Summary:
Disposable handheld nerve stimulators are widely used in peripheral nerve surgery. Such devices stimulate a motor nerve or the motor component of a mixed nerve by applying electrical current to the proximal region, targeting the main nerve trunk. This stimulation then travels along the motor nerve, reaching the distal end to control the corresponding muscle(s). In this study, the authors demonstrate three useful tips and tricks for handheld nerve stimulation during targeted muscle reinnervation and peripheral nerve surgery. The three tips are (1) identification of proximal muscle contraction by retrograde electrical stimulation of a distal sensory nerve; (2) graded stimulation for identifying motor nerves within fibrotic scarred tissue beds or parallel to the major motor/mixed nerve of interest; and (3) proximal stimulation for validation of adequate post-targeted muscle reinnervation coaptation(s).
Takeaways
Question: How to identify the motor branch of muscle efficiently, especially in a revisional amputation full of fibrotic tissue and atrophic muscle?
Findings: This study demonstrates three useful ticks with a handheld nerve stimulator with illustrations, and video demonstrations.
Meaning: Applying these three useful tricks with the handheld nerve stimulator, readers can identify the recipient target nerve efficiently and confirm the quality of nerve coaptation.
INTRODUCTION
Handheld peripheral nerve stimulators can be used during surgery to aid in more efficient dissection, localization, and identification of motor nerves, assessing nerve function, and avoiding nerve injury. These devices have been widely used during nerve transfers for brachial plexus or other peripheral nerve injuries.1
Targeted muscle reinnervation (TMR) is a technique for the surgical prevention and management of neuropathic pain. It can be used during primary amputation surgery2 or following secondary surgery to treat symptomatic neuromas.3 There are three critical steps in TMR surgery: (1) recognizing the donor major sensory or mixed motor/sensory nerve, (2) identifying the recipient motor nerve branches to the target muscle, and (3) securing a functional nerve coaptation.4
During our experience with handheld peripheral nerve stimulators, the authors have developed several strategies that improve speed and accuracy during peripheral nerve surgery and may assist in a wide range of procedures performed by peripheral nerve surgeons. In this article, three useful tips and tricks are demonstrated in handheld intraoperative nerve stimulation to perform TMR and peripheral nerve surgery efficiently and successfully.
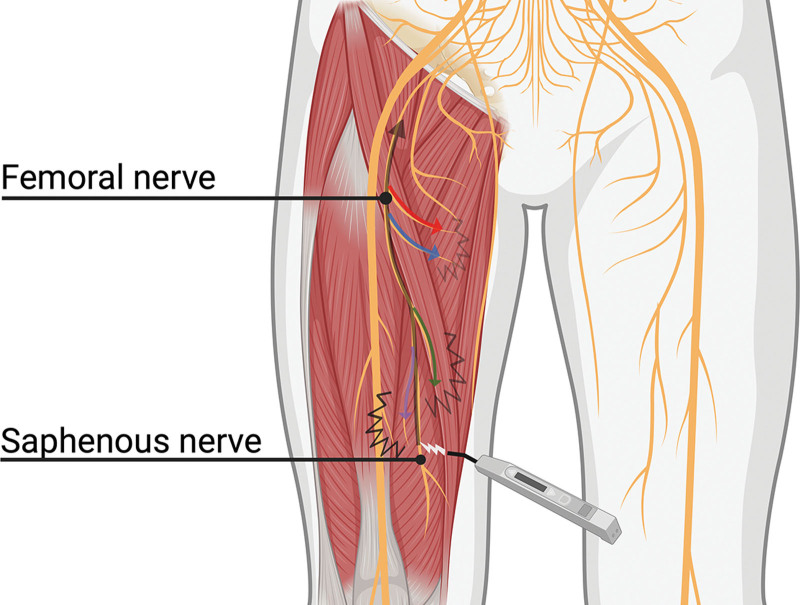
First, we discuss retrograde stimulation for nerve identification. When attempting to discern whether a nerve is sensory, motor, or mixed, one can stimulate the distal nerve ending at 20 mA and observe the anticipated motor response more proximally. Specifically, when stimulating a mixed nerve at the terminal end or a purely sensory nerve, a muscle contraction can be visualized more proximally up the parent nerve tree. This technique can help identify the recipient motor branch to the more proximal muscle for TMR or other nerve transfer procedures. For example, a nerve stimulator can stimulate the saphenous nerve at its distal, purely sensory level. Via retrograde nerve conduction, it will activate motor nerve components of its parent nerve, the femoral nerve. This retrograde contraction is illustrated in Figure 1 and Video 1. Identifying where the motor nerve branches emanate is easier by inducing muscle contraction, especially in a revision amputation with potentially scarred and atrophic muscle. [See Video 1 (online), which demonstrates the retrograde stimulation to identify a sensory nerve.]
Fig. 1.
When the distal part of the saphenous nerve is stimulated using 20 mA, the stimulus travels proximally to the femoral nerve. It distributes the electrical pulse toward the motor branches of the quadriceps muscle. We notice contraction of the proximal portion of the quadriceps.
Video 1. demonstrates the retrograde stimulation to identify a sensory nerve. As the electrical amplitude of nerve stimulation is gradually increased, the distal part of the saphenous nerve is stimulated using 20 mA. This electrical pulse, transmitted proximally to the femoral nerve, is strong enough to distribute distally toward the motor branches of the quadriceps and show contraction of the muscles.
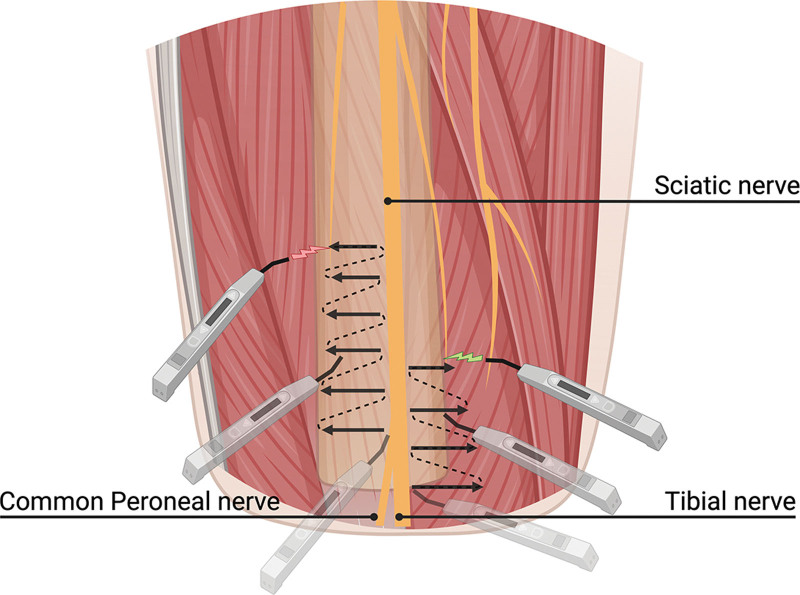
Second, progressive stimulation for identifying motor nerves can be used. After identifying the major nerve used during TMR, nerve stimulation may further discriminate recipient motor nerve branches. Particularly when conducting surgery in nonvirgin terrain, fibrosis and scar tissue may cause motor nerve identification challenging. In this case, one can use an intraoperative handheld nerve stimulator and probe transversely over the muscle in a meandering “back and forth” pattern using a 2-mA amplitude to determine the main locations for recipient, motor nerves. The differential muscle responses can be honed in on the more specific location of a preferred target motor nerve recipient. If a muscle response is visualized, the current gradually decreases to 0.5 mA, allowing for more selective identification of the specific motor nerve branch location. An example of this technique for the sciatic motor nerve branches in an above-knee-amputation model is shown in Figure 2 and Video 2. [See Video 2 (online), which demonstrates employing an intraoperative handheld nerve stimulator and probes transversely over the muscle in a meandering “back and forth” pattern using a 2-mA amplitude to determine the main locations for the recipient, motor nerves.]
Fig. 2.
In targeted muscle reinnervation surgery, especially in a secondary setting, it may be challenging to identify the motor branches within fibrotic tissue. We demonstrate the sciatic nerve in an above-knee-amputation model. After identifying the major motor nerve, one adopted a side-to-side approach from the sciatic nerve with a nerve stimulator. Then, we could search for the motor branches of the hamstring (green flash) and biceps femoris (red flash) by noticing any muscle contraction.
Video 2. demonstrates employing an intraoperative handheld nerve stimulator and probes transversely over the muscle in a meandering “back and forth” pattern using a 2-mA amplitude to determine the main locations for the recipient, motor nerves.
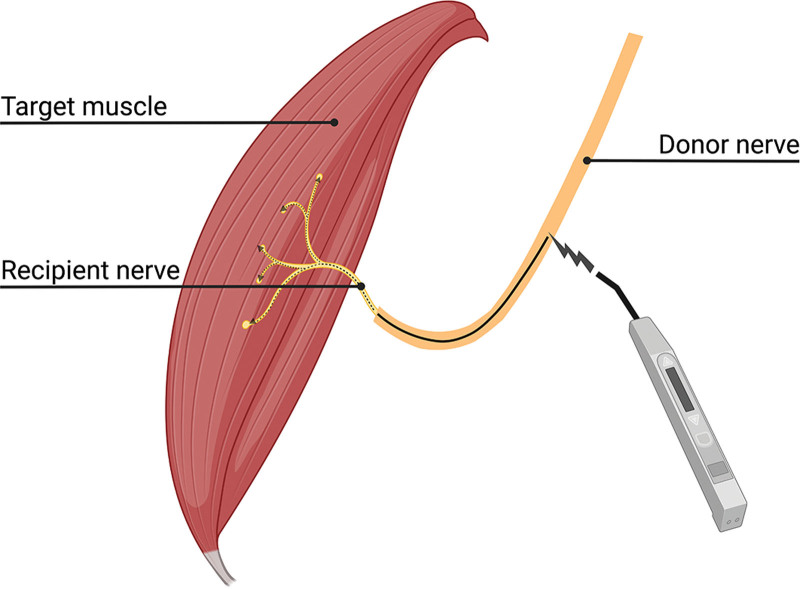
Third, TMR and other nerve coaptations can be validated by proximal stimulation. To validate the appropriate technical performance of a TMR or motor nerve coaptation, intraoperative confirmation can be obtained by directly stimulating the donor nerve proximally to the coaptation site to determine if the distal motor end plates sufficiently receive an excitatory electrical current past the coaptation site. If target muscle contraction is observed, we have found this to indicate a technically acceptable coaptation. Although there is not yet axonal continuity, it is possible to transmit the electrical signal through the coaptation and thus stimulate the distal target muscle (Figure 3). [See Video 3 (online), which demonstrates performing a targeted muscle reinnervation coaptation.] Although we have confirmed the effectiveness of end-to-end alignment in facilitating electrical current transmission and muscle contraction, the precise achievement of end-to-end alignment in this method remains unverified. Similar to its application in TMR surgery, this technique is used for surgical exploration of sharp transection nerve injuries when performed within the first 72 hours, as the distal segment remains able to be stimulated.5
Fig. 3.
A size discrepancy frequently occurs between the major transected nerve and the targeted motor points in targeted muscle reinnervation surgery. We will stimulate the nerve proximal to the coaptation after the mismatch in nerve diameter. If the large-to-small nerve coaptation is performed with a proper motor fascicular end-to-end alignment, we can detect localized muscle contractions using a nerve stimulator at an amplitude of 20 mA. If muscle contraction fails to occur, this might indicate misalignment of end-to-end motor fascicles; thus, we prefer to revise the nerve coaptation.
Video 3. demonstrates performing a targeted muscle reinnervation coaptation. Due to the significant size difference between the motor nerve and the recipient’s nerve, we aim to match the size of the donor nerve with the nerve branch to the muscle at approximately a 2:1 ratio. This video shows the sciatic nerve being split into 3-4 bundles of fascicles. Using a nerve stimulator, we confirm the passage of electrical current across the coaptation and observe muscle contraction. To minimize collateral neural sprouting, we will then wrap the coaptation with a vascularized muscle flap.
DISCUSSION
During TMR and other peripheral nerve operations, using an intraoperative handheld nerve stimulator can effectively streamline the identification of donor and recipient nerves. There are two kinds of handheld nerve stimulators: non-sterile and disposable ones. Anesthesiologists commonly use nonsterile nerve stimulators connected to a sterile wire and needle for nerve blocks, and they can also be used by surgeons intraoperatively. These stimulators deliver a stimulus in 0.1 mA increments, in the range of 0.1–5 mA.6 During this nerve stimulation, the surgeon must instruct the anesthetist or circulating nurse to adjust the current.
In contrast, with disposable intraoperative nerve stimulators, surgeons can adjust electrical amplitude directly. These types of nerve stimulators also provide limited choices of stimulation amplitudes, with the lowest mA of disposable nerve stimulators used by many surgeons being 0.5 mA. Inadvertent stimulation of adjacent fascicles can be an issue during inter-fascicular dissection in some nerve transfer procedures. Because 2.0 mA is typically used in TMR surgery, the stimulus of 0.5 mA may be adequate for more specific identification of a target motor nerve recipient. With a more precise stimulation using a lower setting of electrical amplitude, there may be a role for bipolar nerve stimulators to confirm the fascicular mapping. However, they are less efficient in searching for recipient motor branches.
Although a handheld nerve stimulator is often beneficial, there are circumstances when it may not function in the intended manner. The use of paralytic agents for induction of anesthesia may adversely influence the ability to stimulate by reducing or completely blocking the anticipated muscle excitability. Also, prolonged duration of elevated tourniquet times can reduce or temporarily cause paralysis within muscles, rendering them unable to be excited by intraoperative stimulation.7
In conclusion, these three tips and tricks with a handheld nerve stimulator may optimize the efficient and successful conduction of TMR and other peripheral nerve procedures.
DISCLOSURES
Dr. Eberlin is a consultant for AxoGen Inc, Checkpoint Surgical Inc, Integra Lifesciences Inc, Tissium, Tulavi Therapeutics Inc, and Biocircuit. Dr. Valerio is a consultant for AxoGen Inc, Checkpoint Surgical Inc, and Integra Lifesciences Inc. All the other authors have no financial interest to declare in relation to the content of this article. This work was supported in part by the Jesse B. Jupiter Research Fund/Wyss Medical Foundation.
ACKNOWLEDGMENT
The figures presented in this study were created with BioRender.com.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
Drs Liu and Raasveld contributed equally to this work.
REFERENCES
- 1.Phillips BZ, Franco MJ, Yee A, et al. Direct radial to ulnar nerve transfer to restore intrinsic muscle function in combined proximal median and ulnar nerve injury: case report and surgical technique. J Hand Surg Am. 2014;39:1358–1362. [DOI] [PubMed] [Google Scholar]
- 2.Frantz TL, Everhart JS, West JM, et al. Targeted muscle reinnervation at the time of major limb amputation in traumatic amputees: early experience of an effective treatment strategy to improve pain. JB JS Open Access. 2020;5:e0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dumanian GA, Potter BK, Mioton LM, et al. Targeted muscle reinnervation treats neuroma and phantom pain in major limb amputees: a randomized clinical trial. Ann Surg. 2019;270:238–246. [DOI] [PubMed] [Google Scholar]
- 4.Eberlin KR, Brown DA, Gaston RG, et al. A consensus approach for targeted muscle reinnervation in amputees. Plast Reconstr Surg Glob Open. 2023;11:e4928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008;119:1951–1965. [DOI] [PubMed] [Google Scholar]
- 6.Thallaj A, Alotaibi WM, AlZahrani T, et al. Intraoperative nerve stimulation during brachial plexus surgery: comparison between a totally disposable nerve stimulator and nerve stimulator normally used for nerve blocks. Plast Surg (Oakv). 2017;25:171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanberg P, Bue M, Kabel J, et al. Tourniquet-induced ischemia and reperfusion in subcutaneous tissue, skeletal muscle, and calcaneal cancellous bone. APMIS. 2021;129:225–231. [DOI] [PubMed] [Google Scholar]