Regardless, additional factors beyond first product use likely play a substantial role in substance use over time (e.g., peer use, availability, parental monitoring). The design of the present study precludes testing of temporal associations between any of these variables, and longitudinal data are necessary to establish prospective associations among initial product use, mental health, and neuropsychological functioning into adulthood. As noted previously, we did not distinguish between modes of delivery (e.g., combustible products vs. ENDS), which have been linked to co-use behaviors (Agrawal & Lynskey, 2009), thus limiting our ability to disentangle effects of substance type from mode of delivery. This study was retrospective in nature, which introduces the possibility of recall bias for both age of initiation and lifetime substance use. However, the impact of this issue is likely mitigated by the relatively young age of the sample and limited time of recall and, as such, is not a major area of concern. Finally, the study sample was predominantly White, and results may not generalize to more racially diverse samples.
This study is the first to test how adolescent/young adult nicotine users’ first used substance relates to outcomes, including lifetime individual and simultaneous use of NTPs and cannabis, and mental health symptoms. The results add to previous investigations of first used NTPs by considering simultaneous use with cannabis, which is increasingly common within adolescents/young adults and is linked to adverse health and psychosocial outcomes. Longitudinal studies that prospectively test the impact of first used cannabis/nicotine products on developmental trajectories of substance use are necessary to understand the consequences of substance co-use on health and psychosocial outcomes in adulthood.
Funding:
This work was supported by the National Institute on Drug Abuse (U01 DA041089, R21 DA047953), the California Tobacco-Related Disease Research Grants Program Office of the University of California (580264 and T30IP0962), and the National Institute on Alcohol Abuse and Alcoholism (T32 AA013525).
Footnotes
Declaration of interest: none
Disclosure of interest
The authors report no conflict of interest.
References
- Abrantes AM, Lee CS, MacPherson L, Strong DR, Borrelli B, & Brown RA (2009). Health risk behaviors in relation to making a smoking quit attempt among adolescents. Journal of Behavioral Medicine, 32(2), 142–149. 10.1007/s10865-008-9184-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Budney AJ, & Lynskey MT (2012). The co-occurring use and misuse of cannabis and tobacco: A review: Cannabis and tobacco review. Addiction, 107(7), 1221–1233. 10.1111/j.1360-0443.2012.03837.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, & Lynskey MT (2009). Tobacco and cannabis co-occurrence: Does route of administration matter? Drug and Alcohol Dependence, 99(1–3), 240–247. 10.1016/j.drugalcdep.2008.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Madden PAF, Bucholz KK, Heath AC, & Lynskey MT (2008). Transitions to regular smoking and to nicotine dependence in women using cannabis. Drug and Alcohol Dependence, 95(1–2), 107–114. 10.1016/j.drugalcdep.2007.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azagba S, Latham K, & Shan L. (2019). Cigarette, smokeless tobacco, and alcohol use among transgender adults in the United States. International Journal of Drug Policy, 73, 163–169. 10.1016/j.drugpo.2019.07.024 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown G. (1996). Beck depression inventory–II. Psychological Assessment.
- Behrendt S, Beesdo-Baum K, Höfler M, Perkonigg A, Bühringer G, Lieb R, & Wittchen H-U (2012). The relevance of age at first alcohol and nicotine use for initiation of cannabis use and progression to cannabis use disorders. Drug and Alcohol Dependence, 123(1–3), 48–56. 10.1016/j.drugalcdep.2011.10.013 [DOI] [PubMed] [Google Scholar]
- Berg CJ, Stratton E, Schauer GL, Lewis M, Wang Y, Windle M, & Kegler M. (2015). Perceived Harm, Addictiveness, and Social Acceptability of Tobacco Products and Marijuana Among Young Adults: Marijuana, Hookah, and Electronic Cigarettes Win. Substance Use & Misuse, 50(1), 79–89. 10.3109/10826084.2014.958857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, & Vik PW (1998). Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol, 59(4), 427–438. [DOI] [PubMed] [Google Scholar]
- Cohn AM, Abudayyeh H, Perreras L, & Peters EN (2019). Patterns and correlates of the co-use of marijuana with any tobacco and individual tobacco products in young adults from Wave 2 of the PATH Study. Addictive Behaviors, 92, 122–127. 10.1016/j.addbeh.2018.12.025 [DOI] [PubMed] [Google Scholar]
- Cohn AM, Johnson AL, Rose SW, Pearson JL, Villanti AC, & Stanton C. (2018). Population-level patterns and mental health and substance use correlates of alcohol, marijuana, and tobacco use and co-use in US young adults and adults: Results from the population assessment for tobacco and health: Population-Level Patterns of Substance Use and Co-Use. The American Journal on Addictions, 27(6), 491–500. 10.1111/ajad.12766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney KE, Baca R, Doran N, Jacobson A, Liu TT, & Jacobus J. (2020). The effects of nicotine and cannabis co-use during adolescence and young adulthood on white matter cerebral blood flow estimates. Psychopharmacology, 237, 3615–3624. 10.1007/s00213-020-05640-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney KE, Sorg S, Baca R, Doran N, Jacobson A, Liu A, & Jacobus TT (2022). The Effects of Nicotine and Cannabis Co-Use During Late Adolescence on White Matter Fiber Tract Microstructure. Journal of Studies on Alcohol and Drugs 83(2), 287–295. 10.15288/jsad.2022.83.287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranza JR, Savageau JA, Fletcher K, Ockene JK, Rigotti NA, McNeill AD, Coleman M, & Wood C. (2002). Measuring the Loss of Autonomy Over Nicotine Use in Adolescents: The DANDY (Development and Assessment of Nicotine Dependence in Youths) Study. Archives of Pediatrics & Adolescent Medicine, 156(4), 397. 10.1001/archpedi.156.4.397 [DOI] [PubMed] [Google Scholar]
- Dunbar MS, Davis JP, Tucker JS, Seelam R, Shih RA, & D’Amico EJ (2020). Developmental Trajectories of Tobacco/Nicotine and Cannabis Use and Patterns of Product Co-use in Young Adulthood. Tobacco Use Insights, 13, 1179173X2094927. 10.1177/1179173X20949271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford DE, Vu HT, & Anthony JC (2002). Marijuana use and cessation of tobacco smoking in adults from a community sample. Drug and Alcohol Dependence, 67(3), 243–248. 10.1016/S0376-8716(02)00066-2 [DOI] [PubMed] [Google Scholar]
- Gentzke AS, Wang TW, Cornelius M, Park-Lee E, Ren C, Sawdey MD, Cullen KA, Loretan C, Jamal A, & Homa DM (2022). Tobacco Product Use and Associated Factors Among Middle and High School Students—National Youth Tobacco Survey, United States, 2021. MMWR. Surveillance Summaries, 71(5), 1–29. 10.15585/mmwr.ss7105a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiades K, & Boyle MH (2007). Adolescent tobacco and cannabis use: Young adult outcomes from the Ontario Child Health Study. Journal of Child Psychology and Psychiatry, 48(7), 724–731. 10.1111/j.1469-7610.2007.01740.x [DOI] [PubMed] [Google Scholar]
- Hernandez Mejia M, Wade NE, Baca R, Diaz VG, & Jacobus J. (2021). The Influence of Cannabis and Nicotine Co-use on Neuromaturation: A Systematic Review of Adolescent and Young Adult Studies. Biological Psychiatry, 89(2), 162–171. 10.1016/j.biopsych.2020.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Serrano O, Gras M, & Font-Mayolas S. (2018). Concurrent and Simultaneous Use of Cannabis and Tobacco and Its Relationship with Academic Achievement amongst University Students. Behavioral Sciences, 8(3), 31. 10.3390/bs8030031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindocha C, Brose LS, Walsh H, & Cheeseman H. (2021). Cannabis use and co‐use in tobacco smokers and non‐smokers: Prevalence and associations with mental health in a cross‐sectional, nationally representative sample of adults in Great Britain, 2020. Addiction, 116(8), 2209–2219. 10.1111/add.15381 [DOI] [PubMed] [Google Scholar]
- Jacobus J, Taylor CT, Gray KM, Meredith LR, Porter AM, Li I, Castro N, & Squeglia LM (2018). A multi-site proof-of-concept investigation of computerized approach-avoidance training in adolescent cannabis users. Drug and Alcohol Dependence, 187, 195–204. 10.1016/j.drugalcdep.2018.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson V, & White HR (1989). An investigation of factors related to intoxicated driving behaviors among youth. Journal of Studies on Alcohol, 50(4), 320–330. [DOI] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2022). Monitoring the Future national survey results on drug use, 1975–2021: Overview, key findings on adolescent drug use.
- Kandel D, & Kandel E. (2015). The Gateway Hypothesis of substance abuse: Developmental, biological and societal perspectives. Acta Paediatrica, 104(2), 130–137. 10.1111/apa.12851 [DOI] [PubMed] [Google Scholar]
- Karoly HC, Schacht JP, Jacobus J, Meredith LR, Taylor CT, Tapert SF, Gray KM, & Squeglia LM (2019). Preliminary evidence that computerized approach avoidance training is not associated with changes in fMRI cannabis cue reactivity in non-treatment-seeking adolescent cannabis users. Drug and Alcohol Dependence, 200, 145–152. 10.1016/j.drugalcdep.2019.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karoly HC, Schacht JP, Meredith LR, Jacobus J, Tapert SF, Gray KM, & Squeglia LM (2019). Investigating a novel fMRI cannabis cue reactivity task in youth. Addictive Behaviors, 89, 20–28. 10.1016/j.addbeh.2018.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai S, Lai H, Page JB, & McCoy CB (2000). The Association Between Cigarette Smoking and Drug Abuse in the United States. Journal of Addictive Diseases, 19(4), 11–24. 10.1300/J069v19n04_02 [DOI] [PubMed] [Google Scholar]
- Lanza HI, Bello MS, Cho J, Barrington-Trimis JL, McConnell R, Braymiller JL, Krueger EA, & Leventhal AM (2021). Tobacco and cannabis poly-substance and poly-product use trajectories across adolescence and young adulthood. Preventive Medicine, 148, 106545. 10.1016/j.ypmed.2021.106545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Martinez JA, Muñoz García MA, & Sher KJ (2009). A new minimum legal drinking age (MLDA)? Some findings to inform the debate. Addictive Behaviors, 34(4), 407–410. 10.1016/j.addbeh.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier E, & Hatsukami DK (2016). A review of the additive health risk of cannabis and tobacco co-use. Drug and Alcohol Dependence, 166, 6–12. 10.1016/j.drugalcdep.2016.07.013 [DOI] [PubMed] [Google Scholar]
- Moore BA, & Budney AJ (2001). Tobacco smoking in marijuana-dependent outpatients. Journal of Substance Abuse, 13(4), 583–596. 10.1016/S0899-3289(01)00093-1 [DOI] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Carlin JB, Sawyer SM, & Lynskey M. (2005). Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence. Addiction, 100(10), 1518–1525. 10.1111/j.1360-0443.2005.01220.x [DOI] [PubMed] [Google Scholar]
- Peters EN, Schwartz RP, Wang S, O’Grady KE, & Blanco C. (2014). Psychiatric, psychosocial, and physical health correlates of co-occurring cannabis use disorders and nicotine dependence. Drug and Alcohol Dependence, 134, 228–234. 10.1016/j.drugalcdep.2013.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Delucchi KL, Hall SM, Liu H, & Prochaska JJ (2013). Marijuana and Tobacco Co-Use in Young Adults: Patterns and Thoughts About Use. Journal of Studies on Alcohol and Drugs, 74(2), 301–310. 10.15288/jsad.2013.74.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross JC, Suerken CK, King JL, Wiseman KD, Noar SM, Wagoner KG, & Sutfin EL (2018). Adolescents’ First Tobacco Product: Results from a Nationally Representative Survey. Tobacco Regulatory Science, 4(3), 38–46. 10.18001/TRS.4.3.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saban A, & Flisher AJ (2010). The association between psychopathology and substance use in young people: A review of the literature. Journal of Psychoactive Drugs, 42(1), 37–47. [DOI] [PubMed] [Google Scholar]
- Saddleson ML, Kozlowski LT, Giovino GA, Hawk LW, Murphy JM, MacLean MG, Goniewicz ML, Homish GG, Wrotniak BH, & Mahoney MC (2015). Risky behaviors, e-cigarette use and susceptibility of use among college students. Drug and Alcohol Dependence, 149, 25–30. 10.1016/j.drugalcdep.2015.01.001 [DOI] [PubMed] [Google Scholar]
- Schauer GL, Rosenberry ZR, & Peters EN (2017). Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addictive Behaviors, 64, 200–211. 10.1016/j.addbeh.2016.09.001 [DOI] [PubMed] [Google Scholar]
- Simon P, Buta E, Jackson A, Camenga DR, Kong G, Morean ME, Bold KW, Davis DR, Krishnan-Sarin S, & Gueorguieva R. (2023). The first nicotine product tried is associated with current multiple nicotine product use and nicotine dependence among a nationally representative sample of U.S. youths. Preventive Medicine, 169, 107437. 10.1016/j.ypmed.2023.107437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, Gotway MB, Crotty Alexander LE, & Hariri LP (2021). Vaping-related lung injury. Virchows Archiv, 478(1), 81–88. 10.1007/s00428-020-02943-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, & Lushene RE (1970). The State-Trait Anxiety Inuentory (test manual). Consulting Psychologists Press. [Google Scholar]
- Squeglia LM, Jacobus J, & Tapert SF (2009). The Influence of Substance Use on Adolescent Brain Development. Clinical EEG and Neuroscience, 40(1), 31–38. 10.1177/155005940904000110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staff J, Maggs JL, Seto C, Dillavou J, & Vuolo M. (2020). Electronic and Combustible Cigarette Use in Adolescence: Links With Adjustment, Delinquency, and Other Substance Use. Journal of Adolescent Health, 66(1), 39–47. 10.1016/j.jadohealth.2019.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutfin EL, Sparks A, Pockey JR, Suerken CK, Reboussin BA, Wagoner KG, Spangler J, & Wolfson M. (2015). First tobacco product tried: Associations with smoking status and demographics among college students. Addictive Behaviors, 51, 152–157. 10.1016/j.addbeh.2015.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Rodriguez A, Dunbar MS, Pedersen ER, Davis JP, Shih RA, & D’Amico EJ (2019). Cannabis and tobacco use and co-use: Trajectories and correlates from early adolescence to emerging adulthood. Drug and Alcohol Dependence, 204, 107499. 10.1016/j.drugalcdep.2019.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tullis LM, Dupont R, Frost-Pineda K, & Gold MS (2003). Marijuana and Tobacco: A Major Connection? Journal of Addictive Diseases, 22(3), 51–62. 10.1300/J069v22n03_05 [DOI] [PubMed] [Google Scholar]
- Vogel EA, Rubinstein ML, Prochaska JJ, & Ramo DE (2018). Associations between marijuana use and tobacco cessation outcomes in young adults. Journal of Substance Abuse Treatment, 94, 69–73. 10.1016/j.jsat.2018.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H. (2011). Ggplot2. Wiley Interdisciplinary Reviews: Computational Statistics, 3(2), 180–185. [Google Scholar]
- Yuan M, Cross SJ, Loughlin SE, & Leslie FM (2015). Nicotine and the adolescent brain. The Journal of Physiology, 593(16), 3397–3412. 10.1113/JP270492 [DOI] [PMC free article] [PubMed] [Google Scholar]