Abstract
Introduction and importance:
Cecal foreign bodies are uncommon causes of acute abdomen, and their presentation can often mimic acute appendicitis (AA), making it challenging to diagnose. The authors present the case of a 12-year-old male from Ethiopia who initially presented with symptoms suggestive of AA. However, during surgery, the authors found a multiple magnetic fields result in perforation. This case highlights the importance of considering unusual etiologies.
Case presentation:
A 12-year-old boy with AA associated with anorexia, nausea, and low-grade fever was referred from a private clinic. Otherwise, no history of recent respiratory infection and diarrhea, and was previously in good health. The patient did not report any history of a foreign body (FB), even to his own family, and, except for himself, no one was aware of the ingested FB. The work has been reported in line with the Surgical CAse REport (SCARE) 2023 criteria.
Discussion:
In this case, the authors experienced multiple magnetic FB in the cecum, which were not observed on ultrasound (U/S). However, this case closely resembled appendicitis. U/S can aid in differentiation. However, it may not always identify the underlying etiology, specifically in a resource-limited setting.
Conclusion:
Based on the patient’s presentation, AA was diagnosed and emergency surgery was presumed to be inflamed. However, three magnetic FB were the underlying cause of the presentation, which created pressure on the cecal wall, and the authors successfully performed surgical management. This case reminds us of uncommon etiologies, such as magnets in patients with symptoms of appendicitis. This underscores the importance of an open-minded approach to unexpected findings during surgery.
Keywords: case report, cecal foreign body, cecal perforation, mimic acute appendicitis
Introduction
Highlights
Magnetic foreign bodies (MFB) are rare causes of acute abdominal pain, often mimicking symptoms of acute appendicitis, leading to diagnostic challenges.
The case involves a 12-year-old boy initially diagnosed with acute appendicitis; however, surgery resulted in three MFB causing perforation, highlighted the difficulty in diagnosis.
The patient did not disclose any history of ingesting a MFB, making the diagnosis more challenging, as even close family members were unaware of the incident.
Ultrasonography (U/S) failed to detect the three MFB, emphasizing the limitations of certain imaging alone, particularly in resource-limited settings, where highly digitalized ultrasound not found.
The case underscores the importance of an open-minded approach to unexpected findings during surgery.
Family should follow their children, where and what they have been doing on a day-to-day basis through smooth and free communication.
Acute abdominal pain is a common presentation in pediatric patients and can have various underlying causes1,2. Acute appendicitis (AA) is one of the most frequent surgical emergencies in both children and adolescents, with a common clinical presentation of right lower quadrant (RLQ) pain accompanied by anorexia, nausea, and vomiting3. However, not all RLQ pain cases have been attributed to AA4. Unusual etiologies should be considered, specifically in children and adolescents with such clinical presentations, to avoid complications5. The incidence of AA in developed nations is estimated to be ~0.001 per thousand6. This may be more so than in the developing regions.
Evidence shows that foreign bodies (FB) are the rarest possible cause of AA, specifically in adolescents, although the majority of FB cases pass through the gastrointestinal tract without causing symptoms or complications7–9. Less than 1% of FB that enter the lumen of the appendix (vermiform appendix) result in hemorrhage and perforation, which result in complications and surgery7. Patients management depends on the clinical presentation, as well as the duration, sharpness, size, shape, and location of the FB3,5,7. Some case reports have described FB that may mimic appendicitis, such as screws, seeds, tongue piercing, needles, toothpicks, hair, and plant materials7,10. More than 80% of the cases pass spontaneously, while ~20% can be removed endoscopically and with surgical intervention (Ambe et al., 2012; Arztebl Int 20128,9.
Cecal foreign bodies (CFB) caused by multiple high-power magnets are rare and can pose a diagnostic challenge because of pressure on the cecal wall, which mimics the clinical features of AA. Owing to its anatomical location and function, the cecum is an infrequent site for FB impaction; however, when it occurs, it can lead to severe complications including hemorrhage and cecal perforation. In this report, we present the case of a 12-year-old male from Ethiopia who initially presented with symptoms suggestive of AA, in addition to an ultrasound investigation suggestive of AA. However, during the surgical exploration, a magnetic foreign body (MFB) was identified as the underlying cause of the patient’s potential presentation. In our case, we experienced successful surgical removal of magnetic material, and we recognized surgical exploration in an unconfirmed FB by ultrasound, specifically in a resource-limited setting. The work has been reported in line with the SCARE 2023 criteria11.
Case presentation
A 12-year-old boy was referred from a private higher clinic with a diagnosis of AA presenting with dullaching abdominal pain RLQ for 2 days, associated with anorexia, nausea, and low-grade fever. Otherwise, he had no history of vomiting, diarrhea, recent upper respiratory tract infections, or urinary symptoms and was previously in good health, as reported by the patient’s family on the day of admission. The patient did not report any history of a FB, even to his own family, and no one had knowledge of the foreign body he had ingested, except for himself.
The patient also presented with abdominal ultrasound (AU) findings suggestive of AA. Saying that ‘appendix had an edematous wall with a wall-to-wall diameter of 0.7 cm, and periappendiceal fat stranding was observed, whereas the distal ileum and cecum had edematous walls’ (Fig. 1). Upon examination, the child was acutely sick (in pain), with a pulse rate of 108 bpm, temperature of 37.8°C, and oxygen saturation of 94%. On abdominal examination, the abdomen was flat, move with respiration and only had deep rebound tenderness localized to RLQ. Other system examination was nonrevealing. Finally, with the same impression of AA, blood samples were collected for complete blood count and grouping, white blood cell count (WBC=7.5×103), Hemoglobin=15.5 g/dl, and platelet count (Plt=238×103 cells. These clinical findings were consistent with the sonographic findings and further supported the diagnosis (Fig. 1).
Figure 1.

Abdominal ultrasound findings suggestive of acute appendicitis.
Diagnosis and intraoperative management
The decision was made to proceed with emergency appendectomy to address the presumed diagnosis (AA) based on clinical and sonographic findings. Written informed consent was obtained from the patient’s family. The child was kept nothing per os (NPO per the guideline), placed on calculated maintenance fluid, ceftriaxone 750 mg IV, metronidazole 350 mg IV TID was initiated, and tramadol 50 mg IV was administered for the pain. Anesthetists performed a preanesthetic evaluation, prepared for the surgery, and then transferred to the operation theater for appendectomy. Preoxygenation was performed with 100% oxygen using face mask ventilation, premeditated with fentanyl (1 μg/kg) to suppress airway reflex. General anesthesia was administered using ketofol (1:1), followed by short-acting muscle relaxants then endotracheal tube was secured, and maintained with inhalational anesthesia in the supine position. Following this, the patient’s abdomen was meticulously prepared by cleansing with 70% alcohol and povidone-iodine and draped in four quadrants.
The incision was made via the RLQ transverse to access the peritoneal cavity (Figs 2, 3). Initially, we saw the FB, assumed that it was a delivered appendicolith, and tried to pick it using forceps; however, it pulled the forceps and anchored the cecal wall. The overall intraoperative findings were minimal adhesion between the cecum, omentum, and anterolateral interior abdominal wall, grossly inflamed appendix, and longitudinal folding of the cecal wall. In such a way that the right and left sides of the free teniae coli adhered together by joining a piece of three magnets creating pressure necrosis by adjoining the cecal wall with the resultant two cecal perforations. Moreover, multiple mesenteric lymphadenopathies and minimal reactive fluid levels were observed (Fig. 2).
Figure 2.
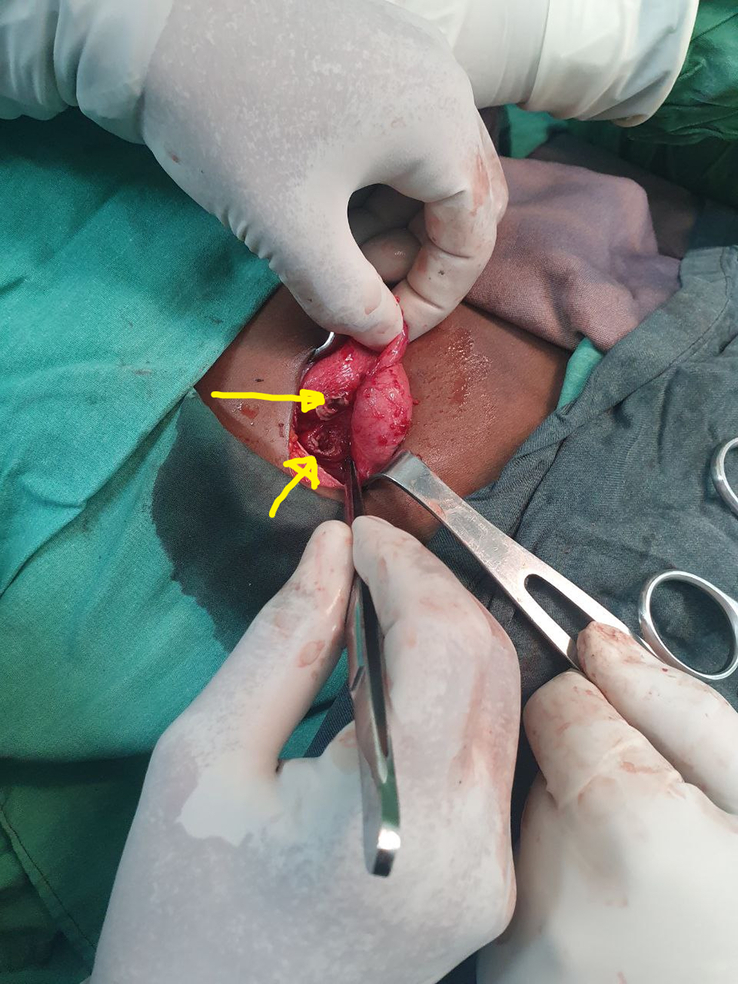
An image taken during surgery showing an inflamed cecum and appendix with a two-site cecal perforation. Image taken during surgery showing a grossly inflamed cecum.
Figure 3.

Image taken during surgery showing the magnetic foreign body.
Preforming appendectomy with two-site cecal perforation repair was deferred because cecostomy and cecal repair have a high failure rate with increased patient morbidity. Subsequently, the family was recommunicated based on the intraoperative findings to perform a right hemicolectomy and agreed on it, and the incision was then moved to the midline. The cecum and right/ascending colon were mobilized medially with dissection along the white line of Toldt. The right branch of the middle xolic artery was identified, divided, and ligated distally. The right colic artery distal to the branch of the ileal artery was divided and ligated. A right colectomy was performed, the distal stump of the transverse colon was closed in the double layer, and bowel continuity was restored with end-to-side ileo-transverse anastomosis. The mesenteric defect was closed, and both incisions were closed layer-by-layer. Finally, resected sample were sent for histological examination. The patient was transferred to the postanesthesia care unit with stable vital signs, and abdominal field block was performed for pain in the OR. Postoperatively he was put on maintenance fluid, analgesic, and antibiotics was also continued.
Outcome and postoperative course
To the surprise of the family and surgical team, intraoperative findings did not reveal AA but instead identified three magnetic pieces of foreign body lodged within the wall of the cecum, causing cecal perforation (Fig. 3). The findings were communicated to the family, and they were amazed at how the child had been hiding from them.
After the patient became fully awake from the effects of anesthesia in the recovery room, he asked for the magnetic FB he swallowed and replied that ‘I feared communicating that I had swallowed it’. The family agreed and believed that the magnetic field was a real scenario obtained from the body of the child during surgery. Sips were initiated on postoperative day two and the child had a smooth postoperative course, except for mild surgical site pain in which tramadol was administered. Tramadol resulted in nausea and vomiting then changed to diclofenac, and paracetamol and his symptoms were relieved on the fourth postoperative day. The patient was closely followed-up for complications, such as anastomotic leak, abscess formation, peritonitis. However, the postoperative course was uneventful, and discharged after a smooth recovery on the seventh postoperative day. Provided instructions for follow-up to observe progress, and to bring the histology report (revealed nonspecific colitis, cecal inflammatory polyps, and reactive lymph node changes). During the first appointment, patients had no complaints. The surgical wounds healed well, and stitch removed. The child was further followed-up with two subsequent appointments 1 month apart, we found the patient with a smooth course.
Discussion
In this case report, we describe a CFB that mimicked AA, resulting in a diagnostic challenge with ultrasound due to multiple powered magnetic lodges in the cecum, which was rare and intriguing in our patient, highlighting the importance of unusual etiologies when faced with abdominal pain and symptoms that mimic AA. Although this case is unique in its presentation, it is essential to discuss its implications for its diagnosis and management. In our case, the initial clinical impression was AA, which led us to decide to perform surgical appendectomy, during which the unexpected discovery of a MFB ingested by a 12-year-old boy and cecal perforation led us to change the diagnosis and management during the surgery (Fig. 1). This led us to highlight the importance of maintaining an open mind during any surgery, ready to adapt to unexpected surgical findings, as a delay in recognizing the true etiology may lead to adverse outcomes, particularly in resource-limited countries, where highly digitalized imaging is not accessible.
Ingestion of a MFB poses a significant sequence of health risks to patients. Owing to the nature of the magnet or its attraction to each other through the wall12, the anatomical location of the cecum for FB impaction can lead to severe complications, including hemorrhage and cecal perforation with sub sequential general peritonitis. Specifically, in our case, the three pieces of MFB swallowed by this patient may have resulted in pressure and narrowing of the cecal wall, leading to obstruction/tissue damage and perforation13. Due to the anatomical location of the cecal, prolonged pressure may weaken the wall, eventually resulting in ischemia, bowel perforation, or fistula formation13. In addition, it mimics the symptoms of AA, which may make accurate diagnosis difficult, causing abdominal pain and systemic inflammation, with the potential for severe complications, such as sepsis. Immediate medical attention is crucial to address these emergent complications and mitigate the risks associated with MFB ingestion14. The cecal perforations identified in our case was due to pressure or attraction created by the three MFB swallowed resulted in perforation of the cecal wall that we managed surgically.
Various foreign bodies have been found to cause perforation, including fish bones, animal bones, bone fragments, and toothpicks15. However, an entire tooth or part of it in the appendix is a rare cause of AA. However, the prevalence of appendicitis caused by foreign bodies remains low. The results obtained by Collins et al.16 reported that out of 71 000 appendectomies, 51.8% were caused by obstruction, of which most were parasitic worms or feces, and only 5.5% were considered unusual foreign bodies, in other report FB account for ~0.0005%10. The ingestion of FB generally does not cause gastrointestinal complications, such as AA, and can occur within a week with less than a 1% rate of complications17. In the United States FB ingestion occurs in more than 1%18. More than 80% of these patients are children17. Approximately 80–90% of ingested FB are thought to transit through the gastrointestinal tract without causing harm; however, with ~1% of FB remain lodged inside the colon and cause perforation19 during endoscopy20,21. However, bleeding, perforation, erosion, and ulceration of the gastrointestinal tract may occur in the presence of high-pressure or sharp metallic FB. Because of these complications, endoscopic intervention is recommended within 24 h22. However, in our case, it failed to arrive at a true diagnosis, as some case reports have reported that types of FB, such as needles, tongue piercing, screws, crown posts, teeth, and pins can cause AA10. In this case, we experienced multiple magnetic FB in the appendix, which were not obtained in the AU.
Ingested objects differ in their ability to injure the appendix wall if entrapped at this site3,5,7. Changes in the types of ingestions encountered, specifically high-power magnet ingestions, create a challenge for children that leads to morbidity and mortality5. Despite the clinical similarities, there are key differences in the diagnostic approach and management of CFB compared with AA. The primary goal of AA is the removal of the inflamed appendix, whereas in cases of MFB, the main focus is to identify and remove the FB and address any associated complications. Preoperative ultrasonography imaging can help differentiate between these conditions but may not always be conclusive and cannot be confirmed.
Most FB spontaneously pass without symptoms. However, ingestion of metallic FB resulted in gastric obstruction reported in Asia (Japan, China, and Korea), where magnets are used as traditional medicine. When more than one magnet is ingested, they can be attracted to each other through the intestinal wall, causing necrosis, intestinal perforation, or fistula. However, in our country, there have been no such reports before this date. Therefore, they should be removed while still being accessible with an endoscope23,24. The management of CFB caused by magnetic bodies typically involves removal of foreign objects and repair of any associated perforation. Timely intervention is crucial to reduce the risk of complications including abscess formation, sepsis, and peritonitis. Therefore, patients should receive appropriate intervention to prevent complications.
Strengths and limitations
In this case report, we describe a rare FB that mimicked AA, resulting in a diagnostic challenge with AU alone because of the nature and pressure created by three magnet lodges in the cecum of our patient, highlighting the importance of unusual etiologies reflective of the pediatric, specifically the adolescent age group, for the first time. Moreover, there may be bias due to the diagnosis made at a private clinic before patients presented to our hospital for emergency surgery. Despite this limitation, we highlighted unexpected surgical findings with review of literature, as a delay in recognizing the true etiology may lead to adverse outcomes, specifically in resource-limited countries.
Conclusion
In conclusion, MFB were found to mimic the symptoms of appendicitis, perforation, periappendiceal abscess, and subsequent peritonitis. Surgery should be considered to remove the MFB, and this case could be used as a reminder to maintain a high index of suspicion, particularly in resource-limited settings, where highly digitalized imaging is not accessible. Appropriate surgical management is essential for successful treatment of patients with this rare and challenging condition. The patient was discharged after a smooth recovery on the 7th day of admission, with instructions for follow-up to observe the progress. In our case, we experienced fear of communicating what had happened to him, even for his family. Finally, the family should follow their children, where and what they have been doing on a day-to-day basis through smooth and free communication with their children.
Ethical approval
The case reports were exempted from ethical review and approval at our institution.
Consent
Written informed consent was obtained from the father of the child, including the images (figure), for publication in a journal for educational purposes. The mother understands that their names and initials will not be published and due efforts will be made to conceal their identity (Declaration of Helsinki ethical principles); however, anonymity cannot be guaranteed. Data were obtained through direct observation and perioperative medical, anesthetic, and surgical management. A copy of the written consent form is available for review by the Editor-in-Chief upon request.
Sources of funding
None.
Author contribution
The case report was conducted in collaboration with all the authors. The corresponding author (A.F.I.) conceived the idea, prepared the case report, prepared the manuscript, journal selection, and sent for publication. The authors (M.S.H., Y.T., and H.M.) contributed in writing, re-writing, and edition. Finally, all authors have read and approved the case report for publication.
Conflicts of interest disclosure
All authors declared that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this case report.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
The corresponding author (A. F. I.) E-mail: amanhoney9182@gmail.com, Tel.: +251 917 509 182. P.O. Box 1362.
Data availability statement
The data used in this case report are available from the corresponding author.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
The authors would like to thank the study participants, and healthcare professionals for their support in collecting clinical data.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 5 January 2024
Contributor Information
Amelmasin Faris Ibrahim, Email: amelmasin.faris@ddu.edu.et.
Mohammed Seid Hussen, Email: mametinishu@gmail.com.
Yared Tekle, Email: yaredtkl@gmail.com.
Hussen Mohammed, Email: hus.aliya@gmail.com.
References
- 1.Hijaz NM, Friesen CA. Managing acute abdominal pain in pediatric patients: current perspectives. Pediatric Health Med Ther 2017;8:83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thees-Laurenz R. Covered perforation of the ileum caused by an ingested blister pill pack–a rare sonographic diagnosis. J Ultrasound 2021;42:553–554. [DOI] [PubMed] [Google Scholar]
- 3.Echevarria S, Rauf F, Hussain N, et al. Typical and atypical presentations of appendicitis and their implications for diagnosis and treatment: a literature review. Cureus 2023;15:e37024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunter TB, Taljanovic MS. Foreign bodies. Radiographics: a review publication of the Radiological Society of North America, Inc 2003;23:731–757. [DOI] [PubMed] [Google Scholar]
- 5.Kramer RE, Lerner DG, Lin T, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr 2015;60:562–574. [DOI] [PubMed] [Google Scholar]
- 6.Ferris M, Quan S, Kaplan BS, et al. The global incidence of appendicitis: a systematic review of population-based studies. Ann Surg 2017;266:237–241. [DOI] [PubMed] [Google Scholar]
- 7.Omling E, Salo M, Saluja S, et al. Nationwide study of appendicitis in children. Br J Surg 2019;106:1623–1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ambe P, Weber SA, Schauer M, et al. Swallowed foreign bodies in adults. Dtsch Arztebl Int 2012;109:869–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chawla S, Choudhary V, Kasniya R. Lollipop stick en-route cecum: mimic of appendicitis. Case Rep Clin Radiol 2023;1:138–139. [Google Scholar]
- 10.Simkovic D, Hladík P, Lochman P. Unusual cause of the acute appendicitis. Rozhl Chir 2004;83:365–367. [PubMed] [Google Scholar]
- 11.Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2023;109:1136–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicoara M, Liu S, Ferzli G. Laws of attraction: management of magnetic foreign body ingestion. BMJ Case Rep 2018;2018. doi: 10.1136/bcr-2018-225939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hussain SZ, Bousvaros A, Gilger M, et al. Management of ingested magnets in children. J Pediatr Gastroenterol Nutr 2012;55:239–242. [DOI] [PubMed] [Google Scholar]
- 14.Hernandez Anselmi E, Gutierrez San Roman C, Barrios Fontoba JE, et al. Intestinal perforation caused by magnetic toys. J Pediatr Surg 2007;42:E13–E16. [DOI] [PubMed] [Google Scholar]
- 15.Cheng He R, Nobel T, Greenstein AJ. A case report of foreign body appendicitis caused by tongue piercing ingestion. Int J Surg Case Rep 2021;81:105808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collins DC. A study of 50,000 specimens of the human vermiform appendix. Surg Gynaecol Obstet 1955;101:437–445. [PubMed] [Google Scholar]
- 17.Antonacci N, Labombarda M, Ricci C, et al. A bizarre foreign body in the appendix: a case report. World J Gastrointest Surg 2013;5:195–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kay M, Wyllie R. Pediatric foreign bodies and their management. Curr Gastroenterol Rep 2005;7:212–218. [DOI] [PubMed] [Google Scholar]
- 19.Nicolodi GC, Trippia CR, Caboclo MF, et al. Intestinal perforation by an ingested foreign body. Radiol Bras 2016;49:295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen J, Ferm S, Schwarzbaum D, et al. Novel approach to endoscopic foreign body retrieval from the gastric body. J Investig Med High Impact Case Rep 2021;9:23247096211040631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pahuja HDDS, Palsodkar SR, Lande SA. Anaesthetic management of neonate with giant occipital meningoencephalocele: case report. Int J Res Med Sci 2015;3:334–337. [Google Scholar]
- 22.Wu WT, Chiu CT, Kuo CJ, et al. Endoscopic management of suspected esophageal foreign body in adults. Dis Esophagus 2011;24:131–137. [DOI] [PubMed] [Google Scholar]
- 23.Chung JH, Kim JS, Song YT. Small bowel complication caused by magnetic foreign body ingestion of children: two case reports. J Pediatr Surg 2003;38:1548–1550. [DOI] [PubMed] [Google Scholar]
- 24.Kubota Y, Tokiwa K, Tanaka S, et al. Intestinal obstruction in an infant due to magnet ingestion. Eur J Pediatr Surg 1995;5:119–120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this case report are available from the corresponding author.


