Abstract
Background:
Postoperative pain is poorly studied in developing countries. Severe pain after surgery remains a major problem, occurring in 50–70% of the patients. Differences exist across countries. Despite numerous published studies, the degree of pain following many types of surgery in everyday clinical practice is unknown. To improve postoperative pain-treatment and develop procedure-specific, optimized pain-treatment protocols, the prevalence and severity of postoperative pain must first be identified.
Objective:
This study aimed to determine the prevalence and intensity of acute postoperative pain and the practice of postoperative pain management.
Methods:
A total of 180 patients were enrolled in the study, with 160 calculated using a single population proportion formula and a 10% attrition rate added, with proportionate stratification according to the size of each ward to obtain the number of participants from each specialty ward. A multistage sampling with stratified proportionate at the initial stages and a simple random sampling technique at the final stage was used. The patients completed a numerical pain rating scale for pain immediately after surgery for the first 72 h after surgery. The prevalence of mild, moderate, or severe pain was calculated. The evaluation was performed at eight time points including immediately after surgery: T2, T4, T8, T12, T24, T48, and T72.
Result:
The prevalence of severe pain in patients who underwent elective surgery in the study period measured by numeric rating scale was 21.6, 43.9, 45.6, 28.9, 39.4, 10.5, and 13.4% at 2nd, 4th, 8th, 12th, 24th, 48th and 72 h, respectively.
Conclusion:
The prevalence of moderate-to-severe pain within 72 h postoperatively was slightly lower than that other studies conducted in Ethiopia reported. This was still high, indicating better pain management in the postoperative period. Involvement of the anesthetist in pain management is crucial for better patient management.
Keywords: DCSH, Dessie, Ethiopia, postoperative pain
Introduction
Highlights
Acute postoperative pain is the most common distressing aspect of the surgery.
The prevalence of severe postoperative pain in DCSH was 21.6, 43.9, 28.9, 39.4, 10.5, and 13.4% at 2nd, 4th, 8th, 12th, 24th, 48th and 72 h, respectively.
Acute postoperative pain that is not appropriately managed has multiple short-term adverse effects include physical limitation, emotional status, and mood disturbance.
Patients postoperative satisfaction is dependent on pain management.
Background
Pain is the most common distressing aspect of the surgery. The prevalence of postoperative pain is high, with an increasing number of annual surgical procedures worldwide1. Despite an increased understanding of pain and the development of new technological advances in the treatment of pain, many surveys over a long period have shown that many patients still experience moderate to severe postoperative pain. This shows that pain management practices remains challenging in the surgical field2.
The intensity of postoperative pain depends on several factors, including patient and surgery-dependent factors. The intensity and rate of postoperative pain vary depending on the type of analgesic/anesthetic intervention used, surgery performed, and the time elapsed after surgery. Postoperative pain can consist of a mixture of nociceptive, neuropathic, and visceral pain3.
Inadequate pain relief in the postoperative phase is a well-known global problem. It may be associated with harmful physiological and psychological consequences, resulting in negative clinical and economical outcomes such us increased postoperative morbidity, reduced quality of life, delayed recovery, discharge to home, the development of persistent postsurgical pain, and increased resource utilization. More aggressive anesthesia/analgesia methods are needed to reduce the incidence and intensity of acute pain during and immediately after surgery to minimize the associated complications of postoperative pain. Globally, the prevalence of postoperative pain varies among studies. From the results of the literature search, it was clear that there is limited research on postoperative pain prevalence and management. Most studies have aimed to evaluate postoperative pain4–8.
Efforts to identify and implement effective interventions at the patient, health and policy levels to manage postoperative pain are ongoing. During the past two decades, there has been increased attention on improving postoperative pain management because of several new guidelines and improvements in techniques for managing perioperative pain. Despite these improvements, the postoperative pain management is often unsatisfactory. Recent studies have revealed a high incidence of moderate or severe postoperative pain in both developed (41–61%) and developing (60–80%) countries. The American Pain Society suggests that prevalence has remained consistently high with more than 80%3,9,10.
Numerous factors may be responsible for inadequate pain management, including inadequate staff training, insufficient knowledge of nurses and physicians, unhelpful staff and patient attitudes, fear of analgesic side effects, a lack of accountability, and poor pain assessment. There is a need to improve the treatment of acute postoperative pain by administering effective methods of analgesic control through organized and systematized care, consistent with the requirements of each hospital6,11–13.
Studies have shown gaps or inconsistencies between practices for acute pain management and have proposed updates and recommendations for these best practices. Further studies are required to develop a better understanding of the mechanisms of pain, preventive measures, and medications to prevent postoperative pain and its associated complications. However, a lack of sufficient data regarding its magnitude leads to an underestimation of the adverse effects of postoperative pain.
Furthermore, almost all studies on this topic have been conducted in well-resourced settings. Due to the obvious variances in healthcare across settings, the same risk factors, clinical practice, and magnitude of acute postoperative pain cannot be assumed. Interpatient variability exists in pain perception, which is affected by genetic, social, cultural, and cognitive factors. Again, there is interprofessional variability in the assessment and recognition of postoperative pain. Due to inter-individual and interprofessional variability, patients’ experiences of postoperative pain vary. Therefore, extrapolating the results of studies conducted in the other areas is difficult because of the variability. Therefore, this study is relevant to the society because it provides a voice for postoperative patients.
Objective
The objective of this study aimed to assess the status of postoperative pain and the practice of postoperative pain management.
Hypothesis
We hypothesized that 50% of the patients undergoing surgery would have moderate to severe pain (score 6–10 on the VAS) after the surgical procedure within the first 72 h.
Methodology
Study design and setting
The study design was a prospective hospital-based descriptive observational study. Adult patients who underwent elective major surgery during the study period were recruited. Patients who satisfy the screening inclusion criteria were invited to participate in the study.
The study was conducted at a public hospital. The hospital is located in which is 400 km from. It is intended to serve 5 million populations and there are more than 300 beds. The hospital performs all the major surgical and medical activities. It has nine operation tables, including obstetric surgery. All patients who underwent major surgery and were hospitalized for 72 h postsurgery were included in the study. On an average, 10–12 patients per day undergo surgery with an average length of stay of 3–5 days.
This prospective observational study was conducted between February 2023 and April 2023.
Study population
All eligible patients who underwent elective surgery during the study period were included.
Sample size and sampling procedure
The sample size was calculated using the magnitude of postoperative pain from the previous study7 using a single population proportion formula with a 95% CI, 5% level of significance, and 5% margin of error. The sample size calculated as follows as:
In order to ensure a minimum of 160 patients were required, an additional 20 patients (≈10%) were enrolled to account for potential protocol violations and missing data.
Sampling method and data collection procedures
The study population included patients who were admitted to the surgical wards. From the records obtained in the statistics office; 2850 patients will be admitted to surgical wards in different surgical specialties: urology, orthopedics, general surgery, obstetrics, gynecologic, and neurosurgery within 6 months.
Considering that the wards did not have the same capacity to accommodate patients, we calculated the sample size using proportionate stratification to the size of each ward to obtain the number of participants from each specialty ward Table 1.
Table 1.
Number of participants from each ward.
| Ward by specialties | Strata capacity | Sample |
|---|---|---|
| Urology | 80 | 13 |
| Orthopedics | 200 | 33 |
| General surgery | 200 | 33 |
| Obstetrics | 400 | 62 |
| Gynecologic | 200 | 30 |
| Neurosurgery | 20 | 3 |
| ENT and maxillofacial | 40 | 6 |
| Total | 1100 | 180 |
* Layer Size (stratum population size)
A multistage sampling with stratified proportionate at the initial stages and simple random sampling technique at the final stage was used. Eligible patients were selected using the lottery method for selection and exclusion, with a sealed, nontransparent envelope leveled as selected or unselected.
Preoperative day
The principal investigator (PI) evaluated the inclusion and exclusion criteria of the subjects scheduled for elective major abdominal, gynecologic, obstetric, and orthopedic surgeries during their preoperative visit. Once subjects met the inclusion criteria, they were discussed the study purpose, risks, benefits, and confidentiality and provided informed consent by the PI. Patient were asked about their level of pain before surgery and show how to score pain using an NRS (0=no pain, 1–3=mild pain, 4–6=moderate pain, 7–10=severe pain) before they underwent the surgical procedure and were asked to score pain when back in the recovery room and ward.
On the day of surgery
A sociodemographic data were completed during the preoperative visit, premedication (analgesia) in the holding area upon admission for surgery, and intraoperative and postoperative analgesia (systemic or interventional) before arrival at the PACU. Additionally, base-line pain scores and vital signs, including blood pressure, heart rate, respiratory rate, and oxygen saturation, were measured and recorded before the participant’s arrival to the operating room.
At PACU arrival
Upon arrival at the PACU, the level of sedation was assessed to identify subjects who were excluded from the study owing to their level of consciousness. Pain assessment was performed using a data collection form with established time intervals. Pain was reported by the patient’s verbal response using a 0–10 numerical scale, and the maximum pain experienced in the preceding 24 h (‘worst pain over 24 h”) was assessed according to the Brief Pain Inventory. Postoperatively, pain and analgesics were scored on arrival, at 2, 4, 8, 12, 24, 48, and 72 h. Postoperative telephone calls were made when the patients were discharged before 72 h to assess the progress of postoperative pain while at home. Additionally, the type or technique of postoperative analgesia (systemic or interventional) was recorded in the PACU and the ward.
Numerical pain rating scale
There are different types of self-reported pain rating scale. The numerical rating scales (NRS, 0–10 used to assess pain intensity in these studies is one of the most commonly used rating scales of pain intensity in pain research. The NRS is often presented as a 10 cm long line where patients rate their pain by marking between the extremes of ‘no pain at all’ (0) and ‘worst pain imaginable’ (10). Pain scores were divided into four broad categories based on pain intensity14.
No pain : 0.
Mild pain: 1–3.
Moderate pain: 4–6.
Severe pain: 7–10.
Inclusion and exclusion criteria
Inclusion criteria
Age ≥18 years old.
Able to provide informed consent.
Able to verbalize or indicate pain using a traditional verbal scale such as the numeric rating scale (NRS) at the 2 h of PACU arrival.
Exclusion criteria
Patients are unable to self-report acute pain.
History of chronic pain and moderate-to-high acute pain prior to surgery.
Patients with a previous diagnosis of chronic cognitive impairment (Dementia, Alzheimer).
Patients with a previous diagnosis of neurologic impairment (paraplegia, quadriplegia…).
The patients excluded from the study will patients with mental and psychological problems.
Study variables
Dependent variable
Prevalence of postoperative pain in the first 72 h.
Intensity of postoperative pain in the first 72 h.
Patient satisfaction with postoperative pain management.
Independent variables
Sociodemographic variables: age, sex, weight, residence, and educational status.
Preoperative clinical condition: ASA status and coexisting diseases.
Intraoperative factors: type of surgery, type of anesthesia, duration of surgery, duration of anesthesia, induction agents, preoperative analgesia, and intraoperative analgesia.
Age (year).
Sex (M/F).
Marital status.
Ethnicity.
Education.
Occupation.
Induction agents.
Preoperative anxiety (STAI).
Type of anesthesia.
Intraoperative and postoperative pain management modalities.
Duration of the surgery.
Type of surgery (elective/emergency).
Preoperative pain intensity (NRS 0–10).
Preoperative chronic pain (yes/no).
Statistical analysis
Pain assessment data and satisfaction scores were entered into SPSS version 20 for analysis. Sociodemographic data, pain intensity, and satisfaction with pain management were summarized using descriptive statistics.
Data quality management
To ensure the quality of the data quality the questionnaire was pretested on 5% of the sample. The nine peoples involved in the pretest were selected from each group of surgery specialty and they explained how the questionnaire was easy to understand. The data collectors were trained and oriented regarding the objective and process of data collection, and the collected data were checked for completeness, accuracy, and clarity. The PI supervised the data collection.
This research has been reported in line with the strengthening the reporting of cohort, cross-sectional, and case–control studies in surgery STROCSS criteria15.
Result
Demographical characteristics
This study included 180 participants who underwent major surgery during the study period February 2023 and April 2023. All the patients enrolled in this study were interviewed. The majority of the patients enrolled were with in the 18–30 age groups (26.7%). Forty-one percent of the patients were male. The number of patients recruited from different surgical specialties was stratified between the specialties; with obstetrics surgery had the highest number of participants (34.4%), while neurosurgery had the lowest (1.7%). Most of the patients had no preoperative pain (73.3%) Table 2.
Table 2.
Socio-demographic characters.
| Variables | Groups | Frequency (%) |
|---|---|---|
| Age | 18–30 | 48 (26.7) |
| 31–40 | 45 (25) | |
| 41–50 | 25 (13.4) | |
| 51–60 | 41 (22.8) | |
| 61–70 | 21 (12.1) | |
| Sex | Male | 74 (41) |
| Female | 106 (59) | |
| Weight | 40–60 | 87 (48.3) |
| 61–80 | 69 (38.3) | |
| 81–100 | 24 (13.4) | |
| ASA | ASA I | 93 (51.7) |
| ASA II | 79 (43.9) | |
| ASA III | 8 (4.4) | |
| Preoperative existing pain (NRS) | 0 | 132 (73.3) |
| 0–3 | 23 (12.8) | |
| 4–6 | 25 (13.9) | |
| 7–10 | 0 (0) | |
| Type of surgery | General surgery | 33 (18.3) |
| Orthopedics | 33 (18.3) | |
| ENT and maxillofacial | 6 (3.3) | |
| Neurosurgery | 3 (1.7) | |
| Gynecology | 30 (16.7) | |
| Obstetrics | 62 (34.4) | |
| Urology surgery | 13 (7.3) | |
| Type of anesthesia | General anesthesia | 109 (60.6) |
| Regional anesthesia | 71 (39.4) | |
| Premedication | Dexamethasone | 165 (91.7) |
| Paracetamol | 4 (2.2) | |
| Dexamethasone + pcm | 4 (2.2) | |
| Metoclopramide | 76 (42.2) | |
| Intraoperative analgesia | Morphine | 143 (79.4) |
| Pethidine | 37 (20.5) | |
| Morphine and diclofenac | 78 (43.3) | |
| Pethidine and diclofenac | 12 (6.7) | |
| Postoperative analgesic | Tramadol | 167 (92.8) |
| Diclofenac | 22 (12.2) | |
| Tramadol + diclofenac | 18 (10) |
Prevalence of pain
The prevalence of pain in patients who underwent elective surgery during the study period ranged from hours to hour (Fig. 1). The prevalence of severe pain measured with NRS was 21.6, 43.9, 45.6, 28.9, 39.4, 10.5, and 13.4% at 2, 4, 8, 12, 24, 48, and 72 h, respectively.
Figure 1.
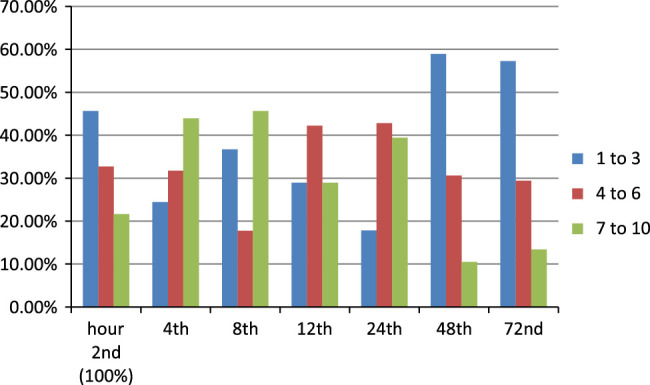
Prevalence of pain at 2, 4, 8, 12, 24, 48, and 72 h postoperatively.
The complications resulting from pain in the 24 h postoperative period
The effect of pain on physical activity is shown in Figure 2. Pain in the postoperative period had the greatest effect on the walking ability of patients, with 67.8% of the patients stating the pain had complete and moderate interference in their walking ability. The majority of the patients 93.3% had no problems with interacting with others. Coughing and deep breathing abilities were completely affected by pain in 13.3% of the patients.
Figure 2.
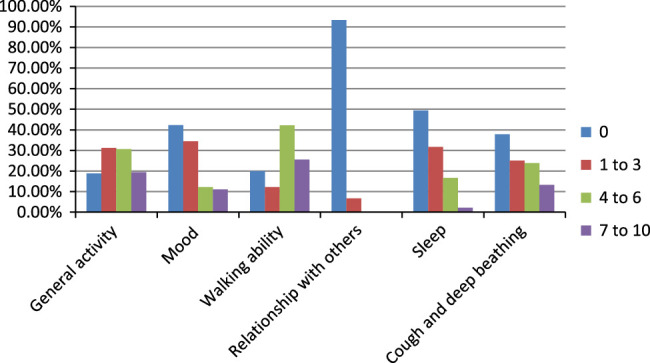
Pain interference on physical activity in 24 h.
The emotional effects of pain are presented in Table 3. Most of the patients were not affected by pain. Three point three percent of the patients explained they had moderate anxiety associated with pain. None of the patients had experienced extreme anxiety, depression, fear, or helplessness.
Table 3.
Pain effect on mood and emotions in 24 h.
| Score | Frequency (%) | |
|---|---|---|
| Anxious | 0 | 156 (86.7) |
| 1–3 | 18 (10) | |
| 4–6 | 6 (3.3) | |
| 7–10 | 0 (0) | |
| Depressed | 0 | 169 (93.9) |
| 1–3 | 6 (3.3) | |
| 4–6 | 5 (2.85) | |
| 7–10 | 0 (0) | |
| Frightened | 0 | 168 (93.3) |
| 1–3 | 12 (6.7) | |
| 4–6 | 0 (0) | |
| 7–10 | 0 (0) | |
| Helpless | 0 | 174 (96.7) |
| 1–3 | 4 (2.3) | |
| 4–6 | 0 (0) | |
| 7–10 | 0 (0) |
The adverse effects of pain explained by the American Pain Society are presented in Table 4. Severe nausea associated with pain was observed in 45% of the patients. Most of the patients felt drowsy and 55.6% of the patients associating it with the postoperative pain. Itching and dizziness were the least common complications, with 6.6 and 5% patients, respectively, having moderate manifestations.
Table 4.
Side effects associated with postoperative pain.
| Frequency (%) | |
|---|---|
| Nausea | |
| 0 | 68 (37.8) |
| 1–3 | 31 (17.2) |
| 4–6 | 72 (40) |
| 7–10 | 9 (5) |
| Drowsiness | |
| 0 | 55 (30.65) |
| 1–3 | 25 (13.95) |
| 4–6 | 82 (45.6) |
| 7–10 | 18 (10) |
| Itching | |
| 0 | 136 (75.6) |
| 1–3 | 32 (17.8) |
| 4–6 | 12 (6.6) |
| 7–10 | 0 (0) |
| Dizziness | |
| 0 | 159 (88.3) |
| 1–3 | 12 (6.7) |
| 4–6 | 9 (5) |
| 7–10 | 0 (0) |
Patients satisfaction on postoperative pain management
Six point seven percent of the patients were extremely dissatisfied with the pain management they received while 31.1% of them were extremely satisfied. The remaining patients were moderately satisfied with pain management. The majority (86.7%) of the patients were not allowed to participate in their pain management decisions. The analgesic prescription was mostly 80.7% was done by the surgeon while the rest were performed by an anesthetist and a nurse Table 5.
Table 5.
Patients satisfaction on pain management in the first 24 h postoperatively.
| Category | Frequency (%) | |
|---|---|---|
| Pain relief | 0% (no relief) | 51 (28.3) |
| 10–30 (mild relief) | 71 (39.4) | |
| 40–60 (moderate relief) | 45 (25) | |
| 70–100 (complete relief) | 13 (7.3) | |
| Patients allowed to participate in pain management decision | 0 not at all | 156 (86.7) |
| 1–3 | 20 (11.1) | |
| 4–6 | 4 (2.2) | |
| 7–10 very much | 0 (0) | |
| Satisfaction | 0 extremely dissatisfied | 12 (6.7) |
| 1–3 dissatisfied | 45 (25) | |
| 4–6 satisfied | 67 (37.2) | |
| 7–10 extremely satisfied | 56 (31.1) | |
| Asked about pain relief | Never | 23 (12.8) |
| Sometimes | 46 (25.6) | |
| Often | 78 (43.3) | |
| Always | 33 (18.3) | |
| Information given to patients about pain relive stratagem | 0 no information given | 92 (51.2) |
| 1–3 some given | 54 (30) | |
| 4–6 | 17 (9.4) | |
| 7–10 adequate given | 17 (9.4) | |
| Pain control type | Pain pills | 14 (7.8) |
| Pain injections IM | 35 (19.4) | |
| Pain injections IV | 118 (65.6) | |
| Peripheral nerve block | 13 (7.2) | |
| Level of pain | Less than expected | 29 (16.1) |
| As expected | 94 (52.2) | |
| More than expected | 57 (31.7) | |
| Analgesics prescribed by | Surgeon | 145 (80.6) |
| Anesthetist | 24 (13.3) | |
| Nurse | 11 (6.1) |
Discussion
This study aimed to assess the prevalence of postoperative pain in the first 72 h, determine the intensity of postoperative pain in the first 72 h, and assess overall patient satisfaction with postoperative pain management. The majority of patients (more than 75%) of the patients experienced moderate to severe pain in the first 72 h after surgery. The prevalence of pain ranged in different hours; pain intensity was the most severe in the 8 h with 45.6% of the patients experiencing a pain score of 7–10 NRS. The pain showed a decrease in intensity over the 72 h period.
The prevalence of pain was lower than that reported in other studies conducted in Ethiopia. Woldehaimano used a cross-sectional study to describe the processes and outcomes of pain management among 252 patients at Jimma University Hospital found that prevalence of 91.4% postoperative pain and 80.1% of the patients were undertreated8. The other a hospital-based cross-sectional study (n=150) performed at Gonder University Hospital found a prevalence of 57 and 78% moderate-to-severe pain immediate postoperative period (2 h after the end of surgery) and in the first 12 h, respectively11. A recent longitudinal study evaluating the quality of postoperative pain management in Jimma University Hospital reported prevalence of 88.2% moderate to moderate-to-severe postoperative pain, and in 58.4% of these patients, pain was inadequately treated7. Difference in the prevalence of pain could arise from the different pain management practices in these hospitals.
The prevalence of severe pain was highest at the 4 43.9% and 8 h 45.6%, patients mostly experienced mild to moderate pain in the first 4 h. The prevalence of severe pain decreased in the 12 h (28.9%) and increased back in the 24 h (39.4%), but there was a significant decline in the 48 (10.5%) and 72 h (13.4%). The probable cause of this pattern could be analgesics administered during the intraoperative and recovery periods. This pattern of pain progression with-in 72 h after surgery was also observed in a study conducted by G Mwaka in Nairobi 201316.
Acute postoperative pain that is not appropriately managed has multiple short-term and long-term consequences. The short-term effects include physical limitation, emotional status, and mood disturbance, whereas the long-term effects include morbidity, development of chronic postoperative pain, impaired recovery from surgery, prolonged opioid use, and increased medical costs3.
In this study, we assessed the short-term effects of postoperative pain on the physical activity, emotional response, and mood of patients. From physical status, walking ability, coughing, and breathing were the most affected parameters, with 67.8 and 13.3% of the patients complaining complete interference with their walking, cough, and breathing ability. Postoperative pain did not appear to have a significant effect on the emotional status of the patient, with most of the patients feeling no anxiety, depression, fright, or helplessness with percentage of 86.7, 93.9, 93.9, and 96.7%, respectively.
Pain management satisfaction of patients at the 24 h after operation at was assessed, and 68.3% of the patients felt satisfied, while 6.7% of the patients were extremely dissatisfied. This is similar to a study conducted by Yosef Belay Bizuneh in Gonder 2020, with 72% patient satisfaction with their postoperative pain management17.
Limitation
The study had a small sample size to identify the actual prevalence of postoperative pain.
Conclusion
The prevalence of moderate to severe pain within 72 h postoperatively was slightly lower than that in other studies conducted in Ethiopia. This was still high, indicating better pain management in the postoperative period. Involvement of anesthetists in pain management is crucial for better patient management.
Ethical considerations
Ethical approval was obtained from institutional review board. Official support letters were written. The purpose and importance of the study were explained and written informed consent was obtained from each participant. Confidentiality was maintained at all levels of the study by avoiding using codes to identify patients. The patients were also informed about their right to withdraw from the study at any time without giving any reason and that the withdrawal would not affect their treatment.
Consent for publication
Written informed consent was obtained from the patient for publication and any accompanying
images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
The researchers did not receive any funding.
Author contribution
S.T.: wrote the proposal, manuscript, and cover letter; drafted the questionnaire; assessed the data quality; and was also involved in the analysis and data presentation; A.B.: wrote the proposal, manuscript, prepared figures and tables, and was involved in data analysis; F.S.: prepared figures and tables that were involved in the data presentation and assessed data quality. All authors reviewed the manuscript and cover letter.
Conflicts of interests disclosures
There are no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Research registration unique identifying number (UIN)
Name of the registry: clinicaltrials.
Unique identifying number or registration ID: NCT06065683.
Hyperlink to your specific registration: https://register.clinicaltrials.gov/prs/app/action/SelectProtocol?sid=S000DIBI&selectaction=Edit&uid=U0006LYC&ts=2&cx=p8s2n4.
Guarantor
Sara Timerga.
Availability data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files, Supplemental Digital Content 1, http://links.lww.com/MS9/A353).
Provenance and peer review
This paper is not invited.
Supplementary Material
Acknowledgement
The authors would like to extend our appreciation to our colleague and others who participated in the preparation of this proposal by providing constructive comments and editorial advice starting with title selection.
Finally, we would like to thank the authors and researchers for the valuable works we have read and cited.
Footnotes
The corresponding author of this manuscript is Sara Timerga and the co-authors are Aynalem Befkadu and Fetene Seyoum. We confirm that this work is original work and has not been published elsewhere, nor is currently under consideration for publication elsewhere.
Name and contact address of investigators: Sara Timerga: (MSc in advanced clinical anesthesia) PI, E-mail: sara24tn@gmail.com. Tel.: +251 925 044 807. Aynalem Befkadu: (MSc in advanced clinical anesthesia), E-mail: aynalembefkadu31@gmail.com Tel.: +251 916 583 316. Fetene Seyoum: (MSc in advanced clinical anesthesia), E-mail: fetseyo@gmail.com Tel.: +251 910 941 716.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 22 January 2024
Contributor Information
Sara Timerga, Email: sara24tn@gmail.com.
Aynalem Befkadu, Email: aynalembefkadu31@mail.com.
Fetene Seyoum, Email: fetseyo@gmail.com.
References
- 1.Weiser TG, Haynes AB, Molina G, et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ 2016;94:201–9F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andres J, Pogatzki-Zahn E, Huygen F, et al. Controlling acute pain to improve the quality of postoperative pain management: an update from the European Society of Regional Anesthesia meeting held in Maastricht (September 2016). Pain Manag 2017;7:513–522. [DOI] [PubMed] [Google Scholar]
- 3.Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 2017;10:2287–2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haile M, Desalegn N, Akalu L. Practice of regional anesthesia and analgesia in Ethiopian hospital. Int J Med Med Sci 2015;7:130–138. [Google Scholar]
- 5.Menlah A, Garti I, Amoo SA, et al. Knowledge, attitudes, and practices of postoperative pain management by nurses in selected district hospitals in Ghana. SAGE Open Nurs 2018;4:2377960818790383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mwashambwa MY, Yongolo IM, Kapalata SNw, et al. Post-operative pain prevalence, predictors, management practices and satisfaction among operated cases at a Regional Referral Hospital in Dar es Salaam, Tanzania. Tanzania J Health Res 2018;20:768–776. [Google Scholar]
- 7.Eshete MT, Baeumler PI, Siebeck M, et al. Quality of postoperative pain management in Ethiopia: a prospective longitudinal study. PLoS ONE 2019;14:e0215563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woldehaimanot TE, Eshetie TC, Kerie MW. Postoperative pain management among surgically treated patients in an Ethiopian hospital. PLoS ONE 2014;9:e102835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Apfelbaum JL, Chen C, Mehta SS, et al. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesthesia Anal 2003;97:534–540. [DOI] [PubMed] [Google Scholar]
- 10.Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American pain society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain 2016;17:131–157. [DOI] [PubMed] [Google Scholar]
- 11.Admasu W, Hailekiros A, Abdissa Z. Severity and risk factors of post-operative pain in university of gondar hospital, Northeast Ethiopa. J Anesth Clin Res 2016;7:675. [Google Scholar]
- 12.Sommer M, de Rijke JM, van Kleef M, et al. Predictors of acute postoperative pain after elective surgery. Clin J Pain 2010;26:87–94. [DOI] [PubMed] [Google Scholar]
- 13.Yang MM, Hartley RL, Leung AA, et al. Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ Open 2019;9:e025091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breivik H, Borchgrevink P, Allen S, et al. Assessment of pain. Br J Anaesth 2008;101:17–24. [DOI] [PubMed] [Google Scholar]
- 15.Mathew G, Agha R, Albrecht J, et al. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 2021;96:106165. [DOI] [PubMed] [Google Scholar]
- 16.Mwaka G, Thikra S, Mung’ayi V. The prevalence of postoperative pain in the first 48 hours following day surgery at a tertiary hospital in Nairobi. Afr Health Sci 2013;13:768–776; PubMed PMID: 24250320. Pubmed Central PMCID: PMC3824427. Epub 2013/11/20. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Belay Bizuneh Y, Fitiwi Lema G, Yilkal Fentie D, et al. Assessment of patient’s satisfaction and associated factors regarding postoperative pain management at the University of Gondar compressive specialized hospital, Northwest Ethiopia. Pain Res Manag 2020;2020:8834807. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


